Carfilzomib, Lenalidomide, and Dexamethasone Followed by Salvage Autologous Stem Cell Transplant with or without Maintenance for Relapsed or Refractory Multiple Myeloma
Abstract
:Simple Summary
Abstract
1. Introduction
2. Patients and Methods
2.1. Patients
2.2. Assessments
2.3. Treatment
2.4. Statistics
3. Results
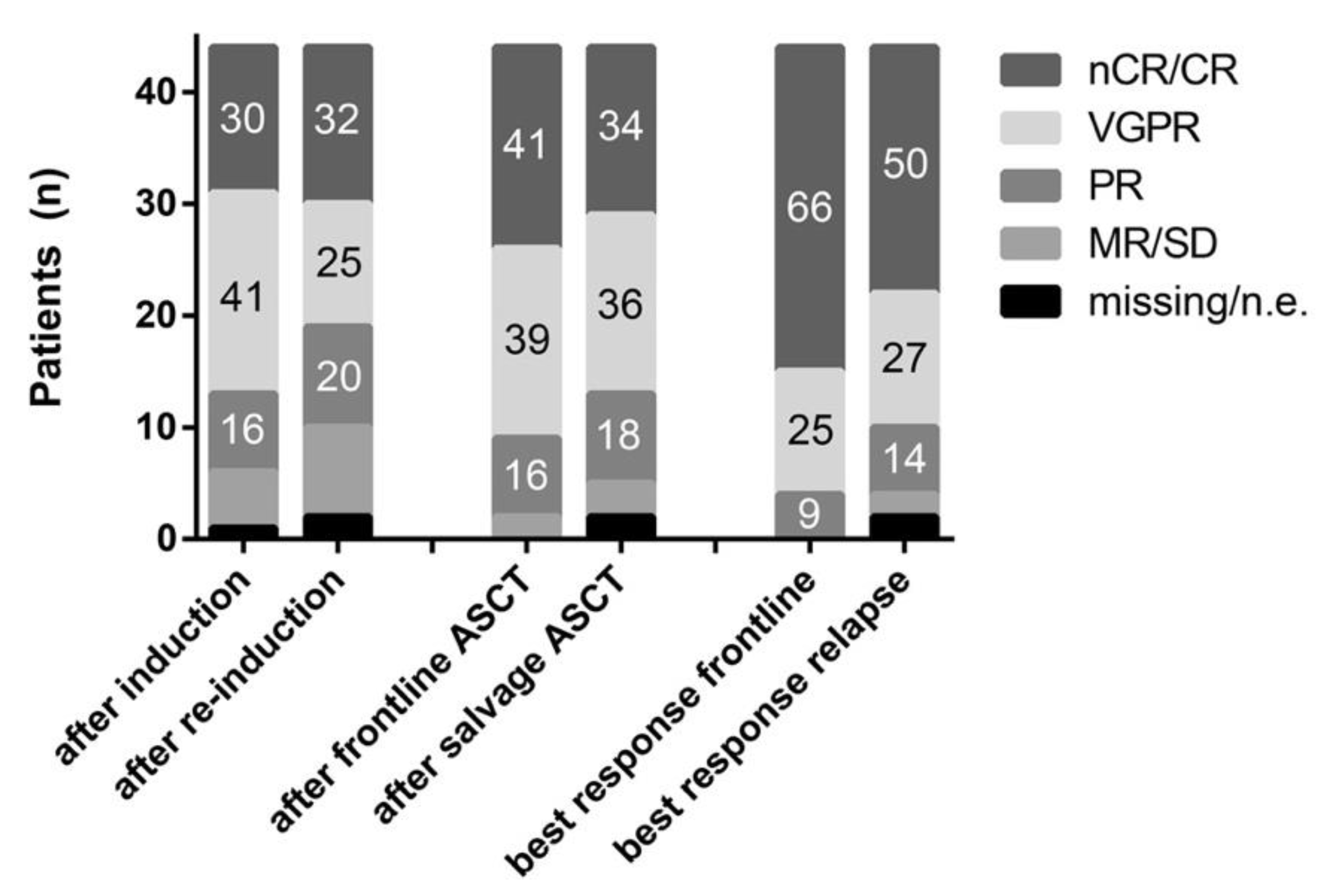
3.1. Response and Survival
3.2. Prognostic Factors
3.3. Safety
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gandhi, U.H.; Cornell, R.F.; Lakshman, A.; Gahvari, Z.J.; McGehee, E.; Jagosky, M.H.; Gupta, R.; Varnado, W.; Fiala, M.A.; Chhabra, S.; et al. Outcomes of patients with multiple myeloma refractory to CD38-targeted monoclonal antibody therapy. Leukemia 2019, 33, 2266–2275. [Google Scholar] [CrossRef]
- Moreau, P.; San Miguel, J.; Sonneveld, P.; Mateos, M.V.; Zamagni, E.; Avet-Loiseau, H.; Hajek, R.; Dimopoulos, M.A.; Ludwig, H.; Einsele, H.; et al. Multiple myeloma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017, 28, iv52–iv61. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.K.; Callander, N.S.; Alsina, M.; Atanackovic, D.; Biermann, J.S.; Chandler, J.C.; Costello, C.; Faiman, M.; Fung, H.C.; Gasparetto, C.; et al. Multiple Myeloma, Version 3.2017, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2017, 15, 230–269. [Google Scholar] [CrossRef] [PubMed]
- Moreau, P.; Attal, M.; Hulin, C.; Arnulf, B.; Belhadj, K.; Benboubker, L.; Béné, M.C.; Broijl, A.; Caillon, H.; Caillot, D.; et al. Bortezomib, thalidomide, and dexamethasone with or without daratumumab before and after autologous stem-cell transplantation for newly diagnosed multiple myeloma (CASSIOPEIA): A randomised, open-label, phase 3 study. Lancet 2019, 394, 29–38. [Google Scholar] [CrossRef]
- Stewart, A.K.; Rajkumar, S.V.; Dimopoulos, M.A.; Masszi, T.; Špička, I.; Oriol, A.; Hájek, R.; Rosiñol, L.; Siegel, D.S.; Mihaylov, G.G.; et al. Carfilzomib, Lenalidomide, and Dexamethasone for Relapsed Multiple Myeloma. N. Engl. J. Med. 2014, 372, 141206080130007. [Google Scholar] [CrossRef]
- Lonial, S.; Dimopoulos, M.; Palumbo, A.; White, D.; Grosicki, S.; Spicka, I.; Walter-Croneck, A.; Moreau, P.; Mateos, M.-V.; Magen, H.; et al. Elotuzumab Therapy for Relapsed or Refractory Multiple Myeloma. N. Engl. J. Med. 2015, 373, 621–631. [Google Scholar] [CrossRef] [Green Version]
- Dimopoulos, M.A.; Oriol, A.; Nahi, H.; San-Miguel, J.; Bahlis, N.J.; Usmani, S.Z.; Rabin, N.; Orlowski, R.Z.; Komarnicki, M.; Suzuki, K.; et al. Daratumumab, Lenalidomide, and Dexamethasone for Multiple Myeloma. N. Engl. J. Med. 2016, 375, 1319–1331. [Google Scholar] [CrossRef] [Green Version]
- Palumbo, A.; Chanan-Khan, A.; Weisel, K.; Nooka, A.K.; Masszi, T.; Beksac, M.; Spicka, I.; Hungria, V.; Munder, M.; Mateos, M.V.; et al. Daratumumab, Bortezomib, and Dexamethasone for Multiple Myeloma. N. Engl. J. Med. 2016, 375, 754–766. [Google Scholar] [CrossRef]
- Moreau, P.; Masszi, T.; Grzasko, N.; Bahlis, N.J.; Hansson, M.; Pour, L.; Sandhu, I.; Ganly, P.; Baker, B.W.; Jackson, S.R.; et al. Oral Ixazomib, Lenalidomide, and Dexamethasone for Multiple Myeloma. N. Engl. J. Med. 2016, 374, 1621–1634. [Google Scholar] [CrossRef]
- Cook, G.; Williams, C.; Brown, J.M.; Cairns, D.A.; Cavenagh, J.; Snowden, J.A.; Ashcroft, A.J.; Fletcher, M.; Parrish, C.; Yong, K.; et al. High-dose chemotherapy plus autologous stem-cell transplantation as consolidation therapy in patients with relapsed multiple myeloma after previous autologous stem-cell transplantation (NCRI Myeloma X Relapse [Intensive trial]): A randomised, open-label. Lancet Oncol. 2014, 15, 874–885. [Google Scholar] [CrossRef]
- Cook, G.; Ashcroft, A.J.; Cairns, D.A.; Williams, C.D.; Brown, J.M.; Cavenagh, J.D.; Snowden, J.A.; Parrish, C.; Yong, K.; Cavet, J.; et al. The effect of salvage autologous stem-cell transplantation on overall survival in patients with relapsed multiple myeloma (final results from BSBMT/UKMF Myeloma X Relapse [Intensive]): A randomised, open-label, phase 3 trial. Lancet Haematol. 2016, 3, e340–e351. [Google Scholar] [CrossRef] [Green Version]
- Hagen, P.A.; Stiff, P. The Role of Salvage Second Autologous Hematopoietic Cell Transplantation in Relapsed Multiple Myeloma. Biol. Blood Marrow Transplant. 2019, 25, e98–e107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldschmidt, H.; Baertsch, M.A.; Schlenzka, J.; Becker, N.; Habermehl, C.; Hielscher, T.; Raab, M.S.; Hillengass, J.; Sauer, S.; Müller-Tidow, C.; et al. Salvage autologous transplant and lenalidomide maintenance vs. lenalidomide/dexamethasone for relapsed multiple myeloma: The randomized GMMG phase III trial ReLApsE. Leukemia 2020, 35, 1134–1144. [Google Scholar] [CrossRef]
- Durie, B.G.M.; Harousseau, J.-L.; Miguel, J.S.; Bladé, J.; Barlogie, B.; Anderson, K.; Gertz, M.; Dimopoulos, M.; Westin, J.; Sonneveld, P.; et al. International uniform response criteria for multiple myeloma. Leukemia 2006, 20, 1467–1473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sorror, M.L.; Maris, M.B.; Storb, R.; Baron, F.; Sandmaier, B.M.; Maloney, D.G.; Storer, B. Hematopoietic cell transplantation (HCT)-specific comorbidity index: A new tool for risk assessment before allogeneic HCT. Blood 2005, 106, 2912–2919. [Google Scholar] [CrossRef] [Green Version]
- Greipp, P.R.; San Miguel, J.; Durie, B.G.M.; Crowley, J.J.; Barlogie, B.; Bladé, J.; Boccadoro, M.; Child, J.A.; Avet-Loiseau, H.; Harousseau, J.-L.; et al. International staging system for multiple myeloma. J. Clin. Oncol. 2005, 23, 3412–3420. [Google Scholar] [CrossRef]
- Neben, K.; Lokhorst, H.M.; Jauch, A.; Bertsch, U.; Hielscher, T.; van der Holt, B.; Salwender, H.; Blau, I.W.; Weisel, K.; Pfreundschuh, M.; et al. Administration of bortezomib before and after autologous stem cell transplantation improves outcome in multiple myeloma patients with deletion 17p. Blood 2012, 119, 940–948. [Google Scholar] [CrossRef] [Green Version]
- Bladé, J.; Samson, D.; Reece, D.; Apperley, J.; Björkstrand, B.; Gahrton, G.; Gertz, M.; Giralt, S.; Jagannath, S.; Vesole, D. Criteria for evaluating disease response and progression in patients with multiple myeloma treated by high-dose therapy and haemopoietic stem cell transplantation. Myeloma Subcommittee of the EBMT. European Group for Blood and Marrow Transplant. Br. J. Haematol. 1998, 102, 1115–1123. [Google Scholar] [CrossRef]
- Richardson, P.G.; Barlogie, B.; Berenson, J.; Singhal, S.; Jagannath, S.; Irwin, D.; Rajkumar, S.V.; Srkalovic, G.; Alsina, M.; Alexanian, R.; et al. A Phase 2 Study of Bortezomib in Relapsed, Refractory Myeloma. N. Engl. J. Med. 2003, 348, 2609–2617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. WHO Handbook for Reporting Results of Cancer Treatment; WHO: Geneva, Switzerland, 1979; Available online: https://apps.who.int/iris/handle/10665/37200 (accessed on 5 August 2021).
- Dimopoulos, M.A.; Moreau, P.; Terpos, E.; Mateos, M.-V.; Zweegman, S.; Cook, G.; Delforge, M.; Hájek, R.; Schjesvold, F.; Cavo, M.; et al. Multiple Myeloma: EHA-ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-up. HemaSphere 2021, 5, e528. [Google Scholar] [CrossRef]
- Manjappa, S.; Fiala, M.A.; King, J.; Kohnen, D.A.; Vij, R. The efficacy of salvage autologous stem cell transplant among patients with multiple myeloma who received maintenance therapy post initial transplant. Bone Marrow Transplant. 2018, 53, 1483–1486. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, P.L.; Holstein, S.A.; Petrucci, M.T.; Richardson, P.G.; Hulin, C.; Tosi, P.; Bringhen, S.; Musto, P.; Anderson, K.C.; Caillot, D.; et al. Lenalidomide maintenance after autologous stem-cell transplantation in newly diagnosed multiple myeloma: A meta-analysis. J. Clin. Oncol. 2017, 35, 3279–3289. [Google Scholar] [CrossRef]
- Siegel, D.S.; Dimopoulos, M.A.; Ludwig, H.; Facon, T.; Goldschmidt, H.; Jakubowiak, A.; San-Miguel, J.; Obreja, M.; Blaedel, J.; Stewart, A.K. Improvement in Overall Survival With Carfilzomib, Lenalidomide, and Dexamethasone in Patients with Relapsed or Refractory Multiple Myeloma. J. Clin. Oncol. 2018, 36, 728–734. [Google Scholar] [CrossRef] [PubMed]
- Bahlis, N.J.; Dimopoulos, M.A.; White, D.J.; Benboubker, L.; Cook, G.; Leiba, M.; Ho, P.J.; Kim, K.; Takezako, N.; Moreau, P.; et al. Daratumumab plus lenalidomide and dexamethasone in relapsed/refractory multiple myeloma: Extended follow-up of POLLUX, a randomized, open-label, phase 3 study. Leukemia 2020, 34, 1875–1884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hari, P.; Mateos, M.-V.; Abonour, R.; Knop, S.; Bensinger, W.; Ludwig, H.; Song, K.; Hajek, R.; Moreau, P.; Siegel, D.S.; et al. Efficacy and safety of carfilzomib regimens in multiple myeloma patients relapsing after autologous stem cell transplant: ASPIRE and ENDEAVOR outcomes. Leukemia 2017, 31, 2630–2641. [Google Scholar] [CrossRef] [PubMed]
- Mikhael, J. Treatment Options for Triple-class Refractory Multiple Myeloma. Clin. Lymphoma Myeloma Leuk. 2020, 20, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Dimopoulos, M.; Quach, H.; Mateos, M.V.; Landgren, O.; Leleu, X.; Siegel, D.; Weisel, K.; Yang, H.; Klippel, Z.; Zahlten-Kumeli, A.; et al. Carfilzomib, dexamethasone, and daratumumab versus carfilzomib and dexamethasone for patients with relapsed or refractory multiple myeloma (CANDOR): Results from a randomised, multicentre, open-label, phase 3 study. Lancet 2020, 396, 186–197. [Google Scholar] [CrossRef]
- Gregersen, H.; Peceliunas, V.; Remes, K.; Schjesvold, F.; Abildgaard, N.; Nahi Nahi, H.; Frost Andersen, N.; Vangsted, A.J.; Tobias, W.K.; Helleberg, C.; et al. Carfilzomib and dexamethasone maintenance prolong time to progression following salvage ASCT in multiple myeloma: A randomized phase 2 trial by the nordic myeloma study group. HemaSphere 2019, 3, 737–738. Available online: https://journals.lww.com/hemasphere/abstract/2019/06001/s1602_carfilzomib_and_dexamethasone_maintenance.1480.aspx (accessed on 5 August 2021). [CrossRef]
- Baertsch, M.-A.; Schlenzka, J.; Habermehl, C.; Hielscher, T.; Raab, M.S.; Hillengass, J.; Müller-Tidow, C.; Luntz, S.; Jauch, A.; Brossart, P.; et al. Subgroup Analyses of the Randomized GMMG Phase III Multicenter Trial Relapse Suggest Survival Benefit of Salvage Autologous Transplant Primarily in Low Risk Multiple Myeloma. Blood 2018, 132 (Suppl. 1), 254. [Google Scholar] [CrossRef]




| Frontline Transplant | Salvage Transplant | |
|---|---|---|
| Age (median (range)) | 54.8 (36–68) | 58.9 (40–71) |
| Sex | ||
| Female | 22 (50%) | |
| Male | 22 (50%) | |
| WHO PS | ||
| 0 | 15/44 (34%) | - |
| 1 | 22/44 (50%) | - |
| 2 | 7/44 (16%) | - |
| Sorror comorbidity score | ||
| 0 | 23/44 (52%) | 11/44 (25%) |
| 1 | 5/44 (11%) | 8/44 (18%) |
| 2 | 8/44 (18%) | 10/44 (23%) |
| 3 | 7/44 (16%) | 9/44 (21%) |
| ≥4 | 1 (2%) | 6/44 (14%) |
| Myeloma subtype | ||
| IgG | 17/44 (39%) | |
| IgA | 11/44 (25%) | |
| IgD | 1/44 (2%) | |
| Bence Jones | 8/44 (18%) | |
| Hyposecretory | 7/44 (16%) | |
| Light chain subtype | ||
| Kappa | 29/44 (66%) | |
| Lambda | 15/44 (34%) | |
| ISS | ||
| I | 23/42 (55%) | - |
| II | 9/42 (21%) | - |
| III | 10/42 (24%) | - |
| Cytogenetics | ||
| Standard risk | 27/37 (73%) | - |
| High risk | 10/37 (27%) | - |
| Serum creatinine | ||
| ≤2 | 35/44 (80%) | 42/43 (98%) |
| >2 | 9/44 (20%) | 1/43 (2%) |
| LDH | ||
| Normal | 41/42 (98%) | 38/42 (90%) |
| Elevated | 1/42 (2%) | 4/42 (10%) |
| Prior lines of treatment | ||
| 1 | - | 38/44 (86%) |
| 2 | - | 3/44 (7%) |
| 3 | - | 3/44 (7%) |
| (Re-)Induction treatment | ||
| PAD | 20/44 (46%) | - |
| VCD | 18/44 (41%) | - |
| VAD | 4/44 (9%) | - |
| Other | 2/44 (5%) | - |
| KRD | - | 41/44 (93%) */& |
| KD | - | 3/44 (7%) |
| Cycles of (Re-)Induction | ||
| 3 | 34/44 (77%) | 38/44 (86%) |
| 4 | 8/44 (18%) | 5/44 (11%) |
| 6 | 2/44 (5%) | - |
| 9 | - | 1/44 (2%) |
| HD-Melphalan | ||
| 200 mg/m2 | 41/44 (93%) | 41/44 (93%) |
| 140 mg/m2 | - | 2/44 (5%) |
| 100 mg/m2 | 3/44 (7%) | 1/44 (2%) |
| Single vs. tandem transplant | ||
| Single | 28/44 (64%) | 44/44 (100%) |
| Tandem | 16/44 (36%) | - |
| Maintenance treatment | 22/44 (50%) | 17/44 (39%) |
| Lenalidomide | 8/44 (18%) | 16/44 (36%) § |
| Thalidomide | 7/44 (16%) | - |
| Bortezomib | 5/44 (11%) | 1/44 (2%) |
| Interferon | 2/44 (5%) | - |
| Lenalidomide pretreatment | - | 16/44 (36%) |
| Variable | n | HR | 95% CI | p |
|---|---|---|---|---|
| Age | 44 | 1.01 | 0.95–1.06 | 0.83 |
| Prior lines of therapy (>1 vs. 1) | 6/44 | 5.70 | 2.04–15.90 | 0.001 |
| TTP1 (per 1 year increase) | 44 | 0.79 | 0.62–1.01 | 0.06 |
| Response status at time of salvage transplant (≥VGPR vs. <VGPR) | 24/44 | 0.19 | 0.07–0.49 | 0.001 |
| Maintenance (salvage transplant) | 17/44 | 0.20 | 0.06–0.66 | 0.009 |
| Prior lenalidomide | 16/44 | 2.68 | 1.17–6.12 | 0.02 |
| Maintenance (frontline transplant) | 22/44 | 0.58 | 0.25–1.35 | 0.21 |
| Response status after frontline transplant | ||||
| ≥VGPR vs. <VGPR ≥nCR vs. <nCR | 35/44 | 0.90 | 0.30–0.27 | 0.85 |
| 18/44 | 0.89 | 0.38–2.11 | 0.80 | |
| Best response during frontline treatment | ||||
| ≥VGPR vs. <VGPR ≥nCR vs. <nCR | 40/44 | 0.93 | 0.22–3.99 | 0.92 |
| 29/44 | 0.78 | 0.32–1.89 | 0.57 |
| Variable | HR | 95% CI | p |
|---|---|---|---|
| TTP1 | 0.74 | 0.50–1.09 | 0.13 |
| Prior lines of therapy (>1 vs. 1) | 1.80 | 0.46–7.03 | 0.40 |
| Response status at time of salvage transplant * | 0.18 | 0.06–0.48 | 0.001 |
| Maintenance (salvage transplant) | 0.22 | 0.06–0.81 | 0.02 |
| Prior lenalidomide | 2.07 | 0.78–5.48 | 0.14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baertsch, M.-A.; Fougereau, M.; Hielscher, T.; Sauer, S.; Breitkreutz, I.; Jordan, K.; Müller-Tidow, C.; Goldschmidt, H.; Raab, M.-S.; Hillengass, J.; et al. Carfilzomib, Lenalidomide, and Dexamethasone Followed by Salvage Autologous Stem Cell Transplant with or without Maintenance for Relapsed or Refractory Multiple Myeloma. Cancers 2021, 13, 4706. https://doi.org/10.3390/cancers13184706
Baertsch M-A, Fougereau M, Hielscher T, Sauer S, Breitkreutz I, Jordan K, Müller-Tidow C, Goldschmidt H, Raab M-S, Hillengass J, et al. Carfilzomib, Lenalidomide, and Dexamethasone Followed by Salvage Autologous Stem Cell Transplant with or without Maintenance for Relapsed or Refractory Multiple Myeloma. Cancers. 2021; 13(18):4706. https://doi.org/10.3390/cancers13184706
Chicago/Turabian StyleBaertsch, Marc-Andrea, Mathilde Fougereau, Thomas Hielscher, Sandra Sauer, Iris Breitkreutz, Karin Jordan, Carsten Müller-Tidow, Hartmut Goldschmidt, Marc-Steffen Raab, Jens Hillengass, and et al. 2021. "Carfilzomib, Lenalidomide, and Dexamethasone Followed by Salvage Autologous Stem Cell Transplant with or without Maintenance for Relapsed or Refractory Multiple Myeloma" Cancers 13, no. 18: 4706. https://doi.org/10.3390/cancers13184706






