A Novel Role of Interleukin 13 Receptor alpha2 in Perineural Invasion and its Association with Poor Prognosis of Patients with Pancreatic Ductal Adenocarcinoma †
Abstract
1. Introduction
2. Results
2.1. Demographic and Clinicopathological Correlates of Tumor Samples at Presentation in Patients with PDAC
2.2. IHC Results of IL-13Rα2 Expression in PDAC Correlate with Pathologic Grade and Clinical Stage of PDAC
2.3. Expression of IL-13Rα2 mRNA by ISH in PDAC Correlates with Pathologic Grade and Clinical Stage
2.4. Heterogeneity in IL-13Rα2 Expression is Associated with Clinicopathological Attributes of PDAC
2.5. Association of IL-13Rα2 with Perineural Invasion
2.6. IL-13Rα2 is Associated with Overall Survival of PDAC Patients
2.7. Analysis of Clinicopathological Findings and Prognostic Factors by Multivariate Analysis
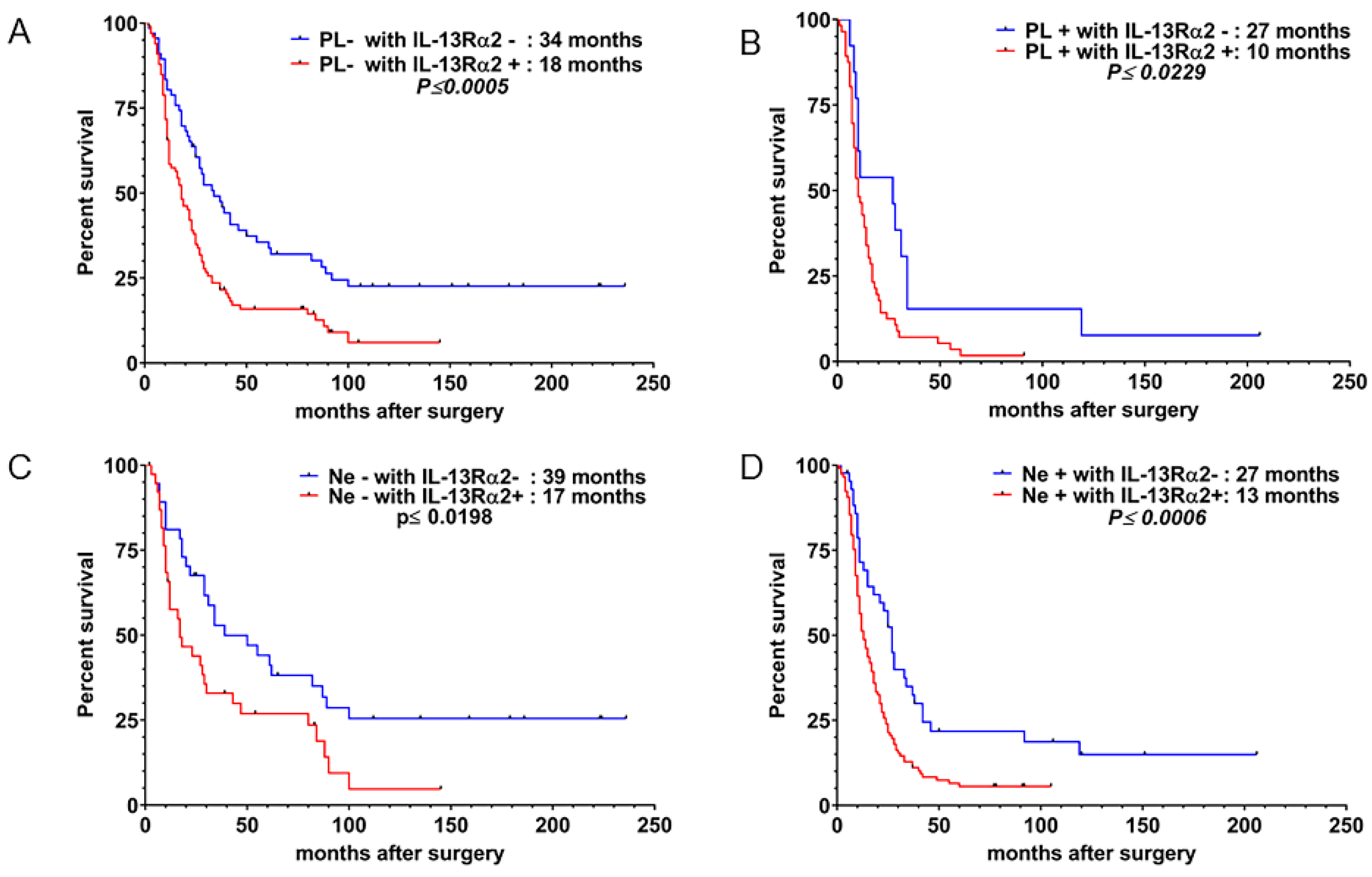
2.8. IL-13Rα2 in PNI is Postively Correlated with Decreased Survival in PDAC Patients
3. Discussion
4. Patients and Methods
4.1. Immunohistochemistry (IHC)
4.2. In Situ Hybridization Analysis (ISH)
4.3. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| IL-13Rα2 | Interleukin-13 Receptorα2 |
| UICC | Union Internationale Contre le Cancer |
| JPS | Japan Pancreas Society |
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Bramhall, S.R. Stromal degradation by the malignant epithelium in pancreatic cancer and the therapeutic potential of proteolytic inhibition. J. Hepatobiliary Pancreat. Surg. 1998, 5, 392–401. [Google Scholar] [CrossRef] [PubMed]
- Feig, C.; Gopinathan, A.; Neesse, A.; Chan, D.S.; Cook, N.; Tuveson, D.A. The pancreas cancer microenvironment. Clin. Cancer Res. 2012, 18, 4266–4276. [Google Scholar] [CrossRef] [PubMed]
- Ozdemir, B.C.; Pentcheva-Hoang, T.; Carstens, J.L.; Zheng, X.; Wu, C.C.; Simpson, T.R.; Laklai, H.; Sugimoto, H.; Kahlert, C.; Novitskiy, S.V.; et al. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell 2014, 25, 719–734. [Google Scholar] [CrossRef]
- Badger, S.A.; Brant, J.L.; Jones, C.; McClements, J.; Loughrey, M.B.; Taylor, M.A.; Diamond, T.; McKie, L.D. The role of surgery for pancreatic cancer: A 12-year review of patient outcome. Ulst. Med. J. 2010, 79, 70–75. [Google Scholar]
- Chen, J.W.; Bhandari, M.; Astill, D.S.; Wilson, T.G.; Kow, L.; Brooke-Smith, M.; Toouli, J.; Padbury, R.T. Predicting patient survival after pancreaticoduodenectomy for malignancy: Histopathological criteria based on perineural infiltration and lymphovascular invasion. HPB (Oxford) 2010, 12, 101–108. [Google Scholar] [CrossRef]
- Bapat, A.A.; Hostetter, G.; Von Hoff, D.D.; Han, H. Perineural invasion and associated pain in pancreatic cancer. Nat. Rev. Cancer 2011, 11, 695–707. [Google Scholar] [CrossRef]
- Ceyhan, G.O.; Michalski, C.W.; Demir, I.E.; Muller, M.W.; Friess, H. Pancreatic pain. Best Pract. Res. Clin. Gastroenterol. 2008, 22, 31–44. [Google Scholar] [CrossRef]
- Di Mola, F.F.; di Sebastiano, P. Pain and pain generation in pancreatic cancer. Langenbeck’s Arch. Surg. 2008, 393, 919–922. [Google Scholar] [CrossRef]
- Zhu, Z.; Friess, H.; diMola, F.F.; Zimmermann, A.; Graber, H.U.; Korc, M.; Buchler, M.W. Nerve growth factor expression correlates with perineural invasion and pain in human pancreatic cancer. J. Clin. Oncol. 1999, 17, 2419–2428. [Google Scholar] [CrossRef]
- Schneider, M.B.; Standop, J.; Ulrich, A.; Wittel, U.; Friess, H.; Andren-Sandberg, A.; Pour, P.M. Expression of nerve growth factors in pancreatic neural tissue and pancreatic cancer. J. Histochem. Cytochem. 2001, 49, 1205–1210. [Google Scholar] [CrossRef] [PubMed]
- He, S.; Chen, C.H.; Chernichenko, N.; He, S.; Bakst, R.L.; Barajas, F.; Deborde, S.; Allen, P.J.; Vakiani, E.; Yu, Z.; et al. GFRalpha1 released by nerves enhances cancer cell perineural invasion through GDNF-RET signaling. Proc. Natl. Acad. Sci. USA 2014, 111, E2008–E2017. [Google Scholar] [CrossRef] [PubMed]
- Deng, H.; Zeng, J.; Zhang, T.; Gong, L.; Zhang, H.; Cheung, E.; Jones, C.; Li, G. Histone H3.3K27M mobilizes multiple Cancer/Testis (CT) antigens in pediatric glioma. Mol. Cancer Res. 2018, 16, 623–633. [Google Scholar] [CrossRef] [PubMed]
- Taguchi, A.; Taylor, A.D.; Rodriguez, J.; Celiktas, M.; Liu, H.; Ma, X.; Zhang, Q.; Wong, C.H.; Chin, A.; Girard, L.; et al. A search for novel cancer/testis antigens in lung cancer identifies VCX/Y genes, expanding the repertoire of potential immunotherapeutic targets. Cancer Res. 2014, 74, 4694–4705. [Google Scholar] [CrossRef] [PubMed]
- Joshi, B.H.; Hogaboam, C.; Dover, P.; Husain, S.R.; Puri, R.K. Role of interleukin-13 in cancer, pulmonary fibrosis, and other T(H)2-type diseases. Vitam. Horm. 2006, 74, 479–504. [Google Scholar] [CrossRef]
- Suzuki, A.; Leland, P.; Joshi, B.H.; Puri, R.K. Targeting of IL-4 and IL-13 receptors for cancer therapy. Cytokine 2015, 75, 79–88. [Google Scholar] [CrossRef]
- Joshi, B.H.; Kawakami, K.; Leland, P.; Puri, R.K. Heterogeneity in interleukin-13 receptor expression and subunit structure in squamous cell carcinoma of head and neck: Differential sensitivity to chimeric fusion proteins comprised of interleukin-13 and a mutated form of Pseudomonas exotoxin. Clin. Cancer Res. 2002, 8, 1948–1956. [Google Scholar]
- Joshi, B.H.; Puri, R.K. Optimization of expression and purification of two biologically active chimeric fusion proteins that consist of human interleukin-13 and Pseudomonas exotoxin in Escherichia coli. Protein Expr. Purif. 2005, 39, 189–198. [Google Scholar] [CrossRef]
- Murata, T.; Puri, R.K. Comparison of IL-13- and IL-4-induced signaling in EBV-immortalized human B cells. Cell. Immunol. 1997, 175, 33–40. [Google Scholar] [CrossRef]
- Zurawski, G.; de Vries, J.E. Interleukin 13, an interleukin 4-like cytokine that acts on monocytes and B cells, but not on T cells. Immunol. Today 1994, 15, 19–26. [Google Scholar] [CrossRef]
- Shimamura, T.; Fujisawa, T.; Husain, S.R.; Joshi, B.; Puri, R.K. Interleukin 13 mediates signal transduction through interleukin 13 receptor alpha2 in pancreatic ductal adenocarcinoma: Role of IL-13 Pseudomonas exotoxin in pancreatic cancer therapy. Clin. Cancer Res. 2010, 16, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, M.; Leland, P.; Kawakami, K.; Puri, R.K. Mutation and functional analysis of IL-13 receptors in human malignant glioma cells. Oncol. Res. 2001, 12, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Obiri, N.I.; Debinski, W.; Leonard, W.J.; Puri, R.K. Receptor for interleukin 13. Interaction with interleukin 4 by a mechanism that does not involve the common gamma chain shared by receptors for interleukins 2, 4, 7, 9, and 15. J. Biol. Chem. 1995, 270, 8797–8804. [Google Scholar] [CrossRef] [PubMed]
- Obiri, N.I.; Leland, P.; Murata, T.; Debinski, W.; Puri, R.K. The IL-13 receptor structure differs on various cell types and may share more than one component with IL-4 receptor. J. Immunol. 1997, 158, 756–764. [Google Scholar] [PubMed]
- Fichtner-Feigl, S.; Strober, W.; Kawakami, K.; Puri, R.K.; Kitani, A. IL-13 signaling through the IL-13alpha2 receptor is involved in induction of TGF-beta1 production and fibrosis. Nat. Med. 2006, 12, 99–106. [Google Scholar] [CrossRef]
- Fujisawa, T.; Joshi, B.H.; Puri, R.K. IL-13 regulates cancer invasion and metastasis through IL-13Ralpha2 via ERK/AP-1 pathway in mouse model of human ovarian cancer. Int. J. Cancer 2012, 131, 344–356. [Google Scholar] [CrossRef]
- Dey, P.; Li, J.; Zhang, J.; Chaurasiya, S.; Strom, A.; Wang, H.; Liao, W.T.; Cavallaro, F.; Denz, P.; Bernard, V.; et al. Oncogenic KRAS-driven metabolic reprogramming in pancreatic cancer cells utilizes cytokines from the tumor microenvironment. Cancer Discov. 2020, 10, 608–625. [Google Scholar] [CrossRef]
- Fujisawa, T.; Joshi, B.H.; Puri, R.K. Histone modification enhances the effectiveness of IL-13 receptor targeted immunotoxin in murine models of human pancreatic cancer. J. Transl. Med. 2011, 9, 37. [Google Scholar] [CrossRef]
- Fujisawa, T.; Joshi, B.; Nakajima, A.; Puri, R.K. A novel role of interleukin-13 receptor alpha2 in pancreatic cancer invasion and metastasis. Cancer Res. 2009, 69, 8678–8685. [Google Scholar] [CrossRef]
- Minn, A.J.; Gupta, G.P.; Siegel, P.M.; Bos, P.D.; Shu, W.; Giri, D.D.; Viale, A.; Olshen, A.B.; Gerald, W.L.; Massague, J. Genes that mediate breast cancer metastasis to lung. Nature 2005, 436, 518–524. [Google Scholar] [CrossRef]
- Ceyhan, G.O.; Bergmann, F.; Kadihasanoglu, M.; Altintas, B.; Demir, I.E.; Hinz, U.; Muller, M.W.; Giese, T.; Buchler, M.W.; Giese, N.A.; et al. Pancreatic neuropathy and neuropathic pain--a comprehensive pathomorphological study of 546 cases. Gastroenterology 2009, 136, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Ceyhan, G.O.; Liebl, F.; Maak, M.; Schuster, T.; Becker, K.; Langer, R.; Demir, I.E.; Hartel, M.; Friess, H.; Rosenberg, R. The severity of neural invasion is a crucial prognostic factor in rectal cancer independent of neoadjuvant radiochemotherapy. Ann. Surg. 2010, 252, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Demir, I.E.; Ceyhan, G.O.; Rauch, U.; Altintas, B.; Klotz, M.; Muller, M.W.; Buchler, M.W.; Friess, H.; Schafer, K.H. The microenvironment in chronic pancreatitis and pancreatic cancer induces neuronal plasticity. Neurogastroenterol. Motil. 2010, 22, 480–490. [Google Scholar] [CrossRef] [PubMed]
- Tieftrunk, E.; Demir, I.E.; Friess, H.; Ceyhan, G.O. Back pain as a potential indicator of local recurrence in pancreatic cancer. J. Surg. Case Rep. 2015, 2015. [Google Scholar] [CrossRef][Green Version]
- Liang, D.; Shi, S.; Xu, J.; Zhang, B.; Qin, Y.; Ji, S.; Xu, W.; Liu, J.; Liu, L.; Liu, C.; et al. New insights into perineural invasion of pancreatic cancer: More than pain. Biochim. Biophys. Acta 2016, 1865, 111–122. [Google Scholar] [CrossRef]
- Sobin, L.H.; Greene, F.L. Global TNM advisory group. Cancer 2004, 100, 1106. [Google Scholar] [CrossRef]
- Joshi, B.H.; Puri, R.A.; Leland, P.; Varricchio, F.; Gupta, G.; Kocak, M.; Gilbertson, R.J.; Puri, R.K.; Consortium, U.S.P.B.T. Identification of interleukin-13 receptor alpha2 chain overexpression in situ in high-grade diffusely infiltrative pediatric brainstem glioma. Neuro-Oncol. 2008, 10, 265–274. [Google Scholar] [CrossRef]
- Agresti, A.; Min, Y. Unconditional small-sample confidence intervals for the odds ratio. Biostatistics 2002, 3, 379–386. [Google Scholar] [CrossRef]
- Corcoran, C.; Mehta, C.R. Exact level and power of permutation, bootstrap and asymptotic tests of trend. J. Mod. Appl. Stat. Methods 2002, 1, 42–51. [Google Scholar] [CrossRef]
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression, 2nd ed.; John Wiley and Sons, Inc.: Hoboken, NJ, USA, 2000. [Google Scholar]



| Parameter | Number (% of the Total) |
|---|---|
| Sex | |
| Male | 148 (63) |
| Female | 88 (37) |
| Median age | 65.3 ± 5 |
| Tumor Location | |
| Head | 161 (68) |
| Body & Tail | 75 (32) |
| Clinical Stage (Union Internationale Contre le Cancer—UICC) | |
| I | 28 (12) |
| II | 89 (38) |
| III | 85 (36) |
| IV | 34 (14) |
| Pathologic Findings | |
| Well differentiated | 80 (34.5) |
| Moderately differentiated | 131 (55.5) |
| Poorly differentiated | 25 (10.5) |
| Diabetes (before surgery) | 77 (33) |
| Carbohydrate associated antigen (CA 19-9, U/mL) | 1037 ± 202 |
| Pathological Findings | Comparison | Number (of Patients) | Median Survival (Months) | p-Value |
|---|---|---|---|---|
| Differentiation | Well: mod-poor | 081:155 | 21:17 | 0.0005 |
| Invasion | ||||
| …to bile duct (CH) | −ve: +ve | 133: 103 | 20:16 | 0.027 |
| …to duodenum (DU) | −ve: +ve | 163: 073 | 21:13 | 0.005 |
| …to front constructs of pancreas (S) | −ve: +ve | 127: 109 | 22:14 | 0.001 |
| …to back constructs of pancreas (RP) | −ve: +ve | 078: 158 | 29:15 | ≤0.001 |
| …to portal vein (PV) | −ve: +ve | 172: 064 | 22:11 | ≤0.001 |
| …to artery (A) | −ve: + ve | 222: 014 | 19:09 | 0.003 |
| …to peripancreatic neuroplexus (PL) | −ve: + ve | 167: 069 | 23:11 | ≤0.001 |
| …to the other organs (OO) | −ve: + ve | 223: 013 | 18:12 | 0.011 |
| …to lymph duct in the pancreas (Ly) | ≤1: ≥1 | 162:074 | 22:12 | ≤0.001 |
| …to vein in the pancreas (V) | ≤1: ≥1 | 095: 141 | 27:14 | 0.002 |
| …to nerve in the pancreas (Ne) | ≤1: ≥1 | 076: 160 | 29:15 | ≤0.001 |
| …to main pancreatic duct (Mpd) | −ve: + ve | 124:112 | 21:16 | 0.317 |
| Pathologic Type | Patients with IHC Staining for IL-13Rα2 | ||||
|---|---|---|---|---|---|
| Positive (≥1+) | MST (months) | Negative (≤1+) | MST (months) | ||
| PL | Positive | 56 (36%) * | 10 | 13 (16%) | 27 |
| Negative | 100 (64%) | 18 | 67 (84%) | 34 | |
| Ne | Positive | 117 (75%) * | 13 | 43 (54%) | 27 |
| Negative | 39 (25%) | 17 | 37 (46%) | 29 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fujisawa, T.; Shimamura, T.; Goto, K.; Nakagawa, R.; Muroyama, R.; Ino, Y.; Horiuchi, H.; Endo, I.; Maeda, S.; Harihara, Y.; et al. A Novel Role of Interleukin 13 Receptor alpha2 in Perineural Invasion and its Association with Poor Prognosis of Patients with Pancreatic Ductal Adenocarcinoma. Cancers 2020, 12, 1294. https://doi.org/10.3390/cancers12051294
Fujisawa T, Shimamura T, Goto K, Nakagawa R, Muroyama R, Ino Y, Horiuchi H, Endo I, Maeda S, Harihara Y, et al. A Novel Role of Interleukin 13 Receptor alpha2 in Perineural Invasion and its Association with Poor Prognosis of Patients with Pancreatic Ductal Adenocarcinoma. Cancers. 2020; 12(5):1294. https://doi.org/10.3390/cancers12051294
Chicago/Turabian StyleFujisawa, Toshio, Takeshi Shimamura, Kaku Goto, Ryo Nakagawa, Ryosuke Muroyama, Yoshinori Ino, Hajime Horiuchi, Itaru Endo, Shin Maeda, Yasushi Harihara, and et al. 2020. "A Novel Role of Interleukin 13 Receptor alpha2 in Perineural Invasion and its Association with Poor Prognosis of Patients with Pancreatic Ductal Adenocarcinoma" Cancers 12, no. 5: 1294. https://doi.org/10.3390/cancers12051294
APA StyleFujisawa, T., Shimamura, T., Goto, K., Nakagawa, R., Muroyama, R., Ino, Y., Horiuchi, H., Endo, I., Maeda, S., Harihara, Y., Nakajima, A., Matsuhashi, N., Kato, N., Isayama, H., Puri, A., Suzuki, A., Bellayr, I., Leland, P., Joshi, B. H., & Puri, R. K. (2020). A Novel Role of Interleukin 13 Receptor alpha2 in Perineural Invasion and its Association with Poor Prognosis of Patients with Pancreatic Ductal Adenocarcinoma. Cancers, 12(5), 1294. https://doi.org/10.3390/cancers12051294








