Long-Term Dynamic Changes in Cosmetic Outcomes and Patient Satisfaction after Implant-Based Postmastectomy Breast Reconstruction and Contralateral Mastopexy with or without an Ultrapro Mesh Sling Used for the Inner Bra Technique. A Retrospective Correlational Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Patients and Methods
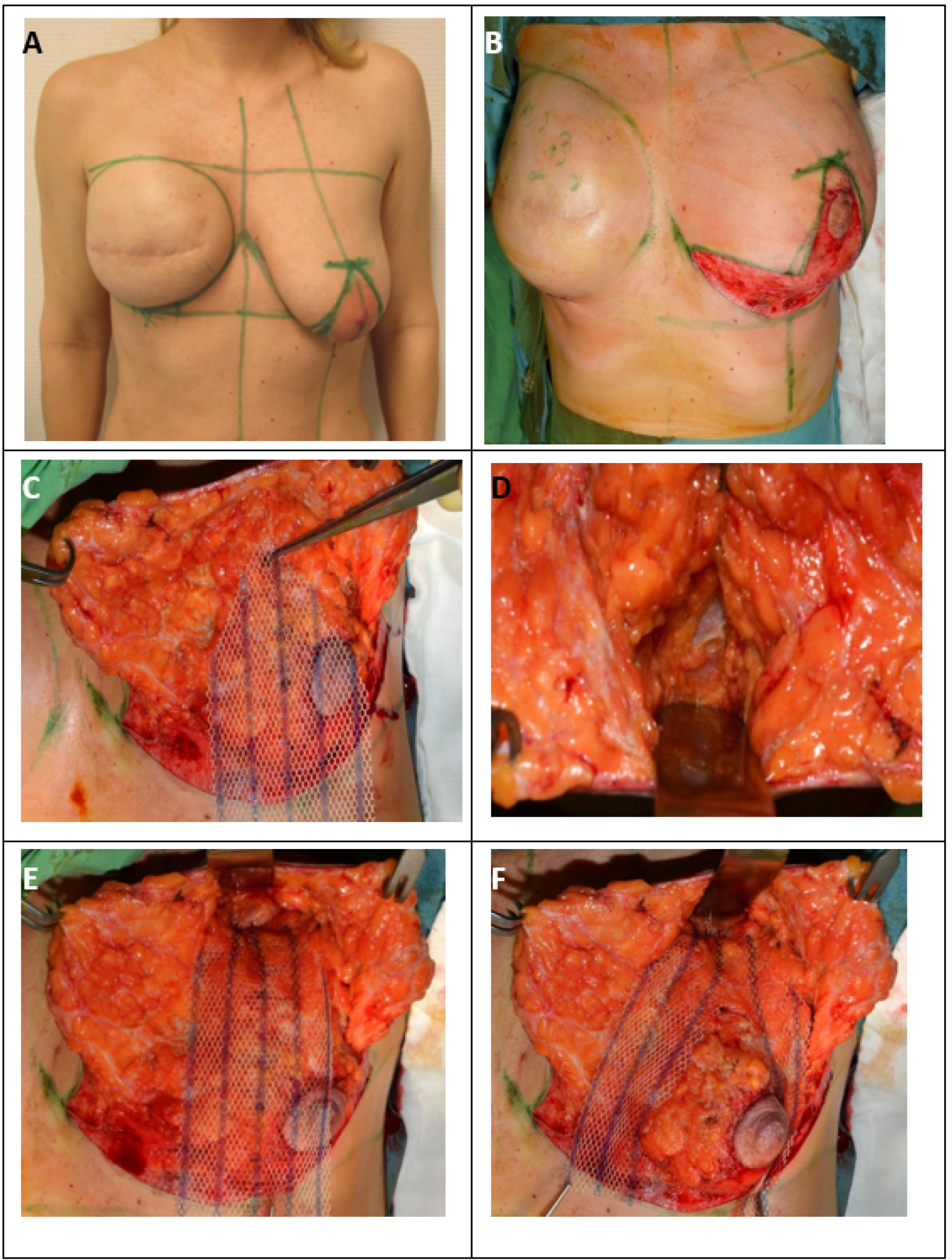
Surgical Therapy for Inferior or Modified Central Pedicled Inverted-T Mastopexy with ULTRAPRO® Sling Mesh
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rowland, J.H.; Desmond, K.A.; Meyerowitz, B.E.; Belin, T.R.; Wyatt, G.E.; Ganz, P.A. Role of breast reconstructive surgery in physical and emotional outcomes among breast cancer survivors. J. Natl. Cancer Inst. 2000, 92, 1422–1429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, S.Y.; Shu, B.C.; Chang, Y.J. The effect of breast reconstruction surgery on body image among women after mastectomy: A meta-analysis. Breast Cancer Res. Treat. 2013, 137, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Dorogi, B.; Matrai, T.; Ujhelyi, M.; Kenessey, I.; Kelemen, P.; Savolt, A.; Huszar, O.; Ping, O.; Pukancsik, D.; Matrai, Z. Assessing the needs of Hungarian breast cancer patients for modern oncoplastic breast surgical treatment. Questionnaire study of 500 patients. Orvosi Hetilap 2020, 161, 1221–1228. [Google Scholar] [CrossRef] [PubMed]
- Egro, F.M.; Pinell-White, X.; Hart, A.M.; Losken, A. The use of reduction mammaplasty with breast conservation therapy: An analysis of timing and outcomes. Plastic Reconstr. Surg. 2015, 135, 963e–971e. [Google Scholar] [CrossRef]
- Deigni, O.A.; Baumann, D.P.; Adamson, K.A.; Garvey, P.B.; Selber, J.C.; Caudle, A.S.; Smith, B.D.; Hanson, S.E.; Robb, G.L.; Schaverien, M.V. Immediate Contralateral Mastopexy/Breast Reduction for Symmetry Can Be Performed Safely in Oncoplastic Breast-Conserving Surgery. Plast. Reconstr. Surg. 2020, 145, 1134–1142. [Google Scholar] [CrossRef]
- Rykala, J.; Szychta, P.; Kruk-Jeromin, J. Delayed two-stage breast reconstruction with implants: The authors’ recent experience. Can. J. Plast. Surg. 2011, 19, 88–92. [Google Scholar] [CrossRef]
- Sigalove, S.; Maxwell, G.P.; Sigalove, N.M.; Storm-Dickerson, T.L.; Pope, N.; Rice, J.; Gabriel, A. Prepectoral Implant-Based Breast Reconstruction: Rationale, Indications, and Preliminary Results. Plast. Reconstr. Surg. 2017, 139, 287–294. [Google Scholar] [CrossRef]
- Teoh, V.; Gui, G. Direct to implant breast reconstruction with biological acellular dermal matrices. Br. J. Hosp. Med. 2020, 81, 1–7. [Google Scholar] [CrossRef]
- Dorogi, B.; Ujhelyi, M.; Kenessey, I.; Ivady, G.; Matrai, Z. Clinicopathological correlations of areola-sparing mastectomies versus nipple-sparing mastectomies: Analysis of the oncological and cosmetic importance of the components of the nipple-areola complex. Breast J. 2020. [Google Scholar] [CrossRef]
- Leone, M.S.; Priano, V.; Franchelli, S.; Puggioni, V.; Merlo, D.F.; Mannucci, M.; Santi, P.L. Factors affecting symmetrization of the contralateral breast: A 7-year unilateral postmastectomy breast reconstruction experience. Aesthet. Plast. Surg. 2011, 35, 446–451. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA: Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Pozner, J.N.; White, J.B.; Newman, M.I. Use of porcine acellular dermal matrix in revisionary cosmetic breast augmentation. Aesthet. Surg. J. 2013, 33, 681–690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spring, M.A.; Hartmann, E.C.; Stevens, W.G. Strategies and Challenges in Simultaneous Augmentation Mastopexy. Clin. Plast. Surg. 2015, 42, 505–518. [Google Scholar] [CrossRef] [PubMed]
- Graf, R.; Ricardo Dall Oglio Tolazzi, A.; Balbinot, P.; Pazio, A.; Miguel Valente, P.; da Silva Freitas, R. Influence of the Pectoralis Major Muscle Sling in Chest Wall-Based Flap Suspension After Vertical Mammaplasty: Ten-Year Follow-Up. Aesthet. Surg. J. 2016, 36, 1113–1121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sivakumar, B.; Sadr, A.H.; Smith, R.; Mosahebi, A. The ‘criss-cross sling’ modification of the vertical scar mastopexy. J. Plast. Reconstr. Aesthet. Surg. JPRAS 2010, 63, e312–e314. [Google Scholar] [CrossRef] [PubMed]
- Colwell, A.S.; Breuing, K.H. Improving shape and symmetry in mastopexy with autologous or cadaveric dermal slings. Ann. Plast. Surg. 2008, 61, 138–142. [Google Scholar] [CrossRef]
- Macadam, S.A.; Lennox, P.A. Acellular dermal matrices: Use in reconstructive and aesthetic breast surgery. Can. J. Plast. Surg. 2012, 20, 75–89. [Google Scholar] [CrossRef] [Green Version]
- Dieterich, M.; Dieterich, H.; Timme, S.; Reimer, T.; Gerber, B.; Stubert, J. Using a titanium-coated polypropylene mesh (TiLOOP((R)) Bra) for implant-based breast reconstruction: Case report and histological analysis. Arch. Gynecol. Obstet. 2012, 286, 273–276. [Google Scholar] [CrossRef]
- Dieterich, M.; Stubert, J.; Gerber, B.; Reimer, T.; Richter, D.U. Biocompatibility, cell growth and clinical relevance of synthetic meshes and biological matrixes for internal support in implant-based breast reconstruction. Arch. Gynecol. Obstet. 2015, 291, 1371–1379. [Google Scholar] [CrossRef]
- Pompei, S.; Evangelidou, D.; Arelli, F.; Ferrante, G. The Use of TIGR Matrix in Breast Aesthetic and Reconstructive Surgery: Is a Resorbable Synthetic Mesh a Viable Alternative to Acellular Dermal Matrices? Clin. Plast. Surg. 2018, 45, 65–73. [Google Scholar] [CrossRef]
- Klosterhalfen, B.; Junge, K.; Klinge, U. The lightweight and large porous mesh concept for hernia repair. Exp. Rev. Med. Dev. 2005, 2, 103–117. [Google Scholar] [CrossRef] [PubMed]
- Senkus, E.; Kyriakides, S.; Ohno, S.; Penault-Llorca, F.; Poortmans, P.; Rutgers, E.; Zackrisson, S.; Cardoso, F.; Committee, E.G. Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2015, 26, v8–v30. [Google Scholar] [CrossRef] [PubMed]
- Regnault, P. Breast ptosis. Definition and treatment. Clin. Plast. Surg. 1976, 3, 193–203. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibanes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef] [Green Version]
- Dikmans, R.E.G.; Nene, L.E.H.; Bouman, M.B.; de Vet, H.C.W.; Mureau, M.A.M.; Buncamper, M.E.; Winters, H.A.H.; Ritt, M.; Mullender, M.G. The Aesthetic Items Scale: A Tool for the Evaluation of Aesthetic Outcome after Breast Reconstruction. Plast. Reconstr. Surg. Glob. Open 2017, 5, e1254. [Google Scholar] [CrossRef]
- Pusic, A.L.; Klassen, A.F.; Scott, A.M.; Klok, J.A.; Cordeiro, P.G.; Cano, S.J. Development of a new patient-reported outcome measure for breast surgery: The BREAST-Q. Plast. Reconstr. Surg. 2009, 124, 345–353. [Google Scholar] [CrossRef]
- Kelemen, P.; Pukancsik, D.; Ujhelyi, M.; Kovacs, E.; Stamatiou, A.; Ivady, G.; Kenessey, I.; Kovacs, T.; Smanyko, V.; Rubovszky, G.; et al. Evaluation of the central pedicled, modified Wise-pattern technique as a standard level II oncoplastic breast-conserving surgery: A retrospective clinicopathological study of 190 breast cancer patients. Breast J. 2019, 25, 922–926. [Google Scholar] [CrossRef]
- Ribeiro, L. A new technique for reduction mammaplasty. Plast. Reconstr. Surg. 1975, 55, 330–334. [Google Scholar] [CrossRef]
- Manrique, O.J.; Huang, T.C.; Martinez-Jorge, J.; Ciudad, P.; Forte, A.J.; Bustos, S.S.; Boughey, J.C.; Jakub, J.W.; Degnim, A.C.; Galan, R. Prepectoral Two-Stage Implant-Based Breast Reconstruction with and without Acellular Dermal Matrix: Do We See a Difference? Plast. Reconstr. Surg. 2020, 145, 263e–272e. [Google Scholar] [CrossRef]
- Li, L.; Su, Y.; Xiu, B.; Huang, X.; Chi, W.; Hou, J.; Zhang, Y.; Tian, J.; Wang, J.; Wu, J. Comparison of prepectoral and subpectoral breast reconstruction after mastectomies: A systematic review and meta analysis. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 2019, 45, 1542–1550. [Google Scholar] [CrossRef] [PubMed]
- Pukancsik, D.; Kelemen, P.; Gulyas, G.; Ujhelyi, M.; Kovacs, E.; Eles, K.; Meszaros, N.; Kenessey, I.; Palhazi, P.; Kovacs, T.; et al. Clinical experiences with the use of ULTRAPRO((R)) mesh in single-stage direct-to-implant immediate postmastectomy breast reconstruction in 102 patients: A retrospective cohort study. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 2017, 43, 1244–1251. [Google Scholar] [CrossRef] [PubMed]
- Hansson, E.; Edvinsson, A.C.; Elander, A.; Kolby, L.; Hallberg, H. First-year complications after immediate breast reconstruction with a biological and a synthetic mesh in the same patient: A randomized controlled study. J. Surg. Oncol. 2020. [Google Scholar] [CrossRef] [PubMed]




| Characteristics | Mesh Group | Non-Mesh Group | p Value |
|---|---|---|---|
| n (%) | n (%) | ||
| Total number of patients | 59 | 58 | |
| Age | 49 (35–69) | 48.5 (34–78) | 0.735 (Mann–Whitney) |
| (year; median, min–max) | |||
| Height (cm; median, min–max) | 165 (154–180) | 165 (135–185) | 0.753 (Mann–Whitney) |
| Weight (kg; median, min–max) | 69 (52–106) | 69.5 (47–106) | 0.733 (Mann–Whitney) |
| BMI (median, min–max) | 24.6 (20.1–35) | 25.7 (17.3–35.9) | 0.544 (Mann–Whitney) |
| Smoking habits | 0.749 (Fisher) | ||
| yes | 7 (11.9 %) | 4 (6.9 %) | |
| no | 44 (74.6 %) | 37 (63.8 %) | |
| no data | 8 (13.5 %) | 17 (29.3 %) | |
| Comorbidities | 0.211 (chi-square) | ||
| yes | 43 (72.9 %) | 36 (62.1 %) | |
| no | 16 (27.2 %) | 22 (37.9 %) | |
| Laterality | 0.307 (chi-square) | ||
| left | 28 (47.5 %) | 33 (56.9 %) |
| Surgical Procedure-Related Characteristics | Mesh Group | Non-Mesh Group | p Value |
|---|---|---|---|
| n (%) | n (%) | ||
| Number of months elapsed between the primary and symmetrization surgery (month; median, min–max) | 16 (3–91) | 15 (5–66) | 0.506 (Mann–Whitney) |
| Duration of operation (minutes; median, min–max) | 70 (45–120) | 70 (30–120) | 0.371 (Mann–Whitney) |
| Type of surgery | 0.032 (chi-square) | ||
| mastopexy | 32 (54.3%) | 26 (44.8%) | |
| breast reduction | 12 (20.3%) | 5 (8.6%) | |
| implant and mastopexy | 15 (25.4%) | 27 (46.6%) | |
| Size of the implant used on the tumour side | 685 (380–1010) | 620 (375–920) | 0.012 (Mann–Whitney) |
| (cc; median, min–max) | |||
| Shape of the implant | 0.204 (Fisher) | ||
| anatomical | 56 (94.9%) | 51 (87.9%) | |
| round | 3 (5.1%) | 7 (12.1%) | |
| Size of the implant used on the symmetrization side | 0 (0–225) | 0 (0–325) | 0.055 (Mann–Whitney) |
| BREAST-Q Postoperative Questions | Mesh Group | Non-Mesh Group | p Value |
|---|---|---|---|
| Postop-Q1 (median, min–max) | 57 (18–100) | 49 (0–100) | 0.0004 (Wald–Wolfowitz) |
| Postop-Q2 (median, min–max) | 62 (34–100) | 62 (37–100) | 0.432 (Wald–Wolfowitz) |
| Postop-Q3 (median, min–max) | 76 (36–100) | 72 (24–100) | 0.012 (Wald–Wolfowitz) |
| Postop-Q4 (median, min–max) | 50 (14–91) | 41 (0–100) | 0.047 (Wald–Wolfowitz) |
| Measurments | Mesh Group | Non-Mesh Group | p Value |
|---|---|---|---|
| Total number of patients | 59 | 58 | |
| Sternal notch-to-nipple distance on the symmetrization side at the end of the follow-up (cm; median, min–max) | 22 (19.5–27.5) | 23.5 (19–26.5) | 0.00001 (Mann–Whitney) |
| Nipple-to-IMF distance on the symmetrization side at the end of the follow-up (cm; median, min–max) | 7.5 (5.5–13) | 6.75 (5–9.5) | 0.001 (Mann–Whitney) |
| Nipple-to-midline distance on the symmetrization side at the end of the follow-up (cm; median, min–max) | 11.5 (9–15.5) | 12 (8–15) | 0.118 (Mann–Whitney) |
| Sternal notch-to-nipple/neo-NAC distance on the mastectomy side at the end of the follow-up (cm; median, min–max) | 21 (18.5–27) | 21 (18–24) | 0.354 (Mann–Whitney) |
| Nipple/neo-NAC-IMF distance on the mastectomy side at the end of the follow-up (cm; median, min–max) | 7 (5–11) | 7,5 (4,5–10) | 0.733 (Mann–Whitney) |
| Nipple/neo-NAC-midline distance on the mastectomy side at the end of the follow-up (cm; median, min–max) | 10.5 (9–15) | 10,5 (8,5–15) | 0.402 (Mann–Whitney) |
| Sternal notch-to-nipple distance on the symmetrization side | 21 (18–26) | 20 (18–21) | 0.000009 (Mann–Whitney) |
| at the first week (cm; median, min–max) | |||
| Nipple-to-IMF distance on the symmetrization side at the first week (cm; median, min–max) | 7 (5–11) | 6 (5–8) | 0.0002 (Mann–Whitney) |
| Nipple-to-midline distance on the symmetrization side at the first week (cm; median, min–max) | 11 (9–15) | 11 (8–14) | 0.494 (Mann–Whitney) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
József, Z.; Újhelyi, M.; Ping, O.; Domján, S.; Fülöp, R.; Ivády, G.; Tislér, R.; Rubovszky, G.; Mészáros, N.; Kenessey, I.; et al. Long-Term Dynamic Changes in Cosmetic Outcomes and Patient Satisfaction after Implant-Based Postmastectomy Breast Reconstruction and Contralateral Mastopexy with or without an Ultrapro Mesh Sling Used for the Inner Bra Technique. A Retrospective Correlational Study. Cancers 2021, 13, 73. https://doi.org/10.3390/cancers13010073
József Z, Újhelyi M, Ping O, Domján S, Fülöp R, Ivády G, Tislér R, Rubovszky G, Mészáros N, Kenessey I, et al. Long-Term Dynamic Changes in Cosmetic Outcomes and Patient Satisfaction after Implant-Based Postmastectomy Breast Reconstruction and Contralateral Mastopexy with or without an Ultrapro Mesh Sling Used for the Inner Bra Technique. A Retrospective Correlational Study. Cancers. 2021; 13(1):73. https://doi.org/10.3390/cancers13010073
Chicago/Turabian StyleJózsef, Zsófia, Mihály Újhelyi, Orsolya Ping, Szilárd Domján, Rita Fülöp, Gabriella Ivády, Ráhel Tislér, Gábor Rubovszky, Norbert Mészáros, István Kenessey, and et al. 2021. "Long-Term Dynamic Changes in Cosmetic Outcomes and Patient Satisfaction after Implant-Based Postmastectomy Breast Reconstruction and Contralateral Mastopexy with or without an Ultrapro Mesh Sling Used for the Inner Bra Technique. A Retrospective Correlational Study" Cancers 13, no. 1: 73. https://doi.org/10.3390/cancers13010073
APA StyleJózsef, Z., Újhelyi, M., Ping, O., Domján, S., Fülöp, R., Ivády, G., Tislér, R., Rubovszky, G., Mészáros, N., Kenessey, I., & Mátrai, Z. (2021). Long-Term Dynamic Changes in Cosmetic Outcomes and Patient Satisfaction after Implant-Based Postmastectomy Breast Reconstruction and Contralateral Mastopexy with or without an Ultrapro Mesh Sling Used for the Inner Bra Technique. A Retrospective Correlational Study. Cancers, 13(1), 73. https://doi.org/10.3390/cancers13010073





