Light Therapy for Cancer-Related Fatigue in (Non-)Hodgkin Lymphoma Survivors: Results of a Randomized Controlled Trial
Abstract
Simple Summary
Abstract
1. Introduction
2. Patients and Methods
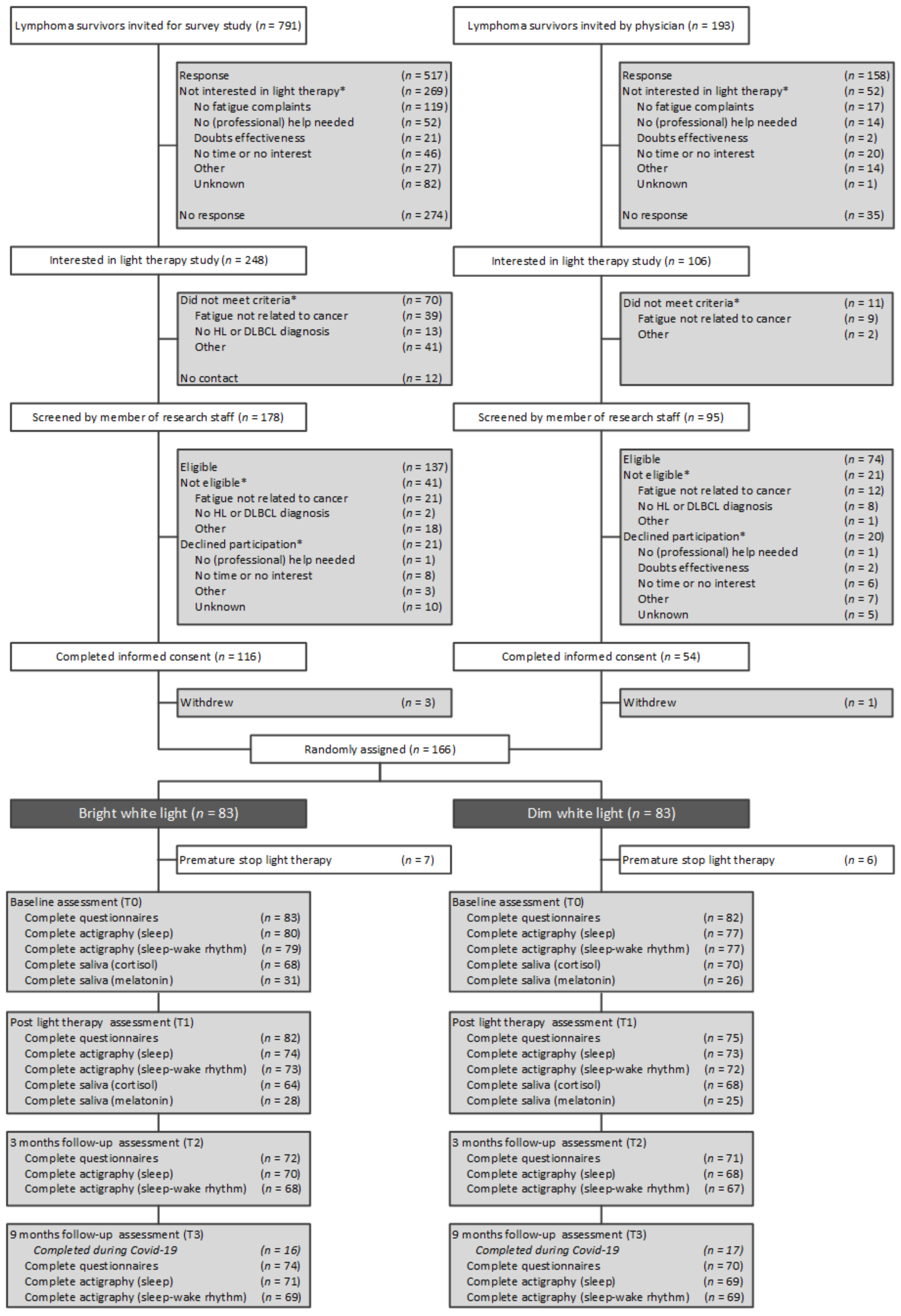
2.1. Research Design and Study Sample
2.2. Procedure, Randomization, and Timing of Assessments
2.3. Intervention
2.4. Study Measures
2.5. Statistical Analyses
3. Results
3.1. Primary Outcomes
3.2. Secondary Outcomes
3.3. Adverse Effects
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Prior Presentations
Conflicts of Interest
References
- Daniëls, L.; Oerlemans, S.; Krol, A.; Creutzberg, C.; van de Poll-Franse, L. Chronic fatigue in Hodgkin lymphoma survivors and associations with anxiety, depression and comorbidity. Br. J. Cancer 2014, 110, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Oerlemans, S.; Mols, F.; Issa, D.E.; Pruijt, J.; Peters, W.G.; Lybeert, M.; Zijlstra, W.; Coebergh, J.W.W.; van de Poll-Franse, L.V. A high level of fatigue among long-term survivors of non-Hodgkin’s lymphoma: Results from the longitudinal population-based PROFILES registry in the south of the Netherlands. Haematologica 2013, 98, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Busson, R.; van der Kaaij, M.; Mounier, N.; Aleman, B.M.; Thiéblemont, C.; Stamatoullas, A.; Ribrag, V.; Tilly, H.; Haioun, C.; Casasnovas, R.-O. Fatigue level changes with time in long-term Hodgkin and non-Hodgkin lymphoma survivors: A joint EORTC-LYSA cross-sectional study. Health Qual. Life Outcomes 2019, 17, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Mounier, N.; Anthony, S.; Busson, R.; Thieblemont, C.; Ribrag, V.; Tilly, H.; Haioun, C.; Casasnovas, R.O.; Morschhauser, F.; Feugier, P. Long-term fatigue in survivors of non-Hodgkin lymphoma: The Lymphoma Study Association SIMONAL cross-sectional study. Cancer 2019, 125, 2291–2299. [Google Scholar] [CrossRef]
- Bower, J.E.; Bak, K.; Berger, A.; Breitbart, W.; Escalante, C.P.; Ganz, P.A.; Schnipper, H.H.; Lacchetti, C.; Ligibel, J.A.; Lyman, G.H. Screening, assessment, and management of fatigue in adult survivors of cancer: An American Society of Clinical oncology clinical practice guideline adaptation. J. Clin. Oncol. 2014, 32, 1840–1850. [Google Scholar] [CrossRef]
- Agasi-Idenburg, S.; Thong, M.; Punt, C.; Stuiver, M.; Aaronson, N.K. Comparison of symptom clusters associated with fatigue in older and younger survivors of colorectal cancer. Support. Care Cancer 2017, 25, 625–632. [Google Scholar] [CrossRef]
- Kwekkeboom, K.L. Cancer symptom cluster management. Semin. Oncol. Nurs. 2016, 32, 373–382. [Google Scholar] [CrossRef]
- Barsevick, A.M. The elusive concept of the symptom cluster. Oncol. Nurs. Forum. 2007, 34, 971–980. [Google Scholar] [CrossRef]
- Gehrman, P.R.; Garland, S.N.; Matura, L.A.; Mao, J.J.P. Insomnia in breast cancer: Independent symptom or symptom cluster? Palliat. Support. Care 2017, 15, 369–375. [Google Scholar] [CrossRef]
- Innominato, P.F.; Roche, V.P.; Palesh, O.G.; Ulusakarya, A.; Spiegel, D.; Lévi, F.A. The circadian timing system in clinical oncology. Ann. Med. 2014, 46, 191–207. [Google Scholar] [CrossRef]
- Payne, J.K. Altered circadian rhythms and cancer-related fatigue outcomes. Integr. Cancer Ther. 2011, 10, 221–233. [Google Scholar] [CrossRef]
- Rich, T.A. Symptom clusters in cancer patients and their relation to EGFR ligand modulation of the circadian axis. J. Support. Oncol. 2007, 5, 167–174. [Google Scholar]
- Weinrib, A.Z.; Sephton, S.E.; DeGeest, K.; Penedo, F.; Bender, D.; Zimmerman, B.; Kirschbaum, C.; Sood, A.K.; Lubaroff, D.M.; Lutgendorf, S.K. Diurnal cortisol dysregulation, functional disability, and depression in women with ovarian cancer. Cancer 2010, 116, 4410–4419. [Google Scholar] [CrossRef]
- Innominato, P.F.; Mormont, M.-C.; Rich, T.A.; Waterhouse, J.; Lévi, F.A.; Bjarnason, G.A. Circadian disruption, fatigue, and anorexia clustering in advanced cancer patients: Implications for innovative therapeutic approaches. Integr. Cancer Ther. 2009, 8, 361–370. [Google Scholar] [CrossRef]
- Schrepf, A.; Clevenger, L.; Christensen, D.; DeGeest, K.; Bender, D.; Ahmed, A.; Goodheart, M.J.; Dahmoush, L.; Penedo, F.; Lucci, J.A. Cortisol and inflammatory processes in ovarian cancer patients following primary treatment: Relationships with depression, fatigue, and disability. Brain. Behav. Immun. 2013, 30, S126–S134. [Google Scholar] [CrossRef]
- Pail, G.; Huf, W.; Pjrek, E.; Winkler, D.; Willeit, M.; Praschak-Rieder, N.; Kasper, S. Bright-light therapy in the treatment of mood disorders. Neuropsychobiology 2011, 64, 152–162. [Google Scholar] [CrossRef]
- Terman, M.; Terman, J.S. Light therapy for seasonal and nonseasonal depression: Efficacy, protocol, safety, and side effects. CNS Spectr. 2005, 10, 647–663. [Google Scholar] [CrossRef]
- Golden, R.N.; Gaynes, B.N.; Ekstrom, R.D.; Hamer, R.M.; Jacobsen, F.M.; Suppes, T.; Wisner, K.L.; Nemeroff, C.B. The efficacy of light therapy in the treatment of mood disorders: A review and meta-analysis of the evidence. Am. J. Psychiatry 2005, 162, 656–662. [Google Scholar] [CrossRef]
- Åkerstedt, T.; Landström, U.; Byström, M.; Nordström, B.; Wibom, R. Bright light as a sleepiness prophylactic: A laboratory study of subjective ratings and EEG. Percept. Mot. Ski. 2003, 97, 811–819. [Google Scholar] [CrossRef]
- Van Maanen, A.; Meijer, A.M.; van der Heijden, K.B.; Oort, F.J. The effects of light therapy on sleep problems: A systematic review and meta-analysis. Sleep Med. Rev. 2016, 29, 52–62. [Google Scholar] [CrossRef]
- Küller, R. The influence of light on circarhythms in humans. J. Physiol. Anthropol. Appl. Hum. Sci. 2002, 21, 87–91. [Google Scholar] [CrossRef]
- Lucas, R.J.; Peirson, S.N.; Berson, D.M.; Brown, T.M.; Cooper, H.M.; Czeisler, C.A.; Figueiro, M.G.; Gamlin, P.D.; Lockley, S.W.; O’Hagan, J.B. Measuring and using light in the melanopsin age. Trends Neurosci. 2014, 37, 1–9. [Google Scholar] [CrossRef]
- Schmidt, T.M.; Chen, S.-K.; Hattar, S. Intrinsically photosensitive retinal ganglion cells: Many subtypes, diverse functions. Trends Neurosci. 2011, 34, 572–580. [Google Scholar] [CrossRef]
- Ancoli-Israel, S.; Rissling, M.; Neikrug, A.; Trofimenko, V.; Natarajan, L.; Parker, B.A.; Lawton, S.; Desan, P.; Liu, L. Light treatment prevents fatigue in women undergoing chemotherapy for breast cancer. Support. Care Cancer 2012, 20, 1211–1219. [Google Scholar] [CrossRef]
- Redd, W.H.; Valdimarsdottir, H.; Wu, L.M.; Winkel, G.; Byrne, E.E.; Beltre, M.A.; Liebman, E.S.; Erazo, T.; Hayes, J.A.; Isola, L. Systematic light exposure in the treatment of cancer-related fatigue: A preliminary study. Psychooncology 2014, 23, 1431–1434. [Google Scholar] [CrossRef]
- Johnson, J.A.; Garland, S.N.; Carlson, L.E.; Savard, J.; Simpson, J.S.A.; Ancoli-Israel, S.; Campbell, T.S. Bright light therapy improves cancer-related fatigue in cancer survivors: A randomized controlled trial. J. Cancer Surviv. 2017, 12, 1–10. [Google Scholar] [CrossRef]
- Wu, L.M.; Amidi, A.; Valdimarsdottir, H.; Ancoli-Israel, S.; Liu, L.; Winkel, G.; Byrne, E.E.; Sefair, A.V.; Vega, A.; Bovbjerg, K. The effect of systematic light exposure on sleep in a mixed group of fatigued cancer survivors. J. Clin. Sleep Med. 2018, 14, 31–39. [Google Scholar] [CrossRef]
- Fox, R.S.; Baik, S.H.; McGinty, H.; Garcia, S.F.; Reid, K.J.; Bovbjerg, K.; Fajardo, P.; Wu, L.M.; Shahabi, S.; Ong, J.C.; et al. Feasibility and Preliminary Efficacy of a Bright Light Intervention in Ovarian and Endometrial Cancer Survivors. Int. J. Behav. Med. 2021, 28, 83–95. [Google Scholar] [CrossRef]
- Garland, S.N.; Johnson, J.A.; Carlson, L.E.; Rash, J.A.; Savard, J.; Campbell, T.S. Light therapy for insomnia symptoms in fatigued cancer survivors: A secondary analysis of a randomized controlled trial. J. Psychosoc. Oncol. Res. Pract. 2020, 2, e27. [Google Scholar] [CrossRef]
- Jeste, N.; Liu, L.; Rissling, M.; Trofimenko, V.; Natarajan, L.; Parker, B.A.; Ancoli-Israel, S. Prevention of quality-of-life deterioration with light therapy is associated with changes in fatigue in women with breast cancer undergoing chemotherapy. Qual. Life Res. 2013, 22, 1239–1244. [Google Scholar] [CrossRef]
- Neikrug, A.B.; Rissling, M.; Trofimenko, V.; Liu, L.; Natarajan, L.; Lawton, S.; Parker, B.A.; Ancoli-Israel, S. Bright light therapy protects women from circadian rhythm desynchronization during chemotherapy for breast cancer. Behav. Sleep Med. 2012, 10, 202–216. [Google Scholar] [CrossRef] [PubMed]
- Starreveld, D.E.J.; Daniels, L.A.; Valdimarsdottir, H.B.; Redd, W.H.; de Geus, J.L.; Ancoli-Israel, S.; Lutgendorf, S.; Korse, C.M.; Kieffer, J.M.; van Leeuwen, F.; et al. Light therapy as a treatment of cancer-related fatigue in (non-) Hodgkin lymphoma survivors (SPARKLE trial): Study protocol of a multicenter randomized controlled trial. BMC Cancer 2018, 18, 880. [Google Scholar] [CrossRef] [PubMed]
- Starreveld, D.E.J.; Habers, G.E.A.; Valdimarsdottir, H.B.; Kessels, R.; Daniëls, L.A.; van Leeuwen, F.E.; Bleiker, E.M.A. Cancer-related Fatigue in Relation to Chronotype and Sleep Quality in (Non-) Hodgkin Lymphoma Survivors. J. Biol. Rhythm. 2021, 36, 71–83. [Google Scholar] [CrossRef] [PubMed]
- Oldenmenger, W.H.; Pleun, J.; de Klerk, C.; van der Rijt, C.C. Cut points on 0–10 numeric rating scales for symptoms included in the Edmonton Symptom Assessment Scale in cancer patients: A systematic review. J. Pain Symptom Manag. 2013, 45, 1083–1093. [Google Scholar] [CrossRef]
- Smets, E.; Garssen, B.; Bonke, B.d.; De Haes, J. The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J. Psychosom. Res. 1995, 39, 315–325. [Google Scholar] [CrossRef]
- Kieffer, J.M.; Starreveld, D.E.J.; Boekhout, A.; Bleiker, E.M.A. A questionable factor structure of the multidimensional fatigue inventory in the general Dutch population. J. Clin. Epidemiol. 2021, 137, 266–276. [Google Scholar] [CrossRef]
- Mundt, J.C.; Marks, I.M.; Shear, M.K.; Greist, J.M. The Work and Social Adjustment Scale: A simple measure of impairment in functioning. BJPsych 2002, 180, 461–464. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D scale a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Van der Bij, A.K.; de Weerd, S.; Cikot, R.J.; Steegers, E.A.; Braspenning, J.C.C. Validation of the dutch short form of the state scale of the Spielberger State-Trait Anxiety Inventory: Considerations for usage in screening outcomes. Public Health Genom. 2003, 6, 84–87. [Google Scholar] [CrossRef]
- Hays, R.D.; Sherbourne, C.D.; Mazel, R.M. The rand 36-item health survey 1.0. Health Econ. 1993, 2, 217–227. [Google Scholar] [CrossRef]
- Van der Zee, K.; Sanderman, R. Het Meten van de Algemene Gezondheidstoestand Met de RAND-36: Een Handleiding; Noordelijk Centrum Voor Gezondheidsvraagstukken: Groningen, The Netherlands, 1993; pp. 1–23. [Google Scholar]
- Ancoli-Israel, S.; Martin, J.L.; Blackwell, T.; Buenaver, L.; Liu, L.; Meltzer, L.J.; Sadeh, A.; Spira, A.P.; Taylor, D.J. The SBSM guide to actigraphy monitoring: Clinical and research applications. Behav. Sleep Med. 2015, 13, S4–S38. [Google Scholar] [CrossRef]
- Van Someren, E.J.; Swaab, D.F.; Colenda, C.C.; Cohen, W.; McCall, W.V.; Rosenquist, P.B. Bright light therapy: Improved sensitivity to its effects on rest-activity rhythms in Alzheimer patients by application of nonparametric methods. Chronobiol. Int. 1999, 16, 505–518. [Google Scholar] [CrossRef]
- Stalder, T.; Kirschbaum, C.; Kudielka, B.M.; Adam, E.K.; Pruessner, J.C.; Wüst, S.; Dockray, S.; Smyth, N.; Evans, P.; Hellhammer, D.H. Assessment of the cortisol awakening response: Expert consensus guidelines. Psychoneuroendocrinology 2016, 63, 414–432. [Google Scholar] [CrossRef]
- Keijzer, H.; Smits, M.G.; Duffy, J.F.; Curfs, L.M. Why the dim light melatonin onset (DLMO) should be measured before treatment of patients with circadian rhythm sleep disorders. Sleep Med. Rev. 2014, 18, 333–339. [Google Scholar] [CrossRef]
- Danilenko, K.V.; Verevkin, E.G.; Antyufeev, V.S.; Wirz-Justice, A.; Cajochen, C. The hockey-stick method to estimate evening dim light melatonin onset (DLMO) in humans. Chronobiol. Int. 2014, 31, 349–355. [Google Scholar] [CrossRef]
- Norman, G.R.; Sloan, J.A.; Wyrwich, K.W. Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Med. Care 2003, 41, 582–592. [Google Scholar] [CrossRef]
- Schwarz, G. Estimating the dimension of a model. Ann. Stat. 1978, 6, 461–464. [Google Scholar] [CrossRef]
- Akaike, H. Information theory and an extension of the maximum likelihood principle. In Selected Papers of Hirotugu Akaike; Parzen, E., Tanabe, K., Kitagawa, G., Eds.; Springer: New York, NY, USA, 1998; pp. 199–213. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Earlbaum Associates: Hillsdale, NJ, USA, 1988; Volume 2. [Google Scholar]
- Schwarz, R.; Krauss, O.; Hinz, A. Fatigue in the general population. Oncol. Res. Treat. 2003, 26, 140–144. [Google Scholar] [CrossRef]
- Khanna, D.; Pope, J.E.; Khanna, P.P.; Maloney, M.; Samedi, N.; Norrie, D.; Ouimet, G.; Hays, R.D. The minimally important difference for the fatigue visual analog scale in patients with rheumatoid arthritis followed in an academic clinical practice. J. Rheumatol 2008, 35, 2339–2343. [Google Scholar] [CrossRef]
- Purcell, A.; Fleming, J.; Bennett, S.; Burmeister, B.; Haines, T. Determining the minimal clinically important difference criteria for the Multidimensional Fatigue Inventory in a radiotherapy population. Support. Care Cancer 2010, 18, 307–315. [Google Scholar] [CrossRef]
- Streiner, D.L.; Norman, G.R.; Cairney, J. Health Measurement Scales: A Practical Guide to Their Development and Use, 5th ed.; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Aoki, H.; Yamada, N.; Ozeki, Y.; Yamane, H.; Kato, N. Minimum light intensity required to suppress nocturnal melatonin concentration in human saliva. Neurosci. Lett. 1998, 252, 91–94. [Google Scholar] [CrossRef]
- Figueiro, M.; Nagare, R.; Price, L. Non-visual effects of light: How to use light to promote circadian entrainment and elicit alertness. Light. Res. Technol. 2018, 50, 38–62. [Google Scholar] [CrossRef]
- Valdimarsdottir, H.B.; Figueiro, M.G.; Holden, W.; Lutgendorf, S.; Wu, L.M.; Ancoli-Israel, S.; Chen, J.; Hoffman-Peterson, A.; Granski, J.; Prescott, N. Programmed environmental illumination during autologous stem cell transplantation hospitalization for the treatment of multiple myeloma reduces severity of depression: A preliminary randomized controlled trial. Cancer Med. 2018, 7, 4345–4353. [Google Scholar] [CrossRef]
- Mustian, K.M.; Alfano, C.M.; Heckler, C.; Kleckner, A.S.; Kleckner, I.R.; Leach, C.R.; Mohr, D.; Palesh, O.G.; Peppone, L.J.; Piper, B.F. Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: A meta-analysis. JAMA Oncol. 2017, 3, 961–968. [Google Scholar] [CrossRef]
- Persoon, S.; Kersten, M.J.; van der Weiden, K.; Buffart, L.M.; Nollet, F.; Brug, J.; Chinapaw, M.J. Effects of exercise in patients treated with stem cell transplantation for a hematologic malignancy: A systematic review and meta-analysis. Cancer Treat. Rev. 2013, 39, 682–690. [Google Scholar] [CrossRef]
- Gielissen, M.F.; Verhagen, S.; Witjes, F.; Bleijenberg, G. Effects of cognitive behavior therapy in severely fatigued disease-free cancer patients compared with patients waiting for cognitive behavior therapy: A randomized controlled trial. J. Clin. Oncol. 2006, 24, 4882–4887. [Google Scholar] [CrossRef]
- McCarney, R.; Warner, J.; Iliffe, S.; Van Haselen, R.; Griffin, M.; Fisher, P. The Hawthorne Effect: A randomised, controlled trial. BMC Med. Res. Methodol. 2007, 7, 30. [Google Scholar] [CrossRef]
- Junior, P.N.A.; Barreto, C.M.N.; Cubero, D.d.I.G.; Del Giglio, A. The efficacy of placebo for the treatment of cancer-related fatigue: A systematic review and meta-analysis. Support. Care Cancer 2020, 28, 1755–1764. [Google Scholar] [CrossRef]
- Servaes, P.; Verhagen, S.; Schreuder, H.B.; Veth, R.P.; Bleijenberg, G. Fatigue after treatment for malignant and benign bone and soft tissue tumors. J. Pain Symptom Manag. 2003, 26, 1113–1122. [Google Scholar] [CrossRef]
- Hjermstad, M.J.; Fosså, S.D.; Oldervoll, L.; Holte, H.; Jacobsen, A.B.; Loge, J.H. Fatigue in long-term Hodgkin’s Disease survivors: A follow-up study. J. Clin. Oncol. 2005, 23, 6587–6595. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.A.; Subnis, U.; Carlson, L.E.; Garland, S.N.; Santos-Iglesias, P.; Piedalue, K.-A.L.; Deleemans, J.M.; Campbell, T.S. Effects of a light therapy intervention on diurnal salivary cortisol in fatigued cancer survivors: A secondary analysis of a randomized controlled trial. J. Psychosom. Res. 2020, 139, 110266. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.E.; van Hees, V.T.; Mazzotti, D.R.; Marques-Vidal, P.; Sabia, S.; van der Spek, A.; Dashti, H.S.; Engmann, J.; Kocevska, D.; Tyrrell, J. Genetic studies of accelerometer-based sleep measures yield new insights into human sleep behaviour. Nat. Commun. 2019, 10, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Häusler, N.; Marques-Vidal, P.; Haba-Rubio, J.; Heinzer, R. Association between actigraphy-based sleep duration variability and cardiovascular risk factors–Results of a population-based study. Sleep Med. 2020, 66, 286–290. [Google Scholar] [CrossRef]
- Luik, A.I.; Zuurbier, L.A.; Direk, N.; Hofman, A.; Van Someren, E.J.; Tiemeier, H. 24-hour activity rhythm and sleep disturbances in depression and anxiety: A population-based study of middle-aged and older persons. Depress. Anxiety 2015, 32, 684–692. [Google Scholar] [CrossRef]
- Rogers, V.E.; Mowbray, C.; Zhu, S.; Liu, L.; Ancoli-Israel, S.; Barr, E.A.; Hinds, P.S. Circadian activity rhythms and fatigue of adolescent cancer survivors and healthy controls: A pilot study. J. Clin. Sleep Med. 2020, 16, 1141–1147. [Google Scholar] [CrossRef]
- Banthia, R.; Malcarne, V.L.; Roesch, S.C.; Ko, C.M.; Greenbergs, H.L.; Varni, J.W.; Sadler, G.R. Correspondence between daily and weekly fatigue reports in breast cancer survivors. J. Behav. Med. 2006, 29, 269–279. [Google Scholar] [CrossRef]
- Lam, R.; Levitt, A. Canadian Consensus Guidelines for the treatment of SAD. In A Summary of the Report of the Canadian Consensus Group on SAD; Clinical and Academic Publishing: Vancouver, BC, Canada, 1999. [Google Scholar]
- Bauer, M.; Bschor, T.; Pfennig, A.; Whybrow, P.C.; Angst, J.; Versiani, M.; Möller, H.-J.; WFSBP Task Force on Unipolar Depressive Disorders. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders in primary care. World J. Biol. Psychiatry 2007, 8, 67–104. [Google Scholar] [CrossRef]
- Segerstrom, S.C.; Boggero, I.A.; Smith, G.T.; Sephton, S.E. Variability and reliability of diurnal cortisol in younger and older adults: Implications for design decisions. Psychoneuroendocrinology 2014, 49, 299–309. [Google Scholar] [CrossRef]
- Kreissl, S.; Mueller, H.; Goergen, H.; Mayer, A.; Brillant, C.; Behringer, K.; Halbsguth, T.V.; Hitz, F.; Soekler, M.; Shonukan, O.; et al. Cancer-related fatigue in patients with and survivors of Hodgkin’s lymphoma: A longitudinal study of the German Hodgkin Study Group. Lancet Oncol. 2016, 17, 1453–1462. [Google Scholar] [CrossRef]
- Prue, G.; Rankin, J.; Allen, J.; Gracey, J.; Cramp, F. Cancer-related fatigue: A critical appraisal. Eur. J. Cancer 2006, 42, 846–863. [Google Scholar] [CrossRef]
- Servaes, P.; Verhagen, C.; Bleijenberg, G. Fatigue in cancer patients during and after treatment: Prevalence, correlates and interventions. Eur. J. Cancer 2002, 38, 27–43. [Google Scholar] [CrossRef]
- Van Faassen, M.; Bischoff, R.; Kema, I.P. Relationship between plasma and salivary melatonin and cortisol investigated by LC-MS/MS. Clin. Chem. Lab. Med. 2017, 55, 1340–1348. [Google Scholar] [CrossRef]
- Wust, S.; Wolf, J.; Hellhammer, D.H.; Federenko, I.; Schommer, N.; Kirschbaum, C. The cortisol awakening response-normal values and confounds. Noise Health 2000, 2, 79. [Google Scholar]
- Adam, E.K.; Kumari, M. Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology 2009, 34, 1423–1436. [Google Scholar] [CrossRef]
- Pruessner, J.C.; Kirschbaum, C.; Meinlschmid, G.; Hellhammer, D.H. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology 2003, 28, 916–931. [Google Scholar] [CrossRef]
- Smyth, N.; Thorn, L.; Hucklebridge, F.; Clow, A.; Evans, P. Assessment of the cortisol awakening response: Real-time analysis and curvilinear effects of sample timing inaccuracy. Psychoneuroendocrinology 2016, 74, 380–386. [Google Scholar] [CrossRef][Green Version]


| Variable | Assessment | Details |
|---|---|---|
| Primary Outcomes | ||
| Cancer-related fatigue | VAS-fatigue |
|
| MFI |
| |
| Restrictions caused by fatigue | WSAS |
|
| Secondary Outcomes | ||
| Sleep quality | PSQI |
|
| Depression | CES-D |
|
| Anxiety | STAI-6 |
|
| Quality of life | RAND-36 |
|
| Sleep | Wrist actigraphy |
|
| Cortisol | Salivary cortisol |
|
| Melatonin | Salivary melatonin |
|
| Characteristic | No. (%) b | p | N | |||
|---|---|---|---|---|---|---|
| All Survivors | BWL (n = 83) | DWL (n = 83) | ||||
| Age, years | 166 | |||||
| Mean | 45.7 | 46.7 | 44.8 | 0.30 | ||
| SD | 12.2 | 11.9 | 12.5 | |||
| Female | 99 (59.6) | 50 (60.2) | 49 (59.0) | 0.87 | 166 | |
| Education | 0.24 | 165 | ||||
| None/primary | 2 (1.2) | 0 (0.0) | 2 (2.4) | |||
| High school and vocational | 85 (51.5) | 43 (51.8) | 42 (51.2) | |||
| College or university | 78 (47.3) | 40 (48.2) | 38 (46.3) | |||
| Married or in relationship | 130 (78.8) | 71 (85.5) | 59 (72.0) | 0.03 | 165 | |
| Part- or full-time job | 85 (51.5) | 42 (50.6) | 43 (52.4) | 0.81 | 165 | |
| Chronotype | 0.44 | 165 | ||||
| Morning type | 29 (35.4) | 56 (33.9) | 27 (32.5) | |||
| Evening type | 33 (40.2) | 74 (44.8) | 41 (49.4) | |||
| No specific type | 20 (24.4) | 35 (21.2) | 15 (18.1) | |||
| Recruitment | 0.86 | 166 | ||||
| Asked by physician | 50 (30.1) | 24 (28.9) | 26 (31.3) | |||
| Survey study | 98 (59.0) | 49 (59.0) | 49 (59.0) | |||
| Applied for participation | 18 (10.8) | 10 (12.0) | 8 (9.6) | |||
| Diagnosis | 0.68 | 166 | ||||
| HL | 138 (83.1) | 70 (84.3) | 68 (81.9) | |||
| DLBCL | 28 (16.9) | 13 (15.7) | 15 (18.1) | |||
| Ann Arbor stage | 0.64 | 155 | ||||
| I | 21 (12.7) | 10 (12.0) | 11 (13.3) | |||
| II | 87 (52.4) | 40 (48.2) | 47 (56.6) | |||
| III | 25 (15.1) | 14 (16.9) | 11 (13.3) | |||
| IV | 22 (13.3) | 13 (15.7) | 9 (10.8) | |||
| Time since diagnosis, years c | 0.88 | 166 | ||||
| Mean | 12.9 | 13.0 | 12.9 | |||
| SD | 9.9 | 9.6 | 10.3 | |||
| 2–5 years | 41 (24.7) | 20 (24.1) | 21 (25.3) | 0.97 | ||
| 5–10 years | 50 (30.1) | 24 (28.9) | 26 (31.3) | |||
| 10–20 years | 39 (23.5) | 20 (24.1) | 19 (22.9) | |||
| >20 years | 36 (21.7) | 19 (22.9) | 17 (20.5) | |||
| Treatments received | ||||||
| Radiotherapy | 116 (72.0) | 56 (69.1) | 60 (75.0) | 0.41 | 161 | |
| Chemotherapy | 151 (93.2) | 76 (92.7) | 75 (93.8) | 0.79 | 162 | |
| Stem cell transplantation | 19 (11.8) | 8 (9.9) | 11 (13.8) | 0.45 | 161 | |
| Total body irradiation d | 2 (1.2) | 0 (0.0) | 2 (2.5) | 0.24 | 162 | |
| Surgery (splenectomy) d | 6 (3.7) | 3 (3.7) | 3 (3.8) | 1.0 | 162 | |
| Relapse | 25 (15.4) | 13 (15.9) | 12 (15.0) | 0.88 | 162 | |
| Second malignancies | 25 (15.7) | 13 (15.7) | 12 (15.4) | 0.91 | 159 | |
| Hyperthyroidism d,e | 1 (0.6) | 0 (0.0) | 1 (1.3) | 0.49 | 156 | |
| Hypothyroidism e | 36 (23.1) | 21 (26.3) | 15 (19.7) | 0.34 | 156 | |
| Heart complaints, NYHA class 1 or 2 | 33 (20.8) | 19 (23.5) | 14 (17.9) | 0.39 | 159 | |
| Fatigue (baseline) | ||||||
| VAS | 0.09 | 164 | ||||
| Mean | 6.1 | 5.9 | 6.3 | |||
| SD | 1.6 | 1.8 | 1.4 | |||
| MFI general fatigue | 0.76 | 165 | ||||
| Mean | 15.7 | 15.6 | 15.8 | |||
| SD | 2.7 | 2.9 | 2.5 | |||
| Work and social restrictions caused by fatigue (WSAS) | 0.73 | 165 | ||||
| Mean | 20.5 | 20.7 | 20.2 | |||
| SD | 8.2 | 7.8 | 8.5 | |||
| Sleep medication use | 25 (15.2) | 11 (13.3) | 14 (17.1) | 0.49 | 165 | |
| Characteristic | No. (%) a | p | N | |||
|---|---|---|---|---|---|---|
| All Survivors | BWL (n = 83) | DWL (n = 83) | ||||
| Season LT start | 0.94 | 164 | ||||
| Autumn | 42 (25.6) | 23 (27.7) | 19 (23.5) | |||
| Winter | 47 (28.7) | 23 (27.7) | 24 (29.6) | |||
| Spring | 47 (28.7) | 23 (27.7) | 24 (29.6) | |||
| Summer | 28 (17.1) | 14 (16.9) | 14 (17.3) | |||
| LT device | ||||||
| Litebook Edge | 37 (22.6) | 18 (21.7) | 19 (23.5) | 164 | ||
| Luminette | 127 (77.4) | 65 (78.3) | 62 (76.5) | 164 | ||
| Days of LT use based on LT diary b | 0.52 | 155 | ||||
| Mean | 22.7 | 22.5 | 22.9 | |||
| SD | 4.4 | 4.6 | 4.0 | |||
| >25 days c | 3 (1.9) | 0 (0.0) | 3 (3.9) | 0.13 | 155 | |
| 25 days | 58 (37.4) | 33 (41.8) | 25 (32.9) | |||
| 14–24 days | 87 (56.1) | 41 (51.9) | 46 (60.5) | |||
| 1–13 days (premature stop) | 7 (4.5) | 5 (6.3) | 2 (2.6) | |||
| Time difference sleep end and LT start (min) d | 0.13 | 155 | ||||
| Mean | 25.0 | 27.4 | 22.6 | |||
| SD | 19.5 | 22.6 | 15.3 | |||
| Time difference DLMO and LT start (h) | 0.17 | 45 | ||||
| Mean | 11.4 | 11.1 | 11.7 | |||
| SD | 1.5 | 1.0 | 1.9 | |||
| n | 45 | 23 | 22 | |||
| Self-reported side effects | ||||||
| Headache/nausea | 35 (21.6) | 21 (25.6) | 14 (17.5) | 0.21 | 162 | |
| Feeling agitated b | 5 (3.1) | 1 (1.2) | 4 (5.0) | 0.21 | 162 | |
| Tired eyes | 30 (18.5) | 11 (13.4) | 19 (23.8) | 0.09 | 162 | |
| Change in vision b | 8 (4.9) | 5 (6.1) | 3 (3.8) | 0.72 | 162 | |
| Other self-reported side effects e | 15 (9.3) | 6 (7.3) | 9 (11.3) | 0.39 | 162 | |
| Premature stop of LT | 13 (7.8) | 7 (8.4) | 6 (7.2) | 0.77 | 166 | |
| Reasons for premature stop b | 0.21 | 13 | ||||
| Self-reported side effects | 7 (53.8) | 5 (71.4) | 2 (33.3) | |||
| No time or personal circumstances | 6 (46.2) | 2 (28.6) | 4 (66.7) | |||
| Outcome | T0-T1 a | T0-T2 a | T0-T3 a | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. (%) | No. (%) | No. (%) | |||||||||||
| BWL | DWL | pb | OR c | BWL | DWL | pb | OR c | BWL | DWL | pb | OR c | ||
| VAS fatigue | |||||||||||||
| Improved | 34 (42) | 41 (55) | 0.11 | 0.60 | 25 (35) | 37 (52) | 0.04 | 0.50 | 24 (33) | 27 (39) | 0.48 | 0.78 | |
| Not improved | 47 (58) | 34 (45) | 46 (65) | 34 (48) | 49 (67) | 43 (61) | |||||||
| n | 81 | 75 | 71 | 71 | 73 | 70 | |||||||
| MFI general fatigue | |||||||||||||
| Improved | 49 (60) | 47 (63) | 0.71 | 0.89 | 35 (49) | 37 (52) | 0.68 | 0.87 | 36 (49) | 40 (57) | 0.31 | 0.71 | |
| Not improved | 33 (40) | 28 (37) | 37 (51) | 34 (48) | 38 (51) | 30 (43) | |||||||
| n | 82 | 75 | 72 | 71 | 74 | 70 | |||||||
| WSAS | |||||||||||||
| Improved | 33 (40) | 26 (35) | 0.47 | 1.27 | 31 (43) | 27 (39) | 0.59 | 1.20 | 31 (42) | 29 (41) | 0.96 | 1.02 | |
| Not improved | 49 (60) | 49 (65) | 41 (57) | 43 (61) | 43 (58) | 41 (59) | |||||||
| n | 82 | 75 | 72 | 70 | 74 | 70 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Starreveld, D.E.J.; Daniels, L.A.; Kieffer, J.M.; Valdimarsdottir, H.B.; de Geus, J.; Lanfermeijer, M.; van Someren, E.J.W.; Habers, G.E.A.; Bosch, J.A.; Janus, C.P.M.; et al. Light Therapy for Cancer-Related Fatigue in (Non-)Hodgkin Lymphoma Survivors: Results of a Randomized Controlled Trial. Cancers 2021, 13, 4948. https://doi.org/10.3390/cancers13194948
Starreveld DEJ, Daniels LA, Kieffer JM, Valdimarsdottir HB, de Geus J, Lanfermeijer M, van Someren EJW, Habers GEA, Bosch JA, Janus CPM, et al. Light Therapy for Cancer-Related Fatigue in (Non-)Hodgkin Lymphoma Survivors: Results of a Randomized Controlled Trial. Cancers. 2021; 13(19):4948. https://doi.org/10.3390/cancers13194948
Chicago/Turabian StyleStarreveld, Daniëlle E. J., Laurien A. Daniels, Jacobien M. Kieffer, Heiddis B. Valdimarsdottir, Jessie de Geus, Mirthe Lanfermeijer, Eus J. W. van Someren, G. Esther A. Habers, Jos A. Bosch, Cécile P. M. Janus, and et al. 2021. "Light Therapy for Cancer-Related Fatigue in (Non-)Hodgkin Lymphoma Survivors: Results of a Randomized Controlled Trial" Cancers 13, no. 19: 4948. https://doi.org/10.3390/cancers13194948
APA StyleStarreveld, D. E. J., Daniels, L. A., Kieffer, J. M., Valdimarsdottir, H. B., de Geus, J., Lanfermeijer, M., van Someren, E. J. W., Habers, G. E. A., Bosch, J. A., Janus, C. P. M., van Spronsen, D. J., de Weijer, R. J., Marijt, E. W. A., de Jongh, E., Zijlstra, J. M., Böhmer, L. H., Houmes, M., Kersten, M. J., Korse, C. M., ... Bleiker, E. M. A. (2021). Light Therapy for Cancer-Related Fatigue in (Non-)Hodgkin Lymphoma Survivors: Results of a Randomized Controlled Trial. Cancers, 13(19), 4948. https://doi.org/10.3390/cancers13194948






