Oncological Results of Laparoscopically Assisted Radical Vaginal Hysterectomy in Early-Stage Cervical Cancer: Should We Really Abandon Minimally Invasive Surgery?
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Laparoscopy Procedure: SLN Evaluation, Lymphadenectomy, and Radical Hysterectomy Preparation
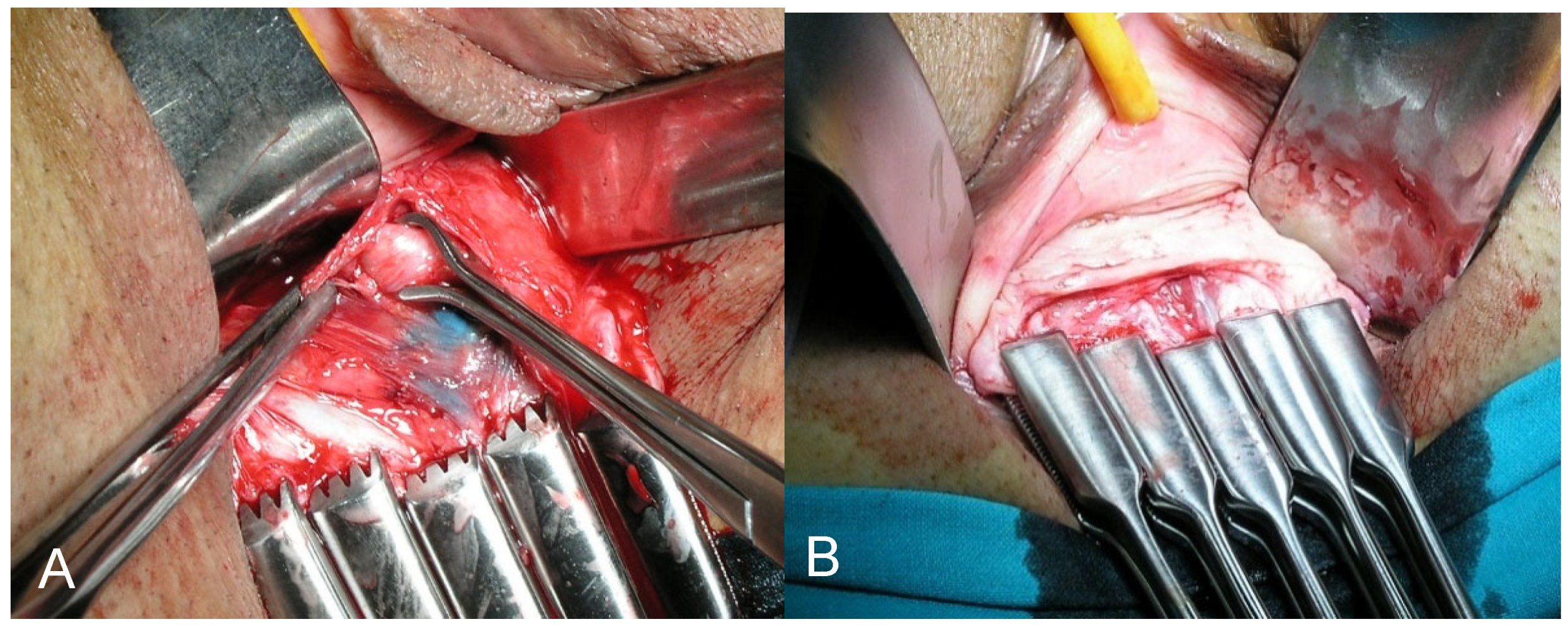
2.3. Vaginal Procedure: Radical Vaginal Hysterectomy
2.4. Adjuvant Treatment and Patient Follow-Up
2.5. Histological SLN Ultrastaging and Evaluation of the Lymphadenectomy Specimens
2.6. Statistical Analysis
3. Results
3.1. General Characteristics
3.2. Surgical Results and Complications
3.3. Follow-Up Data and Survival Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cibula, D.; Pötter, R.; Planchamp, F.; Avall-Lundqvist, E.; Fischerova, D.; Haie Meder, C.; Köhler, C.; Landoni, F.; Lax, S.; Lindegaard, J.C.; et al. The European Society of Gynaecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology guidelines for the management of patients with cervical cancer. Radiother. Oncol. 2018, 127, 404–416. [Google Scholar] [CrossRef] [PubMed]
- Koh, W.; Abu-rustum, N.R.; Bean, S.; Bradley, K.; Campos, S.M.; Cho, K.R.; Chon, H.S.; Chu, C.; Clark, R.; Cohn, D.; et al. Cervical Cancer, Version 3.2019. J. Natl. Compr. Cancer Netw. 2019, 17, 64–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.Z.; Deng, L.; Xu, H.C.; Zhang, Y.; Liang, Z.Q. Laparoscopy versus laparotomy for the management of early stage cervical cancer. BMC Cancer 2015, 15, 928. [Google Scholar] [CrossRef] [Green Version]
- Cao, T.; Feng, Y.; Huang, Q.; Wan, T.; Liu, J. Prognostic and Safety Roles in Laparoscopic Versus Abdominal Radical Hysterectomy in Cervical Cancer: A Meta-analysis. J. Laparoendosc. Adv. Surg. Tech. 2015, 25, 990–998. [Google Scholar] [CrossRef] [Green Version]
- Liu, Z.; Li, X.; Tian, S.; Zhu, T.; Yao, Y.; Tao, Y. Superiority of robotic surgery for cervical cancer in comparison with traditional approaches: A systematic review and meta-analysis. Int. J. Surg. 2017, 40, 145–154. [Google Scholar] [CrossRef]
- Medlin, E.E.; Kushner, D.M.; Barroilhet, L. Robotic surgery for early stage cervical cancer: Evolution and current trends. J. Surg. Oncol. 2015, 112, 772–781. [Google Scholar] [CrossRef] [PubMed]
- Shazly, S.A.M.; Murad, M.H.; Dowdy, S.C.; Gostout, B.S.; Famuyide, A.O. Robotic radical hysterectomy in early stage cervical cancer: A systematic review and meta-analysis. Gynecol. Oncol. 2015, 138, 457–471. [Google Scholar] [CrossRef]
- Lee, E.J.; Kang, H.; Kim, D.H. A comparative study of laparoscopic radical hysterectomy with radical abdominal hysterectomy for early-stage cervical cancer: A long-term follow-up study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 156, 83–86. [Google Scholar] [CrossRef]
- Sert, B.M.; Boggess, J.F.; Ahmad, S.; Jackson, A.L.; Stavitzski, N.M.; Dahl, A.A.; Holloway, R.W. Robot-assisted versus open radical hysterectomy: A multi-institutional experience for early-stage cervical cancer. Eur. J. Surg. Oncol. 2016, 42, 513–522. [Google Scholar] [CrossRef]
- Park, D.A.; Yun, J.E.; Kim, S.W.; Lee, S.H. Surgical and clinical safety and effectiveness of robot-assisted laparoscopic hysterectomy compared to conventional laparoscopy and laparotomy for cervical cancer: A systematic review and meta-analysis. Eur. J. Surg. Oncol. 2017, 43, 994–1002. [Google Scholar] [CrossRef]
- Nevis, I.F.; Vali, B.; Higgins, C.; Dhalla, I.; Urbach, D.; Bernardini, M.Q. Robot-assisted hysterectomy for endometrial and cervical cancers: A systematic review. J. Robot. Surg. 2017, 11, 1–16. [Google Scholar] [CrossRef]
- Ramirez, P.T.; Frumovitz, M.; Pareja, R.; Lopez, A.; Vieira, M.; Ribeiro, R.; Buda, A.; Yan, X.; Shuzhong, Y.; Chetty, N.; et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N. Engl. J. Med. 2018, 379, 1895–1904. [Google Scholar] [CrossRef]
- Melamed, A.; Margul, D.J.; Chen, L.; Keating, N.L.; Del Carmen, M.G.; Yang, J.; Seagle, B.L.L.; Alexander, A.; Barber, E.L.; Rice, L.W.; et al. Survival after Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer. N. Engl. J. Med. 2018, 379, 1905–1914. [Google Scholar] [CrossRef]
- Margul, D.J.; Yang, J.; Seagle, B.L.; Kocherginsky, M.; Shahabi, S. Outcomes and costs of open, robotic, and laparoscopic radical hysterectomy for stage IB1 cervical cancer. J. Clin. Oncol. 2018, 36, 5502. [Google Scholar] [CrossRef]
- NCRAS Cervical Cancer Radical Hysterectomy Analysis. Available online: https://www.bgcs.org.uk/wp-content/uploads/2019/07/NCRAS-cervical-cancer-surgery-analysis-May-2019-final.pdf (accessed on 2 May 2020).
- National Comprehensive Cancer Network Cervical Cancer (Version 1.2021). Available online: https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf (accessed on 29 February 2020).
- Querleu, D.; Cibula, D.; Concin, N.; Fagotti, A.; Ferrero, A.; Fotopoulou, C.; Knapp, P.; Kurdiani, D.; Ledermann, J.A.; Mirza, M.R.; et al. Laparoscopic radical hysterectomy: A European Society of Gynaecological Oncology (ESGO) statement. Int. J. Gynecol. Cancer 2020, 30, 15. [Google Scholar] [CrossRef] [PubMed]
- Kong, T.W.; Chang, S.J.; Piao, X.; Paek, J.; Lee, Y.; Lee, E.J.; Chun, M.; Ryu, H.S. Patterns of recurrence and survival after abdominal versus laparoscopic/robotic radical hysterectomy in patients with early cervical cancer. J. Obstet. Gynaecol. Res. 2016, 42, 77–86. [Google Scholar] [CrossRef]
- Yuan, P.; Liu, Z.; Qi, J.; Yang, X.; Hu, T.; Tan, H. Laparoscopic Radical Hysterectomy with Enclosed Colpotomy and without the Use of Uterine Manipulator for Early-Stage Cervical Cancer. J. Minim. Invasive Gynecol. 2019, 26, 1193–1198. [Google Scholar] [CrossRef]
- Chiva, L.; Zanagnolo, V.; Querleu, D.; Martin-Calvo, N.; Arévalo-Serrano, J.; Căpîlna, M.E.; Fagotti, A.; Kucukmetin, A.; Mom, C.; Chakalova, G.; et al. SUCCOR study: An international European cohort observational study comparing minimally invasive surgery versus open abdominal radical hysterectomy in patients with stage IB1 cervical cancer. Int. J. Gynecol. Cancer 2020, 30, 1269–1277. [Google Scholar] [CrossRef]
- Dargent, D. A new future for Schautas’s operation through presurgical retroperitoneal pelviscopy. Eur. J. Gynaecol. Oncol. 1987, 8, 292–296. [Google Scholar]
- Schauta, F. Die operation des gebaermutterkrebs mittel des schuchardtschen paravaginalschnittes. Monatsschr. Geburtshiffe Gynaekol. 1902, 15, 133–152. [Google Scholar]
- Dargent, D.; Mathevet, P. Hystérectomie élargie laparoscopico-vaginale. J. Gynecol. Obs. Biol. Reprod. 1992, 21, 709–710. [Google Scholar]
- Köhler, C.; Hertel, H.; Herrmann, J.; Marnitz, S.; Mallmann, P.; Favero, G.; Plaikner, A.; Martus, P.; Gajda, M.; Schneider, A. Laparoscopic radical hysterectomy with transvaginal closure of vaginal cuff-a multicenter analysis. Int. J. Gynecol. Cancer 2019, 29, 845–850. [Google Scholar] [CrossRef]
- Pahisa, J.; Martínez-Román, S.; Torné, A.; Fusté, P.; Alonso, I.; Lejárcegui, J.A.; Balasch, J. Comparative study of laparoscopically assisted radical vaginal hysterectomy and open wertheim-meigs in patients with early-stage cervical cancer eleven years of experience. Int. J. Gynecol. Cancer 2010, 20, 173–178. [Google Scholar] [CrossRef]
- Pecorelli, S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int. J. Gynecol. Obstet. 2009, 105, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Dostalek, L.; Åvall-Lundqvist, E.; Creutzberg, C.; Kurdiani, D.; Ponce, J.; Dostalkova, I.; Cibula, D. ESGO Survey on Current Practice in the Management of Cervical Cancer. Int. J. Gynecol. Cancer 2018, 28, 1226–1231. [Google Scholar] [CrossRef] [PubMed]
- Dindo, D.; Demartines, N.; Clavien, P.-A.; Clavien, P.-A. Classification of Surgical Complications A New Proposal With Evaluation in a Cohort of 6336 Patients and Results of a Survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Sedlis, A.; Bundy, B.N.; Rotman, M.Z.; Lentz, S.S.; Muderspach, L.I.; Zaino, R.J. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: A gynecologic oncology group study. Gynecol. Oncol. 1999, 73, 177–183. [Google Scholar] [CrossRef]
- Small, W.; Mell, L.K.; Anderson, P.; Creutzberg, C.; De Los Santos, J.; Gaffney, D.; Jhingran, A.; Portelance, L.; Schefter, T.; Iyer, R.; et al. Consensus Guidelines for Delineation of Clinical Target Volume for Intensity-Modulated Pelvic Radiotherapy in Postoperative Treatment of Endometrial and Cervical Cancer. Int. J. Radiat. Oncol. 2008, 71, 428–434. [Google Scholar] [CrossRef] [Green Version]
- Molina, R.; Filella, X.; Augé, J.M.; Bosch, E.; Torne, A.; Pahisa, J.; Lejarcegui, J.A.; Rovirosa, A. CYFRA 21.1 in Patients with Cervical Cancer: Comparison with SCC and CEA. Anticancer Res. 2005, 25, 1765–1771. [Google Scholar]
- Hertel, H.; Michels, W.; Possover, M.; Tozzi, R.; Schneider, A. Laparoscopic-assisted radical vaginal hysterectomy (LARVH): Prospective evaluation of 200 patients with cervical cancer. Gynecol. Oncol. 2003, 90, 505–511. [Google Scholar] [CrossRef]
- Roy, M.; Plante, M. Place of Schauta’s radical vaginal hysterectomy. Best Pract. Res. Clin. Obstet. Gynaecol. 2011, 25, 227–237. [Google Scholar] [CrossRef]
- Zhang, S.; Wang, S.; Lv, A.; Huang, S. Laparoscopically Assisted Radical Vaginal Hysterectomy for Early-Stage Cervical Cancer. Int. J. Gynecol. Cancer 2016, 26, 1497–1502. [Google Scholar] [CrossRef]
- Kucukmetin, A.; Biliatis, I.; Naik, R.; Bryant, A. Laparoscopically assisted radical vaginal hysterectomy versus radical abdominal hysterectomy for the treatment of early cervical cancer. Cochrane Database Syst. Rev. 2013, 2013. [Google Scholar] [CrossRef]
- Shekhar, S.; Jeyaseelan, L. Laparoscopic or Open Radical Hysterectomy for Early Stage Cancer Cervix: Data Inconsistency of LACC Trial. Asian Pac. J. Cancer Prev. 2019, 20, 2881. [Google Scholar] [CrossRef] [PubMed]
- Brandt, B.; Sioulas, V.; Basaran, D.; Kuhn, T.; LaVigne, K.; Gardner, G.J.; Sonoda, Y.; Chi, D.S.; Long Roche, K.C.; Mueller, J.J.; et al. Minimally invasive surgery versus laparotomy for radical hysterectomy in the management of early-stage cervical cancer: Survival outcomes. Gynecol. Oncol. 2020, 156, 591–597. [Google Scholar] [CrossRef]
- Leitao, M.M., Jr. The aftershocks of the LACC earthquake have begun: Brace yourselves. Int. J. Gynecol. Cancer 2020, 30, 157–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schneider, A.; Köhler, C. Locoregional recurrence after laparoscopic radical trachelectomy: The vaginal cuff must be closed to avoid tumor cell contamination of the peritoneal cavity. Int. J. Gynecol. Cancer 2015, 25, 550. [Google Scholar] [CrossRef] [PubMed]
- Abdollah, F.; Keeley, J.; Menon, M. Minimally Invasive or Abdominal Radical Hysterectomy for Cervical Cancer. N. Engl. J. Med. 2019, 380, 793. [Google Scholar] [CrossRef] [PubMed]
- Groeben, C.; Koch, R.; Baunacke, M.; Wirth, M.; Huber, J.; Leow, J.; Chang, S. A total population analysis of in-hospital outcomes of radical cystectomy in Germany from 2006 to 2013: Impact of surgical approach and annual caseload volume. J. Urol. 2017, 197, e725. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.; Jin, K.; Lee, S.; Hwa, J.; Yun, J.; Kwan, J.; Woo, N. Learning curve could affect oncologic outcome of minimally invasive radical hysterectomy for cervical cancer. Asian J. Surg. 2020, 44, 174–180. [Google Scholar] [CrossRef]


| Feature | Number (Percentage) |
|---|---|
| FIGO classification * | |
| IA1 + LVSI positive | 0 (0.0%) |
| IA2 | 5 (4.3%) |
| IB1 | 108 (93.9%) |
| IIA1 | 2 (1.7%) |
| Histological type | |
| Adenocarcinoma | 33 (29%) |
| Squamous cell carcinoma | 78 (68%) |
| Other histological types | 4 (3%) |
| Histological grade | |
| Grade 1 | 68 (59%) |
| Grade 2 | 29 (25%) |
| Grade 3 | 18 (16%) |
| Lymphovascular space invasion | 29 (25%) |
| Parametrial involvement | 3 (2.6%) |
| Vaginal involvement | 3 (2.6%) |
| Tumor size | |
| ≤2 cm | 71 (61.7%) |
| >2 cm | 44 (38.3%) |
| Lymph node assessment | |
| Sentinel lymph node biopsy and bilateral pelvic lymphadenectomy | 66 (57.4%) |
| Sentinel lymph node biopsy | 49 (42.6%) |
| Intraoperative complications | 9 (7.8%) |
| Incidental cystostomy | 2 (1.7%) |
| Ureteral injury | 6 (5.2%) |
| Bowel-rectal injury | 1 (0.9%) |
| Conversion to laparotomy | 0 (0.0%) |
| Transfusion requirement | 9 (7.8%) |
| Postoperative complications | 6 (5.2%) |
| Infection (requiring antibiotics) | 5 (4.3%) |
| Wound infection-breakdown | 0 (0%) |
| Venous thromboembolism | 1 (0.9%) |
| Bladder dysfunction | 12 (10.4%) |
| Oncological Outcomes | Variables | HR | 95% CI | p |
|---|---|---|---|---|
| Risk of recurrence | Histology | |||
| Squamous cervical cancer | 1 | |||
| Non squamous cervical cancer | 0.4 | 0.10–2.8 | 0.206 | |
| Tumor size | ||||
| ≤2 cm | 1 | |||
| >2 cm | 1.2 | 0.6–5.93 | 0.824 | |
| Lymph node assessment | ||||
| SLN biopsy | 1 | |||
| SLN biopsy + lymphadenectomy | 1.0 | 0.2–5.8 | 0.963 | |
| Adjuvant treatment | ||||
| No | 1 | |||
| Yes | 4.2 | 0.8–21.5 | 0.080 | |
| Risk of mortality | Histology | |||
| Squamous cervical cancer | 1 | |||
| Nonsquamous cervical cancer | 1.4 | 0.1–13.2 | 0.684 | |
| Tumor size | ||||
| <2 cm | 1 | |||
| >2 cm | 1.5 | 0.2–10.9 | 0.668 | |
| Lymph node assessment | ||||
| SLN biopsy | 1 | |||
| SLN biopsy + Lymphadenectomy | 0.7 | 0.1–7.6 | 0.823 | |
| Adjuvant treatment | ||||
| No | 1 | |||
| Yes | 4.9 | 0.5–47.1 | 0.145 |
| Surgical Approach | Study | n | Follow-Up | Disease-Free Survival | Overall Survival | ||
|---|---|---|---|---|---|---|---|
| 3 Years No. at risk (%) | 4.5 Years No. at Risk (%) | 3 Years No. at Risk (%) | 4.5 Years No. at Risk (%) | ||||
| LPS/robot arm | (LACC trial) [12] | 319 | 30 months | 87.1% 142 (45%) | 86% 80 (25%) | 93.8% 150 (47%) | n/a 87 (27%) |
| Laparotomy arm | (LACC trial) [12] | 312 | 30 months | 97.1% 134 (43%) | 96.5% 90 (29%) | 99% 136 (44%) | n/a 90 (29%) |
| LARVH/VALRH | (Köhler et al.) [24] | 389 | 99 months | 96.8% 305 (78%) | 95.8% 271 (70%) | 98.5% 306 (78%) | 97.8% 273 (70%) |
| LARVH | (present study) | 115 | 87.8 months | 97.7% 86 (77%) | 93.5% 65 (58%) | 97.8% 88 (79%) | 94.8% 66 (59%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torné, A.; Pahisa, J.; Ordi, J.; Fusté, P.; Díaz-Feijóo, B.; Glickman, A.; Paredes, P.; Rovirosa, A.; Gaba, L.; Saco, A.; et al. Oncological Results of Laparoscopically Assisted Radical Vaginal Hysterectomy in Early-Stage Cervical Cancer: Should We Really Abandon Minimally Invasive Surgery? Cancers 2021, 13, 846. https://doi.org/10.3390/cancers13040846
Torné A, Pahisa J, Ordi J, Fusté P, Díaz-Feijóo B, Glickman A, Paredes P, Rovirosa A, Gaba L, Saco A, et al. Oncological Results of Laparoscopically Assisted Radical Vaginal Hysterectomy in Early-Stage Cervical Cancer: Should We Really Abandon Minimally Invasive Surgery? Cancers. 2021; 13(4):846. https://doi.org/10.3390/cancers13040846
Chicago/Turabian StyleTorné, Aureli, Jaume Pahisa, Jaume Ordi, Pere Fusté, Berta Díaz-Feijóo, Ariel Glickman, Pilar Paredes, Angels Rovirosa, Lydia Gaba, Adela Saco, and et al. 2021. "Oncological Results of Laparoscopically Assisted Radical Vaginal Hysterectomy in Early-Stage Cervical Cancer: Should We Really Abandon Minimally Invasive Surgery?" Cancers 13, no. 4: 846. https://doi.org/10.3390/cancers13040846






