Subcellular Expression of Maspin in Colorectal Cancer: Friend or Foe
Simple Summary
Abstract
1. Introduction
2. General Data about Maspin
3. Maspin Expression in Malignant Tumors
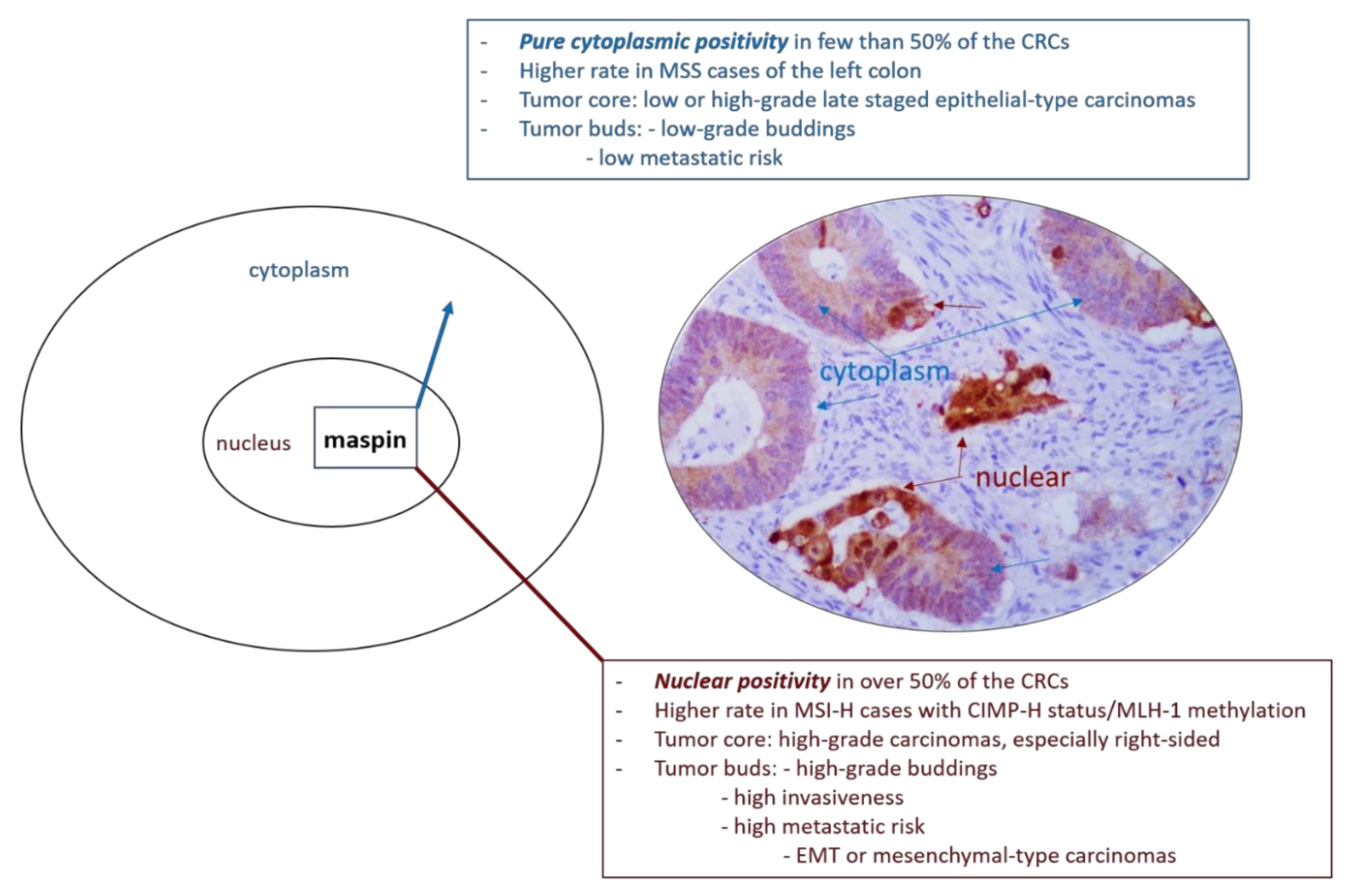
4. Maspin and CRC Budding Degree
5. Maspin and EMT Phenomena
6. Maspin and Molecular Pathways of Colorectal Carcinogenesis
6.1. Maspin and Microsatellite Status
6.2. Maspin and the Serrated Pathway
6.3. Maspin and Colorectal Carcinogenesis via Idiopathic Inflammatory Bowel Disease (IBD)
7. Predictive Value of the Subcellular Maspin Expression
7.1. Maspin and 5-Fluorouracil (5-FU)
7.2. Maspin and Anti-Epidermal Growth Factor Receptor (Anti-EGFR) Therapy
7.3. Maspin and Anti-Angiogenic Targeted Therapy
7.4. Maspin and Immune Checkpoint Blockade
8. Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lugli, A.; Zlobec, I.; Berger, M.D.; Kirsch, R.; Nagtegaal, I.D. Tumour budding in solid cancers. Nat. Rev. Clin. Oncol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Banias, L.; Jung, I.; Bara, T.; Fulop, Z.; Simu, P.; Simu, I.; Satala, C.; Gurzu, S. Immunohistochemical-based molecular subtyping of colorectal carcinoma using maspin and markers of epithelial-mesenchymal transition. Oncol. Lett. 2020, 19, 1487–1495. [Google Scholar] [CrossRef] [PubMed]
- Gurzu, S.; Jung, I. Aberrant pattern of the cytokeratin 7/cytokeratin 20 immunophenotype in colorectal adenocarcinomas with BRAF mutations. Pathol. Res. Pract. 2012, 208, 163–166. [Google Scholar] [CrossRef]
- Tanaka, A.; Wang, J.Y.; Shia, J.; Zhou, Y.; Ogawa, M.; Hendrickson, R.C.; Klimstra, D.S.; Roehrl, M.H.A. Maspin as a prognostic marker for early stage colorectal cancer with microsatellite instability. Front. Oncol. 2020, 10, 945. [Google Scholar] [CrossRef] [PubMed]
- Zou, Z.; Anisowicz, A.; Hendrix, M.J.; Thor, A.; Neveu, M.; Sheng, S.; Rafidi, K.; Seftor, E.; Sager, R. Maspin, a serpin with tumor-suppressing activity in human mammary epithelial cells. Science 1994, 263, 526–529. [Google Scholar] [CrossRef]
- Banias, L.; Jung, I.; Gurzu, S. Subcellular expression of maspin—from normal tissue to tumor cells. World J. Meta-Anal. 2019, 7, 142–155. [Google Scholar] [CrossRef]
- Bodenstine, T.M.; Seftor, R.E.; Khalkhali-Ellis, Z.; Seftor, E.A.; Pemberton, P.A.; Hendrix, M.J. Maspin: Molecular mechanisms and therapeutic implications. Cancer Metastasis Rev. 2012, 31, 529–551. [Google Scholar] [CrossRef]
- Fitzpatrick, P.A.; Wong, D.T.; Barr, P.J.; Pemberton, P.A. Functional implications of the modeled structure of maspin. Protein Eng. 1996, 9, 585–589. [Google Scholar] [CrossRef]
- Baek, J.Y.; Yeo, H.Y.; Chang, H.J.; Kim, K.H.; Kim, S.Y.; Park, J.W.; Park, S.C.; Choi, H.S.; Kim, D.Y.; Oh, J.H. Serpin B5 is a CEA-interacting biomarker for colorectal cancer. Int. J. Cancer 2014, 134, 1595–1604. [Google Scholar] [CrossRef]
- Li, Z.; Shi, H.Y.; Zhang, M. Targeted expression of maspin in tumor vasculatures induces endothelial cell apoptosis. Oncogene 2005, 24, 2008–2019. [Google Scholar] [CrossRef][Green Version]
- Banias, L.; Gurzu, S.; Kovacs, Z.; Bara, T.; Bara, T., Jr.; Jung, I. Nuclear maspin expression: A biomarker for budding assessment in colorectal cancer specimens. Pathol. Res. Pract. 2017, 213, 1227–1230. [Google Scholar] [CrossRef] [PubMed]
- Tamazato Longhi, M.; Cella, N. Tyrosine phosphorylation plays a role in increasing maspin protein levels and its cytoplasmic accumulation. FEBS Open Bio 2012, 2, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, N.; Hoover, B.; Rajendram, M.; Shi, H.Y.; Kawasaki, K.; Weibel, D.B.; Zhang, M. Maspin binds to cardiolipin in mitochondria and triggers apoptosis. FASEB J. 2019, 33, 6354–6364. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Zheng, G.; Liu, H.; Cao, J.; Liu, W.; Li, Y.; Qiao, F.; Deng, D.; Wu, Y. Vascular endothelial growth factor C participates in regulation of maspin in extravillous trophoblast cell migration and invasion. Reprod. Fertil. Dev. 2019, 31, 1410–1418. [Google Scholar] [CrossRef] [PubMed]
- Besgen, P.; Trommler, P.; Vollmer, S.; Prinz, J.C. Ezrin, maspin, peroxiredoxin 2, and heat shock protein 27: Potential targets of a streptococcal-induced autoimmune response in psoriasis. J. Immunol. 2010, 184, 5392–5402. [Google Scholar] [CrossRef] [PubMed]
- Gurzu, S.; Szentirmay, Z.; Popa, D.; Jung, I. Practical value of the new system for Maspin assessment, in colorectal cancer. Neoplasma 2013, 60, 373–383. [Google Scholar] [CrossRef][Green Version]
- Khorsandi, L.; Farasat, M. Zinc oxide nanoparticles enhance expression of maspin in human breast cancer cells. Environ. Sci. Pollut. Res. Int. 2020, 27, 38300–38310. [Google Scholar] [CrossRef]
- Takeda, C.; Takagi, Y.; Shiomi, T.; Nosaka, K.; Yamashita, H.; Osaki, M.; Endo, K.; Minamizaki, T.; Teshima, R.; Nagashima, H.; et al. Cytoplasmic maspin expression predicts poor prognosis of patients with soft tissue sarcomas. Diagn. Pathol. 2014, 9, 205. [Google Scholar] [CrossRef][Green Version]
- Martinoli, C.; Gandini, S.; Luise, C.; Mazzarol, G.; Confalonieri, S.; Pelicci, P.G.; Testori, A.; Ferrucci, P.F. Maspin expression and melanoma progression: A matter of sub-cellular localization. Mod. Pathol. 2014, 27, 412–419. [Google Scholar] [CrossRef][Green Version]
- Gurzu, S.I.; Sugimura, H.; Stefan-van Staden, R.I.; Yamada, H.; Natsume, H.; Iwashita, Y.; Szodorai, R.; Szederjesi, J. Maspin subcellular expression of wild-type- and mutant TP53 gastric cancers. World. J. Gastrointest. Oncol. 2020, 12, 741–755. [Google Scholar] [CrossRef]
- Lin, Y.H.; Tsui, K.H.; Chang, K.S.; Hou, C.P.; Feng, T.H.; Juang, H.H. Maspin is a PTEN-Upregulated and p53-Upregulated Tumor Suppressor Gene and Acts as an HDAC1 Inhibitor in Human Bladder Cancer. Cancers 2019, 12, 10. [Google Scholar] [CrossRef] [PubMed]
- Murnyak, B.; Hortobagyi, T. Immunohistochemical correlates of TP53 somatic mutations in cancer. Oncotarget 2016, 7, 64910–64920. [Google Scholar] [CrossRef] [PubMed]
- Pasz-Walczak, G.; Salagacka, A.; Potemski, P.; Balcerczak, E.; Kordek, R.; Mirowski, M. Maspin and Nm23-H1 expression in colorectal cancer. Neoplasma 2010, 57, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Gurzu, S.; Szentirmay, Z.; Jung, I. Molecular classification of colorectal cancer: A dream that can become a reality. Rom. J. Morphol. Embryol. 2013, 54, 241–245. [Google Scholar]
- Gurzu, S.; Kadar, Z.; Sugimura, H.; Orlowska, J.; Bara, T.; Bara, T., Jr.; Szederjesi, J.; Jung, I. Maspin-related orchestration of aggressiveness of gastric cancer. Appl. Immunohistochem. Mol. Morphol. 2016, 24, 326–336. [Google Scholar] [CrossRef]
- Snoeren, N.; Emmink, B.L.; Koerkamp, M.J.; van Hooff, S.R.; Goos, J.A.; van Houdt, W.J.; de Wit, M.; Prins, A.M.; Piersma, S.R.; Pham, T.V.; et al. Maspin is a marker for early recurrence in primary stage III and IV colorectal cancer. Br. J. Cancer 2013, 109, 1636–1647. [Google Scholar] [CrossRef]
- Markl, B.; Arnholdt, H.M.; Jahnig, H.; Schenkirsch, G.; Herrmann, R.A.; Haude, K.; Spatz, H.; Anthuber, M.; Schlimok, G.; Oruzio, D. Shift from cytoplasmic to nuclear maspin expression correlates with shorter overall survival in node-negative colorectal cancer. Hum. Pathol. 2010, 41, 1024–1033. [Google Scholar] [CrossRef]
- Yang, Q.; Roehrl, M.H.; Wang, J.Y. Proteomic profiling of antibody inducing immunogens in tumor tissue identifies PSMA1, LAP3, ANXA3, and maspin as colon cancer markers. Oncotarget 2017, 9, 3996–4019. [Google Scholar] [CrossRef]
- Wang, Y.; Sun, L.; Song, Z.; Wang, D.; Bao, Y.; Li, Y. Maspin inhibits macrophage phagocytosis and enhances inflammatory cytokine production via activation of NF-κB signaling. Mol. Immunol. 2017, 82, 94–103. [Google Scholar] [CrossRef]
- De Smedt, L.; Palmans, S.; Andel, D.; Govaere, O.; Boeck, B.; Smeets, D.; Galle, E.; Wouters, J.; Barras, D.; Suffiotti, M.; et al. Expression profiling of budding cells in colorectal cancer reveals an EMT-like phenotype and molecular subtype switching. Br. J. Cancer 2017, 116, 58–65. [Google Scholar] [CrossRef]
- Bokhorst, J.M.; Blank, A.; Lugli, A.; Zlobec, I.; Dawson, H.; Vieth, M.; Rijstenberg, L.L.; Brockmoeller, S.; Urbanowicz, M.; Flejou, J.F.; et al. Assessment of individual tumor buds using keratin immunohistochemistry: Moderate interobserver agreement suggests a role for machine learning. Mod. Pathol. 2020, 33, 825–833. [Google Scholar] [CrossRef] [PubMed]
- Gurzu, S.; Serester, O.; Jung, I. Possible neuroendocrine phenotype of poorly differentiated cell clusters in colorectal carcinoma, as a prognostic parameter. Am. J. Surg. Pathol. 2014, 38, 143–144. [Google Scholar] [CrossRef] [PubMed]
- Polari, L.; Alam, C.M.; Nyström, J.H.; Heikkilä, T.; Tayyab, M.; Baghestani, S.; Toivola, D.M. Keratin intermediate filaments in the colon: Guardians of epithelial homeostasis. Int. J. Biochem. Cell Biol. 2020, 129, 105878. [Google Scholar] [CrossRef] [PubMed]
- Nagata, K.; Shinto, E.; Yamadera, M.; Shiraishi, T.; Kajiwara, Y.; Okamoto, K.; Mochizuki, S.; Hase, K.; Kishi, Y.; Ueno, H. Prognostic and predictive values of tumour budding in stage IV colorectal cancer. BJS Open 2020, 4, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Bettstetter, M.; Woenckhaus, M.; Wild, P.J.; Rummele, P.; Blaszyk, H.; Hartmann, A.; Hofstadter, F.; Dietmaier, W. Elevated nuclear maspin expression is associated with microsatellite instability and high tumour grade in colorectal cancer. J. Pathol. 2005, 205, 606–614. [Google Scholar] [CrossRef]
- Bhattacharyya, S.; Feferman, L.; Han, X.; Xia, K.; Zhang, F.; Linhardt, R.J.; Tobacman, J.K. Increased CHST15 follows decline in arylsulfatase B (ARSB) and disinhibition of non-canonical WNT signaling: Potential impact on epithelial and mesenchymal identity. Oncotarget 2020, 11, 2327–2344. [Google Scholar] [CrossRef]
- Kovacs, Z.; Jung, I.; Szalman, K.; Banias, L.; Bara, T.J.; Gurzu, S. Interaction of arylsulfatases A and B with maspin: A possible explanation for dysregulation of tumor cell metabolism and invasive potential of colorectal cancer. World. J. Clin. Cases 2019, 7, 3990–4003. [Google Scholar] [CrossRef]
- Gurzu, S.; Ciortea, D.; Ember, I.; Jung, I. The possible role of Mena protein and its splicing-derived variants in embryogenesis, carcinogenesis, and tumor invasion: A systematic review of the literature. Biomed. Res. Int. 2013, 2013, 365192. [Google Scholar] [CrossRef]
- Fung, C.L.; Chan, C.; Jankova, L.; Dent, O.F.; Robertson, G.; Molloy, M.; Bokey, L.; Chapuis, P.H.; Lin, B.P.; Clarke, S.J. Clinicopathological correlates and prognostic significance of maspin expression in 450 patients after potentially curative resection of node-positive colonic cancer. Histopathology 2010, 56, 319–330. [Google Scholar] [CrossRef]
- Umekita, Y.; Souda, M.; Yoshida, H. Expression of maspin in colorectal cancer. In Vivo 2006, 20, 797–800. [Google Scholar]
- Gurzu, S.; Fetyko, A.M.; Bara, T.; Banias, L.; Butiurca, V.O.; Bara, T., Jr.; Tudorache, V.; Jung, I. Gastrointestinal mixed adenoneuroendocrine carcinoma (MANEC): An immunohistochemistry study of 13 microsatellite stable cases. Pathol. Res. Pract. 2019, 215, 152697. [Google Scholar] [CrossRef] [PubMed]
- Gurzu, S.; Kadar, Z.; Bara, T.; Bara, T., Jr.; Tamasi, A.; Azamfirei, L.; Jung, I. Mixed adenoneuroendocrine carcinoma (MANEC) of gastrointestinal tract: Report of two cases and review of the literature. World. J. Gastroenterol. 2015, 21, 1329–1333. [Google Scholar] [CrossRef] [PubMed]
- Gurzu, S.; Copotoiu, C.; Tugui, A.; Kwizera, C.; Szodorai, R.; Jung, I. Primary gastric choriocarcinoma—a rare and aggressive tumor with multilineage differentiation: A case report. World. J. Clin. Cases 2019, 7, 1837–1843. [Google Scholar] [CrossRef] [PubMed]
- Turdean, S.G.; Gurzu, S.; Jung, I.; Neagoe, R.M.; Sala, D. Unexpected maspin immunoreactivity in Merkel cell carcinoma. Diagn. Pathol. 2015, 10, 206. [Google Scholar] [CrossRef]
- Gurzu, S.; Bara, T.; Molnar, C.; Bara, T., Jr.; Butiurca, V.; Beres, H.; Savoji, S.; Jung, I. The epithelial-mesenchymal transition induces aggressivity of mucinous cystic neoplasm of the pancreas with neuroendocrine component: An immunohistochemistry study. Pathol. Res. Pract. 2019, 215, 82–89. [Google Scholar] [CrossRef]
- Kim, J.H.; Cho, N.Y.; Bae, J.M.; Kim, K.J.; Rhee, Y.Y.; Lee, H.S.; Kang, G.H. Nuclear maspin expression correlates with the CpG island methylator phenotype and tumor aggressiveness in colorectal cancer. Int. J. Clin. Exp. Pathol. 2015, 8, 1920–1928. [Google Scholar]
- Gurzu, S.; Szentirmay, Z.; Toth, E.; Bara, T.; Bara, T., Jr.; Jung, I. Serrated pathway adenocarcinomas: Molecular and immunohistochemical insights into their recognition. PLoS ONE 2013, 8, e57699. [Google Scholar] [CrossRef]
- Rubio, C.A.; Kaufeldt, A.; Bjork, J.; Jaramillo., E. Maspin, a marker of serrated colorectal polyps. Anticancer Res. 2015, 35, 4139–4144. [Google Scholar]
- Rubio, C.A.; Schmidt, P.T. Asymmetric crypt fission in sessile serrated lesions. J. Clin. Pathol. 2020. [Google Scholar] [CrossRef]
- Cao, D.; Wilentz, R.E.; Abbruzzese, J.L.; Ho, L.; Maitra, A. Aberrant expression of maspin in idiopathic inflammatory bowel disease is associated with disease activity and neoplastic transformation. Int. J. Gastrointest. Cancer 2005, 36, 39–46. [Google Scholar] [CrossRef]
- Cheng, L.; Li, L.; Liu, C.; Yan, S.; Li, Y. Meta-analysis of anti-Saccharomyces cerevisiae antibodies as diagnostic markers of Behçet’s disease with gastrointestinal involvement. BMJ Open 2020, 10, e033880. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Silva, M.; Afonso, P.C.; de Souza, P.R.; Peghini, B.C.; Rodrigues-Junior, V.; de Barros Cardoso, C.R. Reappraisal of antibodies against Saccharomyces cerevisiae (ASCA) as persistent biomarkers in quiescent Crohn’s disease. Autoimmunity 2019, 52, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Boltze, C. Loss of maspin is a helpful prognosticator in colorectal cancer: A tissue microarray analysis. Pathol. Res. Pract. 2005, 200, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Gurzu, S.; Szentirmay, Z.; Toth, E.; Jung, I. Possible predictive value of Maspin expression in colorectal cancer. Recent. Pat. Anti-Cancer Drug. Discov. 2013, 8, 183–190. [Google Scholar] [CrossRef]
- Berardi, R.; Morgese, F.; Onofri, A.; Mazzanti, P.; Pistelli, M.; Ballatore, Z.; Savini, A.; De Lisa, M.; Caramanti, M.; Rinaldi, S.; et al. Role of maspin in cancer. Clin. Transl. Med. 2013, 2, 8. [Google Scholar] [CrossRef]
- Song, S.Y.; Lee, S.K.; Kim, D.H.; Son, H.J.; Kim, H.J.; Lim, Y.J.; Lee, W.Y.; Chun, H.K.; Rhee, J.C. Expression of maspin in colon cancers: Its relationship with p53 expression and microvessel density. Dig. Dis. Sci. 2002, 47, 1831–1835. [Google Scholar] [CrossRef]
- Chang, I.W.; Liu, K.W.; Ragunanan, M.; He, H.L.; Shiue, Y.L.; Yu, S.C. SERPINB5 Expression: Association with CCRT Response and Prognostic Value in Rectal Cancer. Int. J. Med. Sci. 2018, 15, 376–384. [Google Scholar] [CrossRef]
- Dietmaier, W.; Bettstetter, M.; Wild, P.J.; Woenckhaus, M.; Rummele, P.; Hartmann, A.; Dechant, S.; Blaszyk, H.; Pauer, A.; Klinkhammer-Schalke, M.; et al. Nuclear Maspin expression is associated with response to adjuvant 5-fluorouracil based chemotherapy in patients with stage III colon cancer. Int. J. Cancer 2006, 118, 2247–2254. [Google Scholar] [CrossRef]
- Hestetun, K.E.; Brydoy, M.; Myklebust, M.P.; Dahl, O. Nuclear maspin expression as a predictive marker for fluorouracil treatment response in colon cancer. Acta. Oncol. 2015, 54, 470–479. [Google Scholar] [CrossRef]
- Boidot, R.; Chevrier, S.; Julie, V.; Ladoire, S.; Ghiringhelli, F. HRAS G13D, a new mutation implicated in the resistance to anti-EGFR therapies in colorectal cancer, a case report. Int. J. Colorectal. Dis. 2016, 31, 1245–1246. [Google Scholar] [CrossRef]
- Ku, B.M.; Choi, M.K.; Sun, J.M.; Lee, S.H.; Ahn, J.S.; Park, K.; Ahn, M.J. Acquired resistance to AZD9291 as an upfront treatment is dependent on ERK signaling in a preclinical model. PLoS ONE 2018, 13, e0194730. [Google Scholar] [CrossRef]
- Shi, P.; Oh, Y.T.; Zhang, G.; Yao, W.; Yue, P.; Li, Y.; Kanteti, R.; Riehm, J.; Salgia, R.; Owonikoko, T.K.; et al. Met gene amplification and protein hyperactivation is a mechanism of resistance to both first and third generation EGFR inhibitors in lung cancer treatment. Cancer Lett. 2016, 380, 494–504. [Google Scholar] [CrossRef] [PubMed]
- Gurzu, S.; Jung, J.; Azamfirei, L.; Mezei, T.; Cîmpean, A.M.; Szentirmay, Z. The angiogenesis in colorectal carcinomas with and without lymph node metastases. Rom. J. Morphol. Embryol. 2008, 49, 149–152. [Google Scholar] [PubMed]
- Morfoisse, F.; Kuchnio, A.; Frainay, C.; Gomez-Brouchet, A.; Delisle, M.B.; Marzi, S.; Helfer, A.C.; Hantelys, F.; Pujol, F.; Guillermet-Guibert, J.; et al. Hypoxia induces VEGF-C expression in metastatic tumor cells via a HIF-1α-independent translation-mediated mechanism. Cell Rep. 2014, 6, 155–167. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, S.; Tobacman, J.K. Hypoxia reduces arylsulfatase B activity and silencing arylsulfatase B replicates and mediates the effects of hypoxia. PLoS ONE 2012, 7, e33250. [Google Scholar] [CrossRef] [PubMed]
- Dzinic, S.H.; Bernardo, M.M.; Oliveira, D.S.; Wahba, M.; Sakr, W.; Sheng, S. Tumor suppressor maspin as a modulator of host immune response to cancer. Bosn. J. Basic Med. Sci. 2015, 15, 1–6. [Google Scholar] [CrossRef]
| Authors, Year [Reference] | No. of Carcinomas and Selection Criteria | Cytoplasmic Expression | Nuclear Expression | Prognostic/Predictive Value of Maspin |
|---|---|---|---|---|
| Boltze et al., 2005 [53] | n = 280 (colon); stages I-IV—TMA blocks-0.6 mm cores | 69% of the cases—cytoplasmic or nuclear; loss of expression—left-sided high-grade (G3) metastatic tumors | Not reported | Cytoplasmic overexpression—suppressive role—better prognosis; loss of expression—short OS |
| Bettstetter et al., 2005 [35] | n = 200 (colon and rectum); 41 MSI and 159 MSS (TMA blocks-2 mm) | 72% in MSS/MSI-L and 78% in MSI-H, upregulated in well-differentiated carcinomas (G1) | 50% in MSS/MSI-L and 73% in MSI-H; upregulated in high-grade (G3) carcinomas, especially in the invasion front | Cytoplasmic expression—tumor suppression role; Nuclear positivity—tumor progression |
| Dietmaier et al., 2006 [58] | n = 172 (colon); stage III—before and after 5-FU based chemotherapy | 71.5%—no correlation with any of the examined parameters | 52.3%—Upregulated in MSI vs. MSS cases and in high-grade (G3) carcinomas | Nuclear overexpression in MSS cases—independent adverse prognostic factor for OS but highly predictive of 5-FU chemotherapy |
| Umekita et al., 2006 [40] | n = 104 (colon and rectum); stages I–III (whole section) | 66% of the cases-correlation with high tumor stage and high budding degree (>9 foci in a field) | Not reported | Cytoplasmic expression—aggressive phenotype but not indicator of OS |
| Markl et al., 2010 [27] | n = 156 (colon and rectum); stages I/II (TMA blocks-2 mm) | Correlation with high tumor grade (72% of the cases) | Correlation with high tumor budding (48% of the cases) | Cytoplasmic expression —tumor suppression role; For pT3/stage II cases, pure nuclear expression—worse OS; even worst OS in maspin negative cases |
| Fung et al., 2010 [39] | n = 450 (colon); stage III (TMA blocks-1 mm) | 80%—Correlation with right-sided high-grade carcinomas | 79%—Correlation with right-sided high-grade carcinomas with at least 4 metastatic lymph nodes | Not independent prognostic value |
| Hestetun et al., 2010 [59] | n = 380 (colon and rectum); stages II/III (TMA blocks)—before and after chemotherapy | 23% of the cases—without other details | 99%—in colon cancers, upregulation after chemotherapy | For colon cancer, nuclear overexpression—resistance to 5-FU/Lev chemotherapy and, after chemotherapy, low DFS and CSS; no prognostic or predictive value for rectal carcinomas |
| Pasz-Walczak et al., 2010 [23] | n = 102 (colon and rectum); stages I–IV (whole section) | 88% of the cases—correlated with high tumor grade (G3), advanced stage, presence of metastases | 58.82%—no correlation with any of the examined parameters | Cytoplasmic overexpression—poor prognosis |
| Gurzu et al., 2013 [16] | n = 121 (colon and rectum); 43 stages I/II and 78 stages III/IV (whole section) | 44%—cytoplasmic predominance; associated with low budding degree (<5 foci in a field) and p53 negativity, more frequent in distal colon | 24%—nuclear predominance and 23% with associated cytoplasmic positivity—mixed expression (40% in MSI cases); nuclear predominance—p53 positive highly angiogenic tumors | Cytoplasmic or mixed expression—better prognosis; nuclear predominance or loss of positivity—low OS; mixed expression in MSI cases—better prognosis; |
| Baek et al., 2014 [9] | n = 377 (colon); 147 stage I/II and 230 stage III/IV | Correlated with high tumor grade (G3), advanced stage, high budding degree, and lymph node metastases, especially if associates nuclear positivity | Correlation with cytoplasmic expression and more expressed on the right-sided colon cancer | Overexpression—reduced DFS and OS, in correlation with CEA serum level |
| Snoeren et al., 2015 [26] | n = 419 (colon and rectum): 243 stage II and 166 stage III (TMA blocks-0.6 mm)—before and after chemotherapy | Correlated with right-sided location, high tumor grade (G3), mucinous differentiation and MSI status, especially if associates nuclear positivity | 0.95% | Mixed overexpression—independent predictor of recurrence, lymphatic spread and DFS in stages III and IV but not stage II |
| Kim et al., 2015 [46] | n = 216 MSI-H carcinomas: 139 stages I/II and 77 stage III/IV (TMA blocks-2 mm) | Not reported | 51%—associated with CIMP-H status, MLH-1 methylation, advanced stage, metastatic status, high tumor budding | Nuclear overexpression—worse DFS but not independent prognostic value |
| Tanaka et al., 2020 [4] | n = 743 (colon); 628 stages I/II and 115 stages III/IV (TMA blocks-2 mm) | Correlation with advanced stage and MSI status (16.4% and 57.4% in early vs. late stages; 22.3% vs. 13.9% in MSI vs. MSS carcinomas) | Correlation with MSI status (22.1% vs. 22.6% in early vs. late stages; 36.9% vs. 19.3% in MSI vs. MSS carcinomas) | Overexpression in MSI early-staged CRCs—better prognosis |
| Banias et al., 2020 [2] | n = 112 (colon and rectum); stages I–III (whole section); 100/112 cases were MSS | 52.7% in tumor core and 19.6% in buds—more frequent in low-grade budding non-metastatic epithelial-type carcinomas with LNR ≤ 0.15 | 27.7% in tumor core and 60.8% in buds—associated with high-grade budding, lymph node metastases, mesenchymal-type carcinomas | Cytoplasmic expression—better OS but not independent prognostic value |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gurzu, S.; Jung, I. Subcellular Expression of Maspin in Colorectal Cancer: Friend or Foe. Cancers 2021, 13, 366. https://doi.org/10.3390/cancers13030366
Gurzu S, Jung I. Subcellular Expression of Maspin in Colorectal Cancer: Friend or Foe. Cancers. 2021; 13(3):366. https://doi.org/10.3390/cancers13030366
Chicago/Turabian StyleGurzu, Simona, and Ioan Jung. 2021. "Subcellular Expression of Maspin in Colorectal Cancer: Friend or Foe" Cancers 13, no. 3: 366. https://doi.org/10.3390/cancers13030366
APA StyleGurzu, S., & Jung, I. (2021). Subcellular Expression of Maspin in Colorectal Cancer: Friend or Foe. Cancers, 13(3), 366. https://doi.org/10.3390/cancers13030366






