Cobaltabis(dicarbollide) ([o-COSAN]−) as Multifunctional Chemotherapeutics: A Prospective Application in Boron Neutron Capture Therapy (BNCT) for Glioblastoma
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Instrumentation and Measurements
2.3. Cell Lines
2.4. Metallabis (Dicarbollides) Solutions Preparation
2.5. Cell Viability of Monolayer Cultures
2.6. 3-D Spheroid Cultures
2.7. Cell Viability of Spheroid Cultures
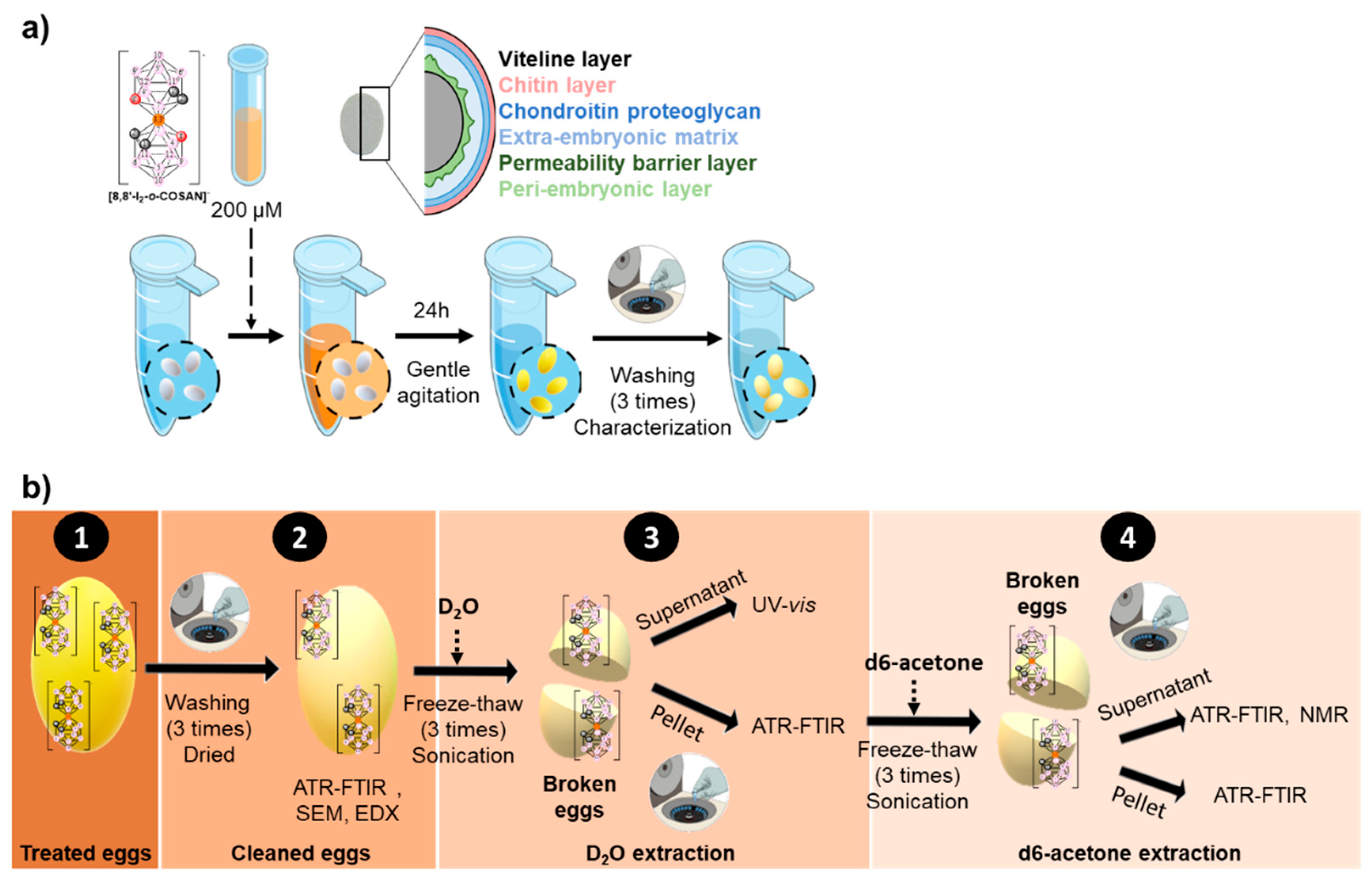
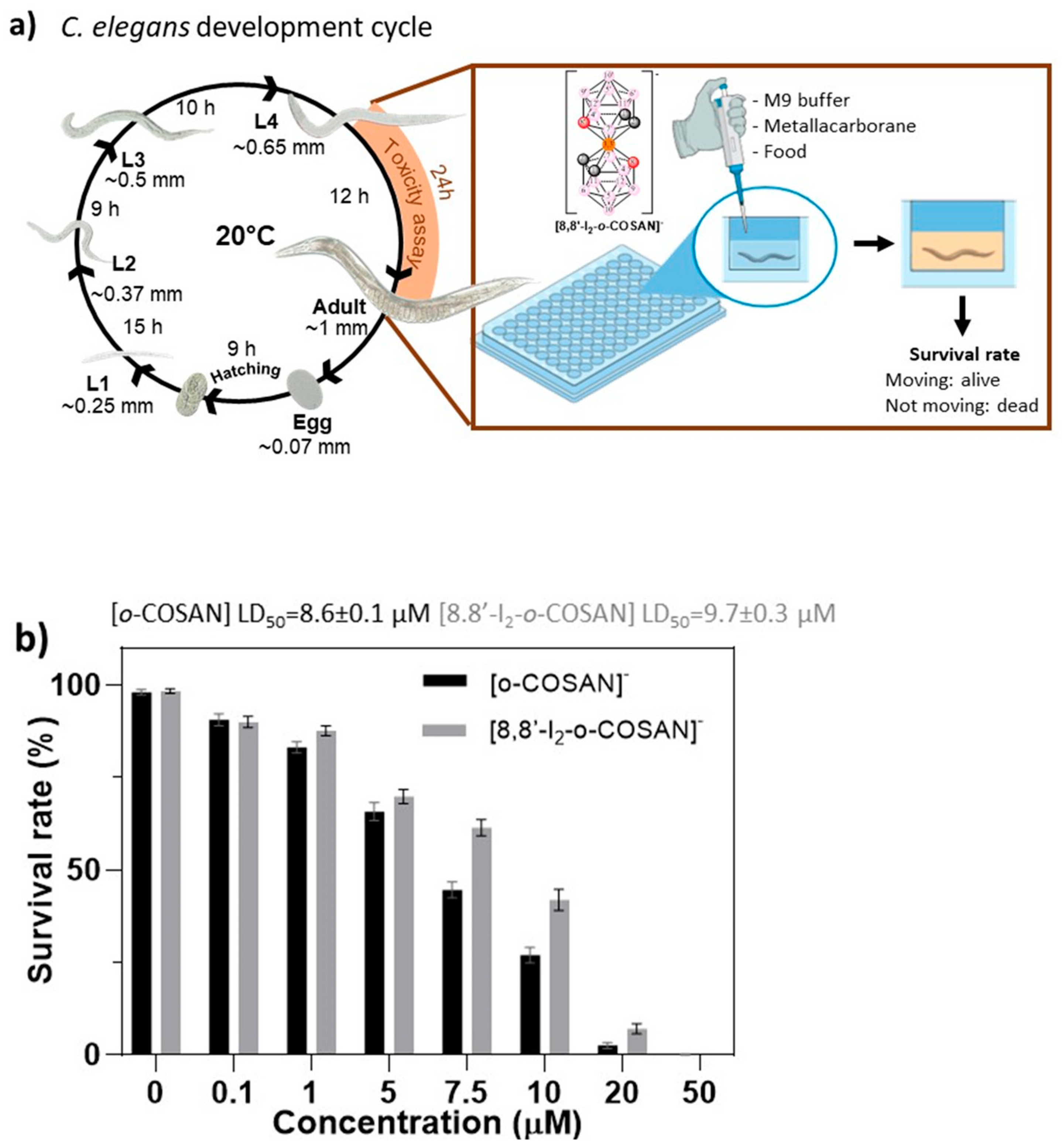
2.8. In Vivo Studies in C. elegans
2.9. Uptake Experiments
2.10. Inductively Coupled Plasma Mass Spectrometry (ICP-MS)
2.11. Neutron Irradiation Experiments
2.12. Statistical Analysis
3. Results and Discussion
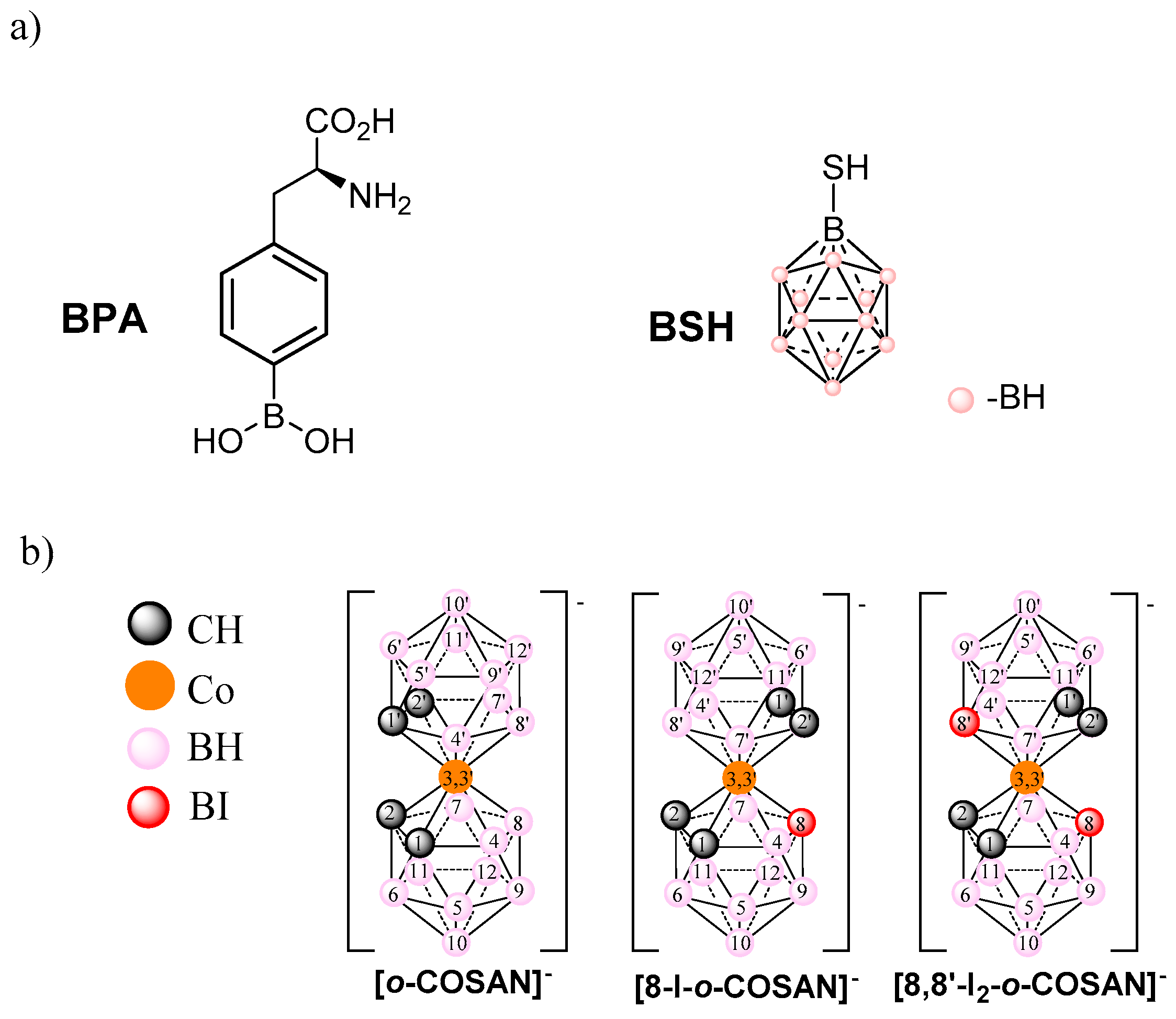
3.1. Physical-Chemical Properties of the Sodium Salts of [o-COSAN]− and [8,8′-I2-o-COSAN]−
3.1.1. Solubility and Lipophilicity of Na[o-COSAN] and Na[8,8′-I2-o-COSAN]
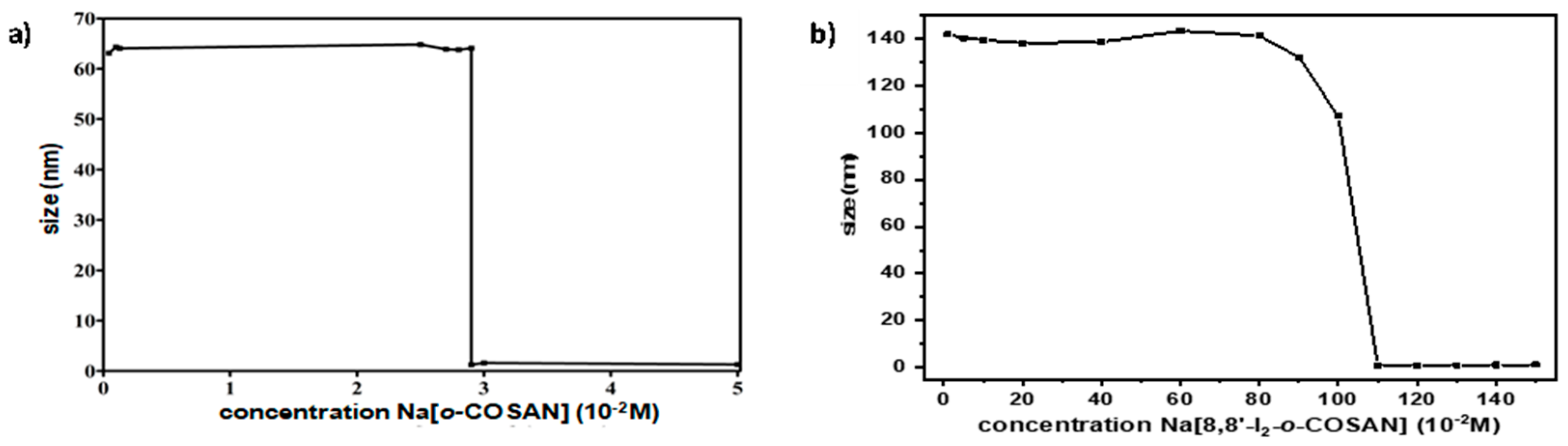
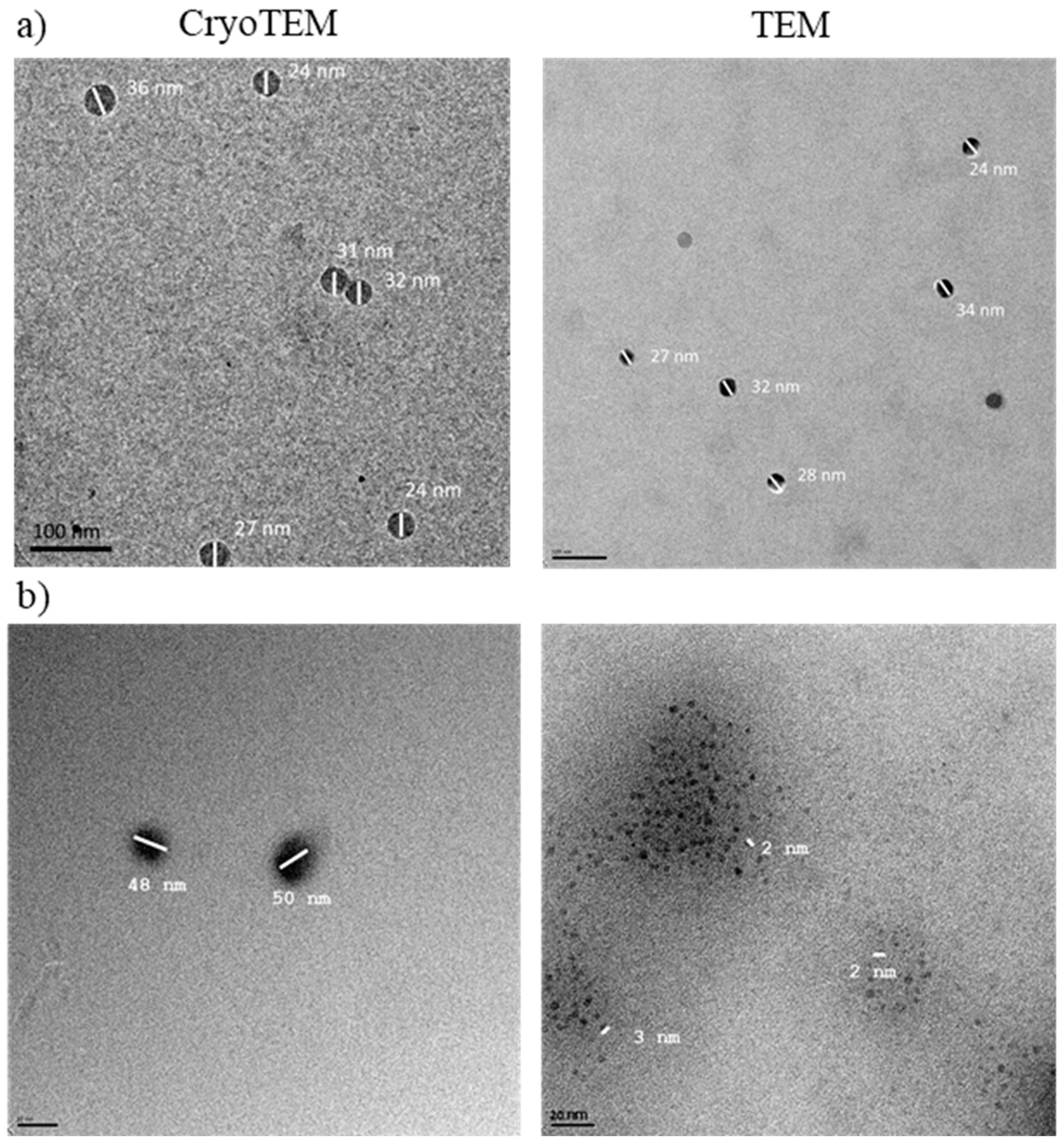
3.1.2. Dynamic Light Scattering and Transmission Electron Microscopy
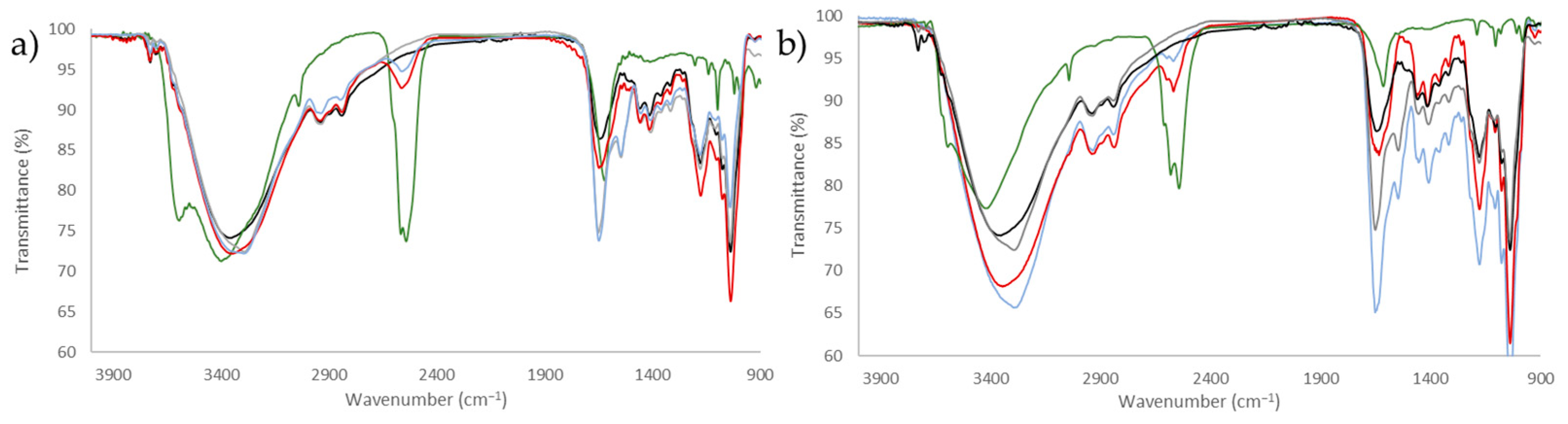
3.1.3. Infrared and NMR Studies
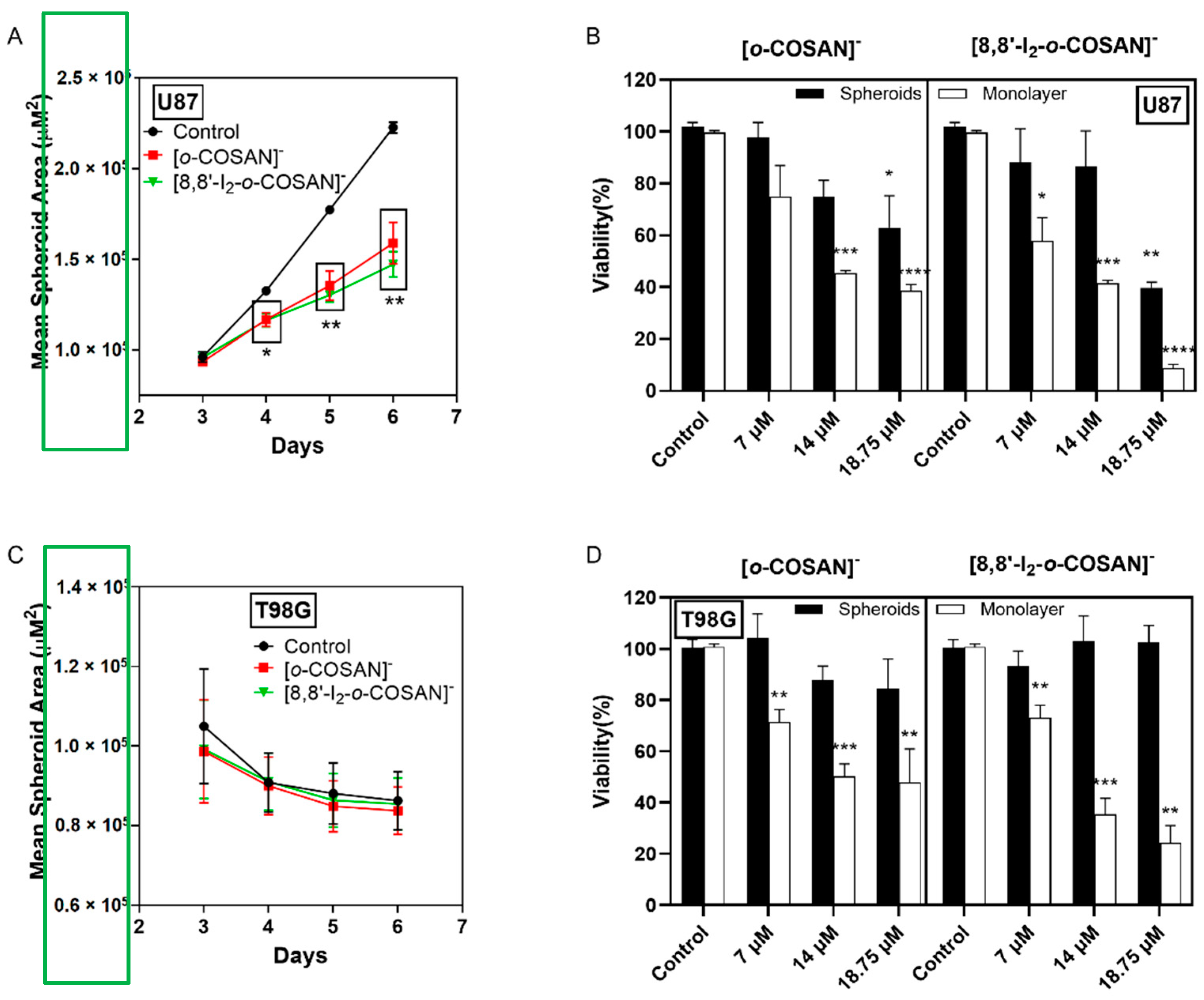
3.2. Cell Viability Assays
3.3. Effect of Cobaltallabis (Dicarbollides) in GBM Spheroids’ Viability
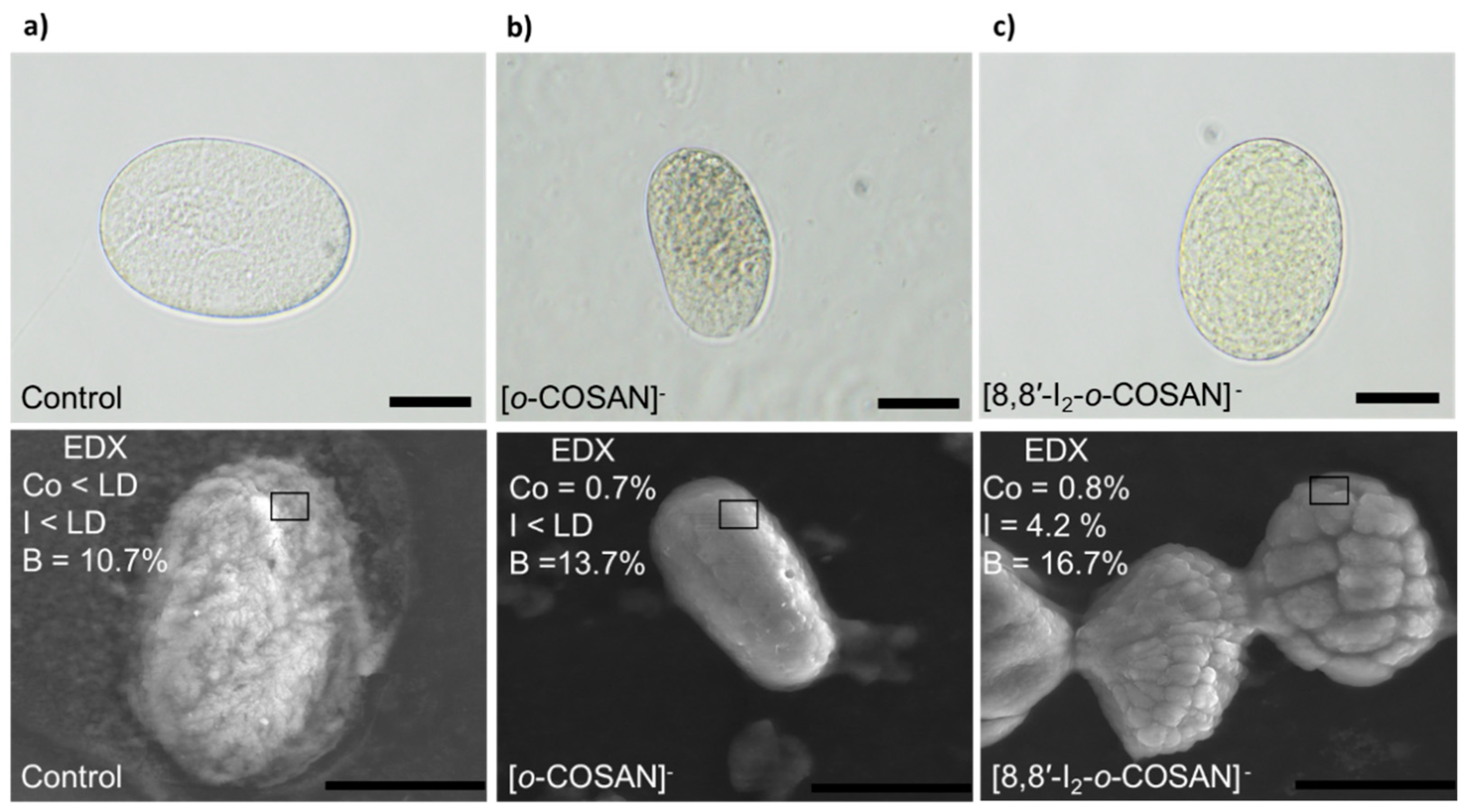
3.4. In Vivo Tests with Caenorhabditis elegans (C. elegans)
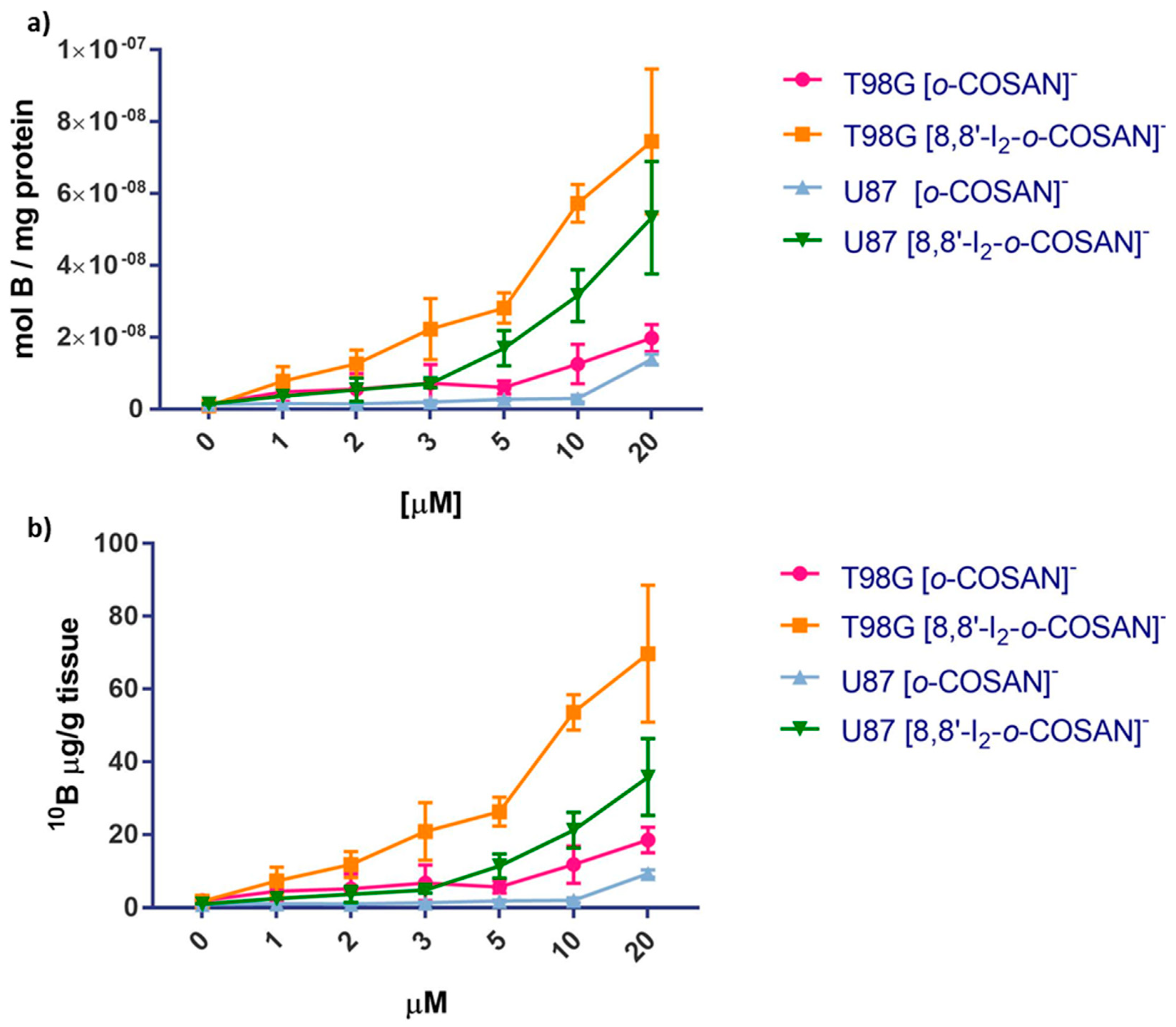
3.5. Cell Uptake Experiments
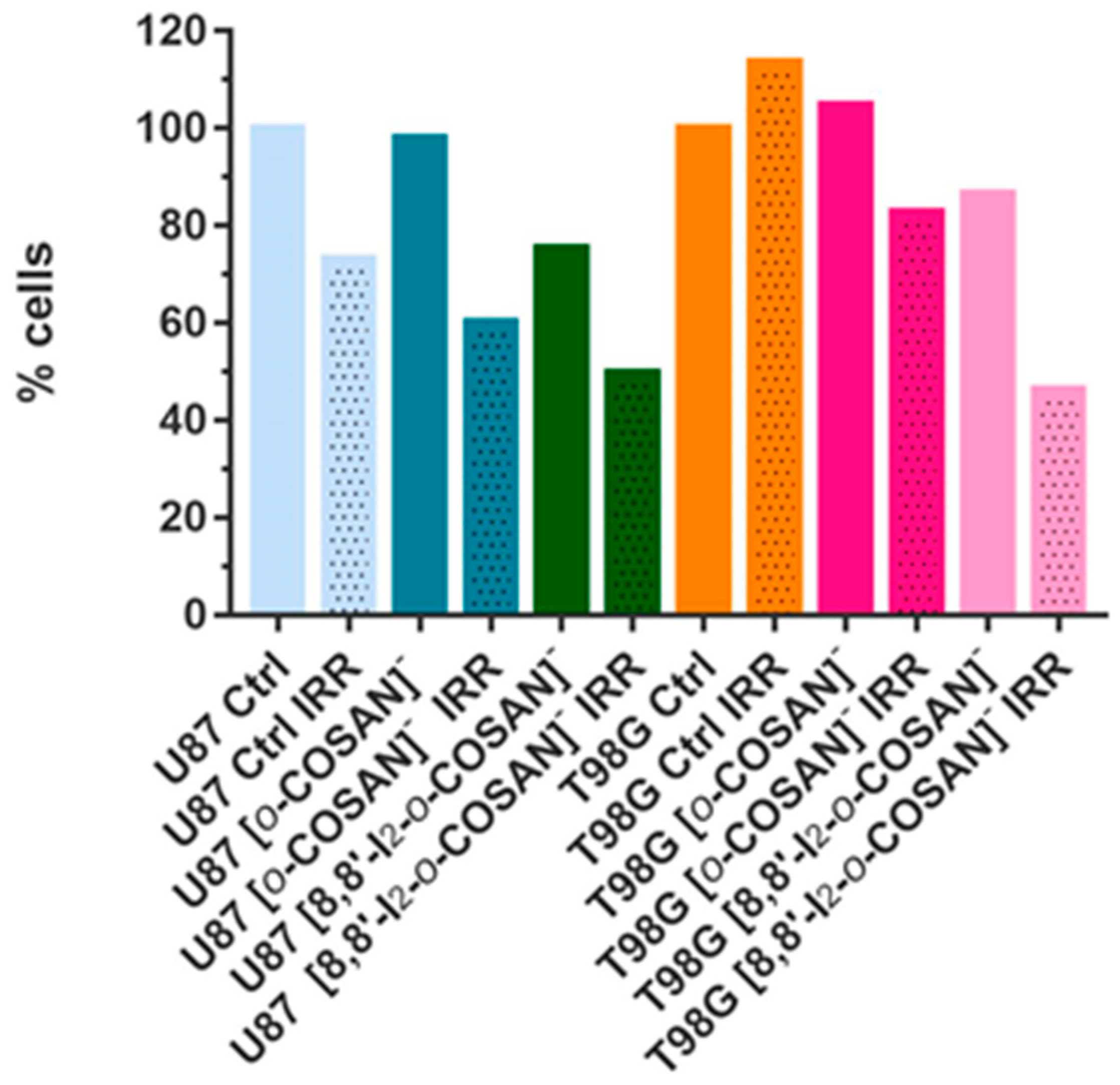
3.6. BNCT Studies in Glioblastoma Cells
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fitzmaurice, C.; Dicker, D.; Pain, A.; Hamavid, H.; Moradi-Lakeh, M.; MacIntyre, M.F.; Allen, C.; Hansen, G.; Woodbrook, R.; Wolfe, C.; et al. The Global Burden of cancer 2013. JAMA Oncol. 2015, 1, 505. [Google Scholar] [CrossRef]
- Ohka, F.; Natsume, A.; Wakabayashi, T. Current trends in targeted therapies for glioblastoma multiforme. Neurol. Res. Int. 2012, 2012, 878425. [Google Scholar] [CrossRef]
- Goellner, E.M.; Grimme, B.; Brown, A.R.; Lin, Y.-C.; Wang, X.-H.; Sugrue, K.F.; Mitchell, L.; Trivedi, R.N.; Tang, J.; Sobol, R.W. Overcoming temozolomide resistance in glioblastoma via dual inhibition of NAD+ biosynthesis and base excision repair. Cancer Res. 2011, 71, 2308–2317. [Google Scholar] [CrossRef] [Green Version]
- Moreno, M.; Pedrosa, L.; Paré, L.; Pineda, E.; Bejarano, L.; Martínez, J.; Balasubramaniyan, V.; Ezhilarasan, R.; Kallarackal, N.; Kim, S.-H.; et al. GPR56/ADGRG1 inhibits mesenchymal differentiation and radioresistance in glioblastoma. Cell Rep. 2017, 21, 2183–2197. [Google Scholar] [CrossRef] [Green Version]
- Stupp, R.; Mason, W.P.; van den Bent, M.J.; Weller, M.; Fisher, B.; Taphoorn, M.J.B.; Belanger, K.; Brandes, A.A.; Marosi, C.; Bogdahn, U.; et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N. Engl. J. Med. 2005, 352, 987–996. [Google Scholar] [CrossRef]
- Nedunchezhian, K.; Aswath, N.; Thiruppathy, M.; Thirugnanamurthy, S. Boron neutron capture therapy—A literature review. J. Clin. Diagn. Res. 2016, 10, ZE01–ZE04. [Google Scholar] [CrossRef]
- Barth, R.F.; Zhang, Z.; Liu, T. A realistic appraisal of boron neutron capture therapy as a cancer treatment modality. Cancer Commun. 2018, 38, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dymova, M.A.; Taskaev, S.Y.; Richter, V.A.; Kuligina, E.V. Boron neutron capture therapy: Current status and future perspectives. Cancer. Commun. 2020, 40, 406–421. [Google Scholar] [CrossRef]
- Sauerwein, W.A.G.; Sancey, L.; Hey-Hawkins, E.; Kellert, M.; Panza, L.; Imperio, D.; Balcerzyk, M.; Rizzo, G.; Scalco, E.; Herrmann, K.; et al. Theranostics in boron neutron capture therapy. Life 2021, 11, 330. [Google Scholar] [CrossRef] [PubMed]
- Imamichi, S.; Masutani, M. Investigation of biological effect of BNCT system in NCC. Cancer Sci. 2018, 109, 753. [Google Scholar] [CrossRef] [Green Version]
- Sköld, K.; Gorlia, T.; Pellettieri, L.; Giusti, V.; Stenstam, B.H.; Hopewell, J.W. Boron neutron capture therapy for newly diagnosed glioblastoma multiforme: An assessment of clinical potential. J. Radiol. 2010, 83, 596–603. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.-W.; Hsueh Liu, Y.-W.; Chou, F.-I.; Jiang, S.-H. Clinical trials for treating recurrent head and neck cancer with boron neutron capture therapy using the Tsing-Hua open pool reactor. Cancer Commun. 2018, 38, 37. [Google Scholar] [CrossRef] [Green Version]
- Sander, A.; Wosniok, W.; Gabel, D. Case numbers for a randomized clinical trial of boron neutron capture therapy for glioblastoma multiforme. Appl. Radiat. Isot. 2014, 88, 16–19. [Google Scholar] [CrossRef]
- Kageji, T.; Nakagawa, Y.; Kitamura, K.; Matsumoto, K.; Hatanaka, H. Pharmacokinetics and boron uptake of BSH (Na2B12H11SH) in patients with intracranial tumors. J. Neuro-Oncol. 1997, 33, 117–130. [Google Scholar] [CrossRef]
- Isono, A.; Tsuji, M.; Sanada, Y.; Matsushita, A.; Masunaga, S.; Hirayama, T.; Nagasawa, H. Design, synthesis, and evaluation of lipopeptide conjugates of mercaptoundecahydrododecaborate for Boron neutron capture therapy. ChemMedChem 2019, 14, 823–832. [Google Scholar] [CrossRef] [PubMed]
- Futamura, G.; Kawabata, S.; Nonoguchi, N.; Hiramatsu, R.; Toho, T.; Tanaka, H.; Masunaga, S.-I.; Hattori, Y.; Kirihata, M.; Ono, K.; et al. Evaluation of a novel sodium borocaptate containing unnatural amino acid as a Boron delivery agent for neutron capture therapy of the F98 rat glioma. Radiat. Oncol. 2017, 12, 26. [Google Scholar] [CrossRef] [Green Version]
- Masunaga, S.; Nagasawa, H.; Gotoh, K.; Uto, Y.; Hori, H.; Sakurai, Y.; Nagata, K.; Suzuki, M.; Maruhashi, A.; Kinashi, Y.; et al. Evaluation of hypoxia-specific cytotoxic bioreductive agent sodium borocaptate-10B conjugates, as 10B-carriers in Boron neutron capture therapy. Radiat. Med. 2006, 24, 98–107. [Google Scholar] [CrossRef]
- Stella Pharma. Available online: https://stella-pharma.co.jp/en/news/ (accessed on 28 April 2020).
- Cerecetto, H.; Couto, M. Medicinal chemistry of boron-bearing compounds for BNCT. In Glioma Treatment: Current Challenges and Perspectives, Glioma Contemporary Diagnostic and Therapeutic Approaches; Omerhodžić, I., Arnautović, K., Eds.; IntechOpen: London, UK, 2018; Available online: https://www.intechopen.com/chapters/61749 (accessed on 15 October 2021). [CrossRef] [Green Version]
- Grimes, R.N. Carboranes, 3rd ed.; Elsevier Inc.: New York, NY, USA, 2016. [Google Scholar]
- Masalles, C.; Llop, J.; Viñas, C.F. Extraordinary overoxidation resistance increase in self-doped polypyrroles by using non-conventional low charge-density anions. Adv. Mater. 2002, 14, 826–829. [Google Scholar] [CrossRef]
- Nuñez, R.; Romero, I.; Teixidor, F.; Viñas, C. Icosahedral boron clusters: A perfect tool for the enhancement of polymer features. Chem. Soc. Rev. 2016, 45, 5147–5173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spryshkova, R.A.; Karaseva, L.I.; Brattsev, V.A.; Serebriakov, N.G. Toxicity of the functional derivatives of polyhedral carboranes. Med. Radiol. 1981, 26, 62–64. [Google Scholar]
- Spryshkova, R.A.; Brattsev, V.A.; Sherman, T.L.; Stanko, V.I. X-ray abolition of the inhibitary effect of the tumor on the regenerative progress. Med. Radiol. 1981, 26, 51–53. [Google Scholar]
- Plesek, J. Potential applications of the boron cluster compounds. Chem. Rev. 1992, 92, 269–278. [Google Scholar] [CrossRef]
- Gona, K.B.; Zaulet, A.; Gomez-Vallejo, V.; Teixidor, F.; Llop, J.; Viñas, C. COSAN as a molecular imaging platform: Synthesis and “in vivo” imaging. Chem. Commun. 2014, 50, 11415–11417. [Google Scholar] [CrossRef]
- Fuentes, I.; García-Mendiola, T.; Sato, S.; Pita, M.; Nakamura, H.; Lorenzo, E.; Teixidor, F.; Marques, F.; Viñas, C. Metallacarboranes on the Road to Anticancer Therapies: Cellular Uptake, DNA Interaction, and Biological Evaluation of Cobaltabisdicarbollide [COSAN]−. Chem. Eur. J. 2018, 24, 17239–17254. [Google Scholar] [CrossRef]
- Fink, K.; Uchman, M. Boron cluster compounds as new chemical leads for antimicrobial therapy. Coord. Chem. Rev. 2021, 431, 213684. [Google Scholar] [CrossRef]
- Poater, J.; Viñas, C.; Bennour, I.; Gordils, S.E.; Solà, M.; Teixidor, F. Too persistent to give up: Aromaticity in boron clusters survives radical structural changes. J. Am. Chem. Soc. 2020, 142, 9396–9407. [Google Scholar] [CrossRef] [PubMed]
- Hardie, M.J.; Raston, C.L. Solid state supramolecular assemblies of charged supermolecules (Na[2.2.2]cryptate) + and anionic carboranes with host cyclotriveratrylene. Chem. Commun. 2001, 2, 905–906. [Google Scholar] [CrossRef]
- Fox, M.A.; Hughes, A.K. Cage C-H⋯X interactions in solid-state structures of icosahedral carboranes. Coord. Chem. Rev. 2004, 248, 457–476. [Google Scholar] [CrossRef]
- Tarrés, M.; Viñas, C.; González-Cardoso, P.; Hänninen, M.M.; Sillanpää, R.; Dordovic, V.; Uchman, M.; Teixidor, F.; Matejicek, P. Aqueous self-assembly and cation selectivity of cobaltabisdicarbollide dianionic dumbbells. Chem. Eur. J. 2014, 20, 6786–6794. [Google Scholar] [CrossRef]
- Brusselle, D.; Bauduin, P.; Girard, L.; Zaulet, A.; Viñas, C.; Teixidor, F.; Ly, I.; Diat, O. Lyotropic Lamellar Phase Formed from Monolayered θ-Shaped Carborane-Cage Amphiphiles. Angew. Chem. Int. Ed. 2013, 52, 12114–12118. [Google Scholar] [CrossRef] [PubMed]
- Bauduin, P.; Prevost, S.; Farràs, P.; Teixidor, F.; Diat, O.; Zemb, T. A theta-shaped amphiphilic cobaltabisdicarbollide anion: Transition from monolayer vesicles to micelles. Angew. Chem. Int. Ed. 2011, 50, 5298–5300. [Google Scholar] [CrossRef] [PubMed]
- Viñas, C.; Tarrés, M.; González-Cardoso, P.; Farràs, P.; Bauduin, P.; Teixidor, F. Surfactant behaviour of metallacarboranes. A study based on the electrolysis of water. Dalton Trans. 2014, 43, 5062–5068. [Google Scholar] [CrossRef]
- Ďorďovič, V.; Tošner, Z.; Uchman, M.; Zhigunov, A.; Reza, M.; Ruokolainen, J.; Pramanik, G.; Cígler, P.; Kalíková, K.; Gradzielski, M.; et al. Stealth Amphiphiles: Self-Assembly of Polyhedral Boron Clusters. Langmuir 2016, 32, 6713–6722. [Google Scholar] [CrossRef]
- Uchman, M.; Ďorďovič, V.; Tošner, Z.; Matějíček, P. Classical Amphiphilic Behavior of Nonclassical Amphiphiles: A Comparison of Metallacarborane Self-Assembly with SDS Micellization. Angew. Chem. Int. Ed. 2015, 54, 14113–14117. [Google Scholar] [CrossRef]
- Tarrés, M.; Canetta, E.; Paul, E.; Forbes, J.; Azzouni, K.; Viñas, C.; Teixidor, F.; Harwood, A.J. Biological interaction of living cells with COSAN-based synthetic vesicles. Sci. Rep. 2015, 5, 7804. [Google Scholar] [CrossRef]
- Navascuez, M.; Dupin, D.; Grand, H.-J.; Gómez-Vallejo, V.; Loinaz, I.; Cosido, U.; Llop, J. COSAN-stabilised omega-3 oil-in-water nanoemulsions to prolong lung residence time for poorly water soluble drugs. Chem. Commun. 2020, 56, 8972–8975. [Google Scholar] [CrossRef] [PubMed]
- Kazheva, O.N.; Alexandrov, G.G.; Kravchenko, A.V.; Starodub, V.A.; Lobanova, I.A.; Sivaev, I.B.; Bregadze, V.I.; Titov, L.V.; Buravov, L.I.; Dyachenko, O.A. Molecular conductors with 8,8′-diiodo cobalt bis(dicarbollide) anion. J. Organomet. Chem. 2009, 694, 2336–2342. [Google Scholar] [CrossRef]
- Zakharkin, L.I.; Olshevskaya, V.A.; Balagurova, E.V.; Petrovskii, P.V. Palladium-catalyzed cross coupling of the bis(9-iodo-1,2-dicarbollyl)cobaltate anion with organic magnesium and zinc compounds, yielding bis[9-alkyl(aryl)-1,2-dicarbollyl]cobaltate anions. Russ. J. Gen. Chem. 2000, 70, 550–551. [Google Scholar]
- Kazheva, O.N.; Aleksandrov, G.G.; Kravchenko, A.V.; Starodub, V.A.; Zhigareva, G.G.; Sivaev, I.B.; Bregadze, V.I.; Buravov, L.I.; Titov, L.V.; Dyachenko, O.A. Synthesis, structures, and conductivities of salts (BEDT-TTF)[9,9′(12′)-I2-3,3′-Co(1,2-C2B9H10)2] and (TTF)[9,9′,12,12′-I4-3,3′-Co(1,2-C2B9H9)2]. Russ. Chem. Bull. 2010, 59, 1137–1144. [Google Scholar] [CrossRef]
- Hurlburt, P.K.; Miller, R.L.; Abney, K.D.; Foreman, T.M.; Butcher, R.J.; Kinkhead, S.A. New synthetic routes to B-halogenated derivatives of cobalt dicarbollide. Inorg. Chem. 1995, 34, 5215–5219. [Google Scholar] [CrossRef]
- Matel, L.; Macasek, F.; Rajec, P.; Hermanek, P.; Plesek, J. B-Halogen derivatives of the bis(1,2-dicarbollyl)cobalt(III) anion. Polyhedron 1982, 1, 511–519. [Google Scholar] [CrossRef]
- Method of Preparation of The Chlorinated Cobaltic Dicarbolide. Patent CS215282B1, 27 August 1982.
- Pepiol, A.; Teixidor, F.; Sillanpää, R.; Lupu, M.; Viñas, C. Stepwise Sequential Redox Potential Modulation Possible on a Single Platform. Angew. Chem. Int. Ed. 2011, 50, 12491–12495. [Google Scholar] [CrossRef]
- Tarrés, M.; Canetta, E.; Viñas, C.; Teixidor, F.; Harwood, A.J. Imaging in living cells using νB–H Raman spectroscopy: Monitoring COSAN uptake. Chem. Commun. 2014, 50, 3370–3372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verdiá-Báguena, C.; Alcaraz, A.; Aguilella, V.M.; Cioran, A.M.; Tachikawa, S.; Nakamura, H.; Teixidor, F.; Viñas, C. Amphiphilic COSAN and I2-COSAN crossing synthetic lipid membranes: Planar bilayers and liposomes. Chem. Commun. 2014, 50, 6700–6703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wiesboeck, R.A.; Hawthorne, M.F. Dicarbaundecaborane(13) and Derivatives. J. Am. Chem. Soc. 1964, 86, 1642–1643. [Google Scholar] [CrossRef]
- Rojo, I.; Teixidor, F.; Viñas, C.; Kivekäs, R.; Sillanpää, R. Methylation and Demethylation in Cobaltabis(dicarbollide) Derivatives. Organometallics 2003, 22, 4642–4646. [Google Scholar] [CrossRef]
- Zaulet, A.; Teixidor, F.; Bauduin, P.; Diat, O.; Hirva, P.; Ofori, A.; Viñas, C. Deciphering the role of the cation in anionic cobaltabisdicarbollide clusters. J. Organomet. Chem. 2018, 865, 214–225. [Google Scholar] [CrossRef]
- Pinto, C.I.G.; Bucar, S.; Alves, V.; Fonseca, A.; Abrunhosa, A.J.; da Silva, C.L.; Guerreiro, J.F.; Mendes, F. Copper-64 Chloride Exhibits Therapeutic Potential in Three-Dimensional Cellular Models of Prostate Cancer. Front. Mol. Biosci. 2020, 7, 609172. [Google Scholar] [CrossRef]
- Brenner, S. The Genetics of Caenorhabditis elegans. Genetics 1974, 77, 71–94. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Moragas, L.; Berto, P.; Vilches, C.; Quidant, R.; Kolovou, A.; Santarella-Mellwig, R.; Schwab, Y.; Stüzenbaum, S.; Roig, A.; Laromaine, A. In vivo testing of gold nanoparticles using the Caenorhabditis elegans model organism. Acta Biomater. 2017, 53, 598–609. [Google Scholar] [CrossRef] [Green Version]
- Lipinski, C.A.; Lombardo, F.; Dominy, B.W.; Feeney, P.J. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv. Drug Deliv. Rev. 2001, 46, 3−26. [Google Scholar] [CrossRef]
- Jorgensen, W.L.; Duffy, E.M. Prediction of drug solubility from structure. Adv. Drug Deliv. Rev. 2002, 54, 355−366. [Google Scholar] [CrossRef]
- Wang, J.; Krudy, G.; Hou, T.; Zhang, W.; Holland, G.; Xu, X. Development of reliable aqueous solubility models and their application in druglike analysis. J. Chem. Inf. Model. 2007, 47, 1395–1404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pike, V.W. PET radiotracers: Crossing the blood–brain barrier and surviving metabolism. Trends Pharmacol. Sci. 2009, 30, 431–440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chevrot, G.; Schurhammer, R.; Wipff, G. Surfactant Behavior of “Ellipsoidal” Dicarbollide Anions: A Molecular Dynamics Study. J. Phys. Chem. B 2006, 110, 9488. [Google Scholar] [CrossRef]
- Matejícek, P.; Cígler, P.; Procházka, K.; Král, V. Molecular Assembly of Metallacarboranes in Water: Light Scattering and Microscopy Study. Langmuir 2006, 22, 575. [Google Scholar] [CrossRef] [PubMed]
- Mata, I.; Alkorta, I.; Molins, E.; Espinosa, E. Electrostatics at the Origin of the Stability of Phosphate-Phosphate Complexes Locked by Hydrogen Bonds. ChemPhysChem 2012, 13, 1421–1424. [Google Scholar] [CrossRef]
- Mata, I.; Alkorta, I.; Molins, E.; Espinosa, E. Tracing environment effects that influence the stability of anion–anion complexes: The case of phosphate–phosphate interactions. Chem. Phys. Lett. 2013, 555, 106–109. [Google Scholar] [CrossRef]
- Mata, I.; Molins, E.; Alkorta, I.; Espinosa, E. The Paradox of Hydrogen-Bonded Anion–Anion Aggregates in Oxoanions: A Fundamental Electrostatic Problem Explained in Terms of Electrophilic·Nucleophilic Interactions. J. Phys. Chem. A 2015, 119, 183–194. [Google Scholar] [CrossRef] [Green Version]
- He, Q.; Tu, P.; Sessler, J.L. Supramolecular Chemistry of Anionic Dimers, Trimers, Tetramers and Clusters. Chem 2018, 4, 46–93. [Google Scholar] [CrossRef] [Green Version]
- Nuez-Martínez, M.; Pedrosa, L.; Martinez-Rovira, I.; Yousef, I.; Diao, D.; Teixidor, F.; Stanzani, E.; Martínez-Soler, F.; Tortosa, A.; Sierra, À.; et al. Synchrotron-based Fourier-transform infrared micro-spectroscopy (SR-FTIRM) fingerprint of the small anionic molecule Cobaltabisdicarbollide uptake in glioma stem cells. Int. J. Mol. Sci. 2021, 22, 9937. [Google Scholar] [CrossRef]
- Leytes, L.A. Vibrational spectroscopy of carboranes and parent boranes and its capabilities in carborane chemistry. Chem. Rev. 1992, 92, 2, 279–323. [Google Scholar] [CrossRef]
- Lee, S.Y. Temozolomide resistance in glioblastoma multiforme. Genes Dis. 2016, 11, 198–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mittler, F.; Obeïd, P.; Rulina, A.V.; Haguet, V.; Gidrol, X.; Balakirev, M.Y. High-Content Monitoring of Drug Effects in a 3D Spheroid Model. Front. Oncol. 2017, 7, 293. [Google Scholar] [CrossRef] [Green Version]
- Gonzalez-Moragas, L.; Yu, S.M.; Murillo-Cremaes, N.; Laromaine, A.; Roig, A. Scale-up synthesis of iron oxide nanoparticles by microwave-assisted thermal decomposition. Chem. Eng. J. 2015, 281, 87–95. [Google Scholar] [CrossRef]
- Gonzalez-Moragas, L.; Yu, S.M.; Benseny-Cases, N.; Stürzenbaum, S.; Roig, A.; Laromaine, A. Toxicogenomics of iron oxide nanoparticles in the nematode C. elegans. Nanotoxicology 2017, 11, 647–657. [Google Scholar] [CrossRef] [Green Version]
- Stoica, A.-I.; Viñas, C.; Teixidor, F. Cobaltabisdicarbollide anion receptor for enantiomer-selective membrane electrodes. Chem. Commun. 2009, 33, 4988–4990. [Google Scholar] [CrossRef] [PubMed]
- Stoica, A.-I.; Viñas, C.; Teixidor, F. Application of the cobaltabisdicarbollide anion to the development of ion selective PVC membrane electrodes for tuberculosis drug analysis. Chem. Commun. 2008, 48, 6492–6494. [Google Scholar] [CrossRef] [PubMed]
- Stoica, A.-I.; Klebera, C.; Viñas, C.; Teixidor, F. Ion selective electrodes for protonable nitrogen containing analytes:Metallacarboranes as active membrane components. Electrochim. Acta 2013, 113, 94–98. [Google Scholar] [CrossRef]
- Krenger, R.; Burri, J.T.; Lehnert, T.; Nelson, B.J.; Gijs, M.A.M. Force microscopy of the Caenorhabditis elegans embryonic eggshell. Microsyst. Nanoeng. 2020, 6, 29. [Google Scholar] [CrossRef]
- García-Mendiola, T.; Bayon-Pizarro, V.; Zaulet, A.; Fuentes, I.; Pariente, F.; Teixidor, F.; Viñas, C.; Lorenzo, E. Metallacarboranes as tunable redox potential electrochemical indicators for screening of gene mutation. Chem. Sci. 2016, 7, 5786–5797. [Google Scholar] [CrossRef] [Green Version]
- Cigler, P.; Kožíšek, M.; Řezáčová, P.; Brynda, J.; Otwinowski, Z.; Pokorna, J.; Kožíšek, M.; Gruner, B.; Dolečková-Marešová, L.; Máša, M.; et al. From nonpeptide toward noncarbon protease inhibitors: Metallacarboranes as specific and potent inhibitors of HIV protease. Proc. Natl. Acad. Sci. USA 2005, 102, 15394–15399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fuentes, I.; Pujols, J.; Viñas, C.; Ventura, S.; Teixidor, F. Dual binding mode of metallacarborane produces a robust shield on proteins. Chem. A Eur. J. 2019, 25, 12820–12829. [Google Scholar] [CrossRef]
- Goszczynski, T.M.; Fink, K.; Kowalski, K.; Lesnikowski, Z.J.; Boratynski, J. Interactions of Boron Clusters and their Derivatives with Serum Albumin. Sci. Rep. 2017, 7, 9800. [Google Scholar] [CrossRef] [Green Version]
- Evans, N.H.; Beer, P.D. Advances in Anion Supramolecular Chemistry: From Recognition to Chemical Applications. Angew. Chem. Int. Ed. 2014, 53, 11716–11754. [Google Scholar] [CrossRef] [Green Version]
- Busschaert, N.; Caltagirone, C.; van Rossom, W.; Gale, P.A. Applications of Supramolecular Anion Recognition. Chem. Rev. 2015, 115, 8038–8055. [Google Scholar] [CrossRef] [PubMed]
- Mathew, B.; Carradori, S.; Guglielmi, P.; Uddin, M.S.; Kim, H. New Aspects of Monoamine Oxidase B Inhibitors: The Key Role of Halogens to Open the Golden Door. Curr. Med. Chem. 2021, 28, 266–283. [Google Scholar] [CrossRef] [PubMed]
- Alkorta, I.; Elguero, J.; Frontera, A. Not Only Hydrogen Bonds: Other Noncovalent Interactions. Crystals 2020, 10, 180. [Google Scholar] [CrossRef] [Green Version]
- Borhani, S.; Mozdarani, H.; Babalui, S.; Bakhshandeh, M.; Nosrati, H. In vitro Radiosensitizing Effects of Temozolomide on U87MG Cell Lines of Human Glioblastoma Multiforme. Iran J. Med. Sci. 2017, 42, 258–265. [Google Scholar]


| Parameters | [o-COSAN]− | [8,8′-I2-o-COSAN]− |
|---|---|---|
| Size (nm) | 1.1 × 0.6 | 1.1 × 0.8 |
| Molecular weight of the anion | 323.75 | 575.54 |
| Rotamer | Cisoid | Transoid |
| Intramolecular interactions | No | Cc-H I |
| Intermolecular interactions in aqueous solution | Yes | Yes |
| Aggregates formation in H2O | Yes [34,51] | Yes [33,51] |
| DLS | Aggregates (d = 64 nm) in the range 1 < c < 29 mM. Aggregates (d = 1.4 nm) c > 29 mM. | Aggregates (d = 107 nm) in the range 1 < c < 110 mM. Aggregates (d = 1.1 nm) at c > 110 mM. |
| Solubility in H2O (mM) | 1509 [32] | 210 [32] |
| logS | 3.18 | 2.32 |
| Lipophilicity (P) | 43.7 | 151.0 |
| logP | 1.64 | 2.18 |
| E1/2 M3+/2+ (in V reference Fc+/Fc) | −2.10 | −1.47 |
| Incubation Time | U87 | T98G | ||
|---|---|---|---|---|
| [o-COSAN]− | [8,8′-I2-o-COSAN]− | [o-COSAN]− | [8,8′-I2-o-COSAN]− | |
| 6 h | 222 ± 127 | 141 ± 85 | 368 ± 202 | 157 ± 84 |
| 24 h | 186 ± 93 | 102 ± 62 | 148 ± 57 | 59 ± 17 |
| 48 h | 127 ± 52 | 51 ± 15 | 57 ± 20 | 24 ± 10 |
| 72 h | 84 ± 31 | 36 ± 15 | 14 ± 8 | 14 ± 6 |
| Concentration (μM) | U87 | T98G | ||
|---|---|---|---|---|
| [o-COSAN]− | [8,8′-I2-o-COSAN]− | [o-COSAN]− | [8,8′-I2-o-COSAN]− | |
| <IC50 | 40 | 35 | 7 | 7 |
| IC50 * | 80 | 50 | 14 | 14 |
| >IC50 | 100 | 100 | 19 | 19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nuez-Martinez, M.; Pinto, C.I.G.; Guerreiro, J.F.; Mendes, F.; Marques, F.; Muñoz-Juan, A.; Xavier, J.A.M.; Laromaine, A.; Bitonto, V.; Protti, N.; et al. Cobaltabis(dicarbollide) ([o-COSAN]−) as Multifunctional Chemotherapeutics: A Prospective Application in Boron Neutron Capture Therapy (BNCT) for Glioblastoma. Cancers 2021, 13, 6367. https://doi.org/10.3390/cancers13246367
Nuez-Martinez M, Pinto CIG, Guerreiro JF, Mendes F, Marques F, Muñoz-Juan A, Xavier JAM, Laromaine A, Bitonto V, Protti N, et al. Cobaltabis(dicarbollide) ([o-COSAN]−) as Multifunctional Chemotherapeutics: A Prospective Application in Boron Neutron Capture Therapy (BNCT) for Glioblastoma. Cancers. 2021; 13(24):6367. https://doi.org/10.3390/cancers13246367
Chicago/Turabian StyleNuez-Martinez, Miquel, Catarina I. G. Pinto, Joana F. Guerreiro, Filipa Mendes, Fernanda Marques, Amanda Muñoz-Juan, Jewel Ann Maria Xavier, Anna Laromaine, Valeria Bitonto, Nicoletta Protti, and et al. 2021. "Cobaltabis(dicarbollide) ([o-COSAN]−) as Multifunctional Chemotherapeutics: A Prospective Application in Boron Neutron Capture Therapy (BNCT) for Glioblastoma" Cancers 13, no. 24: 6367. https://doi.org/10.3390/cancers13246367
APA StyleNuez-Martinez, M., Pinto, C. I. G., Guerreiro, J. F., Mendes, F., Marques, F., Muñoz-Juan, A., Xavier, J. A. M., Laromaine, A., Bitonto, V., Protti, N., Crich, S. G., Teixidor, F., & Viñas, C. (2021). Cobaltabis(dicarbollide) ([o-COSAN]−) as Multifunctional Chemotherapeutics: A Prospective Application in Boron Neutron Capture Therapy (BNCT) for Glioblastoma. Cancers, 13(24), 6367. https://doi.org/10.3390/cancers13246367








