Burden and Trends of Diet-Related Colorectal Cancer in OECD Countries: Systematic Analysis Based on Global Burden of Disease Study 1990–2021 with Projections to 2050
Abstract
1. Background
2. Methods
2.1. Data Source
2.2. GBD Overview
2.3. Data Source and Processing
2.4. Estimating Risk Factors and Attributable Disease Burden
2.5. Statistical Analysis
3. Results
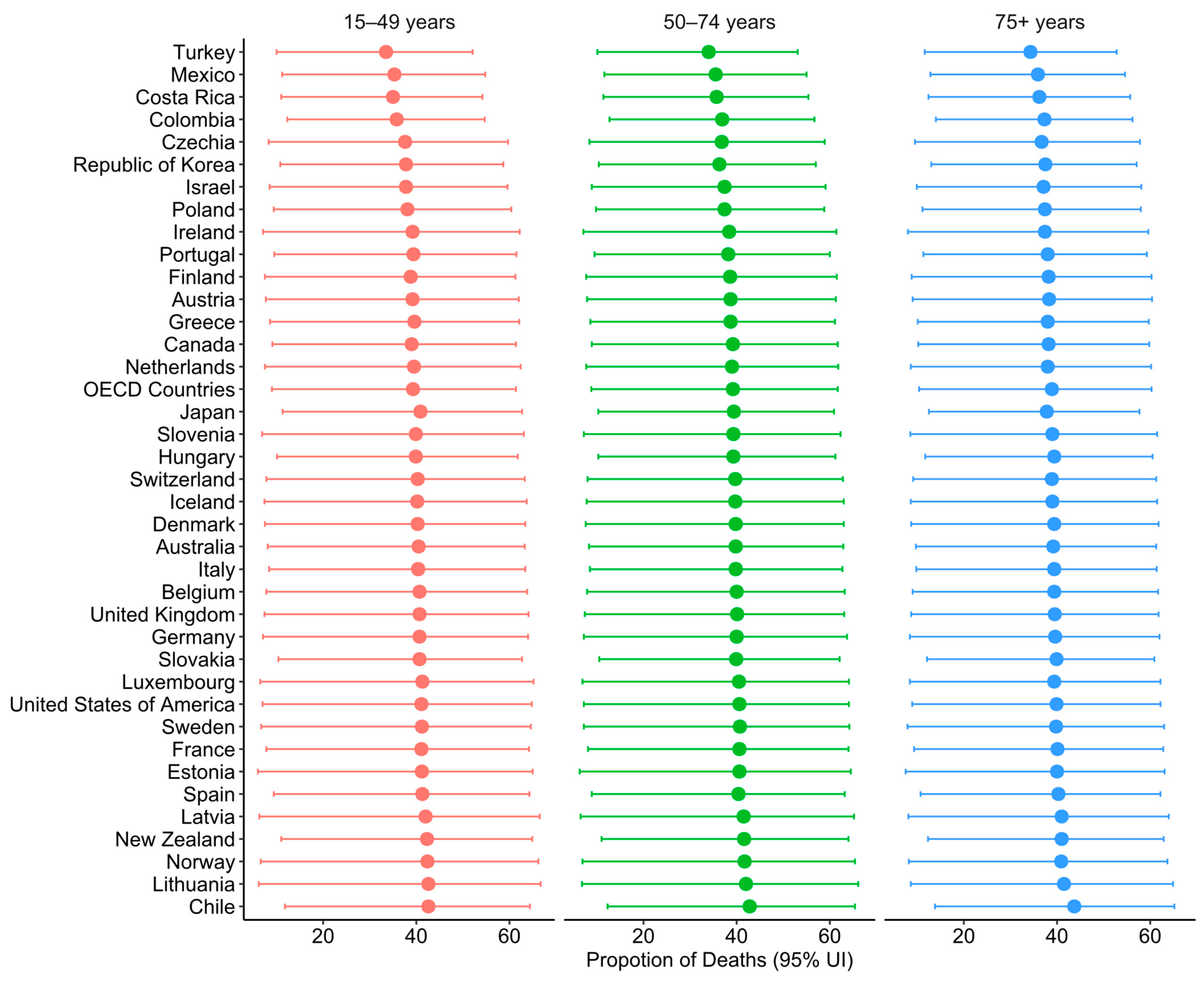
3.1. Diet-Related CRC DALYs and Deaths in 2021
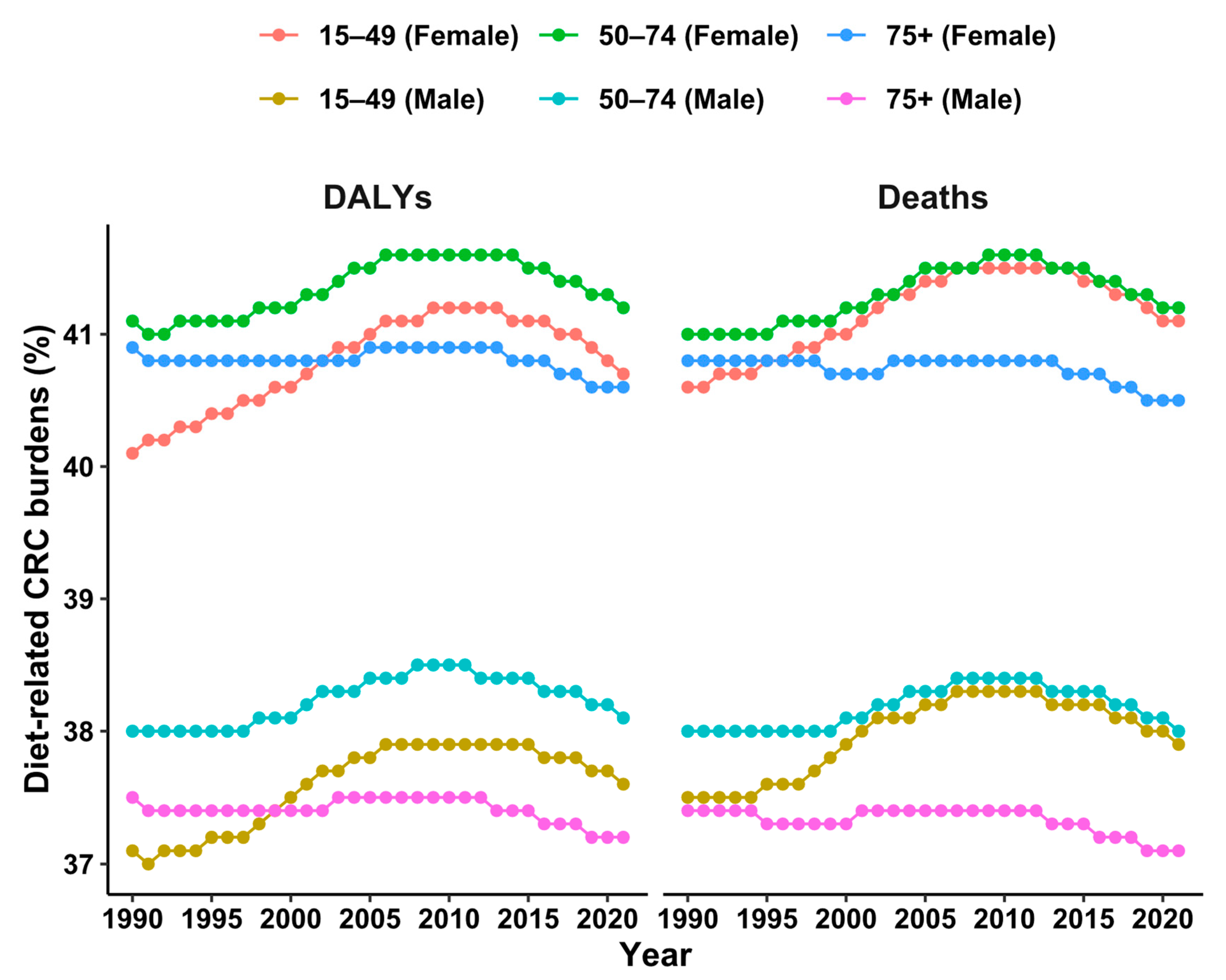
3.2. Trends of Diet-Related CRC DALYs and Deaths Between 1990 and 2021
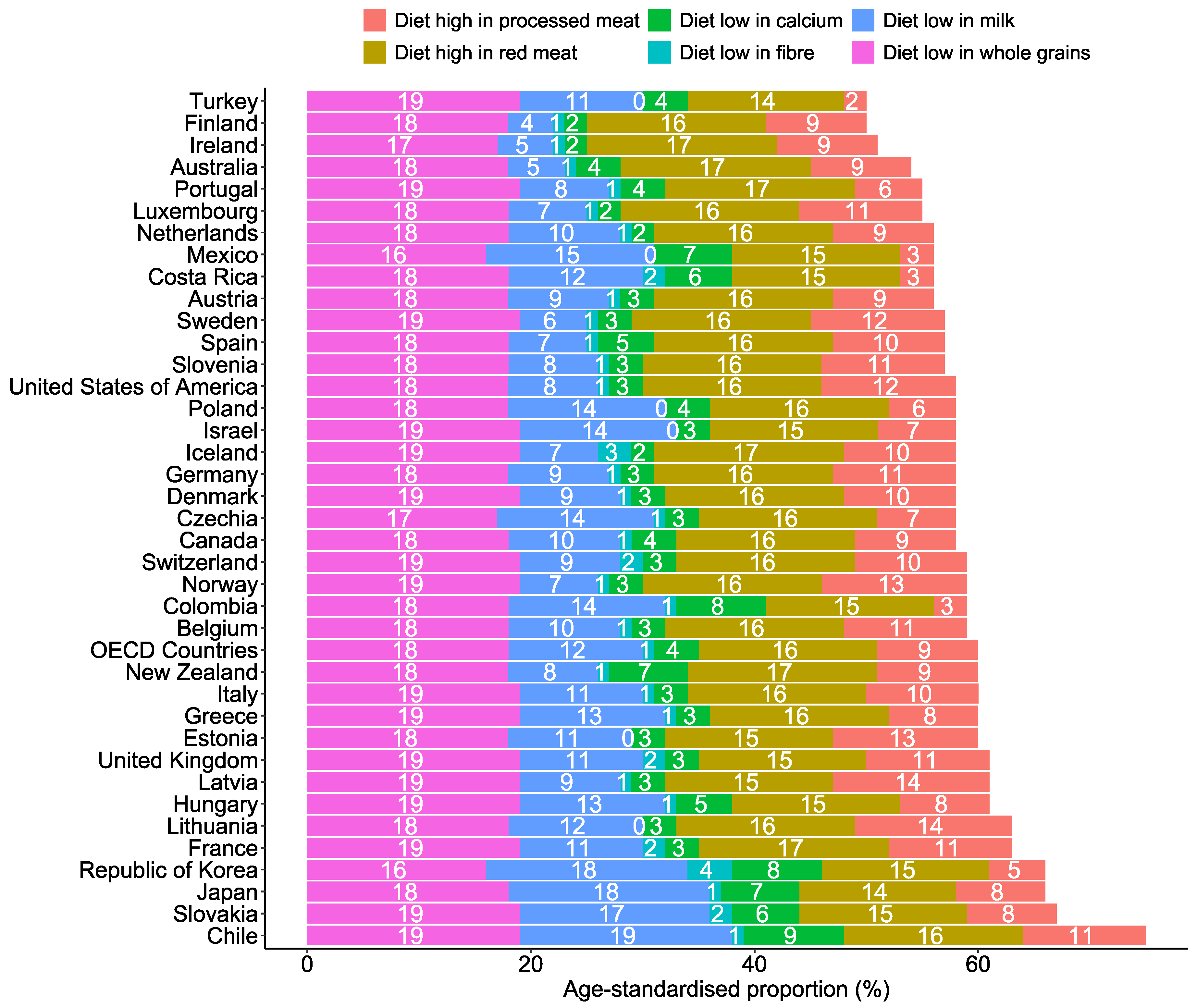
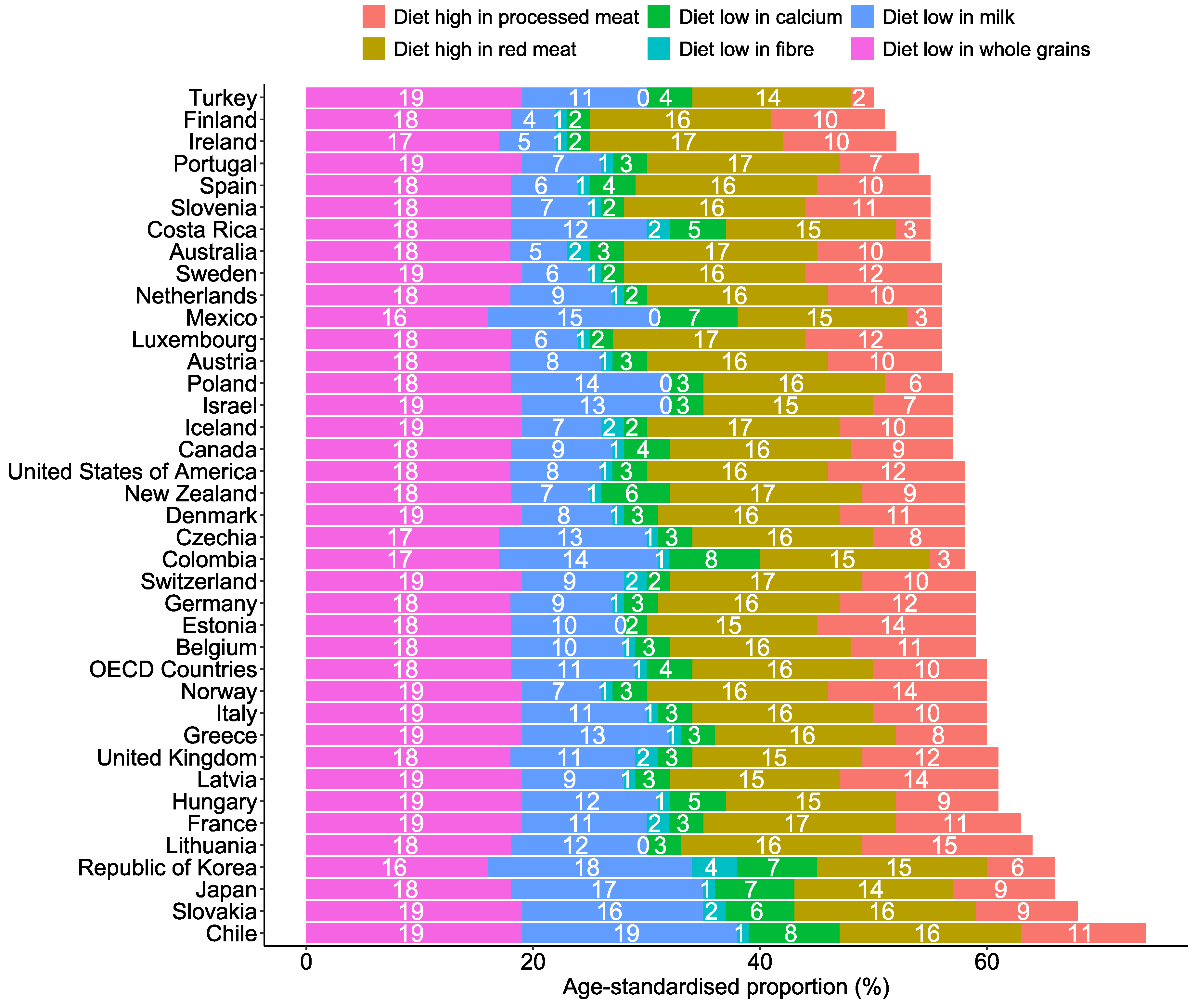
3.3. CRC Death and DALY Burden Attributed to Each Dietary Risk Factor
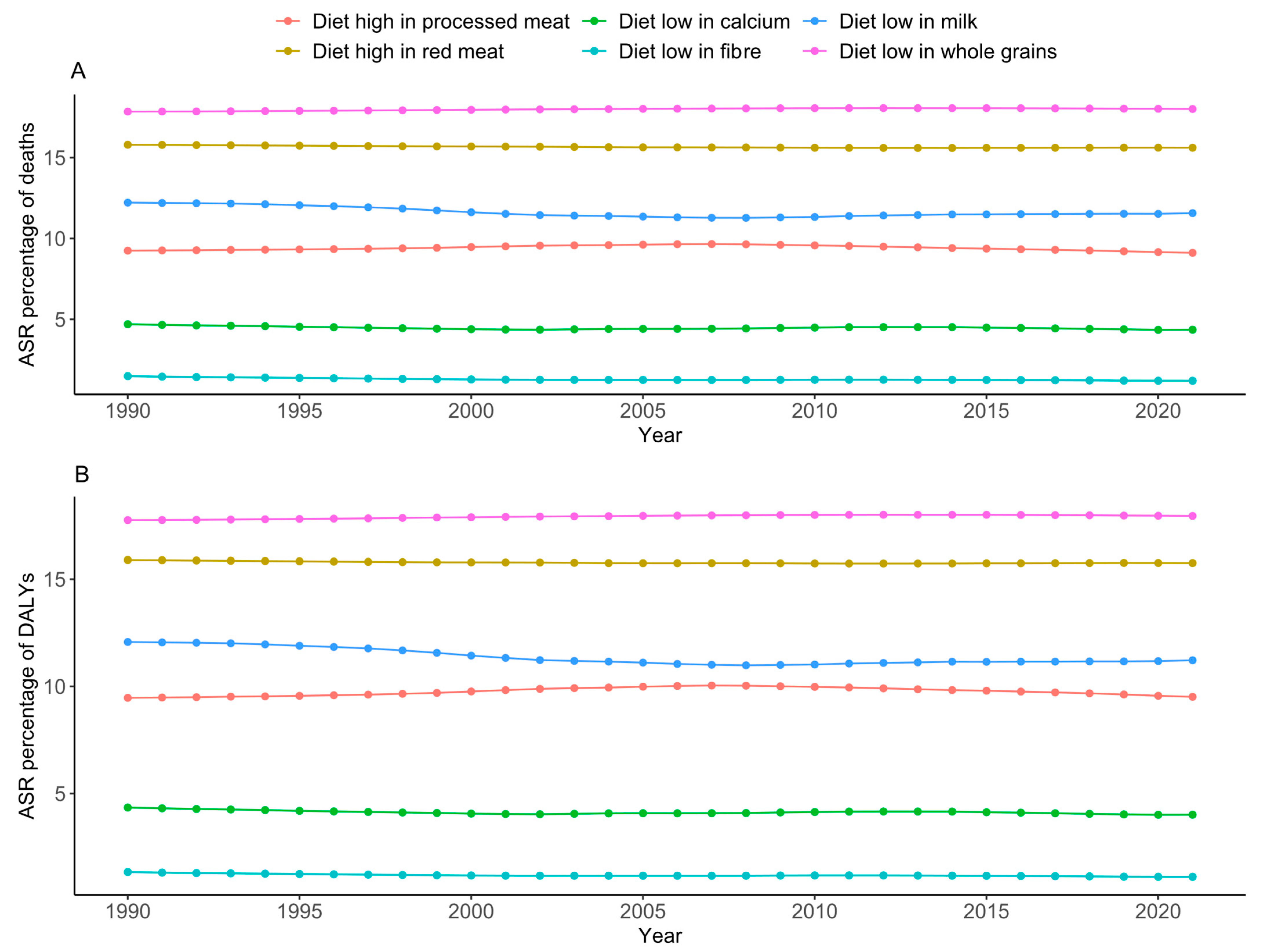
3.4. Relationship Between Socio–Demographic Index and Estimated Annual Percentage of Change in Diet–Related CRC Burdens
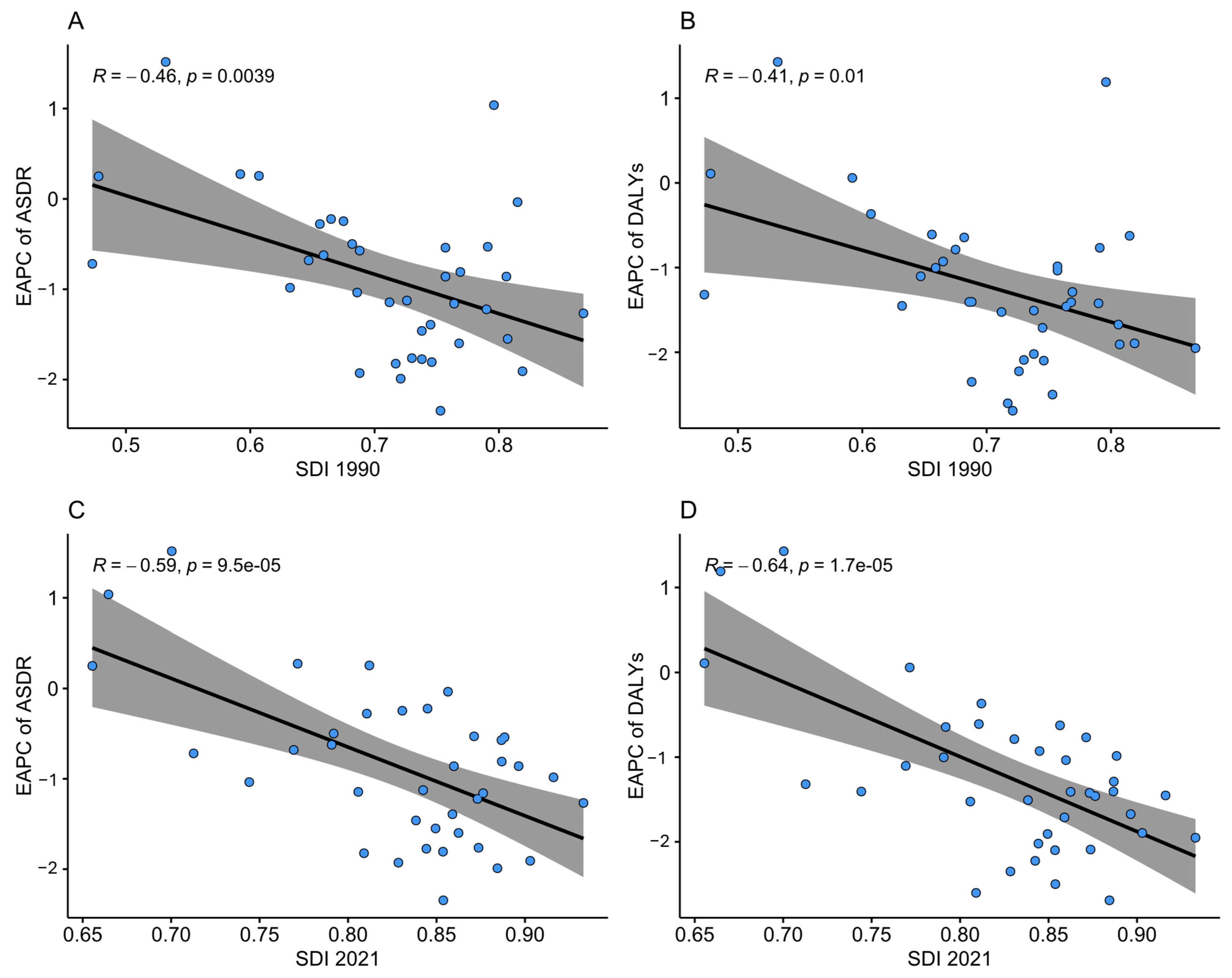
3.5. Diet-Related CRC DALY and Death Burden Projection
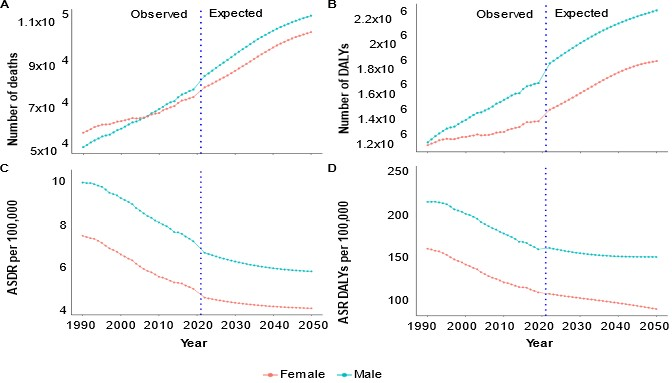
4. Discussion
4.1. Summary of Findings
4.2. Implications of Findings
4.3. The Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Xi, Y.; Xu, P. Global colorectal cancer burden in 2020 and projections to 2040. Transl. Oncol. 2021, 14, 101174. [Google Scholar] [CrossRef] [PubMed]
- Stukalin, I.; Ahmed, N.S.; Fundytus, A.M.; Qian, A.S.; Coward, S.; Kaplan, G.G.; Hilsden, R.J.; Burak, K.W.; Lee, J.K.; Singh, S.; et al. Trends and Projections in National United States Health Care Spending for Gastrointestinal Malignancies (1996–2030). Gastroenterology 2022, 162, 1098–1110.e1092. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Morgan, E.; Arnold, M.; Gini, A.; Lorenzoni, V.; Cabasag, C.; Laversanne, M.; Vignat, J.; Ferlay, J.; Murphy, N.; Bray, F. Global burden of colorectal cancer in 2020 and 2040: Incidence and mortality estimates from GLOBOCAN. Gut 2023, 72, 338–344. [Google Scholar] [CrossRef]
- Sharma, R.; Abbasi-Kangevari, M.; Abd-Rabu, R.; Abidi, H.; Abu-Gharbieh, E.; Acuna, J.M.; Adhikari, S.; Advani, S.M.; Afzal, M.S.; Meybodi, M.A. Global, regional, and national burden of colorectal cancer and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol. Hepatol. 2022, 7, 627–647. [Google Scholar] [CrossRef]
- Safiri, S.; Sepanlou, S.G.; Ikuta, K.S.; Bisignano, C.; Salimzadeh, H.; Delavari, A.; Ansari, R.; Roshandel, G.; Merat, S.; Fitzmaurice, C. The global, regional, and national burden of colorectal cancer and its attributable risk factors in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2019, 4, 913–933. [Google Scholar] [CrossRef]
- Sunkara, V.; Hébert, J.R. The colorectal cancer mortality-to-incidence ratio as an indicator of global cancer screening and care. Cancer 2015, 121, 1563–1569. [Google Scholar] [CrossRef]
- Haggar, F.A.; Boushey, R.P. Colorectal cancer epidemiology: Incidence, mortality, survival, and risk factors. Clin. Colon Rectal Surg. 2009, 22, 191–197. [Google Scholar] [CrossRef]
- AIHW. Overview of Cancer in Australia. 2023. Available online: https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/contents/overview-of-cancer-in-australia-2023 (accessed on 17 May 2024).
- Arnold, M.; Abnet, C.C.; Neale, R.E.; Vignat, J.; Giovannucci, E.L.; McGlynn, K.A.; Bray, F. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology 2020, 159, 335–349.e315. [Google Scholar] [CrossRef]
- Brenner, D.R.; Heer, E.; Sutherland, R.L.; Ruan, Y.; Tinmouth, J.; Heitman, S.J.; Hilsden, R.J. National trends in colorectal cancer incidence among older and younger adults in Canada. JAMA Netw. Open 2019, 2, e198090. [Google Scholar] [CrossRef]
- Decker, K.M.; Lambert, P.; Bravo, J.; Demers, A.; Singh, H. Time trends in colorectal cancer incidence rates by income and age at diagnosis in Canada From 1992 to 2016. JAMA Netw. Open 2021, 4, e2117556. [Google Scholar] [CrossRef] [PubMed]
- Rawla, P.; Sunkara, T.; Barsouk, A. Epidemiology of colorectal cancer: Incidence, mortality, survival, and risk factors. Gastroenterol. Rev./Przegląd Gastroenterol. 2019, 14, 89–103. [Google Scholar] [CrossRef] [PubMed]
- Hua, H.; Jiang, Q.; Sun, P.; Xu, X. Risk factors for early-onset colorectal cancer: Systematic review and meta-analysis. Front. Oncol. 2023, 13, 1132306. [Google Scholar] [CrossRef]
- Elizabeth, L.; Machado, P.; Zinöcker, M.; Baker, P.; Lawrence, M. Ultra-processed foods and health outcomes: A narrative review. Nutrients 2020, 12, 1955. [Google Scholar] [CrossRef] [PubMed]
- Bosetti, C.; Bravi, F.; Turati, F.; Edefonti, V.; Polesel, J.; Decarli, A.; Negri, E.; Talamini, R.; Franceschi, S.; La Vecchia, C. Nutrient-based dietary patterns and pancreatic cancer risk. Ann. Epidemiol. 2013, 23, 124–128. [Google Scholar] [CrossRef]
- Donaldson, M.S. Nutrition and cancer: A review of the evidence for an anti-cancer diet. Nutr. J. 2004, 3, 19. [Google Scholar] [CrossRef]
- Poirier, A.E.; Ruan, Y.; Volesky, K.D.; King, W.D.; O’Sullivan, D.E.; Gogna, P.; Walter, S.D.; Villeneuve, P.J.; Friedenreich, C.M.; Brenner, D.R. The current and future burden of cancer attributable to modifiable risk factors in Canada: Summary of results. Prev. Med. 2019, 122, 140–147. [Google Scholar] [CrossRef]
- Research WCRFAIfC. Body Fatness and Weight Gain and the Risk of Cancer; World Cancer Research Fund International: London, UK, 2018. [Google Scholar]
- World Cancer Research Fund International. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective: A Summary of the Third Expert Report; World Cancer Research Fund International: London, UK, 2018. [Google Scholar]
- Melaku, Y.A.; Renzaho, A.; Gill, T.K.; Taylor, A.W.; Dal Grande, E.; de Courten, B.; Baye, E.; Gonzalez-Chica, D.; Hyppönen, E.; Shi, Z.; et al. Burden and trend of diet-related non-communicable diseases in Australia and comparison with 34 OECD countries, 1990–2015: Findings from the Global Burden of Disease Study 2015. Eur. J. Nutr. 2019, 58, 1299–1313. [Google Scholar] [CrossRef]
- Ferrari, A.J.; Santomauro, D.F.; Aali, A.; Abate, Y.H.; Abbafati, C.; Abbastabar, H.; Abd ElHafeez, S.; Abdelmasseh, M.; Abd-Elsalam, S.; Abdollahi, A. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2133–2161. [Google Scholar]
- Brauer, M.; Roth, G.A.; Aravkin, A.Y.; Zheng, P.; Abate, K.H.; Abate, Y.H.; Abbafati, C.; Abbasgholizadeh, R.; Abbasi, M.A.; Abbasian, M. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2162–2203. [Google Scholar] [CrossRef]
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Lim, S.S.; Abate, D.; Abate, K.H.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar]
- Wang, Y.; Huang, Y.; Chase, R.C.; Li, T.; Ramai, D.; Li, S.; Huang, X.; Antwi, S.O.; Keaveny, A.P.; Pang, M. Global burden of digestive diseases: A systematic analysis of the global burden of diseases study, 1990 to 2019. Gastroenterology 2023, 165, 773–783.e715. [Google Scholar] [CrossRef] [PubMed]
- Ordunez, P.; Martinez, R.; Soliz, P.; Giraldo, G.; Mujica, O.J.; Nordet, P. Rheumatic heart disease burden, trends, and inequalities in the Americas, 1990–2017: A population-based study. Lancet Glob. Health 2019, 7, e1388–e1397. [Google Scholar] [CrossRef] [PubMed]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Stanaway, J.D.; Afshin, A.; Ashbaugh, C.; Bisignano, C.; Brauer, M.; Ferrara, G.; Garcia, V.; Haile, D.; Hay, S.I.; He, J.; et al. Health effects associated with vegetable consumption: A Burden of Proof study. Nat. Med. 2022, 28, 2066–2074. [Google Scholar] [CrossRef]
- Yang, X.; Wu, D.; Liu, Y.; He, Z.; Manyande, A.; Fu, H.; Xiang, H. Global disease burden linked to diet high in red meat and colorectal cancer from 1990 to 2019 and its prediction up to 2030. Front. Nutr. 2024, 11, 1366553. [Google Scholar] [CrossRef]
- Deng, Y.; Wei, B.; Zhai, Z.; Zheng, Y.; Yao, J.; Wang, S.; Xiang, D.; Hu, J.; Ye, X.; Yang, S. Dietary risk-related colorectal cancer burden: Estimates from 1990 to 2019. Front. Nutr. 2021, 8, 690663. [Google Scholar] [CrossRef]
- Knoll, M.; Furkel, J.; Debus, J.; Abdollahi, A.; Karch, A.; Stock, C. An R package for an integrated evaluation of statistical approaches to cancer incidence projection. BMC Med. Res. Methodol. 2020, 20, 257. [Google Scholar] [CrossRef]
- Hall, M.; Friel, N. Mortality projections using generalized additive models with applications to annuity values for the irish population. Ann. Actuar. Sci. 2011, 5, 19–32. [Google Scholar] [CrossRef]
- Ahmad, O.B.; Boschi-Pinto, C.; Lopez, A.D.; Murray, C.J.; Lozano, R.; Inoue, M. Age Standardization of Rates: A New WHO Standard; World Health Organization: Geneva, Swizerland, 2001; Volume 9, pp. 1–14. [Google Scholar]
- Alston, L.; Nichols, M.; Allender, S.; Versace, V.; Brown, L.J.; Schumacher, T.; Howard, G.; Shikany, J.M.; Bolton, K.A.; Livingstone, K.; et al. Dietary patterns in rural and metropolitan Australia: A cross-sectional study exploring dietary patterns, inflammation and association with cardiovascular disease risk factors. BMJ Open 2023, 13, e069475. [Google Scholar] [CrossRef]
- Clements, M.S.; Armstrong, B.K.; Moolgavkar, S.H. Lung cancer rate predictions using generalized additive models. Biostatistics 2005, 6, 576–589. [Google Scholar] [CrossRef] [PubMed]
- Wood, S.; Wood, M.S. Package ‘mgcv’. R Package Version 2015, 1, 729. [Google Scholar]
- Galea, L.M.; Beck, E.J.; Probst, Y.C.; Cashman, C.J. Whole grain intake of Australians estimated from a cross-sectional analysis of dietary intake data from the 2011–13 Australian Health Survey. Public Health Nutr. 2017, 20, 2166–2172. [Google Scholar] [CrossRef] [PubMed]
- Ahluwalia, N.; Herrick, K.A.; Terry, A.L.; Hughes, J.P. Contribution of Whole Grains to Total Grains Intake Among Adults Aged 20 and over: United States, 2013–2016. NCHS Data Brief. 2019, 1–8. [Google Scholar] [PubMed]
- Ritzel, C.; Mann, S. The old man and the meat: On gender differences in meat consumption across stages of human life. Foods 2021, 10, 2809. [Google Scholar] [CrossRef]
- Kubberød, E.; Ueland, Ø.; Rødbotten, M.; Westad, F.; Risvik, E. Gender specific preferences and attitudes towards meat. Food Qual. Prefer. 2002, 13, 285–294. [Google Scholar] [CrossRef]
- Birrell, C.L.; Neale, E.; Probst, Y. Usual intake of meat in Australians: Secondary analysis of the 2011–12 National Nutrition and Physical Activity Survey using the NCI method. J. Hum. Nutr. Diet. 2020, 33, 505–517. [Google Scholar] [CrossRef]
- Celiberto, F.; Aloisio, A.; Girardi, B.; Pricci, M.; Iannone, A.; Russo, F.; Riezzo, G.; D’Attoma, B.; Ierardi, E.; Losurdo, G. Fibres and Colorectal Cancer: Clinical and Molecular Evidence. Int. J. Mol. Sci. 2023, 24, 13501. [Google Scholar] [CrossRef]
- Biswas, V.; Praveen, A.; Marisetti, A.L.; Sharma, A.; Kumar, V.; Sahu, S.K.; Tewari, D. A mechanistic overview on impact of dietary Fibres on gut microbiota and its association with Colon Cancer. Dietetics 2022, 1, 182–202. [Google Scholar] [CrossRef]
- Brusnic, O.; Onisor, D.; Boicean, A.; Hasegan, A.; Ichim, C.; Guzun, A.; Chicea, R.; Todor, S.B.; Vintila, B.I.; Anderco, P.; et al. Fecal Microbiota Transplantation: Insights into Colon Carcinogenesis and Immune Regulation. J. Clin. Med. 2024, 13, 6578. [Google Scholar] [CrossRef]
- Aykan, N.F. Red Meat and Colorectal Cancer. Oncol Rev. 2015, 9, 288. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sifaki-Pistolla, D.; Poimenaki, V.; Fotopoulou, I.; Saloustros, E.; Mavroudis, D.; Vamvakas, L.; Lionis, C. Significant rise of colorectal cancer incidence in younger adults and strong determinants: 30 years longitudinal differences between under and over 50s. Cancers 2022, 14, 4799. [Google Scholar] [CrossRef] [PubMed]
- Tourlouki, E.; Matalas, A.L.; Bountziouka, V.; Tyrovolas, S.; Zeimbekis, A.; Gotsis, E.; Tsiligianni, I.; Protopapa, I.; Protopapas, C.; Metallinos, G.; et al. Are current dietary habits in Mediterranean islands a reflection of the past? Results from the MEDIS study. Ecol. Food Nutr. 2013, 52, 371–386. [Google Scholar] [CrossRef] [PubMed]
- Aira, T.; Vasankari, T.; Heinonen, O.J.; Korpelainen, R.; Kotkajuuri, J.; Parkkari, J.; Savonen, K.; Uusitalo, A.; Valtonen, M.; Villberg, J. Physical activity from adolescence to young adulthood: Patterns of change, and their associations with activity domains and sedentary time. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 85. [Google Scholar] [CrossRef]
- Popkin, B.M.; Ng, S.W. The nutrition transition to a stage of high obesity and noncommunicable disease prevalence dominated by ultra-processed foods is not inevitable. Obes. Rev. 2022, 23, e13366. [Google Scholar] [CrossRef]
- Poobalan, A.S.; Aucott, L.S.; Clarke, A.; Smith, W.C. Diet behaviour among young people in transition to adulthood (18–25 year olds): A mixed method study. Health Psychol. Behav. Med. 2014, 2, 909–928. [Google Scholar] [CrossRef]
- Boutari, C.; Mantzoros, C.S. A 2022 update on the epidemiology of obesity and a call to action: As its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism 2022, 133, 155217. [Google Scholar] [CrossRef]
- Mandic, M.; Li, H.; Safizadeh, F.; Niedermaier, T.; Hoffmeister, M.; Brenner, H. Is the association of overweight and obesity with colorectal cancer underestimated? An umbrella review of systematic reviews and meta-analyses. Eur. J. Epidemiol. 2023, 38, 135–144. [Google Scholar] [CrossRef]
- Parkin, C.; Bell, S.; Mirbagheri, N. Colorectal cancer screening in Australia: An update. Aust. J. Gen. Pract. 2018, 47, 859–863. [Google Scholar] [CrossRef]
- Hyams, T.; Mueller, N.; Curbow, B.; King-Marshall, E.; Sultan, S. Screening for colorectal cancer in people ages 45–49: Research gaps, challenges and future directions for research and practice. Transl. Behav. Med. 2021, 12, 198–202. [Google Scholar] [CrossRef]
- Wu, C.W.; Lui, R.N. Early-onset colorectal cancer: Current insights and future directions. World J. Gastrointest. Oncol. 2022, 14, 230–241. [Google Scholar] [CrossRef] [PubMed]
- Sierra, M.S.; Forman, D. Burden of colorectal cancer in Central and South America. Cancer Epidemiol. 2016, 44, S74–S81. [Google Scholar] [CrossRef] [PubMed]
- OECD. Meat Consumption. 2020. Available online: https://data.oecd.org/agroutput/meat-consumption.htm (accessed on 16 May 2024).
- Chan, D.S.; Lau, R.; Aune, D.; Vieira, R.; Greenwood, D.C.; Kampman, E.; Norat, T. Red and processed meat and colorectal cancer incidence: Meta-analysis of prospective studies. PLoS ONE 2011, 6, e20456. [Google Scholar] [CrossRef] [PubMed]
- Su, J.; Liang, Y.; He, X. The global burden and trends analysis of early-onset colorectal cancer attributable to dietary risk factors in 204 countries and territories, 1990–2019: A secondary analysis for the global burden of disease study 2019. Front. Nutr. 2024, 11, 1384352. [Google Scholar] [CrossRef]
- Tang, X.; Peng, J.; Huang, S.; Xu, H.; Wang, P.; Jiang, J.; Zhang, W.; Shi, X.; Shi, L.; Zhong, X. Global burden of early-onset colorectal cancer among people aged 40–49 years from 1990 to 2019 and predictions to 2030. J. Cancer Res. Clin. Oncol. 2023, 149, 16537–16550. [Google Scholar] [CrossRef]
- Pasdar, Y.; Shadmani, F.K.; Fateh, H.L.; Soleimani, D.; Hamzeh, B.; Ghalandari, M.; Moloudpour, B.; Darbandi, M. The burden of colorectal cancer attributable to dietary risk in Middle East and North African from 1990 to 2019. Sci. Rep. 2023, 13, 20244. [Google Scholar] [CrossRef]
- Lowery, J.T.; Weber, T.K.; Ahnen, D.J.; Schroy III, P.C.; Levell, C.L.; Smith, R.A. An action plan to address the rising burden of colorectal cancer in younger adults. Color. Cancer 2020, 9, CRC24. [Google Scholar] [CrossRef]
- Clinton, S.K.; Giovannucci, E.L.; Hursting, S.D. The world cancer research fund/American institute for cancer research third expert report on diet, nutrition, physical activity, and cancer: Impact and future directions. J. Nutr. 2020, 150, 663–671. [Google Scholar] [CrossRef]
- World Cancer Research Fund International. Wholegrains, vegetables and fruit and the risk of cancer. In Continuous Update Project Expert Report; World Cancer Research Fund International: London, UK, 2018. [Google Scholar]
- Liang, Y.; Zhang, N.; Wang, M.; Liu, Y.; Ma, L.; Wang, Q.; Yang, Q.; Liu, X.; Zhou, F.; Wei, Y. Distributions and Trends of the Global Burden of Colorectal Cancer Attributable to Dietary Risk Factors over the Past 30 Years. Nutrients 2023, 16, 132. [Google Scholar] [CrossRef]
- Veettil, S.K.; Wong, T.Y.; Loo, Y.S.; Playdon, M.C.; Lai, N.M.; Giovannucci, E.L.; Chaiyakunapruk, N. Role of diet in colorectal cancer incidence: Umbrella review of meta-analyses of prospective observational studies. JAMA Netw. Open 2021, 4, e2037341. [Google Scholar] [CrossRef]
- Gao, Z.; Chen, Z.; Sun, A.; Deng, X. Gender differences in cardiovascular disease. Med. Nov. Technol. Devices 2019, 4, 100025. [Google Scholar] [CrossRef]
- Lou, L.; Wang, L.; Zhang, Y.; Chen, G.; Lin, L.; Jin, X.; Huang, Y.; Chen, J. Sex difference in incidence of gastric cancer: An international comparative study based on the Global Burden of Disease Study 2017. BMJ Open 2020, 10, e033323. [Google Scholar] [CrossRef] [PubMed]
- Visioli, F.; Sofi, F. Analyzing the Relationship Between Dietary Patterns, Health Outcomes, and Individual Food Choices. Front. Nutr. 2022, 9, 840554. [Google Scholar] [CrossRef] [PubMed]
- Tan, D.J.H.; Ng, C.H.; Muthiah, M.; Yong, J.N.; Chee, D.; Teng, M.; Wong, Z.Y.; Zeng, R.W.; Chin, Y.H.; Wang, J.-W. Rising global burden of cancer attributable to high BMI from 2010 to 2019. Metabolism 2024, 152, 155744. [Google Scholar] [CrossRef]
- Shaw, E.; Farris, M.S.; Stone, C.R.; Derksen, J.W.; Johnson, R.; Hilsden, R.J.; Friedenreich, C.M.; Brenner, D.R. Effects of physical activity on colorectal cancer risk among family history and body mass index subgroups: A systematic review and meta-analysis. BMC Cancer 2018, 18, 71. [Google Scholar] [CrossRef]
- Wang, J.; Huang, L.; Gao, Y.; Wang, Y.; Chen, S.; Huang, J.; Zheng, W.; Bao, P.; Gong, Y.; Zhang, Y. Physically active individuals have a 23% lower risk of any colorectal neoplasia and a 27% lower risk of advanced colorectal neoplasia than their non-active counterparts: Systematic review and meta-analysis of observational studies. Br. J. Sports Med. 2020, 54, 582–591. [Google Scholar] [CrossRef]
- Tran, K.B.; Lang, J.J.; Compton, K.; Xu, R.; Acheson, A.R.; Henrikson, H.J.; Kocarnik, J.M.; Penberthy, L.; Aali, A.; Abbas, Q. The global burden of cancer attributable to risk factors, 2010–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2022, 400, 563–591. [Google Scholar] [CrossRef]
- Borgas, P.; Gonzalez, G.; Veselkov, K.; Mirnezami, R. Phytochemically rich dietary components and the risk of colorectal cancer: A systematic review and meta-analysis of observational studies. World J. Clin. Oncol. 2021, 12, 482. [Google Scholar] [CrossRef]
- Wu, Z.-Y.; Chen, J.-L.; Li, H.; Su, K.; Han, Y.-W. Different types of fruit intake and colorectal cancer risk: A meta-analysis of observational studies. World J. Gastroenterol. 2023, 29, 2679. [Google Scholar] [CrossRef]
- Riggi, E.; Baccini, M.; Camussi, E.; Gallo, F.; Anatrone, C.; Pezzana, A.; Senore, C.; Giordano, L.; Segnan, N. Promoting healthy lifestyle habits among participants in cancer screening programs: Results of the randomized controlled Sti. Vi study. J. Public Health Res. 2022, 11, 22799036221106542. [Google Scholar] [CrossRef]
- Cena, H.; Calder, P.C. Defining a healthy diet: Evidence for the role of contemporary dietary patterns in health and disease. Nutrients 2020, 12, 334. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Moon, J.Y.; Lim, Y.J. Dietary intervention for preventing colorectal cancer: A practical guide for physicians. J. Cancer Prev. 2022, 27, 139. [Google Scholar] [CrossRef] [PubMed]
- World Cancer Research Fund International. Building Momentum: Lessons on Implementing a Robust Sugar Sweetened Beverage Tax; World Cancer Research Fund International: London, UK, 2018. [Google Scholar]
- Xie, W.; Zuo, J.; Ma, Z.; Yu, W.; Hu, Z.; Yang, T.; Song, Z. The Burden of Colorectal Cancer Attributable to Diet Low in Fiber from 1990 to 2019: A Global, Regional and National Analysis. J. Nutr. Health Aging 2022, 26, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Tapsell, L.C.; Neale, E.P.; Satija, A.; Hu, F.B. Foods, nutrients, and dietary patterns: Interconnections and implications for dietary guidelines. Adv. Nutr. 2016, 7, 445–454. [Google Scholar] [CrossRef]


| Country | Number (95% UI) | ASPD (95% UI) | EAPC in ASPD (95% CI) | ASDR (95% UI) | EAPC in ASDR (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| 1990 | 2021 | 1990 | 2021 | 1990–2021 | 1990 | 2021 | 1990–2021 | |
| OECD | 111,929 (27,640, 173,390) | 154,543 (37,765, 243,081) | 39.4 (9.7, 61.4) | 39.1 (9.5, 61.0) | −0.01 (−0.02, 0) | 8 (2, 13) | 6 (1, 9) | −1.26 (−1.29, −1.23) |
| Australia | 1806 (437, 2869) | 2638 (606, 4237) | 39.2 (9.4, 61.7) | 39.5 (9.1, 62.1) | 0.03 (0.02, 0.04) | 9 (2, 15) | 6 (1, 9) | −1.9 (−2.0, −1.8) |
| Austria | 1167 (283, 1855) | 903 (192, 1451) | 38.6 (9.3, 60.3) | 38.4 (8.6, 60.8) | 0.01 (−0.001, 0.01) | 10 (2, 15) | 5 (1, 7) | −2.42 (−2,47, −2.36) |
| Belgium | 1573 (376, 2454) | 1459 (301, 2332) | 39.3 (9.2, 61.7) | 39.7 (8.6, 62.3) | 0.07 (0.06, 0.08) | 10 (2, 16) | 6 (1, 9) | −1.73 (−1.83, −1.64) |
| Canada | 2637 (702, 4122) | 4159 (989, 6645) | 39.2 (10.7, 61.0) | 38.6 (9.7, 60.7) | −0.04 (−0.05, −0.37) | 8 (2, 13) | 5 (1, 9) | −1.08 (−1.19, −0.98) |
| Chile | 515 (183, 769) | 1476 (428, 2274) | 43.6 (15.3, 64.5) | 43.2 (13, 65.4) | −0.01 (−0.01, 0.03) | 5 (2, 8) | 6 (2, 9) | 0.48 (0.35, 0.61) |
| Colombia | 602 (242, 880) | 2142 (720, 3374) | 38.6 (15.7, 57.2) | 37.0 (13.2, 56.3) | −0.10 (−0.14, −0.06) | 4 (1, 5) | 4 (1, 6) | 0.09 −0.08, 0.27) |
| Costa Rica | 60 (21, 90) | 299 (95, 473) | 37.1 (13.2, 56.4) | 35.9 (11.8, 55.4) | −0.13 (−0.14, −0.12) | 4 (1, 5) | 5 (2, 9) | 1.67 (1.48, 1.86) |
| Czechia | 1784 (459, 2891) | 1663 (417, 2699) | 37.0 (9.7, 58.5) | 36.8 (8.9, 58.4) | −0.02 (−0.03, −0.01) | 13 (3, 21) | 7 (2, 12) | −2.07 (−2.26, −1.89) |
| Denmark | 773 (181, 1233) | 969 (194, 1558) | 39.2 (8.9, 61.5) | 39.5 (8.3, 62.3) | 0.04 (0.03, 0.05) | 9 (2, 15) | 8 (1, 12) | −1.02 (−1.31, −0.74) |
| Estonia | 156 (27, 247) | 213 (34, 348) | 41.3 (7.6, 64.7) | 40.3 (7, 63.7) | −0.08 (−0.1, −0.07) | 8 (1, 12) | 7 (1, 12) | −0.49 (−0.65, −0.33) |
| Finland | 421 (98, 688) | 608 (126, 991) | 38.8 (8.8, 60.9) | 38.4 (8.4, 60.9) | −0.02 (−0.03, −0.01) | 6 (1, 9) | 4 (1, 7) | −0.92 (−1.03, −0.82) |
| France | 8375 (1917, 13,152) | 9905 (2054, 16,027) | 40.1 (8.9, 63.0) | 40.3 (8.8, 63.2) | 0.025 (0.02, 0.03) | 10 (2, 15) | 6 (1, 10) | −1.44 (−1.49, −1.39) |
| Germany | 13,923 (3089, 21,858) | 12,305 (2324, 19,763) | 40.0 (8.8, 62.5) | 39.7 (7.9, 62.7) | −0.015 (−0.02, −01) | 11 (2, 17) | 6 (1, 9) | −2.19 (−2.3, −2.08) |
| Greece | 909 (231, 1429) | 1485 (348, 2396) | 38.1 (9.9, 59.5) | 38.2 (9.6, 60.2) | 0.04 (0.03, 0.05) | 6 (2, 10) | 5 (1, 9) | −0.7 (−0.9, −0.5) |
| Hungary | 1734 (469, 2809) | 2049 (575, 3269) | 38.7 (11.1, 60.1) | 39.3 (10.9, 61) | 0.06 (0.05, 0.08) | 12 (3, 19) | 10 (3, 16) | −0.57 (−0.82, −0.330 |
| Iceland | 19 (4, 30) | 27 (6, 44) | 39.9 (8.6, 62.5) | 39.3 (8.3, 62.2) | −0.07 (−0.08, −0.06) | 6 (1, 10) | 4 (1, 7) | −1.08 (−1.2, −0.96) |
| Ireland | 398 (87, 638) | 449 (95, 741) | 38.1 (8.4, 60.3) | 37.9 (7.6, 60.6) | 0.02 (0.01, 0.03) | 10 (2, 16) | 5 (1, 9) | −1.7 (−1.78, −1.620 |
| Israel | 380 (97, 612) | 656 (177, 1058) | 37.1 (9.9, 57.9) | 37.2 (9.5, 58.5) | 0.025 (0.015, 0.034) | 8 (2, 13) | 5 (1, 8) | −2.11 (−2.41, −1.81) |
| Italy | 7092 (1718, 10,959) | 9281 (2127, 14,597) | 39.9 (9.9, 62.1) | 39.6 (9.4, 62) | −0.013 (−0.018, −0.007) | 8 (2, 12) | 6 (1, 9) | −1.11 (−1.23, −1.0) |
| Japan | 12,011 (3491, 18,581) | 26,082 (8321, 40,865) | 38.3 (11.1, 59.2) | 38.4 (11.9, 58.7) | 0.09 (0.06, 0.12) | 7 (2, 11) | 6 (2, 10) | −0.54 (−0.60, −0.49) |
| Latvia | 268 (48, 427) | 291 (50, 480) | 42.0 (7.5, 65.4) | 41.3 (7.3, 64.6) | −0.07 (−0.09, −0.05) | 7 (1, 12) | 7 (1, 11) | −0.18 (−0.36, 0) |
| Lithuania | 321 (65, 502) | 434 (78, 700) | 43.2 (9.0, 66.3) | 41.8 (7.5, 65.7) | −0.13 (−0.14, −0.11) | 7 (1, 11) | 7 (1, 11) | −0.05 (−0.21, 0.10) |
| Luxembourg | 59 (11, 92) | 67 (12, 107) | 40.4 (8.0, 63.4) | 39.9 (7.8, 63) | −0.04 (−0.05, −0.02) | 11 (2, 17) | 6 (1, 9) | −1.94 (−2.12, −1.77) |
| Mexico | 908 (332, 1378) | 3886 (1303, 6170) | 36.3 (13.4, 55.2) | 35.6 (11.9, 55) | −0.1 (−0.12, −0.08) | 2 (1, 4) | 3 (1, 5) | 1.03 (0.87, 1.19) |
| Netherlands | 1850 (412, 2949) | 2868 (577, 4623) | 37.9 (8.6, 60.0) | 38.5 (8.2, 61.0) | 0.07 (0.06, 0.08) | 9 (2, 14) | 8 (2, 12) | −0.43 (−0.6, −0.26) |
| New Zealand | 468 (122, 734) | 662 (192, 1028) | 39.9 (10.5, 62.0) | 41.3 (11.8, 63.4) | 0.13 (0.1, 0.16) | 12 (3, 19) | 8 (2, 12) | −1.58 (−1.64, −1.51) |
| Norway | 705 (137, 1124) | 820 (149, 1291) | 41.1 (7.9, 64.5) | 41.2 (7.7, 64.3) | 0.02 (0.01, 0.03) | 10 (2, 16) | 7 (1, 12) | −0.96 (−1.05, −0.87) |
| Poland | 3475 (1017, 5382) | 6801 (1903, 10,813) | 37.3 (11.1, 58.2) | 37.4 (10.4, 58.7) | 0.01 (−0.01, 0.04) | 8 (2, 12) | 9 (3, 14) | 0.21 (0.04, 0.38) |
| Portugal | 1185 (388, 1856) | 1783 (467, 2818) | 38.1 (11.8, 58.8) | 38.1 (10.7, 59.6) | 0.04 (0.02, 0.05) | 9 (3, 14) | 7 (2, 10) | −0.85 (−1.04, −0.67) |
| Republic of Korea | 1385 (476, 2189) | 4334 (1406, 7197) | 36.5 (12.1, 55.7) | 37.1 (11.8, 57) | 0.01 (−0.04, 0.06) | 5 (2, 8) | 5 (2, 8) | −0.52 (−0.72, −0.32) |
| Slovakia | 636 (193, 996) | 954 (249, 1530) | 39.2 (11.9, 60.5) | 39.9 (11.1, 61.7) | 0.08 (0.07, 0.09) | 11 (3, 17) | 10 (3, 16) | −0.22 (−0.32, −0.12) |
| Slovenia | 213 (52, 339) | 308 (58, 512) | 40.1 (9.1, 62.9) | 39.1 (8, 62) | −0.09 (−0.1, −0.08) | 9 (2, 14) | 6 (1, 11) | −1.18 (−1.47, −0.89) |
| Spain | 4500 (1055, 7039) | 7332 (1805, 11,511) | 41.4 (10, 63.8) | 40.3 (10, 62.7) | −0.07 (−0.09, −0.06) | 8 (2, 13) | 7 (2, 10) | −0.57 (−0.68, −0.45) |
| Sweden | 1186 (248, 1895) | 1400 (288, 2264) | 39.7 (8.1, 62.8) | 40.1 (7.7, 63.4) | 0.051 (0.047, 0.054) | 7 (2, 12) | 6 (1, 9) | −0.73 (−0.89, −0.57) |
| Switzerland | 636 (139, 1026) | 821 (186, 1329) | 39.1 (8.8, 61.5) | 39.2 (8.7, 61.9) | 0.03 (0.02, 0.04) | 6 (1, 9) | 4 (1, 7) | −1.26 (−1.41, −1.10) |
| Türkiye | 1896 (644, 2988) | 3957 (1236, 6428) | 34.3 (11.3, 53.1) | 34.1 10.7, 53.1) | −0.03 (−0.04, −0.02) | 6 (2, 9) | 4 (1, 7) | −0.86 (−1.2, −0.520 |
| United Kingdom | 9163 (2118, 14,306) | 8801 (1806, 14,038) | 40.4 (9.4, 62.9) | 39.7 (8.2, 62.2) | −0.04 (−0.05, −0.02) | 10 (2, 15) | 6 (1, 10) | −1.48 (−1.6, −1.37) |
| USA | 26,740 (6011, 41,721) | 30,257 (6050, 47,938) | 39.8 (8.9, 62.5) | 40.3 (8, 63.4) | 0.06 (0.05, 0.07) | 8 (2, 13) | 5 (1, 8) | −1.65 (−1.72, −1.58) |
| Country | Number (95% UI) | ASP of DALYs(95% UI) | EAPC in ASP of DALYs (95% CI) | ASR of DALYs (95% UI) | EAPC in ASR of DALYs (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| 1990 | 2021 | 1990 | 2021 | 1990–2021 | 1990 | 2021 | 1990–2021 | |
| OECD | 2,447,568 (587,458, 3,793,421) | 3,088,502 (722,609, 4,844,604) | 39.2 (9.3, 61.3) | 39.1 (9.1, 61.3) | 0.01 (0.0, 0.02) | 185 (44, 286) | 129 (30, 202) | −1.2 1(−1.24, −1.18) |
| Australia | 41,810 (9654, 66,014) | 53,560 (11,898, 85,652) | 39.2 (8.9, 61.8) | 39.7 (8.6, 62.6) | 0.05 (0.04, 0.06) | 217 (50, 343) | 125 (28, 201) | −2.01 (−2.11, −1.9) |
| Austria | 23,934 (5575, 38,183) | 17,098 (3535, 27,380) | 38.6 (8.7, 60.7) | 38.6 (8.1, 61) | 0.02 (0.01, 0.03) | 208 (48, 334) | 98 (20, 157) | −2.44 (−2.49, −2.39) |
| Belgium | 31,156 (7250, 48,714) | 27,094 (5386, 43,031) | 39.1 (8.7, 61.6) | 39.9 (8.1, 62.7) | 0.09 (0.08, 0.100) | 206 (48, 323) | 120 (23, 192) | −1.66 (−1.78, −1.55) |
| Canada | 59,373 (15,197, 92,681) | 83,514 (18,914, 134,678) | 39.4 (10.1, 61.4) | 38.8 (9.3, 61.1) | −0.04 (−0.05, −0.03) | 185 (47, 289) | 123 (28, 199) | −1.12 (−1.21, −1.04) |
| Chile | 11,988 (4091, 18,126) | 31,846 (8928, 49,564) | 43.2 (14.8, 64.2) | 42.9 (12.5, 65.2) | 0.03 (0.01, 0.05) | 118 (41, 179) | 126 (35, 195) | 0.57 (0.43, 0.71) |
| Colombia | 15,613 (6063, 22,799) | 52,113 (17,201, 82,519) | 38.3 (15.3, 57.0) | 36.6 (12.8, 56.0) | −0.07 (−0.11, −0.04 | 84 (33, 123) | 95 (31, 150) | 0.31 (0.13, 0.49) |
| Costa Rica | 1455 (502, 2191) | 7248 (2230, 11,553) | 37 (13, 56.3) | 35.5 (11.4, 55.0) | −0.14 (−0.15, −0.13) | 80 (28, 121) | 132 (41, 210) | 1.85 (1.63, 2.06) |
| Czechia | 40,019 (9904, 64,933) | 34,002 (8091, 56,056) | 37.0 (9.3, 58.5) | 36.8 (8.6, 58.7) | −0.02 (−0.03, −0.01) | 292 (72, 473) | 164 (38, 271) | −2.17 (−2.34, −2) |
| Denmark | 16,097 (3603, 25,778) | 17,938 (3532, 28,801) | 39.1 (8.3, 61.6) | 39.7 (8.0, 62.8) | 0.07 (0.06, 0.07) | 207 (46, 331) | 153 (30, 245) | −1.29 (−1.56, −1.03) |
| Estonia | 3749 (630, 5953) | 4075 (623, 6651) | 41.2 (7.3, 64.7) | 40.5 (6.5, 64.2) | −0.07 (−0.08, −0.06) | 183 (31, 291) | 155 (23, 252) | −0.92 (−1.1, −0.75) |
| Finland | 8961 (2028, 14,537) | 11,372 (2282, 18,457) | 38.7 (8.4, 61.0) | 38.5 (7.9, 61.1) | −0.01 (−0.02, 0.01) | 128 (29, 207) | 94 (19, 152) | −0.98 (−1.06, −0.91) |
| France | 164,856 (36,239, 257,031) | 176,774 (35,873, 283,700 | 40.2 (8.4, 63.2) | 40.5 (8.3, 63.7) | 0.034 (0.029, 0.04) | 204 (44, 318) | 131 (26, 210) | −1.33 (−1.39, −1.28) |
| Germany | 284,382 (60,709, 448,644) | 233,980 (42,468, 377,323) | 39.9 (8.2, 62.7) | 39.9 (7.4, 63.3) | 0.009 (0.0, 0.01) | 228 (48, 359) | 129 (23, 209) | −2.06 (−2.17, −1.96) |
| Greece | 18,682 (4608, 29,483) | 26,319 (5988, 42,194) | 38.2 (9.6, 59.8) | 38.6 (8.9, 60.7) | 0.06 (0.05, 0.07) | 125 (31, 197) | 115 (26, 183) | −0.49 (−0.64, −0.34) |
| Hungary | 39,246 (10,315, 63,541) | 44,491 (12,098, 70,563) | 38.6 (10.8, 60.2) | 39.3 (10.5, 61.1) | 0.08 (0.06, 0.09 | 271 (71, 437) | 242 (65, 384) | −0.46 (−0.7, −0.22) |
| Iceland | 398 (85, 639) | 539 (109, 874) | 40.2 (8.4, 62.9) | 39.5 (8, 62.7) | −0.07 (−0.08, −0.06) | 142 (30, 227) | 95 (19, 154) | −1.26 (−1.36, −1.16) |
| Ireland | 8631 (1819, 13,784) | 9161 (1863, 15,075) | 38.2 (8.2, 60.7) | 38.2 (7.3, 61.1) | 0.04 (0.02, 0.05) | 216 (45, 345) | 118 (24, 194) | −1.8 (−1.87, −1.72) |
| Israel | 8012 (1981, 12,911) | 12,317 (3310, 20,045) | 37.2 (9.6, 58.1) | 37.3 (9.1, 58.9) | 0.03 (0.02, 0.04) | 168 (41, 271) | 101 (27, 165) | −2.09 (−2.38, −1.8) |
| Italy | 152,655 (35,816, 236,320) | 169,830 (38,242, 266,960) | 39.9 (9.5, 62.2) | 39.7 (8.8, 62.5) | −0.006 (−0.01, −0.001) | 177 (41, 273) | 123 (27, 192) | −1.22 (−1.36, −1.08) |
| Japan | 290,209 (80,950, 446,618) | 455,770 (134,725, 709,276) | 38.5 (10.7, 59.6) | 39.3 (10.9, 60.6) | 0.11 (0.07, 0.14) | 171 (48, 264) | 141 (39, 217) | −0.67 (−0.72, −0.61) |
| Latvia | 6464 (1114, 10,336) | 5895 (961, 9689) | 42.1 (7.3, 65.5) | 41.4 (6.8, 65.1) | −0.06 (−0.08, −0.05) | 182 (31, 291) | 158 (25, 260) | −0.49 (−0.65, −0.33) |
| Lithuania | 7731 (1499, 12,025) | 8699 (1464, 13,964) | 43.2 (8.6, 66.5) | 41.9 (7.1, 66) | −0.12 (−0.14, −0.11 | 173 (36, 269) | 159 (26, 255) | −0.32 (−0.49, −0.15) |
| Luxembourg | 1259 (229, 1980) | 1281 (219, 2030) | 40.5 (7.6, 63.7) | 40.2 (7.3, 63.7) | −0.02 (−0.04, −0.002) | 236 (43, 370) | 121 (20, 191) | −2.11 (−2.3, −1.91) |
| Mexico | 23,137 (8256, 35,025) | 103,481 (33,582, 165,002) | 36.2 (13.1, 55.1) | 35.4 (11.6, 54.8) | −0.08 (−0.09, −0.06 | 52 (19, 78) | 79 (26, 126) | 1.47 (1.33, 1.61) |
| Netherlands | 39,915 (8615, 62,804) | 58,703 (11,593, 94,146) | 38.1 (8.3, 60.4) | 38.8 (7.9, 61.5) | 0.08 (0.06, 0.09) | 203 (44, 319) | 172 (34, 277) | −0.43 (−0.6, −0.25) |
| New Zealand | 10,802 (2727, 16,969) | 13,248 (3730, 20,797) | 39.9 (10.1, 62.2) | 41.5 (11.4, 63.8) | 0.15 (0.12, 0.18 | 282 (71, 444) | 162 (45, 255) | −1.9 (−1.97, −1.82 |
| Norway | 14,184 (2642, 22,565) | 15,173 (2627, 23,707) | 41.2 (7.5, 64.9) | 41.5 (7.2, 64.9) | 0.03 (0.025, 0.04) | 219 (40, 348) | 153 (26, 239) | −1.19 (−1.28, −1.09) |
| Poland | 81,586 (23,281, 126,802) | 137,297 (37,548, 218,480) | 37.2 (10.8, 58.1) | 37.4 (10.0, 58.8) | 0.04 (0.01, 0.06) | 187 (53, 290) | 196 (53, 311) | 0.07 (−0.1, 0.24) |
| Portugal | 25,514 (8043, 40,163 | 33,503 (8236, 53,029) | 38.0 (11.5, 58.8) | 38.3 (9.9, 60.0) | 0.07 (0.05, 0.09) | 190 (60, 299) | 146 (35, 232) | −0.7 (−0.93, −0.48) |
| Republic of Korea | 39,094 (12,987, 61,733) | 90,428 (27,166, 151,428 | 36.4 (12.0, 55.6) | 36.8 (11.1, 57.0) | 0.05 (0.0, 0.11) | 122 (42, 193) | 99 (30, 165) | −0.82 (−1.04, −0.59) |
| Slovakia | 15,332 (4510, 23,998) | 21,188 (5375, 34,094) | 39.2 (11.7, 60.5) | 40.0 (10.7, 61.9) | 0.09 (0.08, 0.1) | 256 75, 402) | 225 (57, 362) | −0.4 (−0.5, −0.31) |
| Slovenia | 4874 (1126, 7758) | 5752 (1052, 9567) | 40.0 (8.7, 63) | 39.2 (7.5, 62.2) | −0.08 (−0.09, −0.06 | 198 (46, 315) | 133 (24, 221) | −1.52 (−1.82, −1.22) |
| Spain | 97,143 (21,820, 151,549) | 137,666 (32,843, 216,061) | 41.4 (9.5, 64) | 40.4 (9.4, 63.1) | −0.07 (−0.09, −0.06) | 184 (41, 288) | 146 (34, 229) | −0.67 (−0.78, −0.55) |
| Sweden | 23,510 (4742, 37,458) | 24,843 (5007, 40,676) | 39.7 (7.8, 62.8) | 40.4 (7.3, 63.9) | 0.07 (0.067, 0.08) | 164 (33, 261) | 119 (23, 193) | −0.85 (−1.01, −0.68) |
| Switzerland | 13,252 (2779, 21,276) | 15,328 (3353, 24,440) | 39.2 (8.4, 61.7) | 39.5 (8.2, 62.3) | 0.04 (0.035, 0.05 | 132 (27, 210) | 87 (19, 137) | −1.44 (−1.61, −1.27) |
| Türkiye | 53,019 (17,530, 84,868) | 95,901 (29,451, 157,132) | 34.2 (11.2, 53.1) | 33.8 (10.4, 52.8) | −0.03 (−0.04, −0.02) | 142 (48, 226) | 101 (31, 166) | −1.16 (−1.48, −0.85) |
| United Kingdom | 188,188 (41,836, 291,875) | 165,949 (32,736, 263,323) | 40.4 (8.8, 63.1) | 40.0 (7.7, 62.8) | −0.02 (−0.03, 0) | 216 (47, 335) | 134 (26, 213) | −1.58 (−1.69, −1.46) |
| USA | 581,339 (124,030, 904,032) | 685,126 (130,008, 1,077,155) | 39.8 (8.4, 62.7) | 40.5 (7.5, 63.9) | 0.08 (0.07, 0.09) | 187 (39, 290) | 128 (24, 201) | −1.32 (−1.38, −1.26) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abebe, Z.; Wassie, M.M.; Reynolds, A.C.; Melaku, Y.A. Burden and Trends of Diet-Related Colorectal Cancer in OECD Countries: Systematic Analysis Based on Global Burden of Disease Study 1990–2021 with Projections to 2050. Nutrients 2025, 17, 1320. https://doi.org/10.3390/nu17081320
Abebe Z, Wassie MM, Reynolds AC, Melaku YA. Burden and Trends of Diet-Related Colorectal Cancer in OECD Countries: Systematic Analysis Based on Global Burden of Disease Study 1990–2021 with Projections to 2050. Nutrients. 2025; 17(8):1320. https://doi.org/10.3390/nu17081320
Chicago/Turabian StyleAbebe, Zegeye, Molla Mesele Wassie, Amy C. Reynolds, and Yohannes Adama Melaku. 2025. "Burden and Trends of Diet-Related Colorectal Cancer in OECD Countries: Systematic Analysis Based on Global Burden of Disease Study 1990–2021 with Projections to 2050" Nutrients 17, no. 8: 1320. https://doi.org/10.3390/nu17081320
APA StyleAbebe, Z., Wassie, M. M., Reynolds, A. C., & Melaku, Y. A. (2025). Burden and Trends of Diet-Related Colorectal Cancer in OECD Countries: Systematic Analysis Based on Global Burden of Disease Study 1990–2021 with Projections to 2050. Nutrients, 17(8), 1320. https://doi.org/10.3390/nu17081320







