Diagnostic Agreement for High-Grade Urothelial Cell Carcinoma in Atypical Urine Cytology: A Nationwide Survey Reveals a Tendency for Overestimation in Specimens with an N/C Ratio Approaching 0.5
Abstract
:1. Introduction
2. Results
2.1. Overall Agreement
2.2. Interobserver Concordance
2.3. Accuracy of N/C Ratio Assessment
3. Discussion
4. Materials and Methods
Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rosenthal, D.L.; Wojcik, E.M.; Kurtycz, D.F.I. The Paris System for Reporting Urinary Cytology; Springer: New York, NY, USA, 2015. [Google Scholar]
- Cowan, M.L.; Rosenthal, D.L.; VandenBussche, C.J. Improved risk stratification for patients with high-grade urothelial carcinoma following application of the Paris system for reporting urinary cytology. Cancer 2017, 125, 427–434. [Google Scholar] [CrossRef] [Green Version]
- Hassan, M.; Solanki, S.; Kassouf, W.; Kanber, Y.; Caglar, D.; Auger, M.; Brimo, F. Impact of implementing the paris system for reporting urine cytology in the performance of urine cytology: A correlative study of 124 cases. Am. J. Clin. Pathol. 2016, 146, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Northrup, V.; Acar, B.C.; Hossain, M.; Acker, M.R.; Manuel, E.; Rahmeh, T. Clinical follow up and the impact of the Paris system in the assessment of patients with atypical urine cytology. Diagn. Cytopathol. 2018, 46, 1022–1030. [Google Scholar] [CrossRef] [PubMed]
- Malviya, K.; Fernandes, G.; Naik, L.; Kothari, K.; Agnihotri, M. Utility of the Paris system in reporting urine cytology. Acta Cytol. 2017, 61, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Torous, V.F.; Brancely, D.; VanderLaan, P.A. Implementation of the paris system for reporting urinary cytology results in lower atypical diagnostic rates. J. Am. Soc. Cytopathol. 2017, 6, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Meilleroux, J.; Daniel, G.; Aziza, J.; d’Aure, D.M.; Quintyn-Ranty, M.L.; Basset, C.M.; Evrard, S.M.; Courtade-Saidi, M.M. One year of experience using the Paris system for reporting urinary cytology. Cancer Cytopathol. 2018, 126, 430–436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Granados, R.; Duarte, J.A.; Corrales, T.; Camarmo, E.; Bajo, P. Applying the Paris system for reporting urine cytology increases the rate of atypical urothelial cells in benign cases: A need for patient management recommendations. Acta Cytol. 2017, 61, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Long, T.; Layfield, L.J.; Esebua, M.; Frazier, S.R.; Giorgadze, D.T.; Schmidt, R.L. Interobserver reproducibility of the paris system for reporting urinary cytology. Cytojournal 2017, 14, 17. [Google Scholar] [CrossRef]
- Kurtycz, D.F.I.; Barkan, G.A.; Pavelec, D.M.; Rosenthal, D.L.; Wojcik, E.M.; VandenBussche, C.J.; Mangiulli, K.; Olson, M.T. Paris interobserver reproducibility study (PIRST). J. Am. Soc. Cytopathol. 2018, 7, 174–184. [Google Scholar] [CrossRef]
- Stanzione, N.; Ahmed, T.; Fung, P.C.; Cai, D.; Lu, D.Y.; Sumida, L.C.; Moatamed, M.D.N. The continual impact of the Paris system on urine cytology, a three year experience. Cytopathology 2020, 31, 35–40. [Google Scholar] [CrossRef]
- Mokhtar, G.A.; Al-Dousari, M.; Al-Ghamedi, D. Diagnostic significance of atypical category in the voided urine samples: A retrospective study in a tertiary care center. Urol. Ann. 2010, 2, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, V.; McKee, G.T. Analysis of atypical urine cytology in a tertiary care center. Cancer 2005, 105, 468–475. [Google Scholar] [CrossRef] [PubMed]
- VandenBussche, C.J.; Sathiyamoorthy, S.; Owens, C.L.; Burroughs, F.H.; Rosenthal, D.L.; Guan, H. The Johns Hopkins hospital template for urologic cytology samples: Parts ii and iii: Improving the predictability of indeterminate results in urinary cytologic samples: An outcomes and cytomorphologic study. Cancer Cytopathol. 2013, 121, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Pierconti, F.; Martini, M.; Straccia, P.; Fiorentino, V.; Musarra, T.; Larocca, L.M.; Lopez-Beltran, A. Hypochromatic large urothelial cells in urine cytology are indicative of high grade urothelial carcinoma. APMIS 2018, 126, 705–709. [Google Scholar] [CrossRef] [PubMed]
- Glass, R.; Rosen, L.; Chau, K.; Sheikh-Fayyaz, S.; Farmer, P.; Coutsouvelis, C.; Slim, F.; Brenkert, R.; Das, K.; Raab, S.; et al. Analysis of the cytomorphological features in atypical urine specimens following application of the paris system for reporting urinary cytology. Acta Cytol. 2018, 62, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Hang, J.F.; Charu, V.; Zhang, M.L.; VandenBussche, C.J. Digital image analysis supports a nuclear-to-cytoplasmic ratio cutoff value of 0.5 for atypical urothelial cells. Cancer Cytopathol. 2017, 125, 710–716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, M.L.; Guo, A.X.; VandenBussche, C.J. Morphologists overestimate the nuclear-to-cytoplasmic ratio. Cancer Cytopathol. 2016, 124, 669–677. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Layfield, L.J.; Esebua, M.; Frazier, S.R.; Hammer, R.D.; Bivin, W.W.; Nguyen, V.; Ersoy, I.; Schmidt, R.L. Accuracy and reproducibility of nuclear/cytoplasmic ratio assessments in urinary cytology specimens. Diagn. Cytopathol. 2017, 45, 107–112. [Google Scholar] [CrossRef]
- Gisev, N.; Bell, J.S.; Chen, T.F. Interrater agreement and interrater reliability: Key concepts, approaches, and applications. Res. Soc. Adm. Pharm. 2013, 9, 330–338. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [Green Version]
- Fleiss, J.L.; Levin, B.; Paik, M.C. Statistical Methods for Rates and Proportions; John Wiley & Sons: Hoboken, NJ, USA, 2003. [Google Scholar]
- Sim, J.; Wright, C.C. The kappa statistic in reliability studies: Use, interpretation, and sample size requirements. Phys. Ther. 2005, 85, 257–268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piaton, E.; Advenier, A.S.; Carre, C.; Decaussin-Petrucci, M.; Mege-Lechevallier, F.; Hutin, K.; Nennig, C.; Colombel, M.; Ruffion, A. P16/ki-67 dual labeling and urinary cytology results according to the new paris system for reporting urinary cytology: Impact of extended follow-up. Cancer Cytopathol. 2017, 125, 552–562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Virk, R.K.; Abro, S.; de Ubago, J.M.M.; Pambuccian, S.E.; Quek, M.L.; Wojcik, E.M.; Mehrotra, S.; Chatt, G.U.; Barkan, G.A. The value of the UroVysion® fish assay in the risk-stratification of patients with “atypical urothelial cells” in urinary cytology specimens. Diagn. Cytopathol. 2017, 45, 481–500. [Google Scholar] [CrossRef] [PubMed]

| Profession (n = 137) | Number |
|---|---|
| Cytotechnologist | 91 |
| Cytopathologist | 46 |
| Years of Practice (n = 137) | |
| <5 years | 43 |
| 5–10 years | 32 |
| 10–20 years | 47 |
| >20 years | 15 |
| Types of practice (n = 137) | |
| Medical center | 48 |
| Regional/Local hospital | 68 |
| Central laboratory | 21 |
| Case | NC Ratio | Hyperchromasia | Nuclear Membrane Irregularity | Clumping Chromatin | Diagnosis |
|---|---|---|---|---|---|
| 1 | >0.7 75 (54.74%) | moderate to severe 69 (50.36%) | mild 100 (72.99%) | yes 105 (76.64%) | AUC/SHGUC * 47 (34.30%) |
| 2 | 0.5–0.7 94 (68.61%) | moderate to severe 98 (71.53%) | mild 70 (51.09%) | yes 122 (89.05%) | AUC 56 (40.88%) |
| 3 | >0.7 134 (97.81%) | Mild 64 (46.72%) | no 95 (69.34%) | yes 85 (62.04%) | SHGUC 57 (41.61%) |
| 4 | >0.7 129 (94.16%) | moderate to severe 83 (60.58%) | severe 78 (56.93%) | yes 126 (91.97%) | HGUC 79 (57.66%) |
| 5 | 0.5–0.7 109 (79.56%) | Mild 70 (51.09%) | mild 91 (66.42%) | yes 98 (71.53%) | AUC 78 (56.93%) |
| 6 | 0.5–0.7 72 (52.55%) | Mild 81 (59.12%) | mild 91 (66.42%) | no 89 (64.96%) | NHGUC 62 (45.26%) |
| 7 | <0.5 81 (59.12%) | No 75 (54.74%) | no 86 (62.77%) | no 95 (69.34%) | NHGUC 114 (83.21%) |
| 8 | >0.7 105 (76.64%) | moderate to severe 76 (55.47%) | mild 83 (60.58%) | yes 124 (90.51%) | SHGUC 58 (42.34%) |
| 9 | >0.7 103 (75.18%) | moderate to severe 99 (72.26%) | severe 67 (48.91%) | yes 133 (97.08%) | SHGUC 90 (65.69%) |
| 10 | 0.5–0.7 82 (59.85%) | moderate to severe 82 (59.85%) | mild 64 (46.72%) | yes 108 (8.83%) | AUC 61 (44.53%) |
| Case No. | N/C Ratio | Correct N/C Range (% of Correct Rate) | Most Favored Assessment of N/C Range (% of Response) |
|---|---|---|---|
| 3 | 0.84 | >0.7 (97.8%) | As left |
| 4 | 0.85 | >0.7 (94.2%) | As left |
| 8 | 0.79 | >0.7 (76.6%) | As left |
| 9 | 0.86 | >0.7 (75.2%) | As left |
| 2 | 0.54 | 0.5–0.7 (68.6%) | As left |
| 10 | 0.65 | 0.5–0.7 (59.9%) | As left |
| 7 | 0.43 | <0.5 (59.1%) | As left |
| 6 | 0.42 | <0.5 (46.7%) | 0.5–0.7 (52.6%) |
| 1 | 0.58 | 0.5–0.7 (43.8%) | >0.7 (54.7%) |
| 5 | 0.39 | <0.5 (14.6%) | 0.5–0.7 (79.6%) |
| Case No. | |
|---|---|
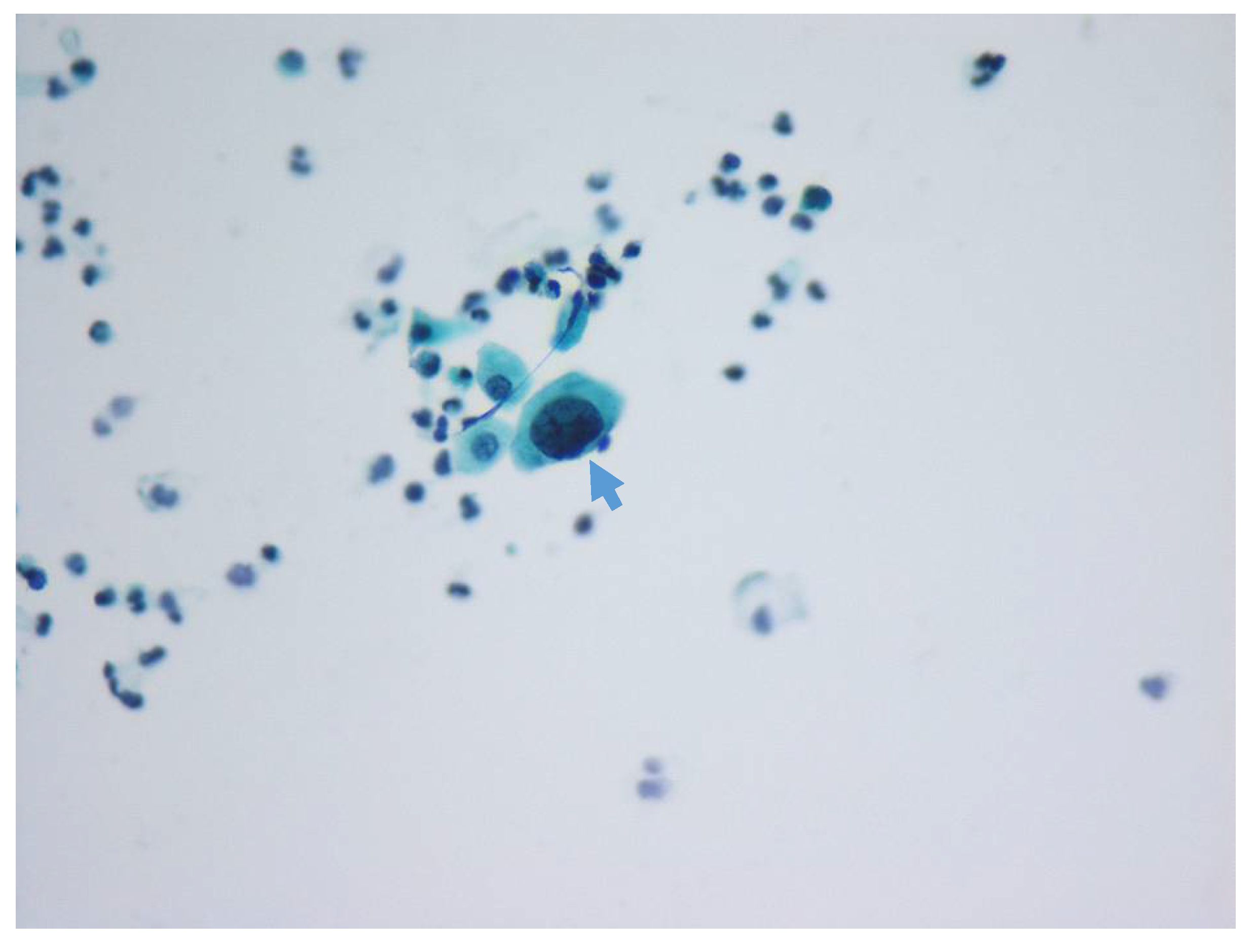
| 400× photo (including only one target cell) | |
| Range of N/C ratio? | Irregular nuclear membrane? |
| □ <0.5 | □ No |
| □ 0.5–0.7 | □ Yes, but minimal |
| □ >0.7 | □ Yes, prominent |
| Degrees of hyperchromasia? | Coarse/Clumping chromatin? |
| □ None | □ No |
| □ Mild | □ Yes |
| □ Moderate to severe | |
| 100× photo (including several cells in clusters or disperse) | |
| Your diagnosis? | |
| □ Negative for HGUC (NHGUC) | |
| □ Atypical urothelial cells (AUC) | |
| □ Suspicious for HGUC (SHGUC) | |
| □ HGUC | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.-H.; Hang, J.-F.; Wen, C.-H.; Liao, K.-C.; Lee, W.-Y.; Lai, C.-R. Diagnostic Agreement for High-Grade Urothelial Cell Carcinoma in Atypical Urine Cytology: A Nationwide Survey Reveals a Tendency for Overestimation in Specimens with an N/C Ratio Approaching 0.5. Cancers 2020, 12, 272. https://doi.org/10.3390/cancers12020272
Wang Y-H, Hang J-F, Wen C-H, Liao K-C, Lee W-Y, Lai C-R. Diagnostic Agreement for High-Grade Urothelial Cell Carcinoma in Atypical Urine Cytology: A Nationwide Survey Reveals a Tendency for Overestimation in Specimens with an N/C Ratio Approaching 0.5. Cancers. 2020; 12(2):272. https://doi.org/10.3390/cancers12020272
Chicago/Turabian StyleWang, Yeh-Han, Jen-Fan Hang, Chien-Hui Wen, Kuan-Cho Liao, Wen-Ying Lee, and Chiung-Ru Lai. 2020. "Diagnostic Agreement for High-Grade Urothelial Cell Carcinoma in Atypical Urine Cytology: A Nationwide Survey Reveals a Tendency for Overestimation in Specimens with an N/C Ratio Approaching 0.5" Cancers 12, no. 2: 272. https://doi.org/10.3390/cancers12020272
APA StyleWang, Y.-H., Hang, J.-F., Wen, C.-H., Liao, K.-C., Lee, W.-Y., & Lai, C.-R. (2020). Diagnostic Agreement for High-Grade Urothelial Cell Carcinoma in Atypical Urine Cytology: A Nationwide Survey Reveals a Tendency for Overestimation in Specimens with an N/C Ratio Approaching 0.5. Cancers, 12(2), 272. https://doi.org/10.3390/cancers12020272





