Role and Mechanism of Short-Chain Fatty Acids in Skeletal Muscle Homeostasis and Exercise Performance
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Inclusion and Exclusion Criteria
3. Results
3.1. Short-Chain Fatty Acids: Types and Sources
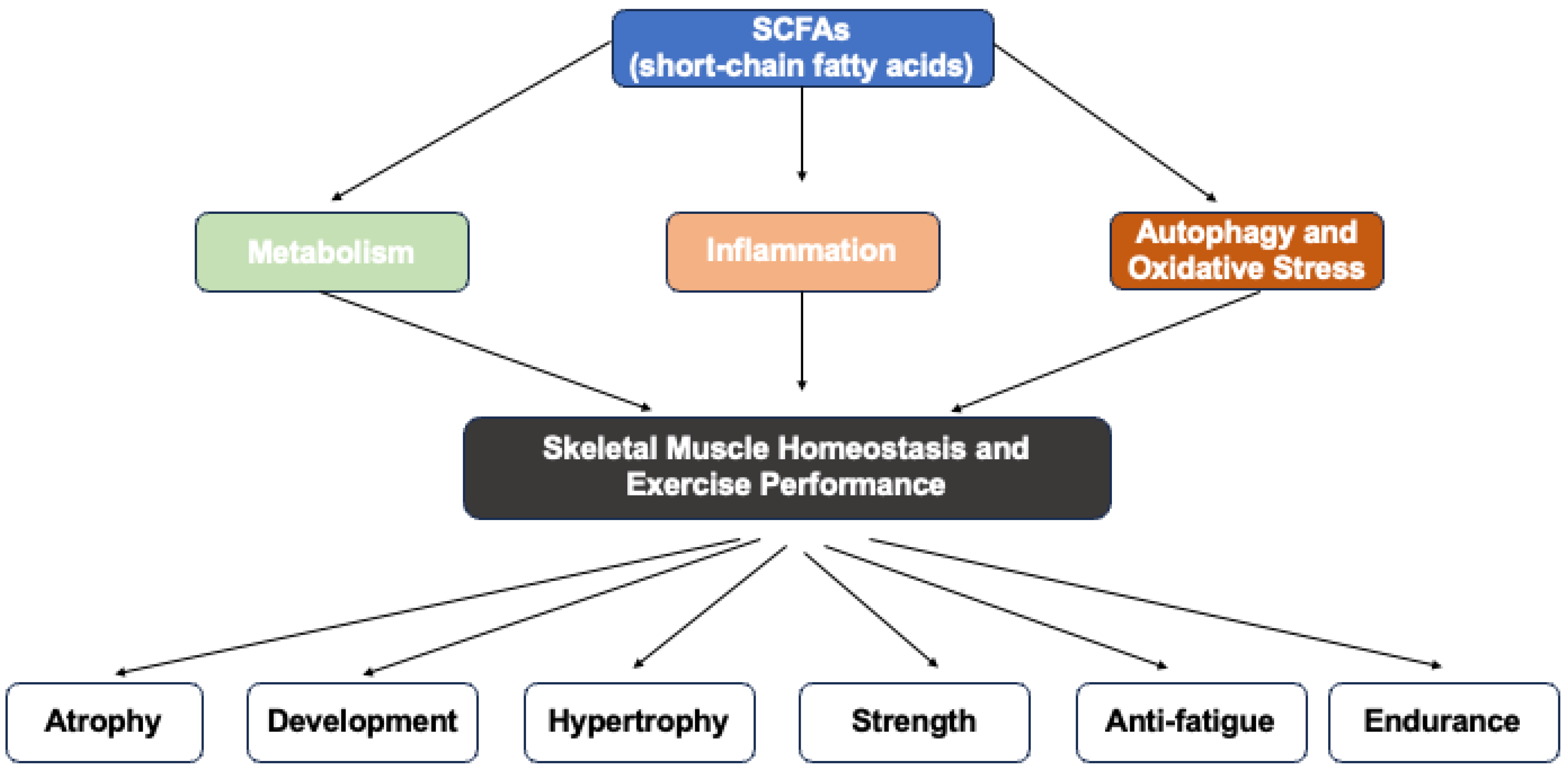
3.2. Role and Mechanisms of SCFAs in Skeletal Muscle Homeostasis and Exercise Performance
3.2.1. SCFAs and Muscle Mass and Exercise Performance
3.2.2. SCFAs and Skeletal Muscle Homeostasis
SCFAs and Protein Synthesis and Degradation
SCFAs and Skeletal Muscle Metabolism
SCFAs Inhibited Skeletal Muscle Autophagy and Oxidative Stress
SCFAs Inhibited Skeletal Muscle Inflammation
4. Conclusions
5. Further Studies Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SCFAs | Short-chain fatty acids |
| GLP-1 | Glucagon-like peptide-1 |
| PYY | Peptide YY |
| PPARδ | Peroxisome proliferator-activated receptor delta |
| AMPK | AMP-activated protein kinase |
| GLUT4 | Glucose transporter type 4 |
| T2DM | Type 2 diabetes mellitus |
| TGF-β | Transforming growth factor beta |
| NF-κB | Nuclear factor kappa B |
| MHC | Myosin heavy chain |
| Mef2a | Myocyte enhancer factor 2A |
| ACECS2 | Acetyl-CoA synthase 2 |
| HOMA2-IR | Homeostasis Model Assessment of Insulin Resistance |
| SAMP8 | Senescence-accelerated mouse prone 8 |
| C2C12 | Mouse myoblast cell line |
| PCOS | Polycystic ovary syndrome |
| IL-8 | Interleukin 8 |
| Tregs | Regulatory T cells |
| RANTES | Regulated upon activation, normal T cell expressed and secreted |
| LPS | Lipopolysaccharide |
| HDAC | Histone deacetylase |
| NLRP3 | NOD-like receptor family, pyrin domain containing 3 |
| SCFAs | Short-chain fatty acids |
References
- Chen, W.; You, W.; Valencak, T.G.; Shan, T. Bidirectional Roles of Skeletal Muscle Fibro-Adipogenic Progenitors in Homeostasis and Disease. Ageing Res. Rev. 2022, 80, 101682. [Google Scholar] [CrossRef] [PubMed]
- Scicchitano, B.M.; Dobrowolny, G.; Sica, G.; Musarò, A. Molecular Insights into Muscle Homeostasis, Atrophy and Wasting. Curr. Genom. 2018, 19, 356–369. [Google Scholar] [CrossRef] [PubMed]
- Yin, L.; Li, N.; Jia, W.; Wang, N.; Liang, M.; Yang, X.; Du, G. Skeletal Muscle Atrophy: From Mechanisms to Treatments. Pharmacol. Res. 2021, 172, 105807. [Google Scholar] [CrossRef] [PubMed]
- Sui, S.X.; Williams, L.J.; Holloway-Kew, K.L.; Hyde, N.K.; Pasco, J.A. Skeletal Muscle Health and Cognitive Function: A Narrative Review. Int. J. Mol. Sci. 2020, 22, 255. [Google Scholar] [CrossRef]
- Damas, F.; Libardi, C.A.; Ugrinowitsch, C. The Development of Skeletal Muscle Hypertrophy through Resistance Training: The Role of Muscle Damage and Muscle Protein Synthesis. Eur. J. Appl. Physiol. 2018, 118, 485–500. [Google Scholar] [CrossRef]
- Damas, F.; Phillips, S.; Vechin, F.C.; Ugrinowitsch, C. A Review of Resistance Training-Induced Changes in Skeletal Muscle Protein Synthesis and Their Contribution to Hypertrophy. Sports Med. 2015, 45, 801–807. [Google Scholar] [CrossRef]
- Hargreaves, M.; Spriet, L.L. Skeletal Muscle Energy Metabolism during Exercise. Nat. Metab. 2020, 2, 817–828. [Google Scholar] [CrossRef]
- Smith, J.A.B.; Murach, K.A.; Dyar, K.A.; Zierath, J.R. Exercise Metabolism and Adaptation in Skeletal Muscle. Nat. Rev. Mol. Cell Biol. 2023, 24, 607–632. [Google Scholar] [CrossRef]
- Zhang, D.; Jian, Y.-P.; Zhang, Y.-N.; Li, Y.; Gu, L.-T.; Sun, H.-H.; Liu, M.-D.; Zhou, H.-L.; Wang, Y.-S.; Xu, Z.-X. Short-Chain Fatty Acids in Diseases. Cell Commun. Signal 2023, 21, 212. [Google Scholar] [CrossRef]
- Mann, E.R.; Lam, Y.K.; Uhlig, H.H. Short-Chain Fatty Acids: Linking Diet, the Microbiome and Immunity. Nat. Rev. Immunol. 2024, 24, 577–595. [Google Scholar] [CrossRef]
- Coppola, S.; Avagliano, C.; Calignano, A.; Berni Canani, R. The Protective Role of Butyrate against Obesity and Obesity-Related Diseases. Molecules 2021, 26, 682. [Google Scholar] [CrossRef] [PubMed]
- Frampton, J.; Murphy, K.G.; Frost, G.; Chambers, E.S. Short-Chain Fatty Acids as Potential Regulators of Skeletal Muscle Metabolism and Function. Nat. Metab. 2020, 2, 840–848. [Google Scholar] [CrossRef] [PubMed]
- Hernández, M.A.G.; Canfora, E.E.; Jocken, J.W.E.; Blaak, E.E. The Short-Chain Fatty Acid Acetate in Body Weight Control and Insulin Sensitivity. Nutrients 2019, 11, 1943. [Google Scholar] [CrossRef]
- Yang, G.; Zhang, J.; Liu, Y.; Sun, J.; Ge, L.; Lu, L.; Long, K.; Li, X.; Xu, D.; Ma, J. Acetate Alleviates Gut Microbiota Depletion-Induced Retardation of Skeletal Muscle Growth and Development in Young Mice. Int. J. Mol. Sci. 2024, 25, 5129. [Google Scholar] [CrossRef]
- Koh, A.; De Vadder, F.; Kovatcheva-Datchary, P.; Bäckhed, F. From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell 2016, 165, 1332–1345. [Google Scholar] [CrossRef]
- Louis, P.; Flint, H.J. Formation of Propionate and Butyrate by the Human Colonic Microbiota. Environ. Microbiol. 2017, 19, 29–41. [Google Scholar] [CrossRef]
- Chambers, E.S.; Viardot, A.; Psichas, A.; Morrison, D.J.; Murphy, K.G.; Zac-Varghese, S.E.K.; MacDougall, K.; Preston, T.; Tedford, C.; Finlayson, G.S.; et al. Effects of Targeted Delivery of Propionate to the Human Colon on Appetite Regulation, Body Weight Maintenance and Adiposity in Overweight Adults. Gut 2015, 64, 1744–1754. [Google Scholar] [CrossRef]
- Morrison, D.J.; Preston, T. Formation of Short Chain Fatty Acids by the Gut Microbiota and Their Impact on Human Metabolism. Gut Microbes 2016, 7, 189–200. [Google Scholar] [CrossRef]
- Rivière, A.; Selak, M.; Lantin, D.; Leroy, F.; De Vuyst, L. Bifidobacteria and Butyrate-Producing Colon Bacteria: Importance and Strategies for Their Stimulation in the Human Gut. Front. Microbiol. 2016, 7, 979. [Google Scholar] [CrossRef]
- Canfora, E.E.; Jocken, J.W.; Blaak, E.E. Short-Chain Fatty Acids in Control of Body Weight and Insulin Sensitivity. Nat. Rev. Endocrinol. 2015, 11, 577–591. [Google Scholar] [CrossRef]
- Hosmer, J.; McEwan, A.G.; Kappler, U. Bacterial Acetate Metabolism and Its Influence on Human Epithelia. Emerg. Top. Life Sci. 2024, 8, 1–13. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Zhang, P.; Shen, L.; Niu, L.; Tan, Y.; Chen, L.; Zhao, Y.; Bai, L.; Hao, X.; Li, X.; et al. Short-Chain Fatty Acids and Their Association with Signalling Pathways in Inflammation, Glucose and Lipid Metabolism. Int. J. Mol. Sci. 2020, 21, 6356. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Fu, C.; Li, F. Acetate Affects the Process of Lipid Metabolism in Rabbit Liver, Skeletal Muscle and Adipose Tissue. Animals 2019, 9, 799. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, E.; Grootaert, C.; Verstraete, W.; Van de Wiele, T. Propionate as a Health-Promoting Microbial Metabolite in the Human Gut. Nutr. Rev. 2011, 69, 245–258. [Google Scholar] [CrossRef]
- Wilson, K.A.; Han, Y.; Zhang, M.; Hess, J.P.; Chapman, K.A.; Cline, G.W.; Tochtrop, G.P.; Brunengraber, H.; Zhang, G.-F. Inter-Relations between 3-Hydroxypropionate and Propionate Metabolism in Rat Liver: Relevance to Disorders of Propionyl-CoA Metabolism. Am. J. Physiol. Endocrinol. Metab. 2017, 313, E413–E428. [Google Scholar] [CrossRef]
- Chambers, E.S.; Byrne, C.S.; Morrison, D.J.; Murphy, K.G.; Preston, T.; Tedford, C.; Garcia-Perez, I.; Fountana, S.; Serrano-Contreras, J.I.; Holmes, E.; et al. Dietary Supplementation with Inulin-Propionate Ester or Inulin Improves Insulin Sensitivity in Adults with Overweight and Obesity with Distinct Effects on the Gut Microbiota, Plasma Metabolome and Systemic Inflammatory Responses: A Randomised Cross-over Trial. Gut 2019, 68, 1430–1438. [Google Scholar] [CrossRef]
- Perry, R.J.; Borders, C.B.; Cline, G.W.; Zhang, X.-M.; Alves, T.C.; Petersen, K.F.; Rothman, D.L.; Kibbey, R.G.; Shulman, G.I. Propionate Increases Hepatic Pyruvate Cycling and Anaplerosis and Alters Mitochondrial Metabolism. J. Biol. Chem. 2016, 291, 12161–12170. [Google Scholar] [CrossRef]
- El Hage, R.; Hernandez-Sanabria, E.; Calatayud Arroyo, M.; Van de Wiele, T. Supplementation of a Propionate-Producing Consortium Improves Markers of Insulin Resistance in an in Vitro Model of Gut-Liver Axis. Am. J. Physiol. Endocrinol. Metab. 2020, 318, E742–E749. [Google Scholar] [CrossRef]
- Yoshida, H.; Ishii, M.; Akagawa, M. Propionate Suppresses Hepatic Gluconeogenesis via GPR43/AMPK Signaling Pathway. Arch. Biochem. Biophys. 2019, 672, 108057. [Google Scholar] [CrossRef]
- Haghikia, A.; Zimmermann, F.; Schumann, P.; Jasina, A.; Roessler, J.; Schmidt, D.; Heinze, P.; Kaisler, J.; Nageswaran, V.; Aigner, A.; et al. Propionate Attenuates Atherosclerosis by Immune-Dependent Regulation of Intestinal Cholesterol Metabolism. Eur. Heart J. 2022, 43, 518–533. [Google Scholar] [CrossRef]
- Liu, H.; Wang, J.; He, T.; Becker, S.; Zhang, G.; Li, D.; Ma, X. Butyrate: A Double-Edged Sword for Health? Adv. Nutr. 2018, 9, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Recharla, N.; Geesala, R.; Shi, X.-Z. Gut Microbial Metabolite Butyrate and Its Therapeutic Role in Inflammatory Bowel Disease: A Literature Review. Nutrients 2023, 15, 2275. [Google Scholar] [CrossRef] [PubMed]
- Eshleman, E.M.; Rice, T.; Potter, C.; Waddell, A.; Hashimoto-Hill, S.; Woo, V.; Field, S.; Engleman, L.; Lim, H.-W.; Schumacher, M.A.; et al. Microbiota-Derived Butyrate Restricts Tuft Cell Differentiation via Histone Deacetylase 3 to Modulate Intestinal Type 2 Immunity. Immunity 2024, 57, 319–332.e6. [Google Scholar] [CrossRef]
- Chen, F.; Li, Q.; Chen, Y.; Wei, Y.; Liang, J.; Song, Y.; Shi, L.; Wang, J.; Mao, L.; Zhang, B.; et al. Association of the Gut Microbiota and Fecal Short-Chain Fatty Acids with Skeletal Muscle Mass and Strength in Children. FASEB J. 2022, 36, e22109. [Google Scholar] [CrossRef]
- Lv, W.-Q.; Lin, X.; Shen, H.; Liu, H.-M.; Qiu, X.; Li, B.-Y.; Shen, W.-D.; Ge, C.-L.; Lv, F.-Y.; Shen, J.; et al. Human Gut Microbiome Impacts Skeletal Muscle Mass via Gut Microbial Synthesis of the Short-Chain Fatty Acid Butyrate among Healthy Menopausal Women. J. Cachexia Sarcopenia Muscle 2021, 12, 1860–1870. [Google Scholar] [CrossRef]
- Liu, C.; Wong, P.Y.; Wang, Q.; Wong, H.Y.; Huang, T.; Cui, C.; Zhang, N.; Cheung, W.H.; Wong, R.M.Y. Short-chain Fatty Acids Enhance Muscle Mass and Function through the Activation of mTOR Signalling Pathways in Sarcopenic Mice. J. Cachexia Sarcopenia Muscle 2024, 15, 2387–2401. [Google Scholar] [CrossRef]
- Tang, G.; Du, Y.; Guan, H.; Jia, J.; Zhu, N.; Shi, Y.; Rong, S.; Yuan, W. Butyrate Ameliorates Skeletal Muscle Atrophy in Diabetic Nephropathy by Enhancing Gut Barrier Function and FFA2-Mediated PI3K/Akt/mTOR Signals. Br. J. Pharmacol. 2022, 179, 159–178. [Google Scholar] [CrossRef]
- Liu, H.; Xi, Q.; Tan, S.; Qu, Y.; Meng, Q.; Zhang, Y.; Cheng, Y.; Wu, G. The Metabolite Butyrate Produced by Gut Microbiota Inhibits Cachexia-Associated Skeletal Muscle Atrophy by Regulating Intestinal Barrier Function and Macrophage Polarization. Int. Immunopharmacol. 2023, 124, 111001. [Google Scholar] [CrossRef]
- Kobayashi, S.; Morino, K.; Okamoto, T.; Tanaka, M.; Ida, S.; Ohashi, N.; Murata, K.; Yanagimachi, T.; Sakai, J.; Maegawa, H.; et al. Acetate Derived from the Intestinal Tract Has a Critical Role in Maintaining Skeletal Muscle Mass and Strength in Mice. Physiol. Rep. 2024, 12, e16047. [Google Scholar] [CrossRef]
- Ismaeel, A.; Valentino, T.R.; Burke, B.; Goh, J.; Saliu, T.P.; Albathi, F.; Owen, A.; McCarthy, J.J.; Wen, Y. Acetate and Succinate Benefit Host Muscle Energetics as Exercise-Associated Post-Biotics. Physiol. Rep. 2023, 11, e15848. [Google Scholar] [CrossRef]
- Lagerwaard, B.; van der Hoek, M.D.; Hoeks, J.; Grevendonk, L.; Nieuwenhuizen, A.G.; Keijer, J.; de Boer, V.C.J. Propionate Hampers Differentiation and Modifies Histone Propionylation and Acetylation in Skeletal Muscle Cells. Mech. Ageing Dev. 2021, 196, 111495. [Google Scholar] [CrossRef] [PubMed]
- Olaniyi, K.S.; Areloegbe, S.E. Acetate Circumvents Impaired Metabolic Switch in Skeletal Muscle of Letrozole-Induced PCOS Rat Model by Suppression of PDK4/NLRP3. Nutrition 2023, 107, 111914. [Google Scholar] [CrossRef] [PubMed]
- Maruta, H.; Yoshimura, Y.; Araki, A.; Kimoto, M.; Takahashi, Y.; Yamashita, H. Activation of AMP-Activated Protein Kinase and Stimulation of Energy Metabolism by Acetic Acid in L6 Myotube Cells. PLoS ONE 2016, 11, e0158055. [Google Scholar] [CrossRef] [PubMed]
- Gao, Z.; Yin, J.; Zhang, J.; Ward, R.E.; Martin, R.J.; Lefevre, M.; Cefalu, W.T.; Ye, J. Butyrate Improves Insulin Sensitivity and Increases Energy Expenditure in Mice. Diabetes 2009, 58, 1509–1517. [Google Scholar] [CrossRef]
- Rios-Morales, M.; Vieira-Lara, M.A.; Homan, E.; Langelaar-Makkinje, M.; Gerding, A.; Li, Z.; Huijkman, N.; Rensen, P.C.N.; Wolters, J.C.; Reijngoud, D.-J.; et al. Butyrate Oxidation Attenuates the Butyrate-Induced Improvement of Insulin Sensitivity in Myotubes. Biochim. Biophys. Acta Mol. Basis Dis. 2022, 1868, 166476. [Google Scholar] [CrossRef]
- Han, J.-H.; Kim, I.-S.; Jung, S.-H.; Lee, S.-G.; Son, H.-Y.; Myung, C.-S. The Effects of Propionate and Valerate on Insulin Responsiveness for Glucose Uptake in 3T3-L1 Adipocytes and C2C12 Myotubes via G Protein-Coupled Receptor 41. PLoS ONE 2014, 9, e95268. [Google Scholar] [CrossRef]
- Otten, B.M.J.; Sthijns, M.M.J.P.E.; Troost, F.J. A Combination of Acetate, Propionate, and Butyrate Increases Glucose Uptake in C2C12 Myotubes. Nutrients 2023, 15, 946. [Google Scholar] [CrossRef]
- Yamashita, H.; Maruta, H.; Jozuka, M.; Kimura, R.; Iwabuchi, H.; Yamato, M.; Saito, T.; Fujisawa, K.; Takahashi, Y.; Kimoto, M.; et al. Effects of Acetate on Lipid Metabolism in Muscles and Adipose Tissues of Type 2 Diabetic Otsuka Long-Evans Tokushima Fatty (OLETF) Rats. Biosci. Biotechnol. Biochem. 2009, 73, 570–576. [Google Scholar] [CrossRef]
- Van, K.; Burns, J.L.; Monk, J.M. Effect of Short-Chain Fatty Acids on Inflammatory and Metabolic Function in an Obese Skeletal Muscle Cell Culture Model. Nutrients 2024, 16, 500. [Google Scholar] [CrossRef]
- Kasiak, P.; Kowalski, T.; Rębiś, K.; Klusiewicz, A.; Ładyga, M.; Sadowska, D.; Wilk, A.; Wiecha, S.; Barylski, M.; Poliwczak, A.R.; et al. Is the Ventilatory Efficiency in Endurance Athletes Different?-Findings from the NOODLE Study. J. Clin. Med. 2024, 13, 490. [Google Scholar] [CrossRef]
| SCFAs | Major Fiber Sources | Key Producing Bacteria | Principal Biological Effects | References |
|---|---|---|---|---|
| Acetate | Resistant starch, inulin, pectin, arabinoxylan, cellulose, fructooligosaccharides (FOS) | Bifidobacterium; Bacteroides; Prevotella; Ruminococcus | Systemic energy metabolism; enhances lipid synthesis; appetite regulation via gut–brain axis; supports mucosal immunity and barrier integrity. | [15,16] |
| Propionate | Resistant starch, arabinoxylan, oat bran, beta-glucan, guar gum, pectin | Bacteroides; Prevotella; Veillonella; Roseburia; Dialister; Akkermansia muciniphila | Regulates hepatic gluconeogenesis; modulates lipid metabolism and cholesterol reduction; induces satiety; anti-inflammatory properties. | [16,17,18] |
| Butyrate | Resistant starch, inulin, pectin, psyllium husk, wheat bran, FOS | Faecalibacterium prausnitzii, Roseburia; Eubacterium rectale; Anaerostipes; Clostridium butyricum | Primary energy source for colonocytes; enhances gut barrier function and integrity; anti-inflammatory and immunomodulatory effects; inhibits colorectal cancer cell growth. | [16,19,20] |
| Objective | Methodology | Main Findings | Implications | References |
|---|---|---|---|---|
| Assess acetate’s effect on muscle development in germ-free mice | Acetate supplementation in germ-free mice | Improved body weight, SDH activity, and expression of myogenic factors | Acetate mitigates microbiota depletion effects on muscle development | [14] |
| Examine propionate’s effect on metabolic health in overweight adults | Inulin–propionate ester supplementation in a crossover trial | Improved insulin sensitivity, reduced inflammation | Propionate beneficial for metabolic improvements via SCFA pathway | [26] |
| Investigate SCFA levels and muscle mass in children | Fecal SCFA measurement and body composition analysis | Higher SCFA levels correlated with greater muscle mass and better muscle-to-fat ratio | SCFAs may support skeletal muscle quality in children | [34] |
| Examine butyrate and muscle mass in menopausal women | Cross-sectional correlation study using serum butyrate and SMI | Serum butyrate is positively associated with skeletal muscle index (SMI) | Butyrate supports muscle preservation in aging populations. | [35] |
| Evaluate SCFA effects in a sarcopenia mouse model | 3-month treatment with SCFA cocktail in SAMP8 mice. | Increased CSA and strength, reduced fatigue. | SCFA supplementation improves muscle mass and endurance | [36] |
| Assess butyrate effects in diabetic nephropathy mice | Dietary butyrate intervention with muscle histology and function | Reduced autophagy markers and improved antioxidant defenses | Butyrate protects muscle via anti-autophagy and anti-oxidative mechanisms | [37] |
| Test butyrate in cachexia-induced muscle loss | Butyrate treatment in tumor-bearing mice | Decreased weight loss, improved strength, and anti-inflammatory response | Butyrate attenuates cachexia and improves muscle inflammation | [38] |
| Evaluate acetate’s role in skeletal muscle maintenance | Acetate supplementation and genetic knockout model | Improved CSA and strength; knockout mice showed reduced muscle mass | Acetate is essential for muscle mass and strength maintenance | [39] |
| Investigate acetate and succinate effects during muscle hypertrophy | Mechanical overload-induced hypertrophy in mice with acetate treatment | Enhanced mitochondrial respiration after 5 days | Acetate supports energetics during muscle hypertrophy | [40] |
| Explore propionate’s effect on myogenesis | In vitro C2C12 differentiation assay | Propionate impaired myogenic differentiation via histone modification | Not all SCFAs are beneficial; propionate may inhibit muscle development | [41] |
| Explore acetate’s role in a PCOS model affecting muscle | Acetate gavage in PCOS rat model | Improved glucose metabolism, decreased inflammation and oxidative stress | Acetate restores metabolic function in skeletal muscle under PCOS | [42] |
| Study acetic acid’s effect on AMPK activation in muscle cells | L6 myotube cells treated with acetic acid | Activated AMPK, increased glucose and FA uptake, reduced TG | Acetic acid boosts energy metabolism and reduces lipid toxicity | [43] |
| Assess butyrate’s impact on insulin sensitivity and energy expenditure | Butyrate incorporated into high-fat diet in mice | Prevented obesity and insulin resistance, increased PGC-1α | Butyrate supports metabolic health via enhanced mitochondrial function | [44] |
| Assess butyrate effects on insulin sensitivity | C2C12 myotube cultures treated with butyrate | Enhanced insulin sensitivity and glycolysis via HDAC inhibition | Butyrate improves insulin action in skeletal muscle cells | [45] |
| Determine SCFAs’ effect on glucose uptake in muscle cells | C2C12 myotubes treated with propionate and valerate | Increased insulin-stimulated glucose uptake via GPR41 | SCFAs enhance glucose handling in skeletal muscle cells | [46] |
| Investigate whether SCFAs increase glucose uptake by upregulating GSH in C2C12 myotubes. | C2C12 myotubes treated with single or combined SCFAs (1, 5, 20 mM) for 24 h; glucose uptake, cytotoxicity, and GSH levels measured. | 5 mM SCFA mixture increased glucose uptake; 20 mM propionate, butyrate, and mixtures reduced glucose uptake; all SCFAs increased GSH levels, but GSH increase not linked to glucose uptake; SCFAs did not prevent menadione-induced glucose uptake decrease. | Physiological levels of SCFAs can improve glucose uptake in muscle cells; however, this effect is not mediated through GSH-related antioxidant mechanisms | [47] |
| Explore acetate’s effect on metabolism in diabetic rats | Long-term acetate administration in OLETF rats | Increased GLUT4 and myoglobin expression, improved glucose homeostasis | Acetate improves muscle insulin sensitivity in diabetic models | [48] |
| Evaluate SCFAs on inflammation in muscle cells | Obese muscle cell model with SCFA treatments | SCFAs reduced pro-inflammatory cytokines in a dose-dependent manner | SCFAs modulate muscle inflammation under obese conditions | [49] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, X.; Xu, M.; Wang, H.; Zhu, L. Role and Mechanism of Short-Chain Fatty Acids in Skeletal Muscle Homeostasis and Exercise Performance. Nutrients 2025, 17, 1463. https://doi.org/10.3390/nu17091463
Liu X, Xu M, Wang H, Zhu L. Role and Mechanism of Short-Chain Fatty Acids in Skeletal Muscle Homeostasis and Exercise Performance. Nutrients. 2025; 17(9):1463. https://doi.org/10.3390/nu17091463
Chicago/Turabian StyleLiu, Xiaoguang, Miaomiao Xu, Huiguo Wang, and Lin Zhu. 2025. "Role and Mechanism of Short-Chain Fatty Acids in Skeletal Muscle Homeostasis and Exercise Performance" Nutrients 17, no. 9: 1463. https://doi.org/10.3390/nu17091463
APA StyleLiu, X., Xu, M., Wang, H., & Zhu, L. (2025). Role and Mechanism of Short-Chain Fatty Acids in Skeletal Muscle Homeostasis and Exercise Performance. Nutrients, 17(9), 1463. https://doi.org/10.3390/nu17091463








