Leydig Cell Tumors of the Testis: An Update of the Imaging Characteristics of a Not So Rare Lesion
Abstract
Simple Summary
Abstract
1. Introduction
2. Literature Review Protocol and Eligibility Criteria
3. Multiparametric Ultrasound
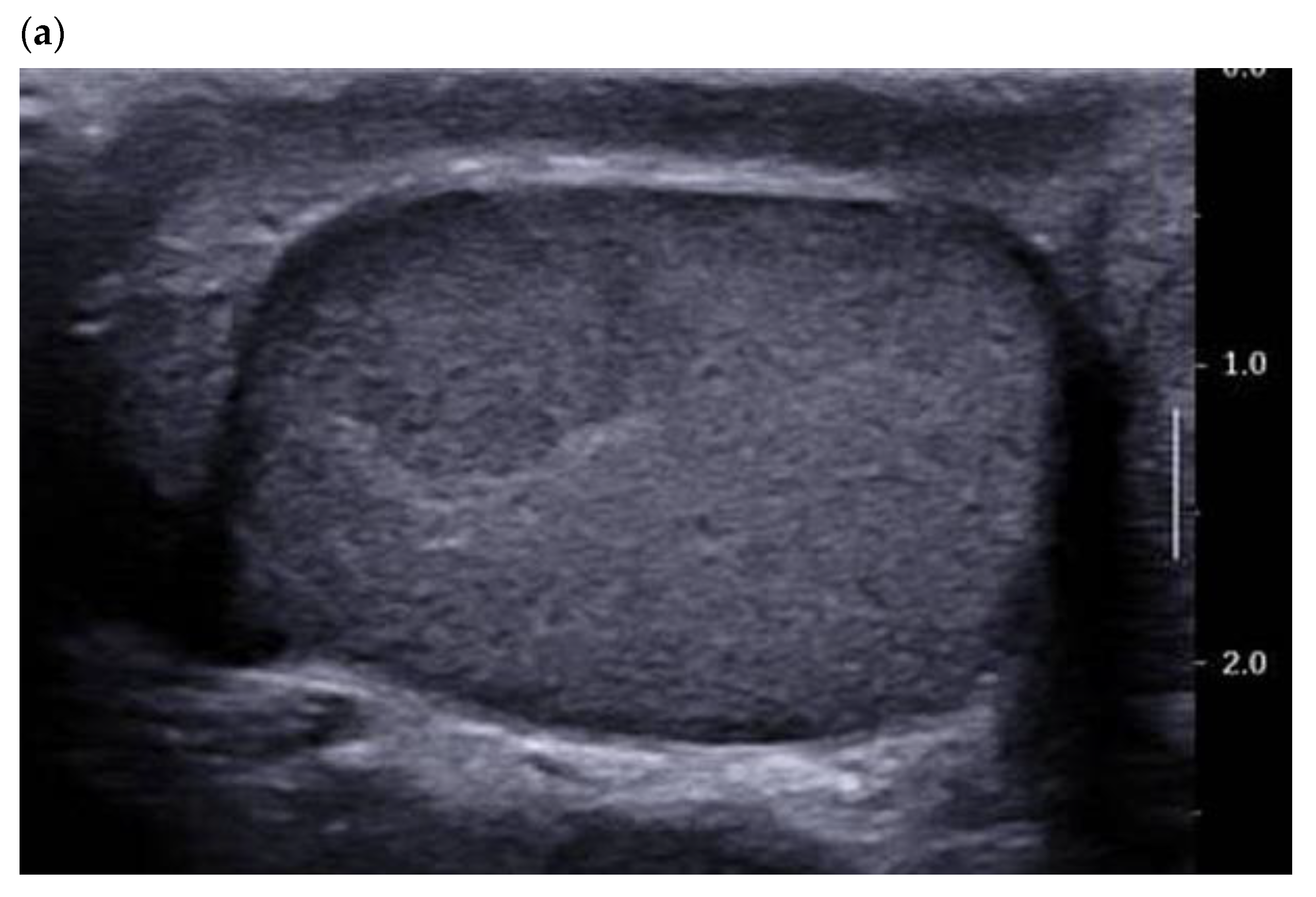
3.1. B-Mode Ultrasound
3.2. Color Doppler and Ultrasensitive Doppler
3.3. Contrast-Enhanced Ultrasound
3.4. Elastography
4. Multi Parametric MRI
4.1. Morphological T1 and T2 Sequences
4.2. Functional Sequences: Diffusion-Weighted Imaging—Apparent Diffusion Coefficient
4.3. Dynamic Contrast-Enhanced MRI
5. Leydig Cell Hyperplasia/Tumor Associated with Klinefelter Syndrome
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kim, I.; Young, R.H.; Scully, R.E. Leydig cell tumors of the testis. A clinicopathological analysis of 40 cases and review of the literature. Am. J. Surg. Pathol. 1985, 9, 177–192. [Google Scholar] [CrossRef]
- Isidori, A.M.; Pozza, C.; Gianfrilli, D.; Giannetta, E.; Lemma, A.; Pofi, R.; Barbagallo, F.; Manganaro, L.; Martino, G.; Lombardo, F.; et al. Differential Diagnosis of Nonpalpable Testicular Lesions: Qualitative and Quantitative Contrast-enhanced US of Benign and Malignant Testicular Tumors. Radiology 2014, 273, 606–618. [Google Scholar] [CrossRef] [PubMed]
- Colecchia, M.; Nistal, M.; Gonzalez-Peramato, P.; Carmignani, L.; Salvioni, R.; Nicolai, N.; Regadera, J. Leydig cell tumor and hyperplasia: A review. Anal. Quant. Cytol. Histol. 2007, 29, 139–147. [Google Scholar]
- Hendry, J.; Fraser, S.; White, J.; Rajan, P.; Hendry, D.S. Retroperitoneal lymph node dissection (RPLND) for malignant phenotype Leydig cell tumours of the testis: A 10-year experience. SpringerPlus 2015, 4, 20. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ruf, C.G.; Sanatgar, N.; Isbarn, H.; Ruf, B.; Simon, J.; Fankhauser, C.D.; Dieckmann, K.-P. Leydig-cell tumour of the testis: Retrospective analysis of clinical and therapeutic features in 204 cases. World J. Urol. 2020, 38, 2857–2862. [Google Scholar] [CrossRef] [PubMed]
- Albers, P.; Albrecht, W.; Algaba, F.; Bokemeyer, C.; Cohn-Cedermark, G.; Fizazi, K.; Horwich, A.; Laguna, M.P.; Nicolai, N.; Oldenburg, J. Guidelines on Testicular Cancer: 2015 Update. Eur. Urol. 2015, 68, 1054–1068. [Google Scholar] [CrossRef]
- Rocher, L.; Ramchandani, P.; Belfield, J.; Bertolotto, M.; Derchi, L.E.; Correas, J.M.; Oyen, R.; Tsili, A.C.; Turgut, A.T.; Dogra, V.; et al. Incidentally detected non-palpable testicular tumours in adults at scrotal ultrasound: Impact of radiological findings on management Radiologic review and recommendations of the ESUR scrotal imaging subcommittee. Eur. Radiol. 2016, 26, 2268–2278. [Google Scholar] [CrossRef] [PubMed]
- Pozza, C.; Pofi, R.; Tenuta, M.; Tarsitano, M.G.; Sbardella, E.; Fattorini, G.; Cantisani, V.; Lenzi, A.; Isidori, A.M.; Gianfrilli, D.; et al. Clinical presentation, management and follow-up of 83 patients with Leydig cell tumors of the testis: A prospective case-cohort study. Hum. Reprod. Oxf. Engl. 2019, 34, 1389–1403. [Google Scholar] [CrossRef] [PubMed]
- Rocher, L.; Moya, L.; Correas, J.M.; Mutuon, P.; Ferlicot, S.; Young, J.; Izard, V.; Benoit, G.; Brailly-Tabard, S.; Bellin, M.F. Testis ultrasound in Klinefelter syndrome infertile men: Making the diagnosis and avoiding inappropriate management. Abdom. Radiol. NY 2016, 41, 1596–1603. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, F.; Izard, V.; Ferlicot, S.; Rachas, A.; Correas, J.-M.; Benoit, G.; Bellin, M.-F.; Rocher, L. Colour Doppler and ultrasound characteristics of testicular Leydig cell tumours. Br. J. Radiol. 2016, 89, 20160089. [Google Scholar] [CrossRef] [PubMed]
- Richenberg, J.; Belfield, J.; Ramchandani, P.; Rocher, L.; Freeman, S.; Tsili, A.C.; Cuthbert, F.; Studniarek, M.; Bertolotto, M.; Turgut, A.T.; et al. Testicular microlithiasis imaging and follow-up: Guidelines of the ESUR scrotal imaging subcommittee. Eur. Radiol. 2015, 25, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Maizlin, Z.V.; Belenky, A.; Kunichezky, M.; Sandbank, J.; Strauss, S. Leydig Cell Tumors of the Testis: Gray scale and color Doppler sonographic appearance. J. Ultrasound. Med. Off. J. Am. Inst. Ultrasound Med. 2004, 23, 959–964. [Google Scholar] [CrossRef] [PubMed]
- Lock, G.; Schröder, C.; Schmidt, C.; Anheuser, P.; Loening, T.; Dieckmann, K.P. Contrast-Enhanced Ultrasound and Real-Time Elastography for the Diagnosis of Benign Leydig Cell Tumors of the Testis—A Single Center Report on 13 Cases. Ultraschall Med. Eur. J. Ultrasound 2014, 35, 534–539. [Google Scholar] [CrossRef]
- Rocher, L.; Ksouri, A.; Maxwell, F.; Bresson, B.; Hindawi, G.; Balasa, C.; Bellin, M.F.; Albiges, L. Testicular tumors: A diagnostic challenge of imaging. Bull. Cancer 2019, 106, 875–886. [Google Scholar] [CrossRef]
- Xu, Z.-Q.; Zhao, D.; Tian, B.-L.; Wang, Y.-B. Ultrasound characteristics of testicular Leydig cell tumors, 1. Zhonghua Nan Ke Xue Natl. J. Androl. 2019, 25, 346–350. [Google Scholar]
- Rocher, L.; Gennisson, J.-L.; Ferlicot, S.; Criton, A.; Albiges, L.; Izard, V.; Bellin, M.F.; Correas, J.-M. Testicular ultrasensitive Doppler preliminary experience: A feasibility study. Acta Radiol. Stockh 1987 2018, 59, 346–354. [Google Scholar] [CrossRef]
- Huang, D.Y.; Sidhu, P.S. Focal testicular lesions: Colour Doppler ultrasound, contrast-enhanced ultrasound and tissue elastography as adjuvants to the diagnosis. Br. J. Radiol. 2012, 85, S41–S53. [Google Scholar] [CrossRef]
- Luzurier, A.; Maxwell, F.; Correas, J.M.; Benoit, G.; Izard, V.; Ferlicot, S.; Teglas, J.; Bellin, M.; Rocher, L. Qualitative and quantitative contrast-enhanced ultrasonography for the characterisation of non-palpable testicular tumours. Clin. Radiol. 2018, 73, 322.e1–322.e9. [Google Scholar] [CrossRef]
- Drudi, F.M.; Valentino, M.; Bertolotto, M.; Malpassini, F.; Maghella, F.; Cantisani, V.; Liberatore, M.; De Felice, C.; D’Ambrosio, F. CEUS Time Intensity Curves in the Differentiation Between Leydig Cell Carcinoma and Seminoma: A Multicenter Study. Ultraschall. Med. Stuttg Ger 1980 2016, 37, 201–205. [Google Scholar] [CrossRef]
- Vandaele, P.; Marcelli, F.; Ouzzane, A.; Puech, P.; Villers, A.; Rigot, J.-M. Testicular nodules of infertile men and contrast enhanced ultrasonography: Preliminary study. Progres. En. Urol. J. Asso.c Francaise Urol. Soc. Francaise Urol. 2015, 25, 274–281. [Google Scholar] [CrossRef]
- Auer, T.; De Zordo, T.; Dejaco, C.; Gruber, L.; Pichler, R.; Jaschke, W.; Dogra, V.S.; Aigner, F. Value of Multiparametric US in the Assessment of Intratesticular Lesions. Radiology 2017, 285, 640–649. [Google Scholar] [CrossRef]
- Goddi, A.; Sacchi, A.; Magistretti, G.; Almolla, J.; Salvadore, M. Real-time tissue elastography for testicular lesion assessment. Eur. Radiol. 2012, 22, 721–730. [Google Scholar] [CrossRef]
- Pozza, C.; Gianfrilli, D.; Fattorini, G.; Giannetta, E.; Barbagallo, F.; Nicolai, E.; Cristini, C.; Di Pierro, G.B.; Franco, G.; Lenzi, A.; et al. Diagnostic value of qualitative and strain ratio elastography in the differential diagnosis of non-palpable testicular lesions. Andrology 2016, 4, 1193–1203. [Google Scholar] [CrossRef]
- Konstantatou, E.; Fang, C.; Romanos, O.; Derchi, L.E.; Bertolotto, M.; Valentino, M.; Kalogeropoulou, C.; Sidhu, P.S. Evaluation of Intratesticular Lesions with Strain Elastography Using Strain Ratio and Color Map Visual Grading: Differentiation of Neoplastic and Nonneoplastic Lesions. Ultrasound Med. Off. J. Am. Inst. J. Ultrasound Med. 2019, 38, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Roy, C.; de Marini, P.; Labani, A.; Leyendecker, P.; Ohana, M. Shear-wave elastography of the testicle: Potential role of the stiffness value in various common testicular diseases. Clin. Radiol. 2020, 75, 560.e9–560.e17. [Google Scholar] [CrossRef]
- Rocher, L.; Criton, A.; Gennisson, J.-L.; Creze, M.; Albiges, L.; Ferlicot, S.; Bellin, M.-F.; Izard, V.; Correas, J.-M. Characterization of Testicular Masses in Adults: Performance of Combined Quantitative Shear Wave Elastography and Conventional Ultrasound. Ultrasound Med. Biol. 2019, 45, 720–731. [Google Scholar] [CrossRef] [PubMed]
- Tsitouridis, I.; Maskalidis, C.; Panagiotidou, D.; Kariki, E.P. Eleven Patients with Testicular Leydig Cell Tumors: Clinical, im-aging, and pathologic correlation. J. Ultrasound Med. Off. J. Am. Inst. J. Ultrasound Med. 2014, 33, 1855–1864. [Google Scholar] [CrossRef]
- Manganaro, L.; Vinci, V.; Pozza, C.; Saldari, M.; Gianfrilli, D.; Pofi, R.; Bernardo, S.; Cantisani, V.; Lenzi, A.; Scialpi, M.; et al. A prospective study on contrast-enhanced magnetic resonance imaging of testicular lesions: Distinctive features of Leydig cell tumours. Eur. Radiol. 2015, 25, 3586–3595. [Google Scholar] [CrossRef]
- El Sanharawi, I.; Correas, J.-M.; Glas, L.; Ferlicot, S.; Izard, V.; Ducot, B.; Bellin, M.-F.; Benoît, G.; Rocher, L. Non-palpable incidentally found testicular tumors: Differentiation between benign, malignant, and burned-out tumors using dynamic contrast-enhanced MRI. Eur. J. Radiol. 2016, 85, 2072–2082. [Google Scholar] [CrossRef] [PubMed]
- Tsili, A.C.; Giannakis, D.; Sylakos, A.; Ntorkou, A.; Astrakas, L.G.; Sofikitis, N.; I Argyropoulou, M. Apparent diffusion coefficient values of normal testis and variations with age. Asian J. Androl. 2014, 16, 493–497. [Google Scholar] [CrossRef]
- Tsili, A.C.; I Argyropoulou, M.; Giannakis, D.; Tsampalas, S.; Sofikitis, N.; Tsampoulas, K. Diffusion-weighted MR imaging of normal and abnormal scrotum: Preliminary results. Asian J. Androl. 2012, 14, 649–654. [Google Scholar] [CrossRef]
- Manganaro, L.; Saldari, M.; Pozza, C.; Vinci, V.; Gianfrilli, D.; Greco, E.; Franco, G.; Sergi, M.E.; Scialpi, M.; Catalano, C.; et al. Dynamic contrast-enhanced and diffusion-weighted MR imaging in the characterisation of small, non-palpable solid testicular tumours. Eur. Radiol. 2018, 28, 554–564. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Dohke, M.; Ohkubo, K.; Ishimori, T.; Amoh, Y.; Okumura, A.; Oda, K.; Hayashi, T.; Dodo, Y.; Arai, Y. Scrotal Disorders: Evaluation of Testicular Enhancement Patterns at Dynamic Contrast-enhanced Subtraction MR Imaging. Radiology 2000, 217, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Lanfranco, F.; Kamischke, A.; Zitzmann, M.; Nieschlag, E. Klinefelter’s syndrome. Lancet 2004, 364, 273–283. [Google Scholar] [CrossRef]
- Aguirre, D.; Nieto, K.; Lazos, M.; Peña, Y.R.; Palma, I.; Kofman-Alfaro, S.; Queipo, G. Extragonadal germ cell tumors are often associated with Klinefelter syndrome. Hum. Pathol. 2006, 37, 477–480. [Google Scholar] [CrossRef]









Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maxwell, F.; Savignac, A.; Bekdache, O.; Calvez, S.; Lebacle, C.; Arama, E.; Garrouche, N.; Rocher, L. Leydig Cell Tumors of the Testis: An Update of the Imaging Characteristics of a Not So Rare Lesion. Cancers 2022, 14, 3652. https://doi.org/10.3390/cancers14153652
Maxwell F, Savignac A, Bekdache O, Calvez S, Lebacle C, Arama E, Garrouche N, Rocher L. Leydig Cell Tumors of the Testis: An Update of the Imaging Characteristics of a Not So Rare Lesion. Cancers. 2022; 14(15):3652. https://doi.org/10.3390/cancers14153652
Chicago/Turabian StyleMaxwell, Florian, Alexia Savignac, Omar Bekdache, Sandra Calvez, Cédric Lebacle, Emmanuel Arama, Nada Garrouche, and Laurence Rocher. 2022. "Leydig Cell Tumors of the Testis: An Update of the Imaging Characteristics of a Not So Rare Lesion" Cancers 14, no. 15: 3652. https://doi.org/10.3390/cancers14153652
APA StyleMaxwell, F., Savignac, A., Bekdache, O., Calvez, S., Lebacle, C., Arama, E., Garrouche, N., & Rocher, L. (2022). Leydig Cell Tumors of the Testis: An Update of the Imaging Characteristics of a Not So Rare Lesion. Cancers, 14(15), 3652. https://doi.org/10.3390/cancers14153652






