Fertility Preservation and Long-Term Monitoring of Gonadotoxicity in Girls, Adolescents and Young Adults Undergoing Cancer Treatment
Abstract
:Simple Summary
Abstract
1. Introduction
2. Agents Affecting Fertility
2.1. Chemotherapy
2.2. Radiotherapy
2.3. Hematopoietic Stem Cell Transplantation (HSCT)
3. Fertility Preservation Methods
3.1. Fertility Preservation
3.2. Fertility Restoration
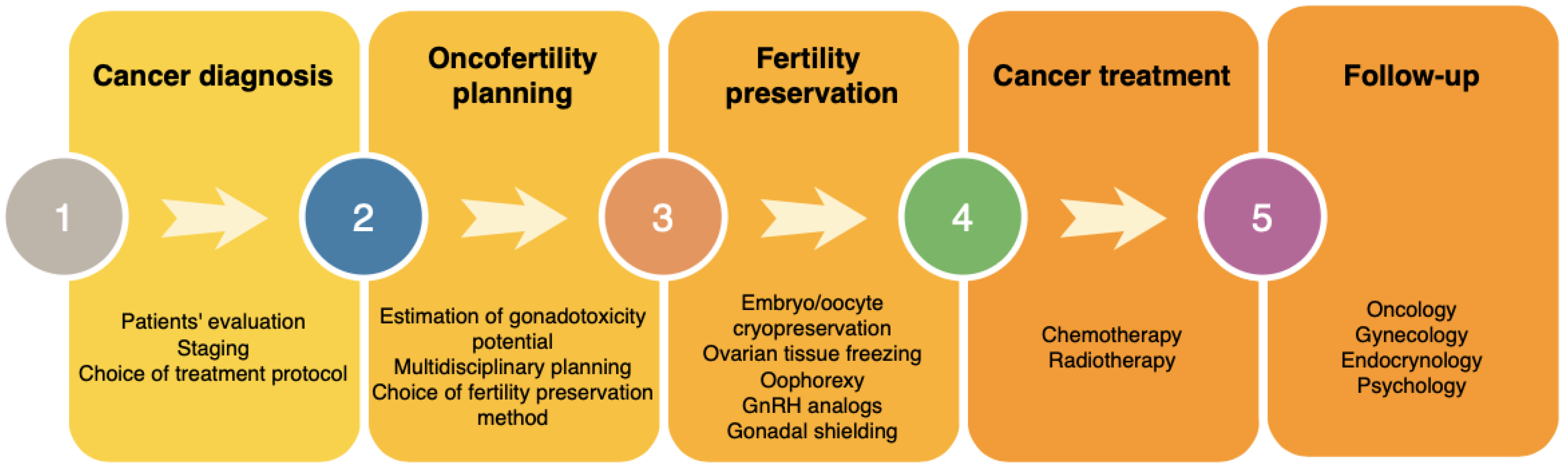
4. Oncofertility Management
5. Psychological Aspects
6. Ethical Considerations
7. Follow-Up and Survivorship Care
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, D.; Jemal, A. Cancer statistics, 2017. CA Cancer J. Clin. 2017, 67, 7–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marchak, J.G.; Elchuri, S.V.; Vangile, K.; Wasilewski-Masker, K.; Mertens, A.C.; Meacham, L.R. Perceptions of Infertility Risks Among Female Pediatric Cancer Survivors Following Gonadotoxic Therapy. J. Pediatr. Hematol. 2015, 37, 368–372. [Google Scholar] [CrossRef] [PubMed]
- Logan, S.; Perz, J.; Ussher, J.M.; Peate, M.; Anazodo, A. Systematic review of fertility-related psychological distress in cancer patients: Informing on an improved model of care. Psycho-Oncology 2019, 28, 22–30. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Logan, S.; Stern, K.; Wakefield, C.E.; Cohn, R.J.; Agresta, F.; Jayasinghe, Y.; Deans, R.; Segelov, E.; McLachlan, R.I.; et al. Supportive oncofertility care, psychological health and reproductive concerns: A qualitative study. Support. Care Cancer 2019, 28, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.A.; Mitchell, R.T.; Kelsey, T.W.; Spears, N.; Telfer, E.E.; Wallace, W.H.B. Cancer treatment and gonadal function: Experimental and established strategies for fertility preservation in children and young adults. Lancet Diabetes Endocrinol. 2015, 3, 556–567. [Google Scholar] [CrossRef] [Green Version]
- Loren, A.; Mangu, P.; Beck, L.; Brennan, L.; Magdalinski, A.J.; Partridge, A.H.; Quinn, G.; Wallace, W.H.; Oktay, K. Fertility Preservation for Patients With Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2013, 31, 2500–2510. [Google Scholar] [CrossRef] [PubMed]
- Peccatori, F.A.; Azim, J.H.A.; Orecchia, R.; Hoekstra, H.J.; Pavlidis, N.; Kesic, V.; Pentheroudakis, G. Cancer, pregnancy and fertility: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2013, 24, vi160–vi170. [Google Scholar] [CrossRef]
- Kim, H.; Ku, S.-Y. Fertility preservation in pediatric and young adult female cancer patients. Ann. Pediatr. Endocrinol. Metab. 2018, 23, 70–74. [Google Scholar] [CrossRef] [Green Version]
- Byrne, J.; Fears, T.R.; Gail, M.; Pee, D.; Connelly, R.R.; Austin, D.F.; Holmes, G.F.; Holmes, F.F.; Latourette, H.B.; Meigs, J.W. Early menopause in long-term survivors of cancer during adolescence. Am. J. Obstet. Gynecol. 1992, 166, 788–793. [Google Scholar] [CrossRef]
- Sklar, C.A.; Mertens, A.C.; Mitby, P.; Whitton, J.; Stovall, M.; Kasper, C.; Mulder, J.; Green, D.; Nicholson, H.S.; Yasui, Y.; et al. Premature Menopause in Survivors of Childhood Cancer: A Report From the Childhood Cancer Survivor Study. J. Natl. Cancer Inst. 2006, 98, 890–896. [Google Scholar] [CrossRef]
- Poorvu, P.D.; Frazier, A.L.; Feraco, A.M.; E Manley, P.; Ginsburg, E.S.; Laufer, M.R.; LaCasce, A.S.; Diller, L.R.; Partridge, A.H. Cancer Treatment-Related Infertility: A Critical Review of the Evidence. JNCI Cancer Spectr. 2019, 3, pkz008. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Schover, L.R.; Partridge, A.H.; Patrizio, P.; Wallace, W.H.; Hagerty, K.; Beck, L.N.; Brennan, L.V.; Oktay, K. American Society of Clinical Oncology Recommendations on Fertility Preservation in Cancer Patients. J. Clin. Oncol. 2006, 24, 2917–2931. [Google Scholar] [CrossRef] [PubMed]
- Lambertini, M.; Peccatori, F.; Demeestere, I.; Amant, F.; Wyns, C.; Stukenborg, J.-B.; Paluch-Shimon, S.; Halaska, M.; Uzan, C.; Meissner, J.; et al. Fertility preservation and post-treatment pregnancies in post-pubertal cancer patients: ESMO Clinical Practice Guidelines. Ann. Oncol. 2020, 31, 1664–1678. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.; Canada, A.; Stern, C.J. Fertility Preservation in Adolescents and Young Adults With Cancer. J. Clin. Oncol. 2010, 28, 4831–4841. [Google Scholar] [CrossRef]
- Wallace, W.H.B.; A Anderson, R.; Irvine, D.S. Fertility preservation for young patients with cancer: Who is at risk and what can be offered? Lancet Oncol. 2005, 6, 209–218. [Google Scholar] [CrossRef]
- Overbeek, A.; Van den Berg, H.; Van Leeuwen, F.E.; Kaspers, G.J.; Lambalk, C.B.; Van Dulmen-den Broeder, E. Chemotherapy-related late adverse effects on ovarian function in female survivors of childhood and young adult cancer: A systematic review. Cancer Treat. Rev. 2017, 53, 10–24. [Google Scholar] [CrossRef]
- Chemaitilly, W.; Mertens, A.C.; Mitby, P.; Whitton, J.; Stovall, M.; Yasui, Y.; Robison, L.L.; Sklar, C.A. Acute Ovarian Failure in the Childhood Cancer Survivor Study. J. Clin. Endocrinol. Metab. 2006, 91, 1723–1728. [Google Scholar] [CrossRef]
- Stroud, J.S.; Mutch, D.; Rader, J.; Powell, M.; Thaker, P.H.; Grigsby, P.W. Special Contributions Effects of cancer treatment on ovarian function. Fertil. Steril. 2009, 92, 417–427. [Google Scholar] [CrossRef]
- Wo, J.Y.; Viswanathan, A.N. Impact of Radiotherapy on Fertility, Pregnancy, and Neonatal Outcomes in Female Cancer Patients. Int. J. Radiat. Oncol. 2009, 73, 1304–1312. [Google Scholar] [CrossRef] [Green Version]
- Lambertini, M.; Del Mastro, L.; Pescio, M.M.; Andersen, C.Y.C.; Azim, H.H.A.; Peccatori, F.A.; Costa, M.M.; Revelli, A.A.; Salvagno, F.F.; Gennari, A.; et al. Cancer and fertility preservation: International recommendations from an expert meeting. BMC Med. 2016, 14, 1. [Google Scholar] [CrossRef]
- Behringer, K.; Mueller, H.; Goergen, H.; Thielen, I.; Eibl, A.D.; Stumpf, V.; Wessels, C.; Wiehlpütz, M.; Rosenbrock, J.; Halbsguth, T.; et al. Gonadal Function and Fertility in Survivors After Hodgkin Lymphoma Treatment Within the German Hodgkin Study Group HD13 to HD15 Trials. J. Clin. Oncol. 2013, 31, 231–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Der Kaaij, M.A.E.; Heutte, N.; Meijnders, P.; Abeilard-Lemoisson, E.; Spina, M.; Moser, E.C.; Allgeier, A.; Meulemans, B.; Simons, A.H.M.; Lugtenburg, P.J.; et al. Premature Ovarian Failure and Fertility in Long-Term Survivors of Hodgkin’s Lymphoma: A European Organisation for Research and Treatment of Cancer Lymphoma Group and Groupe d’Étude des Lymphomes de l’Adulte Cohort Study. J. Clin. Oncol. 2012, 30, 291–299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wallace, W.; Thomson, A.B.; Kelsey, T.W. The radiosensitivity of the human oocyte. Hum. Reprod. 2003, 18, 117–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wallace, W.; Shalet, S.; Crowne, E.; Morris-Jones, P.; Gattamaneni, H. Ovarian failure following abdominal irradiation in childhood: Natural history and prognosis. Clin. Oncol. 1989, 1, 75–79. [Google Scholar] [CrossRef]
- Bath, L.E.; Wallace, W.; Shaw, M.; Fitzpatrick, C.; Anderson, R.A. Depletion of ovarian reserve in young women after treatment for cancer in childhood: Detection by anti-Mullerian hormone, inhibin B and ovarian ultrasound. Hum. Reprod. 2003, 18, 2368–2374. [Google Scholar] [CrossRef] [Green Version]
- Bath, L.E.; Anderson, R.A.; Critchley, H.O.D.; Kelnar, C.J.; Wallace, W.B. Hypothalamic–pituitary–ovarian dysfunction after prepubertal chemotherapy and cranial irradiation for acute leukaemia. Hum. Reprod. 2001, 16, 1838–1844. [Google Scholar] [CrossRef] [Green Version]
- Wallace, W.H.B.; Thomson, A.B.; Saran, F.; Kelsey, T.W. Predicting age of ovarian failure after radiation to a field that includes the ovaries. Int. J. Radiat. Oncol. 2005, 62, 738–744. [Google Scholar] [CrossRef]
- Green, D.M.; Peabody, E.M.; Nan, B.; Peterson, S.; Kalapurakal, J.A.; Breslow, N.E. Pregnancy Outcome After Treatment for Wilms Tumor: A Report From the National Wilms Tumor Study Group. J. Clin. Oncol. 2002, 20, 2506–2513. [Google Scholar] [CrossRef]
- Signorello, L.B.; Cohen, S.S.; Bosetti, C.; Stovall, M.; Kasper, C.E.; Weathers, R.E.; Whitton, J.A.; Green, D.M.; Donaldson, S.S.; Mertens, A.C.; et al. Female Survivors of Childhood Cancer: Preterm Birth and Low Birth Weight Among Their Children. J. Natl. Cancer Inst. 2006, 98, 1453–1461. [Google Scholar] [CrossRef]
- Marci, R.; Mallozzi, M.; Di Benedetto, L.; Schimberni, M.; Mossa, S.; Soave, I.; Palomba, S.; Caserta, D. Radiations and female fertility. Reprod. Biol. Endocrinol. 2018, 16, 112. [Google Scholar] [CrossRef]
- Ogilvy-Stuart, A.L.; Shalet, S.M. Effect of radiation on the human reproductive system. Environ. Health Perspect. 1993, 101 (Suppl. S2), 109–116. [Google Scholar] [PubMed]
- Green, D.M.; Whitton, J.A.; Stovall, M.; Mertens, A.C.; Donaldson, S.S.; Ruymann, F.B.; Pendergrass, T.W.; Robison, L.L. Pregnancy outcome of female survivors of childhood cancer: A report from the childhood cancer survivor study. Am. J. Obstet. Gynecol. 2002, 187, 1070–1080. [Google Scholar] [CrossRef] [PubMed]
- Algarroba, G.N.; Sanfilippo, J.S.; Valli-Pulaski, H. Female fertility preservation in the pediatric and adolescent cancer patient population. Best Pr. Res. Clin. Obstet. Gynaecol. 2018, 48, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Webber, L.; Davies, M.; Anderson, R.; Bartlett, J.; Braat, D.; Cartwright, B.; Cifkova, R.; Keizer-Schrama, S.D.M.; Hogervorst, E.; Janse, F.; et al. ESHRE Guideline: Management of women with premature ovarian insufficiency. Hum. Reprod. 2016, 31, 926–937. [Google Scholar]
- Findlay, J.K.; Hutt, K.J.; Hickey, M.; Anderson, R.A. How Is the Number of Primordial Follicles in the Ovarian Reserve Established? Biol. Reprod. 2015, 93, 111. [Google Scholar] [CrossRef]
- Green, D.M.; Sklar, C.A.; Boice, J.D.; Mulvihill, J.J.; Whitton, J.A.; Stovall, M.; Yasui, Y. Ovarian Failure and Reproductive Outcomes After Childhood Cancer Treatment: Results From the Childhood Cancer Survivor Study. J. Clin. Oncol. 2009, 27, 2374–2381. [Google Scholar] [CrossRef] [Green Version]
- Van Dorp, W.; Mulder, R.L.; Kremer, L.C.; Hudson, M.M.; Heuvel-Eibrink, M.M.V.D.; Berg, M.H.V.D.; Levine, J.M.; Broeder, E.V.D.-D.; Di Iorgi, N.; Albanese, A.; et al. Recommendations for Premature Ovarian Insufficiency Surveillance for Female Survivors of Childhood, Adolescent, and Young Adult Cancer: A Report From the International Late Effects of Childhood Cancer Guideline Harmonization Group in Collaboration With the PanCareSurFup Consortium. J. Clin. Oncol. 2016, 34, 3440–3450. [Google Scholar]
- Tauchmanovà, L.; Selleri, C.; De Rosa, G.; Esposito, M.; Jr, F.O.; Palomba, S.; Bifulco, G.; Nappi, C.; Lombardi, G.; Rotoli, B.; et al. Gonadal status in reproductive age women after haematopoietic stem cell transplantation for haematological malignancies. Hum. Reprod. 2003, 18, 1410–1416. [Google Scholar]
- Tauchmanovà, L.; Selleri, C.; De Rosa, G.; Sammartino, A.; Di Carlo, C.; Musella, T.; Martorelli, C.; Lombardi, G.; Rotoli, B.; Nappi, C.; et al. Estrogen-progestin therapy in women after stem cell transplant: Our experience and literature review. Menopause 2007, 14, 320–330. [Google Scholar]
- Guida, M.; Castaldi, M.A.; Rosamilio, R.; Giudice, V.; Orio, F.; Selleri, C. Reproductive issues in patients undergoing Hematopoietic Stem Cell Transplantation: An update. J. Ovarian Res. 2016, 9, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Orio, F.; Muscogiuri, G.; Palomba, S.; Serio, B.; Sessa, M.; Giudice, V.; Ferrara, I.; Tauchmanovà, L.; Colao, A.; Selleri, C. Endocrinopathies after Allogeneic and Autologous Transplantation of Hematopoietic Stem Cells. Sci. World J. 2014, 2014, 282147. [Google Scholar] [CrossRef] [PubMed]
- Lawrenz, B.; Rothmund, R.; Neunhoeffer, E.; Huebner, S.; Henes, M. Fertility Preservation in Prepubertal Girls Prior to Chemotherapy and Radiotherapy—Review of the Literature. J. Pediatr. Adolesc. Gynecol. 2012, 25, 284–288. [Google Scholar] [CrossRef]
- Salama, M.; Anazodo, A.; Woodruff, T.K. Preserving fertility in female patients with hematological malignancies: A multidisciplinary oncofertility approach. Ann. Oncol. 2019, 30, 1760–1775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salama, M.; Winkler, K.; Murach, K.F.; Seeber, B.; Ziehr, S.C.; Wildt, L. Female fertility loss and preservation: Threats and opportunities. Ann. Oncol. 2013, 24, 598–608. [Google Scholar] [CrossRef] [PubMed]
- Meirow, D.; Ra’Anani, H.; Shapira, M.; Brenghausen, M.; Chaim, S.D.; Aviel-Ronen, S.; Amariglio, N.; Schiff, E.; Orvieto, R.; Dor, J. Transplantations of frozen-thawed ovarian tissue demonstrate high reproductive performance and the need to revise restrictive criteria. Fertil. Steril. 2016, 106, 467–474. [Google Scholar] [CrossRef] [Green Version]
- Chang, E.M.; Song, H.S.; Lee, D.R.; Lee, W.S.; Yoon, T.K. In vitro maturation of human oocytes: Its role in infertility treatment and new possibilities. Clin. Exp. Reprod. Med. 2014, 41, 41–46. [Google Scholar] [CrossRef] [Green Version]
- Morice, P.; Castaigne, D.; Haie-Meder, C.; Pautier, P.; El Hassan, J.; Duvillard, P.; Gerbaulet, A.; Michel, G. Laparoscopic ovarian transposition for pelvic malignancies: Indications and functional outcomes. Fertil. Steril. 1998, 70, 956–960. [Google Scholar] [CrossRef]
- Pahisa, J.; Martínez-Román, S.; Martínez-Zamora, M.A.; Torné, A.; Caparrós, X.; Sanjuán, A.; Lejárcegui, J.A. Laparoscopic ovarian transposition in patients with early cervical cancer. Int. J. Gynecol. Cancer 2008, 18, 584–589. [Google Scholar] [CrossRef]
- Von Wolff, M.; Capp, E.; Jauckus, J.; Strowitzki, T.; Germeyer, A. Timing of ovarian stimulation in patients prior to gonadotoxic therapy: An analysis of 684 stimulations. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 199, 146–149. [Google Scholar] [CrossRef]
- Cakmak, H.; Rosen, M.P. Ovarian stimulation in cancer patients. Fertil. Steril. 2013, 99, 1476–1484. [Google Scholar] [CrossRef]
- Nakasuji, T.; Kawai, K.; Ishikawa, T.; Teraoka, K.; Takeuchi, S.; Miyagawa, T.; Nara, K.; Kidera, N.; Harada, T.; Miyasaka, N. Random-start ovarian stimulation with aromatase inhibitor for fertility preservation in women with Japanese breast cancer. Reprod. Med. Biol. 2019, 18, 167–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodriguez-Wallberg, K.A.; Oktay, K. Fertility Preservation in Women With Breast Cancer. Clin. Obstet. Gynecol. 2010, 53, 753–762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reddy, J.; Oktay, K. Ovarian stimulation and fertility preservation with the use of aromatase inhibitors in women with breast cancer. Fertil. Steril. 2012, 98, 1363–1369. [Google Scholar] [CrossRef]
- Massarotti, C.; Scaruffi, P.P.; Lambertini, M.; Remorgida, V.V.; Del Mastro, L.; Anserini, P.P. State of the art on oocyte cryopreservation in female cancer patients: A critical review of the literature. Cancer Treat. Rev. 2017, 57, 50–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levi-Setti, P.E.; Patrizio, P.; Scaravelli, G. Evolution of human oocyte cryopreservation: Slow freezing versus vitrification. Curr. Opin. Endocrinol. Diabetes Obes. 2016, 23, 445–450. [Google Scholar] [CrossRef]
- Poirot, C.; Brugieres, L.; Yakouben, K.; Prades-Borio, M.; Marzouk, F.; De Lambert, G.; Pacquement, H.; Bernaudin, F.; Neven, B.; Paye-Jaouen, A.; et al. Ovarian tissue cryopreservation for fertility preservation in 418 girls and adolescents up to 15 years of age facing highly gonadotoxic treatment. Twenty years of experience at a single center. Acta Obstet. Gynecol. Scand. 2019, 98, 630–637. [Google Scholar] [CrossRef] [Green Version]
- Demeestere, I.; Simon, P.; Dedeken, L.; Moffa, F.; Tsépélidis, S.; Brachet, C.; Delbaere, A.; Devreker, F.; Ferster, A. Live birth after autograft of ovarian tissue cryopreserved during childhood: Figure 1. Hum. Reprod. 2015, 30, 2107–2109. [Google Scholar] [CrossRef] [Green Version]
- Findeklee, S.; Radosa, J.C.; Takacs, Z.; Hamza, A.; Sima, R.; Solomayer, E.; Sklavounos, P. Fertility preservation in female cancer patients: Current knowledge and future perspectives. Minerva Ginecol. 2019, 71, 298–305. [Google Scholar] [CrossRef]
- Wallace, W.H.; Kelsey, T.W.; Anderson, R.A. Fertility preservation in pre-pubertal girls with cancer: The role of ovarian tissue cryopreservation. Fertil. Steril. 2016, 105, 6–12. [Google Scholar] [CrossRef] [Green Version]
- Shi, Q.; Xie, Y.; Wang, Y.; Li, S. Vitrification versus slow freezing for human ovarian tissue cryopreservation: A systematic review and meta-anlaysis. Sci. Rep. 2017, 7, 1–9. [Google Scholar] [CrossRef]
- Oktay, K.; Cil, A.P.; Bang, H. Efficiency of oocyte cryopreservation: A meta-analysis. Fertil. Steril. 2006, 86, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Salama, M.; Anazodo, A.; Woodruff, T.K. Preserving fertility in female patients with hematological malignancies: The key points. Expert Rev. Hematol. 2019, 12, 375–377. [Google Scholar] [CrossRef] [PubMed]
- Oktay, K.; Harvey, B.E.; Partridge, A.H.; Quinn, G.P.; Reinecke, J.; Taylor, H.S.; Wallace, W.H.; Wang, E.T.; Loren, A.W. Fertility Preservation in Patients With Cancer: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. 2018, 36, 1994–2001. [Google Scholar] [CrossRef] [PubMed]
- Del Mastro, L.; Ceppi, M.; Poggio, F.; Bighin, C.; Peccatori, F.A.; Demeestere, I.; Levaggi, A.; Giraudi, S.; Lambertini, M.; D’Alonzo, A.; et al. Gonadotropin-releasing hormone analogues for the prevention of chemotherapy-induced premature ovarian failure in cancer women: Systematic review and meta-analysis of randomized trials. Cancer Treat. Rev. 2014, 40, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Chen, M.; Fu, F.; Huang, M. Gonadotropin-Releasing Hormone Analog Cotreatment for the Preservation of Ovarian Function during Gonadotoxic Chemotherapy for Breast Cancer: A Meta-Analysis. PLoS ONE 2013, 8, e66360. [Google Scholar] [CrossRef]
- Bedaiwy, M.A.; Abou-Setta, A.M.; Desai, N.; Hurd, W.; Starks, D.; El-Nashar, S.A.; Al-Inany, H.G.; Falcone, T. Gonadotropin-releasing hormone analog cotreatment for preservation of ovarian function during gonadotoxic chemotherapy: A systematic review and meta-analysis. Fertil. Steril. 2011, 95, 906–914.e4. [Google Scholar] [CrossRef]
- Del Mastro, L.; Boni, L.; Michelotti, A.; Gamucci, T.; Olmeo, N.; Gori, S.; Giordano, M.; Garrone, O.; Pronzato, P.; Bighin, C.; et al. Marco Venturini Effect of the gonadotropin-releasing hormone analogue triptorelin on the occurrence of chemotherapy-induced early menopause in premenopausal women with breast cancer: A randomized tria. JAMA J. Am. Med. Assoc. 2011, 306, 269–276. [Google Scholar]
- Clowse, M.E.; Behera, M.A.; Anders, C.K.; Copland, S.; Coffman, C.J.; Leppert, P.C.; Bastian, L.A. Ovarian Preservation by GnRH Agonists during Chemotherapy: A Meta-Analysis. J. Women’s Heal. 2009, 18, 311–319. [Google Scholar] [CrossRef] [Green Version]
- Meli, M.; Caruso-Nicoletti, M.; La Spina, M.; Nigro, L.L.; Samperi, P.; D’Amico, S.; Bellia, F.; Miraglia, V.; Licciardello, M.; Cannata, E.; et al. Triptorelin for Fertility Preservation in Adolescents Treated With Chemotherapy for Cancer. J. Pediatr. Hematol. 2018, 40, 269–276. [Google Scholar] [CrossRef]
- Kumar, P.; Sharma, A. Gonadotropin-releasing hormone analogs: Understanding advantages and limitations. J. Hum. Reprod. Sci. 2014, 7, 170–174. [Google Scholar] [CrossRef]
- Osborne, S.; Detti, L. GnRH-Analogues for Ovarian Protection in Childhood Cancer Patients: How Adult Hypotheses are Relevant in Prepubertal Females. Curr. Drug Targets 2013, 14, 856–863. [Google Scholar] [CrossRef] [PubMed]
- Leonard, R.C.F.; Adamson, D.J.A.; Bertelli, G.; Mansi, J.; Yellowlees, A.; Dunlop, J.; Thomas, G.; Coleman, R.E.; Anderson, R.A. GnRH agonist for protection against ovarian toxicity during chemotherapy for early breast cancer: The Anglo Celtic Group OPTION trial. Ann. Oncol. 2017, 28, 1811–1816. [Google Scholar] [CrossRef] [PubMed]
- Tsampras, N.; Gould, D.; Fitzgerald, C.T. Double ovarian stimulation (DuoStim) protocol for fertility preservation in female oncology patients. Hum. Fertil. 2017, 20, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Rienzi, L.; Gracia, C.; Maggiulli, R.; LaBarbera, A.R.; Kaser, D.J.; Ubaldi, F.M.; Vanderpoel, S.; Racowsky, C. Oocyte, embryo and blastocyst cryopreservation in ART: Systematic review and meta-analysis comparing slow-freezing versus vitrification to produce evidence for the development of global guidance. Hum. Reprod. Updat. 2016, 23, 139–155. [Google Scholar] [CrossRef] [PubMed]
- Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. In vitro maturation: A committee opinion. Fertil. Steril. 2013, 99, 663–666. [Google Scholar] [CrossRef] [PubMed]
- Chian, R.; Uzelac, P.S.; Nargund, G. In vitro maturation of human immature oocytes for fertility preservation. Fertil. Steril. 2013, 99, 1173–1181. [Google Scholar] [CrossRef]
- Berwanger, A.L.; Finet, A.; El Hachem, H.; Le Parco, S.; Hesters, L.; Grynberg, M. New trends in female fertility preservation: In vitro maturation of oocytes. Futur. Oncol. 2012, 8, 1567–1573. [Google Scholar] [CrossRef]
- Silber, S.J.; Woodruff, T.K.; Shea, L.D. To Transplant or Not to Transplant—That Is the Question. Cancer Treat. Res. 2010, 156, 41–54. [Google Scholar]
- Maman, E.; Meirow, D.; Brengauz, M.; Raanani, H.; Dor, J.; Hourvitz, A. Luteal phase oocyte retrieval and in vitro maturation is an optional procedure for urgent fertility preservation. Fertil. Steril. 2011, 95, 64–67. [Google Scholar] [CrossRef] [PubMed]
- Creux, H.; Monnier, P.; Son, W.-Y.; Tulandi, T.; Buckett, W. Immature oocyte retrieval and in vitro oocyte maturation at different phases of the menstrual cycle in women with cancer who require urgent gonadotoxic treatment. Fertil. Steril. 2017, 107, 198–204. [Google Scholar] [CrossRef] [Green Version]
- Boots, C.E.; Meister, M.; Cooper, A.R.; Hardi, A.; Jungheim, E.S. Ovarian stimulation in the luteal phase: Systematic review and meta-analysis. J. Assist. Reprod. Genet. 2016, 33, 971–980. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ellenbogen, A.; Shavit, T.; Shalom-Paz, E. IVM results are comparable and may have advantages over standard IVF. Facts Views Vis. ObGyn 2014, 6, 77–80. [Google Scholar] [PubMed]
- Gellert, S.E.; Pors, S.E.; Kristensen, S.G.; Bay-Bjørn, A.M.; Ernst, E.; Andersen, C.Y. Transplantation of frozen-thawed ovarian tissue: An update on worldwide activity published in peer-reviewed papers and on the Danish cohort. J. Assist. Reprod. Genet. 2018, 35, 561–570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ladanyi, C.; Mor, A.; Christianson, M.S.; Dhillon, N.; Segars, J.H. Recent advances in the field of ovarian tissue cryopreservation and opportunities for research. J. Assist. Reprod. Genet. 2017, 34, 709–722. [Google Scholar] [CrossRef]
- Lang, M.J.; Giese-Davis, J.; Patten, S.B.; Campbell, D.J.T. Does age matter? Comparing post-treatment psychosocial outcomes in young adult and older adult cancer survivors with their cancer-free peers. Psycho-Oncology 2017, 27, 1404–1411. [Google Scholar] [CrossRef] [Green Version]
- Rosen, A.; Rodriguez-Wallberg, K.A.; Rosenzweig, L. Psychosocial Distress in Young Cancer Survivors. Semin. Oncol. Nurs. 2009, 25, 268–277. [Google Scholar] [CrossRef]
- Schover, L.R.; Rybicki, L.A.; Martin, B.A.; Bringelsen, K.A. Having children after cancer: A pilot survey of survivors’ attitudes and experiences. Cancer 1999, 86, 697–709. [Google Scholar] [CrossRef]
- Carter, J.; Rowland, K.; Chi, D.; Brown, C.; Abu-Rustum, N.; Castiel, M.; Barakat, R. Gynecologic cancer treatment and the impact of cancer-related infertility. Gynecol. Oncol. 2005, 97, 90–95. [Google Scholar] [CrossRef]
- Assi, J.; Santos, J.; Bonetti, T.; Serafini, P.C.; Motta, E.L.A.; Chehin, M.B. Psychosocial benefits of fertility preservation for young cancer patients. J. Assist. Reprod. Genet. 2018, 35, 601–606. [Google Scholar] [CrossRef]
- Treves, R.; Grynberg, M.; Parco, S.; Finet, A.; Poulain, M.; Fanchin, R. Female fertility preservation in cancer patients: An instrumental tool for the envisioning a postdisease life. Futur. Oncol. 2014, 10, 969–974. [Google Scholar] [CrossRef] [PubMed]
- Sullivan-Pyke, C.S.; Carlson, C.A.; Prewitt, M.; Gracia, C.R.; Ginsberg, J.P. Ovarian tissue cryopreservation (OTC) in prepubertal girls and young women: An analysis of parents’ and patients’ decision-making. J. Assist. Reprod. Genet. 2018, 35, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Jayasinghe, Y.L.; Kemertzis, M.A.; Moore, P.; Peate, M. Fertility Preservation in Pediatric and Adolescent Oncology Patients: The Decision-Making Process of Parents. J. Adolesc. Young Adult Oncol. 2017, 6, 213–222. [Google Scholar] [CrossRef]
- Duffy, C.; Allen, S. Medical and psychosocial aspects of fertility after cancer. Cancer J. 2009, 15, 27–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deepinder, F.; Agarwal, A. Technical and ethical challenges of fertility preservation in young cancer patients. Reprod. Biomed. Online 2008, 16, 784–791. [Google Scholar] [CrossRef]
- McDougall, R.J.; Gillam, L.; Delany, C.; Jayasinghe, Y. Ethics of fertility preservation for prepubertal children: Should clinicians offer procedures where efficacy is largely unproven? J. Med. Ethic 2017, 44, 27–31. [Google Scholar] [CrossRef] [Green Version]
- Signorello, L.B.; Mulvihill, J.J.; Green, D.M.; Munro, H.M.; Stovall, M.; Weathers, R.E.; Mertens, A.C.; Whitton, J.A.; Robison, L.L.; Boice, J.D. Congenital Anomalies in the Children of Cancer Survivors: A Report From the Childhood Cancer Survivor Study. J. Clin. Oncol. 2012, 30, 239–245. [Google Scholar] [CrossRef]
- Hudson, M.M. Reproductive Outcomes for Survivors of Childhood Cancer. Obstet. Gynecol. 2010, 116, 1171–1183. [Google Scholar] [CrossRef]
- Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in patients facing gonadotoxic therapies: An Ethics Committee opinion. Fertil. Steril. 2018, 110, 380–386. [Google Scholar] [CrossRef] [Green Version]
- Von Wolff, M.; Thaler, C.J.; Frambach, T.; Zeeb, C.; Lawrenz, B.; Popovici, R.M.; Strowitzki, T. Ovarian stimulation to cryopreserve fertilized oocytes in cancer patients can be started in the luteal phase. Fertil. Steril. 2009, 92, 1360–1365. [Google Scholar] [CrossRef]
- Sönmezer, M.; Türküolu, I.; Cokun, U.; Oktay, K. Random-start controlled ovarian hyperstimulation for emergency fertility preservation in letrozole cycles. Fertil. Steril. 2011, 95, 2125.e9–2125.e11. [Google Scholar] [CrossRef]
- Çakmak, H.; Zamah, A.M.; Katz, A.; Cedars, M.; Rosen, M. Effective method for emergency fertility preservation: Random-start controlled ovarian hyperstimulation. Fertil. Steril. 2012, 98, S170. [Google Scholar] [CrossRef]
- Metzger, M.L.; Meacham, L.R.; Patterson, B.; Casillas, J.S.; Constine, L.S.; Hijiya, N.; Kenney, L.B.; Leonard, M.; Lockart, B.A.; Likes, W.; et al. Female Reproductive Health After Childhood, Adolescent, and Young Adult Cancers: Guidelines for the Assessment and Management of Female Reproductive Complications. J. Clin. Oncol. 2013, 31, 1239–1247. [Google Scholar] [CrossRef] [PubMed]
- York, J.M. Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers; Children’s Oncology Group: Monrovia, CA, USA, 2018. [Google Scholar]
- Van Dorp, W.; Haupt, R.; Anderson, R.A.; Mulder, R.L.; van den Heuvel-Eibrink, M.M.; Broeder, E.V.D.-D.; Su, H.I.; Winther, J.F.; Hudson, M.M.; Levine, J.M.; et al. Reproductive Function and Outcomes in Female Survivors of Childhood, Adolescent, and Young Adult Cancer: A Review. J. Clin. Oncol. 2018, 36, 2169–2180. [Google Scholar] [CrossRef]
- Wallace, W.H.; Thompson, L.; Anderson, R.A. On behalf of the Guideline Development Group Long term follow-up of survivors of childhood cancer: Summary of updated SIGN guidance. BMJ 2013, 346, f1190. [Google Scholar] [CrossRef] [PubMed]
- Kelsey, T.W.; Wright, P.; Nelson, S.M.; Anderson, R.A.; Wallace, W.H. A Validated Model of Serum Anti-Müllerian Hormone from Conception to Menopause. PLoS ONE 2011, 6, e22024. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weenen, C.; Laven, J.S.; Von Bergh, A.R.; Cranfield, M.; Groome, N.P.; Visser, J.A.; Kramer, P.; Fauser, B.C.; Themmen, A.P. Anti-Mullerian hormone expression pattern in the human ovary: Potential implications for initial and cyclic follicle recruitment. Mol. Hum. Reprod. 2004, 10, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Durlinger, A.L.L. Anti-Mullerian Hormone Inhibits Initiation of Primordial Follicle Growth in the Mouse Ovary. Endocrinology 2002, 143, 1076–1084. [Google Scholar] [CrossRef]
- Iwase, A.; Nakamura, T.; Osuka, S.; Takikawa, S.; Goto, M.; Kikkawa, F. Anti-Müllerian hormone as a marker of ovarian reserve: What have we learned, and what should we know? Reprod. Med. Biol. 2015, 15, 127–136. [Google Scholar] [CrossRef]
- Van Rooij, I.; Broekmans, F.J.; Scheffer, G.J.; Looman, C.W.; Habbema, J.D.F.; De Jong, F.H.; Fauser, B.J.; Themmen, A.P.; Velde, E.R.T. Serum antimüllerian hormone levels best reflect the reproductive decline with age in normal women with proven fertility: A longitudinal study. Fertil. Steril. 2005, 83, 979–987. [Google Scholar] [CrossRef] [Green Version]
- Fanchin, R.; Schonäuer, L.M.; Righini, C.; Guibourdenche, J.; Frydman, R.; Taieb, J. Serum anti-Mullerian hormone is more strongly related to ovarian follicular status than serum inhibin B, estradiol, FSH and LH on day 3. Hum. Reprod. 2003, 18, 323–327. [Google Scholar] [CrossRef] [Green Version]
- De Vet, A.; Laven, J.S.; De Jong, F.H.; Themmen, A.P.; Fauser, B.C. Antimüllerian hormone serum levels: A putative marker for ovarian aging. Fertil. Steril. 2002, 77, 357–362. [Google Scholar] [CrossRef]
- Anderson, R.A.; Nelson, S.M.; Wallace, W.H. Measuring anti-Müllerian hormone for the assessment of ovarian reserve: When and for whom is it indicated? Maturita 2012, 71, 28–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rizzuto, I.; Behrens, R.F.; Smith, L.A. Risk of ovarian cancer in women treated with ovarian stimulating drugs for infertility. Cochrane Libr. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef] [PubMed]
| Degree of Risk of Permanent Amenorrhea | Chemotherapy Agent | Type of Cancer Treated |
|---|---|---|
| High (>80%) | Bone marrow transplant conditioning Cyclophosphamide > 7.5 g/m2 in females age < 20 | Leukemias, lymphomas non-Hodgkin’s lymphoma, neuroblastoma, acute lymphoblastic leukemia, sarcoma |
| Intermediate (20–80%) | CAF (cyclophosphamide, doxorubicin, fluorouracil) | Breast cancer |
| CEF (cyclophosphamide, epirubicin, fluorouracil) | Breast cancer | |
| CMF (cyclophosphamide, methotrexate, fluorouracil) | Breast cancer | |
| BEACOPP (doxorubicin, bleomycin, vincristine, etoposide, cyclophosphamide, procarbazine) | Hodgkin’s lymphoma | |
| Low (<20%) | ABVD (doxorubicin, bleomycin, vinblastine, prednisone) | Hodgkin’s lymphoma |
| AC (doxorubicin/cyclophosphamide) | Breast cancer | |
| CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone) | Non-Hodgkin’s lymphoma | |
| Anthracycline/cytarabine | Acute myeloid leukemia | |
| CVP (cyclophosphamide, vincristine, prednisone) | Non-Hodgkin’s lymphoma, Follicular lymphoma | |
| MAP (cisplatin, doxorubicin, methotrexate) | Osteosarcoma | |
| VDC/IE (doxorubicin, vincristine, cyclophosphamide, ifosfamide, etoposide) | Ewing’s sarcoma | |
| Very low or no risk | Methotrexate | Leukemia, head, neck, breast, lung cancer, rhabdomyosarcoma |
| Fluorouracil | ||
| Vincristine | ||
| Tamoxifen | ||
| Unknown risk (examples) | Monoclonal antibodies (trastuzumab, bevacizumab, cetuximab) Tyrosine kinase inhibitors (erlotinib, imatinib) Taxanes | Breast, ovarian, colon, lung cancer, glioblastoma, non-small lung cancer, pancreatic cancer, chronic myelogenous leukemia, acute lymphocytic leukemia, gastrointestinal stromal tumors, ovarian, breast, cervical, lung, pancreatic cancer |
| Treatment | Type of Cancer Treated |
|---|---|
| Total body irradiation | Conditioning for bone marrow transplant (leukemias, lymphomas) |
| Pelvic and abdominal radiation ≥6 Gy in adult women ≥10 Gy in postpubertal girls ≥15 Gy in prepubertal girls | Ovarian cancer, endometrial cancer, cervical cancer, Wilm’s tumor, osteosarcoma, Ewing sarcoma, neuroblastoma, rhabdomyosarcoma |
| Method | Can It Be Used in Prepubertal Girls? | Does It Cause Any Treatment Delay? | Does It Involve a Surgical Procedure? | Success Rate | |
|---|---|---|---|---|---|
| Established methods | Embryo cryopreservation | No | Yes | Yes | Live birth rate 27.7% per frozen embryo [43] |
| Oocyte cryopreservation | No | Yes | Yes | Live birth rate of 3–6% per frozen oocyte [43] | |
| Experimental methods | Ovarian tissue freezing and transplantation | Yes | No | Yes | Live birth rate 32% per transplant; endocrine recovery rate was 93% [45] |
| Oocyte in vitro maturation | Maybe | No | Yes | 21.5–55.6% per cycle [46] | |
| Debatable methods | GnRH analogs | No | No | No | Debatable |
| Oophoropexy | Yes | No | Yes | 66–79% of ovarian function preservation [47,48] | |
| Gonadal shielding | Yes | No | No | Debatable | |
| Cancer Treatment | Complication | Risk Factors |
|---|---|---|
| Chemotherapy | Hypogonadism (gonadotropin deficiency, delayed or arrested puberty, acute ovarian failure, premature menopause, infertility) | High doses of alkylating agents, heavy metals and nonclassical alkylators; Combination of chemotherapy and radiation |
| Radiotherapy | Hypogonadism (gonadotropin deficiency, delayed or arrested puberty, acute ovarian failure, premature menopause, infertility) | Prepubertal gonadal irradiation ≥ 10 Gy Pubertal gonadal irradiation ≥ 5 Gy |
| Precocious puberty | Young age at treatment, radiation dose ≥ 18 Gy to cranial regions | |
| Uterine vascular insufficiency | High pelvic radiation dose Radiation dose ≥ 30 Gy Patients with Wilms tumor and Mullerian anomalies | |
| Sexual dysfunction (vaginal fibrosis or stenosis) | Hypogonadism Graft-versus-host disease Prepubertal irradiation ≥ 25 Gy Postpubertal irradiation ≥ 50 Gy | |
| Surgery | Sexual dysfunction (vaginal fibrosis or stenosis) | Spinal cord tumors, vaginal tumors, surgery involving pelvical region |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michalczyk, K.; Cymbaluk-Płoska, A. Fertility Preservation and Long-Term Monitoring of Gonadotoxicity in Girls, Adolescents and Young Adults Undergoing Cancer Treatment. Cancers 2021, 13, 202. https://doi.org/10.3390/cancers13020202
Michalczyk K, Cymbaluk-Płoska A. Fertility Preservation and Long-Term Monitoring of Gonadotoxicity in Girls, Adolescents and Young Adults Undergoing Cancer Treatment. Cancers. 2021; 13(2):202. https://doi.org/10.3390/cancers13020202
Chicago/Turabian StyleMichalczyk, Kaja, and Aneta Cymbaluk-Płoska. 2021. "Fertility Preservation and Long-Term Monitoring of Gonadotoxicity in Girls, Adolescents and Young Adults Undergoing Cancer Treatment" Cancers 13, no. 2: 202. https://doi.org/10.3390/cancers13020202





