Collagen Type XI Alpha 1 (COL11A1): A Novel Biomarker and a Key Player in Cancer
Abstract
:Simple Summary
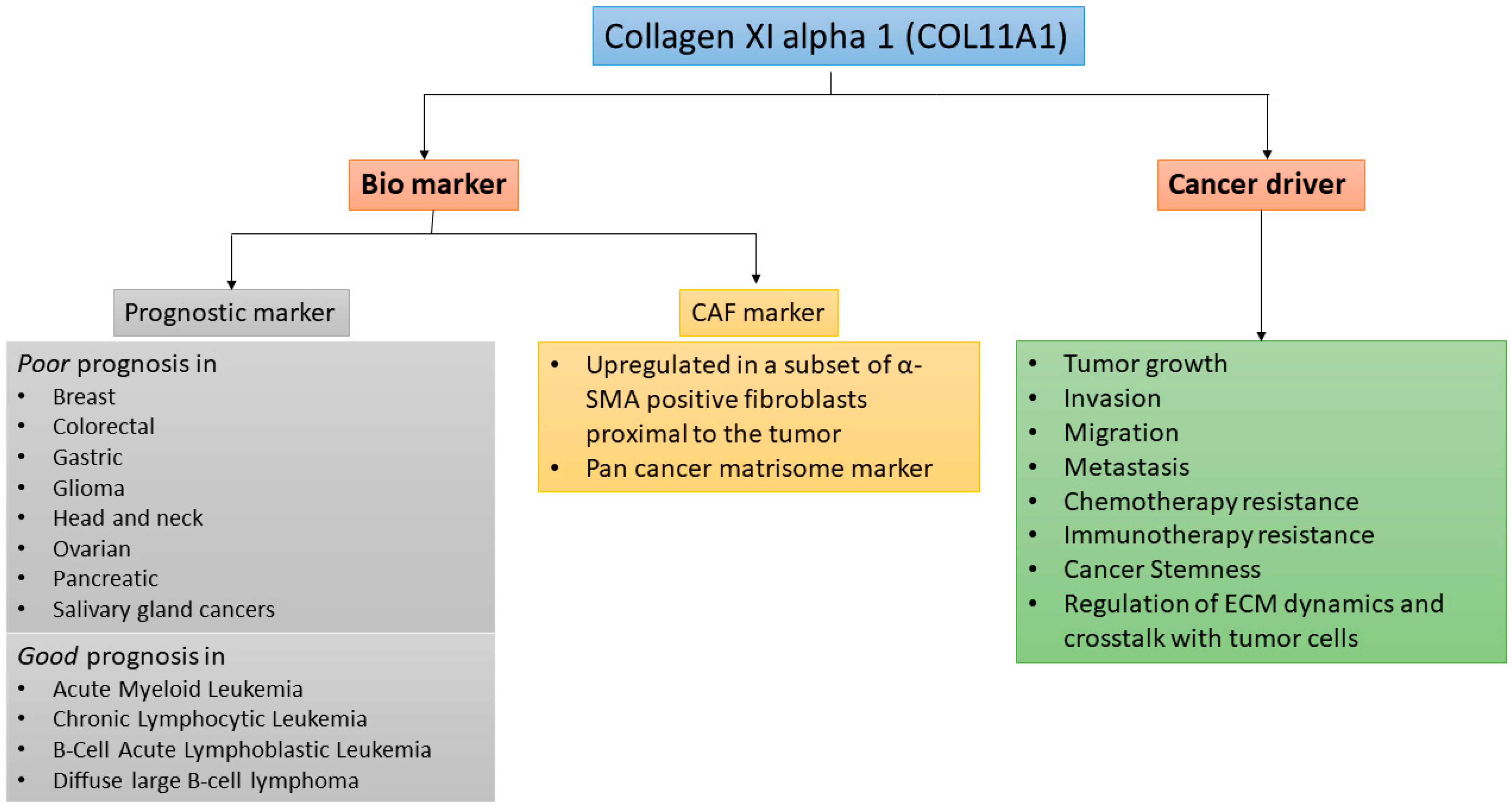
Abstract
1. Introduction
2. COL11A1 Biology and Binding Partners
3. COL11A1 in Tumor Microenvironment
3.1. CAFs Are the Major Source of COL11A1
3.2. COL11A1 Expression in Other Cancer-Associated Cells
3.3. COL11A1 Expression in the Matrisome Is a Pan-Cancer Biomarker
3.4. Mechanical Properties of COL11A1-Rich ECM
4. COL11A1 in Tumor Cell Migration and Metastasis
5. COL11A1 in Cancer Drug Resistance
5.1. Role of COL11A1 in Chemotherapy Resistance
5.2. Role of COL11A1 in Immune Cell Regulation and Immunotherapy Resistance
6. COL11A1 Signaling
6.1. Upstream Regulators
6.2. Receptors
6.3. Downstream Effectors
7. Targeting COL11A1 Signaling
| Drug | Targeted Signaling Molecule | Potential Effects of the Drug in COL11A1 Signaling | Clinical Status | Reference |
|---|---|---|---|---|
| Galunisertib | TβRI kinase | Downregulates COL11A1 expression | Improved OS from phase II clinical trial for HCC | [100] |
| SR-T100 | c/EBPβ | Downregulates COL11A1 expression | Increased chemosensitization in preclinical studies in melanoma and ovarian cancer | [101] |
| AK778 | HSP47 | Inhibits COL11A1 secretion | No cancer trials | [103] |
| Dasatinib | DDR2/Src kinase | Inhibits COL11A1 binding and signaling activation | Well tolerated (phase I); modest clinical efficacy (phase II); less bone metastasis but no OS improvement (phase III) for different cancers | [106,107,108] |
| SAN-300 | α1β1 integrin | Inhibits COL11A1 binding and signaling activation | No cancer trials; well tolerated in phase II clinical trial for rheumatoid arthritis | [109] |
| AZD5363 | Akt | Inhibits COL11A1-induced chemoresistance | Improved PFS in clinical trials for multiple cancers | [110] |
| SC66 | Akt | Inhibits COL11A1-induced chemoresistance | Increased chemosensitization in xenograft mouse models | [94] |
| ASTX660 | IAP | Inhibits COL11A1-induced chemoresistance | Well tolerated in phase I cancer trials | [111] |
| APG-1387 | IAP | Inhibits COL11A1-induced chemoresistance | Well tolerated in phase I clinical trials for solid tumors | [112] |
| LCL161 | IAP | Inhibits COL11A1-induced chemoresistance | Well tolerated in phase II trial in myelofibrosis (a form of leukemia) | [113] |
| Birinapant | XIAP/cIAP1 | Inhibits COL11A1-induced chemoresistance | No clinical benefit in phase II trial for high grade serous ovarian cancer | [114] |
| Etomoxir | CPT1 (FAO enzyme) | Inhibits COL11A1-induced chemoresistance | No cancer trials; phase II trial for diabetes and heart failure suspended due to liver and renal toxicity | [115] |
| Perhexiline | CPT1 (FAO enzyme) | Inhibits COL11A1-induced chemoresistance | No cancer trials; FDA approved for cardiac diseases | [116] |
| Ranolazine | ACAA2 (FAO enzyme) | Inhibits COL11A1-induced chemoresistance | No cancer trials; FDA and EMA approved for angina | [116] |
| Trimetazidine | ACAA2 (FAO enzyme) | Inhibits COL11A1-induced chemoresistance | No cancer trials; EMA approved for angina | [116] |
8. Remaining Challenges
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ricard-Blum, S. The collagen family. Cold Spring Harb. Perspect. Biol. 2011, 3, a004978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vazquez-Villa, F.; Garcia-Ocana, M.; Galvan, J.A.; Garcia-Martinez, J.; Garcia-Pravia, C.; Menedez-Rodriguez, P.; Gonzalez-del Rey, C.; Barneo-Serra, L.; de los Toyos, J.R. COL11A1/(pro)collagen 11A1 expression is a remarkable biomarker of human invasive carcinoma-associated stromal cells and carcinoma progression. Tumor Biol. 2015, 36, 2213–2222. [Google Scholar] [CrossRef] [Green Version]
- Kadler, K.E.; Hill, A.; Canty-Laird, E.G. Collagen fibrillogenesis: Fibronectin, integrins, and minor collagens as organizers and nucleators. Curr. Opin. Cell Biol. 2008, 20, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Eyre, D.R. Collagens and cartilage matrix homeostasis. Clin. Orthop. Relat. Res. 2004. [Google Scholar] [CrossRef] [PubMed]
- Vogiatzi, M.G.; Li, D.; Tian, L.; Garifallou, J.P.; Kim, C.E.; Hakonarson, H.; Levine, M.A. A novel dominant COL11A1 mutation in a child with Stickler syndrome type II is associated with recurrent fractures. Osteoporos. Int. 2018, 29, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Vijzelaar, R.; Waller, S.; Errami, A.; Donaldson, A.; Lourenco, T.; Rodrigues, M.; McConnell, V.; Fincham, G.; Snead, M.; Richards, A. Deletions within COL11A1 in Type 2 stickler syndrome detected by multiplex ligation-dependent probe amplification (MLPA). BMC Med. Genet. 2013, 14. [Google Scholar] [CrossRef] [Green Version]
- Richards, A.J.; Fincham, G.S.; McNinch, A.; Hill, D.; Poulson, A.V.; Castle, B.; Lees, M.M.; Moore, A.T.; Scott, J.D.; Snead, M.P. Alternative splicing modifies the effect of mutations in COL11A1 and results in recessive type 2 Stickler syndrome with profound hearing loss. J. Med. Genet. 2013, 50, 765–771. [Google Scholar] [CrossRef] [Green Version]
- Griffith, A.J.; Sprunger, L.K.; Sirko-Osadsa, D.A.; Tiller, G.E.; Meisler, M.H.; Warman, M.L. Marshall syndrome associated with a splicing defect at the COL11A1 locus. Am. J. Hum. Genet. 1998, 62, 816–823. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, W.J.; Sun, G.S.; Guo, L.S.; Wang, L.L.; Fan, W.Q.; Lang, M.L.; Chen, D.; Yi, X.H. A genetic variant in COL11A1 is functionally associated with lumbar disc herniation in Chinese population. J. Genet. 2017, 96, 867–872. [Google Scholar] [CrossRef]
- Li, Y.; Lacerda, D.A.; Warman, M.L.; Beier, D.R.; Yoshioka, H.; Ninomiya, Y.; Oxford, J.T.; Morris, N.P.; Andrikopoulos, K.; Ramirez, F.; et al. A Fibrillar Collagen Gene, Col11a1, Is Essential for Skeletal Morphogenesis. Cell 1995, 80, 423–430. [Google Scholar] [CrossRef] [Green Version]
- Wenstrup, R.J.; Smith, S.M.; Florer, J.B.; Zhang, G.Y.; Beason, D.P.; Seegmiller, R.E.; Soslowsky, L.J.; Birk, D.E. Regulation of Collagen Fibril Nucleation and Initial Fibril Assembly Involves Coordinate Interactions with Collagens V and XI in Developing Tendon. J. Biol. Chem. 2011, 286, 20455–20465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernandes, R.J.; Weis, M.; Scott, M.A.; Seegmiller, R.E.; Eyre, D.R. Collagen XI chain misassembly in cartilage of the chondrodysplasia (cho) mouse. Matrix Biol. 2007, 26, 597–603. [Google Scholar] [CrossRef] [Green Version]
- Raglow, Z.; Thomas, S.M. Tumor matrix protein collagen XI alpha 1 in cancer. Cancer Lett. 2015, 357, 448–453. [Google Scholar] [CrossRef] [Green Version]
- Jia, D.Y.; Liu, Z.Q.; Deng, N.; Tan, T.Z.; Huang, R.Y.J.; Taylor-Harding, B.; Cheon, D.J.; Lawrenson, K.; Wiedemeyer, W.R.; Walts, A.E.; et al. A COL11A1-correlated pan-cancer gene signature of activated fibroblasts for the prioritization of therapeutic targets. Cancer Lett. 2016, 382, 203–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morris, N.P.; Bachinger, H.P. Type XI collagen is a heterotrimer with the composition (1 alpha, 2 alpha, 3 alpha) retaining non-triple-helical domains. J. Biol. Chem. 1987, 262, 11345–11350. [Google Scholar] [CrossRef]
- Sirko-Osadsa, D.; Murray, M.A.; Scott, J.A.; Lavery, M.A.; Warman, M.L.; Robin, N.H. Stickler syndrome without eye involvement is caused by mutations in COL11A2, the gene encoding the alpha(2)(XI) chain of type XI collagen. J. Pediatrics 1998, 132, 368–371. [Google Scholar] [CrossRef]
- Keene, D.R.; Oxford, J.T.; Morris, N.P. Ultrastructural localization of collagen types II, IX, and XI in the growth plate of human rib and fetal bovine epiphyseal cartilage: Type XI collagen is restricted to thin fibrils. J. Histochem. Cytochem. 1995, 43, 967–979. [Google Scholar] [CrossRef] [Green Version]
- Hansen, U.; Bruckner, P. Macromolecular specificity of collagen fibrillogenesis—Fibrils of collagens I and XI contain a heterotypic alloyed core and a collagen I sheath. J. Biol. Chem. 2003, 278, 37352–37359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoshioka, H.; Iyama, K.; Inoguchi, K.; Khaleduzzaman, M.; Ninomiya, Y.; Ramirez, F. Developmental pattern of expression of the mouse alpha 1 (XI) collagen gene (Col11a1). Dev. Dyn. 1995, 204, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Niyibizi, C.; Eyre, D.R. Identification of the Cartilage-Alpha-1 (Xi) Chain in Type-V Collagen from Bovine Bone. FEBS Lett. 1989, 242, 314–318. [Google Scholar] [CrossRef] [Green Version]
- Kleman, J.P.; Hartmann, D.J.; Ramirez, F.; van der Rest, M. The human rhabdomyosarcoma cell line A204 lays down a highly insoluble matrix composed mainly of alpha 1 type-XI and alpha 2 type-V collagen chains. Eur. J. Biochem. 1992, 210, 329–335. [Google Scholar] [CrossRef]
- Brown, R.J.; Mallory, C.; McDougal, O.M.; Oxford, J.T. Proteomic analysis of Col11a1-associated protein complexes. Proteomics 2011, 11, 4660. [Google Scholar] [CrossRef] [Green Version]
- Ryan, R.E.; Martin, B.; Mellor, L.; Jacob, R.B.; Tawara, K.; McDougal, O.M.; Oxford, J.T.; Jorcyk, C.L. Oncostatin M binds to extracellular matrix in a bioactive conformation: Implications for inflammation and metastasis. Cytokine 2015, 72, 71–85. [Google Scholar] [CrossRef] [Green Version]
- Cheon, D.J.; Tong, Y.G.; Sim, M.S.; Dering, J.; Berel, D.; Cui, X.J.; Lester, J.; Beach, J.A.; Tighiouart, M.; Walts, A.E.; et al. A Collagen-Remodeling Gene Signature Regulated by TGF-beta Signaling Is Associated with Metastasis and Poor Survival in Serous Ovarian Cancer. Clin. Cancer Res. 2014, 20, 711–723. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia-Pravia, C.; Galvan, J.A.; Gutierrez-Corral, N.; Solar-Garcia, L.; Garcia-Perez, E.; Garcia-Ocana, M.; Del Amo-Iribarren, J.; Menendez-Rodriguez, P.; Garcia-Garcia, J.; de los Toyos, J.R.; et al. Overexpression of COL11A1 by Cancer-Associated Fibroblasts: Clinical Relevance of a Stromal Marker in Pancreatic Cancer. PLoS ONE 2013, 8, e78327. [Google Scholar] [CrossRef]
- Fischer, H.; Stenling, R.; Rubio, C.; Lindblom, A. Colorectal carcinogenesis is associated with stromal expression of COL11A1 and COL5A2. Carcinogenesis 2001, 22, 875–878. [Google Scholar] [CrossRef] [Green Version]
- Fuentes-Martinez, N.; Garcia-Pravia, C.; Garcia-Ocana, M.; Menendez-Rodriguez, P.; Del Amo, J.; Suarez-Fernandez, L.; Galvan, J.A.; Toyos, J.R.D.; Barneo, L. Overexpression of proCOL11A1 as a stromal marker of breast cancer. Histol. Histopathol. 2015, 30, 87–93. [Google Scholar] [PubMed]
- Kleinert, R.; Prenzel, K.; Stoecklein, N.; Alakus, H.; Bollschweiler, E.; Holscher, A.; Warnecke-Eberz, U. Gene Expression of Col11A1 Is a Marker Not only for Pancreas Carcinoma But also for Adenocarcinoma of the Papilla of Vater, Discriminating Between Carcinoma and Chronic Pancreatitis. Anticancer Res. 2015, 35, 6153–6158. [Google Scholar] [PubMed]
- Galvan, J.A.; Garcia-Martinez, J.; Vazquez-Villa, F.; Garcia-Ocana, M.; Garcia-Pravia, C.; Menendez-Rodriguez, P.; Gonzalez-del Rey, C.; Barneo-Serra, L.; de los Toyos, J.R. Validation of COL11A1/procollagen 11A1 expression in TGF-beta1-activated immortalised human mesenchymal cells and in stromal cells of human colon adenocarcinoma. BMC Cancer 2014, 14, 867. [Google Scholar] [CrossRef] [Green Version]
- Gaspar, N.J.; Li, L.; Kapoun, A.M.; Medicherla, S.; Reddy, M.; Li, G.; O’Young, G.; Quon, D.; Henson, M.; Damm, D.L.; et al. Inhibition of transforming growth factor beta signaling reduces pancreatic adenocarcinoma growth and invasiveness. Mol. Pharmacol. 2007, 72, 152–161. [Google Scholar] [CrossRef]
- Kim, H.; Watkinson, J.; Varadan, V.; Anastassiou, D. Multi-cancer computational analysis reveals invasion-associated variant of desmoplastic reaction involving INHBA, THBS2 and COL11A1. BMC Med. Genomics 2010, 3. [Google Scholar] [CrossRef] [Green Version]
- Socovich, A.M.; Naba, A. The cancer matrisome: From comprehensive characterization to biomarker discovery. Semin. Cell Dev. Biol. 2019, 89, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.H.; Chang, T.H.; Huang, Y.F.; Huang, H.D.; Chou, C.Y. COL11A1 promotes tumor progression and predicts poor clinical outcome in ovarian cancer. Oncogene 2014, 33, 3432–3440. [Google Scholar] [CrossRef] [PubMed]
- Yuzhalin, A.E.; Urbonas, T.; Silva, M.A.; Muschel, R.J.; Gordon-Weeks, A.N. A core matrisome gene signature predicts cancer outcome. Br. J. Cancer 2018, 118, 435–440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, K.; Cai, L.; Cui, C.; Anastassiou, D. Single-cell analysis reveals the transformation of adipose-derived stromal cells into COL11A1-expressing cancer-associated fibroblasts. bioRxiv 2020. [Google Scholar] [CrossRef]
- Emura, M.; Ochiai, A.; Horino, M.; Arndt, W.; Kamino, K.; Hirohashi, S. Development of myofibroblasts from human bone marrow mesenchymal stem cells cocultured with human colon carcinoma cells and TGF beta 1. In Vitro Cell. Dev. Biol. Anim. 2000, 36, 77–80. [Google Scholar] [CrossRef]
- Karnoub, A.E.; Dash, A.B.; Vo, A.P.; Sullivan, A.; Brooks, M.W.; Bell, G.W.; Richardson, A.L.; Polyak, K.; Tubo, R.; Weinberg, R.A. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature 2007, 449, 557–563. [Google Scholar] [CrossRef]
- Mishra, P.J.; Mishra, P.J.; Humeniuk, R.; Medina, D.J.; Alexe, G.; Mesirov, J.P.; Ganesan, S.; Glod, J.W.; Banerjee, D. Carcinoma-associated fibroblast-like differentiation of human mesenchymal stem cells. Cancer Res. 2008, 68, 4331–4339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buckanovich, R.J.; Sasaroli, D.; O’Brien-Jenkins, A.; Botbyl, J.; Hammond, R.; Katsaros, D.; Sandaltzopoulos, R.; Liotta, L.A.; Gimotty, P.A.; Coukos, G. Tumor vascular proteins as biomarkers in ovarian cancer. J. Clin. Oncol. 2007, 25, 852–861. [Google Scholar] [CrossRef] [Green Version]
- Ridge, S.M.; Sullivan, F.J.; Glynn, S.A. Mesenchymal stem cells: Key players in cancer progression. Mol. Cancer 2017, 16, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erkan, M.; Weis, N.; Pan, Z.; Schwager, C.; Samkharadze, T.; Jiang, X.; Wirkner, U.; Giese, N.A.; Ansorge, W.; Debus, J.; et al. Organ-, inflammation- and cancer specific transcriptional fingerprints of pancreatic and hepatic stellate cells. Mol. Cancer 2010, 9, 88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, Y.; Liu, S.; Zeng, S.; Shen, H. The critical roles of activated stellate cells-mediated paracrine signaling, metabolism and onco-immunology in pancreatic ductal adenocarcinoma. Mol. Cancer 2018, 17, 62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, S.B.; Tan, S.J.; Lim, W.T.; Lim, C.T. An extracellular matrix-related prognostic and predictive indicator for early-stage non-small cell lung cancer. Nat. Commun. 2017, 8, 1734. [Google Scholar] [CrossRef]
- Bin Lim, S.; Chua, M.L.K.; Yeong, J.P.S.; Tan, S.J.; Lim, W.T.; Lim, C.T. Pan-cancer analysis connects tumor matrisome to immune response. NPJ Precis. Oncol. 2019, 3, 15. [Google Scholar] [CrossRef] [Green Version]
- Pearce, O.M.; Delaine-Smith, R.; Maniati, E.; Wang, J.; Nichols, S.; Balkwill, F. Deconstruction of a metastatic tumour microenvironment reveals a common matrix response in human cancers. Int. J. Exp. Pathol. 2017, 98, A2–A3. [Google Scholar]
- Fraley, S.I.; Wu, P.H.; He, L.; Feng, Y.; Krisnamurthy, R.; Longmore, G.D.; Wirtz, D. Three-dimensional matrix fiber alignment modulates cell migration and MT1-MMP utility by spatially and temporally directing protrusions. Sci. Rep. 2015, 5, 14580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, L.H.; Yang, M.; Lin, Q.H.; Zhang, Z.W.; Zhu, B.; Miao, C.H. COL11A1 is overexpressed in recurrent non-small cell lung cancer and promotes cell proliferation, migration, invasion and drug resistance. Oncol. Rep. 2016, 36, 877–885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sok, J.C.; Kuriakose, M.A.; Mahajan, V.B.; Pearlman, A.N.; DeLacure, M.D.; Chen, F.A. Tissue-specific gene expression of head and neck squamous cell carcinoma in vivo by complementary DNA microarray analysis. Arch. Otolaryngol. Head Neck Surg. 2003, 129, 760–770. [Google Scholar] [CrossRef] [Green Version]
- Sok, J.C.; Lee, J.A.; Dasari, S.; Joyce, S.; Contrucci, S.C.; Egloff, A.M.; Trevelline, B.K.; Joshi, R.; Kumari, N.; Grandis, J.R.; et al. Collagen type XI alpha1 facilitates head and neck squamous cell cancer growth and invasion. Br. J. Cancer 2013, 109, 3049–3056. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tu, H.B.; Li, J.; Lin, L.; Wang, L.X. COL11A1 Was Involved in Cell Proliferation, Apoptosis and Migration in Non-Small Cell Lung Cancer Cells. J. Investig. Surg. 2020. [Google Scholar] [CrossRef]
- Zhang, B.; Zhang, C.; Yang, X.; Chen, Y.; Zhang, H.; Liu, J.; Wu, Q. Cytoplasmic collagen XIalphaI as a prognostic biomarker in esophageal squamous cell carcinoma. Cancer Biol. Ther. 2018, 19, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Arolt, C.; Meyer, M.; Hoffmann, F.; Wagener-Ryczek, S.; Schwarz, D.; Nachtsheim, L.; Beutner, D.; Odenthal, M.; Guntinas-Lichius, O.; Buettner, R.; et al. Expression Profiling of Extracellular Matrix Genes Reveals Global and Entity-Specific Characteristics in Adenoid Cystic, Mucoepidermoid and Salivary Duct Carcinomas. Cancers (Basel) 2020, 12, 2466. [Google Scholar] [CrossRef]
- Lopez-Lago, M.A.; Thodima, V.J.; Guttapalli, A.; Chan, T.; Heguy, A.; Molina, A.M.; Reuter, V.E.; Motzer, R.J.; Chaganti, R.S. Genomic deregulation during metastasis of renal cell carcinoma implements a myofibroblast-like program of gene expression. Cancer Res. 2010, 70, 9682–9692. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Halsted, K.C.; Bowen, K.B.; Bond, L.; Luman, S.E.; Jorcyk, C.L.; Fyffe, W.E.; Kronz, J.D.; Oxford, J.T. Collagen alpha1(XI) in normal and malignant breast tissue. Mod. Pathol. 2008, 21, 1246–1254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, H.B.; Ren, Y.L.; Qian, C.; Liu, J.X.; Li, G.; Li, Z.G. Over-expression of CDX2 alleviates breast cancer by up-regulating microRNA let-7b and inhibiting COL11A1 expression. Cancer Cell Int. 2020, 20. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Guo, H.F.; Zhang, Y.L.; Chen, L.; Ying, D.J.; Dong, S.W. MicroRNA-145 Regulates Chondrogenic Differentiation of Mesenchymal Stem Cells by Targeting Sox9. PLoS ONE 2011, 6, e21679. [Google Scholar] [CrossRef] [PubMed]
- Li, A.Q.; Li, J.; Lin, J.P.; Zhuo, W.; Si, J.M. COL11A1 is overexpressed in gastric cancer tissues and regulates proliferation, migration and invasion of HGC-27 gastric cancer cells in vitro. Oncol. Rep. 2017, 37, 333–340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- An, J.H.; Lee, S.Y.; Jeon, J.Y.; Cho, K.G.; Kim, S.U.; Lee, M.A. Identification of gliotropic factors that induce human stem cell migration to malignant tumor. J. Proteome Res. 2009, 8, 2873–2881. [Google Scholar] [CrossRef]
- Chernov, A.V.; Baranovskaya, S.; Golubkov, V.S.; Wakeman, D.R.; Snyder, E.Y.; Williams, R.; Strongin, A.Y. Microarray-based transcriptional and epigenetic profiling of matrix metalloproteinases, collagens, and related genes in cancer. J. Biol. Chem. 2010, 285, 19647–19659. [Google Scholar] [CrossRef] [Green Version]
- Jin, Y.L.; Zhu, H.F.; Cai, W.; Fan, X.Y.; Wang, Y.T.; Niu, Y.L.; Song, F.Z.; Bu, Y.Q. B-Myb Is Up-Regulated and Promotes Cell Growth and Motility in Non-Small Cell Lung Cancer. Int. J. Mol. Sci. 2017, 18, 860. [Google Scholar] [CrossRef] [Green Version]
- Turkowski, K.; Herzberg, F.; Gunther, S.; Brunn, D.; Weigert, A.; Meister, M.; Muley, T.; Kriegsmann, M.; Schneider, M.A.; Winter, H.; et al. Fibroblast Growth Factor-14 Acts as Tumor Suppressor in Lung Adenocarcinomas. Cells-Basel 2020, 9, 1755. [Google Scholar] [CrossRef]
- Wu, Y.H.; Huang, Y.F.; Chang, T.H.; Chou, C.Y. Activation of TWIST1 by COL11A1 promotes chemoresistance and inhibits apoptosis in ovarian cancer cells by modulating NF-kappa B-mediated IKK beta expression. Int. J. Cancer 2017, 141, 2305–2317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rada, M.; Nallanthighal, S.; Cha, J.; Ryan, K.; Sage, J.; Eldred, C.; Ullo, M.; Orsulic, S.; Cheon, D.J. Inhibitor of apoptosis proteins (IAPs) mediate collagen type XI alpha 1-driven cisplatin resistance in ovarian cancer. Oncogene 2018, 37, 4809–4820. [Google Scholar] [CrossRef] [PubMed]
- Nallanthighal, S.; Rada, M.; Heiserman, J.P.; Cha, J.; Sage, J.; Zhou, B.; Yang, W.; Hu, Y.; Korgaonkar, C.; Hanos, C.T.; et al. Inhibition of collagen XI alpha 1-induced fatty acid oxidation triggers apoptotic cell death in cisplatin-resistant ovarian cancer. Cell Death Dis. 2020, 11, 258. [Google Scholar] [CrossRef] [Green Version]
- Wu, Y.H.; Chang, T.H.; Huang, Y.F.; Chen, C.C.; Chou, C.Y. COL11A1 confers chemoresistance on ovarian cancer cells through the activation of Akt/c/EBP beta pathway and PDK1 stabilization. Oncotarget 2015, 6, 23748–23763. [Google Scholar] [CrossRef] [Green Version]
- Yeung, T.L.; Leung, C.S.; Yip, K.P.; Sheng, J.T.; Vien, L.; Bover, L.C.; Birrer, M.J.; Wong, S.T.C.; Mok, S.C. Anticancer Immunotherapy by MFAP5 Blockade Inhibits Fibrosis and Enhances Chemosensitivity in Ovarian and Pancreatic Cancer. Clin. Cancer Res. 2019, 25, 6417–6428. [Google Scholar] [CrossRef]
- Li, Y.; Liu, Z.; Sun, Y.; Hui, D.; Dianyun, R.; Li, Y.; Gou, S. COL11A1 acted as a downstream of Mist1 to promote the EMT in pancreatic cancer. Prepr. Res. Square 2020, in press. [Google Scholar] [CrossRef]
- Feldmann, G.; Habbe, N.; Dhara, S.; Bisht, S.; Alvarez, H.; Fendrich, V.; Beaty, R.; Mullendore, M.; Karikari, C.; Bardeesy, N.; et al. Hedgehog inhibition prolongs survival in a genetically engineered mouse model of pancreatic cancer. Gut 2008, 57, 1420–1430. [Google Scholar] [CrossRef] [Green Version]
- Teng, P.N.; Wang, G.; Hood, B.L.; Conrads, K.A.; Hamilton, C.A.; Maxwell, G.L.; Darcy, K.M.; Conrads, T.P. Identification of candidate circulating cisplatin-resistant biomarkers from epithelial ovarian carcinoma cell secretomes. Br. J. Cancer 2014, 110, 123–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chong, I.W.; Chang, M.Y.; Chang, H.C.; Yu, Y.P.; Sheu, C.C.; Tsai, J.R.; Hung, J.Y.; Chou, S.H.; Tsai, M.S.; Hwang, J.J.; et al. Great potential of a panel of multiple hMTH1, SPD, ITGA11 and COL11A1 markers for diagnosis of patients with non-small cell lung cancer. Oncol. Rep. 2006, 16, 981–988. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giussani, M.; Landoni, E.; Merlino, G.; Turdo, F.; Veneroni, S.; Paolini, B.; Cappelletti, V.; Miceli, R.; Orlandi, R.; Triulzi, T.; et al. Extracellular matrix proteins as diagnostic markers of breast carcinoma. J. Cell Physiol. 2018, 233, 6280–6290. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.B.; Xu, Y. Clinical significance of COL11A1 and its effect on immune infiltration in colorectal cancer. Prepr. Lancet 2020. [Google Scholar] [CrossRef]
- Lim, S.B.; Tan, S.J.; Lim, W.T.; Lim, C.T. Cross-platform meta-analysis reveals common matrisome variation associated with tumor genotypes and immunophenotypes in human cancers. bioRxiv 2018. [Google Scholar] [CrossRef]
- Matsuo, N.; Yu-Hua, W.; Sumiyoshi, H.; Sakata-Takatani, K.; Nagato, H.; Sakai, K.; Sakurai, M.; Yoshioka, H. The transcription factor CCAAT-binding factor CBF/NF-Y regulates the proximal promoter activity in the human alpha 1(XI) collagen gene (COL11A1). J. Biol. Chem. 2003, 278, 32763–32770. [Google Scholar] [CrossRef] [Green Version]
- Hida, M.; Hamanaka, R.; Okamoto, O.; Yamashita, K.; Sasaki, T.; Yoshioka, H.; Matsuo, N. Nuclear factor Y (NF-Y) regulates the proximal promoter activity of the mouse collagen alpha1(XI) gene (Col11a1) in chondrocytes. In Vitro Cell. Dev. Biol. Anim. 2014, 50, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, K.; Hida, M.; Sasaki, T.; Yano, H.; Kawano, K.; Yoshioka, H.; Matsuo, N. Sp1 upregulates the proximal promoter activity of the mouse collagen alpha 1(XI) gene (Col11a1) in chondrocytes. In Vitro Cell. Dev. Biol. Anim. 2016, 52, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Gardner, H.; Strehlow, D.; Bradley, L.; Widom, R.; Farina, A.; de Fougerolles, A.; Peyman, J.; Koteliansky, V.; Korn, J.H. Global expression analysis of the fibroblast transcriptional response to TGFbeta. Clin. Exp. Rheumatol. 2004, 22, S47–S57. [Google Scholar]
- Gu, S.Q.; Luo, J.H.; Yao, W.X. The regulation of miR-139-5p on the biological characteristics of breast cancer cells by targeting COL11A1. Math. Biosci. Eng. 2020, 17, 1428–1441. [Google Scholar] [CrossRef]
- Ripa, R.; Dolfi, L.; Terrigno, M.; Pandolfini, L.; Savino, A.; Arcucci, V.; Groth, M.; Terzibasi Tozzini, E.; Baumgart, M.; Cellerino, A. MicroRNA miR-29 controls a compensatory response to limit neuronal iron accumulation during adult life and aging. BMC Biol. 2017, 15, 9. [Google Scholar] [CrossRef] [Green Version]
- Kamran, F.; Andrade, A.C.; Nella, A.A.; Clokie, S.J.; Rezvani, G.; Nilsson, O.; Baron, J.; Lui, J.C. Evidence That Up-Regulation of MicroRNA-29 Contributes to Postnatal Body Growth Deceleration. Mol. Endocrinol. 2015, 29, 921–932. [Google Scholar] [CrossRef] [Green Version]
- Liao, M.F.; Zou, S.L.; Weng, J.F.; Hon, L.W.; Yang, L.; Zhao, Z.Q.; Bao, J.M.; Jing, Z.P. A microRNA profile comparison between thoracic aortic dissection and normal thoracic aorta indicates the potential role of microRNAs in contributing to thoracic aortic dissection pathogenesis. J. Vasc. Surg. 2011, 53, 1341–1349. [Google Scholar] [CrossRef] [Green Version]
- Kahler, R.A.; Yingst, S.M.; Hoeppner, L.H.; Jensen, E.D.; Krawczak, D.; Oxford, J.T.; Westendorf, J.J. Collagen 11a1 is indirectly activated by lymphocyte enhancer-binding factor 1 (Lef1) and negatively regulates osteoblast maturation. Matrix Biol. 2008, 27, 330–338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gorski, J.P.; Huffman, N.T.; Chittur, S.; Midura, R.J.; Black, C.; Oxford, J.; Seidah, N.G. Inhibition of proprotein convertase SKI-1 blocks transcription of key extracellular matrix genes regulating osteoblastic mineralization. J. Biol. Chem. 2011, 286, 1836–1849. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuhn, K.; Eble, J. The structural bases of integrin-ligand interactions. Trends Cell Biol. 1994, 4, 256–261. [Google Scholar] [CrossRef]
- Camper, L.; Holmvall, K.; Wangnerud, C.; Aszodi, A.; Lundgren-Akerlund, E. Distribution of the collagen-binding integrin alpha10beta1 during mouse development. Cell Tissue Res. 2001, 306, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Tiger, C.F.; Fougerousse, F.; Grundstrom, G.; Velling, T.; Gullberg, D. alpha 11 beta 1 integrin is a receptor for interstitial collagens involved in cell migration and collagen reorganization on mesenchymal nonmuscle cells. Dev. Biol. 2001, 237, 116–129. [Google Scholar] [CrossRef] [Green Version]
- Vogel, W.; Gish, G.D.; Alves, F.; Pawson, T. The discoidin domain receptor tyrosine kinases are activated by collagen. Mol. Cell 1997, 1, 13–23. [Google Scholar] [CrossRef]
- Leitinger, B.; Hohenester, E. Mammalian collagen receptors. Matrix Biol. 2007, 26, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Ren, R.L.; Yang, Z.Z.; Cai, J.; Du, S.X.; Shen, X.H. The COL11A1/Akt/CREB signaling axis enables mitochondrial-mediated apoptotic evasion to promote chemoresistance in pancreatic cancer cells through modulating BAX/BCL-2 function. J. Cancer 2021, 12, 1406–1420. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Bihan, D.; Chang, F.; Huang, P.H.; Farndale, R.W.; Leitinger, B. Discoidin domain receptors promote alpha1beta1- and alpha2beta1-integrin mediated cell adhesion to collagen by enhancing integrin activation. PLoS ONE 2012, 7, e52209. [Google Scholar] [CrossRef]
- Dominguez, C.X.; Muller, S.; Keerthivasan, S.; Koeppen, H.; Hung, J.; Gierke, S.; Breart, B.; Foreman, O.; Bainbridge, T.W.; Castiglioni, A.; et al. Single-Cell RNA Sequencing Reveals Stromal Evolution into LRRC15(+) Myofibroblasts as a Determinant of Patient Response to Cancer Immunotherapy. Cancer Discov. 2020, 10, 232–253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, Y.; Sun, X.; Zhuang, Z. Comprehensive Network Analysis of Integrin α11 Expressed in Human Breast Cancer. Prepr. Res. Square 2019. [Google Scholar] [CrossRef]
- Popova, S.N.; Lundgren-Akerlund, E.; Wiig, H.; Gullberg, D. Physiology and pathology of collagen receptors. Acta Physiol. (Oxf.) 2007, 190, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.H.; Huang, Y.F.; Chen, C.C.; Chou, C.Y. Akt inhibitor SC66 promotes cell sensitivity to cisplatin in chemoresistant ovarian cancer cells through inhibition of COL11A1 expression. Cell Death Dis. 2019, 10, 322. [Google Scholar] [CrossRef] [PubMed]
- Zandi, E.; Rothwarf, D.M.; Delhase, M.; Hayakawa, M.; Karin, M. The IkappaB kinase complex (IKK) contains two kinase subunits, IKKalpha and IKKbeta, necessary for IkappaB phosphorylation and NF-kappaB activation. Cell 1997, 91, 243–252. [Google Scholar] [CrossRef] [Green Version]
- Mikheeva, S.A.; Mikheev, A.M.; Petit, A.; Beyer, R.; Oxford, R.G.; Khorasani, L.; Maxwell, J.P.; Glackin, C.A.; Wakimoto, H.; Gonzalez-Herrero, I.; et al. TWIST1 promotes invasion through mesenchymal change in human glioblastoma. Mol. Cancer 2010, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, L.W.; Lam, C.; Edwards, S.W. Mcl-1; the molecular regulation of protein function. FEBS Lett. 2010, 584, 2981–2989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sainaghi, P.P.; Castello, L.; Bergamasco, L.; Galletti, M.; Bellosta, P.; Avanzi, G.C. Gas6 induces proliferation in prostate carcinoma cell lines expressing the Axl receptor. J. Cell Physiol. 2005, 204, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.Y.; Ann, D.K. When fats commit crimes: Fatty acid metabolism, cancer stemness and therapeutic resistance. Cancer Commun. 2018, 38. [Google Scholar] [CrossRef] [Green Version]
- Huynh, L.K.; Hipolito, C.J.; Ten Dijke, P. A Perspective on the Development of TGF-beta Inhibitors for Cancer Treatment. Biomolecules 2019, 9, 743. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, S.; Sheu, H.M.; Lee, C.H. Solanum incanum extract (SR-T100) induces melanoma cell apoptosis and inhibits established lung metastasis. Oncotarget 2017, 8, 103509–103517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagata, K.; Saga, S.; Yamada, K.M. A major collagen-binding protein of chick embryo fibroblasts is a novel heat shock protein. J. Cell Biol. 1986, 103, 223–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ito, S.; Ogawa, K.; Takeuchi, K.; Takagi, M.; Yoshida, M.; Hirokawa, T.; Hirayama, S.; Shin-Ya, K.; Shimada, I.; Doi, T.; et al. A small-molecule compound inhibits a collagen-specific molecular chaperone and could represent a potential remedy for fibrosis. J. Biol. Chem. 2017, 292, 20076–20085. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beauchamp, E.M.; Woods, B.A.; Dulak, A.M.; Tan, L.; Xu, C.; Gray, N.S.; Bass, A.J.; Wong, K.K.; Meyerson, M.; Hammerman, P.S. Acquired resistance to dasatinib in lung cancer cell lines conferred by DDR2 gatekeeper mutation and NF1 loss. Mol. Cancer Ther. 2014, 13, 475–482. [Google Scholar] [CrossRef] [Green Version]
- Lombardo, L.J.; Lee, F.Y.; Chen, P.; Norris, D.; Barrish, J.C.; Behnia, K.; Castaneda, S.; Cornelius, L.A.M.; Das, J.; Doweyko, A.M.; et al. Discovery of N-(2-chloro-6-methylphenyl)-2-(6-(4-(2-hydroxyethyl)-piperazin-1-yl)-2-methylpyrimidin-4-ylamino)thiazole-5-carboxamide (BMS-354825), a dual Src/Abl kinase inhibitor with potent antitumor activity in preclinical assays. J. Med. Chem. 2004, 47, 6658–6661. [Google Scholar] [CrossRef] [PubMed]
- Haura, E.B.; Tanvetyanon, T.; Chiappori, A.; Williams, C.; Simon, G.; Antonia, S.; Gray, J.; Litschauer, S.; Tetteh, L.; Neuger, A.; et al. Phase I/II Study of the Src Inhibitor Dasatinib in Combination with Erlotinib in Advanced Non-Small-Cell Lung Cancer. J. Clin. Oncol. 2010, 28, 1387–1394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Araujo, J.C.; Trudel, G.C.; Saad, F.; Armstrong, A.J.; Yu, E.Y.; Bellmunt, J.; Wilding, G.; McCaffrey, J.; Serrano, S.V.; Matveev, V.; et al. Overall survival (OS) and safety of dasatinib/docetaxel versus docetaxel in patients with metastatic castration-resistant prostate cancer (mCRPC): Results from the randomized phase III READY trial. J. Clin. Oncol. 2013, 31. [Google Scholar] [CrossRef]
- Morris, P.G.; Rota, S.; Cadoo, K.; Zamora, S.; Patil, S.; D’Andrea, G.; Gilewski, T.; Bromberg, J.; Dang, C.; Dickler, M.; et al. Phase II Study of Paclitaxel and Dasatinib in Metastatic Breast Cancer. Clin. Breast Cancer 2018, 18, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Raab-Westphal, S.; Marshall, J.F.; Goodman, S.L. Integrins as Therapeutic Targets: Successes and Cancers. Cancers 2017, 9, 110. [Google Scholar] [CrossRef] [PubMed]
- Hyman, D.M.; Smyth, L.M.; Donoghue, M.T.A.; Westin, S.N.; Bedard, P.L.; Dean, E.J. Azd5363 Has Clinical Activity in Patients with Akt1-Mutant Solid Tumors. Cancer Discov. 2017, 7, 662. [Google Scholar] [CrossRef] [Green Version]
- Mita, M.M.; LoRusso, P.M.; Papadopoulos, K.P.; Gordon, M.S.; Mita, A.C.; Ferraldeschi, R.; Keer, H.; Oganesian, A.; Su, X.Y.; Jueliger, S.; et al. A Phase I Study of ASTX660, an Antagonist of Inhibitors of Apoptosis Proteins, in Adults with Advanced Cancers or Lymphoma. Clin. Cancer Res. 2020, 26, 2819–2826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, R.H.; Li, Y.H.; Ji, J.; Qiu, M.Z.; Zhang, Y.; Liu, W.Q.; Tian, X.H.; Li, S.; Wang, H.B.; Wang, F.H.; et al. A phase I study of a novel IAP inhibitor APG-1387 in patients with advanced solid tumors. J. Clin. Oncol. 2018, 36. [Google Scholar] [CrossRef]
- Pemmaraju, N.; Carter, B.Z.; Kantarjian, H.M.; Cortes, J.E.; Kadia, T.M.; Garcia-Manero, G.; DiNardo, C.D.; Bose, P.; Daver, N.G.; Konopleva, M.Y.; et al. LCL161, an Oral Smac Mimetic/IAP Antagonist for Patients with Myelofibrosis (MF): Novel Translational Findings Among Long-Term Responders in a Phase 2 Clinical Trial. Blood 2018, 132. [Google Scholar] [CrossRef]
- Noonan, A.M.; Bunch, K.P.; Chen, J.Q.; Herrmann, M.A.; Lee, J.M.; Kohn, E.C.; O’Sullivan, C.C.; Jordan, E.; Houston, N.; Takebe, N.; et al. Pharmacodynamic markers and clinical results from the phase 2 study of the SMAC mimetic birinapant in women with relapsed platinum-resistant or -refractory epithelial ovarian cancer. Cancer 2016, 122, 588–597. [Google Scholar] [CrossRef] [PubMed]
- Ceccarelli, S.M.; Chomienne, O.; Gubler, M.; Arduini, A. Carnitine Palmitoyltransferase (CPT) Modulators: A Medicinal Chemistry Perspective on 35 Years of Research. J. Med. Chem. 2011, 54, 3109–3152. [Google Scholar] [CrossRef]
- Ma, Y.; Temkin, S.M.; Hawkridge, A.M.; Guo, C.; Wang, W.; Wang, X.Y.; Fang, X. Fatty acid oxidation: An emerging facet of metabolic transformation in cancer. Cancer Lett. 2018, 435, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Song, M.Q.; Bode, A.M.; Dong, Z.G.; Lee, M.H. AKT as a Therapeutic Target for Cancer. Cancer Res. 2019, 79, 1019–1031. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernandez-Torres, J.; Martinez-Nava, G.A.; Zamudio-Cuevas, Y.; Martinez-Flores, K.; Mijares-Diaz, F. Multifactor dimensionality reduction reveals a strong gene-gene interaction between STC1 and COL11A1 genes as a possible risk factor of knee osteoarthritis. Mol. Biol. Rep. 2020, 47, 2627–2634. [Google Scholar] [CrossRef] [PubMed]

| Type of Cancer | Role of COL11A1 | Mechanism | References |
|---|---|---|---|
| Breast | increases drug resistance; upregulates EMT; increases cancer cell invasion and metastasis in vitro and tumor growth in vivo | suppresses CDX2/microRNA let-7b expression | [55] |
| miR-139-5 suppresses COL11A1 expression | [56] | ||
| Binds to OSM to activate STAT signaling | [23] | ||
| Colorectal | one of the genes of the “invasion gene signature”; associated with poor survival | TGFβ is an upstream regulator of COL11A1 | [29] |
| co-expressed with COL5A2 | [26] | ||
| Esophageal | increases cancer cell proliferation, migration, and invasion in vitro; positively correlates with advanced clinical stage, invasion depth and lymph node metastases | upregulates EMT in an AKT/ERK/c-Myc dependent manner | [51] |
| Gastric | offers poor prognosis; increases cancer cell proliferation, migration and invasion | upregulates several proliferation genes including CDK6, TIAM1, ITGB8 and WNT5A | [57] |
| Glioma | offers poor prognosis; increases neural stem cell migration to tumor sites and metastasis | activates ERK-dependent migration | [58] |
| hyperacetylates histone H3 and upregulates transcription of tumorigenic factors | [59] | ||
| Head and neck | offers poor prognosis; upregulates cancer cell proliferation, migration, and invasion | [49] | |
| Lung | offers poor prognosis; increases cancer cell proliferation, migration, invasion and drug resistance | upregulates Smad 2 signaling | [47] |
| upregulates p-AKT, p-PI3K and p-ERK | [50] | ||
| B-myb is a transcription factor that increases COL11A1 expression | [60] | ||
| FGF14 upregulates COL11A1 expression | [61] | ||
| Ovary | offers poor prognosis; upregulates EMT; increases cancer cell invasion, metastasis, and drug resistance in vitro; increases tumor growth in vivo | TGFβ is an upstream growth factor that induces COL11A1 expression | [14,24,33] |
| remodels ECM via Ets-1/MMP3 signaling | [62] | ||
| mediates tumor-stroma interaction via α1β1 integrin and DDR2 receptors | [63,64] | ||
| upregulates Akt1/c/EBPβ signaling | [65] | ||
| upregulates IkkB/NFκB-TWIST1 axis | [62] | ||
| upregulates IAPs in a Src-Akt-NFKB dependent manner | [63] | ||
| upregulates fatty acid metabolism in a Scr-Akt-AMPK dependent manner | [64] | ||
| MFAP5 is an upstream growth factor that increases COL11A1 expression in ovarian CAFs | [66] | ||
| Pancreas | associated with poor survival; increases tumor cell invasion, metastasis, and drug resistance in vitro; increases tumor growth in vivo | Mist-1 is a transcriptional repressor of COL11A1 | [67] |
| Gli1 is a transcriptional activator of COL11A1 | [68] | ||
| NF-YA is a transcriptional activator of COL11A1 | [30] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nallanthighal, S.; Heiserman, J.P.; Cheon, D.-J. Collagen Type XI Alpha 1 (COL11A1): A Novel Biomarker and a Key Player in Cancer. Cancers 2021, 13, 935. https://doi.org/10.3390/cancers13050935
Nallanthighal S, Heiserman JP, Cheon D-J. Collagen Type XI Alpha 1 (COL11A1): A Novel Biomarker and a Key Player in Cancer. Cancers. 2021; 13(5):935. https://doi.org/10.3390/cancers13050935
Chicago/Turabian StyleNallanthighal, Sameera, James Patrick Heiserman, and Dong-Joo Cheon. 2021. "Collagen Type XI Alpha 1 (COL11A1): A Novel Biomarker and a Key Player in Cancer" Cancers 13, no. 5: 935. https://doi.org/10.3390/cancers13050935
APA StyleNallanthighal, S., Heiserman, J. P., & Cheon, D.-J. (2021). Collagen Type XI Alpha 1 (COL11A1): A Novel Biomarker and a Key Player in Cancer. Cancers, 13(5), 935. https://doi.org/10.3390/cancers13050935







