Is Curcumin Intake Really Effective for Chronic Inflammatory Metabolic Disease? A Review of Meta-Analyses of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Identification and Selection of Studies
3.2. Inflammatory Markers
3.3. Antioxidant Effects
3.4. Glucose Control
3.5. Lipid Profiles
3.6. Body Weight, Body Mass Index, and Waist Circumference
3.7. Blood Pressure and Endothelial Function
3.8. Depression and Cognitive Function
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bernell, S.; Howard, S.W. Use Your Words Carefully: What Is a Chronic Disease? Front. Public Health 2016, 4, 159. [Google Scholar] [CrossRef]
- Vos, T.; Barber, R.M.; Bell, B.; Bertozzi Villa, A.; Biryukov, S.; Bolliger, I.; Charlson, F.; Davis, A.; Degenhardt, L.; Dicker, D. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 743–800. [Google Scholar] [CrossRef]
- Kimokoti, R.W.; Millen, B.E. Nutrition for the prevention of chronic diseases. Med. Clin. 2016, 100, 1185–1198. [Google Scholar] [CrossRef]
- Reynolds, L.M.; Zamora, C.; Lee, U.J.; Stokes, A.C.; Benjamin, E.J.; Bhatnagar, A.; Payne, T.J.; Rodriguez, C.J. Tobacco use prevalence and transitions from 2013 to 2018 among adults with a history of cardiovascular disease. J. Am. Heart Assoc. 2021, 10, e021118. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary behavior, exercise, and cardiovascular health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef]
- Nugent, R. Preventing and managing chronic diseases. BMJ 2019, 364, l459. [Google Scholar] [CrossRef]
- Furman, D.; Campisi, J.; Verdin, E.; Carrera-Bastos, P.; Targ, S.; Franceschi, C.; Ferrucci, L.; Gilroy, D.W.; Fasano, A.; Miller, G.W. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 2019, 25, 1822–1832. [Google Scholar] [CrossRef] [PubMed]
- Allison, D.J.; Ditor, D.S. The common inflammatory etiology of depression and cognitive impairment: A therapeutic target. J. Neuroinflammation 2014, 11, 151. [Google Scholar] [CrossRef] [PubMed]
- Guo, Q.; Jin, Y.; Chen, X.; Ye, X.; Shen, X.; Lin, M.; Zeng, C.; Zhou, T.; Zhang, J. NF-κB in biology and targeted therapy: New insights and translational implications. Signal Transduct. Target. Ther. 2024, 9, 53. [Google Scholar] [CrossRef]
- Lestari, M.L.; Indrayanto, G. Curcumin. Profiles DrugSubst. Excip. Relat. Methodol. 2014, 39, 113–204. [Google Scholar]
- Vogel, H.; Pelletier, J. Curcumin-biological and medicinal properties. J. Pharma 1815, 2, 24–29. [Google Scholar]
- Prasad, S.; Gupta, S.C.; Tyagi, A.K.; Aggarwal, B.B. Curcumin, a component of golden spice: From bedside to bench and back. Biotechnol. Adv. 2014, 32, 1053–1064. [Google Scholar] [CrossRef]
- Anamika, B. Extraction of curcumin. J. Environ. Sci. Toxicol. Food Technol. 2012, 1, 1–16. [Google Scholar]
- Goel, A.; Kunnumakkara, A.B.; Aggarwal, B.B. Curcumin as “Curecumin”: From kitchen to clinic. Biochem. Pharmacol. 2008, 75, 787–809. [Google Scholar] [CrossRef]
- Anand, P.; Kunnumakkara, A.B.; Newman, R.A.; Aggarwal, B.B. Bioavailability of curcumin: Problems and promises. Mol. Pharm. 2007, 4, 807–818. [Google Scholar] [CrossRef]
- Priyadarsini, K.I.; Maity, D.K.; Naik, G.; Kumar, M.S.; Unnikrishnan, M.; Satav, J.; Mohan, H. Role of phenolic OH and methylene hydrogen on the free radical reactions and antioxidant activity of curcumin. Free. Radic. Biol. Med. 2003, 35, 475–484. [Google Scholar] [CrossRef]
- Jayaraj, R.L.; Tamilselvam, K.; Manivasagam, T.; Elangovan, N. Neuroprotective effect of CNB-001, a novel pyrazole derivative of curcumin on biochemical and apoptotic markers against rotenone-induced SK-N-SH cellular model of Parkinson’s disease. J. Mol. Neurosci. 2013, 51, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Meng, B.; Li, J.; Cao, H. Antioxidant and antiinflammatory activities of curcumin on diabetes mellitus and its complications. Curr. Pharm. Des. 2013, 19, 2101–2113. [Google Scholar] [PubMed]
- Aggarwal, B.B.; Harikumar, K.B. Potential therapeutic effects of curcumin, the anti-inflammatory agent, against neurodegenerative, cardiovascular, pulmonary, metabolic, autoimmune and neoplastic diseases. Int. J. Biochem. Cell Biol. 2009, 41, 40–59. [Google Scholar] [CrossRef]
- He, Y.; Yue, Y.; Zheng, X.; Zhang, K.; Chen, S.; Du, Z. Curcumin, inflammation, and chronic diseases: How are they linked? Molecules 2015, 20, 9183–9213. [Google Scholar] [CrossRef]
- Blagov, A.V.; Summerhill, V.I.; Sukhorukov, V.N.; Zhigmitova, E.B.; Postnov, A.Y.; Orekhov, A.N. Potential use of antioxidants for the treatment of chronic inflammatory diseases. Front. Pharmacol. 2024, 15, 1378335. [Google Scholar] [CrossRef]
- Qiu, L.; Gao, C.; Li, J. Effects of dietary polyphenol curcumin supplementation on metabolic, inflammatory, and oxidative stress indices in patients with metabolic syndrome: A systematic review and meta-analysis of randomized controlled trials. Front. Endocrinol. 2023, 14, 1216708. [Google Scholar] [CrossRef] [PubMed]
- Osali, A. Aerobic exercise and nano-curcumin supplementation improve inflammation in elderly females with metabolic syndrome. Diabetol. Metab. Syndr. 2020, 12, 26. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Hosseini, M.S.; Khalili, N.; Naimi, E.; Simental-Mendía, L.E.; Majeed, M.; Sahebkar, A. Effects of curcumin on serum cytokine concentrations in subjects with metabolic syndrome: A post-hoc analysis of a randomized controlled trial. Biomed. Pharmacother. 2016, 82, 578–582. [Google Scholar] [CrossRef] [PubMed]
- Amin, F.; Islam, N.; Anila, N.; Gilani, A. Clinical efficacy of the co-administration of Turmeric and Black seeds (Kalongi) in metabolic syndrome–A double blind randomized controlled trial–TAK-MetS trial. Complement. Ther. Med. 2015, 23, 165–174. [Google Scholar] [CrossRef]
- Bateni, Z.; Behrouz, V.; Rahimi, H.R.; Hedayati, M.; Afsharian, S.; Sohrab, G. Effects of nano-curcumin supplementation on oxidative stress, systemic inflammation, adiponectin, and NF-κB in patients with metabolic syndrome: A randomized, double-blind clinical trial. J. Herb. Med. 2022, 31, 100531. [Google Scholar] [CrossRef]
- Panahi, Y.; Hosseini, M.S.; Khalili, N.; Naimi, E.; Majeed, M.; Sahebkar, A. Antioxidant and anti-inflammatory effects of curcuminoid-piperine combination in subjects with metabolic syndrome: A randomized controlled trial and an updated meta-analysis. Clin. Nutr. 2015, 34, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Dehzad, M.J.; Ghalandari, H.; Nouri, M.; Askarpour, M. Effects of curcumin/turmeric supplementation on obesity indices and adipokines in adults: A grade-assessed systematic review and dose–response meta-analysis of randomized controlled trials. Phytother. Res. 2023, 37, 1703–1728. [Google Scholar] [CrossRef] [PubMed]
- Funamoto, M.; Shimizu, K.; Sunagawa, Y.; Katanasaka, Y.; Miyazaki, Y.; Kakeya, H.; Yamakage, H.; Satoh-Asahara, N.; Wada, H.; Hasegawa, K. Effects of highly absorbable curcumin in patients with impaired glucose tolerance and non-insulin-dependent diabetes mellitus. J. Diabetes Res. 2019, 2019, 8208237. [Google Scholar] [CrossRef]
- Campbell, M.S.; Ouyang, A.; Krishnakumar, I.; Charnigo, R.J.; Westgate, P.M.; Fleenor, B.S. Influence of enhanced bioavailable curcumin on obesity-associated cardiovascular disease risk factors and arterial function: A double-blinded, randomized, controlled trial. Nutrition 2019, 62, 135–139. [Google Scholar] [CrossRef]
- Chuengsamarn, S.; Rattanamongkolgul, S.; Phonrat, B.; Tungtrongchitr, R.; Jirawatnotai, S. Reduction of atherogenic risk in patients with type 2 diabetes by curcuminoid extract: A randomized controlled trial. J. Nutr. Biochem. 2014, 25, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Ismail, N.A.; Ragab, S.; El-Baky, A.; Hamed, M.; Ibrahim, A. Effect of oral curcumin administration on insulin resistance, serum resistin and fetuin-A in obese children: Randomized placebo-controlled study. Res. J. Pharm. Biol. Chem. Sci. 2014, 5, 887–896. [Google Scholar]
- Lopresti, A.L.; Maes, M.; Meddens, M.J.; Maker, G.L.; Arnoldussen, E.; Drummond, P.D. Curcumin and major depression: A randomised, double-blind, placebo-controlled trial investigating the potential of peripheral biomarkers to predict treatment response and antidepressant mechanisms of change. Eur. Neuropsychopharmacol. 2015, 25, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Mirhafez, S.R.; Farimani, A.R.; Dehhabe, M.; Bidkhori, M.; Hariri, M.; Ghouchani, B.F.N.M.; Abdollahi, F. Effect of phytosomal curcumin on circulating levels of adiponectin and leptin in patients with non-alcoholic fatty liver disease: A randomized, double-blind, placebo-controlled clinical trial. J. Gastrointest. Liver Dis. 2019, 28, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Navekar, R.; Rafraf, M.; Ghaffari, A.; Asghari-Jafarabadi, M.; Khoshbaten, M. Turmeric supplementation improves serum glucose indices and leptin levels in patients with nonalcoholic fatty liver diseases. J. Am. Coll. Nutr. 2017, 36, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Hosseini, M.S.; Khalili, N.; Naimi, E.; Soflaei, S.S.; Majeed, M.; Sahebkar, A. Effects of supplementation with curcumin on serum adipokine concentrations: A randomized controlled trial. Nutrition 2016, 32, 1116–1122. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, A.; Selvarajan, S.; Kamalanathan, S.; Kadhiravan, T.; Prasanna Lakshmi, N.C.; Adithan, S. Effect of Curcuma longa on vascular function in native Tamilians with type 2 diabetes mellitus: A randomized, double-blind, parallel arm, placebo-controlled trial. Phytother. Res. 2019, 33, 1898–1911. [Google Scholar] [CrossRef] [PubMed]
- Adibian, M.; Hodaei, H.; Nikpayam, O.; Sohrab, G.; Hekmatdoost, A.; Hedayati, M. The effects of curcumin supplementation on high-sensitivity C-reactive protein, serum adiponectin, and lipid profile in patients with type 2 diabetes: A randomized, double-blind, placebo-controlled trial. Phytother. Res. 2019, 33, 1374–1383. [Google Scholar] [CrossRef]
- Chuengsamarn, S.; Rattanamongkolgul, S.; Luechapudiporn, R.; Phisalaphong, C.; Jirawatnotai, S. Curcumin extract for prevention of type 2 diabetes. Diabetes Care 2012, 35, 2121–2127. [Google Scholar] [CrossRef]
- Kalhori, A.; Rafraf, M.; Navekar, R.; Ghaffari, A.; Jafarabadi, M.A. Effect of turmeric supplementation on blood pressure and serum levels of sirtuin 1 and adiponectin in patients with nonalcoholic fatty liver disease: A double-blind, randomized, placebo-controlled trial. Prev. Nutr. Food Sci. 2022, 27, 37. [Google Scholar] [CrossRef]
- Salahshooh, M.M.; Parizadeh, S.M.R.; Pasdar, A.; Saberi Karimian, M.; Safarian, H.; Javandoost, A.; Ferns, G.A.; Ghayour-Mobarhan, M.; Sahebkar, A. The effect of curcumin (Curcuma longa L.) on circulating levels of adiponectin in patients with metabolic syndrome. Comp. Clin. Pathol. 2017, 26, 17–23. [Google Scholar] [CrossRef]
- Dehzad, M.J.; Ghalandari, H.; Nouri, M.; Askarpour, M. Antioxidant and anti-inflammatory effects of curcumin/turmeric supplementation in adults: A GRADE-assessed systematic review and dose–response meta-analysis of randomized controlled trials. Cytokine 2023, 164, 156144. [Google Scholar] [CrossRef] [PubMed]
- Alizadeh, F.; Javadi, M.; Karami, A.A.; Gholaminejad, F.; Kavianpour, M.; Haghighian, H.K. Curcumin nanomicelle improves semen parameters, oxidative stress, inflammatory biomarkers, and reproductive hormones in infertile men: A randomized clinical trial. Phytother. Res. 2018, 32, 514–521. [Google Scholar] [CrossRef] [PubMed]
- Jacob, J.; Amalraj, A.; Raj, K.J.; Divya, C.; Kunnumakkara, A.B.; Gopi, S. A novel bioavailable hydrogenated curcuminoids formulation (CuroWhite™) improves symptoms and diagnostic indicators in rheumatoid arthritis patients-A randomized, double blind and placebo controlled study. J. Tradit. Complement. Med. 2019, 9, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Kocher, A.; Bohnert, L.; Schiborr, C.; Frank, J. Highly bioavailable micellar curcuminoids accumulate in blood, are safe and do not reduce blood lipids and inflammation markers in moderately hyperlipidemic individuals. Mol. Nutr. Food Res. 2016, 60, 1555–1563. [Google Scholar] [CrossRef] [PubMed]
- Nieman, D.C.; Cialdella-Kam, L.; Knab, A.M.; Shanely, R.A. Influence of red pepper spice and turmeric on inflammation and oxidative stress biomarkers in overweight females: A metabolomics approach. Plant Foods Hum. Nutr. 2012, 67, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Uchio, R.; Muroyama, K.; Okuda-Hanafusa, C.; Kawasaki, K.; Yamamoto, Y.; Murosaki, S. Hot water extract of Curcuma longa L. improves serum inflammatory markers and general health in subjects with overweight or prehypertension/mild hypertension: A randomized, double-blind, placebo-controlled trial. Nutrients 2019, 11, 1822. [Google Scholar] [CrossRef] [PubMed]
- Abdolahi, M.; Sarraf, P.; Javanbakht, M.H.; Honarvar, N.M.; Hatami, M.; Soveyd, N.; Tafakhori, A.; Sedighiyan, M.; Djalali, M.; Jafarieh, A. A novel combination of ω-3 fatty acids and nano-curcumin modulates interleukin-6 gene expression and high sensitivity C-reactive protein serum levels in patients with migraine: A randomized clinical trial study. CNS Neurol. Disord.-Drug Targets (Former. Curr. Drug Targets-CNS Neurol.Disord.) 2018, 17, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Adab, Z.; Eghtesadi, S.; Vafa, M.R.; Heydari, I.; Shojaii, A.; Haqqani, H.; Arablou, T.; Eghtesadi, M. Effect of turmeric on glycemic status, lipid profile, hs-CRP, and total antioxidant capacity in hyperlipidemic type 2 diabetes mellitus patients. Phytother. Res. 2019, 33, 1173–1181. [Google Scholar] [CrossRef]
- Jazayeri-Tehrani, S.A.; Rezayat, S.M.; Mansouri, S.; Qorbani, M.; Alavian, S.M.; Daneshi-Maskooni, M.; Hosseinzadeh-Attar, M.-J. Nano-curcumin improves glucose indices, lipids, inflammation, and Nesfatin in overweight and obese patients with non-alcoholic fatty liver disease (NAFLD): A double-blind randomized placebo-controlled clinical trial. Nutr. Metab. 2019, 16, 8. [Google Scholar] [CrossRef]
- Mirzabeigi, P.; Mohammadpour, A.H.; Salarifar, M.; Gholami, K.; Mojtahedzadeh, M.; Javadi, M.R. The effect of curcumin on some of traditional and non-traditional cardiovascular risk factors: A pilot randomized, double-blind, placebo-controlled trial. Iran. J. Pharm.Res. IJPR 2015, 14, 479. [Google Scholar]
- Mohammadi, A.; Sahebkar, A.; Iranshahi, M.; Amini, M.; Khojasteh, R.; Ghayour-Mobarhan, M.; Ferns, G.A. Effects of supplementation with curcuminoids on dyslipidemia in obese patients: A randomized crossover trial. Phytother. Res. 2013, 27, 374–379. [Google Scholar] [CrossRef]
- Pakfetrat, M.; Basiri, F.; Malekmakan, L.; Roozbeh, J. Effects of turmeric on uremic pruritus in end stage renal disease patients: A double-blind randomized clinical trial. J. Nephrol. 2014, 27, 203–207. [Google Scholar] [CrossRef]
- Rahimnia, A.-R.; Panahi, Y.; Alishiri, G.; Sharafi, M.; Sahebkar, A. Impact of supplementation with curcuminoids on systemic inflammation in patients with knee osteoarthritis: Findings from a randomized double-blind placebo-controlled trial. Drug Res. 2014, 65, 521–525. [Google Scholar] [CrossRef] [PubMed]
- Saadati, S.; Sadeghi, A.; Mansour, A.; Yari, Z.; Poustchi, H.; Hedayati, M.; Hatami, B.; Hekmatdoost, A. Curcumin and inflammation in non-alcoholic fatty liver disease: A randomized, placebo controlled clinical trial. BMC Gastroenterol. 2019, 19, 133. [Google Scholar] [CrossRef]
- Sadeghi, N.; Mansoori, A.; Shayesteh, A.; Hashemi, S.J. The effect of curcumin supplementation on clinical outcomes and inflammatory markers in patients with ulcerative colitis. Phytother. Res. 2020, 34, 1123–1133. [Google Scholar] [CrossRef] [PubMed]
- Maithili Karpaga Selvi, N.; Sridhar, M.; Swaminathan, R.; Sripradha, R. Efficacy of turmeric as adjuvant therapy in type 2 diabetic patients. Indian J. Clin. Biochem. 2015, 30, 180–186. [Google Scholar] [CrossRef]
- Sohaei, S.; Amani, R.; Tarrahi, M.J.; Ghasemi-Tehrani, H. The effects of curcumin supplementation on glycemic status, lipid profile and hs-CRP levels in overweight/obese women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled clinical trial. Complement. Ther. Med. 2019, 47, 102201. [Google Scholar] [CrossRef] [PubMed]
- Tamaddoni, A.; Nasseri, E.; Mohammadi, E.; Qujeq, D.; Zayeri, F.; Zand, H.; Mir, S.M.; Gholami, M. A double-blind randomized controlled trial of curcumin for improvement in glycemic status, lipid profile and systemic inflammation in β-thalassemia major. J. Herb. Med. 2020, 21, 100324. [Google Scholar] [CrossRef]
- Panahi, Y.; Khalili, N.; Sahebi, E.; Namazi, S.; Simental-Mendía, L.E.; Majeed, M.; Sahebkar, A. Effects of curcuminoids plus piperine on glycemic, hepatic and inflammatory biomarkers in patients with type 2 diabetes mellitus: A randomized double-blind placebo-controlled trial. Drug Res. 2018, 68, 403–409. [Google Scholar] [CrossRef]
- Saberi-Karimian, M.; Parizadeh, S.M.R.; Ghayour-Mobarhan, M.; Salahshooh, M.M.; Dizaji, B.F.; Safarian, H.; Javandoost, A.; Ferns, G.A.; Sahebkar, A.; Ahmadinejad, M. Evaluation of the effects of curcumin in patients with metabolic syndrome. Comp. Clin. Pathol. 2018, 27, 555–563. [Google Scholar] [CrossRef]
- DiSilvestro, R.A.; Joseph, E.; Zhao, S.; Bomser, J. Diverse effects of a low dose supplement of lipidated curcumin in healthy middle aged people. Nutr. J. 2012, 11, 79. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Ghanei, M.; Bashiri, S.; Hajihashemi, A.; Sahebkar, A. Short-term curcuminoid supplementation for chronic pulmonary complications due to sulfur mustard intoxication: Positive results of a randomized double-blind placebo-controlled trial. Drug Res. 2014, 65, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Saadat, A.; Beiraghdar, F.; Sahebkar, A. Adjuvant therapy with bioavailability-boosted curcuminoids suppresses systemic inflammation and improves quality of life in patients with solid tumors: A randomized double-blind placebo-controlled trial. Phytother. Res. 2014, 28, 1461–1467. [Google Scholar] [CrossRef] [PubMed]
- Funamoto, M.; Sunagawa, Y.; Katanasaka, Y.; Miyazaki, Y.; Imaizumi, A.; Kakeya, H.; Yamakage, H.; Satoh-Asahara, N.; Komiyama, M.; Wada, H. Highly absorptive curcumin reduces serum atherosclerotic low-density lipoprotein levels in patients with mild COPD. Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 2029–2034. [Google Scholar]
- Santos-Parker, J.R.; Strahler, T.R.; Bassett, C.J.; Bispham, N.Z.; Chonchol, M.B.; Seals, D.R. Curcumin supplementation improves vascular endothelial function in healthy middle-aged and older adults by increasing nitric oxide bioavailability and reducing oxidative stress. Aging 2017, 9, 187. [Google Scholar] [CrossRef] [PubMed]
- Shao, N.; Jia, H.; Li, Y.; Li, J. Curcumin improves treatment outcome of Takayasu arteritis patients by reducing TNF-α: A randomized placebo-controlled double-blind clinical trial. Immunol. Res. 2017, 65, 969–974. [Google Scholar] [CrossRef] [PubMed]
- Ghaffari, A.; Rafraf, M.; Navekar, R.; Asghari-Jafarabadi, M. Effects of turmeric and chicory seed supplementation on antioxidant and inflammatory biomarkers in patients with non-alcoholic fatty liver disease (NAFLD). Adv. Integr. Med. 2018, 5, 89–95. [Google Scholar] [CrossRef]
- Haroyan, A.; Mukuchyan, V.; Mkrtchyan, N.; Minasyan, N.; Gasparyan, S.; Sargsyan, A.; Narimanyan, M.; Hovhannisyan, A. Efficacy and safety of curcumin and its combination with boswellic acid in osteoarthritis: A comparative, randomized, double-blind, placebo-controlled study. BMC Complement. Altern. Med. 2018, 18, 7. [Google Scholar] [CrossRef]
- Thota, R.N.; Acharya, S.H.; Garg, M.L. Curcumin and/or omega-3 polyunsaturated fatty acids supplementation reduces insulin resistance and blood lipids in individuals with high risk of type 2 diabetes: A randomised controlled trial. Lipids Health Dis. 2019, 18, 31. [Google Scholar] [CrossRef]
- Vafadar_afshar, G.; Khadem-Ansari, M.-H.; Makhdomii, K.; Rasooli, J. The effects of nano-curcumin supplementation on serum level of hs-CRP, adhesion molecules, and lipid profiles in hemodialysis patients, a randomized controlled clinical trial. Iran. J. Kidney Dis. 2020, 14, 52. [Google Scholar] [PubMed]
- Alvarenga, L.; Salarolli, R.; Cardozo, L.F.; Santos, R.S.; de Brito, J.S.; Kemp, J.A.; Reis, D.; de Paiva, B.R.; Stenvinkel, P.; Lindholm, B. Impact of curcumin supplementation on expression of inflammatory transcription factors in hemodialysis patients: A pilot randomized, double-blind, controlled study. Clin. Nutr. 2020, 39, 3594–3600. [Google Scholar] [CrossRef] [PubMed]
- Asan, S.A.; Baş, M.; Eren, B.; Karaca, E. The effects of curcumin supplementation added to diet on anthropometric and biochemical status in women with polycystic ovary syndrome: A randomized, placebo-controlled trial. Prog. Nutr. 2020, 22, e2020089. [Google Scholar]
- Atabaki, M.; Shariati-Sarabi, Z.; Tavakkol-Afshari, J.; Mohammadi, M. Significant immunomodulatory properties of curcumin in patients with osteoarthritis; a successful clinical trial in Iran. Int. Immunopharmacol. 2020, 85, 106607. [Google Scholar] [CrossRef] [PubMed]
- Kuszewski, J.C.; Wong, R.H.; Wood, L.G.; Howe, P.R. Effects of fish oil and curcumin supplementation on cerebrovascular function in older adults: A randomized controlled trial. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Shafabakhsh, R.; Asemi, Z.; Reiner, Ž.; Soleimani, A.; Aghadavod, E.; Bahmani, F. The effects of nano-curcumin on metabolic status in patients with diabetes on hemodialysis, a randomized, double blind, placebo-controlled trial. Iran. J. Kidney Dis. 2020, 14, 290–299. [Google Scholar] [PubMed]
- Shafabakhsh, R.; Mobini, M.; Raygan, F.; Aghadavod, E.; Ostadmohammadi, V.; Amirani, E.; Mansournia, M.A.; Asemi, Z. Curcumin administration and the effects on psychological status and markers of inflammation and oxidative damage in patients with type 2 diabetes and coronary heart disease. Clin. Nutr. ESPEN 2020, 40, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Darmian, M.A.; Hoseini, R.; Amiri, E.; Golshani, S. How combined and separate aerobic training and turmeric supplementation alter lipid profile and glycemic status? A clinical trial in middle-aged females with type 2 diabetes and hyperlipidemia. Int. Cardiovasc. Res. J. 2021, 15, e118791. [Google Scholar]
- Helli, B.; Gerami, H.; Kavianpour, M.; Heybar, H.; Hosseini, S.K.; Haghighian, H.K. Curcumin nanomicelle improves lipid profile, stress oxidative factors and inflammatory markers in patients undergoing coronary elective angioplasty; a randomized clinical trial. Endocr. Metab. Immune Disord.-Drug Targets (Former. Curr. Drug Targets-Immune Endocr. Metab.Disord.) 2021, 21, 2090–2098. [Google Scholar]
- Mokhtari, M.; Razzaghi, R.; Momen-Heravi, M. The effects of curcumin intake on wound healing and metabolic status in patients with diabetic foot ulcer: A randomized, double-blind, placebo-controlled trial. Phytother. Res. 2021, 35, 2099–2107. [Google Scholar] [CrossRef]
- Rodrigues, H.C.N.; Martins, T.F.P.; Braga, C.C.; Silva, M.A.C.; da Cunha, L.C.; de Araújo Sugizaki, C.S.; de Souza Freitas, A.T.V.; Costa, N.A.; Peixoto, M.d.R.G. Antioxidant and anti-inflammatory response to curcumin supplementation in hemodialysis patients: A randomized, double-blind, placebo-controlled clinical trial. Clin. Nutr. ESPEN 2021, 44, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Salehi, M.; Mashhadi, N.S.; Esfahani, P.S.; Feizi, A.; Hadi, A.; Askari, G. The effects of curcumin supplementation on muscle damage, oxidative stress, and inflammatory markers in healthy females with moderate physical activity: A randomized, double-blind, placebo-controlled clinical trial. Int. J. Prev. Med. 2021, 12, 94. [Google Scholar] [PubMed]
- Thanawala, S.; Shah, R.; Somepalli, V.; Alluri, K.V.; Desomayanandam, P.; Bhuvanendran, A. A multicenter, randomized, double-blind, placebo-controlled trial assessing efficacy and safety of a novel low-dose turmeric extract formulation in healthy adults with chronic knee pain. Clin. Pharmacol. Adv. Appl. 2021, 13, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Uchio, R.; Kawasaki, K.; Okuda-Hanafusa, C.; Saji, R.; Muroyama, K.; Murosaki, S.; Yamamoto, Y.; Hirose, Y. Curcuma longa extract improves serum inflammatory markers and mental health in healthy participants who are overweight: A randomized, double-blind, placebo-controlled trial. Nutr. J. 2021, 20, 91. [Google Scholar] [CrossRef] [PubMed]
- Varma, K.; Amalraj, A.; Divya, C.; Gopi, S. The efficacy of the novel bioavailable curcumin (cureit) in the management of sarcopenia in healthy elderly subjects: A randomized, placebo-controlled, double-blind clinical study. J. Med. Food 2021, 24, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Ganjali, S.; Sahebkar, A.; Mahdipour, E.; Jamialahmadi, K.; Torabi, S.; Akhlaghi, S.; Ferns, G.; Parizadeh, S.M.R.; Ghayour-Mobarhan, M. Investigation of the effects of curcumin on serum cytokines in obese individuals: A randomized controlled trial. Sci. World J. 2014, 2014, 898361. [Google Scholar] [CrossRef] [PubMed]
- Khajehdehi, P.; Pakfetrat, M.; Javidnia, K.; Azad, F.; Malekmakan, L.; Nasab, M.H.; Dehghanzadeh, G. Oral supplementation of turmeric attenuates proteinuria, transforming growth factor-β and interleukin-8 levels in patients with overt type 2 diabetic nephropathy: A randomized, double-blind and placebo-controlled study. Scand. J. Urol. Nephrol. 2011, 45, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Abbas, S.H.; Abdulridha, M.K.; Najeb, A.A. Potential benefit of curcumin adjuvant therapy to the standard Helicobacter pylori eradication therapy in patients with peptic ulcer disease. Asian J. Pharm. Clin. Res. 2017, 10, 313–317. [Google Scholar]
- Campbell, M.S.; Berrones, A.J.; Krishnakumar, I.; Charnigo, R.J.; Westgate, P.M.; Fleenor, B.S. Responsiveness to curcumin intervention is associated with reduced aortic stiffness in young, obese men with higher initial stiffness. J. Funct. Foods 2017, 29, 154–160. [Google Scholar] [CrossRef]
- Setiawati, M.C.N.; Ikawati, Z.; Nyoman, K. Effect of Curcuma Xanthorrhiza Roxb. Extract on TNF α concentration and depression’s score in patient with systemic lupus erythematosus. Indones J. Pharm. 2017, 28, 185–190. [Google Scholar] [CrossRef]
- Gupte, P.A.; Giramkar, S.A.; Harke, S.M.; Kulkarni, S.K.; Deshmukh, A.P.; Hingorani, L.L.; Mahajan, M.P.; Bhalerao, S.S. Evaluation of the efficacy and safety of Capsule Longvida® Optimized Curcumin (solid lipid curcumin particles) in knee osteoarthritis: A pilot clinical study. J. Inflamm. Res. 2019, 12, 145–152. [Google Scholar] [CrossRef] [PubMed]
- da Silva, T.A.; de Medeiros, D.C.; da Silva Cunha de Medeiros, R.C.; Medeiros, R.M.; de Souza, L.B.; de Medeiros, J.A.; dos Santos, R.V.; de Alcântara Varela, P.W.; Leite-Lais, L.; Dantas, P.M. Influence of curcumin on glycemic profile, inflammatory markers, and oxidative stress in HIV-infected individuals: A randomized controlled trial. Phytother. Res. 2020, 34, 2323–2330. [Google Scholar] [CrossRef] [PubMed]
- Singgih Wahono, C.; Diah Setyorini, C.; Kalim, H.; Nurdiana, N.; Handono, K. Effect of Curcuma xanthorrhiza supplementation on systemic lupus erythematosus patients with hypovitamin D which were given vitamin D 3 towards disease activity (SLEDAI), IL-6, and TGF-β1 serum. Int. J. Rheumatol. 2017, 2017, 7687053. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, M.; Hajialilo, M.; Dolati, S.; Eghbal-Fard, S.; Heydarlou, H.; Ghaebi, M.; Ghassembaglou, A.; Aghebati-Maleki, L.; Samadi Kafil, H.; Kamrani, A. The effects of nanocurcumin on Treg cell responses and treatment of ankylosing spondylitis patients: A randomized, double-blind, placebo-controlled clinical trial. J. Cell. Biochem. 2020, 121, 103–110. [Google Scholar] [CrossRef]
- Khdair, S.A.; Abdulridha, M.K.; Shafek, M.A. The effect of curcumin adjuvant therapy on pulmonary function and levels of interleukin-6 (IL-6) and superoxide dismutase-3 (EC-SOD3) in patients with chronic bronchial asthma. Indones. J. Pharm. 2021, 32, 232–240. [Google Scholar]
- Rezaie, S.; Askari, G.; Khorvash, F.; Tarrahi, M.J.; Amani, R. Effects of curcumin supplementation on clinical features and inflammation, in migraine patients: A double-blind controlled, placebo randomized clinical trial. Int. J. Prev. Med. 2021, 12, 161. [Google Scholar]
- Vafadar-Afshar, G.; Rasmi, Y.; Yaghmaei, P.; Khadem-Ansari, M.H.; Makhdoomi, K.; Rasouli, J. The effects of nanocurcumin supplementation on inflammation in hemodialysis patients: A randomized controlled trial. Hemodial. Int. 2021, 25, 232–239. [Google Scholar] [CrossRef]
- Srivastava, S.; Saksena, A.K.; Khattri, S.; Kumar, S.; Dagur, R.S. Curcuma longa extract reduces inflammatory and oxidative stress biomarkers in osteoarthritis of knee: A four-month, double-blind, randomized, placebo-controlled trial. Inflammopharmacology 2016, 24, 377–388. [Google Scholar] [CrossRef]
- Shen, W.; Qu, Y.; Jiang, H.; Wang, H.; Pan, Y.; Zhang, Y.; Wu, X.; Zhang, Y. Therapeutic effect and safety of curcumin in women with PCOS: A systematic review and meta-analysis. Front. Endocrinol. 2022, 13, 1051111. [Google Scholar] [CrossRef]
- Sun, Z.; Wei, X.; Bai, J.; Li, W.; Yang, J.; Deng, Z.; Wu, M.; Ying, T.; He, G. The effects of curcumin on anthropometric and cardiometabolic parameters of patients with metabolic related diseases: A systematic review and dose-effect meta-analysis of randomized controlled trials. Crit. Rev. Food Sci. Nutr. 2022, 63, 9282–9298. [Google Scholar] [CrossRef]
- Panahi, Y.; Khalili, N.; Sahebi, E.; Namazi, S.; Reiner, Ž.; Majeed, M.; Sahebkar, A. Curcuminoids modify lipid profile in type 2 diabetes mellitus: A randomized controlled trial. Complement. Ther. Med. 2017, 33, 1–5. [Google Scholar] [CrossRef]
- Futuhi, F.; Naghibzadeh Tahami, A.; Azmandian, J.; Saber, A. The effects of curcumin-containing supplementations on inflammatory markers and lipid profiles in patients with chronic kidney diseases: A systematic review and meta-analysis of randomized controlled trials. J. Complement. Integr. Med. 2022, 19, 531–541. [Google Scholar] [CrossRef] [PubMed]
- Samadian, F.; Dalili, N.; Gholi, F.P.-R.; Fattah, M.; Malih, N.; Nafar, M.; Firoozan, A.; Ahmadpoor, P.; Samavat, S.; Ziaie, S. Evaluation of Curcumin’s effect on inflammation in hemodialysis patients. Clin. Nutr. ESPEN 2017, 22, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Moreillon, J.J.; Bowden, R.G.; Deike, E.; Griggs, J.; Wilson, R.; Shelmadine, B.; Cooke, M.; Beaujean, A. The use of an anti-inflammatory supplement in patients with chronic kidney disease. J. Complement. Integr. Med. 2013, 10, 143–152. [Google Scholar] [CrossRef]
- Gorabi, A.M.; Abbasifard, M.; Imani, D.; Aslani, S.; Razi, B.; Alizadeh, S.; Bagheri-Hosseinabadi, Z.; Sathyapalan, T.; Sahebkar, A. Effect of curcumin on C-reactive protein as a biomarker of systemic inflammation: An updated meta-analysis of randomized controlled trials. Phytother. Res. 2022, 36, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Amalraj, A.; Varma, K.; Jacob, J.; Divya, C.; Kunnumakkara, A.B.; Stohs, S.J.; Gopi, S. A novel highly bioavailable curcumin formulation improves symptoms and diagnostic indicators in rheumatoid arthritis patients: A randomized, double-blind, placebo-controlled, two-dose, three-arm, and parallel-group study. J. Med. Food 2017, 20, 1022–1030. [Google Scholar] [CrossRef]
- Panahi, Y.; Sahebkar, A.; Parvin, S.; Saadat, A. A randomized controlled trial on the anti-inflammatory effects of curcumin in patients with chronic sulphur mustard-induced cutaneous complications. Ann. Clin. Biochem. 2012, 49, 580–588. [Google Scholar] [CrossRef]
- Phrommintikul, A.; Chanchai, R.; Wongcharoen, W. Effects of curcuminoids on myocardial injury after percutaneous coronary intervention. J. Med. Food 2019, 22, 680–684. [Google Scholar] [CrossRef]
- Saraf-Bank, S.; Ahmadi, A.; Paknahad, Z.; Maracy, M.; Nourian, M. Effects of curcumin supplementation on markers of inflammation and oxidative stress among healthy overweight and obese girl adolescents: A randomized placebo-controlled clinical trial. Phytother. Res. 2019, 33, 2015–2022. [Google Scholar] [CrossRef]
- Wongcharoen, W.; Jai-Aue, S.; Phrommintikul, A.; Nawarawong, W.; Woragidpoonpol, S.; Tepsuwan, T.; Sukonthasarn, A.; Apaijai, N.; Chattipakorn, N. Effects of curcuminoids on frequency of acute myocardial infarction after coronary artery bypass grafting. Am. J. Cardiol. 2012, 110, 40–44. [Google Scholar] [CrossRef]
- Ashtary-Larky, D.; Rezaei Kelishadi, M.; Bagheri, R.; Moosavian, S.P.; Wong, A.; Davoodi, S.H.; Khalili, P.; Dutheil, F.; Suzuki, K.; Asbaghi, O. The effects of nano-curcumin supplementation on risk factors for cardiovascular disease: A GRADE-assessed systematic review and meta-analysis of clinical trials. Antioxidants 2021, 10, 1015. [Google Scholar] [CrossRef] [PubMed]
- Abdolahi, M.; Tafakhori, A.; Togha, M.; Okhovat, A.A.; Siassi, F.; Eshraghian, M.R.; Sedighiyan, M.; Djalali, M.; Mohammadzadeh Honarvar, N.; Djalali, M. The synergistic effects of ω-3 fatty acids and nano-curcumin supplementation on tumor necrosis factor (TNF)-α gene expression and serum level in migraine patients. Immunogenetics 2017, 69, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Gorabi, A.M.; Razi, B.; Aslani, S.; Abbasifard, M.; Imani, D.; Sathyapalan, T.; Sahebkar, A. Effect of curcumin on proinflammatory cytokines: A meta-analysis of randomized controlled trials. Cytokine 2021, 143, 155541. [Google Scholar] [CrossRef] [PubMed]
- Usharani, P.; Mateen, A.; Naidu, M.; Raju, Y.; Chandra, N. Effect of NCB-02, atorvastatin and placebo on endothelial function, oxidative stress and inflammatory markers in patients with type 2 diabetes mellitus: A randomized, parallel-group, placebo-controlled, 8-week study. Drugs R D 2008, 9, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Abdelazeem, B.; Abbas, K.S.; Shehata, J.; Baral, N.; Banour, S.; Hassan, M. The effects of curcumin as dietary supplement for patients with polycystic ovary syndrome: An updated systematic review and meta-analysis of randomized clinical trials. Phytother. Res. 2022, 36, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, J.J.; Abbott, K.A.; Garg, M.L. Anti-inflammatory effects of oral supplementation with curcumin: A systematic review and meta-analysis of randomized controlled trials. Nutr. Rev. 2021, 79, 1043–1066. [Google Scholar] [CrossRef] [PubMed]
- Chainani-Wu, N.; Silverman, S., Jr.; Reingold, A.; Bostrom, A.; Mc Culloch, C.; Lozada-Nur, F.; Weintraub, J. A randomized, placebo-controlled, double-blind clinical trial of curcuminoids in oral lichen planus. Phytomedicine 2007, 14, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Cox, K.H.; Pipingas, A.; Scholey, A.B. Investigation of the effects of solid lipid curcumin on cognition and mood in a healthy older population. J. Psychopharmacol. 2015, 29, 642–651. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Khalili, N.; Sahebi, E.; Namazi, S.; Atkin, S.L.; Majeed, M.; Sahebkar, A. Curcuminoids plus piperine modulate adipokines in type 2 diabetes mellitus. Curr. Clin. Pharmacol. 2017, 12, 253–258. [Google Scholar] [CrossRef]
- Wu, S.; Xiao, D. Effect of curcumin on nasal symptoms and airflow in patients with perennial allergic rhinitis. Ann. Allergy Asthma Immunol. 2016, 117, 697–702.e691. [Google Scholar] [CrossRef]
- Soveyd, N.; Abdolahi, M.; Djalali, M.; Hatami, M.; Tafakhori, A.; Sarraf, P.; Honarvar, N.M. The combined effects of ω-3 fatty acids and nano-curcumin supplementation on intercellular adhesion molecule-1 (ICAM-1) gene expression and serum levels in migraine patients. CNS Neurol. Disord.-Drug Targets (Former. Curr. Drug Targets-CNS Neurol.Disord.) 2017, 16, 1120–1126. [Google Scholar] [CrossRef] [PubMed]
- White, C.M.; Pasupuleti, V.; Roman, Y.M.; Li, Y.; Hernandez, A.V. Oral turmeric/curcumin effects on inflammatory markers in chronic inflammatory diseases: A systematic review and meta-analysis of randomized controlled trials. Pharmacol. Res. 2019, 146, 104280. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Rahimnia, A.R.; Sharafi, M.; Alishiri, G.; Saburi, A.; Sahebkar, A. Curcuminoid treatment for knee osteoarthritis: A randomized double-blind placebo-controlled trial. Phytother. Res. 2014, 28, 1625–1631. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Khalili, N.; Sahebi, E.; Namazi, S.; Karimian, M.S.; Majeed, M.; Sahebkar, A. Antioxidant effects of curcuminoids in patients with type 2 diabetes mellitus: A randomized controlled trial. Inflammopharmacology 2017, 25, 25–31. [Google Scholar] [CrossRef]
- Tabrizi, R.; Vakili, S.; Akbari, M.; Mirhosseini, N.; Lankarani, K.B.; Rahimi, M.; Mobini, M.; Jafarnejad, S.; Vahedpoor, Z.; Asemi, Z. The effects of curcumin-containing supplements on biomarkers of inflammation and oxidative stress: A systematic review and meta-analysis of randomized controlled trials. Phytother. Res. 2019, 33, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.S.; Su, Y.F.; Yang, H.W.; Lee, Y.H.; Chou, J.I.; Ueng, K.C. Lipid-lowering effects of curcumin in patients with metabolic syndrome: A randomized, double-blind, placebo-controlled trial. Phytother. Res. 2014, 28, 1770–1777. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.C.; Ghaedi, E.; Arab, A.; Pourmasoumi, M.; Hadi, A. The effect of curcumin supplementation on circulating adiponectin: A systematic review and meta-analysis of randomized controlled trials. Diabetes Metab.Syndr. Clin. Res. Rev. 2019, 13, 2819–2825. [Google Scholar] [CrossRef] [PubMed]
- Simental-Mendia, L.E.; Cicero, A.F.; Atkin, S.L.; Majeed, M.; Sahebkar, A. A systematic review and meta-analysis of the effect of curcuminoids on adiponectin levels. Obes. Res. Clin. Pract. 2019, 13, 340–344. [Google Scholar] [CrossRef] [PubMed]
- Ismail, N.A.; Abd El Dayem, S.M.; Salama, E.; Ragab, S.; Abd El Baky, A.N.; Ezzat, W.M. Impact of curcumin intake on gluco-insulin homeostasis, leptin and adiponectin in obese subjects. Res. J. Pharm. Biol. Chem. Sci. 2016, 7, 1891–1897. [Google Scholar]
- Ohara, K.; Uchida, A.; Nagasaka, R.; Ushio, H.; Ohshima, T. The effects of hydroxycinnamic acid derivatives on adiponectin secretion. Phytomedicine 2009, 16, 130–137. [Google Scholar] [CrossRef]
- Akbari, M.; Lankarani, K.B.; Tabrizi, R.; Ghayour-Mobarhan, M.; Peymani, P.; Ferns, G.; Ghaderi, A.; Asemi, Z. The effects of curcumin on weight loss among patients with metabolic syndrome and related disorders: A systematic review and meta-analysis of randomized controlled trials. Front. Pharmacol. 2019, 10, 649. [Google Scholar] [CrossRef] [PubMed]
- Atkin, S.L.; Katsiki, N.; Derosa, G.; Maffioli, P.; Sahebkar, A. Curcuminoids lower plasma leptin concentrations: A meta-analysis. Phytother. Res. 2017, 31, 1836–1841. [Google Scholar] [CrossRef] [PubMed]
- Derosa, G.; Maffioli, P.; Simental-Mendía, L.E.; Bo, S.; Sahebkar, A. Effect of curcumin on circulating interleukin-6 concentrations: A systematic review and meta-analysis of randomized controlled trials. Pharmacol. Res. 2016, 111, 394–404. [Google Scholar] [CrossRef] [PubMed]
- Na, L.X.; Yan, B.L.; Jiang, S.; Cui, H.L.; Li, Y.; Sun, C.H. Curcuminoids target decreasing serum adipocyte-fatty acid binding protein levels in their glucose-lowering effect in patients with type 2 diabetes. Biomed. Environ. Sci. 2014, 27, 902–906. [Google Scholar] [PubMed]
- Chainani-Wu, N.; Madden, E.; Lozada-Nur, F.; Silverman, S., Jr. High-dose curcuminoids are efficacious in the reduction in symptoms and signs of oral lichen planus. J. Am. Acad. Dermatol. 2012, 66, 752–760. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.C.; Tyagi, A.K.; Deshmukh-Taskar, P.; Hinojosa, M.; Prasad, S.; Aggarwal, B.B. Downregulation of tumor necrosis factor and other proinflammatory biomarkers by polyphenols. Arch. Biochem. Biophys. 2014, 559, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Sahebkar, A.; Cicero, A.F.; Simental-Mendía, L.E.; Aggarwal, B.B.; Gupta, S.C. Curcumin downregulates human tumor necrosis factor-α levels: A systematic review and meta-analysis ofrandomized controlled trials. Pharmacol. Res. 2016, 107, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Khalili, N.; Hosseini, M.S.; Abbasinazari, M.; Sahebkar, A. Lipid-modifying effects of adjunctive therapy with curcuminoids–piperine combination in patients with metabolic syndrome: Results of a randomized controlled trial. Complement. Ther. Med. 2014, 22, 851–857. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.-J.; Pei, L.-B.; Zhang, Y.; Wen, Z.-Y.; Yang, J.-L. Chronic supplementation of curcumin enhances the efficacy of antidepressants in major depressive disorder: A randomized, double-blind, placebo-controlled pilot study. J. Clin. Psychopharmacol. 2015, 35, 406–410. [Google Scholar] [CrossRef]
- Sahebkar, A. Are curcuminoids effective C-reactive protein-lowering agents in clinical practice? Evidence from a meta-analysis. Phytother. Res. 2014, 28, 633–642. [Google Scholar] [CrossRef]
- Panahi, Y.; Sahebkar, A.; Amiri, M.; Davoudi, S.M.; Beiraghdar, F.; Hoseininejad, S.L.; Kolivand, M. Improvement of sulphur mustard-induced chronic pruritus, quality of life and antioxidant status by curcumin: Results of a randomised, double-blind, placebo-controlled trial. Br. J. Nutr. 2012, 108, 1272–1279. [Google Scholar] [CrossRef] [PubMed]
- Belcaro, G.; Cesarone, M.; Dugall, M.; Pellegrini, L.; Ledda, A.; Grossi, M.; Togni, S.; Appendino, G. Product-evaluation registry of Meriva®, a curcumin-phosphatidylcholine complex, for the complementary management of osteoarthritis. Panminerva Med. 2010, 52, 55–62. [Google Scholar] [PubMed]
- Nasseri, E.; Mohammadi, E.; Tamaddoni, A.; Qujeq, D.; Zayeri, F.; Zand, H. Benefits of curcumin supplementation on antioxidant status in β-Thalassemia major patients: A double-blind randomized controlled clinical trial. Ann. Nutr. Metab. 2018, 71, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Hodaei, H.; Adibian, M.; Nikpayam, O.; Hedayati, M.; Sohrab, G. The effect of curcumin supplementation on anthropometric indices, insulin resistance and oxidative stress in patients with type 2 diabetes: A randomized, double-blind clinical trial. Diabetol. Metab. Syndr. 2019, 11, 41. [Google Scholar] [CrossRef] [PubMed]
- Hejazi, J.; Rastmanesh, R.; Taleban, F.-A.; Molana, S.-H.; Hejazi, E.; Ehtejab, G.; Hara, N. Effect of curcumin supplementation during radiotherapy on oxidative status of patients with prostate cancer: A double blinded, randomized, placebo-controlled study. Nutr. Cancer 2016, 68, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Jarhahzadeh, M.; Alavinejad, P.; Farsi, F.; Husain, D.; Rezazadeh, A. The effect of turmeric on lipid profile, malondialdehyde, liver echogenicity and enzymes among patients with nonalcoholic fatty liver disease: A randomized double blind clinical trial. Diabetol. Metab. Syndr. 2021, 13, 112. [Google Scholar] [CrossRef] [PubMed]
- Heshmati, J.; Golab, F.; Morvaridzadeh, M.; Potter, E.; Akbari-Fakhrabadi, M.; Farsi, F.; Tanbakooei, S.; Shidfar, F. The effects of curcumin supplementation on oxidative stress, Sirtuin-1 and peroxisome proliferator activated receptor γ coactivator 1α gene expression in polycystic ovarian syndrome (PCOS) patients: A randomized placebo-controlled clinical trial. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Jakubczyk, K.; Drużga, A.; Katarzyna, J.; Skonieczna-Żydecka, K. Antioxidant potential of curcumin—A meta-analysis of randomized clinical trials. Antioxidants 2020, 9, 1092. [Google Scholar] [CrossRef] [PubMed]
- Mohajer, A.; Ghayour-Mobarhan, M.; Parizadeh, S.M.R.; Tavallaie, S.; Rajabian, M.; Sahebkar, A. Effects of supplementation with curcuminoids on serum copper and zinc concentrations and superoxide dismutase enzyme activity in obese subjects. Trace Elem. Electrolytes 2014, 32, 16–21. [Google Scholar] [CrossRef]
- Alizadeh, M.; Kheirouri, S. Curcumin reduces malondialdehyde and improves antioxidants in humans with diseased conditions: A comprehensive meta-analysis of randomized controlled trials. BioMedicine 2019, 9, 23. [Google Scholar] [CrossRef]
- Jiménez-Osorio, A.S.; García-Niño, W.R.; González-Reyes, S.; Álvarez-Mejía, A.E.; Guerra-León, S.; Salazar-Segovia, J.; Falcón, I.; de Oca-Solano, H.M.; Madero, M.; Pedraza-Chaverri, J. The effect of dietary supplementation with curcumin on redox status and Nrf2 activation in patients with nondiabetic or diabetic proteinuric chronic kidney disease: A pilot study. J. Ren. Nutr. 2016, 26, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Judaki, A.; Rahmani, A.; Feizi, J.; Asadollahi, K.; Ahmadi, M.R.H. Curcumin in combination with triple therapy regimes ameliorates oxidative stress and histopathologic changes in chronic gastritis-associated Helicobacter pylori infection. Arq. Gastroenterol. 2017, 54, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Pakfetrat, M.; Akmali, M.; Malekmakan, L.; Dabaghimanesh, M.; Khorsand, M. Role of turmeric in oxidative modulation in end-stage renal disease patients. Hemodial. Int. 2015, 19, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Ghanei, M.; Hajhashemi, A.; Sahebkar, A. Effects of curcuminoids-piperine combination on systemic oxidative stress, clinical symptoms and quality of life in subjects with chronic pulmonary complications due to sulfur mustard: A randomized controlled trial. J. Diet. Suppl. 2016, 13, 93–105. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Saadat, A.; Beiraghdar, F.; Nouzari, S.M.H.; Jalalian, H.R.; Sahebkar, A. Antioxidant effects of bioavailability-enhanced curcuminoids in patients with solid tumors: A randomized double-blind placebo-controlled trial. J. Funct. Foods 2014, 6, 615–622. [Google Scholar] [CrossRef]
- Panahi, Y.; Alishiri, G.H.; Parvin, S.; Sahebkar, A. Mitigation of systemic oxidative stress by curcuminoids in osteoarthritis: Results of a randomized controlled trial. J. Diet. Suppl. 2016, 13, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Roohi, B.N.; Moradlou, A.N.; Bolboli, L. Influence of curcumin supplementation on exercise-induced oxidative stress. Asian J. Sports Med. 2017, 8, e35776. [Google Scholar]
- Sudheeran, S.P.; Jacob, D.; Mulakal, J.N.; Nair, G.G.; Maliakel, A.; Maliakel, B.; Kuttan, R.; Krishnakumar, I. Safety, tolerance, and enhanced efficacy of a bioavailable formulation of curcumin with fenugreek dietary fiber on occupational stress: A randomized, double-blind, placebo-controlled pilot study. J. Clin. Psychopharmacol. 2016, 36, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Qin, S.; Huang, L.; Gong, J.; Shen, S.; Huang, J.; Tang, Y.; Ren, H.; Hu, H. Meta-analysis of randomized controlled trials of 4 weeks or longer suggest that curcumin may afford some protection against oxidative stress. Nutr. Res. 2018, 60, 1–12. [Google Scholar] [CrossRef]
- Lukkunaprasit, T.; Tansawet, A.; Boonmanunt, S.; Sobhonslidsuk, A.; McKay, G.J.; Attia, J.; Thakkinstian, A. An updated meta-analysis of effects of curcumin on metabolic dysfunction-associated fatty liver disease based on available evidence from Iran and Thailand. Sci. Rep. 2023, 13, 5824. [Google Scholar] [CrossRef]
- Rahmani, S.; Asgary, S.; Askari, G.; Keshvari, M.; Hatamipour, M.; Feizi, A.; Sahebkar, A. Treatment of non-alcoholic fatty liver disease with curcumin: A randomized placebo-controlled trial. Phytother. Res. 2016, 30, 1540–1548. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Valizadegan, G.; Ahamdi, N.; Ganjali, S.; Majeed, M.; Sahebkar, A. Curcuminoids plus piperine improve nonalcoholic fatty liver disease: A clinical trial. J. Cell. Biochem. 2019, 120, 15989–15996. [Google Scholar] [CrossRef] [PubMed]
- Chirapongsathorn, S.; Jearjesdakul, J.; Sanpajit, T.; Juthaputthi, A. Curcumin trend to improve alanine transaminase (ALT) in non-alcoholic fatty liver disease (NAFLD) with abnormal ALT. J. Gastroenterol. Hepatol. 2012, 27, 231–232. [Google Scholar]
- Chashmniam, S.; Mirhafez, S.R.; Dehabeh, M.; Hariri, M.; Azimi Nezhad, M.; Nobakht, M.; Gh, B.F. A pilot study of the effect of phospholipid curcumin on serum metabolomic profile in patients with non-alcoholic fatty liver disease: A randomized, double-blind, placebo-controlled trial. Eur. J. Clin. Nutr. 2019, 73, 1224–1235. [Google Scholar] [CrossRef] [PubMed]
- Saadati, S.; Hatami, B.; Yari, Z.; Shahrbaf, M.A.; Eghtesad, S.; Mansour, A.; Poustchi, H.; Hedayati, M.; Aghajanpoor-Pasha, M.; Sadeghi, A. The effects of curcumin supplementation on liver enzymes, lipid profile, glucose homeostasis, and hepatic steatosis and fibrosis in patients with non-alcoholic fatty liver disease. Eur. J. Clin. Nutr. 2019, 73, 441–449. [Google Scholar] [CrossRef]
- Saberi-Karimian, M.; Keshvari, M.; Ghayour-Mobarhan, M.; Salehizadeh, L.; Rahmani, S.; Behnam, B.; Jamialahmadi, T.; Asgary, S.; Sahebkar, A. Effects of curcuminoids on inflammatory status in patients with non-alcoholic fatty liver disease: A randomized controlled trial. Complement. Ther. Med. 2020, 49, 102322. [Google Scholar] [CrossRef]
- Mirhafez, S.R.; Azimi-Nezhad, M.; Dehabeh, M.; Hariri, M.; Naderan, R.D.; Movahedi, A.; Abdalla, M.; Sathyapalan, T.; Sahebkar, A. The effect of curcumin phytosome on the treatment of patients with non-alcoholic fatty liver disease: A double-blind, randomized, placebo-controlled trial. Adv. Exp. Med. Biol. 2021, 1308, 25–35. [Google Scholar]
- Mirhafez, S.R.; Dehabeh, M.; Hariri, M.; Farimani, A.R.; Movahedi, A.; Naderan, R.D.; Jamialahmadi, T.; Simental-Mendía, L.E.; Sahebkar, A. Curcumin and piperine combination for the treatment of patients with non-alcoholic fatty liver disease: A double-blind randomized placebo-controlled trial. Adv. Exp. Med. Biol. 2021, 1328, 11–19. [Google Scholar]
- Zhang, H. Study on the effect of curcumin on glucose and lipid metabolism in patients with metabolic syndrome. Mod. J. Integr. Tradit. Chin. West. Med. 2019, 28, 1103–1105. [Google Scholar]
- Alidadi, M.; Sahebkar, A.; Eslami, S.; Vakilian, F.; Jarahi, L.; Alinezhad-Namaghi, M.; Arabi, S.M.; Vakili, S.; Tohidinezhad, F.; Nikooiyan, Y.; et al. The Effect of Curcumin Supplementation on Pulse Wave Velocity in Patients with Metabolic Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial. Adv. Exp. Med. Biol. 2021, 1308, 1–11. [Google Scholar] [CrossRef]
- Bateni, Z.; Rahimi, H.R.; Hedayati, M.; Afsharian, S.; Goudarzi, R.; Sohrab, G. The effects of nano-curcumin supplementation on glycemic control, blood pressure, lipid profile, and insulin resistance in patients with the metabolic syndrome: A randomized, double-blind clinical trial. Phytother. Res. 2021, 35, 3945–3953. [Google Scholar] [CrossRef] [PubMed]
- Salimi Avansar, M. The effects of eight weeks interval training and curcumin consumption on TNF-α and BDNF levels in men with metabolic syndrome. J. Ardabil Univ. Med. Sci. 2017, 17, 299–310. [Google Scholar]
- Różański, G.; Tabisz, H.; Zalewska, M.; Niemiro, W.; Kujawski, S.; Newton, J.; Zalewski, P.; Słomko, J. Meta-analysis of exploring the effect of curcumin supplementation with or without other advice on biochemical and anthropometric parameters in patients with metabolic-associated fatty liver disease (MAFLD). Int. J. Environ. Res. Public Health 2023, 20, 4266. [Google Scholar] [CrossRef] [PubMed]
- Moradi Kelardeh, B.; Keshavarz, S.; Karimi, M. Effects of nonlinear resistance training with curcumin supplement on liver enzymes in men with non-alcoholic fatty liver disease. Rep. Health Care 2017, 3, 1–9. [Google Scholar]
- Hariri, M.; Gholami, A.; Mirhafez, S.R.; Bidkhori, M.; Sahebkar, A. A pilot study of the effect of curcumin on epigenetic changes and DNA damage among patients with non-alcoholic fatty liver disease: A randomized, double-blind, placebo-controlled, clinical trial. Complement. Ther. Med. 2020, 51, 102447. [Google Scholar] [CrossRef] [PubMed]
- Kelardeh, B.M.; Rahmati-Ahmadabad, S.; Farzanegi, P.; Helalizadeh, M.; Azarbayjani, M.-A. Effects of non-linear resistance training and curcumin supplementation on the liver biochemical markers levels and structure in older women with non-alcoholic fatty liver disease. J. Bodyw. Mov. Ther. 2020, 24, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Kianpour, P.; Mohtashami, R.; Jafari, R.; Simental-Mendía, L.E.; Sahebkar, A. Curcumin lowers serum lipids and uric acid in subjects with nonalcoholic fatty liver disease: A randomized controlled trial. J. Cardiovasc. Pharmacol. 2016, 68, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Kianpour, P.; Mohtashami, R.; Jafari, R.; Simental-Mendía, L.E.; Sahebkar, A. Efficacy and safety of phytosomal curcumin in non-alcoholic fatty liver disease: A randomized controlled trial. Drug Res. 2017, 67, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Cicero, A.F.; Sahebkar, A.; Fogacci, F.; Bove, M.; Giovannini, M.; Borghi, C. Effects of phytosomal curcumin on anthropometric parameters, insulin resistance, cortisolemia and non-alcoholic fatty liver disease indices: A double-blind, placebo-controlled clinical trial. Eur. J. Nutr. 2020, 59, 477–483. [Google Scholar] [CrossRef]
- Ngu, M.; Norhayati, M.; Rosnani, Z.; Zulkifli, M. Curcumin as adjuvant treatment in patients with non-alcoholic fatty liver (NAFLD) disease: A systematic review and meta-analysis. Complement. Ther. Med. 2022, 68, 102843. [Google Scholar] [CrossRef]
- Saadati, S.; Hekmatdoost, A.; Hatami, B.; Mansour, A.; Zahra, Z.; Hedayati, M.; Sadeghi, A. Comparing different non-invasive methods in assessment of the effects of curcumin on hepatic fibrosis in patients with non-alcoholic fatty liver disease. Gastroenterol. Hepatol. Bed Bench 2018, 11, S8. [Google Scholar] [PubMed]
- Rahimi, H.R.; Mohammadpour, A.H.; Dastani, M.; Jaafari, M.R.; Abnous, K.; Mobarhan, M.G.; Oskuee, R.K. The effect of nano-curcumin on HbA1c, fasting blood glucose, and lipid profile in diabetic subjects: A randomized clinical trial. Avicenna J. Phytomedicine 2016, 6, 567. [Google Scholar]
- Na, L.X.; Li, Y.; Pan, H.Z.; Zhou, X.L.; Sun, D.J.; Meng, M.; Li, X.X.; Sun, C.H. Curcuminoids exert glucose-lowering effect in type 2 diabetes by decreasing serum free fatty acids: A double-blind, placebo-controlled trial. Mol. Nutr. Food Res. 2013, 57, 1569–1577. [Google Scholar] [CrossRef]
- Javandoost, A.; Afshari, A.; Saberi-Karimian, M.; Sahebkar, A.; Safarian, H.; Moammeri, M.; Dizaji, B.F.; Tavalaei, S.; Ferns, G.A.; Pasdar, A. The effects of curcumin and a modified curcumin formulation on serum Cholesteryl Ester Transfer Protein concentrations in patients with metabolic syndrome: A randomized, placebo-controlled clinical trial. Avicenna J. Phytomed. 2018, 8, 330. [Google Scholar]
- Asadi, S.; Gholami, M.S.; Siassi, F.; Qorbani, M.; Khamoshian, K.; Sotoudeh, G. Nano curcumin supplementation reduced the severity of diabetic sensorimotor polyneuropathy in patients with type 2 diabetes mellitus: A randomized double-blind placebo-controlled clinical trial. Complement. Ther. Med. 2019, 43, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Vanaie, A.; Shahidi, S.; Iraj, B.; Siadat, Z.D.; Kabirzade, M.; Shakiba, F.; Mohammadi, M.; Parvizian, H. Curcumin as a major active component of turmeric attenuates proteinuria in patients with overt diabetic nephropathy. J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2019, 24, 77. [Google Scholar]
- Karandish, M.; Mozaffari-khosravi, H.; Mohammadi, S.M.; Cheraghian, B.; Azhdari, M. The effect of curcumin and zinc co-supplementation on glycemic parameters in overweight or obese prediabetic subjects: A phase 2 randomized, placebo-controlled trial with a multi-arm, parallel-group design. Phytother. Res. 2021, 35, 4377–4387. [Google Scholar] [CrossRef] [PubMed]
- Neta, J.F.d.F.; Veras, V.S.; Sousa, D.F.d.; Cunha, M.d.C.d.S.O.; Queiroz, M.V.O.; Neto, J.C.G.L.; Damasceno, M.M.C.; Araújo, M.F.M.d.; Freitas, R.W.J.F.d. Effectiveness of the piperine-supplemented Curcuma longa L. in metabolic control of patients with type 2 diabetes: A randomised double-blind placebo-controlled clinical trial. Int. J. Food Sci. Nutr. 2021, 72, 968–977. [Google Scholar] [CrossRef]
- Thota, R.N.; Rosato, J.I.; Dias, C.B.; Burrows, T.L.; Martins, R.N.; Garg, M.L. Dietary Supplementation with Curcumin Reduce Circulating Levels of Glycogen Synthase Kinase-3β and Islet Amyloid Polypeptide in Adults with High Risk of Type 2 Diabetes and Alzheimer’s Disease. Nutrients 2020, 12, 1032. [Google Scholar] [CrossRef]
- Tian, J.; Feng, B.; Tian, Z. The effect of curcumin on lipid profile and glycemic status of patients with type 2 Diabetes Mellitus: A systematic review and meta-analysis. Evid.-Based Complement. Altern. Med. 2022, 2022, 8278744. [Google Scholar] [CrossRef]
- Abbood, M.S. Hypolipidaemic and anti-inflammatory effects of curcumin versus atorvastatin in type 2 diabetic patients. Int. J. Pharm. Sci. Rev. Res 2018, 49, 1–7. [Google Scholar]
- Nouri, M.; Sohaei, S.; Shalaby, M.N.; Mehrabani, S.; Ramezani, A.; Faghih, S. Effect of curcumin on body mass index and glycemic indices in females with PCOS: A systematic review and meta-analysis of randomized controlled trial. Nutr. Food Sci. 2022, 52, 1129–1141. [Google Scholar] [CrossRef]
- Jamilian, M.; Foroozanfard, F.; Kavossian, E.; Aghadavod, E.; Shafabakhsh, R.; Hoseini, A.; Asemi, Z. Effects of curcumin on body weight, glycemic control and serum lipids in women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Clin. Nutr. ESPEN 2020, 36, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Heshmati, J.; Moini, A.; Sepidarkish, M.; Morvaridzadeh, M.; Salehi, M.; Palmowski, A.; Mojtahedi, M.F.; Shidfar, F. Effects of curcumin supplementation on blood glucose, insulin resistance and androgens in patients with polycystic ovary syndrome: A randomized double-blind placebo-controlled clinical trial. Phytomedicine 2021, 80, 153395. [Google Scholar] [CrossRef] [PubMed]
- Khalili, L.; Nammi, S. The effects of curcumin supplementation on metabolic biomarkers and body mass index in patients with nonalcoholic fatty liver disease: A systematic review and meta-analysis of randomized controlled trials. Curr. Pharm. Des. 2022, 28, 1911–1925. [Google Scholar] [CrossRef] [PubMed]
- Husain, D.; Jarahzadeh, M.; Alavinejad, P.; Rezazadeh, A.; Haghighizadeh, M. Turmeric supplementation in nonalcoholic fatty liver disease. Plant Arch 2020, 20, 3640–3647. [Google Scholar]
- Sohrevardi, S.M.; Heydari, B.; Azarpazhooh, M.R.; Teymourzadeh, M.; Simental-Mendía, L.E.; Atkin, S.L.; Sahebkar, A.; Karimi-Zarchi, M. Therapeutic effect of curcumin in women with polycystic ovary syndrome receiving metformin: A randomized controlled trial. Pharmacol. Prop. Plant-Deriv. Nat. Prod. Implic. Hum. Health 2021, 1308, 109–117. [Google Scholar]
- Wu, J.-L.; Liu, J.-C.; Liu, F.; Deng, X.; Fang, F.; Hu, R.-J.; Zhu, D.-P. Randomized controlled trial of Curcuma longa on improving insulin sensitivity in patients with polycystic ovary syndrome. Chin. J. Integr. Tradit. West. Med. 2022, 42, 444–448. [Google Scholar]
- Wu, J.; Mei, X.; Tang, S.; Fang, F.; Li, S.; Zhang, H. Clinical study of Curcuma longa combined with metformin on improving insulin resistance in patients with polycystic ovary syndrom. Chin. J. Integr. Med. 2020, 40, 406–412. [Google Scholar]
- Zhang, T.; He, Q.; Liu, Y.; Chen, Z.; Hu, H. Efficacy and safety of curcumin supplement on improvement of insulin resistance in people with type 2 diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials. Evid.-Based Complement. Altern. Med. 2021, 2021, 4471944. [Google Scholar] [CrossRef]
- Altobelli, E.; Angeletti, P.M.; Marziliano, C.; Mastrodomenico, M.; Giuliani, A.R.; Petrocelli, R. Potential therapeutic effects of curcumin on glycemic and lipid profile in uncomplicated type 2 diabetes—A meta-analysis of randomized controlled trial. Nutrients 2021, 13, 404. [Google Scholar] [CrossRef] [PubMed]
- Chien, Y.-J.; Chang, C.-Y.; Wu, M.-Y.; Chen, C.-H.; Horng, Y.-S.; Wu, H.-C. Effects of curcumin on glycemic control and lipid profile in polycystic ovary syndrome: Systematic review with meta-analysis and trial sequential analysis. Nutrients 2021, 13, 684. [Google Scholar] [CrossRef] [PubMed]
- Jalali, M.; Mahmoodi, M.; Mosallanezhad, Z.; Jalali, R.; Imanieh, M.H.; Moosavian, S.P. The effects of curcumin supplementation on liver function, metabolic profile and body composition in patients with non-alcoholic fatty liver disease: A systematic review and meta-analysis of randomized controlled trials. Complement. Ther. Med. 2020, 48, 102283. [Google Scholar] [CrossRef] [PubMed]
- Azhdari, M.; Karandish, M.; Mansoori, A. Metabolic benefits of curcumin supplementation in patients with metabolic syndrome: A systematic review and meta-analysis of randomized controlled trials. Phytother. Res. 2019, 33, 1289–1301. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Qin, S.; Huang, L.; Tang, Y.; Ren, H.; Hu, H. Efficacy and safety of Rhizoma curcumea longae with respect to improving the glucose metabolism of patients at risk for cardiovascular disease: A meta-analysis of randomised controlled trials. J. Hum. Nutr. Diet. 2019, 32, 591–606. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-W.; Ha, K.-C.; Choi, E.-K.; Jung, S.-Y.; Kim, M.-G.; Kwon, D.-Y.; Yang, H.-J.; Kim, M.-J.; Kang, H.-J.; Back, H.-I. The effectiveness of fermented turmeric powder in subjects with elevated alanine transaminase levels: A randomised controlled study. BMC Complement. Altern. Med. 2013, 13, 58. [Google Scholar] [CrossRef] [PubMed]
- Tabrizi, R.; Vakili, S.; Lankarani, K.B.; Akbari, M.; Mirhosseini, N.; Ghayour-Mobarhan, M.; Ferns, G.; Karamali, F.; Karamali, M.; Taghizadeh, M. The effects of curcumin on glycemic control and lipid profiles among patients with metabolic syndrome and related disorders: A systematic review and meta-analysis of randomized controlled trials. Curr. Pharm. Des. 2018, 24, 3184–3199. [Google Scholar] [CrossRef] [PubMed]
- Adab, Z.; Eghtesadi, S.; Vafa, M.; Heydari, I.; Shojaei, A.; Haqqani, H.; Khorraminia, N. Effect of turmeric on body measurement indices, glycemic condition, and lipid profile in hyperlipidemic patients with type 2 diabetes. Iran. J. Nutr. Sci. Food Technol. 2013, 8, 217–227. [Google Scholar]
- Ferguson, J.J.; Stojanovski, E.; MacDonald-Wicks, L.; Garg, M.L. Curcumin potentiates cholesterol-lowering effects of phytosterols in hypercholesterolaemic individuals. A randomised controlled trial. Metabolism 2018, 82, 22–35. [Google Scholar] [CrossRef]
- Wen, W.; Zou, Y. Effect of β-cyclodextrin curcumin on lowering blood lipid in human body. Strait Pharm J. 2020, 32, 135–138. [Google Scholar]
- Saeedi, F.; Farkhondeh, T.; Roshanravan, B.; Amirabadizadeh, A.; Ashrafizadeh, M.; Samarghandian, S. Curcumin and blood lipid levels: An updated systematic review and meta-analysis of randomised clinical trials. Arch. Physiol. Biochem. 2022, 128, 1493–1502. [Google Scholar] [CrossRef] [PubMed]
- Murillo Ortiz, B.O.; Fuentes Preciado, A.R.; Ramírez Emiliano, J.; Martínez Garza, S.; Ramos Rodríguez, E.; de Alba Macías, L.A. Recovery of bone and muscle mass in patients with chronic kidney disease and iron overload on hemodialysis and taking combined supplementation with curcumin and resveratrol. Clin. Interv. Aging 2019, 14, 2055–2062. [Google Scholar] [CrossRef] [PubMed]
- Simental-Mendía, L.E.; Pirro, M.; Gotto, A.M., Jr.; Banach, M.; Atkin, S.L.; Majeed, M.; Sahebkar, A. Lipid-modifying activity of curcuminoids: A systematic review and meta-analysis of randomized controlled trials. Crit. Rev. Food Sci. Nutr. 2019, 59, 1178–1187. [Google Scholar] [CrossRef] [PubMed]
- Alwi, I.; Santoso, T.; Suyono, S.; Sutrisna, B.; Suyatna, F.D.; Kresno, S.B.; Ernie, S. The effect of curcumin on lipid level in patients with acute coronary syndrome. Acta Med. Indones. 2008, 40, 201–210. [Google Scholar] [PubMed]
- Baum, L.; Cheung, S.K.; Mok, V.C.; Lam, L.C.; Leung, V.P.; Hui, E.; Ng, C.C.; Chow, M.; Ho, P.C.; Lam, S. Curcumin effects on blood lipid profile in a 6-month human study. Pharmacol. Res. 2007, 56, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Pashine, L.; Singh, J.; Vaish, A.; Ojha, S.; Mahdi, A. Effect of turmeric (Curcuma longa) on overweight hyperlipidemic subjects: Double blind study. Indian J. Community Health 2012, 24, 113–117. [Google Scholar]
- Sukandar, E.Y.; Sudjana, P.; Sigit, J.I.; Leliqia, N.P.E.; Lestari, F. Safety of garlic (Allium sativum) and turmeric (Curcuma domestica) extract in comparison with simvastatin on improving lipid profile in dyslipidemia patients. J. Med. Sci. 2013, 13, 10–18. [Google Scholar] [CrossRef]
- Pungcharoenkul, K.; Thongnopnua, P. Effect of different curcuminoid supplement dosages on total in vivo antioxidant capacity and cholesterol levels of healthy human subjects. Phytother. Res. 2011, 25, 1721–1726. [Google Scholar] [CrossRef]
- Adibian, M.; Hodaie, H.; Hedayati, M.; Sohrab, G. Effect of curcumin supplementation on risk factors of cardiovascular disease in patient with type 2 diabetes. Res. Med. 2017, 41, 86–96. [Google Scholar]
- Amirkhani, Z.; Azarbayjani, M.A.; Peeri, M.; Matin Homaei, H. Effect of combining resistance training and curcumin supplementation on lipid profile in obese women. Iran. J. Obstet. Gynecol. Infertil. 2017, 20, 24–32. [Google Scholar]
- Qin, S.; Huang, L.; Gong, J.; Shen, S.; Huang, J.; Ren, H.; Hu, H. Efficacy and safety of turmeric and curcumin in lowering blood lipid levels in patients with cardiovascular risk factors: A meta-analysis of randomized controlled trials. Nutr. J. 2017, 16, 68. [Google Scholar] [CrossRef] [PubMed]
- Sahebkar, A. A systematic review and meta-analysis of randomized controlled trials investigating the effects of curcumin on blood lipid levels. Clin. Nutr. 2014, 33, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Di Pierro, F.; Bressan, A.; Ranaldi, D.; Rapacioli, G.; Giacomelli, L.; Bertuccioli, A. Potential role of bioavailable curcumin in weight loss and omental adipose tissue decrease: Preliminary data of a randomized, controlled trial in overweight people with metabolic syndrome. Preliminary study. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 4195–4202. [Google Scholar] [PubMed]
- Mirhafez, S.R.; Rezai, A.; Dehabeh, M.; Gh, B.F.N.M.; Bidkhori, M.; Sahebkar, A.; Hariri, M. Efficacy of phytosomal curcumin among patients with non-alcoholic fatty liver disease. Int. J. Vitam. Nutr. Res. 2019, 91, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Mousavi, S.M.; Milajerdi, A.; Varkaneh, H.K.; Gorjipour, M.M.; Esmaillzadeh, A. The effects of curcumin supplementation on body weight, body mass index and waist circumference: A systematic review and dose-response meta-analysis of randomized controlled trials. Crit. Rev. Food Sci. Nutr. 2020, 60, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, A.; Sadeghnia, H.R.; Saberi-Karimian, M.; Safarian, H.; Ferns, G.A.; Ghayour-Mobarhan, M.; Sahebkar, A. Effects of curcumin on serum vitamin E concentrations in individuals with metabolic syndrome. Phytother. Res. 2017, 31, 657–662. [Google Scholar] [CrossRef] [PubMed]
- Jazayeri-Tehrani, S.A.; Rezayat, S.M.; Mansouri, S.; Qorbani, M.; Alavian, S.M.; Daneshi-Maskooni, M.; Hosseinzadeh-Attar, M.-J. The nanocurcumin reduces appetite in obese patients with non-alcoholic fatty liver disease (nafld): A double-blind randomized placebo-controlled clinical trial. Nanomed. J. 2018, 5, 67–76. [Google Scholar]
- Baziar, N.; Parohan, M. The effects of curcumin supplementation on body mass index, body weight, and waist circumference in patients with nonalcoholic fatty liver disease: A systematic review and dose–response meta-analysis of randomized controlled trials. Phytother. Res. 2020, 34, 464–474. [Google Scholar] [CrossRef] [PubMed]
- Sahebkar, A.; Mohammadi, A.; Atabati, A.; Rahiman, S.; Tavallaie, S.; Iranshahi, M.; Akhlaghi, S.; Ferns, G.A.; Ghayour-Mobarhan, M. Curcuminoids modulate pro-oxidant–antioxidant balance but not the immune response to heat shock protein 27 and oxidized LDL in obese individuals. Phytother. Res. 2013, 27, 1883–1888. [Google Scholar] [CrossRef]
- Wei, Z.; Liu, N.; Tantai, X.; Xing, X.; Xiao, C.; Chen, L.; Wang, J. The effects of curcumin on the metabolic parameters of non-alcoholic fatty liver disease: A meta-analysis of randomized controlled trials. Hepatol. Int. 2019, 13, 302–313. [Google Scholar] [CrossRef]
- Guyatt, G.; Oxman, A.D.; Sultan, S.; Brozek, J.; Glasziou, P.; Alonso-Coello, P.; Atkins, D.; Kunz, R.; Montori, V.; Jaeschke, R. GRADE guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. J. Clin. Epidemiol. 2013, 66, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Jafarirad, S.; Mansoori, A.; Adineh, A.; Panahi, Y.; Hadi, A.; Goodarzi, R. Does turmeric/curcumin supplementation change anthropometric indices in patients with non-alcoholic fatty liver disease? A systematic review and meta-analysis of randomized controlled trials. Clin. Nutr. Res. 2019, 8, 196–208. [Google Scholar] [CrossRef] [PubMed]
- Kelardeh, B.M.; Azarbayjani, M.A.; Peeri, M.; Homaee, H. Effect of curcumin supplementation and resistance training in patients with nonalcoholic fatty liver disease. J. Med. Plants 2016, 15, 161–172. [Google Scholar]
- Changal, K.H.; Khan, M.S.; Bashir, R.; Sheikh, M.A. Curcumin preparations can improve flow-mediated dilation and endothelial function: A meta-analysis. Complement. Med. Res. 2020, 27, 272–281. [Google Scholar] [CrossRef] [PubMed]
- Akazawa, N.; Choi, Y.; Miyaki, A.; Tanabe, Y.; Sugawara, J.; Ajisaka, R.; Maeda, S. Curcumin ingestion and exercise training improve vascular endothelial function in postmenopausal women. Nutr. Res. 2012, 32, 795–799. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, H.; Tsuge, N.; Sawada, H.; Masamura, N.; Yamada, S.; Satomi, S.; Higashi, Y. A single consumption of curry improved postprandial endothelial function in healthy male subjects: A randomized, controlled crossover trial. Nutr. J. 2014, 13, 67. [Google Scholar] [CrossRef]
- Oliver, J.M.; Stoner, L.; Rowlands, D.S.; Caldwell, A.R.; Sanders, E.; Kreutzer, A.; Mitchell, J.B.; Purpura, M.; Jäger, R. Novel form of curcumin improves endothelial function in young, healthy individuals: A double-blind placebo controlled study. J. Nutr. Metab. 2016, 2016, 1089653. [Google Scholar] [CrossRef]
- Barber-Chamoux, N.; Milenkovic, D.; Verny, M.A.; Habauzit, V.; Pereira, B.; Lambert, C.; Richard, D.; Boby, C.; Mazur, A.; Lusson, J.R. Substantial variability across individuals in the vascular and nutrigenomic response to an acute intake of curcumin: A randomized controlled trial. Mol. Nutr. Food Res. 2018, 62, 1700418. [Google Scholar] [CrossRef] [PubMed]
- Hallajzadeh, J.; Milajerdi, A.; Kolahdooz, F.; Amirani, E.; Mirzaei, H.; Asemi, Z. The effects of curcumin supplementation on endothelial function: A systematic review and meta-analysis of randomized controlled trials. Phytother. Res. 2019, 33, 2989–2995. [Google Scholar] [CrossRef]
- Sugawara, J.; Akazawa, N.; Miyaki, A.; Choi, Y.; Tanabe, Y.; Imai, T.; Maeda, S. Effect of endurance exercise training and curcumin intake on central arterial hemodynamics in postmenopausal women: Pilot study. Am. J. Hypertens. 2012, 25, 651–656. [Google Scholar] [CrossRef]
- Derosa, G.; Catena, G.; Raddino, R.; Gaudio, G.; Maggi, A.; D’Angelo, A.; Maffioli, P. Effects on oral fat load of a nutraceutical combination of fermented red rice, sterol esters and stanols, curcumin, and olive polyphenols: A randomized, placebo controlled trial. Phytomedicine 2018, 42, 75–82. [Google Scholar] [CrossRef]
- Hadi, A.; Pourmasoumi, M.; Ghaedi, E.; Sahebkar, A. The effect of Curcumin/Turmeric on blood pressure modulation: A systematic review and meta-analysis. Pharmacol. Res. 2019, 150, 104505. [Google Scholar] [CrossRef]
- Khajehdehi, P.; Zanjaninejad, B.; Aflaki, E.; Nazarinia, M.; Azad, F.; Malekmakan, L.; Dehghanzadeh, G.-R. Oral supplementation of turmeric decreases proteinuria, hematuria, and systolic blood pressure in patients suffering from relapsing or refractory lupus nephritis: A randomized and placebo-controlled study. J. Ren. Nutr. 2012, 22, 50–57. [Google Scholar] [CrossRef]
- Akazawa, N.; Choi, Y.; Miyaki, A.; Tanabe, Y.; Sugawara, J.; Ajisaka, R.; Maeda, S. Effects of curcumin intake and aerobic exercise training on arterial compliance in postmenopausal women. Artery Res. 2013, 7, 67–72. [Google Scholar] [CrossRef]
- Wang, Z.; Zhang, Q.; Huang, H.; Liu, Z. The efficacy and acceptability of curcumin for the treatment of depression or depressive symptoms: A systematic review and meta-analysis. J. Affect. Disord. 2021, 282, 242–251. [Google Scholar] [CrossRef]
- Bergman, J.; Miodownik, C.; Bersudsky, Y.; Sokolik, S.; Lerner, P.P.; Kreinin, A.; Polakiewicz, J.; Lerner, V. Curcumin as an add-on to antidepressive treatment: A randomized, double-blind, placebo-controlled, pilot clinical study. Clin. Neuropharmacol. 2013, 36, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Kanchanatawan, B.; Tangwongchai, S.; Sughondhabhirom, A.; Suppapitiporn, S.; Hemrunrojn, S.; Carvalho, A.F.; Maes, M. Add-on treatment with curcumin has antidepressive effects in Thai patients with major depression: Results of a randomized double-blind placebo-controlled study. Neurotox. Res. 2018, 33, 621–633. [Google Scholar] [CrossRef] [PubMed]
- Lopresti, A.L.; Drummond, P.D. Efficacy of curcumin, and a saffron/curcumin combination for the treatment of major depression: A randomised, double-blind, placebo-controlled study. J. Affect. Disord. 2017, 207, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Lopresti, A.L.; Maes, M.; Maker, G.L.; Hood, S.D.; Drummond, P.D. Curcumin for the treatment of major depression: A randomised, double-blind, placebo controlled study. J. Affect. Disord. 2014, 167, 368–375. [Google Scholar] [CrossRef]
- Sanmukhani, J.; Satodia, V.; Trivedi, J.; Patel, T.; Tiwari, D.; Panchal, B.; Goel, A.; Tripathi, C.B. Efficacy and safety of curcumin in major depressive disorder: A randomized controlled trial. Phytother. Res. 2014, 28, 579–585. [Google Scholar] [CrossRef]
- Asadi, S.; Gholami, M.S.; Siassi, F.; Qorbani, M.; Sotoudeh, G. Beneficial effects of nano-curcumin supplement on depression and anxiety in diabetic patients with peripheral neuropathy: A randomized, double-blind, placebo-controlled clinical trial. Phytother. Res. 2020, 34, 896–903. [Google Scholar] [CrossRef] [PubMed]
- Esmaily, H.; Sahebkar, A.; Iranshahi, M.; Ganjali, S.; Mohammadi, A.; Ferns, G.; Ghayour-Mobarhan, M. An investigation of the effects of curcumin on anxiety and depression in obese individuals: A randomized controlled trial. Chin. J. Integr. Med. 2015, 21, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Miodownik, C.; Lerner, V.; Kudkaeva, N.; Lerner, P.P.; Pashinian, A.; Bersudsky, Y.; Eliyahu, R.; Kreinin, A.; Bergman, J. Curcumin as add-on to antipsychotic treatment in patients with chronic schizophrenia: A randomized, double-blind, placebo-controlled study. Clin. Neuropharmacol. 2019, 42, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Setiawati, M.C.; Ikawati, Z.; Kertia, I.N. Antiinflamatory and antidepressive activities of extract Curcuma xanthorrhiza roxb in systemic lupus Erythematosus. Indones. J. Pharm. 2017, 28, 185. [Google Scholar] [CrossRef]
- Fusar-Poli, L.; Vozza, L.; Gabbiadini, A.; Vanella, A.; Concas, I.; Tinacci, S.; Petralia, A.; Signorelli, M.S.; Aguglia, E. Curcumin for depression: A meta-analysis. Crit. Rev. Food Sci. Nutr. 2020, 60, 2643–2653. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Badeli, R.; Karami, G.R.; Sahebkar, A. Investigation of the efficacy of adjunctive therapy with bioavailability-boosted curcuminoids in major depressive disorder. Phytother. Res. 2015, 29, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Ng, Q.X.; Koh, S.S.H.; Chan, H.W.; Ho, C.Y.X. Clinical use of curcumin in depression: A meta-analysis. J. Am. Med. Dir. Assoc. 2017, 18, 503–508. [Google Scholar] [CrossRef]
- Al-Karawi, D.; Al Mamoori, D.A.; Tayyar, Y. The role of curcumin administration in patients with major depressive disorder: Mini meta-analysis of clinical trials. Phytother. Res. 2016, 30, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Tsai, I.-C.; Hsu, C.-W.; Chang, C.-H.; Tseng, P.-T.; Chang, K.-V. The effect of curcumin differs on individual cognitive domains across different patient populations: A systematic review and meta-analysis. Pharmaceuticals 2021, 14, 1235. [Google Scholar] [CrossRef]
- Kuszewski, J.C.; Wong, R.H.X.; Howe, P.R.C. Can curcumin counteract cognitive decline? Clinical trial evidence and rationale for combining ω-3 fatty acids with curcumin. Adv. Nutr. 2018, 9, 105–113. [Google Scholar] [CrossRef]
- Kucukgoncu, S.; Guloksuz, S.; Tek, C. Effects of curcumin on cognitive functioning and inflammatory state in schizophrenia: A double-blind, placebo-controlled pilot trial. J. Clin. Psychopharmacol. 2019, 39, 182–184. [Google Scholar] [CrossRef] [PubMed]
- Wynn, J.K.; Green, M.F.; Hellemann, G.; Karunaratne, K.; Davis, M.C.; Marder, S.R. The effects of curcumin on brain-derived neurotrophic factor and cognition in schizophrenia: A randomized controlled study. Schizophr. Res. 2018, 195, 572–573. [Google Scholar] [CrossRef]
- Rainey-Smith, S.R.; Brown, B.M.; Sohrabi, H.R.; Shah, T.; Goozee, K.G.; Gupta, V.B.; Martins, R.N. Curcumin and cognition: A randomised, placebo-controlled, double-blind study of community-dwelling older adults. Br. J. Nutr. 2016, 115, 2106–2113. [Google Scholar] [CrossRef]
- Ringman, J.M.; Frautschy, S.A.; Teng, E.; Begum, A.N.; Bardens, J.; Beigi, M.; Gylys, K.H.; Badmaev, V.; Heath, D.D.; Apostolova, L.G. Oral curcumin for Alzheimer’s disease: Tolerability and efficacy in a 24-week randomized, double blind, placebo-controlled study. Alzheimer’s Res. Ther. 2012, 4, 43. [Google Scholar] [CrossRef]
- Baum, L.; Lam, C.W.K.; Cheung, S.K.-K.; Kwok, T.; Lui, V.; Tsoh, J.; Lam, L.; Leung, V.; Hui, E.; Ng, C. Six-month randomized, placebo-controlled, double-blind, pilot clinical trial of curcumin in patients with Alzheimer disease. J. Clin. Psychopharmacol. 2008, 28, 110–113. [Google Scholar] [CrossRef]
- Cox, K.H.; White, D.J.; Pipingas, A.; Poorun, K.; Scholey, A. Further evidence of benefits to mood and working memory from lipidated curcumin in healthy older people: A 12-week, double-blind, placebo-controlled, partial replication study. Nutrients 2020, 12, 1678. [Google Scholar] [CrossRef] [PubMed]
- Kuszewski, J.C.; Howe, P.R.; Wong, R.H. Evaluation of cognitive performance following fish-oil and curcumin supplementation in middle-aged and older adults with overweight or obesity. J. Nutr. 2020, 150, 3190–3199. [Google Scholar] [CrossRef]
- Zhu, L.N.; Mei, X.; Zhang, Z.G.; Xie, Y.p.; Lang, F. Curcumin intervention for cognitive function in different types of people: A systematic review and meta-analysis. Phytother. Res. 2019, 33, 524–533. [Google Scholar] [CrossRef] [PubMed]
- Small, G.W.; Siddarth, P.; Li, Z.; Miller, K.J.; Ercoli, L.; Emerson, N.D.; Martinez, J.; Wong, K.-P.; Liu, J.; Merrill, D.A. Memory and brain amyloid and tau effects of a bioavailable form of curcumin in non-demented adults: A double-blind, placebo-controlled 18-month trial. Am. J. Geriatr. Psychiatry 2018, 26, 266–277. [Google Scholar] [CrossRef]
- Sarraf, P.; Parohan, M.; Javanbakht, M.H.; Ranji-Burachaloo, S.; Djalali, M. Short-term curcumin supplementation enhances serum brain-derived neurotrophic factor in adult men and women: A systematic review and dose-response meta-analysis of randomized controlled trials. Nutr. Res. 2019, 69, 1–8. [Google Scholar] [CrossRef]
- Osali, A. The effect of eight-week aerobic exercise and consumption of curcumin on il-6, il-10 and BDNF in 60-65 years women with metabolic syndrome. Med. J. Tabriz Univ. Med. Sci. 2018, 40, 7–14. [Google Scholar]
- Fanaei, H.; Khayat, S.; Kasaeian, A.; Javadimehr, M. Effect of curcumin on serum brain-derived neurotrophic factor levels in women with premenstrual syndrome: A randomized, double-blind, placebo-controlled trial. Neuropeptides 2016, 56, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Naghsh, N.; Musazadeh, V.; Nikpayam, O.; Kavyani, Z.; Moridpour, A.H.; Golandam, F.; Faghfouri, A.H.; Ostadrahimi, A. Profiling Inflammatory Biomarkers following Curcumin Supplementation: An Umbrella Meta-Analysis of Randomized Clinical Trials. Evid.-Based Complement. Altern. Med. 2023, 2023, 4875636. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimzadeh, A.; Abbasi, F.; Ebrahimzadeh, A.; Jibril, A.T.; Milajerdi, A. Effects of curcumin supplementation on inflammatory biomarkers in patients with rheumatoid arthritis and ulcerative colitis: A systematic review and meta-analysis. Complement. Ther. Med. 2021, 61, 102773. [Google Scholar] [CrossRef] [PubMed]
- Rao, C.V. Regulation of COX and LOX by curcumin. Mol. Targets Ther. Uses Curcumin Health Dis. 2007, 595, 213–226. [Google Scholar]
- Mahattanadul, S.; Kongpuckdee, S.; Wiwattanapatapee, R.; Tansakul, P.; Nitiruangjaras, A.; Hansakul, P. Comparative Inhibitory Efficacy on the iNOS/NO System of Curcuminand Tetrahydrocurcumin-Self-Microemulsifying Liquid Formulation in Chronic Gastric Ulcer Model. Curr. Pharm. Biotechnol. 2021, 22, 1005–1012. [Google Scholar] [CrossRef] [PubMed]
- Onoda, M.; Inano, H. Effect of curcumin on the production of nitric oxide by cultured rat mammary gland. Nitric Oxide 2000, 4, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Tang, Q.; Duan, P.; Yang, L. Curcumin as a therapeutic agent for blocking NF-κB activation in ulcerative colitis. Immunopharmacol. Immunotoxicol. 2018, 40, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Ak, T.; Gülçin, I. Antioxidant and radical scavenging properties of curcumin. Chem.-Biol. Interact. 2008, 174, 27–37. [Google Scholar] [CrossRef]
- Lin, X.; Bai, D.; Wei, Z.; Zhang, Y.; Huang, Y.; Deng, H.; Huang, X. Curcumin attenuates oxidative stress in RAW264. 7 cells by increasing the activity of antioxidant enzymes and activating the Nrf2-Keap1 pathway. PLoS ONE 2019, 14, e0216711. [Google Scholar]
- Jagetia, G.C.; Rajanikant, G.K. Curcumin stimulates the antioxidant mechanisms in mouse skin exposed to fractionated γ-irradiation. Antioxidants 2015, 4, 25–41. [Google Scholar] [CrossRef] [PubMed]
- Geng, S.; Wang, S.; Zhu, W.; Xie, C.; Li, X.; Wu, J.; Zhu, J.; Jiang, Y.; Yang, X.; Li, Y. Curcumin attenuates BPA-induced insulin resistance in HepG2 cells through suppression of JNK/p38 pathways. Toxicol. Lett. 2017, 272, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Musazadeh, V.; Roshanravan, N.; Mohammadizadeh, M.; Kavyani, Z.; Dehghan, P.; Mosharkesh, E. Curcumin as a novel approach in improving lipid profile: An umbrella meta-analysis. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 2493–2504. [Google Scholar] [CrossRef] [PubMed]
- Unhapipatpong, C.; Polruang, N.; Shantavasinkul, P.C.; Julanon, N.; Numthavaj, P.; Thakkinstian, A. The effect of curcumin supplementation on weight loss and anthropometric indices: An umbrella review and updated meta-analyses of randomized controlled trials. Am. J. Clin. Nutr. 2023, 117, 1005–1016. [Google Scholar] [CrossRef]
- Hariri, M.; Haghighatdoost, F. Effect of curcumin on anthropometric measures: A systematic review on randomized clinical trials. J. Am. Coll. Nutr. 2018, 37, 215–222. [Google Scholar] [CrossRef]
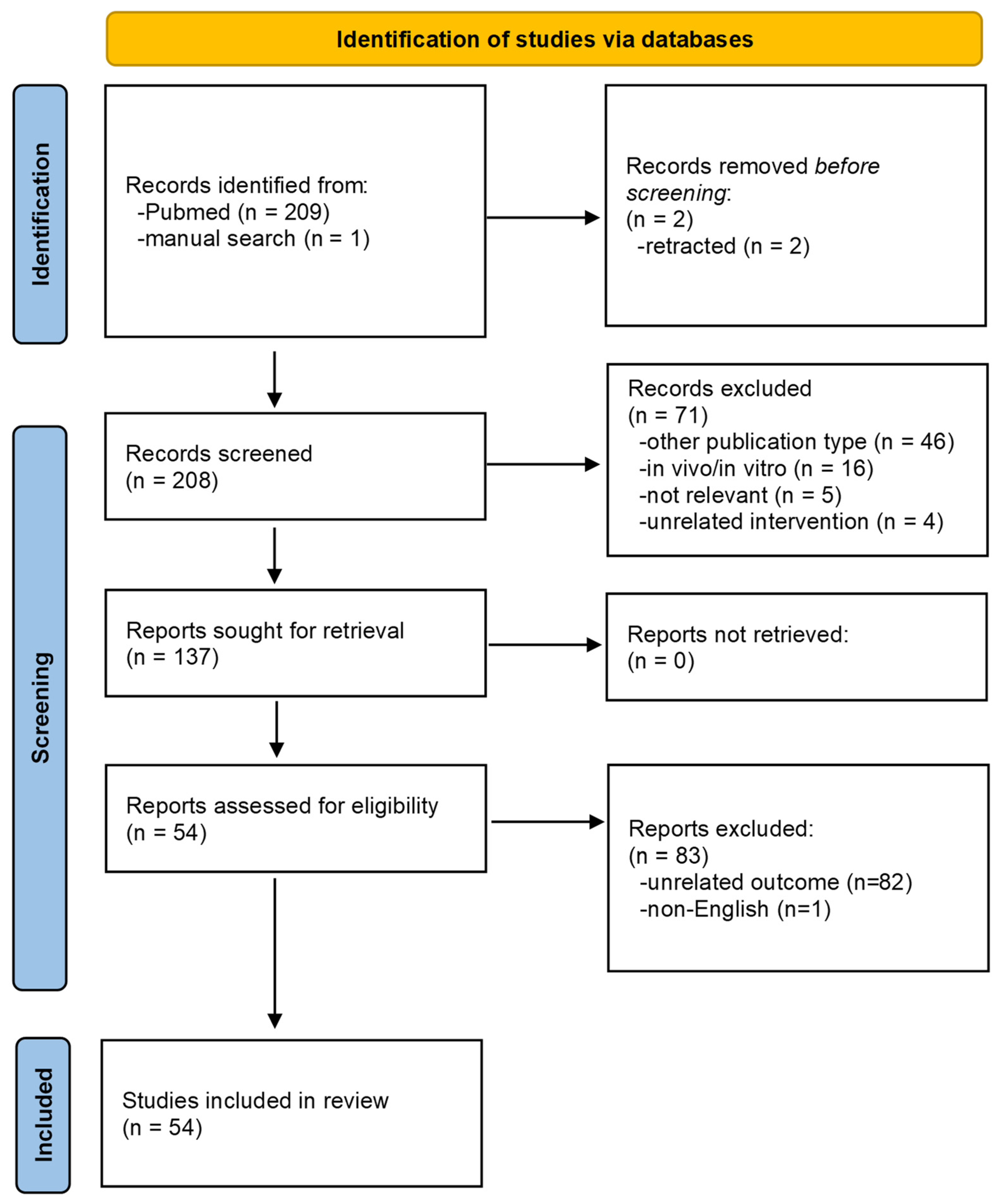
| Ref. | No. of Studies Included | Health Status of Subjects | No. of Subjects | Age of Subjects (Years) | Design | Period (Weeks) | Dose | Outcomes (Effect Size) | Quality of Primary Studies | Databases |
|---|---|---|---|---|---|---|---|---|---|---|
| Qiu et al. 2023 [22] | 2 publications [23,24] | Mets | 122 | 34–64 | P | 6–8 | 80 mg/day of curcumin, 1000 mg/day of curcuminoids | ↔ IL-6 (MD = −1.5 pg/mL; 95% CI −3.97 to 0.97; p = 0.23) ↓ TNF-α (MD = −12.97; 95% CI −18.37 to −7.57; p < 0.00001) | Cochrane risk of bias tool (71.4%) | PubMed, SCOPUS, Cochrane Library, EMBASE, Web of Science, and China Biological Medicine |
| 2 publications [23,25] | Mets | 130 | 54–64 | P | 6–8 | 80 mg/day of nano-curcumin, 2400 mg/day of turmeric | ↓ CRP (MD = −1.24 mg/L; 95% CI −1.71 to −0.77; p < 0.00001) | |||
| 2 publications [26,27] | Mets | 143 | 34–61 | P | 8–12 | 80 mg/day of nano-curcumin, 1000 mg/day of curcuminoids | ↔ hs-CRP (MD = −1.10 mg/L; 95% CI −4.35 to 2.16; p = 0.51) | |||
| Dehzad et al. 2023 [28] | 9 publications [29,30,31,32,33,34,35,36,37] | Healthy, Mets, NAFLD, IGTT, prediabetes, T2DM, major depressive disorder | 1172 | 18–70 | P | 4–42 | 50–1500 mg/day of curcumin | ↓ leptin (WMD = −4.46 ng/mL; 95% CI −6.70 to −2.21; p < 0.001; I2 = 96.1%; p < 0.001) | Cochrane risk of bias tool (61.0%) | PubMed, Scopus, Web of Science, Cochrane Library, and Google Scholar |
| 11 publications [29,30,31,32,34,36,37,38,39,40,41] | Healthy, Mets, IGTT, T2DM, prediabetic, NAFLD | 783 | 18–70 | P | 4–42 | 50–1500 mg/day of curcumin | ↑ adiponectin (WMD = 2.48 μg/mL; 95% CI 1.34 to 3.62; p < 0.001; I2 = 96.3%; p < 0.001) | |||
| Dehzad et al. 2023 [42] | 46 publications [23,29,38,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85] | Mets, healthy, obese, hemodialysis, chronic pulmonary complications, solid tumor, OA, T2DM, CAD, COPD, hyperlipidemia, migraine, infertile men, NAFLD, coronary elective angioplasty, RA, PCOS, Takayasu arteritis, pre-HTN, UC, diabetic foot ulcer | 2873 | 18–70 | P, CO | 4–24 | 80–2000 mg/day of curcumin, 150–1500 mg/day of curcuminoids, 900–3000 mg/day of turmeric | ↓ CRP (WMD = −0.58 mg/L; 95% CI −0.74 to −0.41; p < 0.05) | Cochrane risk of bias tool (84.2%) | PubMed, Scopus, Web of Science, Cochrane Library, and Google Scholar |
| 23 publications [24,43,47,48,50,54,55,56,60,63,64,67,68,71,79,83,86,87,88,89,90,91,92] | Mets, T2DM, OA, PUD, UC, obese, hemodialysis, NAFLD, HIV, solid tumor, migraine, lupus erythematosus, Takayasu arteritis, infertile coronary elective angioplasty | 1488 | 18–70 | P, CO | 4–12 | 80–1500 mg/day of curcumin, 150–1000 mg/day of curcuminoids, 1500–3000 mg/day of turmeric | ↓ TNF-α (WMD = −3.48 pg/mL; 95% CI −4.38 to −2.58; p < 0.05) | |||
| 20 publications [23,24,45,46,47,48,50,54,63,64,68,83,86,89,91,93,94,95,96,97] | Mets, obese, chronic pulmonary complications, solid tumor, OA, hemodialysis, hyperlipidemia, lupus erythematosus, migraine, pre-HTN, ankylosing spondylitis, chronic branchial asthma, chronic knee pain | 1166 | 18–70 | P, CO | 4–12 | 60–1500 mg/day of curcumin, 100–1500 mg/day of curcuminoids, 2800–3000 mg/day of turmeric | ↓ IL-6 (WMD = −1.31 pg/mL; 95% CI −1.58 to −0.67; p < 0.05) | |||
| 6 publications [47,79,86,88,91,98] | Obese, knee OA, PUD, pre-HTN, coronary elective angioplasty | 482 | 18–70 | P, CO | 4–16 | 80–1500 mg/day of curcumin | ↔ IL-1β (WMD = −0.46 pg/mL; 95% CI −1.18 to 0.27; p > 0.05) | |||
| Shen et al. 2022 [99] | 2 publications [58,73] | PCOS | 81 | 24–35 | P | 6–8 | 93.34–1000 mg/day of curcumin | ↓ CRP (WMD = −0.785; 95% CI −1.553 to −0.017; p = 0.045) | Cochrane risk of bias tool (73.5%) | PubMed, Embase, Cochrane Library, Web of Science, Scopus, Clinical Trials, Chinese Clinical Trial Registry, Chinese Biomedical Literature Database, Chinese National knowledge Infrastructure, VIP database, and Wanfang Database |
| Sun et al. 2022 [100] | 9 publications [27,29,38,49,60,61,76,80,101] | Mets, T2DM, DFU, CHD, hyperlipidemia, IGT | 697 | 38–70 | P, CO | 6–24 | 80–2100 mg/day of curcumin | ↓ hs-CRP (WMD = −1.11; 95% CI −2.16 to −0.05; p = 0.039) | Cochrane risk of bias tool (69.3%) Jadad scale (77.0%) | PubMed, Embase, Web of Science, CNKI, Wanfang, and CBM |
| 4 publications [29,31,38,39] | T2DM, IGT | 525 | 57–70 | P, CO | 10–36 | 180–1500 mg/day of curcumin | ↔ adiponectin (WMD = 6.43 ng/mL; 95% CI −1.19 to 14.05; p = 0.98) | |||
| Futuhi et al. 2022 [102] | 5 publications [71,72,81,103,104] | ESRD hemodialysis, CKD | 212 | 32–73 | P | 8–12 | 120 mg/day of curcumin, 1000 mg/day of curcuminoids, 2500 mg/day of turmeric | ↔ CRP (WMD = −0.13 mg/L; 95% CI −3.25 to 3.30; p = 0.93) | Cochrane risk of bias tool (73.0%) | PubMed, Scopus, Cochrane Library, and Web of Science |
| 3 publications [71,103,104] | ESRD, hemodialysis, CKD | 141 | 32–73 | P | 8–12 | 120 mg/day of curcumin, 1500 mg/day of turmeric | ↓ TNF-α (WMD = −18.87 pg/mL; 95% CI −28.36 to −9.38; p < 0.001) | |||
| Gorabi et al. 2022 [105] | 7 publications [25,43,44,45,46,47,106] | Mets, RA, overweight, infertility | 493 | 18–65 | P | 4–12 | 80–1000 mg/day of curcumin, 250–500 mg/day of curcuminoids 900–2400 mg/day of turmeric. | ↓ CRP (WMD = 3.67 mg/L; 95% CI −6.96 to −0.38; p = 0.02; I2 = 99.5%; p < 0.001) ↓ CRP (WMD = −2.77 mg/L; 95% CI −4.34 to −1.19; p < 0.001) at ≤1000 mg/day of curcumin compared with dose > 1000 mg/day of curcumin ↓ CRP (WMD = −3.48 mg/L; 95% CI −5.64 to −1.33; p < 0.001) with intervention duration of >10 weeks | Jadad scale (81.3%) | MEDLINE/ PubMed, Cochrane Library, Web of Science, and Scopus |
| 22 publications [27,29,38,48,49,50,51,52,53,54,55,56,57,58,59,60,61,103,107,108,109,110] | Mets, CAD, chronic cutaneous, ESRD, knee OA, T2DM, migraine | 1142 | 18–73 | P | 3 days–8 weeks | 1000–4000 mg/day of curcuminoids, 1500 mg/day of turmeric | ↓ hs-CRP in RCTs with ≤1000 mg/day and those with ≤10-week intervention period | |||
| Ashtary-Larky et al. 2021 [111] | 5 publications [23,48,50,71,76] | NAFLD, Mets, migraine, T2DM, hemodialysis | 279 | 28–68 | P | 6–12 | 40–120 mg/day of nano-curcumin | ↓ CRP (WMD = −1.29 mg/L; 95% CI −2.15 to −0.44; p = 0.003) | Cochrane risk of bias tool (55.6%) | PubMed, Scopus, Embase, and Web of Science |
| 3 publications [23,48,50] | NAFLD, Mets, migraine | 172 | 28–63 | P | 6–12 | 40–80 mg/day of nano-curcumin | ↓ IL-6 (WMD = −2.78 mg/dL; 95% CI −3.76 to −1.79; p <0.001) | |||
| 2 publications [50,112] | NAFLD, migraine | 122 | 28–49 | P | 8–12 | 40–80 mg/day of nano-curcumin | ↔ TNF-α (WMD = −3.09 mg/dL; 95% CI −8.75 to 2.57; p = 0.284) | |||
| Gorabi et al. 2021 [113] | 3 publications [47,86,98] | Knee OA, overweight | 307 | 18–65 | P | 4–16 | 1000 mg/day of curcuminoids, 500–900 mg/day of turmeric | ↓ IL-1 (WMD = −2.33 pg/mL; 95% CI −3.33 to −1.34; p < 0.001) | Jadad scale (not indicated) | PubMed/MEDLINE, Web of Science, Scopus, and Cochrane Library |
| 12 publications [24,43,46,47,50,54,55,56,86,87,103,114] | Mets, T2DM, overweight, knee OA, NAFLD, ESRD, diabetic nephropathy, infertility, UC | 760 | 18–65 | P | 4–12 | 80–1500 mg/day of curcumin, 300–1500 mg/day of curcuminoids, 112–1500 mg/day of turmeric | ↓ TNF-α (WMD = −1.61 pg/mL; 95% CI −2.72 to −0.51; p < 0.001) | |||
| 12 publications [24,45,46,47,48,50,54,86,103,107,109,114] | Mets, T2DM, overweight, knee OA, hyperlipidemia, ESRD, NAFLD, migraine | 808 | 18–65 | P | 4–12 | 80–1000 mg/day of curcumin, 300–1500 mg/day of curcuminoids, 112–1500 mg/day of turmeric | ↔ IL-6 (WMD = −0.33 pg/mL; 95% CI −0.99 to −0.34; p = 0.33) | |||
| 4 publications [46,86,87,107] | Diabetic nephropathy, chronic cutaneous, overweight | 240 | 18–65 | P | 4–8 | 1000 mg/day of curcuminoids, 112–1500 mg/day of turmeric | ↔ IL-8 (WMD = 0.52 pg/mL; 95% CI −1.13 to −2.17; p = 0.53) | |||
| Abdelazeem et al. 2021 [115] | 2 publications [58,73] | PCOS | 81 | 24–35 | P | 6–8 | 93.34–1000 mg/day of curcumin | ↔ CRP (MD = −0.55; 95% CI −1.64 to 0.54; p = 0.33) | Cochrane risk of bias tool (73.3%) | PubMed, EMBASE, Scopus, Web of Science, and Cochrane Central and Google Scholar |
| Ferguson et al. 2020 [116] | 22 publications [27,38,43,45,46,48,50,51,52,53,57,60,63,65,66,67,70,103,106,107,117,118] | Episodic migraine, T2DM, RA, oral lichen planus, healthy, CAD, hemodialysis patients with pruritus, history of sulfur mustard intoxication, Mets, sulfur mustard-induced cutaneous complications, infertile men, NAFLD, high cholesterol or/and high CRP, overweight/obese, COPD, acute Takayasu arteritis, prediabetes | 1266 | 30–70 | P, CO | 12 days–24 weeks | 46–4560 mg/day of curcumin | ↓ CRP (WMD = −1.55 mg/L; 95% CI −1.81 to −1.30; p < 0.05) | American Dietetic Association’s Quality Criteria Checklist (65.6%) | EMBASE, MEDLINE, CINAHL, Scopus, and Cochrane Library |
| 11 publications [24,45,46,50,63,86,103,107,114,117,118] | Episodic migraine, oral lichen planus, dyslipidemia, obese, healthy, history of sulfur mustard intoxication, Mets, sulfur mustard-induced cutaneous complications, T2DM | 778 | 36–70 | P, CO | 12 days–12 weeks | 80–4560 mg/day of curcumin | ↓ IL-6 (WMD = −1.69 pg/mL; 95% CI −2.56 to −0.82; p < 0.05) | |||
| 12 publications [24,43,46,50,63,67,86,112,114,118,119,120] | Episodic migraine, infertile men, healthy, dyslipidemia, NAFLD, overweight/obese, history of sulfur mustard intoxication, Mets, T2DM, acute Takayasu arteritis | 900 | 30–70 | P, CO | 4–12 | 80–1140 mg/day of curcumin | ↓ TNF-α (WMD = −3.13 pg/mL; 95% CI −4.62 to −1.64; p < 0.05) | |||
| 4 publications [46,63,86,107] | Dyslipidemia, obese, Mets, sulfur mustard-induced cutaneous complications | 539 | 38–56 | P, CO | 4 | 112–1140 mg/day of curcumin | ↓ IL-8 (WMD = −0.54 pg/mL; 95% CI −0.82 to −0.28; p < 0.05) | |||
| 3 publications [24,63,86] | Dyslipidemia, obese, Mets, history of sulfur mustard intoxication | 238 | 38–54 | P, CO | 4–8 | 665–1140 mg/day of curcumin | ↓ MCP-1 (WMD = −2.48 pg/mL; 95% CI −3.96 to −1.00; p < 0.05) | |||
| 2 publications [120,121] | Healthy, episodic migraine | 313 | 36–48 | P | 4–8 | 80–400 mg/day of curcumin | ↔ ICAM-1 (WMD = −86.24 ng/mL; 95% CI −206.80 to 34.32; p > 0.05) | |||
| White et al. 2019 [122] | 5 publications [25,45,46,53,106] | RA, Mets, hyperlipidemia, overweight/obese with CRP ≥ 2 mg/L, ESRD | 376 | 29–69 | P, CO | 4–13 | 20.1–500 mg/day of curcumin | ↔ CRP (MD = −2.71 mg/L; 95%CI −5.73 to 0.31; p = 0.08) | Cochrane risk of bias tool (Supple) | PubMed, Scopus, EMBASE, Web of Science, and Cochrane Library |
| 6 publications [27,51,52,54,57,103] | Mets, obese hyperlipidemia, CAD, knee OA, T2DM, Hemodialysis | 381 | 28–72 | P, CO | 4–12 | 22.1–2000 mg/day of curcumin | ↔ hs-CRP (MD = −1.44 mg/L; 95%CI −2.94 to 0.06; p = 0.06) | |||
| 2 publications [86,98] | Obesity, knee OA | 205 | 42–58.6 | P, CO | 8–12 | 500–1000 mg/day of curcumin | ↔ IL-1β (MD = −4.25 pg/mL; 95%CI −13.32 to 4.82; p = 0.36) | |||
| 7 publications [24,45,86,93,103,114,123] | T2DM, obese, Mets, hyperlipidemia, hemodialysis, knee OA, SLE | 478 | 20–69 | P, CO | 6–12 | 20.1–1000 mg/day of curcumin | ↔ IL-6 (MD = −0.71 pg/mL; 95%CI −1.68 to 0.25; p = 0.15) | |||
| 7 publications [46,86,87,103,114,123,124] | Mets, T2DM, obese, knee OA, hemodialysis, nephropathy | 408 | 34–66 | P, CO | 4–12 | 66.3–1000 mg/day of curcumin | ↔ TNF-α (MD = −1.23 pg/mL; 95%CI −3.01 to 0.55; p = 0.18) | |||
| Tabrizi et al. 2019 [125] | 5 publications [36,45,46,86,114] | Mets, obese, T2DM, hyperlipidemia | 293 | 18–75 | P | 4–8 | 294 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 112 mg/day of turmeric | ↓ IL-6 (SMD = −2.08; 95% CI −3.90 to −0.25; p = 0.02) | Cochrane risk of bias tool (82.9%) | Cochrane Library, Embase, PubMed, and Web of Science |
| 9 publications [25,27,39,45,46,52,57,110,126] | T2DM, Mets, hyperlipidemia, overweight, obese, coronary vascular artery | 832 | 18–75 | P | 3 days–36 weeks | 112–2400 mg/day of turmeric, 4000 mg/day of curcuminoids, 294–1890 mg/day of curcumin | ↓ hs-CRP (SMD = −0.65; 95% CI −1.20 to −0.10; p = 0.02) | |||
| 5 publications [24,46,86,87,114] | Mets, overweight, obese, T2DM, diabetic nephropathy | 291 | 18–75 | P | 4–8 | 112–1500 mg/day of turmeric, 300–1000 mg/day of curcuminoids | ↔ TNF-α (SMD = −1.62; 95% CI −3.60 to 0.36; p = 0.10) | |||
| Clark et al. 2019 [127] | 5 publications [30,31,36,38,41] | Mets, prediabetes, obese, T2DM | 652 | 27.1–59.37 | P | 6–39 | 200–1500 mg/day of curcumin | ↑ adiponectin (WMD = 0.82 Hedges’ g; 95% CI 0.33 to 1.30; p ˂ 0.001) ↑ adiponectin (WMD = 1.05 Hedges’ g; 95% CI 0.64 to 1.45; p ˂ 0.001) for ≤ 10 weeks of follow-up period | Jadad scale (100%) | PubMed/Medline, Scopus, Web of Science, Cochrane Library, and Google scholar |
| Simental-Mendía et al. 2019 [128] | 5 publications [31,39,41,129,130] | Mets, prediabetes, obese, T2DM | 686 | 18–71 | P | 4–36 | 500–1500 mg/day of curcumin | ↑ adiponectin (WMD = 6.47 ng/mL; 95% CI 1.85 to 11.10; p = 0.010) | Cochrane risk of bias tool (60.0%) | PubMed–Medline, Scopus, ISI Web of Science, and Google Scholar |
| Akbari et al. 2019 [131] | 3 publications [24,31,32] | Mets, obese, T2DM | 338 | 8–71 | P | 4–24 | 500–1000 mg/day of curcumin, 1500 mg/day of curcuminoids | ↓ leptin (SMD = −0.97; 95% CI −1.18 to −0.75; p < 0.001) | Cochrane risk of bias tool (77.8%) | Cochrane Library, EMBASE, PubMed, and Web of Science |
| 4 publications [24,31,32,39] | Mets, obese, T2DM | 572 | 8–71 | P | 4–36 | 500–1000 mg/day of curcumin, 1500 mg/day of curcuminoids | ↑ adiponectin (SMD = 1.05; 95% CI 0.23 to 1.87; p = 0.01) | |||
| Atkin et al. 2017 [132] | 4 publications [31,33,36,129] | T2DM, Mets, depression | 465 | 8–61 | P | 4–24 | 250–1000 mg/day of curcuminoids | ↓ leptin (SMD = −0.69; 95% CI −1.16 to −0.23; p = 0.003; I2 = 76.53%) | Jadad scale (40%) | PubMed, Medline, Scopus, Web of Science, and Google Scholar |
| Derosa et al. 2016 [133] | 9 publications [24,54,63,86,107,114,134,135,136] | Mets osteoarthritis, knee OA, oral lichen planus, obesity, T2DM, sulfur mustard intoxication, chronic pruritic skin lesions | 609 | 33–69 | P, CO | 2–32 | 200–6000 mg/day of curcumin | ↓ IL-6 (WMD = −0.60 pg/mL; 95% CI −1.06 to −0.14; p = 0.011) | Cochrane risk of bias tool (44.4%) | Medline, SCOPUS, Web of Science, and Google Scholar |
| Sahebkar et al. 2016 [137] | 9 publications [24,63,86,87,114,123,134,138,139] | Mets, obese, T2DM, type 2 diabetic nephropathy, major depressive disorder, knee OA, sulfur mustard-exposed veterans | 549 | 36–59 | P, CO | 4–12 | 300–1500 mg/day of curcumin | ↓ TNF-α (WMD = −4.69 pg/mL; 95% CI −7.10 to −2.28; p < 0.001) | Cochrane risk of bias tool (42.9%) | Medline, SCOPUS, Web of Science, and Google Scholar |
| Sahebkar et al. 2014 [140] | 7 publications [52,62,107,110,135,141,142] | Healthy, obese, dyslipidemia, chronic complications due to sulfur mustard, oral lichen planus, coronary artery bypass grafting, OA | 342 | 25–70 | P | 4–12 | 80–6000 mg/day of curcumin | ↓ CRP (MD = 6.44 mg/L; 95% CI −10.77 to −2.11; p = 0.004) | Jadad scale (66.7%) | Medline and SCOPUS |
| Ref. | No. of Studies Included | Health Status of Subjects | No. of Subjects | Age of Subjects (Years) | Design | Period (Weeks) | Dose | Outcomes (Effect Size) | Quality of Primary Studies | Databases |
|---|---|---|---|---|---|---|---|---|---|---|
| Qiu et al. 2023 [22] | 2 publications [26,27] | Mets | 165 | 34–64 | P | 6–12 | 80 mg/day of nano-curcumin, 1000 mg/day of curcuminoids | ↓ MDA (MD = −2.35 µmol/L; 95% CI −4.47 to −0.24; p = 0.03) | Cochrane risk of bias tool (71.4%) | PubMed, SCOPUS, Cochrane Library, EMBASE, Web of Science, and China Biological Medicine |
| Dehzad et al. 2023 [42] | 16 publications [23,30,43,49,57,68,76,77,78,79,80,82,88,143,144,145] | Mets, obese, T2DM, prostate cancer, PUD, NAFLD, hemodialysis, infertile men, β-thalassemia, hyperlipidemia, coronary elective angioplasty, DFU, healthy | 857 | 18–70 | P | 4–12 | 80–3000 mg/day of curcumin, 2000–3000 mg/day of turmeric | ↑ TAC (WMD = 0.21 mmol/L; 95% CI 0.08 to 0.33; I2 = 99.6%; p < 0.001) | Cochrane risk of bias tool (84.2%) | PubMed, Scopus, Web of Science, Cochrane Library, and Google Scholar |
| 18 publications [23,43,53,57,60,68,76,77,78,79,80,81,82,92,98,143,144,146] | Mets, hemodialysis, chronic pulmonary complications, T2DM, knee OA, beta-thalassemia, healthy, Takayasu arteritis, infertile men, NAFLD, HIV, hyperlipidemia, coronary elective angioplasty, DFU | 1475 | 18–70 | P | 4–16 | 80–1500 mg/day of curcumin, 1500 mg/day of curcuminoids, 1500–3000 mg/day of turmeric | ↓ MDA (WMD = −0.33 µmol/L; 95% CI −0.53 to −0.12; I2 = 99.6%; p < 0.001) | |||
| 7 publications [60,63,64,79,95,145,147] | T2DM, solid tumor, prostate cancer, chronic pulmonary complications, PCOS, coronary elective angioplasty, chronic bronchial asthma | 497 | 18–70 | P | 4–12 | 80–3000 mg/day of curcumin, 180–1500 mg/day of curcuminoids | ↑ SOD (WMD = 20.51 u/L; 95% CI 7.35 to 33.67; I2 = 95.4%; p < 0.001) | |||
| Jakubc-zyk et al. 2020 [148] | 3 publications [43,109,143] | Overweight/obese, infertile, β-thalassemia major patients | 177 | 13–45 | P | 10–12 | 80–1000 mg/day of curcumin | ↑ TAC (SMD = 2.696; Z = 2.003; 95% CI = 0.058 to 5.335; p = 0.045) | Cochrane risk of bias tool (57.1%) | PubMed/MEDLINE and Embase |
| 3 publications [43,109,143] | Overweight/obese, infertile, β-thalassemia major patients | 177 | 13–45 | P | 10–12 | 80–1000 mg/day of curcumin | ↔ MDA (SMD = −1.579, Z = −1.714, CI = 95%, p = 0.086) | |||
| Tabrizi et al. 2019 [125] | 5 publications [27,57,110,114,124] | Mets, T2DM, coronary vascular artery | 425 | 18–70 | P | 3 days– 8 weeks | 300–4000 mg/day of curcuminoids, 2000 mg/day of turmeric | ↓ MDA (SMD = −3.14; 95% CI −4.76 to −1.53; p < 0.001) | Cochrane risk of bias tool (82.9%) | Cochrane Library, Embase, PubMed, and Web of Science |
| 3 publications [27,124,149] | Mets, obese, T2DM, | 260 | 18–65 | P | 4–8 | 1000 mg/day of curcuminoids | ↔ SOD (SMD 0.34; 95% CI −1.06 to 1.74, p = 0.63) | |||
| Alizadeh et al. 2019 [150] | 12 publications [27,43,98,124,143,151,152,153,154,155,156,157] | Mets, knee OA, T2DM, healthy, infertile oligoasthenospermia, non-diabetic or diabetic proteinuric CKD, chronic gastritis, β-thalassemia, hemodialysis, sulfur mustard Iraq–Iran war chronic pulmonary complications, solid cancer | 1005 | 20–75 | P | 1–16 | 80–1000 mg/day of curcumin, 90–1500 mg/day of curcuminoids, 1500–2100 mg/day of turmeric | ↓ MDA (SMD = −0.46; 95% CI −0.68 to −0.25) | Cochrane risk of bias tool (59.0%) | PubMed, Embase, Cochrane Central, Scopus, and Google Scholar |
| 7 publications [62,124,141,145,155,156,158] | Healthy, prostate cancer treated with radiotherapy, veterans of the Iraq–Iran war with chronic pruritus, sulfur mustard Iraq–Iran war chronic pulmonary complications, solid cancer, Mets, knee OA, T2DM | 618 | 35–79 | P | 4–12 | 900–3000 mg/day of curcuminoids | ↑ SOD (SMD = 0.82; 95% CI 0.27 to 1.38) | |||
| 5 publications [62,141,143,145,155] | Healthy, prostate cancer treated with radiotherapy, β-thalassemia, veterans of the Iraq–Iran war with chronic pruritus, solid cancer | 322 | 20–79 | P | 4–12 | 900–3000 mg/day of curcuminoids | ↑ CAT (SMD = 10.26; 95% CI 0.92 to 19.61) | |||
| 5 publications [62,141,145,151,158] | Non-diabetic or diabetic proteinuric CKD, prostate cancer treated with radiotherapy, veterans of the Iraq-Iran war with chronic pruritus, occupational stress-related anxiety and fatigue | 357 | 26–79 | P | 4–12 | 320–782 mg/day of curcumin, 1000–3000 mg/day of curcuminoids | ↑ GPx (SMD = 8.90; 95% CI 6.62 to 11.19) | |||
| 6 publications [43,88,143,145,152,157] | PUD, infertile oligoasthenospermia, prostate cancer treated with radiotherapy, β-thalassemia, chronic gastritis, healthy | 330 | 22–79 | P | 1–12 | 80–1500 mg/day of curcumin, 90–3000 mg/day of curcuminoids | ↔ TAC (SMD = 0.30; 95% CI −0.20 to 0.81) | |||
| 1 publication [151] | Non-diabetic or diabetic proteinuric CKD | 101 | 37–57 | P | 8 | 320 mg/day of curcumin | ↔ GR (SMD = −0.01; 95% CI −0.03 to 0.02) | |||
| Qin et al. 2018 [159] | 7 publications [27,57,98,114,124,153,156] | T2DM, OA, Mets, end-stage renal disease | 525 | 34–67 | P | 4–8 | 46–1000 mg/day of curcumin | ↓ MDA (SMD = −0.769; 95% CI −1.059 to −0.478) | Cochrane risk of bias tool (54.2%) | PubMed, EMBASE, Web of Science, Medline Ovid, Books@Ovid, Journals@Ovid, and Cochrane Library |
| 4 publications [27,124,141,156] | T2DM, OA, Mets, chronic pruritic skin lesions | 341 | 34–67 | P | 4–8 | 1000–1500 mg/day of curcumin | ↑ SOD (SMD = 1.084; 95% CI 0.487 to 1.680) | |||
| 2 publications [57,153] | T2DM, end-stage renal disease | 108 | 32–67 | P | 4–8 | 46–66.3 mg/day of curcumin | ↔ GPx (SMD = 0.13; 95% CI −0.25 to 0.51) |
| Ref. | No. of Studies Included | Health Status of Subjects | No. of Subjects | Age of Subjects (Years) | Design | Period (Weeks) | Dose | Outcomes (Effect Size) | Quality of Primary Studies | Databases |
|---|---|---|---|---|---|---|---|---|---|---|
| Lukkunaprasit et al. 2023 [160] | 3 publications [50,161,162] | MAFLD | 231 | 26–38 | P | 8–12 | 80–500 mg/day of curcumin | ↔ HbA1c (MD = −0.24; 95% CI −0.66 to 0.18; p > 0.05) | Cochrane risk of bias tool (68.8%) | Medline and SCOPUS |
| 12 publications [34,35,50,146,161,162,163,164,165,166,167,168] | MAFLD | 710 | 18–72 | P | 8–24 | 80–1500 mg/day of curcumin, 2000–3000 mg/day of turmeric | ↓ FBG (MD = −2.05 mg/dL; 95% CI −3.08 to −1.01; p < 0.05) | |||
| Qiu et al. 2023 [22] | 9 publications [23,25,27,61,126,169,170,171,172] | Mets | 576 | 28–81 | P | 4–12 | 80–1500 mg/day of curcumin, 1000 mg/day of curcuminoids, 2400 mg/day of turmeric | ↓ FBG (MD = −8.6 mg/dL; 95% CI −15.45 to −1.75; p = 0.01) | Cochrane risk of bias tool (71.4%) | PubMed, SCOPUS, Cochrane Library, EMBASE, Web of Science, and China Biological Medicine |
| Różański et al. 2023 [173] | 14 publications [34,35,50,55,161,164,165,166,174,175,176,177,178,179] | MAFLD | 847 | 18–70 | P | 8–12 | 70–1500 mg/day of curcuminoids, 80–1000 mg/day of curcumin, 3000 mg/day of turmeric | ↓ Insulin (MD = −1.1430 μIU/mL; 95% CI −1.5439 to −0.7421; p < 0.0001) ↓ HOMA-IR (MD = −0.2884; 95%CI −0.3950 to −0.1817; p < 0.0001) | Cochrane risk of bias tool (90.8%) | PubMed, Web of Science, and Scopus |
| Ngu et al. 2022 [180] | 3 publications [50,177,181] | NAFLD | 238 | 18–70 | P | 8–12 | 80–1500 mg/day of curcumin | ↔ QUICKI (MD = 0.01; 95% CI −0.00 to 0.02; p = 0.30) | Cochrane risk of bias tool (79.5%) | Cochrane Central Register of Controlled Trials, and PubMed |
| Sun et al. 2022 [100] | 23 publications [23,25,27,39,45,49,60,61,70,76,80,87,101,126,169,170,182,183,184,185,186,187,188] | T2DM, obese, nephropathy, proteinuria, hemodialysis, DFU, IFG/IGT, Mets, hyperlipidemia | 1847 | 35–68 | P, CO | 4–36 | 80–2400 mg/day of curcumin | ↓ FBG (WMD = −0.50 mg/dL; 95% CI −0.72 to −0.28) | Cochrane risk of bias tool (69.3%) Jadad scale (77.0%) | PubMed, Embase, Web of Science, CNKI, Wanfang and CBM |
| 16 publications [27,29,39,49,60,70,76,80,101,126,182,183,185,186,187,188] | T2DM, obese, proteinuria, hemodialysis, DFU, IFG/IGT, Mets, hyperlipidemia | 1224 | 35–70 | P, CO | 8–36 | 80–2100 mg/day of curcumin | ↓ Hb1Ac (WMD = −0.42%; 95% CI −0.57 to −0.26) | |||
| 5 publications [45,76,80,187,188] | T2DM, IGT, hyperlipidemia, hemodialysis, DFU | 247 | 35–63 | P, CO | 6–17 | 80–500 mg/day of curcumin | ↓ Insulin (WMD = −1.70 μIU/mL; 95% CI −2.03 to −1.38) | |||
| 11 publications [39,45,49,60,70,76,80,101,183,188,189] | T2DM, obese, hyperlipidemia, hemodialysis, IFG, IGT, DFU | 874 | 42–63 | P, CO | 6–36 | 80–2100 mg/day of curcumin | ↓ HOMA-IR (WMD = −0.71; 95% CI −1.11 to −0.31) | |||
| Tian et al. 2022 [190] | 9 publications [38,49,57,87,101,114,182,183,191] | T2DM | 604 | 41–61 | P | 4–12 | 80–1500 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 1500–2100 mg/day of turmeric | ↓ FBG (WMD = −8.85 mg/dL; 95% CI −14.4 to −3.29; p = 0.002) | Cochrane risk of bias tool (57.1%) | PubMed, EMBASE, Web of Science, and Cochrane Library |
| 8 publications [38,49,57,101,114,182,183,191] | T2DM | 564 | 41–61 | P | 4–12 | 80–1500 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 2100 mg/day of turmeric | ↓ HbA1c (WMD = −0.54; 95% CI −0.81 to −0.27; p ≤ 0.001) | |||
| Nouri et al. 2022 [192] | 4 publications [58,73,193,194] | PCOS | 198 | 28–31 | P | 6–12 | 93.34–1500 mg/day of curcumin | ↓ FBG (ES = −3.62 mg/dL; 95% CI −5.65 to −1.58; p < 0.001) ↓ Insulin (ES = −1.67 mU/mL; 95% CI −3.06 to −0.28; p = 0.018) ↓ HOMA-IR (ES = −0.42; 95% CI −0.76 to −0.09; p < 0.01) | Cochrane risk of bias tool (75.0%) | PubMed, Scopus, and ISI Web of Science |
| Khalili et al. 2022 [195] | 9 publications [34,50,161,164,165,166,177,179,196] | NAFLD | 683 | 42–67 | P | 4–12 | 50–2000 mg/day of curcumin | ↓ FBG (SMD = −0.28; 95% CI −0.46 to −0.09; p = 0.003) | Cochrane risk of bias tool (65.5%) | Web of Science, Science Direct, PubMed, and Embase |
| Shen et al. 2022 [99] | 7 publications [58,73,193,194,197,198,199] | PCOS | 447 | 20–38 | P | 6–24 | 80–1500 mg/day of curcumin | ↓ FBG (WMD = −3.618; 95% CI −5.165 to −2.071; p < 0.001) ↓ Insulin (WMD = −1.834; 95% CI −2.701 to −0.968; p < 0.001) ↓ HOMA-IR (WMD = −0.565; 95% CI −0.779 to −0.351; p < 0.001) | Cochrane risk of bias tool (73.5%) | PubMed, Embase, Cochrane Library, Web of Science, Scopus, Clinical Trials, Chinese Clinical Trial Registry, Chinese Biomedical Literature Database, Chinese National Knowledge Infrastructure, VIP database, and Wanfang Database |
| 4 publications [58,193,194,197] | PCOS | 266 | 23–38 | P | 6–12 | 80–1500 mg/day of curcumin | ↑ QUICKI (WMD = 0.011; 95% CI 0.005 to 0.017; p = 0.001) | |||
| Ashtary-Larky et al. 2021 [111] | 7 publications [23,50,71,76,171,182,185] | Mets, NAFLD, T2DM, hemodialysis | 417 | 36–68 | P | 6–12 | 40–120 mg/day of nano-curcumin | ↓ FBG (WMD = −18.14 mg/dL; 95% CI −29.31 to −6.97; p = 0.001) | Cochrane risk of bias tool (55.6%) | PubMed, Scopus, Embase, and Web of Science |
| 3 publications [50,76,171] | Mets, NAFLD, T2DM, hemodialysis | 180 | 36–68 | P | 12 | 40–80 mg/day of nano-curcumin | ↓ Insulin (WMD = −1.21 mg/dL; 95% CI −1.43 to −1.00; p < 0.001) | |||
| 4 publications [50,171,182,185] | Mets, NAFLD, T2DM | 277 | 36–68 | P | 8–12 | 40–80 mg/day of nano-curcumin | ↓ HbA1c (WMD = −0.66 mg/dL; 95% CI −1.41 to −0.08; p < 0.001) | |||
| 3 publications [50,76,171] | Mets, NAFLD, T2DM, hemodialysis | 180 | 36–68 | P | 12 | 40–80 mg/day of nano-curcumin | ↓ HOMA-IR (WMD = −0.28 mg/dL; 95% CI −0.33 to −0.23; p < 0.001) | |||
| Abdelazeem et al. 2021 [115] | 5 publications [58,73,193,194,197] | PCOS | 296 | 24–39 | P | 6–12 | 80–1500 mg/day of curcumin | ↓ FBG (MD = −3.67; 95% CI −5.25 to −2.08; p < 0.00001) ↓ Insulin (MD = −1.91; 95% CI −2.97 to −0.84; p = 0.0005) ↓ HOMA-IR (MD = −0.55; 95% CI −0.83 to −0.27; p = 0.0001) | Cochrane risk of bias tool (73.3%) | PubMed, EMBASE, Scopus, Web of Science, Cochrane Central, and Google Scholar |
| 4 publications [58,193,194,197] | PCOS | 266 | 24–36 | P | 6–12 | 80–1500 mg/day of curcumin | ↓ QUICKI (MD = 0.01; 95% CI 0.00 to 0.02; p = 0.0005) | |||
| Zhang et al. 2021 [200] | 5 publications [31,60,70,183,185] | T2DM | 524 | 34–70 | P | 8–24 | 80–1500 mg/day of curcumin, 300–1500 mg/day of curcuminoids | ↓ HbA1c (WMD = −0.70; 95% CI −0.87 to −0.54; p < 0.0001) | Cochrane risk of bias tool (69.4%) | Chinese database (CNKI, Wan Fang, VIP, CBM), PubMed, EMBASE, Cochrane Library, Web of Science, Medline Complete and, ClinicalTrials.gov |
| 1 publication [60] | T2DM | 100 | 34–51 | P | 12 | 1000 mg/day of curcuminoids | ↓ HOMA-IR in the Middle East subgroup (WMD = −0.60; 95% CI −0.74 to −0.46; p < 0.00001) | |||
| 2 publications [31,183] | T2DM | 313 | 34–65 | P | 12–24 | 1500 mg/day of curcumin, 300 mg/day of curcuminoids | ↓ HOMA-IR in the Asia subgroup (WMD = −2.41; 95% CI −4.44 to −0.39; p = 0.02) | |||
| 6 publications [31,60,70,87,183,185] | T2DM | 564 | 34–70 | P | 8–24 | 80–1500 mg/day of curcumin, 300–1500 mg/day of curcuminoids, 1500 mg/day of turmeric | ↓ FBG in the Asia subgroup (SMD = −0.57; 95% CI −0.79 to −0.36; p < 0.00001) ↔ FBG in the Middle East subgroup | |||
| Altobelli et al. 2021 [201] | 5 publications [49,114,144,182,183] | T2DM | 333 | 18–80 | P | 8–12 | 80–1500 mg/day of curcumin, 300 mg/day of curcuminoids, 2100 mg/day of turmeric | ↓ HbA1c (ES = −0.42; 95% CI −0.77 to −0.11; p = 0.008) | Cochrane risk of bias tool (93.8%) | Medline, EMBASE, Scopus, ClinicalTrials.gov, Web of Science, and Cochrane Library |
| 4 publications [31,49,144,183] | T2DM | 432 | 18–70 | P | 8–24 | 1500 mg/day of curcumin, 250–300 mg/day of curcuminoids, 2100 mg/day of turmeric | ↓ HOMA-IR (ES = −0.41; 95% CI −0.60 to −0.22; p < 0.001) | |||
| Chien et al. 2021 [202] | 3 publications [58,193,194] | PCOS | 168 | 24–39 | P | 6–12 | 500–1500 mg/day of curcumin | ↓ FBG (MD = −2.77; 95% CI −4.16 to −1.38; p < 0.001) ↓ Insulin (MD = −1.33; 95% CI −2.18 to −0.49; p = 0.002) ↓ HOMA-IR (MD = −0.32; 95% CI −0.52 to −0.12; p = 0.002) ↓ QUICKI (MD = 0.010; 95% CI 0.003 to 0.018; p = 0.005) | Cochrane risk of bias tool (72.2%) | PubMed, Embase, Scopus, Web of Science, and Cochrane Library |
| Jalali et al. 2020 [203] | 6 publications [34,50,161,164,165,177] | NAFLD | 407 | 33–58 | P | 8–12 | 50–1425 mg/day of curcumin | ↔ FBG (MD = −0.22; 95% CI −0.42 to −0.02; p = 0.313) | Jadad scale (88.9%) | PubMed, Embase, Scopus, Web of Science, and Cochrane Library |
| 3 publications [50,165,177] | NAFLD | 211 | 36–58 | P | 8–12 | 80–1425 mg/day of curcumin | ↓HOMA-IR (MD = −0.37; 95% CI −0.70 to −0.03; p = 0.000) ↓ Insulin (MD = −0.49; 95% CI −0.81 to −0.16; p = 0.000) | |||
| Azhda-ri et al. 2019 [204] | 5 publications [25,27,61,126,172] | Mets | 359 | 38–60 | P | 6–12 | 1000–1890 mg/day of curcumin, 1000 mg/day of curcuminoids, 2400 mg/day of turmeric | ↓ FBG (WMD = −9.18 mg/dL; 95% CI −16.70 to −1.66; p = 0.01) | Cochrane risk of bias tool (57.1%) | Web of Science, Medline, Google Scholar, Scopus, Cochrane, and CINAHL |
| Huang et al. 2019 [205] | 13 publications [25,35,39,45,51,57,114,126,161,177,182,183,206] | T2DM, NAFLD, Mets, hyperlipidemia, CAD, high ALT | 1064 | 30–72 | P, CO | 4–12 | 70–1890 mg/day of curcumin, 294–2000 mg/day of curcuminoids, 2400–3000 mg/day of turmeric | ↓ FBG (SMD = −0.382; 95% CI −0.654 to −0.111 mg/dL; p = 0.006) | Cochrane risk of bias tool (83.7%) | PubMed, Cochrane Library, Web of Science, and Embase |
| 7 publications [31,35,39,45,57,177,183] | T2DM, NAFLD, Mets, hyperlipidemia | 821 | 30–72 | P, CO | 4–12 | 1000 mg/day of curcumin, 294–1500 mg/day of curcuminoids, 2000–3000 mg/day of turmeric | ↓ HOMA-IR (SMD = −0.351; 95% CI −0.615 to −0.087; p = 0.009) | |||
| 8 publications [39,57,114,126,161,177,182,183] | T2DM, NAFLD, Mets | 731 | 40–74 | P | 4–12 | 80–1890 mg/day of curcumin, 300–1500 mg/day of curcuminoids, 2000 mg/day of turmeric | ↓ HbA1c (SMD = −0.370; 95% CI −0.631% to −0.110%; p = 0.005) | |||
| 5 publications [35,39,45,57,177] | T2DM, NAFLD, Mets, hyperlipidemia | 507 | 31–71 | P, CO | 4–12 | 1000 mg/day of curcumin, 294–1500 mg/day of curcuminoids, 2000–3000 mg/day of turmeric | ↔ Insulin (SMD = −0.058; 95% CI −0.352 to 0.235; p = 0.697) | |||
| Tabrizi et al. 2018 [207] | 19 publications [25,32,39,45,46,51,57,87,101,114,126,129,161,178,182,183,206,208,209] | T2DM, hyperlipidemia, Mets, obese, diabetic nephropathy, NAFLD, CAD | 1299 | 10–73 | P | 4–24 | 70–2000 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 112–2400 mg/day of turmeric | ↓ FBG (SMD = −0.78; 95% CI −1.20 to −0.37; p < 0.001) | Cochrane risk of bias tool (76.9%) | Cochrane Library, EMBASE, MEDLINE, and Web of Science |
| 7 publications [32,39,45,57,129,178,208] | T2DM, obese, hyperlipidemia, NAFLD | 552 | 18–68 | P | 4–36 | 294 mg/day of curcumin, 500–1000 mg/day of curcuminoids, 2000–2100 mg/day of turmeric | ↑ Insulin (SMD = 0.92; 95% CI 0.06 to 1.78; p = 0.036) | |||
| 8 publications [31,32,39,45,57,178,183,208] | T2DM, obese, hyperlipidemia, NAFLD | 836 | 10–65 | P | 4–36 | 294 mg/day of curcumin, 500–1000 mg/day of curcuminoids, 300–2100 mg/day of turmeric | ↓ HOMA-IR (SMD = −0.91; 95% CI −1.52 to −0.31; p = 0.003) | |||
| 10 publications [39,57,101,114,126,161,178,182,183,208] | T2DM, Mets, obese, hyperlipidemia, NAFLD | 906 | 18–73 | P | 4–36 | 70–1890 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 300–2100 mg/day of turmeric | ↓ HbA1c (SMD = −0.92; 95% CI −1.37 to −0.47; p < 0.001) |
| Ref. | No. of Studies Included | Health Status of Subjects | No. of Subjects | Age of Subjects (Years) | Design | Period (Weeks) | Dose | Outcomes (Effect Size) | Quality of Primary Studies | Databases |
|---|---|---|---|---|---|---|---|---|---|---|
| Lukkunaprasit et al. 2023 [160] | 11 publications [34,50,146,161,162,163,164,165,166,167,168] | MAFLD | 335 | 21–72 | P | 8–24 | 80–1500 mg/day of curcumin, 2000 mg/day of turmeric | ↓ TC (MD = −8.18 mg/dL; 95% CI −14.07 to −2.29; p < 0.05) ↔ TG (MD = −12.03 mg/dL; 95% CI −24.36 to 0.30; p = 0.27) ↔ LDL-C (MD = −4.35 mg/dL; 95% CI −10.93 to 2.23; p = 0.73) | Cochrane risk of bias tool (68.8%) | Medline and SCOPUS |
| 10 publications [34,50,146,161,162,164,165,166,167,168] | MAFLD | 325 | 28–59 | P | 8–12 | 80–1500 mg/day of curcumin, 2000 mg/day of turmeric | ↔ HDL-C (MD = 0.80 mg/dL; 95% CI −2.92 to 4.52; p = 0.41) | |||
| Qiu et al. 2023 [22] | 8 publications [23,25,61,126,169,170,171,172] | Mets | 476 | 28–81 | P | 4–12 | 80–1890 mg/day of curcumin, 2400 mg/day of turmeric | ↔ TG (MD = 1.28 mg/dL; 95% CI −3.75 to 6.30; p = 0.62) ↓ HDL-C (MD = 4.98 mg/dL; 95% CI 2.58 to 7.38; p < 0.0001) | Cochrane risk of bias tool (71.4%) | PubMed, SCOPUS, Cochrane Library, EMBASE, Web of Science, and China Biological Medicine |
| Rozanski et al. 2023 [173] | 14 publications [34,35,50,55,161,164,165,166,174,175,176,177,178,179] | MAFLD | 847 | 18–70 | P | 8–12 | 70–1500 mg/day of curcuminoids, 80–1000 mg/day of curcumin, 3000 mg/day of turmeric | ↓ TG (MD = −12.6001 mg/dL; 95% CI −22.9311 to −2.2692; p = 0.0168) ↓ TC (MD = −15.7896 mg/dL; 95% CI −28.2686 to −3.3106; p = 0.0131) ↓ LDL-C (MD = −14.1699 mg/dL; 95% CI −25.9117 to −2.4281; p = 0.018) | Cochrane risk of bias tool (90.8%) | PubMed, Web of Science, and Scopus |
| Ngu et al. 2022 [180] | 10 publications [34,50,161,162,163,164,165,166,177,196] | NAFLD | 771 | 18–70 | P | 8–24 | 50–1500 mg/day of curcumin, 2000 mg/day of turmeric | ↓ TC (MD = −11.86; 95% CI −19.25 to −4.46; p = 0.002) ↔ LDL-C (MD = −8.78; 95% CI −18.74 to 1.18; p = 0.08) ↓ TG (MD = −13.00; 95% CI −27.94 to 1.94; p = 0.09) | Cochrane risk of bias tool (79.5%) | Cochrane Central Register of Controlled Trials and PubMed |
| 9 publications [34,50,161,162,164,165,166,177,196] | NAFLD | 638 | 18–70 | P | 8–12 | 50–1500 mg/day of curcumin, 2000 mg/day of turmeric | ↔ HDL-C (MD = 0.43; 95% CI −3.88 to 4.74; p = 0.85) | |||
| Shen et al. 2022 [99] | 5 publications [58,73,193,197,199] | PCOS | 380 | 20–38 | P | 6–12 | 80–1500 mg/day of curcumin | ↓ TC (WMD = −15.591; 95% CI −27.908 to −3.273; p = 0.013) ↔ TG (WMD = −8.889; 95% CI −27.246 to 9.468; p = 0.343) ↔ LDL-C (WMD = −6.427; 95% CI −17.343 to 4.489; p = 0.249) ↔ HDL-C (WMD = 3.713; 95% CI −0.786 to 8.211; p = 0.106) | Cochrane risk of bias tool (73.5%) | PubMed, Embase, Cochrane Library, Web of Science, Scopus, Clinical Trials, Chinese Clinical Trial Registry, Chinese Biomedical Literature Database, Chinese National Knowledge Infrastructure, VIP database, and Wanfang Database |
| Tian et al. 2022 [190] | 9 publications [38,49,57,87,101,114,182,183,191] | T2DM | 604 | 41–61 | P | 4–12 | 80–1500 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 1500–2100 mg/day of turmeric | ↓ TG (WMD = −18.97 mg/dL; 95% CI −36.47 to −1.47; p = 0.03) | Cochrane risk of bias tool (57.1%) | PubMed, EMBASE, Web of Science, and Cochrane Library |
| 9 publications [38,49,57,87,101,114,182,183,191] | T2DM | 604 | 41–61 | P | 4–12 | 80–1500 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 1500–2100 mg/day of turmeric | ↓ TC (WMD = −8.91 mg/dL; 95% CI −14.18 to −3.63; p = 0.001) | |||
| 9 publications [38,49,57,87,101,114,182,183,191] | T2DM | 604 | 41–61 | P | 4–12 | 80–1500 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 1500–2100 mg/day of turmeric | ↔ LDL-C (WMD = −4.01 mg/dL; 95% CI −10.96 to 2.95; p = 0.259) | |||
| 9 publications [38,49,57,87,101,114,182,183,191] | T2DM | 604 | 41–61 | P | 4–12 | 80–1500 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 1500–2100 mg/day of turmeric | ↔ HDL-C (WMD = 0.32 mg/dL; 95% CI −0.74 to 1.37; p = 0.557) | |||
| Sun et al. 2022 [100] | 16 publications [25,38,45,49,61,70,76,80,126,169,170,184,186,188,209,210] | Mets, hyperlipidemia, hypercholesterolemia, T2DM, DFU, IGT, IFG, proteinuria, hemodialysis | 1274 | 38–68 | P, CO | 4–16 | 80–2400 mg/day of curcumin | ↔ TC (WMD = −2.45 mg/dL; 95% CI −9.00 to 4.09; p = 0.063) | Cochrane risk of bias tool (69.3%) Jadad scale (77.0%) | PubMed, Embase, Web of Science, CNKI, Wanfang, and CBM |
| 19 publications [23,25,29,38,45,49,61,70,76,126,169,170,182,183,184,186,188,209,210] | Mets, obese, hyperlipidemia, hypercholesterolemia, T2DM, DFU, IGT, IFG, proteinuria, hemodialysis | 1561 | 38–70 | P, CO | 4–24 | 80–2100 mg/day of curcumin | ↔ TG (WMD = −10.50 mg/dL; 95% CI −23.18 to 2.18; p = 0.105) | |||
| 19 publications [23,25,29,38,45,49,61,70,76,126,169,170,182,183,184,186,188,209,210] | Mets, obese, hyperlipidemia, hypercholesterolemia, T2DM, DFU, IGT, IFG, proteinuria, hemodialysis | 1561 | 38–70 | P, CO | 4–24 | 80–2100 mg/day of curcumin | ↑ HDL-C (WMD = 1.73 mg/dL; 95% CI 0.78 to 2.68; p < 0.001) | |||
| 17 publications [25,29,38,45,49,61,70,76,80,169,170,183,184,186,188,209,210] | Mets, obese hyperlipidemia, hypercholesterolemia, T2DM, DFU, IGT, IFG, proteinuria, hemodialysis | 1256 | 39–70 | P, CO | 4–24 | 80–2100 mg/day of curcumin | ↔ LDL-C (WMD = −3.99 mg/dL; 95% CI −8.68 to 0.68; p = 0.094) | |||
| Saeedi et al. 2022 [211] | 10 publications [25,51,101,126,164,165,177,184,191,209] | T2DM, CVD, Mets, dyslipidemia, NAFLD | 726 | 18–65 | P | 4–12 | 50–2000 mg/day of curcumin, 1000 mg/day of curcuminoids, 2100 mg/day of turmeric | ↔ TG (SMD = −0.05; 95% CI −0.20 to 0.11; p = 0.56) ↔ TC (SMD = −0.21; 95% CI −0.55 to 0.13; p = 0.22) ↔ LDL-C (SMD = −0.17; 95% CI −0.43 to 0.09; p = 0.82) ↔ HDL-C (SMD = −0.04; 95% CI −0.36 to 0.29; p = 0.82) | Cochrane risk of bias tool (not indicate) | Ovid-Medline, Web of Science, Scopus, Cochrane, Embase, and ProQuest |
| Futuhi et al. 2022 [102] | 5 publications [71,72,76,151,212] | ESRD, diabetic proteinuric non-diabetic proteinuric CKD, hemodialysis | 276 | 23–69 | P | 8–12 | 80–500 mg/day of curcumin, 2500 mg/day of turmeric | ↓ TC (WMD = −13.77 mg/dL; 95% CI −26.77 to −0.77; p = 0.04) | Cochrane risk of bias tool (73.0%) | PubMed, Scopus, Cochrane Library, and Web of Science |
| 5 publications [71,72,76,151,212] | ESRD, diabetic proteinuric non-diabetic proteinuric CKD, hemodialysis | 276 | 23–69 | P | 8–12 | 80–500 mg/day of curcumin, 2500 mg/day of turmeric | ↔ TG (WMD = −6.37 mg/dL; 95% CI −26.59 to 13.85; p = 0.54) | |||
| 4 publications [71,72,76,212] | ESRD, hemodialysis | 175 | 23–69 | P | 12 | 80–500 mg/day of curcumin, 2500 mg/day of turmeric | ↔ LDL-C (WMD = −5.65 mg/dL; 95% CI −20.81 to 9.50; p = 0.46) | |||
| 4 publications [71,72,76,212] | ESRD, hemodialysis | 175 | 23–69 | P | 12 | 80–500 mg/day of curcumin, 2500 mg/day of turmeric | ↔ HDL-C (WMD = 0.16 mg/dL; 95% CI −2.55 to 2.88; p = 0.91) | |||
| Khalili et al. 2022 [195] | 8 publications [34,50,161,165,166,177,179,196] | NAFLD | 638 | 42–67 | P | 4–12 | 50–2000 mg/day of curcumin | ↓ TG (SMD = −0.49; 95% CI −0.71 to −0.27; p = 0.000) | Cochrane risk of bias tool (65.5%) | Web of Science, Science Direct, PubMed, and Embase |
| 9 publications [34,50,161,164,165,166,177,179,196] | NAFLD | 683 | 42–67 | P | 4–12 | 50–2000 mg/day of curcumin | ↔ LDL-C (SMD = 0.48; 95% CI −0.97 to 0.01; p = 0.053) | |||
| 9 publications [34,50,161,164,165,166,177,179,196] | NAFLD | 683 | 42–67 | P | 4–12 | 50–2000 mg/day of curcumin | ↓ TC (SMD = 0.81; 95% CI −1.34 to −0.27; p = 0.003) | |||
| 8 publications [34,161,164,165,166,177,179,196] | NAFLD | 599 | 42–67 | P | 4–12 | 50–2000 mg/day of curcumin | ↔ HDL-C (SMD = 0.03; 95% CI −0.38 to 0.44; p = 0.886) | |||
| Zhang et al. 2021 [200] | 2 publications [31,183] | T2DM | 313 | 18–65 | P | 12–24 | 1500 mg/day of curcumin, 300 mg/day of curcuminoids | In the Asia subgroup, ↓ TC (WMD = −23.45 mg/dL; 95% CI −40.04 to −6.84; p = 0.006) ↓ TG (WMD = −54.14 mg/dL; 95% CI −95.71 to −12.57; p = 0.01) | Cochrane risk of bias tool (69.4%) | Chinese database (CNKI, Wan Fang, VIP, CBM), PubMed, EMBASE, Cochrane Library, Web of Science, Medline Complete, and ClinicalTrials.gov |
| 2 publications [87,101] | T2DM | 140 | 34–62 | P | 8–12 | 1000 mg/day of curcuminoids, 1500 mg/day of turmeric | In the Middle East subgroup, ↔ TC (WMD = 22.91; 95% CI −16.94 to 62.75; p = 0.26) ↔ TG (WMD = −4.56; 95% CI −19.28 to 10.16; p = 0.54) | |||
| 2 publications [31,183] | T2DM | 313 | 18–65 | P | 12–24 | 1500 mg/day of curcumin, 300 mg/day of curcuminoids | ↓ LDL-C in patients with T2DM in the Asia subgroup only (WMD = −20.85 mg/dL; 95% CI −28.78 to −12.92; p < 0.00001) | |||
| 5 publications [31,38,87,119,183] | T2DM | 497 | 34–70 | P | 8–24 | 1500 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 1500 mg/day of turmeric | ↔ HDL-C (WMD = 2.26 mg/dL; 95% CI −2.03 to 6.55; p = 0.30) | |||
| Altobelli et al. 2021 [201] | 5 publications [38,49,114,182,183] | T2DM | 476 | 18–80 | P | 8–12 | 80–1500 mg/day of curcumin, 300 mg/day of curcuminoids, 2100 mg/day of turmeric | ↓ TG (ES = −0.57; 95% CI −0.83 to −0.31; p < 0.001) | Cochrane risk of bias tool (93.8%) | Medline, EMBASE, Scopus, ClinicalTrials.gov, Web of Science, and Cochrane Library |
| 5 publications [38,49,114,182,183] | T2DM | 312 | 18–80 | P | 8–12 | 80–1500 mg/day of curcumin, 300 mg/day of curcuminoids, 2100 mg/day of turmeric | ↓ TC (ES = −0.30; 95% CI −0.53 to −0.07; p < 0.001) | |||
| 5 publications [38,49,114,182,183] | T2DM | 333 | 18–80 | P | 8–12 | 80–1500 mg/day of curcumin, 300 mg/day of curcuminoids, 2100 mg/day of turmeric | ↔ HDL-C (ES = 0.22; 95% CI −0.08 to 0.52; p = 0.143) | |||
| 5 publications [31,38,49,114,183] | T2DM | 300 | 18–80 | P | 8–12 | 80–1500 mg/day of curcumin, 300 mg/day of curcuminoids, 2100 mg/day of turmeric | ↓ LDL-C (ES = −0.28; 95% CI −0.52 to −0.04; p = 0.021) | |||
| Abdelazeem et al. 2021 [115] | 4 publications [58,73,193,197] | PCOS | 229 | 24–35 | P | 6–12 | 80–1000 mg/day of curcumin | ↔ TG (MD = −10.18; 95% CI −31.20 to 10.83; p = 0.34) ↔ LDL-C (MD = −8.53; 95% CI −22.97 to 5.91; p = 0.25) ↔ HDL-C (MD = 4; 95% CI −1.74 to 9.75; p = 0.17) ↓ TC (MD = −15.55; 95% CI −30.33 to −0.76; p < 0.04) | Cochrane risk of bias tool (73.3%) | PubMed, EMBASE, Scopus, Web of Science, Cochrane Central, and Google Scholar |
| Chien et al. 2021 [202] | 2 publications [58,193] | PCOS | 101 | 24–35 | P | 6–12 | 1000–1500 mg/day of curcumin | ↓ HDL (MD = 1.92; 95% CI 0.33 to 3.51; p = 0.018) ↓ TC (MD = −12.45; 95% CI −22.05 to −2.85; p = 0.011) ↔ LDL (MD = −6.02; 95% CI −26.66 to 14.62; p = 0.567) ↔ TG (MD = 8.22; 95% CI −26.10 to 42.53; p = 0.639) | Cochrane risk of bias tool (72.2%) | PubMed, Embase, Scopus, Web of Science, and Cochrane Library |
| Ashtary-Larky et al. 2021 [111] | 6 publications [23,50,71,76,171,182] | NAFLD, T2DM, Mets, hemodialysis | 337 | 36–68 | P | 6–12 | 40–120 mg/day of nano-curcumin | ↔ TG (WMD = −9.76 mg/dL; 95% CI −32.71 to 13.17; p = 0.404) | Cochrane risk of bias tool (55.6%) | PubMed, Scopus, Embase, and Web of Science |
| 5 publications [50,71,76,171,182] | NAFLD, T2DM, Mets, hemodialysis | 304 | 36–68 | P | 12 | 40–120 mg/day of nano-curcumin | ↔ TC (WMD = −3.34 mg/dL; 95% CI −14.43 to 7.73; p = 0.554) | |||
| 5 publications [50,71,76,171,182] | NAFLD, T2DM, Mets, hemodialysis | 304 | 36–68 | P | 12 | 40–120 mg/day of nano-curcumin | ↔ LDL-C (WMD = −3.59 mg/dL; 95% CI −15.74 to 8.56; p = 0.562) | |||
| 6 publications [23,50,71,76,171,182] | NAFLD, T2DM, Mets, hemodialysis | 337 | 36–68 | P | 6–12 | 40–120 mg/day of nano-curcumin | ↑ HDL-C (WMD = 5.77 mg/dL; 95% CI 2.90 to 8.64; p < 0.001) | |||
| Jalali et al. 2020 [203] | 6 publications [34,50,161,164,165,177] | NAFLD | 407 | 33–58 | P | 8–12 | 50–1425 mg/day of curcumin | ↔ TG (MD = −0.608; 95% CI −1.253 to 0.038; p = 0.065) ↓ LDL-C (MD = −1.028; 95% CI −1.942 to −0.113; p = 0.028) ↓ TC (MD = −0.645; 95% CI −1.047 to −0.243; p = 0.002) ↔ HDL-C (MD = 0.880; 95% CI −0.285 to 2.044; p = 0.139) | Jadad scale (88.9%) | PubMed, Embase, Scopus, Web of Science, and Cochrane Library |
| Mendia et al. 2019 [213] | 17 publications [45,51,52,65,101,114,118,126,138,161,177,182,183,214,215,216,217] | T2DM, Mets, NAFLD, COPD, dyslipidemia, CAD, acute coronary syndrome, healthy, elderly | 1205 | 30–83 | P, CO | 4–24 | 45–4000 mg/day of curcumin, 294–1000 mg/day of curcuminoids, 1200 mg/day of turmeric | ↔ LDL-C (WMD = −5.82 mg/dL; 95% CI −15.80 to 4.16; p = 0.253) | Cochrane risk of bias tool (55.0%) | PubMed–Medline, Scopus, and Web of Science |
| 19 publications [31,45,51,52,62,65,101,114,126,138,161,177,182,183,214,215,216,217,218] | T2DM, Mets, NAFLD, COPD, dyslipidemia, CAD, acute coronary syndrome, healthy, elderly | 1439 | 23–83 | P, CO | 1–24 | 45–6000 mg/day of curcumin, 294–1000 mg/day of curcuminoids, 1200 mg/day of turmeric | ↓ TG (WMD = −21.36 mg/dL; 95% CI −32.18 to −10.53; p < 0.001) | |||
| 18 publications [45,51,52,62,101,114,118,126,138,161,177,182,183,214,215,216,217,218] | T2DM, Mets, NAFLD, COPD, dyslipidemia, CAD, acute coronary syndrome, healthy, elderly | 1247 | 23–83 | P, CO | 1–24 | 45–6000 mg/day of curcumin, 294–1000 mg/day of curcuminoids, 1200 mg/day of turmeric | ↔ TC (WMD = −9.57 mg/dL; 95% CI −20.89 to 1.75; p = 0.098) | |||
| 16 publications [45,51,52,65,101,114,126,138,161,177,182,183,214,215,216,217] | T2DM, Mets, NAFLD, COPD, dyslipidemia, CAD, acute coronary syndrome, elderly | 1145 | 30–83 | P, CO | 4–24 | 45–4000 mg/day of curcumin, 294–1000 mg/day of curcuminoids, 1200 mg/day of turmeric | ↓ HDL-C levels (WMD = 1.42 mg/dL; 95% CI 0.03 to 2.81; p = 0.046) | |||
| Azhdari et al. 2019 [204] | 5 publications [25,61,126,138,172] | Mets | 259 | 30–72 | P | 6–12 | 20–1890 mg/day of curcumin, 1000 mg/day of curcuminoids, 2400 mg/day of turmeric | ↓ TG (WMD = −33.65 mg/dL; 95% CI −51.27 to −16.03; p < 0.001) ↑ HDL-C (WMD = 4.31 mg/dL; 95% CI 1.50 to 7.11; p = 0.003) | Cochrane risk of bias tool (59.2%) | Web of Science, MEDLINE, Google Scholar, Scopus, Cochrane, and CINAHL |
| Tabrizi et al. 2018 [207] | 19 publications [25,31,45,51,52,57,87,101,114,126,138,161,178,183,206,208,214,219,220] | Mets, hyperlipidemia, T2DM, acute coronary syndrome, overweight/obese, diabetic nephropathy, NAFLD, CAD | 1396 | 18–73 | P | 4–24 | 80–2000 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 112–2100 mg/day of turmeric | ↓ TG (SMD = −1.21; 95% CI −1.78 to −0.65; p < 0.001) | Cochrane risk of bias tool (76.9%) | Cochrane Library, EMBASE, MEDLINE, and Web of Science |
| 20 publications [25,45,51,52,57,87,101,114,126,138,161,178,182,183,206,208,209,214,219,220] | Mets, hyperlipidemia, T2DM, acute coronary syndrome, overweight/obese, diabetic nephropathy, NAFLD, CAD | 1229 | 18–73 | P | 4–24 | 70–2000 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 300–2100 mg/day of turmeric | ↓ TC (SMD = −0.73; 95% CI −1.32 to −0.13; p = 0.01) | |||
| 21 publications [25,45,46,51,52,57,87,101,114,126,138,161,178,182,183,206,208,209,214,219,220] | Mets, hyperlipidemia, T2DM, acute coronary syndrome, overweight/obese, diabetic nephropathy, NAFLD, CAD | 1289 | 18–73 | P | 4–24 | 70–2000 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 112–2100 mg/day of turmeric | ↔ LDL-C (SMD = −0.52; 95% CI −1.14 to 0.11; p = 0.10) | |||
| 20 publications [25,45,51,52,57,87,101,114,126,138,161,178,182,183,206,208,209,214,219,220] | Mets, hyperlipidemia, T2DM, acute coronary syndrome, overweight/obese, diabetic nephropathy, NAFLD, CAD | 1229 | 18–73 | P | 4–24 | 70–2000 mg/day of curcumin, 300–1000 mg/day of curcuminoids, 300–2100 mg/day of turmeric | ↔ HDL-C (SMD = 0.28; 95% CI −0.22 to 0.77; p = 0.27) | |||
| Qin et al. 2017 [221] | 7 publications [25,31,57,114,126,161,182] | T2DM, Mets, NAFLD, dyslipidemia, prediabetes, prehypertension | 649 | 28–72 | P | 4–12 | 80 mg/day of curcumin, 70–1890 mg/day of curcuminoids, 2000–2400 mg/day of turmeric | ↓ TG (SMD = −0.214; 95% CI −0.369 to −0.059; p = 0.007) | Cochrane risk of bias tool (57.1%) | PubMed, Embase, Ovid, Medlin, and Cochrane Library |
| 6 publications [25,31,57,126,161,182] | T2DM, Mets, NAFLD, dyslipidemia, prediabetes, prehypertension | 512 | 28–72 | P | 4–12 | 80 mg/day of curcumin, 70–1890 mg/day of curcuminoids, 2000–2400 mg/day of turmeric | ↓ LDL-C (SMD = −0.340; 95% CI −0.530 to −0.150; p < 0.0001) ↔ TC (SMD = −0.38; 95% CI −0.78 to 0.01; p = 0.054) ↔ HDL-C (SMD = 0.09; 95% CI −0.10 to 0.27; p = 0.370) | |||
| Sahebkar et al. 2014 [222] | 5 publications [52,114,214,215,218] | T2DM, healthy obese, dyslipidemia, acute coronary syndrome, Alzheimer’s disease | 197 | 23–83 | P, CO | 1–24 | 45–6000 mg/day of curcuminoids | ↔ TG (MD = −1.29 mg/dL; 95% CI −9.05 to 6.48; p = 0.75) ↔ TC (MD = 8.97 mg/dL; 95% CI −4.56 to 22.51; p = 0.19) | Cochrane risk of bias tool (33.3%) | PubMed–Medline, SCOPUS, Ovid-AMED, ClinicalTrials.gov, and Cochrane Library |
| 4 publications [52,114,214,215] | T2DM, obese, dyslipidemia, acute coronary syndrome, Alzheimer’s disease | 173 | 27–83 | P, CO | 8–24 | 45–4000 mg/day of curcuminoids | ↔ LDL-C (MD = 16.15 mg/dL; 95% CI −4.43 to 36.74; p = 0.12) ↔ HDL-C (MD = −0.59 mg/dL; 95% CI −1.66 to 0.49; p = 0.28) |
| Ref. | No. of Studies Included | Health Status of Subjects | No. of Subjects | Age of Subjects (Years) | Design | Period (Weeks) | Dose | Outcomes (Effect Size) | Quality of Primary Studies | Databases |
|---|---|---|---|---|---|---|---|---|---|---|
| Lukkunaprasit et al. 2023 [160] | 13 publications [34,35,50,161,164,165,166,167,168,175,176,178,181] | MAFLD | 756 | 25–38 | P | 8–12 | 80–1500 mg/day of curcumin, 3000 mg/day of turmeric | ↓ BMI (MD = −0.34; 95% CI −0.62 to −0.05; p < 0.05) | Cochrane risk of bias tool (68.8%) | Medline and SCOPUS |
| Qiu et al. 2023 [22] | 7 publications [23,25,61,170,171,172,223] | Mets | 369 | 28–64 | P | 4–12 | 80–1000 mg/day of curcumin, 2400 mg/day of turmeric | ↓ WC (MD = −2.16; 95% CI −3.78 to −0.54; p = 0.009) | Cochrane risk of bias tool (71.4%) | PubMed, SCOPUS, Cochrane Library, EMBASE, Web of Science, and China Biological Medicine |
| Rozanski et al. 2023 [173] | 14 publications [34,35,50,55,161,164,165,166,174,175,176,177,178,179] | MAFLD | 847 | 18–70 | P | 8–12 | 70–1500 mg/day of curcuminoids, 80–1000 mg/day of curcumin, 3000 mg/day of turmeric | ↓ WC (MD = −2.6303; 95% CI −4.9350 to −0.3256; p = 0.0253) | Cochrane risk of bias tool (90.8%) | PubMed, Web of Science, and Scopus |
| Ngu et al. 2022 [180] | 11 publications [34,35,50,161,164,166,175,178,181,196,224] | NAFLD | 701 | 18–70 | P | 8–12 | 50–1500 mg/day of curcumin, 2000 mg/day of turmeric | ↓ BMI (MD = −0.41; 95% CI −0.75 to − 0.07; p = 0.02) | Cochrane risk of bias tool (79.5%) | Cochrane Central Register of Controlled Trials and PubMed |
| Sun et al. 2022 [100] | 15 publications [23,25,38,49,60,61,70,101,126,170,182,183,185,209,223] | Mets, obese, hyperlipidemia, hypercholesterolemia, T2DM, IGT, IFG, DSPN | 990 | 38–62 | P, CO | 4–12 | 80–2400 mg/day of curcumin | ↓ BW (WMD = −0.94 kg; 95% CI −1.40 to −0.47; p < 0.001) | Cochrane risk of bias tool (69.3%) Jadad scale (77.0%) | PubMed, Embase, Web of Science, CNKI, Wanfang, and CBM |
| 12 publications [23,25,38,49,61,70,170,183,185,188,209,223] | Mets, obese, hypercholesterolemia, T2DM, IGT, IFG, DSPN | 882 | 38–63 | P, CO | 4–17 | 80–2400 mg/day of curcumin | ↔ WC (WMD = −1.41 cm; 95% CI −2.82 to 0.004; p = 0.051) | |||
| 16 publications [23,25,29,49,60,61,76,101,126,170,182,183,185,188,209,223] | Mets, obese, hyperlipidemia, hypercholesterolemia, T2DM, IGT, IFG, DSPN, hemodialysis | 1135 | 38–70 | P, CO | 4–24 | 80–2400 mg/day of curcumin | ↓ BMI (WMD = −0.40 kg/m2; 95% CI −0.60 to −0.19; p < 0.001) | |||
| Khalili et al. 2022 [195] | 9 publications [34,50,161,165,166,176,179,181,196] | NAFLD | 619 | 42–67 | P | 4–12 | 80–2000 mg/day of curcumin | ↔ BMI (SMD = −0.13; 95% CI −0.29 to 0.02; p = 0.096) | Cochrane risk of bias tool (65.5%) | Web of Science, Science Direct, PubMed, and Embase |
| Nouri et al. 2022 [192] | 4 publications [58,73,193,194] | PCOS | 198 | 28–31 | P | 6–12 | 93.34–1500 mg/day of curcumin | ↔ BMI (ES = −0.23 kg/m2; 95% CI −1.46 to 0.99; p = 0.70) | Cochrane risk of bias tool (75.0%) | PubMed, Scopus, and ISI Web of Science |
| Shen et al. 2022 [99] | 7 publications [58,73,193,194,197,198,199] | PCOS | 447 | 20–38 | P | 6–24 | 80–1500 mg/day of curcumin | ↓ BMI (WMD = −0.267; 95% CI −0.450 to −0.084; p = 0.004) | Cochrane risk of bias tool (73.5%) | PubMed, Embase, Cochrane Library, Web of Science, Scopus, Clinical Trials, Chinese Clinical Trial Registry, Chinese Biomedical Literature Database, Chinese National Knowledge Infrastructure, VIP database, and Wanfang Database |
| 4 publications [58,73,193,197] | PCOS | 229 | 24–35 | P | 6–12 | 93.34–1000 mg/day of curcumin | ↔ BW (WMD = −0.924; 95% CI −2.009 to 0.162; p = 0.095) | |||
| 2 publications [73,194] | PCOS | 97 | 24–35 | P | 8–12 | 93.34–1500 mg/day of curcumin | ↔ WC (WMD = −1.475; 95% CI −4.519 to 1.570; p = 0.342) | |||
| Abdelazeem et al. 2021 [115] | 4 publications [58,73,193,197] | PCOS | 229 | 24–35 | P | 6–12 | 80–1000 mg/day of curcumin | ↔ BW (MD = −0.15; 95% CI −0.56 to 0.27; p = 0.49) | Cochrane risk of bias tool (73.3%) | PubMed, EMBASE, Scopus, Web of Science, Cochrane Central, and Google Scholar |
| 2 publications [73,194] | PCOS | 97 | 24–35 | P | 8–12 | 93.34–1500 mg/day of curcumin | ↔ WC (MD = −1.47; 95% CI −4.52 to 1.57; p = 0.34) | |||
| 5 publications [58,73,193,194,197] | PCOS | 296 | 24–39 | P | 6–12 | 80–1500 mg/day of curcumin | ↔ BMI (MD = −0.15; 95% CI −0.56 to 0.27; p = 0.49) | |||
| Altobelli et al. 2021 [201] | 3 publications [49,144,182] | T2DM | 168 | 30–70 | P | 8–12 | 80–1500 mg/day of curcumin, 2100 mg/day of turmeric | ↔ BMI (ES = −0.30 kg/m2; 95% CI −0.62 to 0.02; p = 0.067) | Cochrane risk of bias tool (93.8%) | Medline, EMBASE, ClinicalTrials.gov, Web of Science, Cochrane Library, and Scopus |
| Ashtary-Larky et al. 2021 [111] | 4 publications [23,50,171,185] | Mets, T2DM, NAFLD | 240 | 36–64 | P | 6–12 | 40–80 mg/day of nano-curcumin | ↔ BW (WMD = −0.51 mg/dL; 95% CI −1.85 to 0.82; p = 0.449) | Cochrane risk of bias tool (55.6%) | PubMed, Scopus, Embase, and Web of Science |
| 6 publications [23,50,71,171,182,185] | Mets, T2DM, NAFLD | 364 | 36–67 | P | 6–12 | 40–80 mg/day of nano-curcumin | ↔ BMI (WMD = −0.35 mg/dL; 95% CI −0.76 to 0.04; p = 0.079) | |||
| 4 publications [23,50,171,185] | Mets, T2DM, NAFLD | 240 | 36–64 | P | 6–12 | 40–80 mg/day of nano-curcumin | ↔ WC (WMD = −1.32 mg/dL; 95% CI −3.89 to 1.23; p = 0.310) | |||
| 2 publications [23,171] | Mets, NAFLD | 160 | 36–64 | P | 6–12 | 40–80 mg/day of nano-curcumin | ↔ FM (WMD = −0.86 mg/dL; 95% CI −1.95 to 0.23; p = 0.123) | |||
| Mousavi et al. 2020 [225] | 8 publications [39,52,124,126,161,223,226,227] | Mets, prediabetic, obese, NAFLD, T2DM | 667 | 38–59 | P | 4–39 | 80–200 mg/day of curcumin, 1000–1500 mg/day of curcuminoids | ↓ BW (WMD = −1.14 kg; 95% CI −2.16 to −0.12; p = 0.02) | Jadad scale (81.8%) | PubMed, Medline, SCOPUS, Cochrane Library. and Google Scholar |
| 10 publications [52,89,124,126,161,178,182,223,226,227] | Mets, obese, NAFLD, T2DM | 645 | 26–59 | P | 4–13 | 80–1000 mg/day of curcumin, 1000–1900 mg/day of curcuminoids | ↓ BMI (WMD = −0.48 kg/m2; 95% CI −0.78 to −0.17; p = 0.002) | |||
| 6 publications [39,52,89,178,223,226] | Mets, prediabetic, obese, NAFLD | 456 | 26–57 | P | 4–39 | 200–1000 mg/day of curcumin, 1000–1500 mg/day of curcuminoids | ↔ WC (WMD = −1.51 cm; 95% CI −4.041 to 1.003; p = 0.23) | |||
| Jalali et al. 2020 [203] | 5 publications [34,50,161,164,165] | NAFLD | 270 | 28–59 | P | 8–12 | 50–80 mg/day of curcumin | ↔ BW (MD = −0.051; 95% CI −0.271 to 0.170; p = 0.653) | Jadad scale (88.9%) | PubMed, Embase, Scopus, Web of Science. and Cochrane Library |
| 7 publications [34,50,124,161,164,165,181] | NAFLD | 453 | 28–59 | P | 8–12 | 50–1500 mg/day of curcumin | ↔ BMI (MD = −0.179; 95% CI −0.365 to 0.006; p = 0.058) | |||
| 3 publications [50,124,165] | NAFLD | 269 | 35–58 | P | 8–12 | 80–1425 mg/day of curcumin | ↓ WC (MD = −1.005; 95% CI −1.304 to −0.706; p < 0.0001) | |||
| Baziar et al. 2020 [228] | 6 publications [34,35,50,161,164,165] | NAFLD | 385 | 42–46 | P | 8–12 | 70–1500 mg/day of curcumin, 3000 mg/day of turmeric | ↔ BW (WMD = −0.60 kg; 95% CI −2.07 to 0.87; p = 0.423) | Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) (87.5%) | PubMed/Medline, ISI Web of Science, Scopus, EMBASE, Cochrane Library, Google Scholar, Sid.ir, and Magiran.com |
| 8 publications [34,35,50,161,164,165,178,179] | NAFLD | 567 | 42–54 | P | 8–12 | 70–1500 mg/day of curcumin, 3000 mg/day of turmeric | ↓ BMI (WMD = −0.34 kg/m2; 95% CI −0.64 to −0.0; p < 0.05) | |||
| 4 publications [50,165,178,179] | NAFLD | 318 | 42–54 | P | 8–12 | 70–1500 mg/day of curcumin, 3000 mg/day of turmeric | ↓ WC (WMD = −2.12 cm; 95% CI −3.26 to −0.98; p < 0.001) | |||
| Akbari et al. 2019 [131] | 12 publications [25,45,52,124,126,161,178,182,208,223,226,229] | Mets, obese, T2DM, hyperlipidemia, NAFLD | 854 | 23–72 | P | 4–12 | 80–2400 mg/day of curcumin, 294 mg/day of curcuminoids, 2100 mg/day of turmeric | ↓ BMI (SMD = −0.37; 95% CI −0.61 to 0.13; p < 0.01) | Cochrane risk of bias tool (77.8%) | Cochrane Library, EMBASE, PubMed, and Web of Science |
| 13 publications [25,32,39,45,46,52,126,161,178,208,223,226,229] | Mets, obese, T2DM, hyperlipidemia, NAFLD | 1233 | 10–72 | P | 4–36 | 80–2400 mg/day of curcumin, 294–1500 mg/day of curcuminoids, 2100–2800 mg/day of turmeric | ↓ BW (SMD = −0.23; 95% CI −0.39 to 0.06; p < 0.01) | |||
| 8 publications [25,31,32,39,52,124,223,226] | Mets, obese, T2DM | 848 | 10–72 | P | 4–36 | 200–2400 mg/day of curcumin, 1500 mg/day of curcuminoids | ↓ WC (SMD = −0.25; 95% CI −0.44 to −0.05; p = 0.01) | |||
| 5 publications [25,32,52,223,226] | Mets, obese | 301 | 10–58 | P | 4–8 | 200–2400 mg/day of curcumin | ↔ hip ratio (SMD = −0.17; 95% CI −0.42 to 0.08; p = 0.18) | |||
| Wei et al. 2019 [230] | 2 publications [161,231] | NAFLD | 299 | 41–57 | P | 8–24 | 500–3000 mg/day of curcumin | ↓ BW (MD = −2.27; 95% CI −3.11 to −1.44; p < 0.0001) | Cochrane risk of bias tool (75.0%) | PubMed, EMBASE, and Cochrane Library |
| Azhdari et al. 2019 [204] | 4 publications [25,61,172,223] | Mets | 244 | 38–48 | P | 4–8 | 800–2400 mg/day of curcumin | ↔ WC (WMD = −0.41 cm; 95% CI −1.95 to 1.13; p = 0.6) | Cochrane risk of bias tool (59.2%) | Web of Science, MEDLINE, Google Scholar, Scopus, Cochrane, and CINAHL |
| Jafarirad et al. 2019 [232] | 7 publications [35,146,161,165,177,227,233] | NAFLD | 429 | 40–65 | P | 8–12 | 80–1500 mg/day of curcumin, 2000–3000 mg/day of turmeric | ↔ BMI (WMD = −0.21 kg/m2; 95% CI −0.71 to 0.28; p = 0.39) | Cochrane risk of bias tool (72.9%) | PubMed, Scopus, Cochrane Library, and ISI Web of Science |
| 7 publications [35,146,161,163,165,227,233] | NAFLD | 362 | 40–65 | P | 8–24 | 80–1500 mg/day of curcumin, 3000 mg/day of turmeric | ↔ BW (WMD = −0.54 kg; 95% CI −2.40 to 1.31; p = 0.56) | |||
| 4 publications [146,163,165,177] | NAFLD | 221 | 40–54 | P | 8–24 | 1000–1500 mg/day of curcumin, 2000 mg/day of turmeric | ↔ WC (WMD = −0.88 cm; 95% CI −3.76 to 2.00; p = 0.54) |
| Ref. | No. of Studies Included | Health Status of Subjects | No. of Subjects | Age of Subjects (Years) | Design | Period (Weeks) | Dose | Outcomes (Effect Size) | Quality of Primary Studies | Databases |
|---|---|---|---|---|---|---|---|---|---|---|
| Lukkunaprasit et al. 2023 [160] | 5 publications [50,166,167,168,178] | MAFLD | 358 | 25–36 | P | 8–12 | 80–1000 mg/day of curcumin | ↔ SBP (MD = −0.29; 95% CI −0.91 to 0.34; p = 0.37) ↔ DBP (MD = −0.02; 95% CI −0.55 to 0.52; p = 0.95) | Cochrane risk of bias tool (68.8%) | Medline and SCOPUS |
| Qiu et al. 2023 [22] | 6 publications [23,25,27,61,170,171] | Mets | 405 | 28–61 | P | 6–12 | 80–1000 mg/day of curcumin, 1000 mg/day of curcuminoids, 2400 mg/day of turmeric | ↔ SBP (MD = −4.82; 95% CI −9.98 to 0.35; p = 0.07) | Cochrane risk of bias tool (71.4%) | PubMed, SCOPUS, Cochrane Library, EMBASE, Web of Science, and China Biological Medicine |
| 5 publications [25,27,61,170,171] | Mets | 383 | 28–61 | P | 6–12 | 80–1000 mg/day of curcumin, 1000 mg/day of curcuminoids, 2400 mg/day of turmeric | ↓ DBP (MD = −2.8; 95% CI −4.53 to −1.06; p = 0.002) | |||
| Ashtary-Larky et al. 2021 [111] | 4 publications [23,50,76,171] | Mets, NAFLD, T2DM, hemodialysis | 213 | 37–68 | P | 6–12 | 40–80 mg/day of nano-curcumin | ↓ SBP (WMD = −7.09 mg/dL; 95% CI −12.98 to −1.20; p < 0.001) | Cochrane risk of bias tool (55.6%) | PubMed, Scopus, Embase, and Web of Science |
| 3 publications [50,76,171] | Mets, NAFLD, T2DM, hemodialysis | 180 | 37–68 | P | 12 | 40–80 mg/day of nano-curcumin, | ↔ DBP (WMD = −0.07 mg/dL; 95% CI −1.12 to 0.97; p = 0.891) | |||
| Changal et al. 2020 [234] | 5 publications [66,235,236,237,238] | Healthy, postmenopausal | 733 | 19–70 | P | One time, 8–12 | 25–5000 mg/day of curcumin | ↑ FMD (SDM = 1.379; 95% CI 0.48 to 2.274; p = 0.003) | Not assessed | PubMed, ClinicalTrials.gov, Scopus, and Embase |
| Hallajzadeh et al. 2019 [239] | 2 publications [66,235] | Healthy | 60 | 59–71 | P | 8–12 | 150–2000 mg/day of curcumin | ↑ FMD (WMD = 1.49; 95% CI 0.16 to 2.82; p < 0.05) | Cochrane risk of bias tool (not indicated) | Cochrane Library, EMBASE, PubMed, and Web of Science |
| 4 publications [31,66,89,240] | Healthy, postmenopausal, obese, T2DM | 319 | 22–70 | P | 8–24 | 150–2000 mg/day of curcumin | ↔ PWV (WMD = −41.59; 95% CI −86.59 to 3.42; p > 0.05) | |||
| 2 publications [66,240] | Healthy, postmenopausal | 84 | 53–68 | P | 8–12 | 150–2000 mg/day of curcumin | ↔ Aix (WMD = 0.71; 95% CI −1.37 to 2.79; p > 0.05) | |||
| 3 publications [33,66,114] | Healthy, depressive, T2DM | 133 | 31–67 | P | 8–12 | 150–2000 mg/day of curcumin | ↔ ET-1 (WMD = −0.30; 95% CI −0.96 to 0.37; p > 0.05) | |||
| 3 publications [62,120,241] | Healthy, perennial allergic rhinitis, dyslipidemia | 353 | 26–62 | P | 4–12 | 80–500 mg/day of curcumin | ↔ sICAM-1 (WMD = −10.11; 95% CI −33.67 to 13.46; p > 0.05) | |||
| Hadi et al. 2019 [242] | 11 publications [25,50,61,65,66,89,151,178,219,243,244] | Mets, obese, lupus nephritis, T2DM postmenopausal, CKD, NAFLD, COPD, diabetic proteinuria, healthy, elderly | 734 | 21–74 | P, CO | 8–24 | 80–1000 mg/day of curcumin, 320–2400 mg/day of turmeric | ↔ SBP (ES = −0.69 mmHg; 95% CI −2.01 to 0.64) ↔ DBP (ES = 0.28 mmHg; 95% CI −1.12 to 1.68) | Cochrane risk of bias tool (69.7%) | Medline, EMBASE, SCOPUS, ISI Web of Science, Google Scholar, and Cochrane Library |
| Azhdari et al. 2019 [204] | 3 publications [25,27,61] | Mets | 280 | 38–45 | P | 8 | 1000 mg/day of curcumin, 1000 mg/day of curcuminoids, 2400 mg/day of turmeric | ↔ SBP (WMD = −1.68 mmHg; 95% CI −4.68 to 1.3) ↓ DBP (WMD = −2.96 mmHg; 95% CI −5.09 to −0.83; p = 0.007) | Cochrane risk of bias tool (59.2%) | Web of Science, MEDLINE, Google Scholar, Scopus, Cochrane, and CINAHL |
| Ref. | No. of Studies Included | Health Status of Subjects | No. of Subjects | Age of Subjects (Years) | Design | Period (Weeks) | Dose | Outcomes (Effect Size) | Quality of Primary Studies | Databases |
|---|---|---|---|---|---|---|---|---|---|---|
| Wang et al. 2021 [245] | 6 publications [139,246,247,248,249,250] | MDD (DSM-IV or Mini 6.0) | 520 | 40–76 | P | 5–12 | 500–1500 mg/day of curcumin | ↓ Depression (SMD = −0.35; 95% CI −0.56 to −0.15; I2 = 7%) | Cochrane risk of bias tool (71.7%) | EMBASE, PubMed, PsycINFO, Web of Science, Cochrane Library, and ClinicalTrials.gov |
| 4 publications [251,252,253,254] | T2DM, obesity, schizophrenia (DSM-IV), systemic lupus erythematosus | 77 | 25–68 | P, CO | 4–24 | 80–3000 mg/day of curcumin | ↔ Depressive symptoms (SMD = −0.32; 95% CI −0.50 to −0.13; I2 = 15%) | |||
| 3 publications [139,248,250] | MDD (DSM-IV) | 440 | 23–53 | P | 6–12 | 500–1000 mg/day of curcumin | ↑ Response rates (OR = 3.20; 95% CI 1.28 to 7.99; I2 = 35%) | |||
| Fusar-Poli et al. 2020 [255] | 9 publications [139,246,247,248,249,250,252,254,256] | MDD (DSM-IV), obesity, systemic lupus erythematosus | 599 | 17–81 | P, CO | 4–12 | 150–1500 mg/day of curcumin | ↓ Depression (Hedge’s g = −0.75; 95% CI −1.11 to −0.39; p < 0.001; I2 = 26.28%) | Cochrane risk of bias tool (71.4%) | Web of Science, MEDLINE, KCI, Russian Science Citation Index, SciELO Citation Index, CINAHL, Embase, PsycINFO, and ClinicalTrials.gov |
| 4 publications [248,249,252,256] | MDD (DSM-IV), obesity | 320 | 17–80 | P | 4–12 | 500–1000 mg/day of curcumin | ↓ Anxiety symptoms (Hedge’s g = −2.62; 95% CI −4.06 to −1.17; p < 0.001) | |||
| unNg et al. 2017 [257] | 6 publications [139,246,249,250,252,256] | CGI-S ≥ 4, HAM-D17 ≥ 21, MADRS ≥ 22, BDI-II, DSM-IV, IDS-SR30 ≥ 14, HAM-D17 ≥ 7, HAM-D17 ≥ 10, MADRS ≥ 14 | 377 | 30–76 | P, CO | 4–8 | 500–1000 mg/day of curcumin | ↓ Depressive symptoms (SMD = −0.344; 95% CI −0.558 to −0.129; p = 0.002) | Jadad scale (100%) | PubMed, Ovid, Clinical Trials Register of the Cochrane Collaboration Depression, Anxiety, and Neurosis Group (CCDANTR), and Cochrane Field for Complementary Medicine |
| Al-Karawi et al. 2017 [258] | 6 publications [139,246,249,250,252,256] | CGI-S ≥ 4, HAM-D17 ≥ 21, MADRS ≥ 22, BDI, DSM-IV, IDS-SR30 ≥ 14, HAM-D17 ≥ 7 HAM-D17 ≥ 10, MADRS ≥ 14 | 377 | 30–76 | P, CO | 4–8 | 500–1000 mg/day of curcumin | ↓ Major depression (SMD = −0.34; 95% CI −0.56 to −0.13; p = 0.002) | Quality Assessment Tool for Quantitative Studies (83.3%) | Pubmed, Scopus, Psychinfo, Evidence-Based Medicine Guidelines, DynaMed, JAMA evidence, and Cochrane Library |
| Tsai et al. 2021 [259] | 6 publications [260,261,262,263,264,265] | Alzheimer’s disease, obese, schizophrenia, healthy older adults | 264 | 28–82 | P | 6–24 | 160–4000 mg/day of curcumin | ↔ Cognitive function (Hedges’ g = 0.340; 95% CI −0.353 to 1.033; p = 0.337; I2 = 0.0%) | Cochrane risk of bias tool (89.6%) | PubMed, Embase, ClinicalKey, Cochrane CENTRAL, ProQuest, ScienceDirect, and Web of Science |
| 3 publications [261,266,267] | Schizophrenia, obese, healthy older adults | 160 | 28–76 | P | 8–16 | 80–180 mg/day of curcumin | ↑ Working memory (Hedges’ g = 0.396; 95% CI 0.078 to 0.714; p = 0.015; I2 = 0.0%) | |||
| Zhu et al. 2019 [268] | 3 publications [118,263,269] | healthy, elderly, nondemented | 196 | 54–73 | P | 4–72 | 80–1320 mg/day of curcumin | ↑ Cognitive function in the elderly (SMD = 0.33; 95% CI 0.05 to 0.62; p = 0.02) | Cochrane risk of bias tool (80.0%) | PubMed, Embase, Web of Science, ClinicalTrials.gov, Cochrane Library, Chinese National Knowledge Infrastructure, Wanfang Data, and China Biology Medicine disc |
| Sarraf et al. 2019 [270] | 4 publications [172,262,271,272] | Mets, premenstrual syndrome, schizophrenia, | 139 | 18–65 | P | 8–12 | 200–1820 mg/day of curcumin | ↑ BDNF (WMD = 1789.38 pg/mL; 95% CI 722.04 to 2856.71; p < 0.01; I2 = 83.5%; p < 0.001) | Cochrane risk of bias tool (not indicated) | PubMed, Scopus, Web of Science, Cochrane Library, and Google Scholar |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-M.; Kim, Y. Is Curcumin Intake Really Effective for Chronic Inflammatory Metabolic Disease? A Review of Meta-Analyses of Randomized Controlled Trials. Nutrients 2024, 16, 1728. https://doi.org/10.3390/nu16111728
Lee Y-M, Kim Y. Is Curcumin Intake Really Effective for Chronic Inflammatory Metabolic Disease? A Review of Meta-Analyses of Randomized Controlled Trials. Nutrients. 2024; 16(11):1728. https://doi.org/10.3390/nu16111728
Chicago/Turabian StyleLee, Young-Min, and Yoona Kim. 2024. "Is Curcumin Intake Really Effective for Chronic Inflammatory Metabolic Disease? A Review of Meta-Analyses of Randomized Controlled Trials" Nutrients 16, no. 11: 1728. https://doi.org/10.3390/nu16111728
APA StyleLee, Y.-M., & Kim, Y. (2024). Is Curcumin Intake Really Effective for Chronic Inflammatory Metabolic Disease? A Review of Meta-Analyses of Randomized Controlled Trials. Nutrients, 16(11), 1728. https://doi.org/10.3390/nu16111728





