Association of High-Intensity Exercise with Renal Medullary Carcinoma in Individuals with Sickle Cell Trait: Clinical Observations and Experimental Animal Studies
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
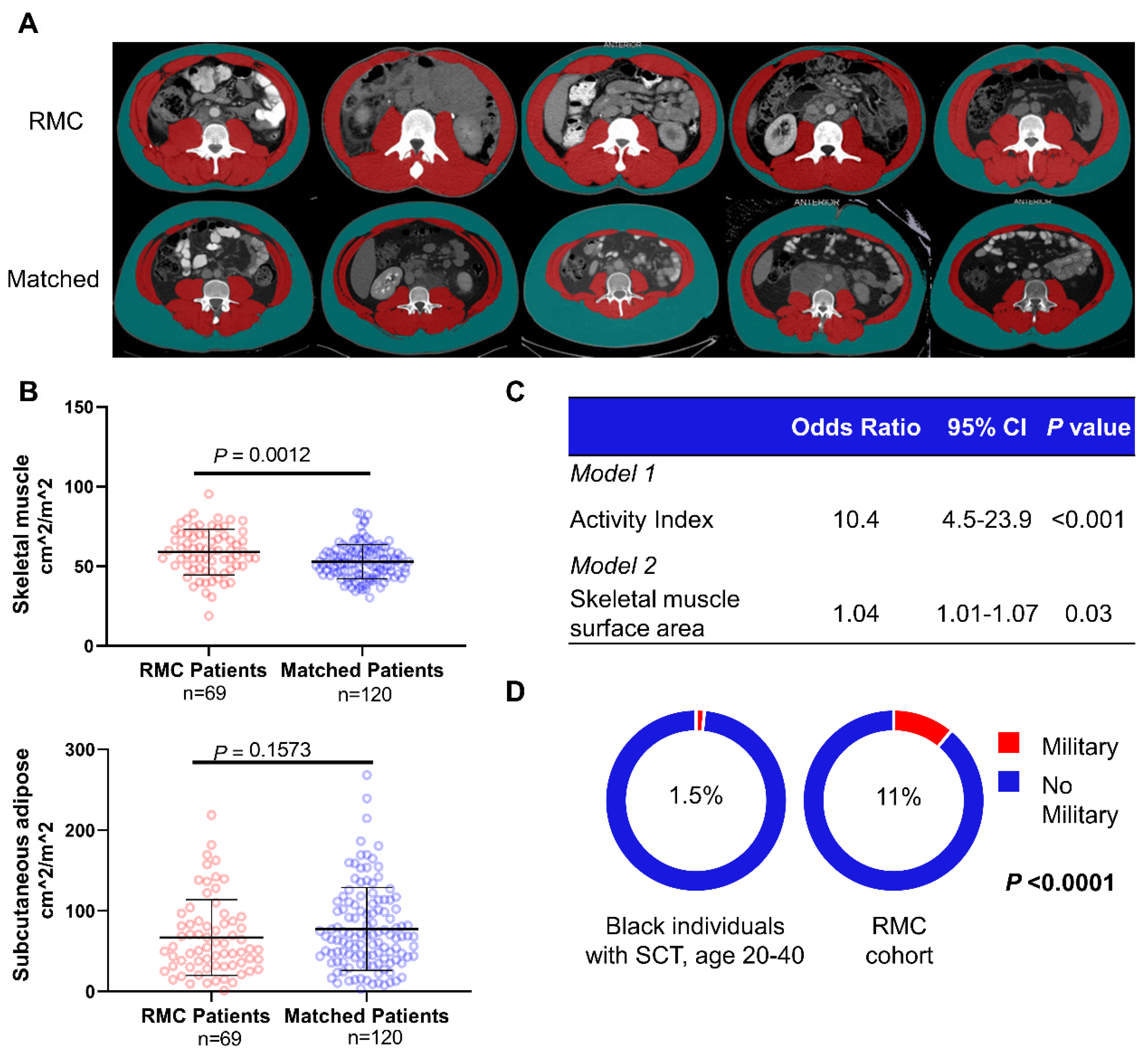
2.2. Anthropometric Analysis
2.3. Epidemiologic Comparison
2.4. Prospective Exercise Evaluation
2.5. Mouse Models
2.6. Statistical Analysis
3. Results
3.1. Retrospective and Prospective Evaluation of Physical Activity
3.2. Sensitivity Analysis
3.3. Comparison of Populations with and without SCT
3.4. Mouse Models of Renal Medullary Hypoxia
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Davis, C.J.; Mostofi, F.K.; Sesterhenn, I.A. Renal medullary carcinoma–The 7th sickle-cell nephropathy. Am. J. Surg. Pathol. 1995, 19, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Msaouel, P.; Hong, A.L.; Mullen, E.A.; Atkins, M.B.; Walker, C.L.; Lee, C.-H.; Carden, M.A.; Genovese, G.; Linehan, W.M.; Rao, P.; et al. Updated Recommendations on the Diagnosis, Management, and Clinical Trial Eligibility Criteria for Patients with Renal Medullary Carcinoma. Clin. Genitourin. Cancer 2019, 17, 1–6. [Google Scholar] [CrossRef]
- Msaouel, P.; Tannir, N.M.; Walker, C.L. A Model Linking Sickle Cell Hemoglobinopathies and SMARCB1 Loss in Renal Medullary Carcinoma. Clin. Cancer Res. 2018, 24, 2044–2049. [Google Scholar] [CrossRef] [Green Version]
- Grant, A.M.; Parker, C.S.; Jordan, L.B.; Hulihan, M.M.; Creary, M.S.; Lloyd-Puryear, M.A.; Goldsmith, J.C.; Atrash, H.K. Public health implications of sickle cell trait: A report of the CDC meeting. Am. J. Prev. Med. 2011, 41, S435–S439. [Google Scholar] [CrossRef]
- Alvarez, O.; Rodriguez, M.M.; Jordan, L.; Sarnaik, S. Renal medullary carcinoma and sickle cell trait: A systematic review. Pediatr. Blood Cancer 2015, 62, 1694–1699. [Google Scholar] [CrossRef]
- Zoumpourlis, P.; Genovese, G.; Tannir, N.M.; Msaouel, P. Systemic Therapies for the Management of Non–Clear Cell Renal Cell Carcinoma: What Works, What Doesn’t, and What the Future Holds. Clin. Genitourin. Cancer 2021, 19, 103–116. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.Y.; Karam, J.A.; Malouf, G.; Rao, P.; Lim, Z.D.; Jonasch, E.; Xiao, L.; Gao, J.; Vaishampayan, U.; Heng, D.Y.; et al. Management and outcomes of patients with renal medullary carcinoma: A multicentre collaborative study. BJU Int. 2016, 120, 782–792. [Google Scholar] [CrossRef] [Green Version]
- Berman, L.B. Sickle cell nephropathy. JAMA 1974, 228, 1279. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.Z.; Thein, S.L. The carrier state for sickle cell disease is not completely harmless. Haematology 2019, 104, 1106–1111. [Google Scholar] [CrossRef] [PubMed]
- Liem, R.I. Balancing exercise risk and benefits: Lessons learned from sickle cell trait and sickle cell anemia. Hematol. Am. Soc. Hematol. Educ. Program 2018, 2018, 418–425. [Google Scholar] [CrossRef] [Green Version]
- Strath, S.J.; Kaminsky, L.A.; Ainsworth, B.E.; Ekelund, U.; Freedson, P.S.; Gary, R.A.; Richardson, C.R.; Smith, D.T.; Swartz, A.M. Guide to the assessment of physical activity: Clinical and research applications: A scientific statement from the american heart association. Circulation 2013, 128, 2259–2279. [Google Scholar] [CrossRef]
- Peterson, S.J.; Mozer, M. Differentiating Sarcopenia and Cachexia Among Patients with Cancer. Nutr. Clin. Pract. 2017, 32, 30–39. [Google Scholar] [CrossRef]
- Chéry, L.; Borregales, L.D.; Fellman, B.; Urbauer, D.L.; Garg, N.; Parker, N.; Katz, M.H.; Wood, C.G.; Karam, J.A. The Effects of Neoadjuvant Axitinib on Anthropometric Parameters in Patients with Locally Advanced Non-metastatic Renal Cell Carcinoma. Urology 2017, 108, 114–121. [Google Scholar] [CrossRef] [PubMed]
- U.S. Census Bureau. Race. 2018. Available online: https://data.Census.Gov/cedsci/table?Q=race&tid=acsdt1y2018.B02001&hidepreview=false (accessed on 21 March 2021).
- Department of Defense. 2018 Demographics Report: Profile of the Military Community. 2018. Available online: https://download.Militaryonesource.Mil/12038/mos/reports/2018-demographics-report.Pdf (accessed on 21 March 2021).
- MacInnis, M.J.; Gibala, M.J. Physiological adaptations to interval training and the role of exercise intensity. J. Physiol. 2017, 595, 2915–2930. [Google Scholar] [CrossRef] [Green Version]
- Schefer, V.; Talan, M.I. Oxygen consumption in adult and aged C57BL/6J mice during acute treadmill exercise of different intensity. Exp. Gerontol. 1996, 31, 387–392. [Google Scholar] [CrossRef]
- Shapiro, D.D.; Msaouel, P. Causal Diagram Techniques for Urologic Oncology Research. Clin. Genitourin. Cancer 2021, 19, 271.e1. [Google Scholar] [CrossRef] [PubMed]
- Griffith, G.J.; Morris, T.T.; Tudball, M.J.; Herbert, A.; Mancano, G.; Pike, L.; Sharp, G.C.; Sterne, J.; Palmer, T.M.; Smith, G.D.; et al. Collider bias undermines our understanding of COVID-19 disease risk and severity. Nat. Commun. 2020, 11, 5749. [Google Scholar] [CrossRef]
- Textor, J.; van der Zander, B.; Gilthorpe, M.S.; Liśkiewicz, M.; Ellison, G.T. Robust causal inference using directed acyclic graphs: The R package ‘dagitty’. Int. J. Epidemiol. 2017, 45, 1887–1894. [Google Scholar] [CrossRef] [Green Version]
- Cinelli, C.; Hazlett, C. Making sense of sensitivity: Extending omitted variable bias. J. R. Stat. Soc. Ser. B Stat. Methodol. 2019, 82, 39–67. [Google Scholar] [CrossRef] [Green Version]
- Vanhoutte, G.; Van De Wiel, M.; Wouters, K.; Sels, M.; Bartolomeeussen, L.; De Keersmaecker, S.; Verschueren, C.; De Vroey, V.; De Wilde, A.; Smits, E.; et al. Cachexia in cancer: What is in the definition? BMJ Open Gastroenterol. 2016, 3, e000097. [Google Scholar] [CrossRef]
- Schwarz, S.; Prokopchuk, O.; Esefeld, K.; Gröschel, S.; Bachmann, J.; Lorenzen, S.; Friess, H.; Halle, M.; Martignoni, M.E. The clinical picture of cachexia: A mosaic of different parameters (experience of 503 patients). BMC Cancer 2017, 17, 130. [Google Scholar] [CrossRef] [Green Version]
- Bilir, C.; Engin, H.; Can, M.; Temi, Y.B.; Demirtas, D. The prognostic role of inflammation and hormones in patients with metastatic cancer with cachexia. Med. Oncol. 2015, 32, 32. [Google Scholar] [CrossRef] [PubMed]
- Safran, M.; Kim, W.Y.; O’Connell, F.; Flippin, L.; Gunzler, V.; Horner, J.W.; DePinho, R.A.; Kaelin, W.G. Mouse model for noninvasive imaging of HIF prolyl hydroxylase activity: Assessment of an oral agent that stimulates erythropoietin production. Proc. Natl. Acad. Sci. USA 2006, 103, 105–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chirico, E.N.; Martin, C.; Faës, C.; Féasson, L.; Oyono-Enguéllé, S.; Aufradet, E.; Dubouchaud, H.; Francina, A.; Canet-Soulas, E.; Thiriet, P.; et al. Exercise training blunts oxidative stress in sickle cell trait carriers. J. Appl. Physiol. 2012, 112, 1445–1453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aufradet, E.; Monchanin, G.; Oyonno-Engelle, S.; Feasson, L.; Messonnier, L.; Francina, A.; Bezin, L.; Serpero, L.D.; Gozal, D.; Dodogba, M.; et al. Habitual Physical Activity and Endothelial Activation in Sickle Cell Trait Carriers. Med. Sci. Sports Exerc. 2010, 42, 1987–1994. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.-T.; Kim, H.; Carrot-Zhang, J.; Zhang, Y.; Kim, W.J.; Kugener, G.; Wala, J.A.; Howard, T.P.; Chi, Y.-Y.; Beroukhim, R.; et al. Haplotype-resolved germline and somatic alterations in renal medullary carcinomas. Genome Med. 2021, 13, 114. [Google Scholar] [CrossRef]
- Calderaro, J.; Masliah-Planchon, J.; Richer, W.; Maillot, L.; Maille, P.; Mansuy, L.; Bastien, C.; de la Taille, A.; Boussion, H.; Charpy, C.; et al. Balanced Translocations Disrupting SMARCB1 Are Hallmark Recurrent Genetic Alterations in Renal Medullary Carcinomas. Eur. Urol. 2016, 69, 1055–1061. [Google Scholar] [CrossRef]
- Carlo, M.I.; Chaim, J.; Patil, S.; Kemel, Y.; Schram, A.M.; Woo, K.; Coskey, D.; Nanjangud, G.J.; Voss, M.H.; Feldman, D.R.; et al. Genomic Characterization of Renal Medullary Carcinoma and Treatment Outcomes. Clin. Genitourin. Cancer 2017, 15, e987–e994. [Google Scholar] [CrossRef]
- Hong, A.L.; Tseng, Y.-Y.; Wala, J.A.; Kim, W.-J.; Kynnap, B.D.; Doshi, M.B.; Kugener, G.; Sandoval, G.J.; Howard, T.P.; Li, J.; et al. Renal medullary carcinomas depend upon SMARCB1 loss and are sensitive to proteasome inhibition. eLife 2019, 8, e44161. [Google Scholar] [CrossRef]
- Jia, L.; Carlo, M.I.; Khan, H.; Nanjangud, G.J.; Rana, S.; Cimera, R.; Zhang, Y.; Hakimi, A.A.; Verma, A.K.; Al-Ahmadie, H.A.; et al. Distinctive mechanisms underlie the loss of SMARCB1 protein expression in renal medullary carcinoma: Morphologic and molecular analysis of 20 cases. Mod. Pathol. 2019, 32, 1329–1343. [Google Scholar] [CrossRef]
- Msaouel, P.; Walker, C.L.; Genovese, G.; Tannir, N.M. Molecular hallmarks of renal medullary carcinoma: More to c-MYC than meets the eye. Mol. Cell. Oncol. 2020, 7, 1777060. [Google Scholar] [CrossRef] [PubMed]
- Wiele, A.; Surasi, D.; Rao, P.; Sircar, K.; Su, X.; Bathala, T.; Shah, A.; Jonasch, E.; Cataldo, V.; Genovese, G.; et al. Efficacy and Safety of Bevacizumab Plus Erlotinib in Patients with Renal Medullary Carcinoma. Cancers 2021, 13, 2170. [Google Scholar] [CrossRef] [PubMed]
- Wilson, N.R.; Wiele, A.J.; Surasi, D.S.; Rao, P.; Sircar, K.; Tamboli, P.; Shah, A.Y.; Genovese, G.; Karam, J.A.; Wood, C.G.; et al. Efficacy and safety of gemcitabine plus doxorubicin in patients with renal medullary carcinoma. Clin. Genitourin. Cancer 2021. [Google Scholar] [CrossRef]
- Msaouel, P.; Malouf, G.G.; Su, X.; Yao, H.; Tripathi, D.; Soeung, M.; Gao, J.; Rao, P.; Coarfa, C.; Creighton, C.J.; et al. Comprehensive Molecular Characterization Identifies Distinct Genomic and Immune Hallmarks of Renal Medullary Carcinoma. Cancer Cell 2020, 37, 720–734.e13. [Google Scholar] [CrossRef]
- Freedman, N.D.; Silverman, D.T.; Hollenbeck, A.R.; Schatzkin, A.; Abnet, C.C. Association between smoking and risk of bladder cancer among men and women. JAMA 2011, 306, 737–745. [Google Scholar] [CrossRef]
- Cumberbatch, M.G.; Rota, M.; Catto, J.W.; La Vecchia, C. The role of tobacco smoke in bladder and kidney carcinogenesis: A comparison of exposures and meta-analysis of incidence and mortality risks. Eur. Urol. 2016, 70, 458–466. [Google Scholar] [CrossRef] [Green Version]
- Brookman-May, S.D.; Campi, R.; Henríquez, J.D.; Klatte, T.; Langenhuijsen, J.F.; Brausi, M.; Linares-Espinós, E.; Volpe, A.; Marszalek, M.; Akdogan, B.; et al. Latest Evidence on the Impact of Smoking, Sports, and Sexual Activity as Modifiable Lifestyle Risk Factors for Prostate Cancer Incidence, Recurrence, and Progression: A Systematic Review of the Literature by the European Association of Urology Section of Oncological Urology (ESOU). Eur. Urol. Focus 2019, 5, 756–787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenland, S.; Gago-Dominguez, M.; Castelao, J.E. The value of risk-factor (“Black-box”) epidemiology. Epidemiol. Camb. Mass. 2004, 15, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control. Fact Sheet: Athletes: Don’t Get Sidelined by Sickle Cell Trait! Play It Safe with These Helpful Tips. Available online: Https://www.Cdc.Gov/ncbddd/sicklecell/documents/sickle-cell-athletes.Pdf (accessed on 13 June 2021).
- Centers for Disease Control. Fact Sheet: Coaches: Don’t Let Your Athletes Get Sidelined by Sickle Cell Trait! Help Them Play It Safe with These Helpful Tips. Available online: Https://www.Cdc.Gov/ncbddd/sicklecell/documents/sickle-cell-coaches.Pdf (accessed on 13 June 2021).
- Centers for Disease Control. Fact Sheet: Team Doctors (Trainers): Don’t Let Your Athletes Get Sidelined by Sickle Cell Trait! Help Them Play It Safe with These Helpful Tips. Available online: Https://www.Cdc.Gov/ncbddd/sicklecell/documents/sickle-cell-doctors.Pdf (accessed on 13 June 2021).
- National Collegiate Athletic Association. Fact Sheet for Student-Athletes: Sickle Cell Trait. Available online: Https://www.Ncaa.Org/sites/default/files/ncaasicklecelltraitforsa.Pdf (accessed on 13 June 2021).
- National Athletic Trainers’ Association Consensus Statement: Sickle Cell Trait and the Athlete. Available online: Https://www.Nata.Org/sites/default/files/sicklecelltraitandtheathlete.Pdf (accessed on 13 June 2021).


| Variable | RMC (N = 71) | Matched (N = 122) | p Value |
|---|---|---|---|
| Age, median (IQR) | 29.6 (23.2–37.5) | 29.9 (23.8–39.6) | 0.5 |
| Biological sex, no. (%) | 0.7 | ||
| Male | 49 (69) | 87 (71) | |
| Female | 22 (31) | 35 (29) | |
| Race, no. (%) | <0.001 | ||
| African American | 61 (86) | 47 (39) | |
| White | 7 (10) | 66 (54) | |
| Hispanic | 2 (3) | 4 (3) | |
| Asian | 1 (1) | 5 (4) | |
| Sickle hemoglobinopathy, no. (%) | 71 (100) | 0 | <0.001 |
| Sickle cell trait | 70 (99) | ||
| Sickle beta-thalassemia | 1 (1) | ||
| Comorbidities, no. (%) | |||
| HTN | 12 (17) | 33 (27) | 0.2 |
| Other comorbidities | 8 (11) | 58 (48) | <0.001 |
| ECOG, no. (%) | <0.001 | ||
| 0 | 15 (21) | 78 (64) | |
| 1 | 42 (59) | 41 (34) | |
| 2 | 10 (14) | 2 (2) | |
| 3 | 4 (6) | 1 (1) | |
| BMI, median (IQR), kg/m2 | 27 (24.3–29.9) | 27.1 (23.9–31.6) | 0.7 |
| Albumin, median (IQR), g/dL | 4.3 (4–4.6) | 4.4 (4.1–4.6) | 0.3 |
| Smoking history, no. (%) | 15 (21) | 56 (46) | 0.001 |
| Exercise history, no. (%) | 36 (51) | 18 (15) | <0.001 |
| Athlete, no. (%) | 24 (34) | 5 (4) | <0.001 |
| Military, no. (%) | 7 (10) | 4 (3) | 0.005 |
| Activity index, no. (%) | 47 (66) | 20 (16) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shapiro, D.D.; Soeung, M.; Perelli, L.; Dondossola, E.; Surasi, D.S.; Tripathi, D.N.; Bertocchio, J.-P.; Carbone, F.; Starbuck, M.W.; Van Alstine, M.L.; et al. Association of High-Intensity Exercise with Renal Medullary Carcinoma in Individuals with Sickle Cell Trait: Clinical Observations and Experimental Animal Studies. Cancers 2021, 13, 6022. https://doi.org/10.3390/cancers13236022
Shapiro DD, Soeung M, Perelli L, Dondossola E, Surasi DS, Tripathi DN, Bertocchio J-P, Carbone F, Starbuck MW, Van Alstine ML, et al. Association of High-Intensity Exercise with Renal Medullary Carcinoma in Individuals with Sickle Cell Trait: Clinical Observations and Experimental Animal Studies. Cancers. 2021; 13(23):6022. https://doi.org/10.3390/cancers13236022
Chicago/Turabian StyleShapiro, Daniel D., Melinda Soeung, Luigi Perelli, Eleonora Dondossola, Devaki Shilpa Surasi, Durga N. Tripathi, Jean-Philippe Bertocchio, Federica Carbone, Michael W. Starbuck, Michael L. Van Alstine, and et al. 2021. "Association of High-Intensity Exercise with Renal Medullary Carcinoma in Individuals with Sickle Cell Trait: Clinical Observations and Experimental Animal Studies" Cancers 13, no. 23: 6022. https://doi.org/10.3390/cancers13236022
APA StyleShapiro, D. D., Soeung, M., Perelli, L., Dondossola, E., Surasi, D. S., Tripathi, D. N., Bertocchio, J.-P., Carbone, F., Starbuck, M. W., Van Alstine, M. L., Rao, P., Katz, M. H. G., Parker, N. H., Shah, A. Y., Carugo, A., Heffernan, T. P., Schadler, K. L., Logothetis, C., Walker, C. L., ... Msaouel, P. (2021). Association of High-Intensity Exercise with Renal Medullary Carcinoma in Individuals with Sickle Cell Trait: Clinical Observations and Experimental Animal Studies. Cancers, 13(23), 6022. https://doi.org/10.3390/cancers13236022







