Advances in Multidisciplinary Management of Skull Base Meningiomas
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Modern Surgical Planning
3.1. The Role of Computer-Aided Approaches
3.2. The Role of Tractography
4. The Role of Surgery
4.1. Intraoperative Neurophysiological Monitoring in Skull Base Meningiomas
4.2. Preoperative Embolization
4.3. Reconstruction of the Surgical Route
5. Histopathological Features
6. Radiation Therapy
6.1. Fractionated Radiotherapy
6.2. Radiosurgery
6.2.1. Overview
6.2.2. Posterior Fossa
6.2.3. WHO Grade II and III
6.2.4. Combined MS–SRS Approach
6.2.5. Long-Term Follow-Up
7. The Role of Systemic Treatments
8. Current Thinking and Future Perspectives
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ostrom, Q.T.; Gittleman, H.; Truitt, G.; Boscia, A.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2011–2015. Neuro-Oncology 2018, 20, iv1–iv86. [Google Scholar] [CrossRef] [Green Version]
- Louis, D.N.; Perry, A.; Reifenberger, G.; von Deimling, A.; Figarella-Branger, D.; Cavenee, W.K.; Ohgaki, H.; Wiestler, O.D.; Kleihues, P.; Ellison, D.W. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: A Summary. Acta Neuropathol. 2016, 131, 803–820. [Google Scholar] [CrossRef] [Green Version]
- Simpson, D. The Recurrence of Intracranial Meningiomas after Surgical Treatment. J. Neurol. Neurosurg. Psychiatry 1957, 20, 22–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flood, L.M. Meningiomas of the Skull Base: Treatment Nuances in Contemporary Neurosurgery; Cappabianca, P., Solari, D., Eds.; Thieme: Stuttgart, NY, USA, 2018; ISBN 978-3-13-241302-3. [Google Scholar]
- Nanda, A.; Bir, S.C.; Maiti, T.K.; Konar, S.K.; Missios, S.; Guthikonda, B. Relevance of Simpson Grading System and Recurrence-Free Survival after Surgery for World Health Organization Grade I Meningioma. J. Neurosurg. 2017, 126, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Wiemels, J.; Wrensch, M.; Claus, E.B. Epidemiology and Etiology of Meningioma. J. Neurooncol. 2010, 99, 307–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Claus, E.B.; Bondy, M.L.; Schildkraut, J.M.; Wiemels, J.L.; Wrensch, M.; Black, P.M. Epidemiology of Intracranial Meningioma. Neurosurgery 2005, 57, 1088–1095. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mansouri, A.; Klironomos, G.; Taslimi, S.; Kilian, A.; Gentili, F.; Khan, O.H.; Aldape, K.; Zadeh, G. Surgically Resected Skull Base Meningiomas Demonstrate a Divergent Postoperative Recurrence Pattern Compared with Non–Skull Base Meningiomas. J. Neurosurg. 2016, 125, 431–440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakamura, M.; Roser, F.; Dormiani, M.; Vorkapic, P.; Samii, M. Surgical Treatment of Cerebellopontine Angle Meningiomas in Elderly Patients. Acta Neurochir. 2005, 147, 603–610. [Google Scholar] [CrossRef]
- Kolakshyapati, M.; Ikawa, F.; Abiko, M.; Mitsuhara, T.; Kinoshita, Y.; Takeda, M.; Kurisu, K. Alumni Association Group of the Department of Neurosurgery at Hiroshima University Multivariate Risk Factor Analysis and Literature Review of Postoperative Deterioration in Karnofsky Performance Scale Score in Elderly Patients with Skull Base Meningioma. Neurosurg. Focus 2018, 44, E14. [Google Scholar] [CrossRef]
- Ichinose, T.; Goto, T.; Ishibashi, K.; Takami, T.; Ohata, K. The Role of Radical Microsurgical Resection in Multimodal Treatment for Skull Base Meningioma: Clinical Article. J. Neurosurg. 2010, 113, 1072–1078. [Google Scholar] [CrossRef]
- Goto, T.; Ohata, K. Surgical Resectability of Skull Base Meningiomas. Neurol. Med. Chir. 2016, 56, 372–378. [Google Scholar] [CrossRef] [Green Version]
- Gousias, K.; Schramm, J.; Simon, M. The Simpson Grading Revisited: Aggressive Surgery and Its Place in Modern Meningioma Management. J. Neurosurg. 2016, 125, 551–560. [Google Scholar] [CrossRef] [Green Version]
- Apra, C.; Peyre, M.; Kalamarides, M. Current Treatment Options for Meningioma. Expert Rev. Neurother. 2018, 18, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.-H.; Zhang, W.-B.; Yu, Y.; Peng, X. Accuracy of Multimodal Image Fusion for Oral and Maxillofacial Tumors: A Revised Evaluation Method and Its Application. J. Cranio-Maxillofac. Surg. 2020, 48, 741–750. [Google Scholar] [CrossRef]
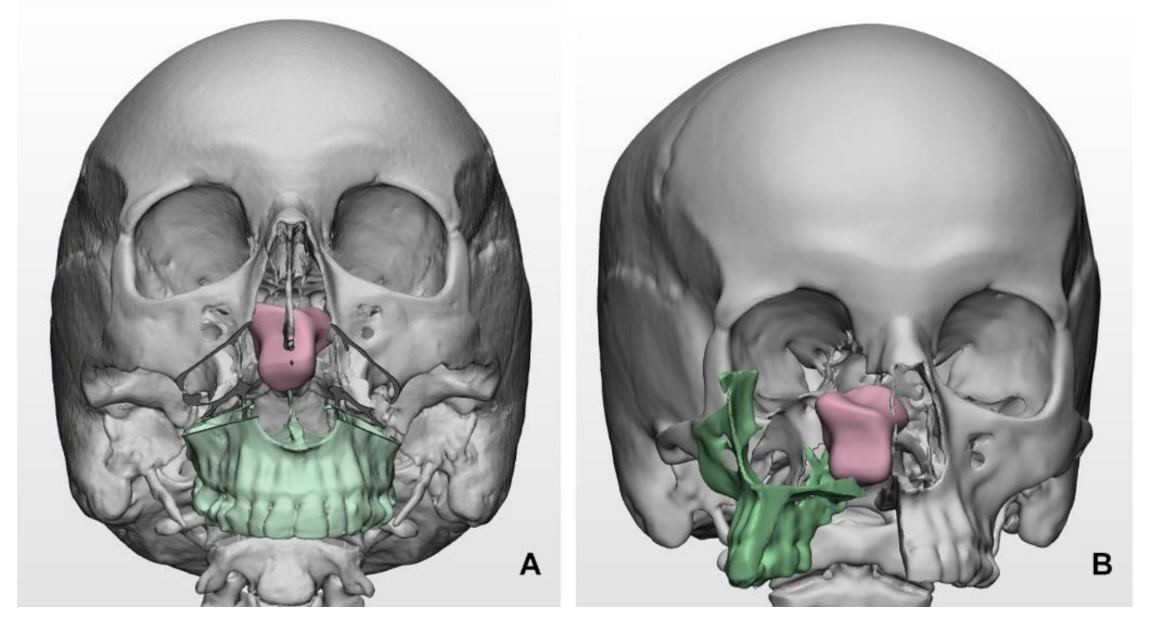
- Tel, A.; Bagatto, D.; Tuniz, F.; Sembronio, S.; Costa, F.; D’Agostini, S.; Robiony, M. The Evolution of Craniofacial Resection: A New Workflow for Virtual Planning in Complex Craniofacial Procedures. J. Cranio-Maxillofac. Surg. 2019, 47, 1475–1483. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Zhou, S.; Wu, Z.; Zhang, B.; Zhao, G. Statistical Modeling and Knowledge-Based Segmentation of Cerebral Artery Based on TOF-MRA and MR-T1. Comput. Methods Programs Biomed. 2020, 186, 105110. [Google Scholar] [CrossRef] [PubMed]
- Segato, A.; Pieri, V.; Favaro, A.; Riva, M.; Falini, A.; De Momi, E.; Castellano, A. Automated Steerable Path Planning for Deep Brain Stimulation Safeguarding Fiber Tracts and Deep Gray Matter Nuclei. Front. Robot. AI 2019, 6, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bücking, T.M.; Hill, E.R.; Robertson, J.L.; Maneas, E.; Plumb, A.A.; Nikitichev, D.I. From Medical Imaging Data to 3D Printed Anatomical Models. PLoS ONE 2017, 12, e0178540. [Google Scholar] [CrossRef] [Green Version]
- Soleman, J.; Leiggener, C.; Schlaeppi, A.-J.; Kienzler, J.; Fathi, A.-R.; Fandino, J. The Extended Subfrontal and Fronto-Orbito-Zygomatic Approach in Skull Base Meningioma Surgery: Clinical, Radiologic, and Cosmetic Outcome. J. Craniofac. Surg. 2016, 27, 433–440. [Google Scholar] [CrossRef]
- Ius, T.; Somma, T.; Baiano, C.; Guarracino, I.; Pauletto, G.; Nilo, A.; Maieron, M.; Palese, F.; Skrap, M.; Tomasino, B. Risk Assessment by Pre-Surgical Tractography in Left Hemisphere Low-Grade Gliomas. Front. Neurol. 2021, 12, 648432. [Google Scholar] [CrossRef]
- Ius, T.; Turella, L.; Pauletto, G.; Isola, M.; Maieron, M.; Sciacca, G.; Budai, R.; D’Agostini, S.; Eleopra, R.; Skrap, M. Quantitative Diffusion Tensor Imaging Analysis of Low-Grade Gliomas: From Preclinical Application to Patient Care. World Neurosurgery 2017, 97, 333–343. [Google Scholar] [CrossRef]
- Campanella, M.; Ius, T.; Skrap, M.; Fadiga, L. Alterations in Fiber Pathways Reveal Brain Tumor Typology: A Diffusion Tractography Study. PeerJ 2014, 2, e497. [Google Scholar] [CrossRef] [Green Version]
- Jacquesson, T.; Cotton, F.; Attyé, A.; Zaouche, S.; Tringali, S.; Bosc, J.; Robinson, P.; Jouanneau, E.; Frindel, C. Probabilistic Tractography to Predict the Position of Cranial Nerves Displaced by Skull Base Tumors: Value for Surgical Strategy Through a Case Series of 62 Patients. Neurosurgery 2019, 85, E125–E136. [Google Scholar] [CrossRef] [PubMed]
- Jacquesson, T.; Frindel, C.; Kocevar, G.; Berhouma, M.; Jouanneau, E.; Attyé, A.; Cotton, F. Overcoming Challenges of Cranial Nerve Tractography: A Targeted Review. Neurosurgery 2019, 84, 313–325. [Google Scholar] [CrossRef]
- Castellaro, M.; Moretto, M.; Baro, V.; Brigadoi, S.; Zanoletti, E.; Anglani, M.; Denaro, L.; Dell’Acqua, R.; Landi, A.; Causin, F.; et al. Multishell Diffusion MRI-Based Tractography of the Facial Nerve in Vestibular Schwannoma. AJNR. Am. J. Neuroradiol. 2020, 41, 1480–1486. [Google Scholar] [CrossRef] [PubMed]
- Jho, H.-D.; Carrau, R.L. Endoscopic Endonasal Transsphenoidal Surgery: Experience with 50 Patients. J. Neurosurg. 1997, 87, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Cappabianca, P.; Alfieri, A.; de Divitiis, E. Endoscopic Endonasal Transsphenoidal Approach to the Sella: Towards Functional Endoscopic Pituitary Surgery (Feps)*. MIN-Minim. Invasive Neurosurg. 1998, 41, 66–73. [Google Scholar] [CrossRef]
- Kassam, A.B.; Gardner, P.; Snyderman, C.; Mintz, A.; Carrau, R. Expanded Endonasal Approach: Fully Endoscopic, Completely Transnasal Approach to the Middle Third of the Clivus, Petrous Bone, Middle Cranial Fossa, and Infratemporal Fossa. Neurosurg. Focus 2005, 19, E6. [Google Scholar] [CrossRef] [Green Version]
- Zada, G.; Du, R.; Laws, E.R. Defining the “Edge of the Envelope”: Patient Selection in Treating Complex Sellar-Based Neoplasms via Transsphenoidal versus Open Craniotomy: Clinical Article. J. Neurosurg. 2011, 114, 286–300. [Google Scholar] [CrossRef]
- De Rosa, A.; Pineda, J.; Cavallo, L.M.; Di Somma, A.; Romano, A.; Topczewski, T.E.; Somma, T.; Solari, D.; Enseñat, J.; Cappabianca, P.; et al. Endoscopic Endo- and Extra-Orbital Corridors for Spheno-Orbital Region: Anatomic Study with Illustrative Case. Acta Neurochir. 2019, 161, 1633–1646. [Google Scholar] [CrossRef]
- Koppe, M.; Gleizal, A.; Orset, E.; Bachelet, J.T.; Jouanneau, E.; Rougeot, A. Superior Eyelid Crease Approach for Transobital Neuroendoscopic Surgery of the Anterior Cranial Fossa. J. Craniofac. Surg. 2013, 24, 1616–1621. [Google Scholar] [CrossRef]
- Abou-Al-Shaar, H.; Krisht, K.M.; Cohen, M.A.; Abunimer, A.M.; Neil, J.A.; Karsy, M.; Alzhrani, G.; Couldwell, W.T. Cranio-Orbital and Orbitocranial Approaches to Orbital and Intracranial Disease: Eye-Opening Approaches for Neurosurgeons. Front. Surg. 2020, 7, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janecka, I.P. Classification of Facial Translocation Approach to the Skull Base. Otolaryngol. Head Neck Surg. 1995, 112, 579–585. [Google Scholar] [CrossRef]
- Skull Base Surgery: Anatomy, Biology, and Technology; Janecka, I.P. (Ed.) Lippincott-Raven: Philadelphia, PA, USA, 1997; ISBN 978-0-397-51716-9. [Google Scholar]
- Inoue, T.; Rhoton, A.L.; Theele, D.; Barry, M.E. Surgical Approaches to the Cavernous Sinus: A Microsurgical Study. Neurosurgery 1990, 26, 903. [Google Scholar] [CrossRef]
- Jannetta, P.J.; Abbasy, M.; Maroon, J.C.; Ramos, F.M.; Albin, M.S. Etiology and Definitive Microsurgical Treatment of Hemifacial Spasm: Operative Techniques and Results in 47 Patients. J. Neurosurg. 1977, 47, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Parkinson, D. The Posterior Cranial Fossa: Microsurgical Anatomy and Surgical Approaches. Neurosurgery 2001, 48, 1196. [Google Scholar] [CrossRef]
- Scerrati, A.; Lee, J.-S.; Zhang, J.; Ammirati, M. Microsurgical Anatomy of the Internal Acoustic Meatus as Seen Using the Retrosigmoid Approach. Otol. Neurotol. 2016, 37, 568–573. [Google Scholar] [CrossRef]
- Scerrati, A.; Lee, J.-S.; Zhang, J.; Ammirati, M. Exposing the Fundus of the Internal Acoustic Meatus without Entering the Labyrinth Using a Retrosigmoid Approach: Is It Possible? World Neurosurg. 2016, 91, 357–364. [Google Scholar] [CrossRef]
- Hakuba, A.; Nishimura, S.; Jang, B.J. A Combined Retroauricular and Preauricular Transpetrosal-Transtentorial Approach to Clivus Meningiomas. Surg. Neurol. 1988, 30, 108–116. [Google Scholar] [CrossRef]
- King, T.T.; Morrison, A.W. Translabyrinthine and Transtentorial Removal of Acoustic Nerve Tumors: Results in 150 Cases. J. Neurosurg. 1980, 52, 210–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seoane, E.; Rhoton, A.L. Suprameatal Extension of the Retrosigmoid Approach: Microsurgical Anatomy. Neurosurgery 1999, 44, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Ercan, S.; Scerrati, A.; Wu, P.; Zhang, J.; Ammirati, M. Is Less Always Better? Keyhole and Standard Subtemporal Approaches: Evaluation of Temporal Lobe Retraction and Surgical Volume with and without Zygomatic Osteotomy in a Cadaveric Model. J. Neurosurg. 2017, 127, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-S.; Scerrati, A.; Zhang, J.; Ammirati, M. Quantitative Analysis of Surgical Exposure and Surgical Freedom to the Anterosuperior Pons: Comparison of Pterional Transtentorial, Orbitozygomatic, and Anterior Petrosal Approaches. Neurosurg. Rev. 2016, 39, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Bassiouni, H.; Ntoukas, V.; Asgari, S.; Sandalcioglu, E.I.; Stolke, D.; Seifert, V. Foramen magnum meningiomas. Neurosurgery 2006, 59, 1177–1187. [Google Scholar] [CrossRef]
- Scheitzach, J.; Schebesch, K.-M.; Brawanski, A.; Proescholdt, M.A. Skull Base Meningiomas: Neurological Outcome after Microsurgical Resection. J. Neurooncol. 2014, 116, 381–386. [Google Scholar] [CrossRef]
- Voß, K.M.; Spille, D.C.; Sauerland, C.; Suero Molina, E.; Brokinkel, C.; Paulus, W.; Stummer, W.; Holling, M.; Jeibmann, A.; Brokinkel, B. The Simpson Grading in Meningioma Surgery: Does the Tumor Location Influence the Prognostic Value? J. Neurooncol. 2017, 133, 641–651. [Google Scholar] [CrossRef] [PubMed]
- Bassiouni, H.; Asgari, S.; Sandalcioglu, I.E.; Seifert, V.; Stolke, D.; Marquardt, G. Anterior Clinoidal Meningiomas: Functional Outcome after Microsurgical Resection in a Consecutive Series of 106 Patients: Clinical Article. J. Neurosurg. 2009, 111, 1078–1090. [Google Scholar] [CrossRef] [Green Version]
- Seifert, V. Clinical Management of Petroclival Meningiomas and the Eternal Quest for Preservation of Quality of Life: Personal Experiences over a Period of 20 Years. Acta Neurochir. 2010, 152, 1099–1116. [Google Scholar] [CrossRef]
- Raheja, A.; Couldwell, W.T. Microsurgical Resection of Skull Base Meningioma—Expanding the Operative Corridor. J. Neurooncol. 2016, 130, 263–267. [Google Scholar] [CrossRef]
- Goto, T.; Muraoka, H.; Kodama, K.; Hara, Y.; Yako, T.; Hongo, K. Intraoperative Monitoring of Motor Evoked Potential for the Facial Nerve Using a Cranial Peg-Screw Electrode and a “Threshold-Level” Stimulation Method. Skull Base 2010, 20, 429–434. [Google Scholar] [CrossRef] [Green Version]
- Cornelius, J.F.; Schipper, J.; Tortora, A.; Krause-Molle, Z.; Smuga, M.; Petridis, A.K.; Steiger, H.-J. Continuous and Dynamic Facial Nerve Mapping during Surgery of Cerebellopontine Angle Tumors: Clinical Pilot Series. World Neurosurg. 2018, 119, e855–e863. [Google Scholar] [CrossRef] [PubMed]
- Slotty, P.J.; Abdulazim, A.; Kodama, K.; Javadi, M.; Hänggi, D.; Seifert, V.; Szelényi, A. Intraoperative Neurophysiological Monitoring during Resection of Infratentorial Lesions: The Surgeon’s View. J. Neurosurg. 2017, 126, 281–288. [Google Scholar] [CrossRef]
- Ilyas, A.; Przybylowski, C.; Chen, C.-J.; Ding, D.; Foreman, P.M.; Buell, T.J.; Taylor, D.G.; Kalani, M.Y.; Park, M.S. Preoperative Embolization of Skull Base Meningiomas: A Systematic Review. J. Clin. Neurosci. 2019, 59, 259–264. [Google Scholar] [CrossRef]
- Yoon, N.; Shah, A.; Couldwell, W.T.; Kalani, M.Y.S.; Park, M.S. Preoperative Embolization of Skull Base Meningiomas: Current Indications, Techniques, and Pearls for Complication Avoidance. Neurosurg. Focus 2018, 44, E5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Maio, S.; Ramanathan, D.; Garcia-Lopez, R.; Rocha, M.H.; Guerrero, F.P.; Ferreira, M.; Sekhar, L.N. Evolution and Future of Skull Base Surgery: The Paradigm of Skull Base Meningiomas. World Neurosurg. 2012, 78, 260–275. [Google Scholar] [CrossRef]
- Jumah, F.; AbuRmilah, A.; Raju, B.; Jaber, S.; Adeeb, N.; Narayan, V.; Sun, H.; Cuellar, H.; Gupta, G.; Nanda, A. Does preoperative embolization improve outcomes of meningioma resection? A systematic review and meta-analysis. Neurosurg. Rev. 2021. [Google Scholar] [CrossRef]
- Ellis, J.A.; D’Amico, R.; Sisti, M.B.; Bruce, J.N.; McKhann, G.M.; Lavine, S.D.; Meyers, P.M.; Strozyk, D. Pre-operative intracranial meningioma embolization. Expert Rev. Neurother. 2011, 11, 545–556. [Google Scholar] [CrossRef] [PubMed]
- Hanasono, M.M. Reconstruction after Open Surgery for Skull-Base Malignancies. J. Neurooncol. 2020, 150, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Gagliardi, F.; Piloni, M.; Bailo, M.; Gragnaniello, C.; Nocera, G.; Boari, N.; Spina, A.; Caputy, A.J.; Mortini, P. Temporal Myofascial Segmentation for Multilayer Reconstruction of Middle Cranial Fossa Floor after Extradural Subtemporal Approach to the Clival and Paraclival Region. Head Neck 2019, 41, 3631–3638. [Google Scholar] [CrossRef]
- Parkes, W.J.; Krein, H.; Heffelfinger, R.; Curry, J. Use of the Anterolateral Thigh in Cranio-Orbitofacial Reconstruction. Plast. Surg. Int. 2011, 2011, 1–6. [Google Scholar] [CrossRef]
- Hadad, G.; Bassagasteguy, L.; Carrau, R.L.; Mataza, J.C.; Kassam, A.; Snyderman, C.H.; Mintz, A. A Novel Reconstructive Technique After Endoscopic Expanded Endonasal Approaches: Vascular Pedicle Nasoseptal Flap. Laryngoscope 2006, 116, 1882–1886. [Google Scholar] [CrossRef] [PubMed]
- Scerrati, A.; Trovalusci, F.; Albanese, A.; Ponticelli, G.S.; Tagliaferri, V.; Sturiale, C.L.; Cavallo, M.A.; Marchese, E. A Workflow to Generate Physical 3D Models of Cerebral Aneurysms Applying Open Source Freeware for CAD Modeling and 3D Printing. Interdiscip. Neurosurg. 2019, 17, 1–6. [Google Scholar] [CrossRef]
- Tel, A. Computer-Guided in-House Cranioplasty: Establishing a Novel Standard for Cranial Reconstruction and Proposal of an Updated Protocol. J. Oral Maxillofac. Surg. 2020, 78, 2297-e1. [Google Scholar] [CrossRef]
- Zheng, J.S.; Liu, X.H.; Chen, X.Z.; Jiang, W.B.; Abdelrehem, A.; Zhang, S.Y.; Chen, M.J.; Yang, C. Customized Skull Base–Temporomandibular Joint Combined Prosthesis with 3D-Printing Fabrication for Craniomaxillofacial Reconstruction: A Preliminary Study. Int. J. Oral Maxillofac. Surg. 2019, 48, 1440–1447. [Google Scholar] [CrossRef]
- Moriwaki, Y.; Tomioka, Y.; Imai, H.; Iida, T.; Yamashita, S.; Kanayama, K.; Iwamoto, N.; Okazaki, M. Treating Pulsatile Exophthalmos in Child with Minimally Invasive Approach and Custom-Made Titanium Mesh Plate. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2070. [Google Scholar] [CrossRef]
- Grob, S.R.; Chen, K.G.; Tao, J.P. Orbital Roof Reconstruction Using Nylon Foil Implants. Ophthal. Plast. Reconstr. Surg. 2019, 35, 286–289. [Google Scholar] [CrossRef]
- Abedalthagafi, M.; Bi, W.L.; Aizer, A.A.; Merrill, P.H.; Brewster, R.; Agarwalla, P.K.; Listewnik, M.L.; Dias-Santagata, D.; Thorner, A.R.; Van Hummelen, P.; et al. Oncogenic PI3K Mutations Are as Common as AKT1 and SMO Mutations in Meningioma. Neuro-Oncology 2016, 18, 649–655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barresi, V.; Alafaci, C.; Caffo, M.; Barresi, G.; Tuccari, G. Clinicopathological Characteristics, Hormone Receptor Status and Matrix Metallo-Proteinase-9 (MMP-9) Immunohistochemical Expression in Spinal Meningiomas. Pathol. Res. Pract. 2012, 208, 350–355. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, M.M.; Worley, S.; Raghavan, A.; Das, P.; Recinos, P.F.; Barnett, G.H.; Kshettry, V.R. Peritumoral Brain Edema and Surgical Outcome in Secretory Meningiomas: A Matched-Cohort Analysis. World Neurosurg. 2021, 145, e170–e176. [Google Scholar] [CrossRef]
- Brastianos, P.K.; Horowitz, P.M.; Santagata, S.; Jones, R.T.; McKenna, A.; Getz, G.; Ligon, K.L.; Palescandolo, E.; Van Hummelen, P.; Ducar, M.D.; et al. Genomic Sequencing of Meningiomas Identifies Oncogenic SMO and AKT1 Mutations. Nat. Genet. 2013, 45, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Clark, V.E.; Erson-Omay, E.Z.; Serin, A.; Yin, J.; Cotney, J.; Ozduman, K.; Avsar, T.; Li, J.; Murray, P.B.; Henegariu, O.; et al. Genomic Analysis of Non-Nf2 Meningiomas Reveals Mutations in Traf7, Klf4, Akt1, and Smo. Science 2013, 339, 1077–1080. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barresi, V.; Simbolo, M.; Fioravanzo, A.; Piredda, M.; Caffo, M.; Ghimenton, C.; Pinna, G.; Longhi, M.; Nicolato, A.; Scarpa, A. Molecular Profiling of 22 Primary Atypical Meningiomas Shows the Prognostic Significance of 18q Heterozygous Loss and CDKN2A/B Homozygous Deletion on Recurrence-Free Survival. Cancers 2021, 13, 903. [Google Scholar] [CrossRef]
- Yesilöz, Ü.; Kirches, E.; Hartmann, C.; Scholz, J.; Kropf, S.; Sahm, F.; Nakamura, M.; Mawrin, C. Frequent AKT1E17K Mutations in Skull Base Meningiomas Are Associated with MTOR and ERK1/2 Activation and Reduced Time to Tumor Recurrence. Neuro-Oncology 2017, 19, 1088–1096. [Google Scholar] [CrossRef] [PubMed]
- Hao, S.; Huang, G.; Feng, J.; Li, D.; Wang, K.; Wang, L.; Wu, Z.; Wan, H.; Zhang, L.; Zhang, J. Non-NF2 Mutations Have a Key Effect on Inhibitory Immune Checkpoints and Tumor Pathogenesis in Skull Base Meningiomas. J. Neurooncol. 2019, 144, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Boetto, J.; Bielle, F.; Sanson, M.; Peyre, M.; Kalamarides, M. Smo Mutation Status Defines a Distinct and Frequent Molecular Subgroup in Olfactory Groove Meningiomas. Neuro-Oncology 2017, 276. [Google Scholar] [CrossRef] [Green Version]
- Clark, V.E.; Harmancı, A.S.; Bai, H.; Youngblood, M.W.; Lee, T.I.; Baranoski, J.F.; Ercan-Sencicek, A.G.; Abraham, B.J.; Weintraub, A.S.; Hnisz, D.; et al. Recurrent Somatic Mutations in POLR2A Define a Distinct Subset of Meningiomas. Nat. Genet. 2016, 48, 1253–1259. [Google Scholar] [CrossRef] [Green Version]
- Goldsmith, B.J.; Wara, W.M.; Wilson, C.B.; Larson, D.A. Postoperative Irradiation for Subtotally Resected Meningiomas: A Retrospective Analysis of 140 Patients Treated from 1967 to 1990. J. Neurosurg. 1994, 80, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Maire, J.-P.; Caudry, M.; Guérin, J.; Célérier, D.; San Galli, F.; Causse, N.; Trouette, R.; Dautheribes, M. Fractionated Radiation Therapy in the Treatment of Intracranial Meningiomas: Local Control, Functional Efficacy, and Tolerance in 91 Patients. Int. J. Radiat. Oncol. 1995, 33, 315–321. [Google Scholar] [CrossRef]
- Nutting, C.; Brada, M.; Brazil, L.; Sibtain, A.; Saran, F.; Westbury, C.; Moore, A.; Thomas, D.G.T.; Traish, D.; Ashley, S. Radiotherapy in the Treatment of Benign Meningioma of the Skull Base. J. Neurosurg. 1999, 90, 823–827. [Google Scholar] [CrossRef] [Green Version]
- Vendrely, V.; Maire, J.P.; Darrouzet, V.; Bonichon, N.; San Galli, F.; Célérier, D.; Causse, N.; Demeaux, H.; Trouette, R.; Dahan, O.; et al. Radiothérapie fractionnée des méningiomes intracrâniens: 15 ans d’expérience au centre hospitalier universitaire de Bordeaux. Cancer/Radiothérapie 1999, 3, 311–317. [Google Scholar] [CrossRef]
- Mendenhall, W.M.; Morris, C.G.; Amdur, R.J.; Foote, K.D.; Friedman, W.A. Radiotherapy Alone or after Subtotal Resection for Benign Skull Base Meningiomas. Cancer 2003, 98, 1473–1482. [Google Scholar] [CrossRef]
- O’steen, L.; Amdur, R.J.; Morris, C.G.; Mendenhall, W.M. Challenging the Concept That Late Recurrence and Death from Tumor Are Common after Fractionated Radiotherapy for Benign Meningioma. Radiother. Oncol. 2019, 137, 55–60. [Google Scholar] [CrossRef]
- Amichetti, M.; Amelio, D.; Minniti, G. Radiosurgery with Photons or Protons for Benign and Malignant Tumours of the Skull Base: A Review. Radiat. Oncol. 2012, 7, 210. [Google Scholar] [CrossRef] [Green Version]
- Crossen, J.R.; Garwood, D.; Glatstein, E.; Neuwelt, E.A. Neurobehavioral Sequelae of Cranial Irradiation in Adults: A Review of Radiation-Induced Encephalopathy. J. Clin. Oncol. 1994, 12, 627–642. [Google Scholar] [CrossRef] [PubMed]
- Maguire, P.D.; Clough, R.; Friedman, A.H.; Halperin, E.C. Fractionated External-Beam Radiation Therapy for Meningiomas of the Cavernous Sinus. Int. J. Radiat. Oncol. 1999, 44, 75–79. [Google Scholar] [CrossRef]
- Dufour, H.; Muracciole, X.; Métellus, P.; Régis, J.; Chinot, O.; Grisoli, F. Long-Term Tumor Control and Functional Outcome in Patients with Cavernous Sinus Meningiomas Treated by Radiotherapy with or without Previous Surgery: Is There an Alternative to Aggressive Tumor Removal? Neurosurgery 2001, 48, 285–296. [Google Scholar] [CrossRef]
- Rogers, L.; Zhang, P.; Vogelbaum, M.A.; Perry, A.; Ashby, L.S.; Modi, J.M.; Alleman, A.M.; Galvin, J.; Brachman, D.; Jenrette, J.M.; et al. Intermediate-Risk Meningioma: Initial Outcomes from NRG Oncology RTOG 0539. J. Neurosurg. 2018, 129, 35–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogers, C.L.; Won, M.; Vogelbaum, M.A.; Perry, A.; Ashby, L.S.; Modi, J.M.; Alleman, A.M.; Galvin, J.; Fogh, S.E.; Youssef, E.; et al. High-Risk Meningioma: Initial Outcomes From NRG Oncology/RTOG 0539. Int. J. Radiat. Oncol. Biol. Phys. 2020, 106, 790–799. [Google Scholar] [CrossRef]
- Jenkinson, M.D.; Javadpour, M.; Haylock, B.J.; Young, B.; Gillard, H.; Vinten, J.; Bulbeck, H.; Das, K.; Farrell, M.; Looby, S.; et al. The ROAM/EORTC-1308 Trial: Radiation versus Observation Following Surgical Resection of Atypical Meningioma: Study Protocol for a Randomised Controlled Trial. Trials 2015, 16, 519. [Google Scholar] [CrossRef] [Green Version]
- Scaringi, C.; Agolli, L.; Minniti, G. Technical Advances in Radiation Therapy for Brain Tumors. Anticancer Res. 2018, 38, 6041–6045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henzel, M.; Gross, M.W.; Hamm, K.; Surber, G.; Kleinert, G.; Failing, T.; Strassmann, G.; Engenhart-Cabillic, R. Significant Tumor Volume Reduction of Meningiomas after Stereotactic Radiotherapy. Neurosurgery 2006, 59, 1188–1194. [Google Scholar] [CrossRef] [PubMed]
- Tanzler, E.; Morris, C.G.; Kirwan, J.M.; Amdur, R.J.; Mendenhall, W.M. Outcomes of Who Grade i Meningiomas Receiving Definitive or Postoperative Radiotherapy. Int. J. Radiat. Oncol. 2011, 79, 508–513. [Google Scholar] [CrossRef] [PubMed]
- Minniti, G.; Clarke, E.; Cavallo, L.; Osti, M.F.; Esposito, V.; Cantore, G.; Cappabianca, P.; Enrici, R.M. Fractionated Stereotactic Conformal Radiotherapy for Large Benign Skull Base Meningiomas. Radiat. Oncol. 2011, 6, 36. [Google Scholar] [CrossRef] [PubMed]
- Soldà, F.; Wharram, B.; De Ieso, P.B.; Bonner, J.; Ashley, S.; Brada, M. Long-Term Efficacy of Fractionated Radiotherapy for Benign Meningiomas. Radiother. Oncol. 2013, 109, 330–334. [Google Scholar] [CrossRef] [PubMed]
- Combs, S.E.; Farzin, M.; Boehmer, J.; Oehlke, O.; Molls, M.; Debus, J.; Grosu, A.-L. Clinical Outcome after High-Precision Radiotherapy for Skull Base Meningiomas: Pooled Data from Three Large German Centers for Radiation Oncology. Radiother. Oncol. 2018, 127, 274–279. [Google Scholar] [CrossRef]
- Fokas, E.; Henzel, M.; Surber, G.; Hamm, K.; Engenhart-Cabillic, R. Stereotactic Radiation Therapy for Benign Meningioma: Long-Term Outcome in 318 Patients. Int. J. Radiat. Oncol. 2014, 89, 569–575. [Google Scholar] [CrossRef]
- Kaul, D.; Budach, V.; Misch, M.; Wiener, E.; Exner, S.; Badakhshi, H. Meningioma of the Skull Base: Long-Term Outcome after Image-Guided Stereotactic Radiotherapy. Cancer/Radiothérapie 2014, 18, 730–735. [Google Scholar] [CrossRef]
- Han, J.; Girvigian, M.R.; Chen, J.C.T.; Miller, M.J.; Lodin, K.; Rahimian, J.; Arellano, A.; Cahan, B.L.; Kaptein, J.S. A Comparative Study of Stereotactic Radiosurgery, Hypofractionated, and Fractionated Stereotactic Radiotherapy in the Treatment of Skull Base Meningioma. Am. J. Clin. Oncol. 2014, 37, 255–260. [Google Scholar] [CrossRef]
- Slater, J.D.; Loredo, L.N.; Chung, A.; Bush, D.A.; Patyal, B.; Johnson, W.D.; Hsu, F.P.K.; Slater, J.M. Fractionated Proton Radiotherapy for Benign Cavernous Sinus Meningiomas. Int. J. Radiat. Oncol. 2012, 83, e633–e637. [Google Scholar] [CrossRef]
- Weber, D.C.; Schneider, R.; Goitein, G.; Koch, T.; Ares, C.; Geismar, J.H.; Schertler, A.; Bolsi, A.; Hug, E.B. Spot Scanning-Based Proton Therapy for Intracranial Meningioma: Long-Term Results from the Paul Scherrer Institute. Int. J. Radiat. Oncol. 2012, 83, 865–871. [Google Scholar] [CrossRef]
- Sanford, N.N.; Yeap, B.Y.; Larvie, M.; Daartz, J.; Munzenrider, J.E.; Liebsch, N.J.; Fullerton, B.; Pan, E.; Loeffler, J.S.; Shih, H.A. Prospective, Randomized Study of Radiation Dose Escalation with Combined Proton-Photon Therapy for Benign Meningiomas. Int. J. Radiat. Oncol. 2017, 99, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Connell, P.P.; Macdonald, R.L.; Mansur, D.B.; Nicholas, M.K.; Mundt, A.J. Tumor Size Predicts Control of Benign Meningiomas Treated with Radiotherapy. Neurosurgery 1999, 44, 1194–1200. [Google Scholar] [CrossRef] [PubMed]
- Torres, R.C.; Frighetto, L.; De Salles, A.A.F.; Goss, B.; Medin, P.; Solberg, T.; Ford, J.M.; Selch, M. Radiosurgery and Stereotactic Radiotherapy for Intracranial Meningiomas. Neurosurg. Focus 2003, 14, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Lo, S.S.; Cho, K.H.; Hall, W.A.; Kossow, R.J.; Hernandez, W.L.; McCollow, K.K.; Gerbi, B.J.; Higgins, P.D.; Lee, C.K.; Dusenbery, K.E. Single Dose versus Fractionated Stereotactic Radiotherapy for Meningiomas. Can. J. Neurol. Sci. J. Can. Sci. Neurol. 2002, 29, 240–248. [Google Scholar] [CrossRef] [Green Version]
- Metellus, P.; Regis, J.; Muracciole, X.; Fuentes, S.; Dufour, H.; Nanni, I.; Chinot, O.; Martin, P.-M.; Grisoli, F. Evaluation of Fractionated Radiotherapy and Gamma Knife Radiosurgery in Cavernous Sinus Meningiomas: Treatment Strategy. Neurosurgery 2005, 57, 873–886. [Google Scholar] [CrossRef]
- Colombo, F.; Casentini, L.; Cavedon, C.; Scalchi, P.; Cora, S.; Francescon, P. Cyberknife Radiosurgery for Benign Meningiomas. Neurosurgery 2009, 64, A7–A13. [Google Scholar] [CrossRef] [PubMed]
- Navarria, P.; Pessina, F.; Cozzi, L.; Clerici, E.; Villa, E.; Ascolese, A.M.; De Rose, F.; Comito, T.; Franzese, C.; D’Agostino, G.; et al. Hypofractionated Stereotactic Radiation Therapy in Skull Base Meningiomas. J. Neurooncol. 2015, 124, 283–289. [Google Scholar] [CrossRef]
- Marchetti, M.; Bianchi, S.; Pinzi, V.; Tramacere, I.; Fumagalli, M.L.; Milanesi, I.M.; Ferroli, P.; Franzini, A.; Saini, M.; DiMeco, F.; et al. Multisession Radiosurgery for Sellar and Parasellar Benign Meningiomas: Long-Term Tumor Growth Control and Visual Outcome. Neurosurgery 2016, 78, 638–646. [Google Scholar] [CrossRef]
- Marchetti, M.; Conti, A.; Beltramo, G.; Pinzi, V.; Pontoriero, A.; Tramacere, I.; Senger, C.; Pergolizzi, S.; Fariselli, L. Multisession Radiosurgery for Perioptic Meningiomas: Medium-to-Long Term Results from a CyberKnife Cooperative Study. J. Neurooncol. 2019, 143, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, E.K.; Nguyen, T.K.; Boldt, G.; Louie, A.V.; Bauman, G.S. Hypofractionated Stereotactic Radiotherapy for Intracranial Meningioma: A Systematic Review. Neuro-Oncol. Pract. 2019, 6, 346–353. [Google Scholar] [CrossRef]
- Milano, M.T.; Sharma, M.; Soltys, S.G.; Sahgal, A.; Usuki, K.Y.; Saenz, J.-M.; Grimm, J.; El Naqa, I. Radiation-Induced Edema after Single-Fraction or Multifraction Stereotactic Radiosurgery for Meningioma: A Critical Review. Int. J. Radiat. Oncol. 2018, 101, 344–357. [Google Scholar] [CrossRef] [Green Version]
- Leksell, L. A Note on the Treatment of Acoustic Tumours. Acta Chir. Scand. 1971, 137, 763–765. [Google Scholar]
- Team, E.W. Leksell Gamma Knife—50 Years of Iconic Brain Care; Elekta: Stockholm, Sweden, 2018. [Google Scholar]
- Pollock, B.E.; Stafford, S.L.; Utter, A.; Giannini, C.; Schreiner, S.A. Stereotactic Radiosurgery Provides Equivalent Tumor Control to Simpson Grade 1 Resection for Patients with Small- to Medium-Size Meningiomas. Int. J. Radiat. Oncol. 2003, 55, 1000–1005. [Google Scholar] [CrossRef]
- Adler, J.R.; Murphy, M.J.; Chang, S.D.; Hancock, S.L. Image-Guided Robotic Radiosurgery. Neurosurgery 1999, 44, 1299–1306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.Y.K.; Niranjan, A.; McInerney, J.; Kondziolka, D.; Flickinger, J.C.; Lunsford, L.D. Stereotactic Radiosurgery Providing Long-Term Tumor Control of Cavernous Sinus Meningiomas. J. Neurosurg. 2002, 97, 65–72. [Google Scholar] [CrossRef]
- Kreil, W. Long Term Experience of Gamma Knife Radiosurgery for Benign Skull Base Meningiomas. J. Neurol. Neurosurg. Psychiatry 2005, 76, 1425–1430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kondziolka, D.; Nathoo, N.; Flickinger, J.C.; Niranjan, A.; Maitz, A.H.; Lunsford, L.D. Long-Term Results after Radiosurgery for Benign Intracranial Tumors. Neurosurgery 2003, 53, 815–822. [Google Scholar] [CrossRef] [PubMed]
- Patibandla, M.R.; Lee, C.; Tata, A.; Addagada, G.C.; Sheehan, J.P. Stereotactic Radiosurgery for WHO Grade I Posterior Fossa Meningiomas: Long-Term Outcomes with Volumetric Evaluation. J. Neurosurg. 2018, 129, 1249–1259. [Google Scholar] [CrossRef] [Green Version]
- Flannery, T.J.; Kano, H.; Lunsford, L.D.; Sirin, S.; Tormenti, M.; Niranjan, A.; Flickinger, J.C.; Kondziolka, D. Long-Term Control of Petroclival Meningiomas through Radiosurgery: Clinical Article. J. Neurosurg. 2010, 112, 957–964. [Google Scholar] [CrossRef] [Green Version]
- Debus, J.; Wuendrich, M.; Pirzkall, A.; Hoess, A.; Schlegel, W.; Zuna, I.; Engenhart-Cabillic, R.; Wannenmacher, M. High Efficacy of Fractionated Stereotactic Radiotherapy of Large Base-of-Skull Meningiomas: Long-Term Results. J. Clin. Oncol. 2001, 19, 3547–3553. [Google Scholar] [CrossRef]
- Aichholzer, M.; Bertalanffy, A.; Dietrich, W.; Roessler, K.; Pfisterer, W.; Ungersboeck, K.; Heimberger, K.; Kitz, K. Gamma Knife Radiosurgery of Skull Base Meningiomas. Acta Neurochir. 2000, 142, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, J.P.; Starke, R.M.; Kano, H.; Barnett, G.H.; Mathieu, D.; Chiang, V.; Yu, J.B.; Hess, J.; McBride, H.L.; Honea, N.; et al. Gamma Knife Radiosurgery for Posterior Fossa Meningiomas: A Multicenter Study. J. Neurosurg. 2015, 122, 1479–1489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Starke, R.M.; Nguyen, J.H.; Rainey, J.; Williams, B.J.; Sherman, J.H.; Savage, J.; Yen, C.P.; Sheehan, J.P. Gamma Knife Surgery of Meningiomas Located in the Posterior Fossa: Factors Predictive of Outcome and Remission: Clinical Article. J. Neurosurg. 2011, 114, 1399–1409. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, J.; Starke, R.; Nguyen, J.; Reames, D.; Rainey, J. Gamma Knife Radiosurgery of Meningiomas Involving the Foramen Magnum. J. Craniovertebral Junction Spine 2010, 1, 23. [Google Scholar] [CrossRef]
- Malik, I.; Rowe, J.; Walton, L.; Radatz, M.; Kemeny, A. The Use of Stereotactic Radiosurgery in the Management of Meningiomas. Br. J. Neurosurg. 2005, 19, 13–20. [Google Scholar] [CrossRef]
- Stieber, V.W. Radiation Therapy for Visual Pathway Tumors. J. Neuroophthalmol. 2008, 28, 222–230. [Google Scholar] [CrossRef]
- Goldbrunner, R.; Minniti, G.; Preusser, M.; Jenkinson, M.D.; Sallabanda, K.; Houdart, E.; von Deimling, A.; Stavrinou, P.; Lefranc, F.; Lund-Johansen, M.; et al. EANO Guidelines for the Diagnosis and Treatment of Meningiomas. Lancet Oncol. 2016, 17, e383–e391. [Google Scholar] [CrossRef] [Green Version]
- Aboukais, R.; Zairi, F.; Lejeune, J.-P.; Le Rhun, E.; Vermandel, M.; Blond, S.; Devos, P.; Reyns, N. Grade 2 Meningioma and Radiosurgery. J. Neurosurg. 2015, 122, 1157–1162. [Google Scholar] [CrossRef] [Green Version]
- Aboukais, R.; Zairi, F.; Reyns, N.; Le Rhun, E.; Touzet, G.; Blond, S.; Lejeune, J.-P. Surgery Followed by Radiosurgery: A Deliberate Valuable Strategy in the Treatment of Intracranial Meningioma. Clin. Neurol. Neurosurg. 2014, 124, 123–126. [Google Scholar] [CrossRef]
- Hasseleid, B.F.; Meling, T.R.; Rønning, P.; Scheie, D.; Helseth, E. Surgery for Convexity Meningioma: Simpson Grade I Resection as the Goal: Clinical Article. J. Neurosurg. 2012, 117, 999–1006. [Google Scholar] [CrossRef]
- Aboukais, R.; Baroncini, M.; Zairi, F.; Reyns, N.; Lejeune, J.-P. Early Postoperative Radiotherapy Improves Progression Free Survival in Patients with Grade 2 Meningioma. Acta Neurochir. 2013, 155, 1385–1390. [Google Scholar] [CrossRef]
- Adeberg, S.; Hartmann, C.; Welzel, T.; Rieken, S.; Habermehl, D.; von Deimling, A.; Debus, J.; Combs, S.E. Long-Term Outcome after Radiotherapy in Patients with Atypical and Malignant Meningiomas—Clinical Results in 85 Patients Treated in a Single Institution Leading to Optimized Guidelines for Early Radiation Therapy. Int. J. Radiat. Oncol. 2012, 83, 859–864. [Google Scholar] [CrossRef]
- Cohen-Inbar, O.; Lee, C.; Schlesinger, D.; Xu, Z.; Sheehan, J.P. Long-Term Results of Stereotactic Radiosurgery for Skull Base Meningiomas. Neurosurgery 2016, 79, 58–68. [Google Scholar] [CrossRef]
- Talacchi, A.; Hasanbelliu, A.; D’Amico, A.; Regge Gianas, N.; Locatelli, F.; Pasqualin, A.; Longhi, M.; Nicolato, A. Long-Term Follow-up after Surgical Removal of Meningioma of the Inner Third of the Sphenoidal Wing: Outcome Determinants and Different Strategies. Neurosurg. Rev. 2020, 43, 109–117. [Google Scholar] [CrossRef]
- Hardesty, D.A.; Wolf, A.B.; Brachman, D.G.; McBride, H.L.; Youssef, E.; Nakaji, P.; Porter, R.W.; Smith, K.A.; Spetzler, R.F.; Sanai, N. The Impact of Adjuvant Stereotactic Radiosurgery on Atypical Meningioma Recurrence Following Aggressive Microsurgical Resection: Clinical Article. J. Neurosurg. 2013, 119, 475–481. [Google Scholar] [CrossRef] [Green Version]
- Frostell, A.; Hakim, R.; Dodoo, E.; Sinclair, G.; Ohlsson, M.; Förander, P.; Milovac, B.; Brundin, L.; Svensson, M. Adjuvant Stereotactic Radiosurgery Reduces Need for Retreatments in Patients with Meningioma Residuals. World Neurosurg. 2016, 88, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Iwai, Y.; Yamanaka, K.; Ikeda, H. Gamma Knife Radiosurgery for Skull Base Meningioma: Long-Term Results of Low-Dose Treatment: Clinical Article. J. Neurosurg. 2008, 109, 804–810. [Google Scholar] [CrossRef]
- Kondziolka, D.; Mathieu, D.; Lunsford, L.D.; Martin, J.J.; Madhok, R.; Niranjan, A.; Flickinger, J.C. Radiosurgery as Definitive Management of Intracranial Meningiomas. Neurosurgery 2008, 62, 53–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kondziolka, D.; Patel, A.D.; Kano, H.; Flickinger, J.C.; Lunsford, L.D. Long-Term Outcomes after Gamma Knife Radiosurgery for Meningiomas. Am. J. Clin. Oncol. 2016, 39, 453–457. [Google Scholar] [CrossRef]
- McClelland, S.; Ciporen, J.N.; Mitin, T.; Jaboin, J.J. Long-Term Stroke Risk of Single-Fraction Photon-Based Stereotactic Radiosurgery for Meningioma. Clin. Neurol. Neurosurg. 2018, 173, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Mason, W.P.; Gentili, F.; Macdonald, D.R.; Hariharan, S.; Cruz, C.R.; Abrey, L.E. Stabilization of Disease Progression by Hydroxyurea in Patients with Recurrent or Unresectable Meningioma. J. Neurosurg. 2002, 97, 341–346. [Google Scholar] [CrossRef]
- Rosenthal, M.A.; Ashley, D.L.; Cher, L. Treatment of High Risk or Recurrent Meningiomas with Hydroxyurea. J. Clin. Neurosci. Off. J. Neurosurg. Soc. Australas. 2002, 9, 156–158. [Google Scholar] [CrossRef]
- Newton, H.B.; Scott, S.R.; Volpi, C. Hydroxyurea Chemotherapy for Meningiomas: Enlarged Cohort with Extended Follow-Up. Br. J. Neurosurg. 2004, 18, 495–499. [Google Scholar] [CrossRef] [PubMed]
- Mazza, E.; Brandes, A.; Zanon, S.; Eoli, M.; Lombardi, G.; Faedi, M.; Franceschi, E.; Reni, M. Hydroxyurea with or without Imatinib in the Treatment of Recurrent or Progressive Meningiomas: A Randomized Phase II Trial by Gruppo Italiano Cooperativo Di Neuro-Oncologia (GICNO). Cancer Chemother. Pharmacol. 2016, 77, 115–120. [Google Scholar] [CrossRef]
- Chamberlain, M.C. Adjuvant Combined Modality Therapy for Malignant Meningiomas. J. Neurosurg. 1996, 84, 733–736. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, J.W.; Crowley, J.; Eyre, H.J.; Stafford, B.; Jaeckle, K.A.; Townsend, J.J. A Phase II Evaluation of Tamoxifen in Unresectable or Refractory Meningiomas: A Southwest Oncology Group Study. J. Neurooncol. 1993, 15, 75–77. [Google Scholar] [CrossRef]
- Ji, Y.; Rankin, C.; Grunberg, S.; Sherrod, A.E.; Ahmadi, J.; Townsend, J.J.; Feun, L.G.; Fredericks, R.K.; Russell, C.A.; Kabbinavar, F.F.; et al. Double-Blind Phase III Randomized Trial of the Antiprogestin Agent Mifepristone in the Treatment of Unresectable Meningioma: SWOG S9005. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015, 33, 4093–4098. [Google Scholar] [CrossRef]
- Touat, M.; Lombardi, G.; Farina, P.; Kalamarides, M.; Sanson, M. Successful Treatment of Multiple Intracranial Meningiomas with the Antiprogesterone Receptor Agent Mifepristone (RU486). Acta Neurochir. 2014, 156, 1831–1835. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, M.C.; Glantz, M.J.; Fadul, C.E. Recurrent Meningioma: Salvage Therapy with Long-Acting Somatostatin Analogue. Neurology 2007, 69, 969–973. [Google Scholar] [CrossRef] [PubMed]
- Simo, M.; Argyriou, A.A.; Macia, M.; Plans, G.; Majos, C.; Vidal, N.; Gil, M.; Bruna, J. Recurrent High-Grade Meningioma: A Phase II Trial with Somatostatin Analogue Therapy. Cancer Chemother. Pharmacol. 2014, 73, 919–923. [Google Scholar] [CrossRef]
- Graillon, T.; Sanson, M.; Campello, C.; Idbaih, A.; Peyre, M.; Peyrière, H.; Basset, N.; Autran, D.; Roche, C.; Kalamarides, M.; et al. Everolimus and Octreotide for Patients with Recurrent Meningioma: Results from the Phase II CEVOREM Trial. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2020, 26, 552–557. [Google Scholar] [CrossRef]
- Kaley, T.J.; Wen, P.; Schiff, D.; Ligon, K.; Haidar, S.; Karimi, S.; Lassman, A.B.; Nolan, C.P.; DeAngelis, L.M.; Gavrilovic, I.; et al. Phase II Trial of Sunitinib for Recurrent and Progressive Atypical and Anaplastic Meningioma. Neuro-Oncology 2015, 17, 116–121. [Google Scholar] [CrossRef] [Green Version]
- Nayak, L.; Iwamoto, F.M.; Rudnick, J.D.; Norden, A.D.; Lee, E.Q.; Drappatz, J.; Omuro, A.; Kaley, T.J. Atypical and Anaplastic Meningiomas Treated with Bevacizumab. J. Neurooncol. 2012, 109, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Grimm, S.A.; Kumthekar, P.; Chamberlain, M.C.; Schiff, D.; Wen, P.Y.; Iwamoto, F.M.; Reardon, D.A.; Purow, B.; Raizer, J.J. Phase II Trial of Bevacizumab in Patients with Surgery and Radiation Refractory Progressive Meningioma. J. Clin. Oncol. 2015, 33, 2055. [Google Scholar] [CrossRef]
- Shih, K.C.; Chowdhary, S.; Rosenblatt, P.; Weir, A.B., 3rd; Shepard, G.C.; Williams, J.T.; Shastry, M.; Burris, H.A., 3rd; Hainsworth, J.D. A Phase II Trial of Bevacizumab and Everolimus as Treatment for Patients with Refractory, Progressive Intracranial Meningioma. J. Neurooncol. 2016, 129, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Scerrati, A.; Mongardi, L.; Visani, J.; Lofrese, G.; Cavallo, M.A.; Fiorentino, A.; De Bonis, P. The Controversial Role of Bevacizumab in the Treatment of Patients with Intracranial Meningioma: A Comprehensive Literature Review. Expert Rev. Anticancer Ther. 2020, 20, 197–203. [Google Scholar] [CrossRef]
- Raizer, J.J.; Grimm, S.A.; Rademaker, A.; Chandler, J.P.; Muro, K.; Helenowski, I.; Rice, L.; McCarthy, K.; Johnston, S.K.; Mrugala, M.M.; et al. A Phase II Trial of PTK787/ZK 222584 in Recurrent or Progressive Radiation and Surgery Refractory Meningiomas. J. Neurooncol. 2014, 117, 93–101. [Google Scholar] [CrossRef]
- Plotkin, S.; Jordan, J.; Beauchamp, R.; Muzikansky, A.; Stemmer-Rachamimov, A.; Ramesh, V. ACTR-36. A Single Arm Phase 2 Study of the Dual Mtorc1/Mtorc2 Inhibitor Vistusertib Provided on an Intermittent Schedule FOR Neurofibromatosis 2 Patients with Progressive or Symptomatic Meningiomas. Neuro-Oncology 2018, 20, vi19. [Google Scholar] [CrossRef] [Green Version]
- Demetri, G.D.; von Mehren, M.; Jones, R.L.; Hensley, M.L.; Schuetze, S.M.; Staddon, A.; Milhem, M.; Elias, A.; Ganjoo, K.; Tawbi, H.; et al. Efficacy and Safety of Trabectedin or Dacarbazine for Metastatic Liposarcoma or Leiomyosarcoma After Failure of Conventional Chemotherapy: Results of a Phase III Randomized Multicenter Clinical Trial. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2016, 34, 786–793. [Google Scholar] [CrossRef] [PubMed]
- Monk, B.J.; Herzog, T.J.; Kaye, S.B.; Krasner, C.N.; Vermorken, J.B.; Muggia, F.M.; Pujade-Lauraine, E.; Lisyanskaya, A.S.; Makhson, A.N.; Rolski, J.; et al. Trabectedin plus Pegylated Liposomal Doxorubicin in Recurrent Ovarian Cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2010, 28, 3107–3114. [Google Scholar] [CrossRef] [PubMed]
- Preusser, M.; Silvani, A.; Le Rhun, E.; Soffietti, R.; Lombardi, G.; Sepúlveda, J.M.; Brandal, P.; Beaney, R.P.; Bonneville-Levard, A.; Lorgis, V.; et al. Trabectedin for Recurrent WHO Grade II or III Meningioma: A Randomized Phase II Study of the EORTC Brain Tumor Group (EORTC-1320-BTG). J. Clin. Oncol. 2019, 37, 2007. [Google Scholar] [CrossRef]
- Zhao, L.; Zhao, W.; Hou, Y.; Wen, C.; Wang, J.; Wu, P.; Guo, Z. An Overview of Managements in Meningiomas. Front. Oncol. 2020, 10, 1523. [Google Scholar] [CrossRef] [PubMed]
- Kim, L. A Narrative Review of Targeted Therapies in Meningioma. Chin. Clin. Oncol. 2020, 9, 76. [Google Scholar] [CrossRef] [PubMed]


| Skull Base Region | Location | Incidence | Surgical Approaches | IONM | Surgical Pitfalls | Complications | ||
|---|---|---|---|---|---|---|---|---|
| Vascular | Nerves | Others | Clinical Manifestations | |||||
| Anterior Fossa 4, 27–36,49,51 | Olfactory Groove Meningiomas | 8–13% | Subfrontal approach Transbasal Approach Pterional approach Fronto-lateral approach Supraorbital keyhole Endoscopic endonasal approach *Transfacial reconstitutive approach also known as facial translocation, further subdivided into:
| EEG, MEPs, SSEPs, VEPs (in selected cases) | branches of the OA, ICA, ACoA, A2 Ethmoidal arteries | CN I, II, III, IV | EOM | Anosmia, CSF leak Visual disturbances (diplopia, anopsia, eye globe injury) Hemorrhage Hemorrhage, epiphora, diplopia and dystopia, soft tissue swelling, ectropion (associated with Weber–Ferguson incision). Poor bone consolidation, misalignment (related to bad osteosynthesis), wound dehiscence (cutaneous and intraoral) |
| Sphenoid wing Meningiomas | 11–20% | Pterional approach Fronto-temporal-orbito-zygomatic approach Lateral, superior, medial orbitotomy | anterior circulation arteries Ethmoidal artery in medial accesses | CN II, III, VI supraorbital nerve, facial nerve | EOM, medial and lateral canthal tendons | |||
| Tuberculum Sellae/Planum Meningiomas | 5–10% | Pterional approach Endoscopic endonasal approach Supraorbital key-hole | Anterior circulation arteries | CN II, III, IV, V, VI | aesthetic orbital reconstruction | |||
| Cavernous Sinus Meningiomas | 1% | Pterional approach Fronto-temporo-orbito- Zygomatic approach | Anterior circulation arteries | CN II, III, IV, V, VI | ||||
| Middle Fossa 4,35,44 | Middle fossa and Sphenoid wing | 1.1–1.4% | Pterional approach (anterolateral approach) Fronto-temporo-orbito- zygomatic | EEG, MEPs, SSEPs EMG CNs III, IV, VI can be considered | ICA Vein of Labbè | CN II, III, IV, V, VI | Temporal lobe | Language deficit, hemiparesis, hemianopsia, hemorrhages, temporal lobe edema, trigeminal anesthesia, |
| Middle fossa and cavernous sinus | ||||||||
| Middle fossa with infratemporal extension | Subtemporal approach (lateral approach) | |||||||
| Middle fossa and petrous ridge | ||||||||
| Posterior Fossa 4,35,38–43,45,46,51 | Cerebellopontine Angle | 10% | Anterior Petrosectomy Approach Posterior and Combined Petrosal Approaches Retrolabyrinthine Approach Translabyrinthine Approach Combined Petrosal Approach Retrosigmoid approach | EEG, MEPs, SSEPs, CB-MEP (CN VII) EMG (CNs VI, VII) BAERs | Intrapetrous ICA, SCA and AICA encasement | CN V, VI, VII, VIII | Brainstem adhesion | Brain steam and cerebellum edema, CSF leak Venous infarction Cranial nerve injury Vertebral artery injury, Hydrocephalus, CSF leak Infection Hemorrhage, cerebrospinal fluid leakage, soft tissue edema of the oral cavity, infection, wound dehiscence, velopalatine dysfunction, malocclusion, dysphagia, malocclusion when osteotomies are required, oro-nasal fistula, laceration of nasal mucosa, lesion of teeth apices |
| Foramen Magnum | 2.5% | Posterior Suboccipital Approach with C1 laminectomy; Far Lateral Approach Extreme Lateral Approach | EEG, MEPs, SSEPs, CB-MEP (CN VII, IX, X, XI, XII) EMG (CNs VI, VII, IX, X, XI, XII) BAERs | VA encasement JV encasement | CN IX, X, XI, XII | Brainstem adhesion Extradural extension | ||
| Clival Meningiomas | <1% | Retrosigmoid approach Petrosal approach Transoral:
far-lateral approach Endoscopic approach | Internal maxillary artery Palatine artery | CN VI, VII, VIII, XI, X, XI, XII | Brainstem adhesion | |||
| Petroclival Meningiomas | 2% of posterior fossa meningiomas | Retrosigmoid approach Combined transpetrosal Retrolabyrinthine Approach Translabyrinthine Approach | BA BA perforating arteries | CN V, VI, VII, VIII | Brainstem adhesion | |||
| Altered Gene | Preferential Tumor Localization | Main Histotype |
|---|---|---|
| NF2 | Posterior and lateral skull base | Fibrous, Transitional, Atypical |
| AKT1, PI3K | Anterior and middle skull base | Meningothelial |
| SMO | Olfactory groove | Meningothelial * |
| TRAF7/KLF4 | Middle skull base | Meningothelial, Secretory for co-occurring TRAF7/KLF4 |
| POL2RA | Tuberculum sellae | Meningothelial |
| Authors | Patients (N) | Radiation Modality | Median Dose/ Dose per Fraction (Gy) | Median Volume (mL) | Median Follow-Up (Months) | Local Control | Late Toxicity (%) |
|---|---|---|---|---|---|---|---|
| Goldsmith et al., 1994 [79] | 117 | CRT | 54 | NA | 40 | 89 at 5 and 77 at 10 years | 3.6 |
| Maire et al., 1995 [80] | 91 | CRT | 52 | NA | 40 | 94 | 6.5 |
| Nutting et al., 1999 [81] | 82 | CRT | 55–60 | NA | 41 | 92 at 5 and 83 at 10 years | 14 |
| Vendrely et al., 1999 [82] | 156 | 3D-RT | 50 | NA | 40 | 79 at 5 years | 11.5 |
| Mendenhall et al., 2003 [83] | 101 | 3D-RT | 54 | NA | 64 | 95 at 5, 92 at 10 and 15 years | 8 |
| Henzel et al., 2006 [93] | 84 | fSRT | 56 | 11,1 | 30 | 100 | NA |
| Tanzler et al., 2010 [94] | 144 | fSRT | 52.7 | NA | 87 | 97 at 5 and 95 at 10 years | 7 |
| Minniti et al., 2011 [95] | 52 | fSRT | 50 | 35.4 | 42 | 93 at 5 years | 5.5 |
| Slater et al., 2012 [101] | 68 | Protons | 56 | 27.6 | 74 | 99 at 5 years | 9 |
| Weber et al., 2012 [102] | 24 | Protons | 56/1.8–2.0 | 21.5 | 62 | 100 at 5 years | 15.5 |
| Solda et al., 2013 [96] | 222 | fSRT | 50/55 | 12 | 43 | 100 at 5 and 10 years | 4.5 |
| Combs et al., 2013 [97] | 507 | fSRT/IMRT | 57.6/1.8–2.0 | 53.4 | 107 | 95.5 at 5 and 88 at 10 years | 1.8 |
| Fokas et al., 2014 [98] | 253 * | fSRT | 55.8/1.8–2.0 | 16 | 50 | 92.9 at 5 and 87.5 at 10 years | 12 (G2) |
| Han et al., 2014 [100] | 143 | fSRT | 50.4/1.8 | 11.1 | 32 | 95% | 0.7 |
| Kaul et al., 2014 [104] | 136 | fSRT | 57/1.8–2.0 | 24 | 44.9 | 93.8 at 5 and 91.5 at 10 years | G1 only |
| Sanford et al., 2017 [103] | 44 | Protons | 55.8–63 | 39.7/13.2 | 195 | 98 at 10 and 90 at 15 years | 59% (≥G2) |
| Lillie O’steen et al., 2019 [84] | 149 | 3D-RT | 50–52/1.7–1.8 | NA | 144 | 95 at 10 and 92 at 20 years | NA |
| Authors | Patients (N) | Technique | Median Dose (Gy)/Fractions | Median Volume (mL) | Median Follow-Up (Months) | Local Control | Late Toxicity |
|---|---|---|---|---|---|---|---|
| Colombo et al., 2009 [108] | 150 * | CK | 16–25/2–5 | 7.5 (0.1–64) | 30 | 96 | 3.5 |
| Fokas et al., 2014 [98] | 49 * | LINAC | 25–35/5 | 6.11 (1.9–35.7) | 50 | 92.9 at 5 and 87.5 at 10 years | 12 (G2) |
| Han et al., 2014 [100] | 22 * | LINAC | 25/5 | 4.8 (0.88–20.38) | 32 | 95 | 0.7 |
| Navarria et al., 2015 [109] | 26 | LINAC | 25/5 | 13° | 24.5 | 93% at 2 years | G3, none |
| Marchetti et al., 2016 [110] | 143 | CK | 21–25/2–5 | 8 (0.1–126.3) | 44 | 93 at 5 years | 5.1 |
| Marchetti et al., 2019 [111] | 168 | CK | 25/5 | 7.3 (0.1–76.8) | 51 | 94% at 5 years | 3.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ius, T.; Tel, A.; Minniti, G.; Somma, T.; Solari, D.; Longhi, M.; De Bonis, P.; Scerrati, A.; Caccese, M.; Barresi, V.; et al. Advances in Multidisciplinary Management of Skull Base Meningiomas. Cancers 2021, 13, 2664. https://doi.org/10.3390/cancers13112664
Ius T, Tel A, Minniti G, Somma T, Solari D, Longhi M, De Bonis P, Scerrati A, Caccese M, Barresi V, et al. Advances in Multidisciplinary Management of Skull Base Meningiomas. Cancers. 2021; 13(11):2664. https://doi.org/10.3390/cancers13112664
Chicago/Turabian StyleIus, Tamara, Alessandro Tel, Giuseppe Minniti, Teresa Somma, Domenico Solari, Michele Longhi, Pasquale De Bonis, Alba Scerrati, Mario Caccese, Valeria Barresi, and et al. 2021. "Advances in Multidisciplinary Management of Skull Base Meningiomas" Cancers 13, no. 11: 2664. https://doi.org/10.3390/cancers13112664







