A Multicenter Analysis of the Outcome of Cancer Patients with Neutropenia and COVID-19 Optionally Treated with Granulocyte-Colony Stimulating Factor (G-CSF): A Comparative Analysis
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Descriptive Analysis of Baseline Clinical Characteristics
3.2. Descriptive Analysis of COVID-19 Disease and Treatments
3.3. Descriptive Analysis of Neutropenia Characteristics and G-CSF Administration
3.4. Bivariate Analyses of COVID-19 Infection in Patients with Neutropenia: Death Risk Factors
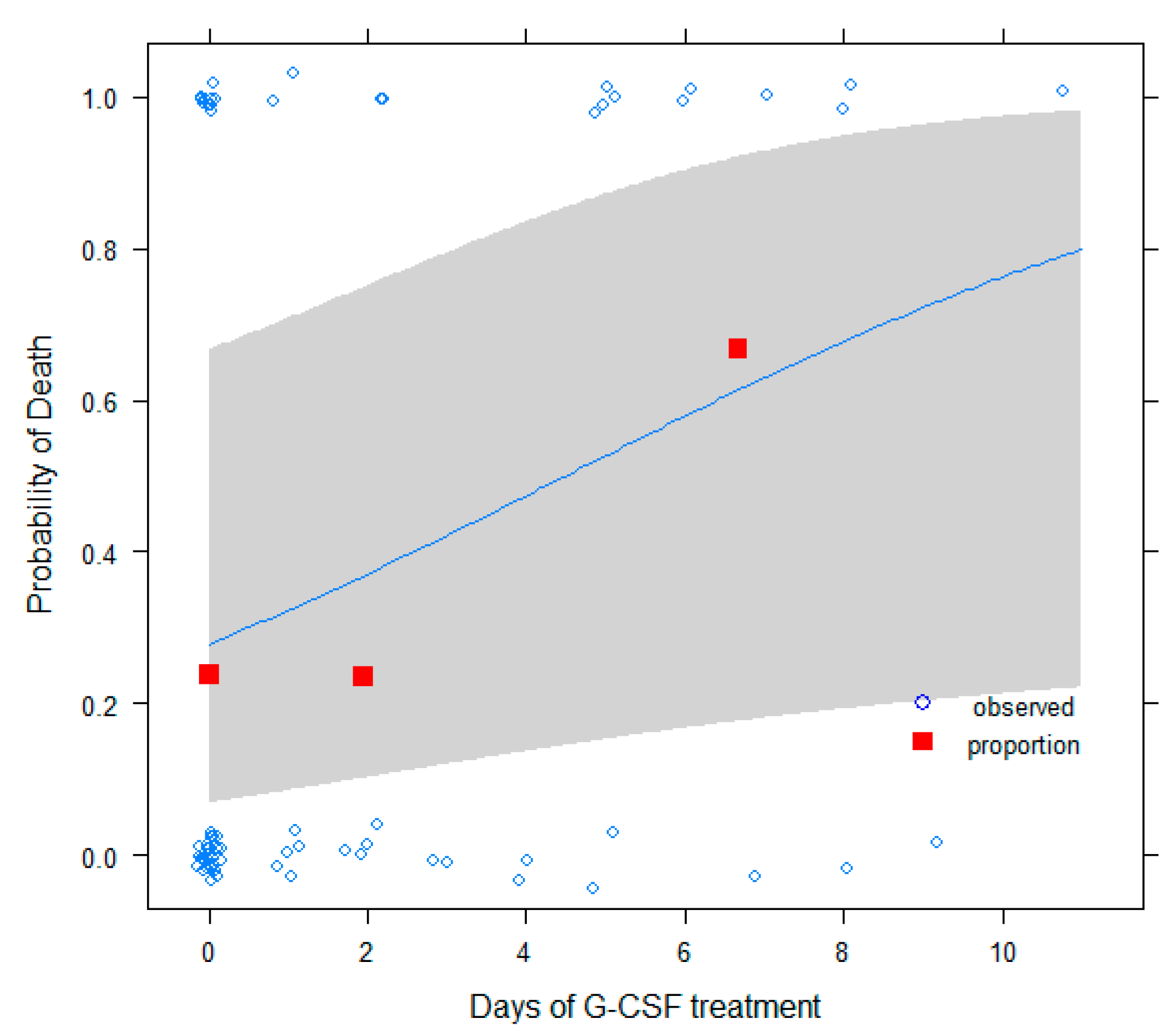
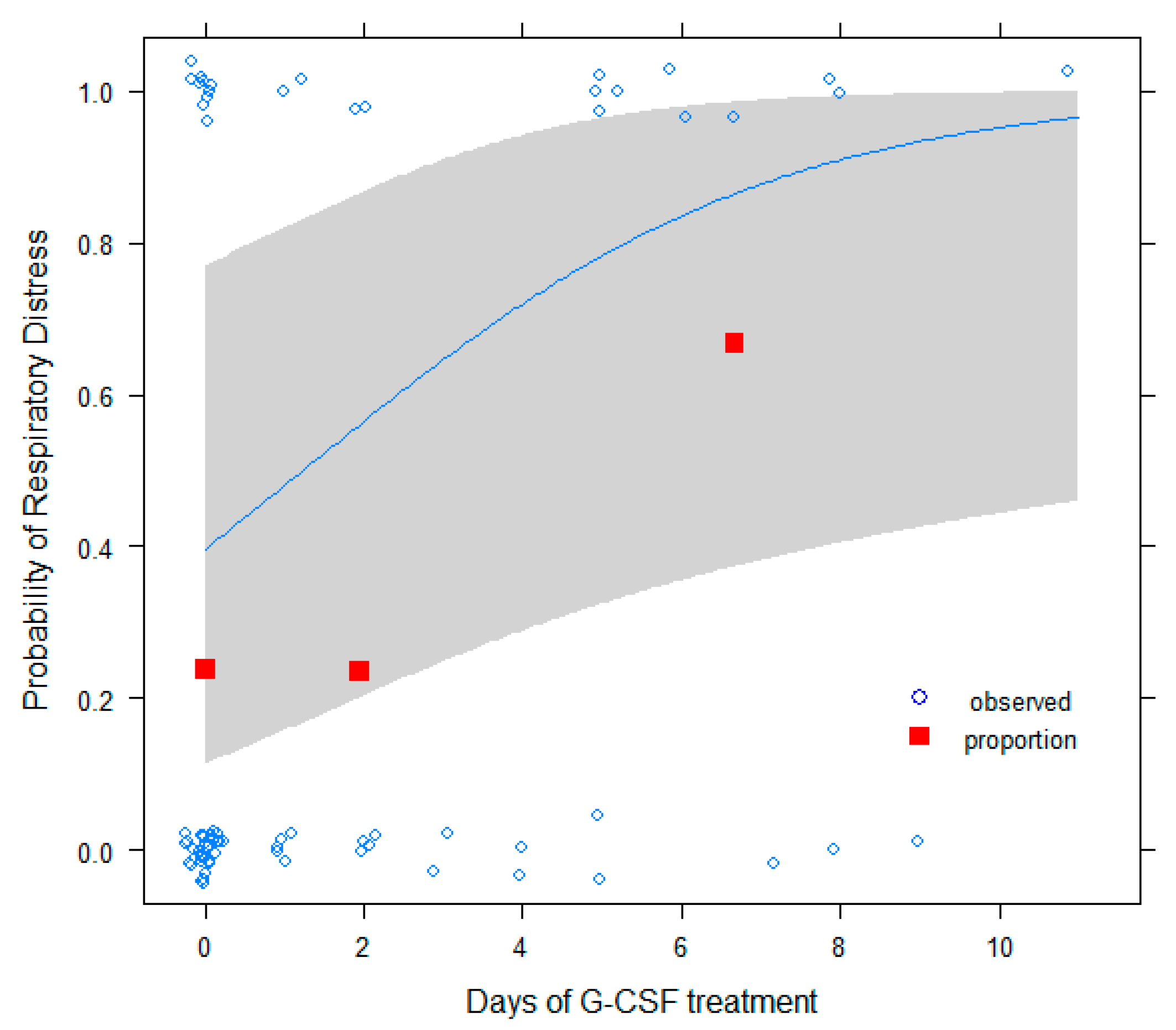
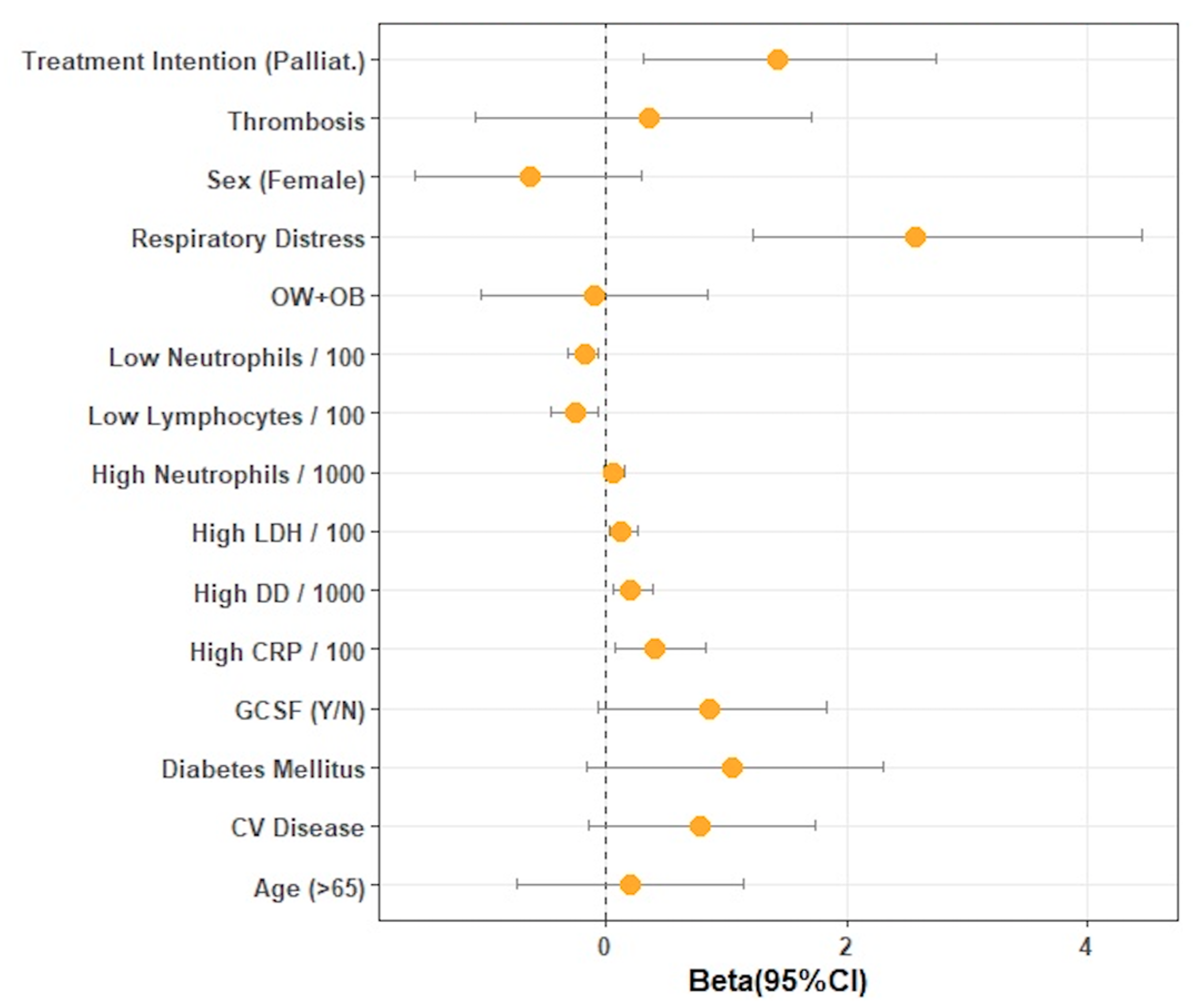
3.5. A Multivariable Model to Test the Effect of G-CSF on COVID-19 Severity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Chen, N.; Zhou, M. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Crisci, C.D.; Ardusso, L.R.F. Precision Medicine Approach to SARS-CoV-2 Pandemic Management. Curr. Treat. Options Allergy 2020, 8, 1–19. [Google Scholar] [CrossRef]
- Vijayvargiya, P.; Esquer Garrigos, Z. Treatment Considerations for COVID-19: A Critical Review of the Evidence (or Lack Thereof). Mayo Clin. Proc. 2020, 95, 1454–1466. [Google Scholar] [CrossRef]
- Qin, C.; Zhou, L.; Hu, Z.; Zhang, S.; Yang, S.; Tao, Y.; Xie, C.; Ma, K.; Shang, K.; Wang, W.; et al. Dysregulation of Immune Response in Patients with Coronavirus 2019 (COVID-19) in Wuhan, China. Clin. Infect. Dis. 2020, 71, 762–768. [Google Scholar] [CrossRef]
- Delang, L.; Neyts, J. Medical treatment options for COVID-19. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhu, F.; Xie, L.; Wang, C.; Wang, J.; Chen, R.; Jia, P.; Guan, H.Q.; Peng, L.; Chen, Y.; et al. Clinical characteristics of COVID-19-infected cancer patients: A retrospective case study in three hospitals within Wuhan, China. Ann. Oncol. 2020, 31, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Ouyang, W.; Chua, M.L.K.; Xie, C. SARS-CoV-2 Transmission in Patients with Cancer at a Tertiary Care Hospital in Wuhan, China. JAMA Oncol. 2020, 7, 1108–1110. [Google Scholar] [CrossRef]
- Kim, J.S.; Lee, K.H.; Kim, G.E.; Kim, S.; Yang, J.W.; Li, H.; Hong, S.H.; Ghayda, R.A.; Kronbichler, A.; Koyanagi, A.; et al. Clinical characteristics and mortality of patients with hematologic malignancies and COVID-19: A systematic review. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 11926–11933. [Google Scholar] [PubMed]
- El Gohary, G.M.; Hashmi, S.; Styczynski, J.; Kharfan-Dabaja, M.A.; Alblooshi, R.M.; de la Cámara, R.; Mohamed, S.; Alshaibani, A.; Cesaro, S.; El-Aziz, N.A.; et al. The risk and prognosis of COVID-19 infection in cancer patients: A systematic review and meta-analysis. Hematol. Stem Cell Ther. 2020, 30, 1206–1213. [Google Scholar] [CrossRef]
- Liang, W.; Guan, W. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020, 21, 335–337. [Google Scholar] [CrossRef]
- Kasi, P.M.; Grothey, A. Chemotherapy-Induced Neutropenia as a Prognostic and Predictive Marker of Outcomes in Solid-Tumor Patients. Drugs 2018, 78, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Felsenstein, S.; Herbert, J.; McNamara, P.S.; Hedrich, C.M. COVID-19: Immunology and treatment options. Clin. Immunol. 2020, 215, 108448. [Google Scholar] [CrossRef]
- Aapro, M.; Bohlius, J.; Cameron, D.; Lago, L.D.; Donnelly, J.P.; Kearney, N.; Lyman, G.; Pettengell, R.; Tjan-Heijnen, V.; Walewski, J.; et al. 2010 update of EORTC guidelines for the use of granulocyte-colony stimulating factor to reduce the incidence of chemotherapy-induced febrile neutropenia in adult patients with lymphoproliferative disorders and solid tumours. Eur. J. Cancer 2011, 47, 8–32. [Google Scholar] [CrossRef] [PubMed]
- Wiedermann, F.J. Acute lung injury during G-CSF-induced neutropenia recovery: Effect of G-CSF on pro- and anti-inflammatory cytokines. Bone Marrow Transplant. 2005, 36, 731. [Google Scholar] [CrossRef][Green Version]
- Słomka, A.; Kowalewski, M.; Żekanowska, E. Coronavirus Disease 2019 (COVID–19): A Short Review on Hematological Manifestations. Pathogens 2020, 9, 493. [Google Scholar] [CrossRef] [PubMed]
- Taha, M.; Sharma, A.; Soubani, A. Clinical deterioration during neutropenia recovery after G-CSF therapy in patient with COVID-19. Respir. Med. Case Rep. 2020, 31, 101231. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Kuderer, N.M.; Choueiri, T.K.; Shah, D.P.; Shyr, Y.; Rubinstein, S.M.; Rivera, D.R.; Shete, S.; Hsu, C.-Y.; Desai, A.; de Lima Lopes, G.; et al. Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet 2020, 395, 1907–1918. [Google Scholar] [CrossRef]
- Zhang, A.W.; Morjaria, S.; Kaltsas, A.; Hohl, T.M.; Parameswaran, R.; Patel, D.; Zhou, W.; Predmore, J.; Perez-Johnston, R.; Jee, J.; et al. The Effect of Neutropenia and Filgrastim (G-CSF) in Cancer Patients With COVID-19 Infection. Clin. Infect. Dis. 2021, 15. [Google Scholar] [CrossRef]
- Fu, J.; Kong, J.; Wang, W.; Wu, M.; Yao, L.; Wang, Z.; Jin, J.; Wu, D.; Yu, X. The clinical implication of dynamic neutrophil to lymphocyte ratio and D-dimer in COVID-19: A retrospective study in Suzhou China. Thromb. Res. 2020, 192, 3–8. [Google Scholar] [CrossRef]
- Sun, S.; Cai, X.; Wang, H.; He, G.; Lin, Y.; Lu, B.; Chen, C.; Pan, Y.; Hu, X. Abnormalities of peripheral blood system in patients with COVID-19 in Wenzhou, China. Clin. Chim. Acta 2020, 507, 174–180. [Google Scholar] [CrossRef]
- Nawar, T.; Morjaria, S.; Kaltsas, A.; Patel, D.; Perez-Johnston, R.; Daniyan, A.F.; Mailankody, S.; Parameswaran, R. Granulocyte-colony stimulating factor in COVID-19: Is it stimulating more than just the bone marrow? Am. J. Hematol. 2020, 95, 210–213. [Google Scholar] [CrossRef]
- Guan, W.-J.; Ni, Z.-Y.; Hu, Y.; Liang, W.-H.; Ou, C.-Q.; He, J.-X.; Liu, L.; Shan, H.; Lei, C.-L.; Hui, D.S.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Zemans, R.L.; Matthay, M.A. What drives neutrophils to the alveoli in ARDS? Thorax 2017, 72, 1–3. [Google Scholar] [CrossRef]
- Balsat, M.; Xhaard, A.; Lengline, E.; Tavernier, E.; Cornillon, J.; Guyotat, D.; Darmon, M. Worsening of Respiratory Status during Neutropenia Recovery in Noncritically Ill Hematological Patients: Results of a Prospective Multicenter Study. Respiration 2015, 90, 229–234. [Google Scholar] [CrossRef]
- Fox, S.E.; Akmatbekov, A.; Harbert, J.L.; Li, G.; Brown, J.Q.; Heide, R.S.V. Pulmonary and cardiac pathology in African American patients with COVID-19: An autopsy series from New Orleans. Lancet Respir. Med. 2020, 8, 681–686. [Google Scholar] [CrossRef]
- Barnes, B.J.; Adrover, J.M.; Baxter-Stoltzfus, A.; Borczuk, A.; Cools-Lartigue, J.; Crawford, J.M.; Daßler-Plenker, J.; Guerci, P.; Huynh, C.; Knight, J.S.; et al. Targeting potential drivers of COVID-19: Neutrophil extracellular traps. J. Exp. Med. 2020, 217, e20200652. [Google Scholar] [CrossRef] [PubMed]
- Nicolai, L.; Leunig, A.; Brambs, S.; Kaiser, R.; Joppich, M.; Hoffknecht, M.; Gold, C.; Engel, A.; Polewka, V.; Muenchhoff, M.; et al. Vascular neutrophilic inflammation and immunothrombosis distinguish severe COVID-19 from influenza pneumonia. J. Thromb. Haemost. 2021, 19, 574–581. [Google Scholar] [CrossRef]
- Thålin, C.; Hisada, Y. Neutrophil Extracellular Traps: Villains and Targets in Arterial, Venous, and Cancer-Associated Thrombosis. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 1724–1738. [Google Scholar] [CrossRef]
- Yang, L.; Liu, Q.; Zhang, X.; Liu, X.; Zhou, B.; Chen, J.; Huang, D.; Li, J.; Li, H.; Chen, F.; et al. DNA of neutrophil extracellular traps promotes cancer metastasis via CCDC25. Nature 2020, 583, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Leppkes, M.; Knopf, J.; Naschberger, E.; Lindemann, A.; Singh, J.; Herrmann, I.; Stürzl, M.; Staats, L.; Mahajan, A.; Schauer, C.; et al. Vascular occlusion by neutrophil extracellular traps in COVID-19. EBioMedicine 2020, 58, 102925. [Google Scholar] [CrossRef] [PubMed]
- Middleton, E.A.; He, X.-Y.; Denorme, F.; Campbell, R.A.; Ng, D.; Salvatore, S.P.; Mostyka, M.; Baxter-Stoltzfus, A.; Borczuk, A.C.; Loda, M.; et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood 2020, 136, 1169–1179. [Google Scholar] [CrossRef]
- Wang, J.; Li, Q.; Yin, Y.; Zhang, Y.; Cao, Y.; Lin, X.; Huang, L.; Hoffmann, D.; Lu, M.; Qiu, Y. Excessive Neutrophils and Neutrophil Extracellular Traps in COVID-19. Front. Immunol. 2020, 11, 2063. [Google Scholar] [CrossRef]
- Skendros, P.; Mitsios, A.; Chrysanthopoulou, A.; Mastellos, D.C.; Metallidis, S.; Rafailidis, P.; Ntinopoulou, M.; Sertaridou, E.; Tsironidou, V.; Tsigalou, C.; et al. Complement and tissue factor–enriched neutrophil extracellular traps are key drivers in COVID-19 immunothrombosis. J. Clin. Investig. 2020, 130, 6151–6157. [Google Scholar] [CrossRef] [PubMed]
- Roberts, A.W. G-CSF: A key regulator of neutrophil production, but that’s not all! Growth Factors 2005, 23, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Sahu, K.K.; Siddiqui, A.D. From Hematologist’s desk: The effect of COVID-19 on the blood system. Am. J. Hematol. 2020, 95, E213–E215. [Google Scholar] [CrossRef]
- Mertens, J.; Laghrib, Y.; Kenyon, C. A Case of Steroid-Responsive, COVID-19 Immune Reconstitution Inflammatory Syndrome Following the Use of Granulocyte Colony-Stimulating Factor. Open Forum Infect. Dis. 2020, 7, ofaa326. [Google Scholar] [CrossRef] [PubMed]
- Moss, D.L.; Rappaport, J. The good, the bad and the ugly: G-CSF, ageing and neutrophils-Implications for severe COVID-19. J. Leukoc. Biol. 2021, 109, 1017. [Google Scholar] [CrossRef]
- Tralongo, A.C.; Danova, M. Granulocyte colony-stimulating factors (G-CSF) and COVID-19: A double-edged sword? Infez. Med. 2020, 28, 459–460. [Google Scholar]
- Lasagna, A.; Zuccaro, V.; Ferraris, E.; Rizzo, G.; Tancredi, R.J.; Pedrazzoli, P. How to Use Prophylactic G-CSF in the Time of COVID-19. JCO Oncol. Pract. 2020, 16, 771–772. [Google Scholar] [CrossRef]
- Lazarus, H.M.; Gale, R.P. Is G-CSF Dangerous in COVID-19: Why Not Use GM-CSF? Acta Haematol. 2021, 144, 350–351. [Google Scholar] [CrossRef]
- Chen, G.-B.; Lin, J.-T.; Zhang, Z.; Liu, L. Effect of recombinant human granulocyte colony-stimulating factor on lymphocyte subsets in patients with COVID-19. Infect. Dis. 2020, 52, 759–761. [Google Scholar] [CrossRef] [PubMed]
| Baseline Characteristics | Total | Without G-CSF | With G-CSF | p-Value |
|---|---|---|---|---|
| Age | 0.8 | |||
| <70 | 36 (43.4%) | 19 (44.2%) | 17 (42.5%) | |
| >70 | 47 (56.6%) | 24 (55.8%) | 23 (57.5%) | |
| Sex | 1 | |||
| Male | 41 (49.4%) | 21 (48.8%) | 20 (50%) | |
| Female | 42 (50.6%) | 22 (51.2%) | 20 (50%) | |
| ECOG | 0.15 | |||
| 0 | 24 (30%) | 14 (34%) | 10 (25.6%) | |
| 1 | 46 (37.5%) | 25 (61%) | 21 (53.8%) | |
| 2 | 9 (11.25%) | 2 (4.9%) | 7 (18%) | |
| 3 | 1 (1.25%) | 0 | 1 (2.6%) | |
| Cardiovascular disease * | 1 | |||
| No | 47 (57.3%) | 24 (57.14%) | 23 (57.5%) | |
| Yes | 35 (42.7%) | 18 (42.9%) | 17 (42.5%) | |
| Diabetes mellitus | 0.37 | |||
| No | 69 (84.1%) | 37 (88.1%) | 32 (80%) | |
| Yes | 13 (15.9%) | 5 (11.9%) | 8 (20%) | |
| Body Mass Index | 0.44 | |||
| <20 | 7 (10.1%) | 5 (16.13%) | 2 (5.26%) | |
| 20–25 | 25 (36.2%) | 9 (29%) | 16 (42.11%) | |
| 25–30 | 23 (33.3%) | 11 (35.5%) | 12 (31.6%) | |
| >30 | 14 (20.3%) | 6 (19.3%) | 8 (21%) | |
| Smoking | 0.57 | |||
| No | 34 (41.5%) | 17 (40.5%) | 17 (42.5%) | |
| Smoker | 17 (20.7%) | 7 (16.7%) | 10 (25%) | |
| Previous smoker | 31 (37.8%) | 18 (19.3%) | 13 (32.5%) | |
| Primary tumor | 0.66 | |||
| Lung | 22 (26.8%) | 11 (26.2%) | 11 (27.5%) | |
| Colorectal | 11 (13.4%) | 8 (19%) | 3 (7.5%) | |
| Other digestive | 14 (17.1%) | 5 (11.9%) | 9 (22.5%) | |
| Breast | 18 (22%) | 9 (21.4%) | 9 (22.5%) | |
| Gynecological | 6 (7.3%) | 4 (9.5%) | 2 (5%) | |
| Urothelial | 3 (3.7%) | 1 (2.4%) | 2 (5%) | |
| Sarcoma | 2 (2.4%) | 0 | 2 (5%) | |
| Head and neck | 5 (6.1%) | 3 (7.1%) | 2 (5%) | |
| Others | 1 (1.22%) | 1 (2.4%) | 0 | |
| Stage | 0.88 | |||
| II | 11 (13.4%) | 5 (11.9%) | 6 (15%) | |
| III | 16 (19.5%) | 9 (21.4%) | 7 (17.5%) | |
| IV | 55 (67.1%) | 28 (66.7%) | 27 (67.5%) | |
| Type of treatment | 0.001 | |||
| Chemotherapy | 63 (75.6%) | 25 (59.5%) | 38 (95%) | |
| Immunotherapy | 1 (1.2%) | 1 (2.4%) | 0 | |
| Chemoimmunotherapy | 15 (12.2%) | 13 (31%) | 2 (5%) | |
| Other | 3 (3.7%) | 3 (7.1%) | 0 | |
| Treatment intention | 1 | |||
| Curative | 27 (32.9%) | 14 (33.3%) | 13 (32.5%) | |
| Palliative | 55 (67.1%) | 28 (66.7%) | 27 (67.5%) |
| COVID-19 Features | Total | Without G-CSF | With G-CSF | p-Value |
|---|---|---|---|---|
| Respiratory failure | <0.001 | |||
| No | 30 (36.6%) | 23 (54.8%) | 7 (17.5%) | |
| Yes | 52 (63.4%) | 19 (45.2%) | 33 (82.5%) | |
| Oxygen support | 0.002 | |||
| No | 21 (25.6%) | 16 (38.1%) | 5 (12.5%) | |
| <35% | 30 (36.5%) | 17 (40.5%) | 13 (32.5%) | |
| 35-50% | 6 (7.3%) | 0 | 6 (15%) | |
| >50% | 25 (30.5%) | 9 (21.4%) | 16 (40%) | |
| Fever | 1 | |||
| No | 11 (13.4%) | 6 (14.3%) | 5 (12.5%) | |
| Yes | 71 (86.6%) | 36 (85.7%) | 35 (87.5%) | |
| Pneumonia | 0.38 | |||
| No | 19 (23.2%) | 12 (28.6%) | 7 (17.5%) | |
| Unilobar | 18 (22.4%) | 10 (23.8%) | 8 (20%) | |
| Multilobar/bilateral | 45 (54.9%) | 20 (47.6%) | 25 (62.5%) | |
| Thrombosis | 0.18 | |||
| No | 73 (87.9%) | 40 (93.02%) | 33 (82.5%) | |
| Suspicious/confirmed | 10 (12.1%) | 3 (6.98%) | 7 (17.5%) | |
| In-hospital days (mean ± SD) | 11.9 ± 9.6 | 10.6 ± 7 | 13.6 ± 11.6 | 0.09 |
| Clinical evolution after neutropenia | 0.45 | |||
| Better/no changes | 62 (78.4%) | 34 (79.07%) | 28 (70%) | |
| Worse | 17 (21.5%) | 9 (20.93%) | 12 (30%) | |
| Death | 0.1 | |||
| Yes | 27 (32.9%) | 10 (23.8%) | 17 (42.5%) | |
| No | 55 (67.1%) | 32 (76.19%) | 26 (57.5%) | |
| Evolution after discharge *: | 0.25 | |||
| -No change of treatment | 37 (68.5%) | 24 (75%) | 13 (59.1%) | |
| -Change of treatment | 19 (31.5%) | 8 (25%) | 9 (40.9%) |
| Neutropenia and Inflammation Variables | Total | Without G-CSF | With G-CSF | p-Value |
|---|---|---|---|---|
| Lowest neutrophils count | 616 ± 419 | 691 ± 369 | 541 ± 457 | 0.11 |
| Highest neutrophils count | 5423 ± 5078 | 3409 ± 2973 | 7538 ± 5940 | <0.001 |
| Lowest lymphocyte count | 473 ± 310 | 467 ± 269 | 469 ± 356 | 0.77 |
| Highest D-dymer | 4513 ± 10134 | 2401 ± 3180 | 7456 ± 14880 | 0.062 |
| Highest LDH | 685 ± 1410 | 585 ± 604 | 792 ± 1943 | 0.86 |
| Highest calcitonin | 2.5 ± 5.3 | 2.6 ± 6.2 | 2.4 ± 3.6 | 0.06 |
| Highest C-reactive protein | 115 ± 143 | 90 ± 140 | 143 ± 143 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sereno, M.; Jimenez-Gordo, A.M.; Baena-Espinar, J.; Aguado, C.; Mielgo, X.; Pertejo, A.; Álvarez-Álvarez, R.; Sánchez, A.; López, J.L.; Molina, R.; et al. A Multicenter Analysis of the Outcome of Cancer Patients with Neutropenia and COVID-19 Optionally Treated with Granulocyte-Colony Stimulating Factor (G-CSF): A Comparative Analysis. Cancers 2021, 13, 4205. https://doi.org/10.3390/cancers13164205
Sereno M, Jimenez-Gordo AM, Baena-Espinar J, Aguado C, Mielgo X, Pertejo A, Álvarez-Álvarez R, Sánchez A, López JL, Molina R, et al. A Multicenter Analysis of the Outcome of Cancer Patients with Neutropenia and COVID-19 Optionally Treated with Granulocyte-Colony Stimulating Factor (G-CSF): A Comparative Analysis. Cancers. 2021; 13(16):4205. https://doi.org/10.3390/cancers13164205
Chicago/Turabian StyleSereno, María, Ana María Jimenez-Gordo, Javier Baena-Espinar, Carlos Aguado, Xabier Mielgo, Ana Pertejo, Rosa Álvarez-Álvarez, Ana Sánchez, Jose Luis López, Raquel Molina, and et al. 2021. "A Multicenter Analysis of the Outcome of Cancer Patients with Neutropenia and COVID-19 Optionally Treated with Granulocyte-Colony Stimulating Factor (G-CSF): A Comparative Analysis" Cancers 13, no. 16: 4205. https://doi.org/10.3390/cancers13164205
APA StyleSereno, M., Jimenez-Gordo, A. M., Baena-Espinar, J., Aguado, C., Mielgo, X., Pertejo, A., Álvarez-Álvarez, R., Sánchez, A., López, J. L., Molina, R., López-Alfonso, A., Hernández, B., Chiara, L. E., Martín, A. M., López-Martín, A., Dorta, M., Collazo-Lorduy, A., Casado, E., de Molina, A. R., & Colmenarejo, G. (2021). A Multicenter Analysis of the Outcome of Cancer Patients with Neutropenia and COVID-19 Optionally Treated with Granulocyte-Colony Stimulating Factor (G-CSF): A Comparative Analysis. Cancers, 13(16), 4205. https://doi.org/10.3390/cancers13164205






