EBV-Driven Lymphoproliferative Disorders and Lymphomas of the Gastrointestinal Tract: A Spectrum of Entities with a Common Denominator (Part 3)
Abstract
Simple Summary
Abstract
1. Introduction
2. CAEBV of T-Cell and NK-Cell Type, Systemic Form
2.1. General Features and Etiology
2.2. CAEBV and GIT
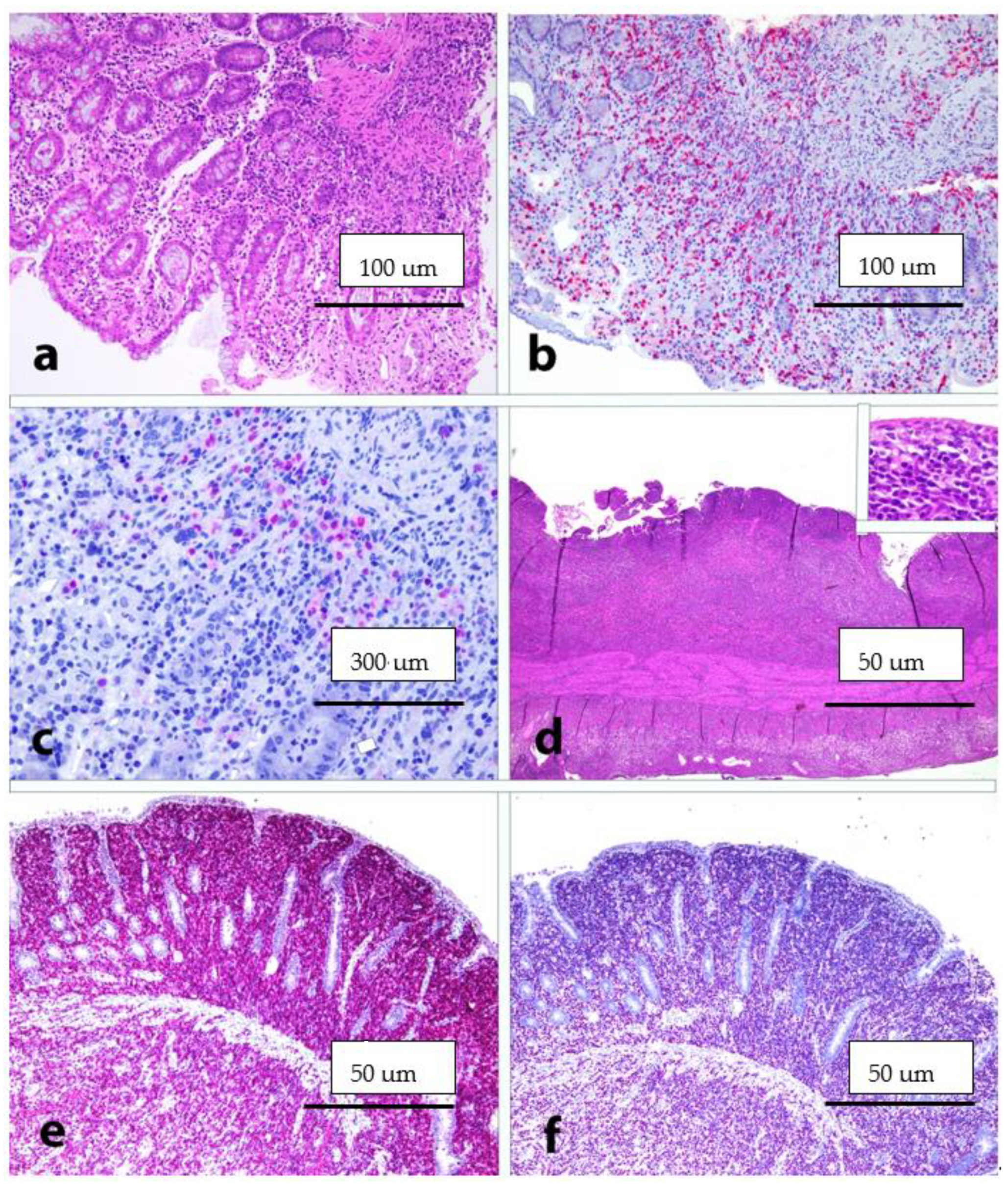
2.3. Histology, Immunophenotype and Genetic Profile
2.4. Differential Diagnosis
2.5. Treatment and Outcome
3. ENKTL-NT
3.1. General Features and Etiology
3.2. ENKTL-NT and GIT
3.3. Histology, Immunophenotype and Genetic Profile
3.4. Differential Diagnosis
3.5. Treatment and Oucome
4. PTLDs
4.1. General Features and Etiology
4.2. PTLDs and GIT
4.3. Histology, Immunophenotype and Genetic Profile
4.4. Differential Diagnosis
4.5. Treatment and Outcome
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Taylor, G.S.; Long, H.M.; Brooks, J.M.; Rickinson, A.B.; Hislop, A.D. The immunology of Epstein-Barr virus induced disease. Annu. Rev. Immunol. 2015, 33, 787–821. [Google Scholar] [CrossRef]
- Young, L.S.; Yap, L.F.; Murray, P.G. Epstein-Barr virus: More than 50 years old and still providing surprises. Nat. Rev. Cancer 2016, 16, 789–802. [Google Scholar] [CrossRef]
- Resk, S.A.; Weiss, L.M. Epstein-Barr virus-associated lymphoproliferative disorders. Hum. Pathol. 2007, 38, 1293–1304. [Google Scholar] [CrossRef]
- Tanner, J.E.; Alfieri, C. The Epstein-Barr virus and post-transplant lymphoproliferative disease: Interplay of immunosuppression, EBV, and the immune system in disease pathogenesis. Transpl. Infect. Dis. 2001, 3, 60–69. [Google Scholar] [CrossRef]
- Hakim, F.T.; Gress, R.E. Immunosenescence: Deficits in adaptative immunity in the elderly. Tissue Antigens 2007, 70, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Ghia, P.; Prato, G.; Stella, S.; Scielzo, C.; Geuna, M.; Caligaris-Cappio, F. Age-dependent accumulation of monoclonal CD4+ CD8+ double positive T lymphocytes in the peripheral blood of the elderly. Br. J. Haematol. 2007, 139, 780–790. [Google Scholar] [CrossRef] [PubMed]
- Dolcetti, R.; Dal Col, J.; Martorelli, D.; Carbone, A.; Klein, E. Interplay among viral antigens, cellular pathways and tumor microenvironment in the pathogenesis of EBV-driven lymphoma. Semin. Cancer Biol. 2013, 13, 441–456. [Google Scholar] [CrossRef]
- Swerdlow-SH, C.E.; Harris, N.L. WHO Classification of Tumours Haematopoietic and Lymphoid Tissues, Revised 4th ed.; WHO Classification of Tumours Editorial Board, Ed.; IARC: Lyon, France, 2017. [Google Scholar]
- Dunmire, S.K.; Hogquist, K.A.; Balfour, H.H. Infectious mononucleosis. Curr. Top. Microbiol. 2015, 390, 151–209. [Google Scholar]
- Rickinson, A.B. Co-infections, inflammation and oncogenesis: Future directions for EBV research. In Seminars in Cancer Biology; Academic Press: Cambridge, MA, USA, 2014; pp. 99–115. [Google Scholar]
- Price, A.M.; Luftig, M.A. To be or not IIb: A multi-step process for Epstein-Barr virus latency establishment and consequences for B cell tumorigenesis. PLoS Pathog. 2015, 11, e1004656. [Google Scholar] [CrossRef]
- Dojcinov, S.D.; Fend, F.; Quintanilla-Martinez, L. EBV-positive lymphoproliferation of B-T- and NK-cell derivation in non-immunocompromised hosts. Pathogens 2018, 7, 28. [Google Scholar] [CrossRef]
- Fujiwara, S.; Kimura, H. Editorial: Epstein-Barr virus-associated T/NK-cell lymphoproliferative diseases. Front. Pediatr. 2019, 7, 285. [Google Scholar] [CrossRef]
- Kim, W.Y.; Montes-Mojarro, I.A.; Fend, F.; Quintanilla-Martinez, L. Epstein-Barr virus-associated T and NK-cell lymphoproliferative diseases. Front. Pediatr. 2019, 7, 71. [Google Scholar] [CrossRef]
- Kimura, H.; Fujiwara, S. Overview of EBV-associated T/NK-cell lymphoproliferative diseases. Front. Pediatr. 2019, 6, 417. [Google Scholar] [CrossRef]
- Dojcinov, S.D.; Venkataraman, G.; Raffeld, M.; Pittaluga, S.; Jaffe, E.S. EBV positive mucocutaneous ulcer. A study of 26 cases associated with various sources of immunosuppression. Am. J. Surg. Pathol. 2010, 34, 405–417. [Google Scholar] [CrossRef]
- Ikeda, T.; Gion, Y.; Yoshino, T.; Sato, Y. A review of EBV-positive mucocutaneous ulcers focusing on clinical and pathological aspects. J. Clin. Exp. Hematopath. 2019, 59, 64–71. [Google Scholar] [CrossRef]
- Ikeda, T.; Gion, Y.; Nishimura, M.F.; Yoshino, T.; Sato, Y. Epstein-Barr Virus-positive mucocutaneous ulcer: A unique and curious disease entity. Int. J. Mol. Sci. 2021, 22, 1053. [Google Scholar] [CrossRef]
- Matnani, R.; Peker, D. Azathioprine induced Epstein Barr virus-positive mucocutaneous ulcer arising in perianal fistula and abscess associated with Crohn’s disease. J. Crohn’s Colitis 2014, 8, 1747–1748. [Google Scholar] [CrossRef] [PubMed]
- Moran, N.R.; Webster, B.; Lee, K.M.; Trotman, J.; Kwan, Y.-L.; Napoli, J.; Leong, R.W. Epstein Barr virus-positive mucocutaneous ulcer of the colon associated Hodgkin lymphoma in Crohn’s disease. World J. Gastroenterol. 2015, 21, 6072–6076. [Google Scholar] [CrossRef]
- Juan, A.; Lobaton, T.; Tapja, G.; Manosa, M.; Cabrè, E. Epstein-Barr virus-positive mucocutaneous ulcer in Crohn’s disease. A condition to consider in immunosuppressed IBD patients. Dig. Liver Dis. 2017, 49, 934–937. [Google Scholar] [CrossRef] [PubMed]
- Zanelli, M.; Mengoli, M.C.; Valli, R.; Froio, E.; Bisagni, A.; Zizzo, M.; De Marco, L.; Ascani, S. Primary classic Hodgkin lymphoma of the ileum and Epstein-Barr virus mucocutaneous ulcer of the colon: Two entities compared. Virchows Archiv. 2019, 474, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Osman, M.; Al Salihi, M.; Abu Sitta, E.; Al Hadidi, S. A rare case of Epstein-Barr virus mucocutaneous ulcer of the colon. BMJ Case Rep. 2017, bcr2017220717. [Google Scholar] [CrossRef]
- Zanelli, M.; Zizzo, M.; Foroni, M.; De Marco, L.; Martino, G.; Ascani, S. EBV-positive mucocutaneous ulcer within colonic diverticulitis mimicking diffuse large B-cell lymphoma. Ann. Hematol. 2019, 98, 1795–1797. [Google Scholar] [CrossRef] [PubMed]
- Volaric, A.K.; Singh, K.; Gru, A.A. Rare EBV-associated B cell neoplasms of the gastrointestinal tract. Semin. Diagn. Pathol. 2021, 38, 38–45. [Google Scholar] [CrossRef]
- Ikeda, T.; Gion, Y.; Sakamoto, M.; Tachibana, T.; Nishikori, A.; Nishimura, M.F.; Yoshino, T.; Sato, Y. Clinicopathological analysis of 34 Japanese patients with EBV-positive mucocutaneous ulcer. Mod. Pathol. 2020, 33, 2437–2448. [Google Scholar] [CrossRef] [PubMed]
- Prieto-Torres, L.; Erana, I.; Gil-Redondo, R.; de la Riva, I.G.; Manso, R.; Pajares, R.; Cordoba, R.; Machan, S.; Ara, M.; Requena, L.; et al. The spectrum of EBV-positive mucocutaneous ulcer: A study of 9 cases. Am. J. Surg. Pathol. 2019, 43, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Goetgebuer, R.L.; van der Woude, C.J.; de Ridder, L.; Doukas, M.; de Vries, A.C. Clinical and endoscopic complications of Epstein-Barr virus in inflammatory bowel disease: An illustrative case series. Int. J. Colorectal. Dis. 2019, 34, 923–926. [Google Scholar] [CrossRef]
- Pugh, M.R.; Leopold, G.D.; Morgan, M.; Christian, A.D.; Hewett, R.; Durai, D.; Wagstaff, J.; Harris, D.; Dojcinov, S.D. Epstein Barr virus-positive mucocutaneous ulcers complicate colitis caused by immune checkpoint regulator therapy and associate with colon perforation. Clin. Gastroenterol. Hepatol. 2020, 18, 1785. [Google Scholar] [CrossRef]
- Daroontum, T.; Kohno, K.; Eladi, A.E.; Satou, A.; Sakakibara, A.; Matsukage, S.; Yakushiji, N.; Ya-In, C.; Nakamura, S.; Asano, N.; et al. Comparison of Epstein-Barr virus-positive mucocutaneous ulcer associated with treated lymphoma or methotrexate in Japan. Histopathology 2018, 72, 1115–1127. [Google Scholar] [CrossRef]
- Morita, N.; Okuse, C.; Suetani, K.; Nakano, H.; Hiraishi, T.; Ishigooka, S.; Mori, S.; Shimamura, T.; Asakura, T.; Koike, J.; et al. A rare case of Epstein-Barr virus-positive mucocutaneous ulcer that developed into an intestinal obstruction: A case report. BMC Gastroenterol. 2020, 20, 9. [Google Scholar] [CrossRef]
- Ishikawa, E.; Satou, A.; Nakamura, M.; Nakamura, S.; Fujishiro, M. Epstein-Barr virus positive B-cell lymphoproliferative disorders of the gastrointestinal tract. Cancers 2021, 13, 3815. [Google Scholar] [CrossRef]
- Sinit, R.B.; Horan, K.L.; Dorer, R.K.; Aboulafia, D.M. Epstein-Barr virus-positive mucocutaneous ulcer: Case report and review of the first 100 published cases. Clin. Lymphoma Myeloma Leuk. 2019, 19, E81–E92. [Google Scholar] [CrossRef] [PubMed]
- Miyagi, S.; Ishikawa, E.; Nakamura, M.; Shimada, K.; Yamamura, T.; Furukawa, K.; Tanaka, T.; Mabuchi, S.; Tsuyuki, Y.; Kohno, K.; et al. Reappraisal of primary Epstein-Barr virus (EBV)-positive diffuse large B-cell lymphoma of the gastrointestinal tract. Am. J. Surg. Pathol. 2020, 44, 1173–1183. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, E.; Kato, S.; Shimada, K.; Tanaka, T.; Suzuki, Y.; Satou, A.; Kohno, K.; Sakakibara, A.; Yamamura, T.; Nakamura, M.; et al. Clinicopathological analysis of primary intestinal diffuse large B-cell lymphoma: Prognostic evaluation of CD5, PD-L1 and Epstein-Barr virus on tumor cells. Cancer Med. 2018, 7, 6051–6063. [Google Scholar] [CrossRef]
- Castillo, J.J.; Beltran, B.E.; Miranda, R.N.; Young, K.H.; Chavez, J.C.; Sotomayor, E.M. EBV-positive large B-cell lymphoma, not otherwise specified: 2018 update on diagnosis, risk-stratification and management. Am. J. Hematol. 2018, 93, 953–962. [Google Scholar] [CrossRef]
- Sanguedolce, F.; Zanelli, M.; Ascani, S.; Zizzo, M.; Tortorella, S.; Soriano, A.; Fiorelli, A.; Cocco, G.; Ardò, N.; Sollitto, F.; et al. PD-L1 as a prognostic and predictive biomarker in neuroendocrine tumors of the lung: State of the art and future perspectives. Minerva Respir. Med. 2021, 60, 36–51. [Google Scholar] [CrossRef]
- Hu, L.Y.; Xu, X.L.; Rao, H.L.; Chen, J.; Lai, R.C.; Huang, H.Q.; Jiang, W.Q.; Lin, T.Y.; Xia, Z.J.; Cai, Q.Q. Expression and clinical value of programmed cell death-ligand 1 (PD-L1) in diffuse large B-cell lymphoma: A retrospective study. Clin. J. Cancer 2017, 36, s40880. [Google Scholar] [CrossRef]
- Georgiou, K.; Chen, L.; Berglund, M.; Ren, W.; de Miranda, N.; Lisboa, S.; Fangazio, M.; Zhu, S.D.; Hou, Y.; Wu, K.; et al. Genetic basis of PD-L1 overexpression in diffuse large B-cell lymphoma. Blood 2016, 127, 3026–3034. [Google Scholar] [CrossRef] [PubMed]
- McCord, R.; Bolen, C.R.; Koeppen, H.; Kadel, E.E.; Oestergaard, M.Z.; Nielsen, T.; Sehn, L.H.; Venstrom, J.M. PD-L1 and tumor-associated macrophages in de novo DLBCL. Blood Adv. 2019, 3, 531–540. [Google Scholar] [CrossRef]
- Kiyasu, J.; Miyoshi, H.; Hirata, A.; Arakawa, F.; Ichikawa, A.; Niino, D.; Sugita, Y.; Yufu, Y.; Choi, I.; Abe, Y.; et al. Expression of programmed cell death ligand 1 is associated with poor overall survival in patients with diffuse large B-cell lymphoma. Blood 2015, 126, 2193–2201. [Google Scholar] [CrossRef]
- Ishikawa, E.; Nakamura, M.; Shimada, K.; Tanaka, T.; Satou, A.; Kohno, K.; Sakakibara, A.; Furukawa, K.; Yamamura, T.; Miyahara, R. Prognostic impact of PD-L1 expression in primary gastric and intestinal diffuse large B-cell lymphoma. J. Gastroenterol. 2020, 55, 39–50. [Google Scholar] [CrossRef]
- Devaney, K.; Jaffe, E.S. The surgical pathology of gastrointestinal Hodgkin’s disease. Am. J. Clin. Pathol. 1991, 95, 794–801. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Wang, Y.; Zhao, H.; Liu, S.; Li, Q.; Lin, L.; Yue, Y.; Wang, X.; Zhao, Z.; Yu, Y.; et al. Clinical characteristics of 26 patients with primary extranodal Hodgkin lymphoma. Int. J. Clin. Exp. Pathol. 2014, 7, 5045–5050. [Google Scholar]
- Morgan, P.B.; Kessel, I.L.; Xiao, S.Y.; Colman, M. Uncommon presentations of Hodgkin’s disease. Case 1. Hodgkin’s disease of the jejunum. J. Clin. Oncol. 2004, 22, 193–195. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, A.; Flora, A.C.; Soares, F.A.; de Lima, V.C.C. Primary Hodgkin lymphoma of the rectum: An unusual presentation. J. Clin. Oncol. 2011, 29, 268–270. [Google Scholar] [CrossRef]
- Sharma, S.; Rana, S.; Kapur, S.; Jairajpuri, Z.S. Primary intestinal Hodgkin lymphoma: An uncommon presentation. J. Lab. Physicians 2013, 5, 124–126. [Google Scholar] [PubMed]
- Vaduvesan, J.A.; Nair, R.A.; Nambiar, K.R. Primary classical Hodgkin lymphoma of rectum: Report of an extremely rare case and review of the literature. Indian J. Pathol. Microbiol. 2017, 60, 412–414. [Google Scholar]
- Parente, P.; Zanelli, M.; Zizzo, M.; Carosi, I.; Di Candia, L.; Sperandeo, M.; Lacedonia, D.; Fesce, V.F.; Ascani, S.; Graziano, P. Primary pulmonary Hodgkin lymphoma presenting as multiple cystic lung lesions: Diagnostic usefulness of cell block. Cytopathology 2020, 31, 236–239. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Fend, F.; Quintanilla-Martinez, L.; Kingma, D.; Sorbara, L.; Raffeld, M.; Banks, P.M.; Jaffe, E.S. Epstein-Barr virus-positive primary gastrointestinal Hodgkin’s disease: Association with inflammatory bowel disease and immunosuppression. Am. J. Surg. Pathol. 2000, 24, 66. [Google Scholar] [CrossRef] [PubMed]
- Barzilai, M.; Polliack, A.; Avivi, I.; Herishanu, Y.; Ram, R.; Tang, C.; Perry, C.; Sarid, N. Hodgkin lymphoma of the gastrointestinal tract in patients with inflammatory bowel disease: Portrait of a rare entity. Leuk. Res. 2018, 71, 1–5. [Google Scholar] [CrossRef]
- Gibson, B.; Bajramovic Podoli, M.; Baumgartner, E.M.; Haninger Maley, D. Syncitial variant of nodular sclerosis classical Hodgkin lymphoma of the terminal ileum in a patient with lonstanding Crohn’s disease. Ann. Clin. Lab. Sci. 2016, 46, 219–221. [Google Scholar]
- Gualco, G.; Ortega, V.; Chioato, L.; Musto, M.L.; Bacchi, L.M.; Weiss, L.M.; Bacchi, C.E. Hodgkin’s lymphoma presenting as dominant gastric lesion in immunocompetent patients: Report of 5 cases with EBV analysis. Int. J. Surg. Pathol. 2011, 19, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Parente, P.; Zanelli, M.; Sanguedolce, F.; Mastracci, L.; Graziano, P. Hodgkin Reed-Sternberg-like cells in non-Hodgkin lymphoma. Diagnostics 2020, 10, 1019. [Google Scholar] [CrossRef] [PubMed]
- Ansell, S.M. Hodgkin lymphoma: A 2020 update on diagnosis, risk stratification and management. Am. J. Haematol. 2020, 95, 978–989. [Google Scholar] [CrossRef] [PubMed]
- Delecleuse, H.J.; Anagnostopoulos, I.; Dallenbach, F.; Hummel, M.; Marafioti, T.; Schneider, U.; Huhn, D.; Schmidt-Westhausen, A.; Reichart, P.A.; Gross, U.; et al. Plasmablastic lymphomas of the oral cavity: A new entity associated with the human immunodeficiency virus infection. Blood 1997, 89, 1413–1420. [Google Scholar] [CrossRef]
- Zizzo, M.; Zanelli, M.; Martiniani, R.; Sanguedolce, F.; De Marco, L.; Martino, G.; Parente, P.; Annessi, V.; Manzini, L.; Ascani, S. Oral plasmablastic lymphoma: A case report. Medicine 2020, 99, e22335. [Google Scholar] [CrossRef]
- Morscio, J.; Dierickx, D.; Nijs, J.; Verhoef, G.; Bittoun, E.; Vanoeteren, X.; Wlodarska, I.; Sagaert, X.; Tousseyn, T. Clinicopathologic comparison of plasmablastic lymphoma in HIV-positive, immunocompetent and posttransplant patients single-center series of 25 cases and meta-analysis of 277 reported cases. Am. J. Surg. Pathol. 2014, 38, 875–886. [Google Scholar] [CrossRef]
- Castillo, J.J.; Bibas, M.; Miranda, R.N. The biology and treatment of plasmablastic lymphoma. Blood 2015, 125, 2323–2330. [Google Scholar] [CrossRef]
- Harmon, C.M.; Smith, L.B. Plasmablastic lymphoma a review of clinicopathologic features and differential diagnosis. Arch. Pathol. Lab. Med. 2016, 140, 1074–1078. [Google Scholar] [CrossRef]
- Sanguedolce, F.; Zanelli, M.; Zizzo, M.; Martino, G.; Rossi, C.; Parente, P.; Ascani, S. Clinical, pathological and molecular features of plasmablastic lymphoma arising in the gastrointestinal tract: A review and reappraisal. Pathol. Res. Pract. 2020, 216, 152973. [Google Scholar] [CrossRef]
- Lopez, A.; Abrisqueta, P. Plasmablastic lymphoma: Current perspectives. Blood Lymph. Cancer Targets Ther. 2018, 8, 63–70. [Google Scholar] [CrossRef]
- Luria, L.; Nguyen, J.; Zhou, J.; Jaglal, M.; Sokol, L.; Messina, J.L.; Coppola, D.; Zhang, L. Manifestations of gastrointestinal plasmablastic lymphoma: A case series with literature review. World J. Gastroenterol. 2014, 20, 11894–11903. [Google Scholar] [CrossRef]
- Liu, C.; Varikatt, W.; Ping, C.H. Plasmablastic lymphoma presenting as a colonic stricture in Crohn’s disease. Pathology 2014, 46, 77–78. [Google Scholar] [CrossRef]
- Zanelli, M.; Ragazzi, M.; Valli, R.; De Marco, L.; Cecinato, P.; Azzolini, F.; Ferrari, A.; Bacci, F.; Ascani, S. Unique presentation of a plasmablastic lymphoma superficially involving the entire large bowel. Pathol. Res. Pract. 2015, 211, 1030–1033. [Google Scholar] [CrossRef]
- Valera, A.; Balague, O.; Colomo, L.; Martinez, A.; Delabie, J.; Taddesse-Heath, L.; Jaffe, E.S.; Campo, E. IG/MYC rearrangements are the main cytogenetic alteration in plasmablastic lymphomas. Am. J. Surg. Pathol. 2010, 34, 1686–1694. [Google Scholar] [CrossRef]
- Montes-Moreno, S.; Martinez-Magunacelaya, N.; Zecchini-Barrese, T.; Gonzalez de Villambrosia, S.; Linares, E.; Ranchal, T.; Rodriguez-Pinilla, M.; Battle, A.; Cereceda-Company, L.; Revert-Arce, J.B.; et al. Plasmablastic lymphoma phenotype is determined by genetic alterations in MYC and PRDM1. Mod. Pathol. 2017, 30, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Castillo, J.J. Plasmablastic lymphoma: Are more intensive regimens needed? Leuk. Res. 2011, 35, 1547–1548. [Google Scholar] [CrossRef] [PubMed]
- Pretscher, D.; Kalish, A.; Wilhelm, M.; Birkmann, J. Refractory plasmablastic lymphoma. A review of treatment options beyond standard therapy. Ann. Hematol. 2017, 96, 967–970. [Google Scholar] [CrossRef]
- Castillo, J.J.; Reagan, J.L.; Sikov, W.M.; Winer, E.S. Bortezomib in combination with infusional dose-adjusted EPOCH for the treatment of plasmablastic lymphoma. Br. J. Haematol. 2015, 169, 352–355. [Google Scholar] [CrossRef]
- Al-Malki, M.M.; Castillo, J.J.; Sloan, J.M.; Re, A. Hematopoietic cell transplantation for plasmablastic lymphoma: A review. Biol. Blood Marrow Transplant. 2014, 20, 1877–1884. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.J.; Chuang, S.S. Lymphoid neoplasms with plasmablastic differentiation: A comprehensive review and diagnostic approaches. Adv. Anat. Pathol. 2020, 27, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Loghavi, S.; Alayed, K.; Aladily, T.N.; Zuo, Z.; Ng, S.B.; Tang, G.; Hu, S.; Yin, C.C.; Miranda, R.N.; Medeiros, L.J.; et al. Stage, age and EBV status impact outcomes of plasmablastic lymphoma patients: A clinicopathologic analysis of 61 patients. J. Hematol. Oncol. 2015, 8, 65. [Google Scholar] [CrossRef] [PubMed]
- Laurent, C.; Fabiani, B.; Do, C.; Tchernonog, E.; Cartron, G.; Gravelle, P.; Amara, N.; Malot, S.; Palisoc, M.M.; Copie-Bergman, C.; et al. Immune-checkpoint expression in Epstein-Barr virus positive and negative plasmablastic lymphoma: A clinical and pathological study in 82 patients. Haematologica 2016, 101, 976–984. [Google Scholar] [CrossRef]
- Zanelli, M.; Sanguedolce, F.; Zizzo, M.; Palicelli, A.; Bassi, M.C.; Santandrea, G.; Martino, G.; Soriano, A.; Caprera, C.; Corsi, M.; et al. Primary effusion lymphoma occurring in the setting of transplanted patients: A systematic review of a rare, life-threatening post-transplantation occurrence. BMC Cancer 2021, 21, 468. [Google Scholar] [CrossRef]
- Chadburn, A.; Hyjek, E.; Mathew, S.; Cesarman, E.; Said, J.; Knowles, D.M. KSHV-positive solid lymphomas represent an extra-cavitary variant of primary effusion lymphoma. Am. J. Surg. Pathol. 2004, 28, 1401–1416. [Google Scholar] [CrossRef]
- Kim, Y.; Leventaki, V.; Bhaijee, F.; Jackson, C.C.; Medeiros, L.J.; Vega, F. Extracavitary/solid variant of primary effusion lymphoma. Ann. Diagn. Pathol. 2012, 16, 441–446. [Google Scholar] [CrossRef]
- Pan, Z.G.; Zhang, Q.Y.; Lu, Z.B.L.; Quinto, T.; Rozenvald, I.B.; Liu, L.T.; Wilson, D.; Reddy, V.; Huang, Q.; Wang, H.Y.; et al. Extracavitary KSHV-associated large B-cell lymphoma: A distinct entity or a subtype of primary effusion lymphoma? Study of 9 cases and review of an additional 43 cases. Am. J. Surg. Pathol. 2012, 36, 1129–1140. [Google Scholar] [CrossRef] [PubMed]
- Costes, V.; Faumont, N.; Cesarman, E.; Rousset, T.; Meggetto, F.; Delsol, G.; Brousset, P. Human herpes-virus-8-associated lymphoma of the bowel in human immunodeficiency virus-positive patients without history of primary effusion lymphoma. Hum. Pathol. 2002, 33, 846–849. [Google Scholar] [CrossRef]
- Navarro, J.T.; Ribera, J.M.; Juncà, J.; Millà, F. Anorectal lymphoma without effusion associated with human herpesvirus-8 and type 1 Epstein-Barr virus in an HIV infected patient. Hum. Pathol. 2003, 34, 630. [Google Scholar] [CrossRef]
- Liao, G.; Cai, J.; Yue, C.; Quing, X. Extracavitary/solid variant of primary effusion lymphoma presenting as a gastric mass. Exp. Mol. Pathol. 2015, 99, 445–448. [Google Scholar] [CrossRef] [PubMed]
- Pantanowitz, L.; Wu, Z.; Dezube, B.J.; Pihan, G. Extracavitary primary effusion lymphoma of the anorectum. Clin. Lymphoma Myeloma 2005, 6, 149–152. [Google Scholar] [CrossRef]
- Zanelli, M.; Bertuzzi, C.; Zizzo, M.; Martino, G.; Sabattini, E.; Ascani, S. Extracavitary primary effusion lymphoma in a post-transplantation patient. Br. J. Hematol. 2019, 187, 55. [Google Scholar] [CrossRef]
- DePond, W.; Said, J.W.; Tasaka, T.; de Vos, S.; Kahn, D.; Cesarman, E.; Knowles, D.M.; Koeffler, H.P. Kaposi’s sarcoma-associated herpesvirus and human herpesvirus 8 (KSHV/HHV8)-associated lymphoma of the bowel. Report of two cases in HIV-positive men with secondary effusion lymphomas. Am. J. Surg. Pathol. 1997, 21, 719–724. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Chang, K.L.; Gaal, K.; Aber, D.A. Primary effusion lymphoma with subsequent development of a small bowel mass in an HIV-seropositive patient: A case report and literature review. Am. J. Surg. Pathol. 2002, 26, 1363–1367. [Google Scholar] [CrossRef] [PubMed]
- Oster, C.; Stein, T.; Kitahara, S.; Alkan, S.; Huang, Q. Kaposi sarcoma-associated herpesvirus/human herpesvirus 8-associated extracavitary primary effusion lymphoma presenting as multiple lymphomatous polyposis. Hum. Pathol. 2018, 79, 177–183. [Google Scholar] [CrossRef]
- Pellet Madan, R.; Hand, J. Human herpesvirus 6, 7, and 8 in solid organ transplantation: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clinical. Transplant. 2019, 33, e13518. [Google Scholar] [CrossRef] [PubMed]
- Zanelli, M.; Zizzo, M.; Bisagni, A.; Froio, E.; De Marco, L.; Valli, R.; Filosa, A.; Luminari, S.; Martino, G.; Massaro, F.; et al. Germinotropic lymphoproliferative disorder: A systematic review. Ann. Hematol. 2020, 99, 2243–2253. [Google Scholar] [CrossRef]
- Zanelli, M.; Fraternali Orcioni, G.; Zizzo, M.; De Marco, L.; Martino, G.; Cerrone, G.; Cabra, A.D.; Ascani, S. HHV-8- and EBV-positive germinotropic lymphoproliferative disorder. Ann. Hematol. 2019, 98, 2439–2441. [Google Scholar] [CrossRef]
- Zanelli, M.; Stingeni, L.; Zizzo, M.; Martino, G.; Sanguedolce, F.; Marra, A.; Crescenzi, B.; Pileri, S.A. HHV8-positive Castleman disease and in situ mantle cell neoplasia within dermatopathic lymphadenitis, in longstanding psoriasis. Diagnostics 2021, 11, 1150. [Google Scholar] [CrossRef]
- Lurain, K.; Polizzotto, M.N.; Aleman, K.; Bhutani, M.; Wyvill, K.M.; Goncalves, P.H.; Ramaswami, R.; Marshall, V.A.; Miley, W.; Steinberg, S.M.; et al. Viral, immunologic and clinical features of primary effusion lymphoma. Blood 2019, 133, 1753–1761. [Google Scholar] [CrossRef]
- Okada, S.; Goto, H.; Yotsumoto, M. Current status of treatment for primary effusion lymphoma. Intractable Rare Dis. Res. 2014, 3, 65–74. [Google Scholar] [CrossRef]
- Burkitt, D. A sarcoma involving the jaw of African children. Br. J. Surg. 1958, 46, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Epstein, M.A.; Achong, B.G.; Barr, Y.M. Virus particle in cultured lymphoblasts from Burkitt’s lymphoma. Lancet 1964, 1, 702–703. [Google Scholar] [CrossRef]
- De Thé, G.; Geser, A.; Day, N.E.; Tukei, P.M.; Williams, E.H.; Beri, D.P.; Smith, P.G.; Dean, A.G.; Bronkamm, G.W.; Feorino, P.; et al. Epidemiological evidence for causal relationship between Epstein-Barr virus and Burkitt’s lymphoma from Ugandan prospective study. Nature 1978, 274, 756–761. [Google Scholar] [CrossRef]
- Van Den Bosch, C. A role for RNA viruses in the pathogenesis of Burkitt’s lymphoma: The need for reappraisal. Adv. Hematol. 2012, 2012, 494758. [Google Scholar] [CrossRef] [PubMed]
- Abate, F.; Ambrosio, M.R.; Mundo, L.; Laginestra, M.A.; Fulingni, F.; Rossi, M.; Zairis, S.; Gazaneo, S.; De Falco, G.; Lazzi, S.; et al. Distinct viral and mutational spectrum of endemic Burkitt lymphoma. PLoS Pathog. 2015, 11, e1005158. [Google Scholar] [CrossRef]
- De Thè, G. Is Burkitt’s lymphoma related to perinatal infection by Epstein-Barr virus? Lancet 1977, 309, 335–338. [Google Scholar] [CrossRef]
- Satou, A.; Asano, N.; Nakazawa, A.; Osumi, T.; Tsurusawa, M.; Ishiguro, A.; Elsayed, A.A.; Nakamura, N.; Ohshima, K.; Kinoshita, T.; et al. Epstein-Barr virus (EBV)-positive sporadic Burkitt lymphoma: And age-related lymphoproliferative disorder? Am. J. Surg. Pathol. 2015, 39, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Mbulaiteye, S.M.; Anderson, W.F.; Ferlay, J.; Bhatia, K.; Chang, C.; Rosenberg, P.S.; Devesa, S.S.; Parkin, D.M. Pediatric, elderly and emerging adult-onset peaks in Burkitt’s lymphoma incidence diagnosed in four continents, excluding Africa. Am. J. Hematol. 2012, 87, 573–578. [Google Scholar] [CrossRef]
- Gibson, T.M.; Morton, L.M.; Shiels, M.S.; Clarke, C.A.; Engels, E.A. Risk of non-Hodgkin lymphoma subtypes in HIV-infected people during the HAART era: A population-based study. AIDS 2014, 28, 2313–2318. [Google Scholar] [CrossRef]
- Molyneux, E.M.; Rochford, R.; Griffin, B.; Newton, R.; Jackson, G.; Menon, G.; Harrison, C.J.; Israels, T.; Bailey, S. Burkitt’s lymphoma. Lancet 2012, 379, 1234–1244. [Google Scholar] [CrossRef]
- England, R.J.; Oillay, K.; Davidson, A.; Numanoglu, A.; Millar, A.J. Intussusception as a presenting feature of Burkitt lymphoma: Implications for management and outcome. Pediatr. Surg. Int. 2012, 28, 267–270. [Google Scholar] [CrossRef] [PubMed]
- Rowe, M.; Kelly, G.L.; Bell, A.I.; Rickinson, A.B. Burkitt’s lymphoma: The Rosetta stone deciphering Epstein-Barr virus biology. Sem. Cancer Biol. 2009, 19, 377–388. [Google Scholar] [CrossRef]
- Allday, M.J. How does Epstein-Barr virus (EBV) complement the activation of MYC in the pathogenesis of Burkitt’s lymphoma? Semin. Cancer Biol. 2009, 19, 366–376. [Google Scholar] [CrossRef]
- Duleavy, K.; Little, R.F.; Wilson, W.H. Update on Burkitt lymphoma. Hematol. Oncol. Clin. N. Am. 2016, 30, 1333–1343. [Google Scholar] [CrossRef]
- Zanelli, M.; Sanguedolce, F.; Palicelli, A.; Zizzo, M.; Martino, G.; Caprera, C.; Fragliasso, V.; Soriano, A.; Valle, L.; Ricci, S.; et al. EBV-driven lymphoproliferative disorders and lymphomas of the gastrointestinal tract: A spectrum of entities with a common denominator (Part 1). Cancers 2021, 13, 4578. [Google Scholar] [CrossRef]
- Zanelli, M.; Sanguedolce, F.; Palicelli, A.; Zizzo, M.; Martino, G.; Caprera, C.; Fragliasso, V.; Soriano, A.; Valle, L.; Ricci, S.; et al. EBV-driven lymphoproliferative disorders and lymphomas of the gastrointestinal tract: A spectrum of entities with a common denominator (Part 2). Cancers 2021, 13, 4527. [Google Scholar] [CrossRef]
- Straus, S.E. The chronic mononucleosis syndrome. J. Infect. Dis. 1988, 157, 405–412. [Google Scholar] [CrossRef]
- Jones, J.; Shurin, S.; Abramowsky, C.; Tubbs, R.R.; Sciotto, C.G.; Wahl, R.; Sands, J.; Gottman, D.; Katz, B.Z.; Sklar, J. T-cell lymphomas containing Epstein-Barr viral DNA in patients with chronic Epstein-Barr virus infections. N. Engl. J. Med. 1988, 318, 733–741. [Google Scholar] [CrossRef]
- Okano, M.; Kawa, K.; Kimura, H.; Yachie, A.; Wakiguchi, H.; Maeda, A.; Imai, S.; Ohga, S.; Kanegane, H.; Tsuchiya, S.; et al. Proposed guidelines for diagnosing chronic active Epstein-Barr virus infection. Am. J. Hematol. 2005, 80, 64–69. [Google Scholar] [CrossRef]
- Cohen, J.I.; Jaffe, E.S.; Dale, J.K.; Pittaluga, S.; Heslop, H.E.; Rooney, C.M.; Gottschalk, S.; Bollard, C.M.; Rao, V.K.; Marques, A.; et al. Characterization and treatment of chronic active Epstein-Barr virus disease: A 28-year experience in the United States. Blood 2011, 117, 5835–5849. [Google Scholar] [CrossRef]
- Arai, A.; Imadome, K.; Watanabe, Y.; Yoshimori, M.; Koyama, T.; Kawaguchi, T.; Nakaseko, C.; Fujiwara, S.; Miura, O. Clinical features of adult-onset chronic active Epstein-Barr virus infection: A retrospective analysis. Int. J. Hematol. 2011, 93, 602–609. [Google Scholar] [CrossRef] [PubMed]
- Kimura, H.; Hoshino, Y.; Hara, S.; Sugaya, N.; Kawada, J.; Shibata, Y.; Kojima, S.; Nagasaka, T.; Kuzushima, K.; Morishima, T. Differences between T-cell type and natural killer cell-type chronic active Epstein-Barr virus infection. J. Infect. Dis. 2005, 191, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Kimura, H.; Morishima, T.; Kanegane, H.; Ohga, S.; Hoshino, Y.; Maeda, A.; Imai, S.; Okano, M.; Morio, T.; Yokota, S.; et al. Prognostic factors for chronic active Epstein-Barr virus infection. J. Infect. Dis. 2003, 187, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Isobe, Y.; Aritaka, N.; Setoguchi, Y.; Ito, K.; Kimura, H.; Hamano, Y.; Sugimoto, K.; Komatsu, N. T/NK cell type chronic active Epstein-Barr virus disease in adults: An underlying condition for Epstein-Barr virus-associated T/NK-cell lymphoma. J. Clin. Pathol. 2012, 65, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Roth, D.E.; Jones, A.; Smith, L.; Lai, R.; Preiksaitis, J.; Robinson, J. Severe chronic active Epstein-Barr virus infection mimicking steroid-dependent inflammatory bowel disease. Pediatr. Infect. Dis. J. 2005, 24, 261–264. [Google Scholar] [CrossRef]
- Liu, R.; Wang, M.; Zhang, L.; Zhou, W.; Huang, Y.; Guo, H.; Gu, Y.; Chen, Y.; Li, Y.; Chen, C.; et al. The clinicopathologic features of chronic active Epstein-Barr virus infective enteritis. Mod. Pathol. 2019, 32, 387–395. [Google Scholar] [CrossRef]
- Xu, W.; Jiang, X.; Chen, J.; Mao, Q.; Zhao, X.; Sun, X.; Zhong, L.; Rong, L. Chronic active Epstein-Barr virus infection involving gastrointestinal tract mimicking inflammatory bowel disease. BMC Gastroenterol. 2020, 20, 257. [Google Scholar] [CrossRef] [PubMed]
- Tian, S.; Westbrook, L.M.; Xiao, S.Y.; Zhang, Y.; Huang, Y.; Wang, H.L. The morphologic features of primary Epstein-Barr virus infection in the gastrointestinal tract. An approach to correct diagnosis. Am. J. Surg. Pathol. 2019, 43, 1253–1263. [Google Scholar] [CrossRef]
- Kimura, H.; Ito, Y.; Kawabe, S.; Gotoh, K.; Takahashi, Y.; Kojima, S.; Naoe, T.; Esaki, S.; Kikuta, A.; Sawada, A.; et al. EBV-associated T/NK-cell lymphoproliferative diseases in nonimmunocompromised hosts: Prospective analysis of 108 cases. Blood 2012, 119, 673–686. [Google Scholar] [CrossRef] [PubMed]
- Ohshima, K.; Kimura, H.; Yoshino, T.; Kim, C.W.; Ko, H.Y.; Lee, S.S.; Peh, S.C.; Chan, J.K.C. Proposed categorization of pathological states of EBV-associated T/natural killer-cell lymphoproliferative disorder (LPD) in children and young adults: Overlap chronic active EBV infection and infantile fulminant EBV T-LPD. Pathol. Int. 2008, 58, 209–217. [Google Scholar] [CrossRef]
- Kawa, K.; Sawada, A.; Sato, M.; Okamura, T.; Sakata, N.; Kondo, O.; Kimoto, T.; Yamada, K.; Tokimasa, S.; Yasui, M.; et al. Excellent outcome of allogenic hematopoietic SCT with reduced-intensity conditioning for the treatment of chronic active EBV infection. Bone Marrow Transplant. 2011, 46, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Arai, A. Advances in the study of chronic active Epstein-Barr virus infection: Clinical features under the 2016 WHO classification and mechanisms of development. Front. Pediatr. 2019, 7, 14. [Google Scholar] [CrossRef]
- Fujiwara, S.; Nakamura, H. Chronic active Epstein-Barr virus infection: Is it immunodeficiency, malignancy or both? Cancers 2020, 12, 3202. [Google Scholar] [CrossRef]
- Sanchez-Romero, C.; Bogna-Molina, R.; Paes de Almeda, O.; Santos-Silva, A.; Prado-Ribeiro, A.C.; Brandao, T.B.; Carlos, R. Extranodal NK/T cell lymphoma, nasal type: An updated overview. Crit. Rev. Oncol. Hematol. 2021, 159, 103237. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; De Leval, L.; Gaulard, P. Molecular underpinning of extranodal NK-T-cell lymphoma. Best. Pract. Res. Clin. Haematol. 2013, 26, 57–74. [Google Scholar] [CrossRef]
- Takada, H.; Imadome, K.I.; Shibayama, H.; Yoshimori, M.; Wang, L.; Saitoh, Y.; Uota, S.; Yamaoka, S.; Koyama, T.; Shimizu, N.; et al. EBV induces persistent NF-kB activation and contributes to survival of EBV-positive neoplastic T-or NK-cells. PLoS ONE 2017, 12, e0174136. [Google Scholar]
- Huang, Y.; De Reynies, A.; De Leval, L.; Ghazi, B.; Martin-Garcia, N.; Travert, M.; Bosq, J.; Briere, J.; Petit, B.; Thomas, E.; et al. Gene expression profiling identified emerging oncogenic pathways operating in extranodal NK/T-cell lymphoma, nasal type. Blood 2010, 115, 1226–1237. [Google Scholar] [CrossRef]
- Lee, S.; Park, H.Y.; Kang, S.Y.; Kim, S.J.; Hwang, J.; Lee, S.; Kwak, S.H.; Park, K.S.; Yoo, H.Y.; Kim, W.S.; et al. Genetic alterations of JAK/STAT cascade and histone modification in extranodal NK/T-cell lymphoma nasal type. Oncotarget 2015, 6, 17764–17776. [Google Scholar] [CrossRef]
- Jiang, L.; Gu, Z.H.; Yan, Z.Y.; Zhao, X.; Xie, Y.Y.; Zhang, Z.G.; Pan, C.M.; Hu, Y.; Cai, C.P.; Dong, Y.; et al. Exome sequencing identifies somatic mutations of DDX3X in natural killer/T-cell lymphoma. Nat. Genet. 2015, 47, 1061–1066. [Google Scholar] [CrossRef] [PubMed]
- Takata, K.; Hong, M.E.; Sitthinamsuwan, P.; Loong, F.; Tan, S.Y.; Liau, J.Y.; Hsieh, P.P.; Ng, S.B.; Yang, S.F.; Pongpruttipan, T.; et al. Primary cutaneous NK/T-cell lymphoma, nasal type and CD56-positive peripheral T-cell lymphoma: A cellular lineage and clinicopathologic study of 60 patients from Asia. Am. J. Surg. Pathol. 2015, 39, 1–12. [Google Scholar] [CrossRef]
- Chim, C.S.; Au, W.Y.; Shek, T.W.; Ho, Y.; Choy, C.; Ma, S.K.; Tung, H.M.; Liang, R.; Kwong, Y.L. CD56 positive lymphomas of the gastrointestinal tract. Cancer 2001, 91, 525–533. [Google Scholar] [CrossRef]
- Kim, S.J.; Jung, H.A.; Chuang, S.S.; Hong, H.; Guo, C.C.; Cao, J.; Hong, X.N.; Suzuki, R.; Kang, H.J.; Won, J.H.; et al. Extranodal natural killer/T-cell lymphoma involving the gastrointestinal tract: Analysis of clinical features and outcomes from the Asia Lymphoma Study Group. J. Hematol. Oncol. 2013, 16, 86. [Google Scholar] [CrossRef]
- Hue, S.S.-S.; Oon, M.L.; Wang, S.; Tan, S.Y.; Ng, S.B. Epstein-Barr virus associated T-and NK-cell lymphoproliferative diseases: An update and diagnostic approach. Pathology 2020, 52, 111–127. [Google Scholar] [CrossRef] [PubMed]
- Chim, C.S.; Ma, E.S.; Loong, F.; Kwong, Y.L. Diagnostic clues for natural killer lymphoma: Primary nodal presentation and the role of in situ hybridization for Epstein-Barr virus encoded early small RNA in detecting occult bone marrow involvement. J. Clin. Pathol. 2005, 58, 443–445. [Google Scholar] [CrossRef]
- Yu, B.H.; Shui, R.H.; Sheng, W.Q.; Wang, C.F.; Lu, H.F.; Zhou, X.Y.; Zhu, X.Z.; Li, X.Q. Primary intestinal extranodal natural killer/T-cell lymphoma, nasal type: A comprehensive clinicopathological analysis of 55 cases. PLoS ONE 2016, 11, e0161831. [Google Scholar] [CrossRef]
- Susan, S.H.; Ng, S.B.; Wang, S.; Tan, S.Y. Diagnostic approach to T- and NK-cell lymphoproliferative disorders in the gastrointestinal tract. Semin. Diagn. Pathol. 2021, 38, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Zhao, W.L. Advances in multiple omics of natural-killer/T-cell lymphoma. J. Hematol. Oncol. 2018, 11, 134. [Google Scholar] [CrossRef]
- McKelvie, P.A.; Climent, F.; Krings, G.; Hasserjian, R.P.; Abramson, J.S.; Pilch, B.Z.; Lee Harris, N.; Ferry, J.A.; Zukenberg, L.R.; Sohani, A.R. Small-cell predominant extranodal NK/T cell lymphoma, nasal type: Clinicopathological analysis of a series of cases diagnosed in a western population. Histopathology 2016, 69, 667–679. [Google Scholar] [CrossRef]
- Zanelli, M.; Ragazzi, M.; Fiorino, S.; Foroni, M.; Cecinato, P.; Del Mar Jordana Sanchez, M.; Ascani, S.; De Marco, L. An italian case of intestinal anisakiasis with a presurgical diagnosis: Could this parasite represent an emerging disease? Pathol. Res. Pract. 2017, 213, 558–564. [Google Scholar] [CrossRef]
- Melani, C.; Jaffe, E.S.; Wilson, W.H. Pathobiology and treatment of lymphomatoid granulomatosis, a rare EBV-driven disorder. Blood 2020, 135, 1344–1352. [Google Scholar] [CrossRef]
- Sanguedolce, F.; Zanelli, M.; Zizzo, M.; Bisagni, A.; Soriano, A.; Cocco, G.; Palicelli, A.; Santandrea, G.; Caprera, C.; Corsi, M.; et al. Primary pulmonary B-cell lymphoma: A review and update. Cancers 2021, 13, 415. [Google Scholar] [CrossRef]
- Van Vliet, C.; Spagnolo, D.V. T- and NK-cell lymphoproliferative disorders of the gastrointestinal tract: Review and update. Pathology 2020, 52, 128–141. [Google Scholar] [CrossRef] [PubMed]
- Sanguedolce, F.; Zanelli, M.; Zizzo, M.; Luminari, S.; Martino, G.; Soriano, A.; Ricci, L.; Caprera, C.; Ascani, S. Indolent T-cell lymphoproliferative disorders of gastrointestinal tract (iTLPD-GI): A review. Cancers 2021, 13, 2790. [Google Scholar] [CrossRef]
- Kwong, Y.-L.; Chan, T.S.Y.; Tan, D.; Kim, S.J.; Poon, L.-M.; Mow, B.; Khong, P.-L.; Loong, F.; Au-Yeung, R.; Iqbal, J.; et al. PD1 blockade with pembrolizumab is highly effective in relapsed or refractory NK/T-cell lymphoma failing l-asparaginase. Blood 2017, 129, 2437–2442. [Google Scholar] [CrossRef]
- Hari, P.; Raj, R.V.; Olteanu, H. Targeting CD38 in refractory extranodal natural killer cell-T-cell lymphoma. N. Engl. J. Med. 2016, 375, 1501–1502. [Google Scholar] [CrossRef] [PubMed]
- De Mel, S.; Hue, S.S.S.; Jeyasekharan, A.D.; Chng, W.J.; Ng, S.B. Molecular pathogenetic pathways in extranodal NK/T cell lymphoma. J. Hematol. Oncol. 2019, 12, 33. [Google Scholar] [CrossRef]
- Gupta, D.; Mendonca, S.; Chakraborty, S.; Chatterjee, T. Post-transplant lymphoproliferative disorder. Indian J. Hemato. Blood Transfus. 2020, 36, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Al-Mansour, Z.; Nelson, B.P.; Evens, A.M. Post-transplant lymphoproliferative disease (PTLD): Risk factors, diagnosis and current treatment strategies. Curr. Hematol. Malig. Rep. 2013, 8, 173–183. [Google Scholar] [CrossRef]
- Abbas, F.; El Kossi, M.; Shaheen, I.S.; Sharma, A.; Halawa, A. Post-transplantation lymphoproliferative disorders: Current concepts and future therapeutic approaches. World J. Transplant. 2020, 10, 29–46. [Google Scholar] [CrossRef] [PubMed]
- Parker, A.; Bowles, K.; Bradley, A.; Emery, V.; Featherstone, C.; Gupte, G.; Marcus, R.; Parameshwar, J.; Ramsay, A.; Newstead, C. Diagnosis of post-transplant lymphoproliferative disorder in solid organ transplant recipients-BCSH and BTS Guidelines. Br. J. Haematol. 2010, 149, 675–692. [Google Scholar] [CrossRef] [PubMed]
- Dolcetti, R. B lymphocytes and Epstein-Barr virus: The lesson of post-transplant lymphoproliferative disorders. Autoimmun. Rev. 2007, 7, 96–101. [Google Scholar] [CrossRef]
- Fujimoto, A.; Suzuki, R. Epstein-Barr virus-associated post-transplant lymphoproliferative disorders after hematopoietic stem cell transplantation: Pathogenesis, risk factors and clinical outcomes. Cancers 2020, 12, 328. [Google Scholar] [CrossRef] [PubMed]
- Nelson, B.P.; Nalesnik, M.A.; Bahler, D.W.; Locker, J.; Fung, J.J.; Swerdlow, S.H. Epstein-Barr virus-negative post-transplant lymphoproliferative disorders: A distinct entity? Am. J. Surg. Pathol. 2000, 24, 375–385. [Google Scholar] [CrossRef]
- Ferla, V.; Rossi, F.G.; Goldaniga, M.C.; Baldini, L. Biological difference between Epstein-Barr virus positive and negative post-transplant lymphoproliferative disorders and their clinical impact. Front. Oncol. 2020, 10, 506. [Google Scholar] [CrossRef] [PubMed]
- Menter, T.; Juskevicius, D.; Alikian, M.; Steiger, J.; Dirnhofer, S.; Tzankov, A.; Naresh, K.N. Mutational landscape of B-cell post-transplant lymphoproliferative disorders. Br. J. Hematol. 2017, 178, 48–56. [Google Scholar] [CrossRef]
- Opelz, G.; Dohler, B. Lymphomas after solid organ transplantation: A collaborative transplant study report. Am. J. Transplant. 2004, 4, 222–230. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, J.A.; Cogley, C.; Burton, M.; Lancaster-Weiss, K.; Cordle, R.A. Posttransplantation lymphoproliferative disorder: Endoscopic findings. J. Pediatr. Gastroenterol. Nutr. 2000, 31, 458–461. [Google Scholar] [CrossRef]
- Cruz, R.J.; Ramachandra, S.; Sasatomi, E.; Di Martini, A.; de Vera, M.; Fontes, P.; Hughes, C.; Humar, A. Surgical management of gastrointestinal posttransplant lymphoproliferative disorders in liver transplant recipients. Transplantation 2012, 94, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Gibson, S.E.; Swerdlow, S.H.; Graing, F.E.; Surti, U.; Cook, J.R.; Nalesnik, M.A.; Lowe, C.; Wood, K.M.; Bacon, C.M. EBV-positive extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue in the posttransplant setting: A distinct type of posttransplant lymphoproliferative disorder? Am. J. Surg. Pathol. 2011, 35, 807–815. [Google Scholar] [CrossRef] [PubMed]
- Djokic, M.; Le Beau, M.M.; Swinnen, L.J.; Smith, S.M.; Rubin, C.M.; Anastasi, J.; Carlson, K.M. Post-transplant lymphoproliferative disorder subtypes correlate with different recurring chromosomal abnormalities. Genes 2006, 45, 313–318. [Google Scholar] [CrossRef]
- Pitman, S.D.; Huang, Q.; Zuppan, C.W.; Rowsell, E.H.; Cao, J.D.; Berdeja, J.G.; Weiss, L.M.; Wang, J. Hodgkin lymphoma-like postratnsplant lymphoproliferative disorder (HL-like PTLD) simulates monomorphic B-cell PTLD both clinically and pathologically. Am. J. Surg. Pathol. 2006, 30, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Soriano-Lopez, D.P.; Alcantar-Fierros, J.M.; Hernandez-Plata, J.A.; Gonzalez-Jorge, A.L.; Velazquez-Ramos, S.; Flores-Hernandez, M.A.; Fuentes, V.; Castaneda, P.; Nieto, J.; Sanchez, J.L.; et al. A scheduled program of molecular screening for Epstein-Barr virus decreases the incidence of post-transplantation lymphoproliferative diseases in pediatric liver transplantation. Transpl. Proc. 2016, 48, 654–657. [Google Scholar] [CrossRef] [PubMed]
- Nelson, B.P.; Wolniak, K.L.; Evens, A.; Chenn, A.; Maddalozzo, J.; Proytcheva, M. Early posttransplant lymphoproliferative disease: Clinicopathologic features and correlation with mTOR signaling pathway activation. Am. J. Clin. Pathol. 2012, 138, 568–578. [Google Scholar] [CrossRef]
- Reshef, R.; Vardhanabhuti, S.; Luskin, M.R.; Heitjan, D.F.; Hadjiliadis, D.; Goral, S.; Krok, K.L.; Goldberg, L.R.; Porter, D.L.; Stadtmauer, E.A.; et al. Reduction of immunosuppression as initial therapy for posttransplantation lymphoproliferative disorder. Am. J. Transplant. 2011, 11, 336–347. [Google Scholar] [CrossRef]
- Choquet, S.; Leblond, V.; Herbrecht, R.; Socié, G.; Stoppa, A.-M.; Vandenberghe, P.; Fischer, A.; Morschhauser, F.; Salles, G.; Feremans, W.; et al. Efficacy and safety of rituximab in B-cell post-transplantation lymphoproliferative disorders: Results of a prospective multicenter phase 2 study. Blood 2006, 107, 3053–3057. [Google Scholar] [CrossRef]
- Trappe, R.U.; Dierickx, D.; Zimmermann, H.; Morschhauser, F.; Mollee, P.; Zaucha, J.M.; Dreyling, M.H.; Duhrsen, U.; Reinke, P.; Verhoef, G.; et al. Response to Rituximab induction is a predictive marker in B-cell post-transplant lymphoproliferative disorder and allows successful stratification into Rituximab or R-CHOP consolidation in an International, prospective, multicenter phase II trial. J. Clin. Oncol. 2017, 35, 536–543. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, J.; Othman, J.; Heldman, M.R.; Slavin, M.A. Epstein-Barr virus posttransplant lymphoproliferative disorder: Update on management and outcomes. Curr. Opin. Infect. Dis. 2021, 34, 635–645. [Google Scholar] [CrossRef] [PubMed]
- Doubrovina, E.; Oflaz-Sozmen, B.; Prockop, S.E.; Kernan, N.A.; Abramson, S.; Teruya-Feldstein, J.; Hedvat, C.; Chou, J.F.; Heller, G.; Barker, J.N.; et al. Adoptive immunotherapy with unselected or EBV-specific T cells for biopsy-proven EBV+ lymphomas after allogenic hematopoietic cell transplantation. Blood 2012, 119, 2644–2656. [Google Scholar] [CrossRef] [PubMed]
- De Pasquale, M.D.; Mastronuzzi, A.; De Vito, R.; Cometa, A.; Inserra, A.; Russo, C.; De Ioris, M.A.; Locatelli, F. Unmanipulated donor lymphocytes for EBV-related PTLD after T-cell depleted HLA-haploidentical transplantation. Pediatrics 2012, 129, e189–e194. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Xu, L.; Zhang, Y.; Huang, F.; Liu, D.; Sun, J.; Song, C.; Liang, X.; Fan, Z.; Zhou, H.; et al. Rituximab-based treatments followed by adoptive cellular immunotherapy for biopsy-proven EBV-associated post-transplant lymphoproliferative disease in recipients of allogeneic hematopoietic stem cell transplantation. Oncoimmunology 2016, 10, e1139274. [Google Scholar] [CrossRef][Green Version]
- Prockop, S.; Doubrovina, E.; Suser, S.; Heller, G.; Barker, J.; Dahi, P.; Perales, M.A.; Papadopoulos, E.; Sauter, C.; Castro-Malaspina, H.; et al. Off-the-shelf EBV-specific T cell immunotherapy for rituximab-refractory EBV-associated lymphoma following transplantation. J. Clin. Investig. 2020, 130, 733–747. [Google Scholar] [CrossRef] [PubMed]
| Variation | ENKTL-NT | CAEBV | EATL | MEITL | ITLPD |
|---|---|---|---|---|---|
| Sites of GIT (in order of frequency) | Small bowel Large bowel Stomach Esophagus | Large bowel Small bowel Stomach | Small bowel; Large bowel Stomach | Small bowel; large bowel; stomach | All sites of GIT; Small bowel or large bowel (more often) |
| Macroscopic features | Mucosal ulcer or ulcerating mass | Ulcer | Ulcerating lesion or stricture | Tumor mass | Subtle features: hyperaemic mucosa; nodularity; Prominent folds; polyps |
| Coeliac disease | No | No | Yes | No | No |
| Histology | Cells of variable size; Admixed inflammation; Necrosis; Angioinvasive/angiocentric pattern | Infiltrate within mucosa, rarely submucosa or muscle layer involvement; Small/medium-sized cells often with mild atypia | Medium/ large- sized cells; Admixed inflammation; Necrosis; Angioinvasive/ angiocentric pattern | Monomorphic Medium- Sized cells; Epitheliotropism (often) | Non-destructive mucosal infiltrate (rarely muscolaris mucosae or submucosa involved) |
| Cell of origin | NK-cell often; T-cell | T-cell (59%); NK-cell (41%); B-cell rarely | T-cell | T-cell | T-cell |
| IHC | NK cell origin: CD2+ cCD3+ CD56- cytotoxic molecules+ CD7+/− CD30+/− sCD3−, CD4− CD8− CD5− CD16− CD57− MATK+. T-cell origin: sCD3+ CD5+ CD8+ MATK+ | T-cell origin: CD4 > CD8 | CD3+ CD7+ CD103+ CD5− CD4− CD8− often cytotoxic molecules+ CD30+ (often) TCRB+ (in some cases) TCRG+ (in some cases) | CD3+ CD8+ CD56+ CD5− TCRG+ (often) TIA1+ CD20 aberrant+ (20% of cases) MATK+ | CD3+ CD8+ often; CD4+ some cases; CD4− CD8− rarely; CD2+ CD5+ CD7+/− TIA1+ Granzyme B− TCR alfa beta+ CD56- |
| EBER-ISH | Positive | Positive | Negative | Negative | Negative |
| Proliferative fraction | High | Low | High | High | Low |
| T-cell clonality | T-cell clonality in cases of T-cell origin | T-cell clonality; more rarely oligoclonality or polyclonality | T-cell clonality | T-cell clonality | |
| Clinical course | Aggressive | Variable (NK forms: more favorable course) | Aggressive | Aggressive | Indolent |
| WHO Classification | EBV Association | Time of Post-Transplant Onset | Clonality |
|---|---|---|---|
| Non-destructive PTLD | Often EBV-positive | Often early | Often polyclonal (oligoclonality may be present) |
| Polymorphic PTLD | Often EBV-positive | Often early | Often monoclonal |
| Monomorphic PTLD (B-cell origin) | EBV-positive and EBV-negative | Both early and late | B-cell clonality present; sometimes T-cell clonality |
| Monomorphic PTLD (T/NK-cell origin) | T-cell origin: often EBV negative; NK-cell origin: often EBV-positive | Often late | T-cell clonality in PTLDs of T-cell origin |
| cHL-PTLD | Often EBV-positive | Often late | Clonality rarely detected |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zanelli, M.; Sanguedolce, F.; Palicelli, A.; Zizzo, M.; Martino, G.; Caprera, C.; Fragliasso, V.; Soriano, A.; Gozzi, F.; Cimino, L.; et al. EBV-Driven Lymphoproliferative Disorders and Lymphomas of the Gastrointestinal Tract: A Spectrum of Entities with a Common Denominator (Part 3). Cancers 2021, 13, 6021. https://doi.org/10.3390/cancers13236021
Zanelli M, Sanguedolce F, Palicelli A, Zizzo M, Martino G, Caprera C, Fragliasso V, Soriano A, Gozzi F, Cimino L, et al. EBV-Driven Lymphoproliferative Disorders and Lymphomas of the Gastrointestinal Tract: A Spectrum of Entities with a Common Denominator (Part 3). Cancers. 2021; 13(23):6021. https://doi.org/10.3390/cancers13236021
Chicago/Turabian StyleZanelli, Magda, Francesca Sanguedolce, Andrea Palicelli, Maurizio Zizzo, Giovanni Martino, Cecilia Caprera, Valentina Fragliasso, Alessandra Soriano, Fabrizio Gozzi, Luca Cimino, and et al. 2021. "EBV-Driven Lymphoproliferative Disorders and Lymphomas of the Gastrointestinal Tract: A Spectrum of Entities with a Common Denominator (Part 3)" Cancers 13, no. 23: 6021. https://doi.org/10.3390/cancers13236021
APA StyleZanelli, M., Sanguedolce, F., Palicelli, A., Zizzo, M., Martino, G., Caprera, C., Fragliasso, V., Soriano, A., Gozzi, F., Cimino, L., Masia, F., Moretti, M., Foroni, M., De Marco, L., Pellegrini, D., De Raeve, H., Ricci, S., Tamagnini, I., Tafuni, A., ... Ascani, S. (2021). EBV-Driven Lymphoproliferative Disorders and Lymphomas of the Gastrointestinal Tract: A Spectrum of Entities with a Common Denominator (Part 3). Cancers, 13(23), 6021. https://doi.org/10.3390/cancers13236021









