Laser Immunotherapy: A Potential Treatment Modality for Keratinocyte Carcinoma
Abstract
:Simple Summary
Abstract
1. Introduction
2. Rationales for Immunotherapy in Keratinocyte Carcinoma
3. Keratinocyte Carcinoma Immunotherapy: Current Status
4. Immunological Responses to Laser: Preclinical Evidence
5. Immunological Responses to Laser: Clinical Evidence
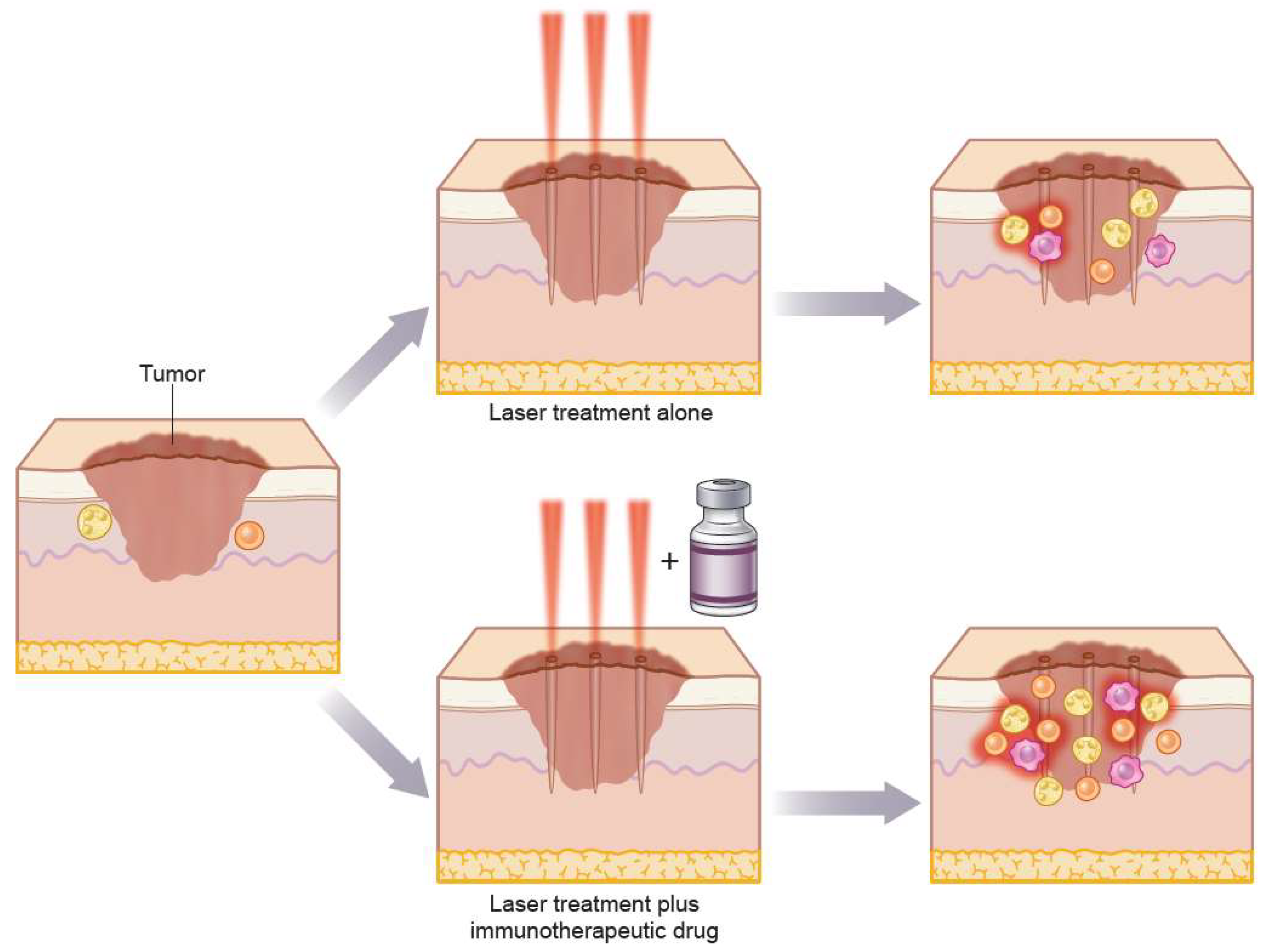
6. Laser Immunotherapy
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| KC | keratinocyte carcinoma |
| BCC | basal cell carcinoma |
| SCC | squamous cell carcinoma |
| AFL | ablative fractionated laser |
| LIT | Laser immunotherapy |
| MM | malignant melanoma |
| PD1 | programmed death 1 |
| PD-L1 | programmed death ligand 1 |
| IHC | immunohistochemistry |
| TILs | tumor infiltrating lymphocytes |
| T-regs | regulatory T-cells |
| TMB | tumor mutational burden |
| TLR | Toll like receptor |
| IL6 | interleukin 6 |
| MCP1 | monocyte chemoattractant protein 1 |
| TGF-β | transforming growth factor-β |
| HSP | heat shock proteins |
| NIR | near-infrared lasers |
| CTLA4 | cytotoxic T-lymphocyte antigen-4 |
References
- Goldmann, L. Biomedical Aspects of the Laser: The Introduction of Laser Applications into Biology and Medicine; Springer: Berlin/Heidelberg, Germany, 1967. [Google Scholar]
- Shah, S.M.; Konnikov, N.; Duncan, L.M.; Tannous, Z.S. The effect of 595 nm pulsed dye laser on superficial and nodular basal cell carcinomas. Lasers Surg. Med. 2009, 41, 417–422. [Google Scholar] [CrossRef]
- Ortiz, A.E.; Anderson, R.R.; Avram, M.M. 1064 nm long-pulsed Nd:YAG laser treatment of basal cell carcinoma. Lasers Surg. Med. 2015, 47, 106–110. [Google Scholar] [CrossRef]
- Haedersdal, M.; Erlendsson, A.M.; Paasch, U.; Anderson, R.R. Translational medicine in the field of ablative fractional laser (AFXL)-assisted drug delivery: A critical review from basics to current clinical status. J. Am. Acad. Dermatol. 2016, 74, 981–1004. [Google Scholar] [CrossRef]
- Wenande, E.; Anderson, R.R.; Haedersdal, M. Fundamentals of fractional laser-assisted drug delivery: An in-depth guide to experimental methodology and data interpretation. Adv. Drug Deliv. Rev. 2020, 153, 169–184. [Google Scholar] [CrossRef]
- Cives, M.; Mannavola, F.; Lospalluti, L.; Sergi, M.C.; Cazzato, G.; Filoni, E.; Cavallo, F.; Giudice, G.; Stucci, L.S.; Porta, C.; et al. Non-Melanoma Skin Cancers: Biological and Clinical Features. Int. J. Mol. Sci. 2020, 21, 5394. [Google Scholar] [CrossRef]
- Donia, M.; Ellebaek, E.; Øllegaard, T.H.; Duval, L.; Aaby, J.B.; Hoejberg, L.; Køhler, U.H.; Schmidt, H.; Bastholt, L.; Svane, I.M. The real-world impact of modern treatments on the survival of patients with metastatic melanoma. Eur. J. Cancer 2019, 108, 25–32. [Google Scholar] [CrossRef]
- Chang, J.; Zhu, G.; Cheung, C.; Li, S.; Kim, J.; Chang, A.L.S. Association Between Programmed Death Ligand 1 Expression in Patients With Basal Cell Carcinomas and the Number of Treatment Modalities. JAMA Dermatol. 2017, 153, 285–290. [Google Scholar] [CrossRef]
- Lipson, E.J.; Lilo, M.T.; Ogurtsova, A.; Esandrio, J.; Xu, H.; Brothers, P.; Schollenberger, M.; Sharfman, W.H.; Taube, J.M. Basal cell carcinoma: PD-L1/PD-1 checkpoint expression and tumor regression after PD-1 blockade. J. Immunother. Cancer 2017, 5, 23. [Google Scholar] [CrossRef] [Green Version]
- Migden, M.R.; Khushalani, N.I.; Chang, A.L.S.; Lewis, K.D.; Schmults, C.D.; Hernandez-Aya, L.; Meier, F.; Schadendorf, D.; Guminski, A.; Hauschild, A.; et al. Cemiplimab in locally advanced cutaneous squamous cell carcinoma: Results from an open-label, phase 2, single-arm trial. Lancet Oncol. 2020, 21, 294–305. [Google Scholar] [CrossRef]
- Gambichler, T.; Schröter, U.; Höxtermann, S.; Susok, L.; Stockfleth, E.; Becker, J.C. Decline of programmed death-1-positive circulating T regulatory cells predicts more favourable clinical outcome of patients with melanoma under immune checkpoint blockade. Br. J. Dermatol. 2019, 182, 1214–1220. [Google Scholar] [CrossRef]
- Kaporis, H.G.; Guttman-Yassky, E.; Lowes, M.A.; Haider, A.S.; Fuentes-Duculan, J.; Darabi, K.; Whynot-Ertelt, J.; Khatcherian, A.; Cardinale, I.; Novitskaya, I.; et al. Human Basal Cell Carcinoma Is Associated with Foxp3+ T cells in a Th2 Dominant Microenvironment. J. Investig. Dermatol. 2007, 127, 2391–2398. [Google Scholar] [CrossRef] [Green Version]
- Zhang, B.; Chikuma, S.; Hori, S.; Fagarasan, S.; Honjo, T. Nonoverlapping roles of PD-1 and FoxP3 in maintaining immune tolerance in a novel autoimmune pancreatitis mouse model. Proc. Natl. Acad. Sci. USA 2016, 113, 8490–8495. [Google Scholar] [CrossRef] [Green Version]
- Kamada, T.; Togashi, Y.; Tay, C.; Ha, D.; Sasaki, A.; Nakamura, Y.; Sato, E.; Fukuoka, S.; Tada, Y.; Tanaka, A.; et al. PD-1+ regulatory T cells amplified by PD-1 blockade promote hyperprogression of cancer. Proc. Natl. Acad. Sci. USA 2019, 116, 9999–10008. [Google Scholar] [CrossRef] [Green Version]
- Wojas-Krawczyk, K.; Kalinka, E.; Grenda, A.; Krawczyk, P.; Milanowski, J. Beyond PD-L1 Markers for Lung Cancer Immunotherapy. Int. J. Mol. Sci. 2019, 20, 1915. [Google Scholar] [CrossRef] [Green Version]
- Chalmers, Z.R.; Connelly, C.F.; Fabrizio, D.; Gay, L.; Ali, S.M.; Ennis, R.; Schrock, A.; Campbell, B.; Shlien, A.; Chmielecki, J.; et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 2017, 9, 1–14. [Google Scholar] [CrossRef]
- Goodman, A.M.; Kato, S.; Cohen, P.R.; Boichard, A.; Frampton, G.; Miller, V.; Stephens, P.J.; Daniels, G.A.; Kurzrock, R. Genomic landscape of advanced basal cell carcinoma: Implications for precision treatment with targeted and immune therapies. OncoImmunology 2018, 7, e1404217. [Google Scholar] [CrossRef] [Green Version]
- Hartevelt, M.M.; Bavinck, J.N.B.; Kootte, A.M.M.; Vermeer, B.J.; Vandenbroucke, J.P. Incidence of skin cancer after renal transplantation in The Netherlands. Transplantation 1990, 49, 506–509. [Google Scholar] [CrossRef]
- Omland, S.H.; Gniadecki, R.; Hædersdal, M.; Helweg-Larsen, J.; Omland, L.H. Skin cancer risk in hematopoietic stem-cell transplant recipients compared with background population and renal transplant recipients a population-based cohort study. JAMA Dermatol. 2016, 152, 177–183. [Google Scholar] [CrossRef]
- Vaddepally, R.K.; Kharel, P.; Pandey, R.; Garje, R.; Chandra, A.B. Review of Indications of FDA-Approved Immune Checkpoint Inhibitors per NCCN Guidelines with the Level of Evidence. Cancers 2020, 12, 738. [Google Scholar] [CrossRef] [Green Version]
- Migden, M.R.; Rischin, D.; Schmults, C.D.; Guminski, A.; Hauschild, A.; Lewis, K.D.; Chung, C.H.; Hernandez-Aya, L.; Lim, A.M.; Chang, A.L.S.; et al. PD-1 Blockade with Cemiplimab in Advanced Cutaneous Squamous-Cell Carcinoma. N. Engl. J. Med. 2018, 379, 341–351. [Google Scholar] [CrossRef] [Green Version]
- Zhao, C.Y.; Hwang, S.J.E.; Anforth, R.; Carlos, G.; Chou, S.; Carlino, M.; Fernández-Peñas, P. Incidence of Basal Cell Carcinoma and Squamous Cell Carcinoma in Patients on Antiprogrammed Cell Death-1 Therapy for Metastatic Melanoma. J. Immunother. 2018, 41, 343–349. [Google Scholar] [CrossRef]
- Falchook, G.S.; Leidner, R.; Stankevich, E.; Piening, B.; Bifulco, C.; Lowy, I.; Fury, M.G. Responses of metastatic basal cell and cutaneous squamous cell carcinomas to anti-PD1 monoclonal antibody REGNJ. Immunother. Cancer 2016, 4, 70. [Google Scholar] [CrossRef] [Green Version]
- Ikeda, S.; Goodman, A.M.; Cohen, P.R.; Jensen, T.J.; Ellison, C.K.; Frampton, G.; Miller, V.; Patel, S.P.; Kurzrock, R. Metastatic basal cell carcinoma with amplification of PD-L1: Exceptional response to anti-PD1 therapy. NPJ Genom. Med. 2016, 1, 16037. [Google Scholar] [CrossRef] [Green Version]
- Cohen, P.R.; Kato, S.; Goodman, A.M.; Ikeda, S.; Kurzrock, R. Appearance of New Cutaneous Superficial Basal Cell Carcinomas during Successful Nivolumab Treatment of Refractory Metastatic Disease: Implications for Immunotherapy in Early Versus Late Disease. Int. J. Mol. Sci. 2017, 18, 1663. [Google Scholar] [CrossRef]
- Cannon, J.G.; Russell, J.S.; Kim, J.; Chang, A.L.S. A case of metastatic basal cell carcinoma treated with continuous PD-1 inhibitor exposure even after subsequent initiation of radiotherapy and surgery. JAAD Case Rep. 2018, 4, 248–250. [Google Scholar] [CrossRef] [Green Version]
- Winkler, J.; Schneiderbauer, R.; Bender, C.; Sedlaczek, O.; Fröhling, S.; Penzel, R.; Enk, A.; Hassel, J.C. Anti-programmed cell death-1 therapy in nonmelanoma skin. Br. J. Dermatol. 2017, 176, 498–502. [Google Scholar]
- Jørgensen, N.; Kaae, J.; Grauslund, J.; Met, Ö.; Nielsen, S.; Pedersen, A.; Svane, I.; Ehrnrooth, E.; Andersen, M.; Zachariae, C.; et al. Vaccination against PD-L1 with IO103 a Novel Immune Modulatory Vaccine in Basal Cell Carcinoma: A Phase IIa Study. Cancers 2021, 13, 911. [Google Scholar] [CrossRef]
- Peris, K.; Fargnoli, M.C.; Garbe, C.; Kaufmann, R.; Bastholt, L.; Seguin, N.B.; Bataille, V.; Marmol, V.D.; Dummer, R.; Harwood, C.A.; et al. Diagnosis and treatment of basal cell carcinoma: European consensus–based interdisciplinary guidelines. Eur. J. Cancer 2019, 118, 10–34. [Google Scholar] [CrossRef] [Green Version]
- Dummer, R.; Urosevic, M.; Kempf, W.; Hoek, K.; Hafner, J.; Burg, G. Imiquimod in basal cell carcinoma: How does it work? Br. J. Dermatol. 2003, 149, 57–58. [Google Scholar] [CrossRef]
- Vidal, D.; Matías-Guiu, X.; AlOmar, A. Open study of the efficacy and mechanism of action of topical imiquimod in basal cell carcinoma. Clin. Exp. Dermatol. 2004, 29, 518–525. [Google Scholar] [CrossRef]
- MacFarlane, D.; El Tal, A. Cryoimmunotherapy: Superficial basal cell cancer and squamous cell carcinoma in situ treated with liquid nitrogen followed by imiquimod. Arch Dermatol. 2011, 147, 1326–1327. [Google Scholar]
- Gaitanis, G.; Nomikos, K.; Vava, E.; Alexopoulos, E.; Bassukas, I.; Alexopoulos, E. Immunocryosurgery for basal cell carcinoma: Results of a pilot, prospective, open-label study of cryosurgery during continued imiquimod application. J. Eur. Acad. Dermatol. Venereol. 2009, 23, 1427–1431. [Google Scholar] [CrossRef]
- Kawakubo, M.; Demehri, S.; Manstein, D. Fractional laser exposure induces neutrophil infiltration (N1 phenotype) into the tumor and stimulates systemic anti-tumor immune response. PLoS ONE 2017, 12, e0184852. [Google Scholar] [CrossRef] [Green Version]
- Wenande, E.; Tam, J.; Bhayana, B.; Schlosser, S.K.; Ishak, E.; Farinelli, W.A.; Chłopik-Olkiewicz, A.; Hoang, M.P.; Pinkhasov, O.R.; Caravan, P.; et al. Laser-assisted delivery of synergistic combination chemotherapy in in vivo skin. J. Control. Release 2018, 275, 242–253. [Google Scholar] [CrossRef]
- Fontenete, S.; Lerche, C.M.; Paasch, U.; Perez-Moreno, M.; Olesen, U.H.; Haedersdal, M. Tumor Clearance and Immune Cell Recruitment in UV-Induced Murine Squamous Cell Carcinoma Exposed to Ablative Fractional Laser and Imiquimod Treatment. Lasers Surg. Med. 2021, 53, 1227–1237. [Google Scholar] [CrossRef]
- DeBruler, D.M.; Blackstone, B.N.; Baumann, M.E.; McFarland, K.L.; Wulff, B.C.; Wilgus, T.A.; Bailey, J.; Supp, D.; Powell, H.M. Inflammatory responses, matrix remodeling, and re-epithelialization after fractional CO2 laser treatment of scars. Lasers Surg. Med. 2017, 49, 675–685. [Google Scholar] [CrossRef]
- Kawakubo, M.; Cunningham, T.J.; Demehri, S.; Manstein, D. Fractional Laser Releases Tumor-Associated Antigens in Poorly Immunogenic Tumor and Induces Systemic Immunity. Sci. Rep. 2017, 7, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Isbert, C.; Ritz, J.-P.; Roggan, A.; Schuppan, D.; Rühl, M.; Buhr, H.J.; Germer, C.-T. Enhancement of the immune response to residual intrahepatic tumor tissue by laser-induced thermotherapy (LITT) compared to hepatic resection. Lasers Surg. Med. 2004, 35, 284–292. [Google Scholar] [CrossRef]
- Helbig, D.; Bodendorf, M.O.; Grunewald, S.; Kendler, M.; Simon, J.C.; Paasch, U. Immunohistochemical investigation of wound healing in response to fractional photothermolysis. J. Biomed. Opt. 2009, 14, 064044. [Google Scholar] [CrossRef] [Green Version]
- Prignano, F.; Campolmi, P.; Bonan, P.; Ricceri, F.; Cannarozzo, G.; Troiano, M.; Lotti, T. Fractional CO2laser: A novel therapeutic device upon photobiomodulation of tissue remodeling and cytokine pathway of tissue repair. Dermatol. Ther. 2009, 22, S8–S15. [Google Scholar] [CrossRef]
- Grunewald, S.; Bodendorf, M.; Illes, M.; Kendler, M.; Simon, J.C.; Paasch, U. In vivowound healing and dermal matrix remodelling in response to fractional CO2laser intervention: Clinicopathological correlation in non-facial skin. Int. J. Hyperth. 2011, 27, 811–818. [Google Scholar] [CrossRef]
- Odo, L.M.; Odo, M.E.Y.; Guedes, F.; Sotto, M.; Cucé, L.C. Immunohistochemical Evaluation of Skin Before and After Micro-Ablative Fractional Erbium-Doped Yttrium Aluminum Garnet Laser Treatment. Dermatol. Surg. 2011, 37, 246–248. [Google Scholar] [CrossRef]
- Schmitt, L.; Amann, P.M.; Marquardt, Y.; Heise, R.; Czaja, K.; Gerber, P.A.; Steiner, T.; Hölzle, F.; Baron, J.M. Molecular effects of fractional ablative erbium:YAG laser treatment with multiple stacked pulses on standardized human three-dimensional organotypic skin models. Lasers Med. Sci. 2017, 32, 805–814. [Google Scholar] [CrossRef]
- Fisher, D.T.; Appenheimer, M.M.; Evans, S.S. The two faces of IL-6 in the tumor microenvironment. Semin. Immunol. 2014, 26, 38–47. [Google Scholar] [CrossRef] [Green Version]
- Yoshimura, T. The chemokine MCP-1 (CCL2) in the host interaction with cancer: A foe or ally? Cell. Mol. Immunol. 2018, 15, 335–345. [Google Scholar] [CrossRef] [Green Version]
- Brábek, J.; Jakubek, M.; Vellieux, F.; Novotný, J.; Kolář, M.; Lacina, L.; Szabo, P.; Strnadová, K.; Rösel, D.; Dvořánková, B.; et al. Interleukin-6: Molecule in the Intersection of Cancer, Ageing and COVID-19. Int. J. Mol. Sci. 2020, 21, 7937. [Google Scholar] [CrossRef]
- Sorg, H.; Tilkorn, D.J.; Hager, S.; Hauser, J.; Mirastschijski, U. Skin Wound Healing: An Update on the Current Knowledge and Concepts. Eur. Surg. Res. 2017, 58, 81–94. [Google Scholar] [CrossRef]
- Yang, L.; Pang, Y.; Moses, H.L. TGF-β and immune cells: An important regulatory axis in the tumor microenvironment and progression. Trends Immunol. 2010, 31, 220–227. [Google Scholar] [CrossRef] [Green Version]
- Colaco, C.A.; Bailey, C.R.; Walker, K.B.; Keeble, J. Heat Shock Proteins: Stimulators of Innate and Acquired Immunity. BioMed Res. Int. 2013, 2013, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Vidyarthi, A.; Khan, N.; Agnihotri, T.; Negi, S.; Das, D.K.; Aqdas, M.; Chatterjee, D.; Colegio, O.; Tewari, M.K.; Agrewala, J.N. TLR-3 Stimulation Skews M2 Macrophages to M1 Through IFN-αβ Signaling and Restricts Tumor Progression. Front. Immunol. 2018, 9, 1–14. [Google Scholar] [CrossRef]
- Qiu, L.-L.; Zhang, X.-G.; Chen, G.; Dang, Y.-W.; Huang, Z.-G.; Li, M.-X.; Liang, Y.; Huang, S.-N.; Tang, X.-Z.; Chen, X.-X.; et al. Clinical Significance of the Interleukin 24 mRNA Level in Head and Neck Squamous Cell Carcinoma and Its Subgroups: An In Silico Investigation. J. Oncol. 2020, 2020, 1–15. [Google Scholar] [CrossRef]
- Lippitz, B.E. Cytokine patterns in patients with cancer: A systematic review. Lancet Oncol. 2013, 14, e218–e228. [Google Scholar] [CrossRef]
- Kashiwagi, S. Laser adjuvant for vaccination. FASEB J. 2020, 34, 3485–3500. [Google Scholar] [CrossRef] [Green Version]
- Wang, T.; Wang, D.; Yu, H.; Feng, B.; Zhou, F.; Zhang, H.; Zhou, L.; Jiao, S.; Li, Y. A cancer vaccine-mediated postoperative immunotherapy for recurrent and metastatic tumors. Nat. Commun. 2018, 9, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Lopes, P.; Todorov, G.; Pham, T.; Nesburn, A.; Bahraoui, E.; BenMohamed, L. Laser Adjuvant-Assisted Peptide Vaccine Promotes Skin Mobilization of Dendritic Cells and Enhances Protective CD8 + T EM and T RM Cell Responses against Herpesvirus In-fection and Disease. Jour. Virol. 2018, 92, 1–18. [Google Scholar]
- Chen, X.; Kim, P.; Farinelli, B.; Doukas, A.; Yun, S.-H.; Gelfand, J.A.; Anderson, R.R.; Wu, M.X. A Novel Laser Vaccine Adjuvant Increases the Motility of Antigen Presenting Cells. PLoS ONE 2010, 5, e13776. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.R.; Adams, R.L.; Carubelli, R.; Nordquist, R.E. Laser-photosensitizer assisted immunotherapy: A novel modality for cancer treatment. Cancer Lett. 1997, 115, 25–30. [Google Scholar] [CrossRef]
- Chen, W.R.; Singhal, A.K.; Liu, H.; Nordquist, R.E. Antitumor immunity induced by laser immunotherapy and its adoptive trans-fer. Cancer Res. 2001, 61, 459–461. [Google Scholar]
- Chen, W.R.; Liu, H.; Ritchey, J.W.; Bartels, K.E.; Lucroy, M.D.; Nordquist, R.E. Effect of different components of laser immunotherapy in treatment of metastatic tumors in rats. Cancer Res. 2002, 62, 4295–4299. [Google Scholar]
- Chen, W.; Liu, H.; Nordquist, J.; Nordquist, R. Tumour cell damage and leucocyte infiltration after laser immunotherapy treat-ment. Lasers Med. Sci. 2000, 15, 43–48. [Google Scholar]
- Luo, M.; Shi, L.; Zhang, F.; Zhou, F.; Zhang, L.; Wang, B.; Wang, P.; Zhang, Y.; Zhang, H.; Yang, D.; et al. Laser Immunotherapy for Cu-taneous Squamous Cell Carcinoma with Optimal Thermal Effects to Enhance Tumor Immunogenicity. Inj. J. Hyperth. 2018, 34, 1337–1350. [Google Scholar] [CrossRef]
- Lo, J.A.; Kawakubo, M.; Juneja, V.R.; Su, M.Y.; Erlich, T.H.; LaFleur, M.W.; Kemeny, L.V.; Rashid, M.; Malehmir, M.; Rabi, S.A.; et al. Epitope spreading toward wild-type melanocyte-lineage antigens rescues suboptimal immune checkpoint blockade responses. Sci. Transl. Med. 2021, 13, 1–13. [Google Scholar] [CrossRef]
- Luo, L.; Yang, J.; Zhu, C.; Jiang, M.; Guo, X.; Li, W.; Yin, X.; Yin, H.; Qin, B.; Yuan, X.; et al. Sustained release of anti-PD-1 peptide for perdurable immunotherapy together with photothermal ablation against primary and distant tumors. J. Control. Release 2018, 278, 87–99. [Google Scholar] [CrossRef]
- Chen, Q.; Xu, L.; Liang, C.; Wang, C.; Peng, R.; Liu, Z. Photothermal therapy with immune-adjuvant nanoparticles together with checkpoint blockade for effective cancer immunotherapy. Nat. Commun. 2016, 7, 13193. [Google Scholar] [CrossRef]
- Cao, Q.; Wang, W.; Zhou, M.; Huang, Q.; Wen, X.; Zhao, J.; Shi, S.; Geng, K.; Li, F.; Hatakeyama, H.; et al. Induction of antitumor immunity in mice by the combination of nanoparticle-based photothermolysis and anti-PD-1 checkpoint inhibition. Nanomed. Nanotechnol. Biol. Med. 2020, 25, 102169. [Google Scholar] [CrossRef]
- Li, X.; Naylor, M.F.; Le, H.; Nordquist, R.E.; Teague, K.; Howard, C.A.; Murray, C.; Chen, W.R. Clinical effects of in situ photoimmunotherapy on late-stage melanoma patients: A preliminary study. Cancer Biol. Ther. 2010, 10, 1081–1087. [Google Scholar] [CrossRef] [Green Version]
- St Pierre, S.; Rommel, J.; Ciurea, A.; Fife, D.; Yoo, S.S.; Martinin, M.; Kuzel, T.M.; Wayne, J.; Rademaker, A.; West, D.P.; et al. In situ pho-toimmunotherapy: A surgery- and limb-sparing approach to the treatment of cutaneous metastases in advanced melanoma. Arch Dermatol. 2010, 146, 831–834. [Google Scholar]
- Song, S.; Zhou, F.; Nordquist, R.E.; Carubelli, R.; Liu, H.; Chen, W.R. Glycated chitosan as a new non-toxic immunological stimulant. Immunopharmacol. Immunotoxicol. 2009, 31, 202–208. [Google Scholar] [CrossRef]
- Highton, A.J.; Girardin, A.; Bell, G.M.; Hook, S.M.; Kemp, R.A. Chitosan gel vaccine protects against tumour growth in an intracaecal mouse model of cancer by modulating systemic immune responses. BMC Immunol. 2016, 17, 39. [Google Scholar] [CrossRef] [Green Version]
- Czarnecka, A.; Rutkowski, P. An update on the safety of nivolumab for the treatment of advanced melanoma. Expert Opin. Drug Saf. 2020, 19, 409–421. [Google Scholar] [CrossRef] [Green Version]
- Hendel, K.K.; Bagger, C.; Olesen, U.H.; Janfelt, C.; Hansen, S.H.; Haedersdal, M.; Lerche, C.M. Fractional laser-assisted topical delivery of bleomycin quantified by LC-MS and visualized by MALDI mass spectrometry imaging. Drug Deliv. 2019, 26, 244–251. [Google Scholar] [CrossRef] [Green Version]
- Erlendsson, A.M.; Olesen, U.H.; Haedersdal, M.; Rossi, A.M. Ablative fractional laser-assisted treatments for keratinocyte carcinomas and its precursors–Clinical review and future perspectives. Adv. Drug Deliv. Rev. 2020, 153, 185–194. [Google Scholar] [CrossRef]
- Christensen, R.L.; Omland, S.H.; Persson, D.P.; Husted, S.; Hædersdal, M.; Olesen, U.H. Topical Delivery of Nivolumab, a Therapeutic Antibody, by Fractional Laser and Pneumatic Injection. Lasers Surg. Med. 2021, 53, 154–161. [Google Scholar] [CrossRef]


| Reference | Study Type | Laser Intervention | Major Findings |
|---|---|---|---|
| Kawakubo M et al. [34] 2017 | Preclinical in vivo mouse tumor study | Fractional CO2 laser 100 mJ/mb 5% density | 24 h Neutrophil infiltration 5 d: Abrogated increase of T-regs Tumor-specific CD8+ T-cell response (IHC & flow cytometry) |
| Wenande E et al. [35] 2018 | Preclinical in vivo drug delivery pig study Extracted data on laser monotherapy from a larger study | Fractional CO2 laser 50 mJ/mb 5% density | 48 h: neutrophil infiltration and perivascularlymphocytes 120 h: macrophage infiltration (H&E) |
| Fontenete S et al. [36] 2021 | Preclinical in vivo mouse SCC-study Extracted data on laser monotherapy from a larger study | Fractional CO2 laser 100 mJ/mb 5% density | Tumor reduction Increased T-cell infiltration (IHC & flow cytometry) |
| DeBruler DM et al. [37] 2017 | Preclinical in vivo porcine scar model | Fractional CO2 laser 70 mJ 5% density | 1 h: increase of IL6 and MCP-1 Up to 168 h: increase of TGF-β (qRT-PCR) |
| Kawakubo M et al. [38] 2017 | Preclinical in vivo mouse tumor study Extracted data on laser monotherapy from a larger study | Fractional CO2 laser 100 mJ/mb 5% density | Direct and indirect tumor response 5 d: increased T-cell infiltration and CD8/T-reg ratio (Flow cytometry) |
| Isbert C et al. [39] 2004 | Preclinical in vivo rat tumor study comparing laser and surgery | Nd:Yag 1064 nm 2 W | Indirect tumor response of untreated tumor in laser but not surgery group. T-cell infiltration at untreated tumor border in laser group (IHC) |
| Helbig D et al. [40] 2009 | Clinical tissue remodeling study on healthy individuals with photodamaged skin | Fractional CO2-laser 50, 64, 300 mJ 150 ablation zones per cm2 | Day 3–14: increase of mast cells 1 h–3 days: increased TGFβ expression Day 3–14: increased HSPs, CD3, CD20, CD68 expression (IHC) |
| Prignano F et al. [41] 2009 | Clinical tissue remodeling study on individuals with photodamaged skin | Fractional CO2-laser 2.07, 2.77, 4.15 J/cm2 | Increased cytokine and growth factor infiltration with peak at day 3 with medium energy |
| Grunewald S et al. [42] 2011 | Clinical study on individuals with photodamaged skin | Fractional CO2-laser 50 mJ, 100 mJ, 300 mJ | Increased lymphocyte infiltration from day 1 to 21 (H&E) |
| Odo LM et al. [43] 2011 | Clinical study on individuals with normal skin | Fractional Er:YAG 1400 mJ/cm2 | Progressive reduction of Langerhans cells, TLR 2&9 up to day 14 Increase of TLR3 |
| Schmitt L et al. [44] 2017 | Human 3D organotypic skin model Morphological and molecular changes upon laser | Fractional Er:YAG 4–10 J/cm2 | 48–72 h: upregulated expression of chemokines IL6,8,24 Downregulated expression of IL18,36β (qRT-PCR) |
| Reference | Study Type | Laser Intervention and Immunostimulant | Major Findings |
| Chen W et al. [58] 1997 | Preclinical in vivo rat tumor study | Laser: 805 nm diode 2–5 W Photosensitizer: Indocyanine green (ICG) Immunostimulant: Glycated chitosan gel (GC) (intratumoral injection) | Increase in survival rate, tumor eradication (primary and metastatic) Resistance to tumor rechallenge in successfully treated rats |
| Chen W et al. [59] 2001 | Preclinical in vivo rat tumor study | Laser: 805 nm diode 2 W Photosensitizer: ICG Immunostimulant: GC (intratumoral injection) | LIT-cured rats showed total resistance to tumor reinoculation Spleen cells from LIT-cured rats provided 100% protection to the naïve recipient rats |
| Chen W et al. [60] 2002 | Preclinical in vivo rat tumor study | Laser: 805 nm diode 2 W Photosensitizer: ICG Immunostimulant: GC (intratumoral injection) | Increased survival Reduced tumor-growth 3-component treatment was superior |
| Chen W et al. [61] 2000 | Preclinical in vivo rat tumor study | Laser: 805 nm diode 2 W 1200 J Photosensitizer: ICG Immunostimulant: GC (intratumoral injection) | Lymphocyte and plasma cell infiltration (Electron microscopy, optical microscopy) |
| Luo M et al. [62] 2018 | Preclinical in vivo mouse SCC study Clinical case on one patient with refractory SCC | Laser: 808-nm diode 1 W/cm2 Immunostimulant: Imiquimod (topical) | LIT-treated tumors showed no growth Increased survival Increased infiltration of lymphocytes in patient SCC and tumor reduction (H&E) |
| Kawakubo M et al. [38] 2017 | Preclinical in vivo mouse tumor study | Laser: Fractional CO2 laser 100 mJ/mb 5% density Immunostimulant: Anti-PD1 (intraperitoneal injection) | Direct and indirect tumor response Systemic immunity observed Increased T-cell infiltration (Flow cytometry) |
| Fontenete S et al. [36] 2021 | Preclinical in vivo mouse SCC-study | Laser: Fractional CO2 100 mJ/mb 5% density Immunostimulant: Imiquimod (topical) | Direct tumor response AFL+imiquimod superior to monotherapy on tumor shrinkage and innate and adaptive immune cell recruitment (Flow cytometry & IHC) |
| Lo JA et al. [63] 2021 | Preclinical in vivo mouse tumor study | Laser: Fractional CO2 100 mJ/mb 5% density Immunostimulants: Anti-PD1 (systemic) Anti-CTLA4 (systemic) Imiquimod (topical) | Direct and indirect tumor response Superior efficacy with combination of imiquimod + AFL + anti–PD1 Increased CD8:Treg ratio (Flow cytometry) |
| Luo L et al. [64] 2018 | Nanoparticle LIT preclinical in vivo mouse tumor study | Laser: near-infrared (NIR) 2 W/cm2 Immunostimulant: Anti-PD1 in nanoparticles (anti-PD1-NP) (intratumoral injection) | (anti-PD1-NP) + laser: stronger inhibition of tumor growth compared with (anti-PD1-NP) without laser Infiltration of T-cells (Flow cytometry) |
| Chen Q et al. [65] 2016 | Nanoparticle LIT preclinical in vivo mouse tumor study Multiple groups with different interventions | Laser: NIR Immunostimulant: ICG + TLR (subcutaneous & IV) Anti-CTLA4 (IV injection) 0,5 W/cm2 | Combinatory treatment led to increased DC and interleukin infiltration/release Almost completely inhibited growth of secondary tumor with combined laser-nano (ICG + TLR) and injected CTLA4 (Flow cytometry & ELISA) |
| Cao Q et al. [66] 2020 | Nanoparticle preclinical in vivo mouse tumor study Multiple groups with different interventions | Laser: 1064 Q-switched Nd:Yag Copper monosulfide nanoparticles (Cus NP) 2,2 W/cm2 Immunostimulant: Anti-PD1 (IV and intraperitoneal injection) TLR (intratumoral injection) | Direct and indirect tumor response Increase in survival rate Infiltration of T-cells and dendritic cells (Flow cytometry) |
| Li X et al. [67] 2010 | Clinical case study on 11 patients with late-stage MM | Laser: NIR 805 nm 1 W/cm2 Immunostimulant: Imiquimod (topical) | CR in 6/11 patients Complete local response in 8/11 patients AE: Rash, pruritus (H&E) |
| St Pierre et al. [68] 2010 | Clinical case study on 64-year-old man with recurrence of MM on the toe | Laser: 810-nm diode 1 j/cm2 Immunostimulant: Imiquimod (topical) | Initial CR on treated tumors and PR of non-treated tumor but recurrence Repeated treatment episodes with continued response. No visceral metastases |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Omland, S.H.; Wenande, E.C.; Svane, I.M.; Tam, J.; Olesen, U.H.; Hædersdal, M. Laser Immunotherapy: A Potential Treatment Modality for Keratinocyte Carcinoma. Cancers 2021, 13, 5405. https://doi.org/10.3390/cancers13215405
Omland SH, Wenande EC, Svane IM, Tam J, Olesen UH, Hædersdal M. Laser Immunotherapy: A Potential Treatment Modality for Keratinocyte Carcinoma. Cancers. 2021; 13(21):5405. https://doi.org/10.3390/cancers13215405
Chicago/Turabian StyleOmland, Silje Haukali, Emily Cathrine Wenande, Inge Marie Svane, Joshua Tam, Uffe Høgh Olesen, and Merete Hædersdal. 2021. "Laser Immunotherapy: A Potential Treatment Modality for Keratinocyte Carcinoma" Cancers 13, no. 21: 5405. https://doi.org/10.3390/cancers13215405
APA StyleOmland, S. H., Wenande, E. C., Svane, I. M., Tam, J., Olesen, U. H., & Hædersdal, M. (2021). Laser Immunotherapy: A Potential Treatment Modality for Keratinocyte Carcinoma. Cancers, 13(21), 5405. https://doi.org/10.3390/cancers13215405







