Baseline Splenic Volume Outweighs Immuno-Modulated Size Changes with Regard to Survival Outcome in Patients with Hepatocellular Carcinoma under Immunotherapy
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Diagnosis, Treatment, and Follow-Up
2.3. Splenic Volume Assessment
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
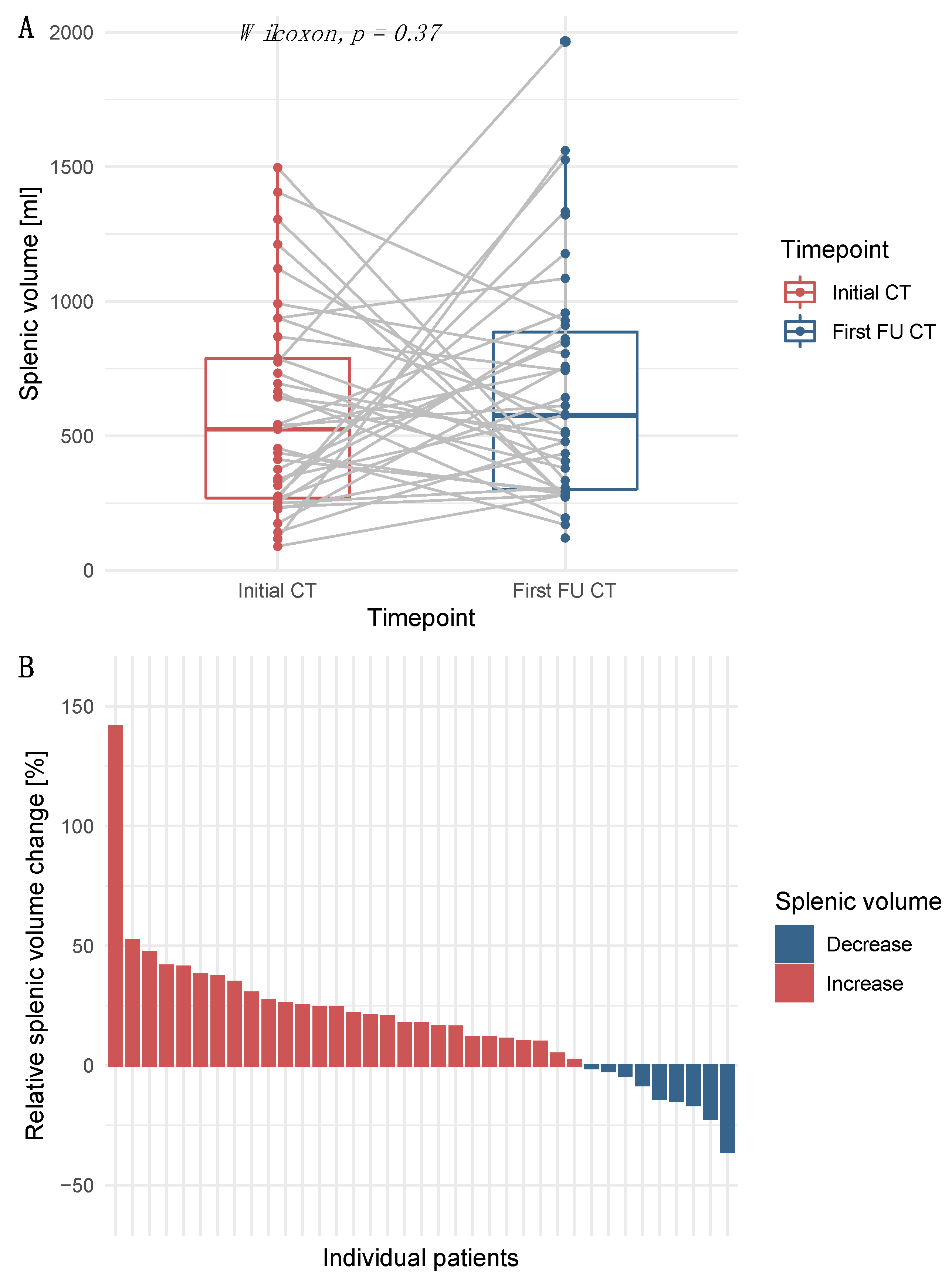
3.2. Increase in Splenic Volume after Initiation of Immunotherapy
3.3. Correlation of Splenic Volume with Parameters of Liver Function, but Not with Tumor Burden
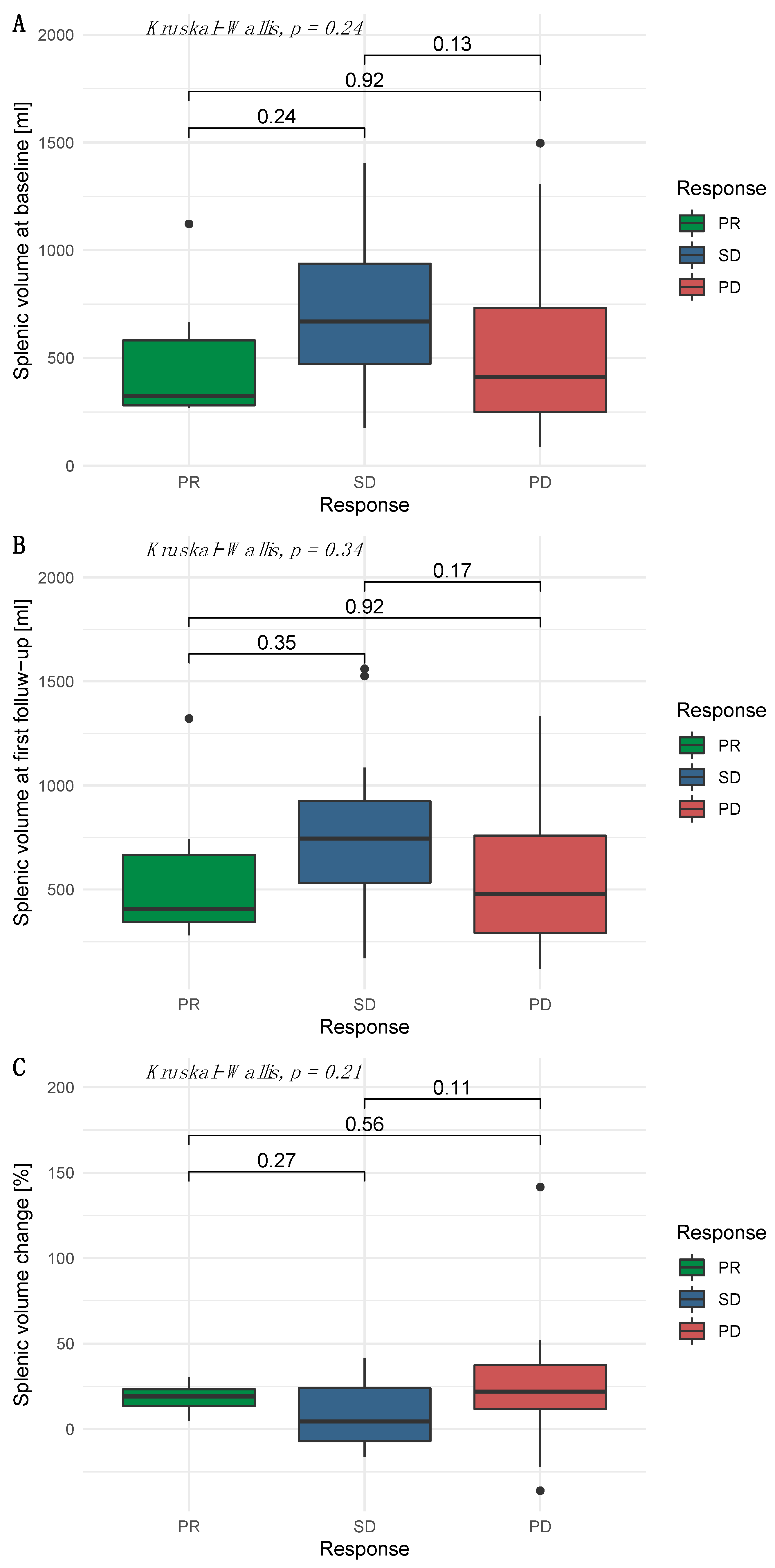
3.4. Independence of Splenic Volume and Radiological Response
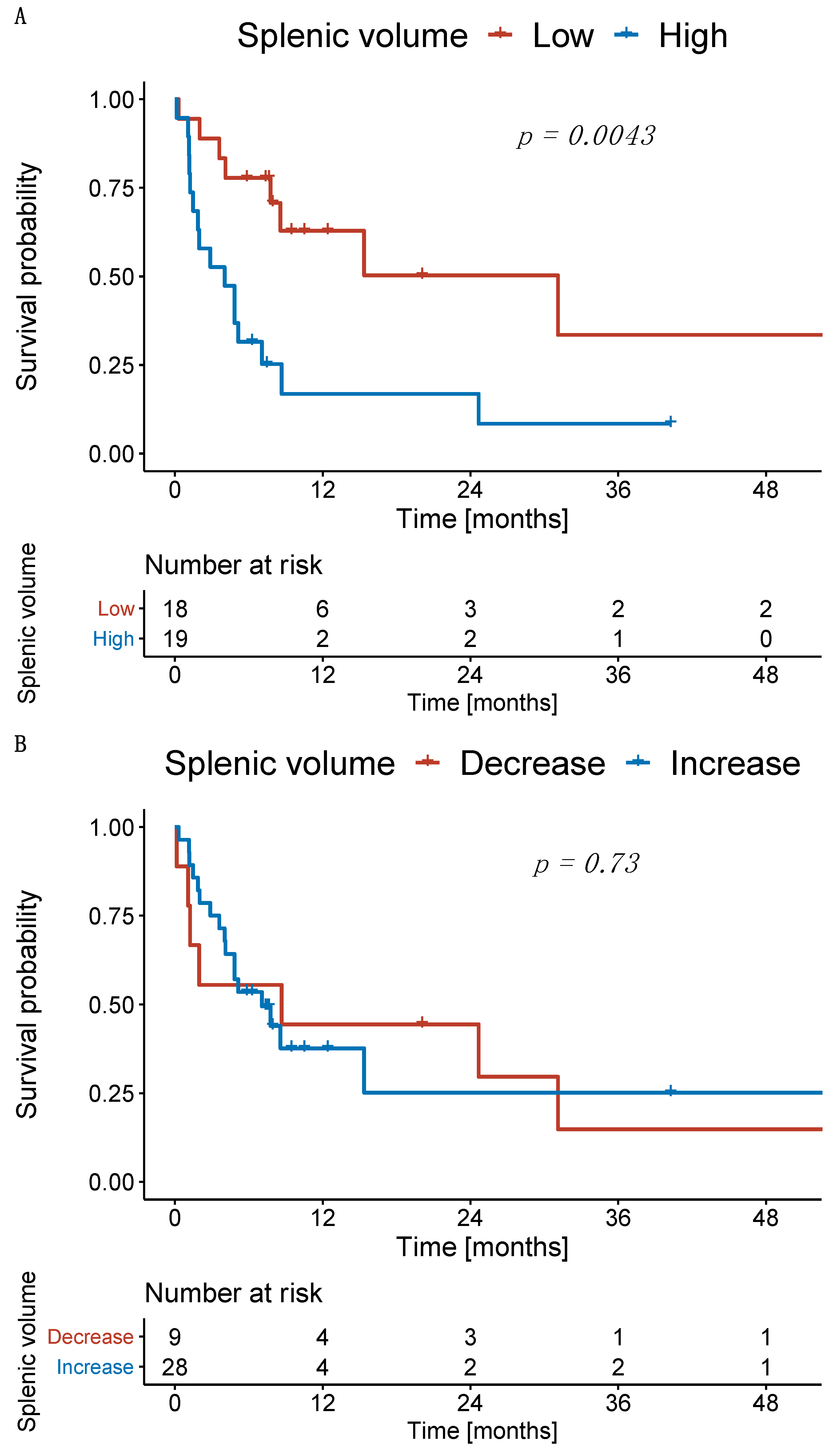
3.5. Significant Impact of High Splenic Volume at Treatment Initiation and during Follow-Up on Overall Survival
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galle, P.R.; Forner, A.; Llovet, J.M.; Mazzaferro, V.; Piscaglia, F.; Raoul, J.-L.; Schirmacher, P.; Vilgrain, V. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iwakiri, Y. Pathophysiology of Portal hypertension. Clin. Liver Dis. 2014, 18, 281–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosch, J.; Abraldes, J.G.; Berzigotti, A.; García-Pagan, J.C. The clinical use of HVPG measurements in chronic liver disease. Nat. Rev. Gastroenterol. Hepatol. 2009, 6, 573. [Google Scholar] [CrossRef]
- Berzigotti, A.; Reig, M.; Abraldes, J.G.; Bosch, J.; Bruix, J. Portal hypertension and the outcome of surgery for hepatocellular carcinoma in compensated cirrhosis: A systematic review and meta-analysis. Hepatology 2015, 61, 526–536. [Google Scholar] [CrossRef]
- Müller, L.; Hahn, F.; Mähringer-Kunz, A.; Stoehr, F.; Gairing, S.J.; Foerster, F.; Weinmann, A.; Galle, P.R.; Mittler, J.; Pinto dos Santos, D. Prevalence and clinical significance of clinically evident portal hypertension in patients with hepatocellular carcinoma undergoing transarterial chemoembolization. United Eur. Gastroenterol. J. 2022, 10, 41–53. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.H.; Lee, T.; Cho, Y.K.; Kim, B.I.; Kim, H.J. Impact of clinically evident portal hypertension on clinical outcome of patients with hepatocellular carcinoma treated by transarterial chemoembolization. J. Gastroenterol. Hepatol. 2018, 33, 1397–1406. [Google Scholar] [CrossRef]
- European Association For The Study Of The Liver. EASL–EORTC clinical practice guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2012, 56, 908–943. [Google Scholar]
- Choi, J.W.; Chung, J.W.; Lee, D.H.; Kim, H.-C.; Hur, S.; Lee, M.; Jae, H.J. Portal hypertension is associated with poor outcome of transarterial chemoembolization in patients with hepatocellular carcinoma. Eur. Radiol. 2018, 28, 2184–2193. [Google Scholar] [CrossRef]
- Iranmanesh, P.; Vazquez, O.; Terraz, S.; Majno, P.; Spahr, L.; Poncet, A.; Morel, P.; Mentha, G.; Toso, C. Accurate computed tomography-based portal pressure assessment in patients with hepatocellular carcinoma. J. Hepatol. 2014, 60, 969–974. [Google Scholar] [CrossRef]
- Takeishi, K.; Kawanaka, H.; Itoh, S.; Harimoto, N.; Ikegami, T.; Yoshizumi, T.; Shirabe, K.; Maehara, Y. Impact of splenic volume and splenectomy on prognosis of hepatocellular carcinoma within Milan criteria after curative hepatectomy. World J. Surg. 2018, 42, 1120–1128. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.S.; Lee, D.H.; Yoo, J.; Yi, N.-J.; Lee, K.-W.; Suh, K.-S.; Kim, H.; Lee, K.B. Association between spleen volume and the post-hepatectomy liver failure and overall survival of patients with hepatocellular carcinoma after resection. Eur. Radiol. 2021, 31, 2461–2471. [Google Scholar] [CrossRef] [PubMed]
- Ha, Y.; Kim, D.; Han, S.; Chon, Y.E.; Lee, Y.; Bin, Y.L.; Kim, M.N.; Lee, J.H.; Park, H.; Rim, K.S.; et al. Sarcopenia predicts prognosis in patients with newly diagnosed hepatocellular carcinoma, independent of tumor stage and liver function. Cancer Res. Treat. Off. J. Korean Cancer Assoc. 2018, 50, 843. [Google Scholar]
- Wu, W.-C.; Chiou, Y.-Y.; Hung, H.-H.; Kao, W.-Y.; Chou, Y.-H.; Su, C.-W.; Wu, J.-C.; Huo, T.-I.; Huang, Y.-H.; Lee, K.-C. Prognostic significance of computed tomography scan-derived splenic volume in hepatocellular carcinoma treated with radiofrequency ablation. J. Clin. Gastroenterol. 2012, 46, 789–795. [Google Scholar] [CrossRef]
- Müller, L.; Kloeckner, R.; Mähringer-Kunz, A.; Stoehr, F.; Düber, C.; Arnhold, G.; Gairing, S.J.; Foerster, F.; Weinmann, A.; Galle, P.R.; et al. Fully automated AI-based splenic segmentation for predicting survival and estimating the risk of hepatic decompensation in TACE patients with HCC. Eur. Radiol. 2022. [Google Scholar] [CrossRef]
- Lee, C.; Lee, S.S.; Choi, W.-M.; Kim, K.M.; Sung, Y.S.; Lee, S.; Lee, S.J.; Yoon, J.S.; Suk, H.-I. An index based on deep learning–measured spleen volume on CT for the assessment of high-risk varix in B-viral compensated cirrhosis. Eur. Radiol. 2021, 31, 3355–3365. [Google Scholar] [CrossRef]
- Reig, M.; Forner, A.; Rimola, J.; Ferrer-Fábrega, J.; Burrel, M.; Garcia-Criado, A.; Kelley, R.K.; Galle, P.R.; Mazzaferro, V.; Salem, R. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J. Hepatol. 2022, 76, 681–693. [Google Scholar] [CrossRef]
- Galle, P.R.; Dufour, J.-F.; Peck-Radosavljevic, M.; Trojan, J.; Vogel, A. Systemic therapy of advanced hepatocellular carcinoma. Futur. Oncol. 2021, 17, 1237–1251. [Google Scholar] [CrossRef]
- Foerster, F.; Gairing, S.J.; Ilyas, S.I.; Galle, P.R. Emerging Immunotherapy for Hepatocellular Carcinoma: A Guide for Hepatologists. Hepatology 2022, 75, 1604–1626. [Google Scholar] [CrossRef]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef]
- Cheng, A.-L.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Lim, H.Y.; Kudo, M.; Breder, V.; Merle, P. Updated efficacy and safety data from IMbrave150: Atezolizumab plus bevacizumab vs. sorafenib for unresectable hepatocellular carcinoma. J. Hepatol. 2022, 76, 862–873. [Google Scholar] [CrossRef] [PubMed]
- Foerster, F.; Galle, P.R. The current landscape of clinical trials for systemic treatment of hcc. Cancers 2021, 13, 1962. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.M.; Castet, F.; Heikenwalder, M.; Maini, M.K.; Mazzaferro, V.; Pinato, D.J.; Pikarsky, E.; Zhu, A.X.; Finn, R.S. Immunotherapies for hepatocellular carcinoma. Nat. Rev. Clin. Oncol. 2022, 19, 151–172. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Casals, M.; Brahmer, J.R.; Callahan, M.K.; Flores-Chávez, A.; Keegan, N.; Khamashta, M.A.; Lambotte, O.; Mariette, X.; Prat, A.; Suárez-Almazor, M.E. Immune-related adverse events of checkpoint inhibitors. Nat. Rev. Dis. Prim. 2020, 6, 1–21. [Google Scholar] [CrossRef]
- Susok, L.; Reinert, D.; Lukas, C.; Stockfleth, E.; Gambichler, T. Volume increase of spleen in melanoma patients undergoing immune checkpoint blockade. Immunotherapy 2021, 13, 885–891. [Google Scholar] [CrossRef]
- Galland, L.; Lecuelle, J.; Favier, L.; Fraisse, C.; Lagrange, A.; Kaderbhai, C.; Truntzer, C.; Ghiringhelli, F. Splenic Volume as a Surrogate Marker of Immune Checkpoint Inhibitor Efficacy in Metastatic Non Small Cell Lung Cancer. Cancers 2021, 13, 3020. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Müller, L.; Hahn, F.; Mähringer-Kunz, A.; Stoehr, F.; Gairing, S.J.; Foerster, F.; Weinmann, A.; Galle, P.R.; Mittler, J.; Pinto dos Santos, D. Immunonutritive Scoring in Patients With Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization: Prognostic Nutritional Index or Controlling Nutritional Status Score? Front. Oncol. 2021, 11, 2205. [Google Scholar] [CrossRef]
- Müller, D.; Kramer, F. MIScnn: A framework for medical image segmentation with convolutional neural networks and deep learning. BMC Med. Imaging 2021, 21, 1–11. [Google Scholar] [CrossRef]
- Nioche, C.; Orlhac, F.; Boughdad, S.; Reuzé, S.; Goya-Outi, J.; Robert, C.; Pellot-Barakat, C.; Soussan, M.; Frouin, F.; Buvat, I. LIFEx: A freeware for radiomic feature calculation in multimodality imaging to accelerate advances in the characterization of tumor heterogeneity. Cancer Res. 2018, 78, 4786–4789. [Google Scholar] [CrossRef] [Green Version]
- Nuffer, Z.; Marini, T.; Rupasov, A.; Kwak, S.; Bhatt, S. The best single measurement for assessing splenomegaly in patients with cirrhotic liver morphology. Acad. Radiol. 2017, 24, 1510–1516. [Google Scholar] [CrossRef] [PubMed]


| Parameter | All Patients (n = 50) |
|---|---|
| Age, years * | 67.2 (9.0) |
| Sex *** | |
| Female | 10 (20.0) |
| Male | 40 (80.0) |
| Etiology of cirrhosis *** | |
| Alcohol | 19 (38.0) |
| Viral | 7 (14.0) |
| Other | 11 (22.0) |
| No cirrhosis | 13 (26.0) |
| Child–Pugh stage *** | |
| A | 25 (50.0) |
| B | 10 (20.0) |
| C | 2 (4.0) |
| No cirrhosis | 13 (26.0) |
| ECOG *** | |
| ≤1 | 47 (94.0) |
| 2 | 3 (6.0) |
| BCLC stage *** | |
| B | 5 (10.0) |
| C | 42 (84.0) |
| D | 3 (6.0) |
| Portal vein invasion *** | |
| Yes | 26 (52.0) |
| No | 24 (48.0) |
| Distant metastasis *** | |
| Yes | 25 (50.0) |
| No | 25 (50.0) |
| Focality of the liver lesions *** | |
| Unifocal | 11 (22.0) |
| Multifocal | 39 (78.0) |
| Sum of the target lesion sizes, mm ** | 83 (51–135) |
| AFP, ng/mL ** | 277 (16–4485) |
| Albumin, g/L * | 30.4 (5.4) |
| Bilirubin, mg/dL ** | 1.5 (0.7–2.3) |
| INR ** | 1.2 (1.1–1.3) |
| Creatinine, mg/dL ** | 0.9 (0.7–1.1) |
| Thrombocytes, per nL ** | 139 (94–260) |
| Immunotherapy agent *** | |
| Atezolizumab + bevazizumab | 29 (58.0) |
| Pembrolizumab | 11 (22.0) |
| Nivolumab | 10 (20.0) |
| Line of systemic treatment *** | |
| First | 29 (58.0) |
| Second | 11 (22.0) |
| Third | 10 (20.0) |
| Previous therapy *** | |
| Yes | 42 (84.0) |
| No | 8 (16.0) |
| Subsequent therapy *** | |
| Yes | 13 (26.0) |
| No | 37 (64.0) |
| Parameter | Low SV (n = 25) | High SV (n = 25) | p-Value |
|---|---|---|---|
| Liver function | |||
| Albumin, g/L * | 32.2 (5.9) | 28.5 (4.21) | 0.014 |
| Bilirubin, mg/dL ** | 0.8 (0.6–1.6) | 2.1 (1.5–2.7) | <0.001 |
| Thrombocytes, per nL ** | 224 (138–315) | 101 (75–139) | <0.001 |
| INR ** | 1.1 (1.1–1.3) | 1.2 (1.1–1.4) | 0.190 |
| Tumor burden | |||
| Sum of the target lesions, mm ** | 76 (50–122) | 88 (51–156) | 0.663 |
| Presence of portal vein infiltration *** | 13 (52.0) | 13 (52.0) | 1.000 |
| Presence of distant metastasis *** | 16 (64.0) | 9 (36.0) | 0.089 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Müller, L.; Gairing, S.J.; Kloeckner, R.; Foerster, F.; Weinmann, A.; Mittler, J.; Stoehr, F.; Emrich, T.; Düber, C.; Galle, P.R.; et al. Baseline Splenic Volume Outweighs Immuno-Modulated Size Changes with Regard to Survival Outcome in Patients with Hepatocellular Carcinoma under Immunotherapy. Cancers 2022, 14, 3574. https://doi.org/10.3390/cancers14153574
Müller L, Gairing SJ, Kloeckner R, Foerster F, Weinmann A, Mittler J, Stoehr F, Emrich T, Düber C, Galle PR, et al. Baseline Splenic Volume Outweighs Immuno-Modulated Size Changes with Regard to Survival Outcome in Patients with Hepatocellular Carcinoma under Immunotherapy. Cancers. 2022; 14(15):3574. https://doi.org/10.3390/cancers14153574
Chicago/Turabian StyleMüller, Lukas, Simon Johannes Gairing, Roman Kloeckner, Friedrich Foerster, Arndt Weinmann, Jens Mittler, Fabian Stoehr, Tilman Emrich, Christoph Düber, Peter Robert Galle, and et al. 2022. "Baseline Splenic Volume Outweighs Immuno-Modulated Size Changes with Regard to Survival Outcome in Patients with Hepatocellular Carcinoma under Immunotherapy" Cancers 14, no. 15: 3574. https://doi.org/10.3390/cancers14153574
APA StyleMüller, L., Gairing, S. J., Kloeckner, R., Foerster, F., Weinmann, A., Mittler, J., Stoehr, F., Emrich, T., Düber, C., Galle, P. R., & Hahn, F. (2022). Baseline Splenic Volume Outweighs Immuno-Modulated Size Changes with Regard to Survival Outcome in Patients with Hepatocellular Carcinoma under Immunotherapy. Cancers, 14(15), 3574. https://doi.org/10.3390/cancers14153574








