Demographic and Epidemiological Contributions to Recent Trends in Cancer Incidence in Hong Kong
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Statistical Analyses
3. Results
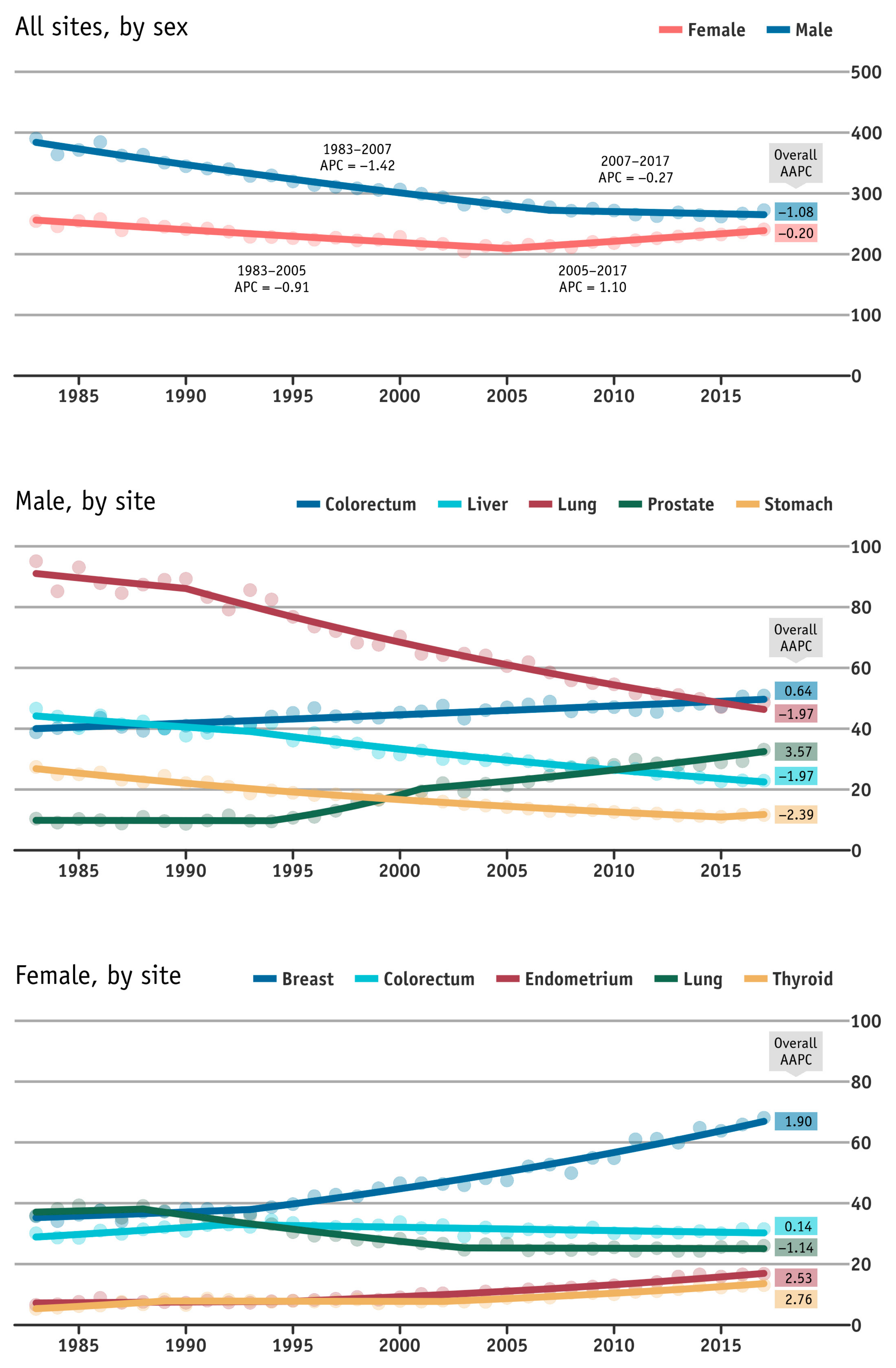
3.1. Trends of the Major Cancers in Hong Kong
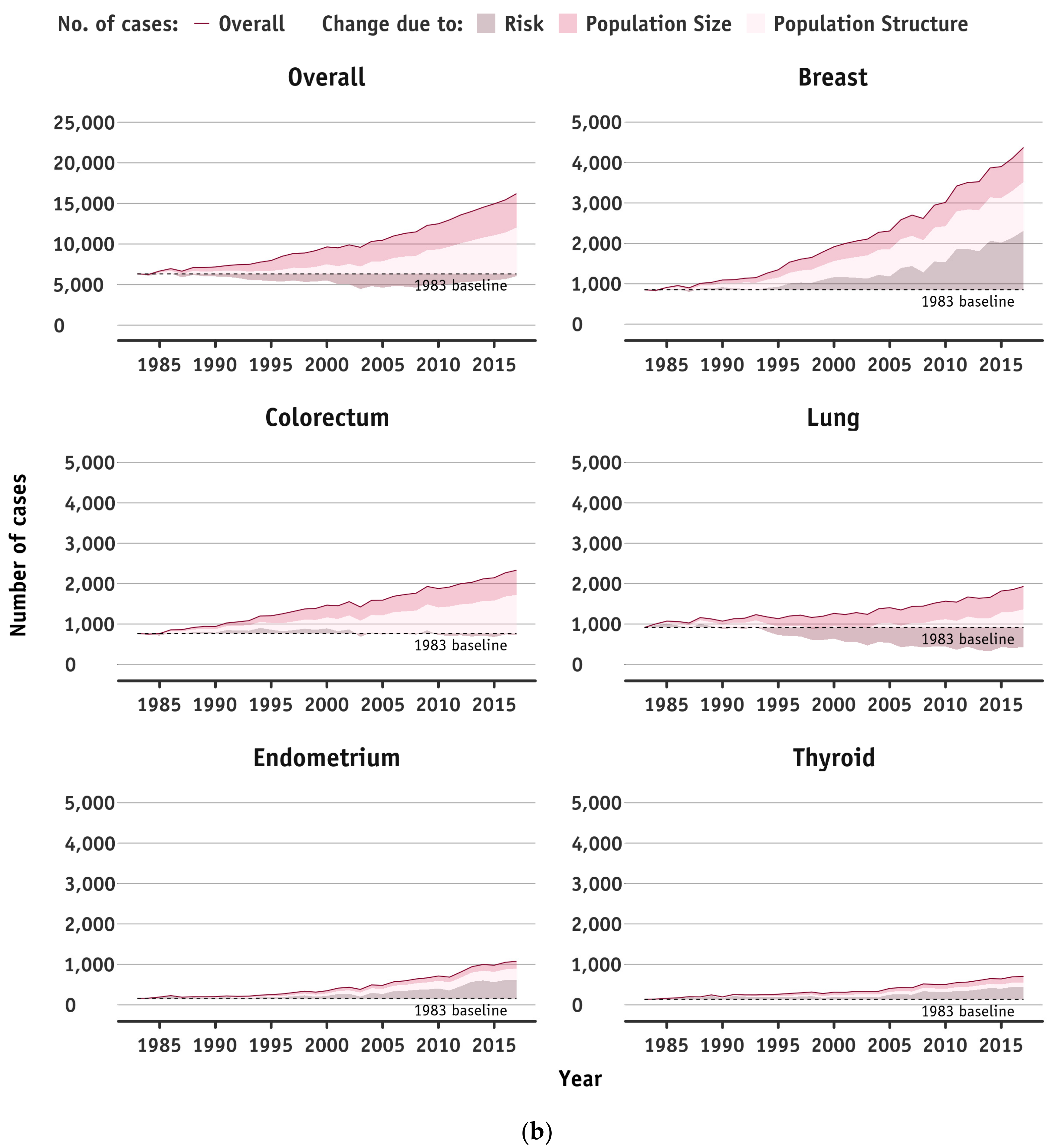
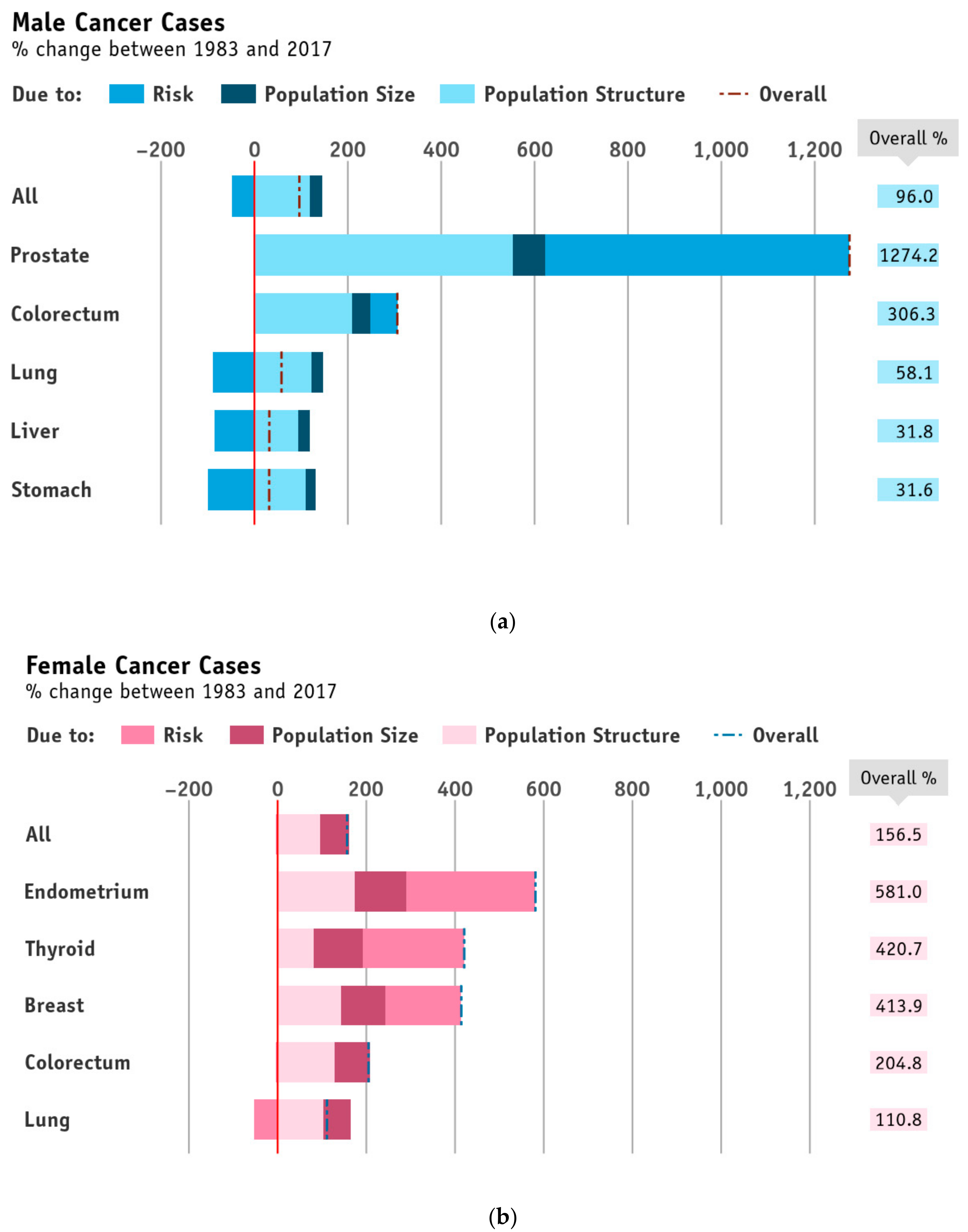
3.2. Apportioned Number of New Cases into the Contribution from the Change in Population Risk, and Changes in Population Size and Age Structure Combined
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Wild, C.P. The global cancer burden: Necessity is the mother of prevention. Nat. Rev. Cancer 2019, 19, 123–124. [Google Scholar] [CrossRef]
- Thun, M.J.; DeLancey, J.O.; Center, M.M.; Jemal, A.; Ward, E.M. The global burden of cancer: Priorities for prevention. Carcinogenesis 2010, 31, 100–110. [Google Scholar] [CrossRef] [Green Version]
- Omran, A.R. The Epidemiologic Transition: A Theory of the Epidemiology of Population Change. Milbank Mem. Fund Q. 1971, 49, 50938. [Google Scholar] [CrossRef]
- The World Bank (IBRD). Data Bank. 2019. Available online: https://data.worldbank.org/ (accessed on 10 January 2021).
- Census and Statistics Department. Population Estimates 2019. Available online: https://www.censtatd.gov.hk/hkstat/sub/sp150.jsp (accessed on 1 December 2019).
- World Health Organisation. Ageing and Health 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 1 April 2021).
- Hong Kong Cancer Registry. Overview of Hong Kong Cancer Statistics of 2017. Available online: https://www3.ha.org.hk/cancereg/pdf/overview/Overview%20of%20HK%20Cancer%20Stat%202017.pdf (accessed on 1 April 2021).
- Valls, J.; Clèries, R.; Gálvez, J.; Moreno, V.; Gispert, R.; Borrás, J.M.; Ribes, J. RiskDiff: A web tool for the analysis of the difference due to risk and demographic factors for incidence or mortality data. BMC Public Health 2009, 9, 4731–4738. [Google Scholar] [CrossRef]
- Hong Kong Cancer Registry. Cancer Statistics Query Systems 2018. Available online: http://www3.ha.org.hk/cancereg/allages.asp (accessed on 1 December 2019).
- Institute for Health Metrics and Evaluation. Global Health Data Exchange. Available online: http://ghdx.healthdata.org/ (accessed on 1 April 2021).
- Kim, H.-J.; Fay, M.P.; Feuer, E.J.; Midthune, D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2001, 20, 335–351, Correction in 2001, 20, 655. [Google Scholar] [CrossRef]
- Bashir, S.; Estève, J. Analysing the difference due to risk and demographic factors for incidence or mortality. Int. J. Epidemiol. 2000, 29, 878–884. [Google Scholar] [CrossRef] [Green Version]
- Weir, H.K.; Bs, T.D.T.; Soman, A.; Møller, B.; Ms, S.L. The past, present, and future of cancer incidence in the United States: 1975 through 2020. Cancer 2015, 121, 1827–1837. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.; Naghavi, M.; Allen, C.; Barber, R.M.; Bhutta, Z.A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; Coates, M.M.; et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1459–1544. [Google Scholar] [CrossRef] [Green Version]
- Cheng, X.; Tan, L.; Gao, Y.; Yang, Y.; Schwebel, D.C.; Hu, G. A new method to attribute differences in total deaths between groups to population size, age structure and age-specific mortality rate. PLoS ONE 2019, 14, e0216613. [Google Scholar] [CrossRef]
- Møller, B.; Weedon-Fekjaer, H.; Hakulinen, T.; Tryggvadottir, L.; Storm, H.; Talbäck, M.; Haldorsen, T. The influence of mammographic screening on national trends in breast cancer incidence. Eur. J. Cancer Prev. 2005, 14, 117–128. [Google Scholar] [CrossRef]
- Potosky, A.L.; Feuer, E.J.; Levin, D.L. Impact of screening on incidence and mortality of prostate cancer in the United States. Epidemiol. Rev. 2001, 23, 181–186. [Google Scholar] [CrossRef] [Green Version]
- Xie, S.-H.; Chen, J.; Zhang, B.; Wang, F.; Li, S.-S.; Xie, C.-H.; Tse, L.-A.; Cheng, J.-Q. Time trends and age-period-cohort analyses on incidence rates of thyroid cancer in Shanghai and Hong Kong. BMC Cancer 2014, 14, 975. [Google Scholar] [CrossRef]
- Lin, A.W.C.; Wong, B.; Lam, P.; Chan, W.K.; Chan, K. Surveillance of Viral Hepatitis in Hong Kong: 2015 Update Report; Department of Health: Hong Kong, China, 2016.
- Hong Kong Census and Statistics Department. Thematic Household Survey, Report No. 59: Pattern of Smoking; Census and Statistics Department: Hong Kong, China, 2016.
- Wong, B.C.-Y.; Lam, S.K.; Wong, W.M.; Chen, J.S.; Zheng, T.T.; Feng, R.E.; Lai, K.C.; Hu, W.H.C.; Yuen, S.T.; Leung, S.Y.; et al. Helicobacter pylori Eradication to Prevent Gastric Cancer in a High-Risk Region of China. JAMA 2004, 291, 187–194. [Google Scholar] [CrossRef] [Green Version]
- Ford, A.C.; Yuan, Y.; Moayyedi, P. Helicobacter pylori eradication therapy to prevent gastric cancer: Systematic review and meta-analysis. Gut 2020, 69, 2113–2121. [Google Scholar] [CrossRef]
- Howson, C.P.; Hiyama, T.; Wynder, E.L. The Decline in Gastric Cancer: Epidemiology of an Unplanned Triumph. Epidemiol. Rev. 1986, 8, 1–27. [Google Scholar] [CrossRef]
- McPherson, K.; Steel, C.M.; Dixon, J.M. Breast cancer—Epidemiology, risk factors, and genetics. BMJ 2000, 321, 624–628. [Google Scholar] [CrossRef] [Green Version]
- Sheikh, M.A.; Althouse, A.D.; Freese, K.E.; Soisson, S.; Edwards, R.P.; Welburn, S.; Sukumvanich, P.; Comerci, J.; Kelley, J.; LaPorte, R.E.; et al. USA Endometrial Cancer Projections to 2030: Should we be concerned? Future Oncol. 2014, 10, 2561–2568. [Google Scholar] [CrossRef]
- Felix, A.S.; Brinton, L.A. Cancer Progress and Priorities: Uterine Cancer. Cancer Epidemiol. Biomark. Prev. 2018, 27, 985–994. [Google Scholar] [CrossRef] [Green Version]
- McCracken, K.; Phillips, D.R. Demographic and epidemiological transition. In International Encyclopedia of Geography: People, the Earth, Environment and Technology; John Wiley & Sons: Hoboken, NJ, USA, 2016; pp. 1–8. [Google Scholar]
- Stewart, B.W.; Wild, C.P. World Cancer Report 2014; France International Agency for Research on Cancer: Lyon, France, 2014.
- Wong, I.O.L.; Cowling, B.J.; Law, S.C.K.; Mang, O.W.K.; Schooling, C.M.; Leung, G.M. Understanding sociohistorical imprint on cancer risk by age-period-cohort decomposition in Hong Kong. J. Epidemiol. Community Health 2010, 64, 596–603. [Google Scholar] [CrossRef] [Green Version]
- Smith, B.; Smith, G.; Hurria, A.; Hortobagyi, G.N.; Buchholz, T.A. Future of Cancer Incidence in the United States: Burdens Upon an Aging, Changing Nation. J. Clin. Oncol. 2009, 27, 2758–2765. [Google Scholar] [CrossRef]
- Møller, B.; Fekjaer, H.; Hakulinen, T.; Tryggvadóttir, L.; Storm, H.H.; Talbäck, M.; Haldorsen, T. Prediction of cancer incidence in the Nordic countries up to the year 2020. Eur. J. Cancer Prev. 2002, 11, S1–S96. [Google Scholar]
- Tsoi, K.K.F.; Hirai, H.W.; Chan, F.C.H.; Griffiths, S.; Sung, J.J.Y. Cancer burden with ageing population in urban regions in China: Projection on cancer registry data from World Health Organization. Br. Med. Bull. 2016, 121, 83–94. [Google Scholar] [CrossRef]
- Aitken, J.; Allemani, C.; de Silva, A.G.; Bonaventure, A.; Chen, W.; Coleman, M. Global surveillance of trends in cancer survival: Analysis of individual records for 37,513,025 patients diagnosed with one of 18 cancers during 2000–2014 from 322 population-based registries in 71 countries (CONCORD-3). Lancet 2018, 391, 1023–1075. [Google Scholar]
- Etemadi, A.; Safiri, S.; Sepanlou, S.G.; Ikuta, K.; Bisignano, C.; Shakeri, R.; Zamani, M.; Fitzmaurice, C.; Nixon, M.; Abbasi, N.; et al. The global, regional, and national burden of stomach cancer in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 42–54. [Google Scholar] [CrossRef] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wong, I.O.L.; Lam, Y.T.; Lam, K.F.; Cowling, B.J.; Leung, G.M. Demographic and Epidemiological Contributions to Recent Trends in Cancer Incidence in Hong Kong. Cancers 2021, 13, 5727. https://doi.org/10.3390/cancers13225727
Wong IOL, Lam YT, Lam KF, Cowling BJ, Leung GM. Demographic and Epidemiological Contributions to Recent Trends in Cancer Incidence in Hong Kong. Cancers. 2021; 13(22):5727. https://doi.org/10.3390/cancers13225727
Chicago/Turabian StyleWong, Irene Oi Ling, Yan Ting Lam, Kwok Fai Lam, Benjamin John Cowling, and Gabriel Matthew Leung. 2021. "Demographic and Epidemiological Contributions to Recent Trends in Cancer Incidence in Hong Kong" Cancers 13, no. 22: 5727. https://doi.org/10.3390/cancers13225727





