Durvalumab after Chemoradiotherapy for PD-L1 Expressing Inoperable Stage III NSCLC Leads to Significant Improvement of Local-Regional Control and Overall Survival in the Real-World Setting
Abstract
:Simple Summary
Abstract
1. Introduction
2. Patients and Methods
2.1. Patient Characterstics
2.2. Chemoradiotherapy
2.3. Patient Follow-Up
2.4. Statistical Analysis
3. Results
3.1. Patient and Tumor Characteristics
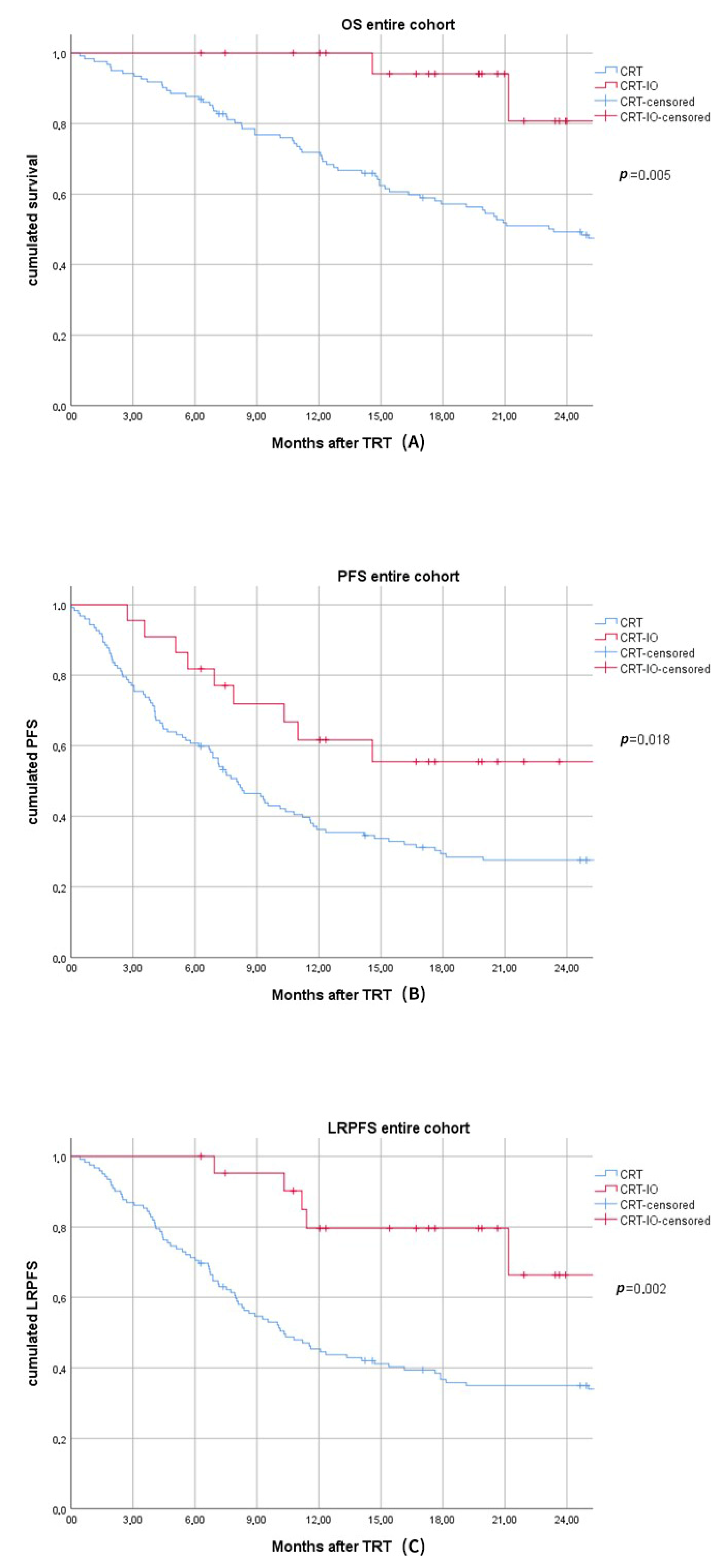
3.2. Comparison of CRT and CRT-IO in the Entire Cohort
3.3. PSM with Exact T- and N-Stage Matching
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Taugner, J.; Kasmann, L.; Eze, C.; Dantes, M.; Roengvoraphoj, O.; Gennen, K.; Karin, M.; Petruknov, O.; Tufman, A.; Belka, C.; et al. Survival score to characterize prognosis in inoperable stage III NSCLC after chemoradiotherapy. Transl. Lung Cancer Res. 2019, 8, 593–604. [Google Scholar] [CrossRef]
- Gennen, K.; Kasmann, L.; Taugner, J.; Eze, C.; Karin, M.; Roengvoraphoj, O.; Neumann, J.; Tufman, A.; Orth, M.; Reu, S.; et al. Prognostic value of PD-L1 expression on tumor cells combined with CD8+ TIL density in patients with locally advanced non-small cell lung cancer treated with concurrent chemoradiotherapy. Radiat. Oncol. 2020, 15, 5. [Google Scholar] [CrossRef]
- Roengvoraphoj, O.; Wijaya, C.; Eze, C.; Li, M.; Dantes, M.; Taugner, J.; Tufman, A.; Huber, R.M.; Belka, C.; Manapov, F. Analysis of primary tumor metabolic volume during chemoradiotherapy in locally advanced non-small cell lung cancer. Strahlenther. Onkol. 2018, 194, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Brundage, M.D.; Davies, D.; Mackillop, W.J. Prognostic factors in non-small cell lung cancer: A decade of progress. Chest 2002, 122, 1037–1057. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexander, M.; Wolfe, R.; Ball, D.; Conron, M.; Stirling, R.G.; Solomon, B.; MacManus, M.; Officer, A.; Karnam, S.; Burbury, K.; et al. Lung cancer prognostic index: A risk score to predict overall survival after the diagnosis of non-small-cell lung cancer. Br. J. Cancer 2017, 117, 744–751. [Google Scholar] [CrossRef] [Green Version]
- Rotow, J.; Bivona, T.G. Understanding and targeting resistance mechanisms in NSCLC. Nat. Rev. Cancer 2017, 17, 637–658. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.M.; Shaikh, T.; Hallman, M. Therapeutic management options for stage III non-small cell lung cancer. World J. Clin. Oncol. 2017, 8, 1–20. [Google Scholar] [CrossRef]
- Thomas, A.; Liu, S.V.; Subramaniam, D.S.; Giaccone, G. Refining the treatment of NSCLC according to histological and mo-lecular subtypes. Nat. Rev. Clin. Oncol. 2015, 12, 511–526. [Google Scholar] [CrossRef]
- Taugner, J.; Eze, C.; Käsmann, L.; Roengvoraphoj, O.; Gennen, K.; Karin, M.; Petrukhnov, O.; Tufman, A.; Belka, C.; Manapov, F. Pattern-of-failure and salvage treatment analysis after chemoradiotherapy for inoperable stage III non-small cell lung cancer. Radiat. Oncol. 2020, 15, 1–9. [Google Scholar] [CrossRef]
- Käsmann, L.; Taugner, J.; Eze, C.; Roengvoraphoj, O.; Dantes, M.; Gennen, K.; Karin, M.; Petrukhnov, O.; Tufman, A.; Belka, C.; et al. Performance Status and Its Changes Predict Outcome for Patients with Inoperable Stage III NSCLC Undergoing Multimodal Treatment. Anticancer Res. 2019, 39, 5077–5081. [Google Scholar] [CrossRef] [PubMed]
- Käsmann, L.; Young DEGRO Trial Group; Niyazi, M.; Blanck, O.; Baues, C.; Baumann, R.; Dobiasch, S.; Eze, C.; Fleischmann, D.; Gauer, T.; et al. Predictive and prognostic value of tumor volume and its changes during radical radiotherapy of stage III non-small cell lung cancer. Strahlenther. Onkol. 2018, 194, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Aupérin, A.; Le Péchoux, C.; Rolland, E.; Curran, W.J.; Furuse, K.; Fournel, P.; Belderbos, J.; Clamon, G.; Ulutin, H.C.; Paulus, R.; et al. Meta-Analysis of Concomitant Versus Sequential Radiochemotherapy in Locally Advanced Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2010, 28, 2181–2190. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Herndon, J., II; Langer, M.; Kohman, L.J.; Elias, A.D.; Kass, F.C.; Eaton, W.L.; Seagren, S.L.; Green, M.R.; Sugarbaker, D.J. Patterns of disease failure after trimodality therapy of nonsmall cell lung carcinoma pathologic stage IIIA (N2). Analysis of Cancer and Leukemia Group B Protocol 8935. Cancer 1996, 77, 2393–2399. [Google Scholar] [CrossRef]
- Terakedis, B.M.; Sause, W.T. Radiation Dose Escalation in Stage III Non-Small-Cell Lung Cancer. Front. Oncol. 2011, 1, 47. [Google Scholar] [CrossRef] [Green Version]
- Dillman, R.O.; Herndon, J.; Seagren, S.L.; Eaton, J.W.L.; Green, M.R. Improved Survival in Stage III Non-Small-Cell Lung Cancer: Seven-Year Follow-up of Cancer and Leukemia Group B (CALGB) 8433 Trial. J. Natl. Cancer Inst. 1996, 88, 1210–1215. [Google Scholar] [CrossRef] [PubMed]
- Bradley, J.D.; Paulus, R.; Komaki, R.; Masters, G.; Blumenschein, G.; Schild, S.; Bogart, J.; Hu, C.; Forster, K.; Magliocco, A.; et al. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): A randomised, two-by-two factorial phase 3 study. Lancet Oncol. 2015, 16, 187–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bradley, J.D.; Hu, C.; Komaki, R.R.; Masters, G.A.; Blumenschein, G.R.; Schild, S.E.; Bogart, J.A.; Forster, K.M.; Magliocco, A.M.; Kavadi, V.S.; et al. Long-Term Results of NRG Oncology RTOG 0617: Standard-Versus High-Dose Chemoradiotherapy with or without Cetuximab for Unresectable Stage III non–small-cell lung cancer. J. Clin. Oncol. 2020, 38, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Curran, W.J.; Paulus, R.; Langer, C.J.; Komaki, R.; Lee, J.S.; Hauser, S.; Movsas, B.; Wasserman, T.; Rosenthal, S.A.; Gore, E.; et al. Sequential vs Concurrent Chemoradiation for Stage III non-small cell lung cancer: Randomized Phase III Trial RTOG 9410. J. Natl. Cancer Inst. 2011, 103, 1452–1460. [Google Scholar] [CrossRef] [Green Version]
- Antonia, S.J.; Villegas, A.; Daniel, D.; Vicente, D.; Murakami, S.; Hui, R.; Yokoi, T.; Chiappori, A.; Lee, K.H.; De Wit, M.; et al. Durvalumab after Chemoradiotherapy in Stage III Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2017, 377, 1919–1929. [Google Scholar] [CrossRef]
- Antonia, S.J.; Villegas, A.; Daniel, D.; Vicente, D.; Murakami, S.; Hui, R.; Kurata, T.; Chiappori, A.; Lee, K.H.; De Wit, M.; et al. Overall Survival with Durvalumab after Chemoradiotherapy in Stage III NSCLC. N. Engl. J. Med. 2018, 379, 2342–2350. [Google Scholar] [CrossRef]
- Gray, J.E.; Villegas, A.; Daniel, D.; Vicente, D.; Murakami, S.; Hui, R.; Kurata, T.; Chiappori, A.; Lee, K.H.; Cho, B.C.; et al. Three-Year Overall Survival with Durvalumab after Chemoradiotherapy in Stage III NSCLC—Update from PACIFIC. J. Thorac. Oncol. 2020, 15, 288–293. [Google Scholar] [CrossRef] [Green Version]
- Käsmann, L.; Eze, C.; Taugner, J.; Roengvoraphoj, O.; Dantes, M.; Schmidt-Hegemann, N.S.; Schiopu, S.; Belka, C.; Manapov, F. Chemoradioimmunotherapy of inoperable stage III non-small cell lung cancer: Immunological rationale and current clinical trials establishing a novel multimodal strategy. Radiat. Oncol. 2020, 15, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Shaverdian, N.; Offin, M.D.; Rimner, A.; Shepherd, A.F.; Wu, A.J.; Rudin, C.M.; Hellmann, M.D.; Chaft, J.E.; Gomez, D.R. Utilization and factors precluding the initiation of consolidative durvalumab in unresectable stage III non-small cell lung cancer. Radiother. Oncol. 2020, 144, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, T.; Ito, K.; Furuhashi, K.; Nakamura, Y.; Suzuki, Y.; Nishii, Y.; Taguchi, O.; Hataji, O. Patients with unresectable stage III non-small cell lung cancer eligible to receive consolidation therapy with durvalumab in clinical practice based on PACIFIC study criteria. Respir. Investig. 2019, 57, 466–471. [Google Scholar] [CrossRef]
- Hosoya, K.; Fujimoto, D.; Kawachi, H.; Sato, Y.; Kogo, M.; Nagata, K.; Nakagawa, A.; Tachikawa, R.; Hiraoka, S.; Kokubo, M.; et al. Ineligibility for the PACIFIC trial in unresectable stage III non-small cell lung cancer patients. Cancer Chemother. Pharmacol. 2019, 84, 275–280. [Google Scholar] [CrossRef]
- Shaverdian, N.; Thor, M.; Shepherd, A.F.; Offin, M.D.; Jackson, A.; Wu, A.J.; Gelblum, D.Y.; Yorke, E.D.; Ii, C.B.S.; Chaft, J.E.; et al. Radiation pneumonitis in lung cancer patients treated with chemoradiation plus durvalumab. Cancer Med. 2020, 9, 4622–4631. [Google Scholar] [CrossRef]
- Vansteenkiste, J.; Naidoo, J.; Faivre-Finn, C.; Özgürŏglu, M.; Villegas, A.; Daniel, D.; Murakami, S.; Hui, R.; Lee, K.; Cho, B.; et al. MA05.02 PACIFIC Subgroup Analysis: Pneumonitis in Stage III, Unresectable NSCLCPatients Treated with Durvalumab vs. Placebo After CRT.J. Thorac. Oncol. 2018, 13, S370–S371. [Google Scholar] [CrossRef] [Green Version]
- Vansteenkiste, J.; Naidoo, J.; Faivre-Finn, C.; Özgüroğlu, M.; Villegas, A.; Daniel, D.; Murakami, S.; Hui, R.; Lee, K.; Cho, B.; et al. Efficacy of durvalumab in patients with stage III NSCLC who experience pneumonitis (PACIFIC). Ann. Oncol. 2019, 30, v592–v593. [Google Scholar] [CrossRef]
- Offin, M.; Shaverdian, N.; Rimner, A.; Lobaugh, S.; Shepherd, A.F.; Simone, C.B.; Gelblum, D.Y.; Wu, A.J.; Lee, N.; Kris, M.G.; et al. Clinical outcomes, local–regional control and the role for metastasis-directed therapies in stage III non-small cell lung cancers treated with chemoradiation and durvalumab. Radiother. Oncol. 2020, 149, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.A.; Noh, J.M.; Sun, J.-M.; Lee, S.-H.; Ahn, J.S.; Ahn, M.-J.; Pyo, H.; Ahn, Y.C.; Park, K. Real world data of durvalumab consolidation after chemoradiotherapy in stage III non-small-cell lung cancer. Lung Cancer 2020, 146, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.; Chiu, T.; Wang, C.; Chang, W.; Huang, A.C.; Liu, C.; Wang, C.; Ko, H.; Chung, F.; Hsu, P.; et al. Consolidation treatment of durvalumab after chemoradiation in real-world patients with stage III unresectable non-small cell lung cancer. Thorac. Cancer 2020, 11, 1541–1549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nestle, U.; De Ruysscher, D.; Ricardi, U.; Geets, X.; Belderbos, J.; Pöttgen, C.; Dziadiuszko, R.; Peeters, S.; Lievens, Y.; Hurkmans, C.; et al. ESTRO ACROP guidelines for target volume definition in the treatment of locally advanced non-small cell lung cancer. Radiother. Oncol. 2018, 127, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Bertsekas, D.P.; Tseng, P. Relaxation methods for minimum cost ordinary and generalized network flow problems. Oper. Res. 1988, 36, 93–114. [Google Scholar] [CrossRef] [Green Version]
- Hansen, B.B. Full matching in an observational study of coaching for the SAT. J. Am. Stat. Assoc. 2004, 99, 609–618. [Google Scholar] [CrossRef] [Green Version]
- Ho, D.E.; Imai, K.; King, G.; Stuart, E.A. MatchIt: Nonparametric preprocessing for parametric causal inference. J. Stat. Softw. 2011, 42, 1–28. [Google Scholar] [CrossRef] [Green Version]
- Ho, D.E.; Imai, K.; King, G.; Stuart, E.A. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Polit. Anal. 2007, 15, 199–236. [Google Scholar] [CrossRef] [Green Version]
- Thoemmes, F. Propensity Score Matching in SPSS. 2012. Available online: https://arxiv.org/pdf/1201.6385 (accessed on 20 December 2020).
- Flentje, M.; Huber, R.M.; Engel-Riedel, W.; Andreas, S.; Kollmeier, J.; Staar, S.; Dickgreber, N.; Vaissiere, N.; De Almeida, C.; Edlich, B.; et al. GILT—A randomised phase III study of oral vinorelbine and cisplatin with concomitant radiotherapy followed by either consolidation therapy with oral vinorelbine and cisplatin or best supportive care alone in stage III non-small cell lung cancer. Strahlenther. Onkol. 2016, 192, 216–222. [Google Scholar] [CrossRef]
- Machtay, M.; Paulus, R.; Moughan, J.; Komaki, R.; Bradley, J.E.; Choy, H.; Albain, K.; Movsas, B.; Sause, W.T.; Curran, W.J. Defining local-regional control and its importance in locally advanced non-small cell lung carcinoma. J. Thorac. Oncol. 2012, 7, 716–722. [Google Scholar] [CrossRef] [Green Version]
- Desilets, A.; Blanc-Durand, F.; Lau, S.; Hakozaki, T.; Kitadai, R.; Malo, J.; Belkaid, W.; Richard, C.; Messaoudene, M.; Cvetkovic, L.; et al. Durvalumab therapy following chemoradiation compared with a historical cohort treated with chemoradiation alone in patients with stage III non–small cell lung cancer: A real-world multicentre study. Eur. J. Cancer 2021, 142, 83–91. [Google Scholar] [CrossRef]
- Abe, T.; Saito, S.; Iino, M.; Aoshika, T.; Ryuno, Y.; Ohta, T.; Igari, M.; Hirai, R.; Kumazaki, Y.; Miura, Y.; et al. Effect of durvalumab on local control after concurrent chemoradiotherapy for locally advanced non-small cell lung cancer in comparison with chemoradiotherapy alone. Thorac. Cancer 2021, 12, 245–250. [Google Scholar] [CrossRef]
- Ohri, N.; Halmos, B.; Bodner, W.R.; Cheng, H.; Garg, M.K.; Gucalp, R.; Guha, C. Who benefits the most from adjuvant durvalumab after chemoradiotherapy for non-small cell lung cancer? An exploratory analysis. Pract. Radiat. Oncol. 2021, 11, e172–e179. [Google Scholar] [CrossRef] [PubMed]

| Entire Cohort N (%) | CRT Subgroup N (%) | PSM-CRT Subgroup N (%) | CRT-IO Subgroup N (%) | |
|---|---|---|---|---|
| Total | 144 | 122 | 44 | 22 |
| Age | ||||
| median years | 68.4 | 68.5 | 67.9 | 67.6 |
| >65 years | 93 (64.6) | 80 (65.6) | 27 (61.4) | 13 (59.1) |
| Gender | ||||
| Male | 97 (67.4) | 81 (66.4) | 27 (61.4) | 16 (72.7) |
| Female | 47 (32.6) | 41 (33.6) | 17 (38.6) | 6 (27.3) |
| T-stage | ||||
| 1 | 16 (11.1) | 15 (12.3) | 2 (4.5) | 1 (4.5) |
| 2 | 29 (20.1) | 24 (19.7) | 20 (22.7) | 5 (22.7) |
| 3 | 37 (25.7) | 30 (24.6) | 14 (31.8) | 7 (31.8) |
| 4 | 62 (43.1) | 53 (43.4) | 18 (40.9) | 9 (40.9) |
| N-stage | ||||
| 0 | 20 (13.9) | 15 (12.3) | 8 (18.2) | 4 (18.2) |
| 1 | 12 (8.3) | 11 (9.0) | 2 (4.5) | 1 (4.5) |
| 2 | 53 (36.8) | 42 (34.4) | 22 (50.0) | 11 (50.0) |
| 3 | 59 (41.0) | 54 (44.3) | 12 (27.3) | 6 (27.3) |
| UICC-stage | ||||
| IIIA | 50 (34.7) | 42 (34.4) | 16 (36.4) | 8 (36.4) |
| IIIB | 56 (38.9) | 45 (36.9) | 22 (50.0) | 11 (50.0) |
| IIIC | 38 (26.4) | 35 (28.7) | 6 (13.6) | 3 (13.6) |
| Planning target volume (PTV)-size | ||||
| median cc | 720.1 | 732.0 | 634.9 | 680.3 |
| ≥700 ccm | 75 (52.1) | 65 (53.3) | 17 (38.6) | 10 (45.5) |
| Histology | ||||
| Squamous cell carcinoma (SCC) | 66 (45.8) | 57 (46.7) | 21 (47.7) | 9 (40.9) |
| Adenocarcinoma (AC) | 65 (45.1) | 54 (44.3) | 22 (50.0) | 11 (50.0) |
| Not otherwise specified (NOS) | 13 (9.0) | 11 (9.0) | 1 (2.3) | 2 (9.1) |
| Radiographic imaging | ||||
| PET-CT | 135 (93.8) | 114 (93.4) | 41 (93.2) | 21 (95.5) |
| cMRI | 79 (54.9) | 59 (48.4) | 25 (56.8) | 20 (90.9) |
| Treatment | ||||
| Concurrent chemoradiation (CRT) | 122 (84.7) | 100 (82.0) | 44 (100) | 22 (100) |
| Induction chemotherapy | 60 (41.6) | 54 (44.3) | 21 (47.7) | 6 (27.3) |
| 3DCRT | 48 (33.3) | 48 (39.3) | 17 (38.6) | 0 (0) |
| IMRT/VMAT | 96 (66.7) | 74 (60.7) | 27 (61.4) | 22 (100) |
| Median-FU months | 33.1 | 49.9 | 62.0 | 19.8 |
| OS | ||||
| 6-months | 129 (89.6) | 107 (87.7) | 38 (86.4) | 22 (100) |
| 12-months | 103 (75.4) | 85 (71.4) | 31 (70.5) | 19 (100) |
| Progression-free survival (PFS) | ||||
| 6-months | 92 (63.8) | 74 (60.7) | 24 (54.5) | 18 (81.8) |
| 12-months | 55 (39.3) | 43 (35.8) | 14 (31.8) | 12 (60.0) |
| Local-regional-free-survival (LRPFS) | ||||
| 6-months | 109 (75.7) | 87 (71.3) | 31 (70.5) | 22 (100) |
| 12-months | 69 (51.4) | 54 (44.5) | 20 (45.5) | 15 (78.9) |
| Entire Cohort N (%) | OS p | PFS p | LRPFS p | |
|---|---|---|---|---|
| Total | 144 (100) | |||
| Age | ||||
| >65 years | 93 (64.6) | 0.054 | 0.783 | 0.475 |
| Gender | ||||
| Male | 97 (67.4) | 0.053 | 0.485 | 0.324 |
| T-stage | ||||
| 4 | 62 (43.1) | 0.694 | 0.757 | 0.278 |
| N-stage | ||||
| 3 | 59 (41.0) | 0.522 | 0.083 | 0.370 |
| UICC-stage | ||||
| IIIC | 38 (26.4) | 0.320 | 0.150 | 0.108 |
| PTV-size | ||||
| ≥700 ccm | 75 (52.1) | 0.045 | 0.061 | 0.039 |
| Histology | ||||
| SCC + NOS | 79 (54.9) | 0.023 | 0.972 | 0.018 |
| Treatment | ||||
| Induction chemotherapy | 60 (41.6) | 0.269 | 0.214 | 0.111 |
| Absence of concurrent chemoradiation | 23 (16.0) | 0.356 | 0.699 | 0.382 |
| 3DCRT | 48 (33.3) | 0.223 | 0.531 | 0.374 |
| Durvalumab consolidation | 22 (15.3) | |||
| CRT-IO | 0.005 | 0.018 | 0.002 |
| PSM-CRT Subgroup N (%) | CRT-IO Subgroup N (%) | p-Value | |
|---|---|---|---|
| Total | 44 | 22 | |
| Age | |||
| median years | 67.9 | 67.6 | |
| >65 years | 27 (61.4) | 13 (59.1) | 0.895 |
| Gender | |||
| Male | 27 (61.4) | 16 (72.7) | |
| Female | 17 (38.6) | 6 (27.3) | 0.246 |
| T-stage | |||
| 1 | 2 (4.5) | 1 (4.5) | |
| 2 | 20 (22.7) | 5 (22.7) | |
| 3 | 14 (31.8) | 7 (31.8) | |
| 4 | 18 (40.9) | 9 (40.9) | 0.078 |
| N-stage | |||
| 0 | 8 (18.2) | 4 (18.2) | |
| 1 | 2 (4.5) | 1 (4.5) | |
| 2 | 22 (50.0) | 11 (50.0) | |
| 3 | 12 (27.3) | 6 (27.3) | 0.468 |
| UICC-stage | |||
| IIIA | 16 (36.4) | 8 (36.4) | |
| IIIB | 22 (50.0) | 11 (50.0) | |
| IIIC | 6 (13.6) | 3 (13.6) | 0.663 |
| PTV-size | |||
| median cc | 634.9 | 680.3 | |
| ≥700 ccm | 17 (38.6) | 10 (45.5) | 0.608 |
| Histology | |||
| Squamous cell carcinoma (SCC) | 21 (47.7) | 9 (40.9) | |
| Adenocarcinoma (AC) | 22 (50.0) | 11 (50.0) | |
| Not otherwise specified (NOS) | 1 (2.3) | 2 (9.1) | 0.066 |
| Radiographic imaging | |||
| PET-CT | 41 (93.2) | 21 (95.5) | 0.977 |
| cMRI | 25 (56.8) | 20 (90.9) | 0.762 |
| Treatment | |||
| Concurrent chemoradiation (CRT) | 44 (100) | 22 (100) | 0.303 |
| Induction chemotherapy | 21 (47.7) | 6 (27.3) | 0.009 |
| Median-FU months | 62.0 | 19.8 | |
| OS | |||
| 6-months | 38 (86.4) | 22 (100) | |
| 12-months | 31 (70.5) | 19 (100) | |
| PFS | |||
| 6-months | 24 (54.5) | 18 (81.8) | |
| 12-months | 14 (31.8) | 12 (60.0) | |
| LRPFS | |||
| 6-months | 31 (70.5) | 22 (100) | |
| 12-months | 20 (45.5) | 15 (78.9) |
| Authors | Title | Year | Results |
|---|---|---|---|
| Michael Offin et al. [29] | Clinical outcomes, local–regional control, and the role for metastasis-directed therapies in stage III non-small cell lung cancers treated with chemoradiation and durvalumab | 2020 | 62 NSCLC stage III patients treated with CRT+ durvalumab. Median follow-up for all patients was 12 months. Estimated 12-month PFS 65% (95% CI: 51–79%) and OS 85% (95% CI: 75–95%). 12-month incidence of local–regional and distant failures were 18% (95% CI: 5.9–30%) and 30% (95% CI: 16.3–44.5%). High tumor mutation burden or PD-L1 did not predict improved PFS. |
| Hyun Ae Jung et al. [30] | Real world data of durvalumab consolidation after chemoradiotherapy in stage III non-small-cell lung cancer | 2020 | 21 NSCLC stage III patients treated with CRT+ durvalumab. Median PFS of all patients: not reached versus 9.6 (95 % CI 4.5–14.8) months (p = 0.060). Durvalumab consolidation treatment was associated with favorable PFS in patients who did not meet the criteria of the PACIFIC study. |
| Chia-Hsun Chu et al. [31] | Consolidation treatment of durvalumab after chemoradiation in real-world patients with stage III unresectable non-small cell lung cancer | 2020 | 31 NSCLC stage III patients treated with CRT+ durvalumab. 12-month PFS and time to metastatic disease or death-free rate were 56.4 and 66.9%, respectively. Patients with low neutrophil-to-lymphocyte ratio showed a significantly longer post-CRT PFS (p = 0.040). |
| Nitin Ohri et al. [42] | Who benefits the most from adjuvant durvalumab after chemoradiotherapy for non-small cell lung cancer? An exploratory analysis | 2020 | 35 NSCLC stage III patients treated with CRT+ durvalumab, 70 patients treated with CRT alone. Patients treated with CRT+ durvalumab had significantly improved 12-month-PFS of 67 vs. 39% (p = 0.006) and 12-month-OS of 88 vs. 76% (p = 0.041). Neutrophil-to-lymphocyte ratio <4.3 after TRT was associated with improved PFS in the durvalumab cohort. |
| Takanori Abe et al. [41] | Effect of durvalumab on local control after concurrent chemoradiotherapy for locally advanced non-small cell lung cancer in comparison with chemoradiotherapy alone | 2020 | 44 NSCLC stage III patients treated with CRT+ durvalumab, 76 patients treated with CRT alone. Median follow-up 17 months. 12-months local-control, distant metastasis, PFS, and OS rates (from start of TRT) 86, 29, 58, and 84% in the CRT+ durvalumab vs. 62, 31, 57, and 89% in the CRT alone cohort. Local control was significantly improved in the durvalumab cohort (p = 0.005). |
| Antoine Desilets et al. [40] | Durvalumab therapy following chemoradiation compared with a historical cohort treated with chemoradiation alone in patients with stage III non-small cell lung cancer: A real-world multicentre study | 2020 | 147 NSCLC stage III patients treated with CRT+ durvalumab, 121 patients treated with CRT alone. Median OS not reached for CRT + durvalumab vs. 26.9 months in CRT patients (p = 0.001). Improved 12-month OS in patients with PD-L1 expression ≥50% in the durvalumab cohort (100% vs. 86%, p = 0.007) |
| Present study | Durvalumab after chemoradiotherapy for PD-L1 expressing inoperable stage III NSCLC leads to significant improvement of the local-regional control and overall survival in the real-world setting | 2020 | 22 NSCLC stage III patients treated with CRT+ durvalumab, 122 patients treated with CRT alone. Median follow-up 19.8 months. After PSM 12-month LRPFS, PFS, and OS-rates in the CRT-IO vs. CRT cohort were 78.9 vs. 45.5% (p = 0.002), 60.0 vs. 31.8% (p = 0.007) and 100 vs. 86.4% (p = 0.003), respectively |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taugner, J.; Käsmann, L.; Eze, C.; Tufman, A.; Reinmuth, N.; Duell, T.; Belka, C.; Manapov, F. Durvalumab after Chemoradiotherapy for PD-L1 Expressing Inoperable Stage III NSCLC Leads to Significant Improvement of Local-Regional Control and Overall Survival in the Real-World Setting. Cancers 2021, 13, 1613. https://doi.org/10.3390/cancers13071613
Taugner J, Käsmann L, Eze C, Tufman A, Reinmuth N, Duell T, Belka C, Manapov F. Durvalumab after Chemoradiotherapy for PD-L1 Expressing Inoperable Stage III NSCLC Leads to Significant Improvement of Local-Regional Control and Overall Survival in the Real-World Setting. Cancers. 2021; 13(7):1613. https://doi.org/10.3390/cancers13071613
Chicago/Turabian StyleTaugner, Julian, Lukas Käsmann, Chukwuka Eze, Amanda Tufman, Niels Reinmuth, Thomas Duell, Claus Belka, and Farkhad Manapov. 2021. "Durvalumab after Chemoradiotherapy for PD-L1 Expressing Inoperable Stage III NSCLC Leads to Significant Improvement of Local-Regional Control and Overall Survival in the Real-World Setting" Cancers 13, no. 7: 1613. https://doi.org/10.3390/cancers13071613
APA StyleTaugner, J., Käsmann, L., Eze, C., Tufman, A., Reinmuth, N., Duell, T., Belka, C., & Manapov, F. (2021). Durvalumab after Chemoradiotherapy for PD-L1 Expressing Inoperable Stage III NSCLC Leads to Significant Improvement of Local-Regional Control and Overall Survival in the Real-World Setting. Cancers, 13(7), 1613. https://doi.org/10.3390/cancers13071613









