Surgery vs. Biopsy in the Treatment of Butterfly Glioblastoma: A Systematic Review and Meta-Analysis
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Data Extraction
2.3. Quality Assessment
2.4. Statistical Methods and Analysis
2.5. Heterogeneity Assessment and Analysis
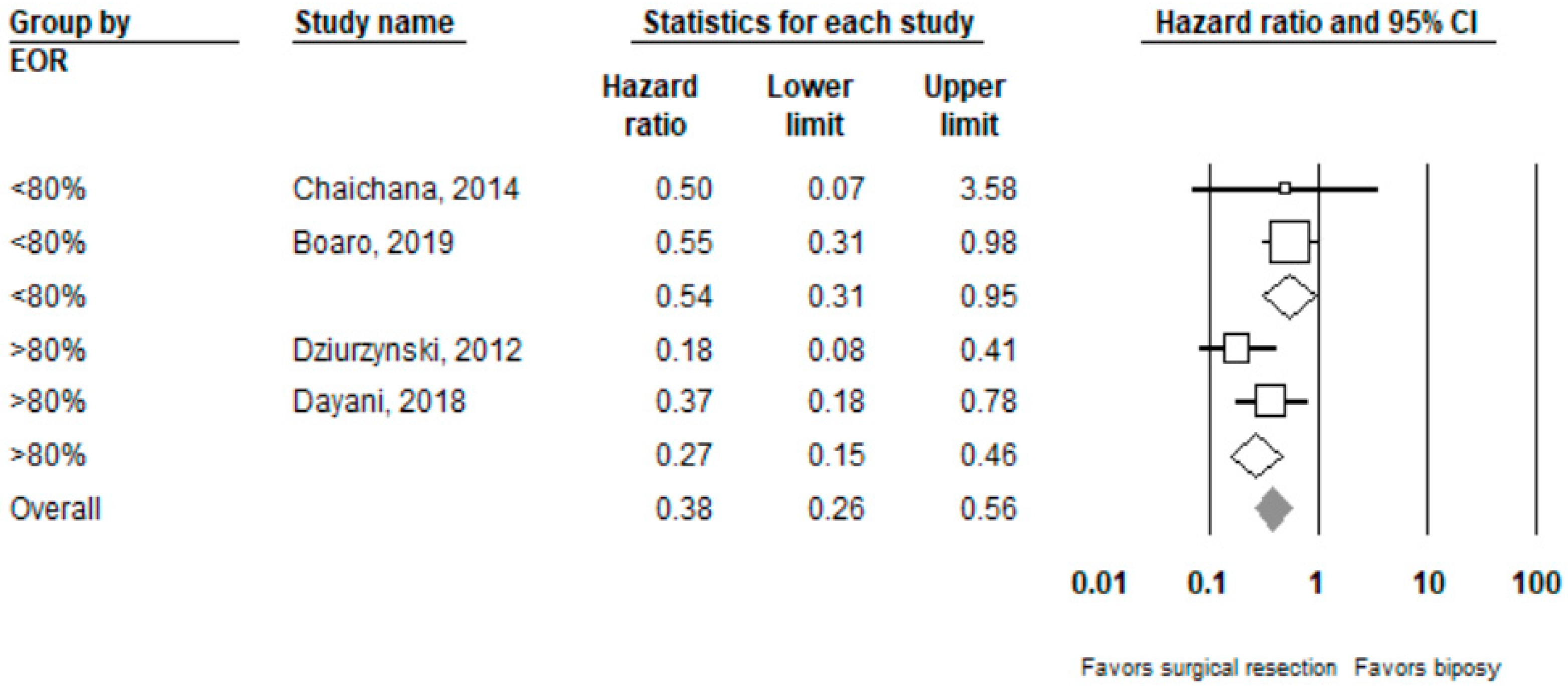
3. Results
3.1. Characteristics of Included Trials
3.2. Complications and Clinical Outcomes
3.3. Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
Appendix B
- calculate the test statistic for a normal distribution test, z, from P3: z = −0.862 + √[0.743 − 2.404 × log(P)].
- Est = log(HR).
- calculate the standard error: SE = − Est/z (ignoring minus signs).
- calculate the 95% CI: Est − 1.96 × SE to Est + 1.96 × SE.
- Convert to natural scale.
Appendix C
| Reference | Resection | Biopsy |
|---|---|---|
| Dziurzynski, 2012 | NR | NR |
| Chaichana, 2014 | Motor deficit—3 (10%) Language deficit—3 (10%) Vision deficit—1 (3%) | Motor deficit—3 (16%) Language deficit—1 (5%) Vision deficit—0 (0%) |
| Dayani, 2018 | N—4/14 Four cases with immediate post-op deficits, one with persistent post-op deficits 1—Rt-sided hemiplegia, rt-sided neglect, slurred speech; slight improvement but persistent deficit 2—Blurred vision, seizure; improved to baseline levels 3—Lt-sided neglect, lt-sided weakness, apraxia; lost to FU 4—Expressive aphasia, perceptual motor difficulties, mild rt visual field cut; improved to baseline levels | NR |
| OpokuDarko, 2018 | N—2/10 1—A significant thromboembolic complication resulting in multifocal infarcts in the peritumoral area and distal left ACA territory. Resulted in right hemiparesis, expressive dysphasia, and abulia 2—A postoperative epidural hemorrhage requiring evacuation and admission to the intensive care unit. | N—1/20 1—Postprocedural hemorrhage leading to obstructive hydrocephalus that required permanent placement of a ventriculoperitoneal shunt. |
| Boaro, 2019 | N—10/26 with new post-operative deficits Motor deficit—5 Language deficit—3 Cognitive deficit—5 Other: Seizures—3 Post-op hydrocephalus—5 Deep Vein Thrombosis/Pulmonary Embolism—4 | NR |
| Hall, 2019 | 7/36 with postoperative complications | 5/36 with postoperative complications |
| Franco, 2020 | N—8/25 Hemorrhage—3 Ischemia—1 Cranial nerve deficit—1 Meningitis—2 Hydrocephalus—1 Aphasia—1 Pneumonia—0 | N—5/30 Hemorrhage—0 Ischemia—0 Cranial nerve deficit—0 Meningitis—0 Hydrocephalus—2 Aphasia—2 Pneumonia—1 |
Appendix D
| Study | Clear Study Objectives/Question | Well Defined Study Protocol | Explicit Inclusion/Exclusion Criteria for Participants | Specified Time Interval for Patient Recruitment | Consecutive Patient Enrolment | Clinically Relevant Outcomes | Prospective Outcome Data Collection | High Follow-Up Rate | Overall |
|---|---|---|---|---|---|---|---|---|---|
| Dziurzynski, 2012 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Chaichana, 2014 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 6 |
| Dayani, 2018 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 6 |
| OpokuDarko, 2018 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 6 |
| Boaro, 2019 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 6 |
| Franco, 2020 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 6 |
References
- Balaña, C.; Capellades, J.; Teixidor, P.; Roussos, I.; Ballester, R.; Cuello, M.; Arellano, A.; Florensa, R.; Rosell, R. Clinical course of high-grade glioma patients with a “biopsy-only” surgical approach: A need for individualised treatment. Clin. Transl. Oncol. 2007, 9, 797–803. [Google Scholar] [CrossRef] [PubMed]
- Chaichana, K.L.; Jusue-Torres, I.; Lemos, A.M.; Gokaslan, A.; Cabrera-Aldana, E.E.; Ashary, A.; Olivi, A.; Quinones-Hinojosa, A. The butterfly effect on glioblastoma: Is volumetric extent of resection more effective than biopsy for these tumors? J. Neurooncol. 2014, 120, 625–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dziurzynski, K.; Blas-Boria, D.; Suki, D.; Cahill, D.; Prabhu, S.S.; Puduvalli, V.; Levine, N. Butterfly glioblastomas: A retrospective review and qualitative assessment of outcomes. J. Neurooncol. 2012, 109, 555–563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stensjøen, A.L.; Solheim, O.; Berntsen, E.M. Sommerfugl-gliom. Tidsskr. Den Nor. Legeforening 2014, 134, 309. [Google Scholar] [CrossRef] [PubMed]
- Van Kessel, E.; Baumfalk, A.E.; Van Zandvoort, M.J.E.; Robe, P.A.; Snijders, T. Tumor-related neurocognitive dysfunction in patients with diffuse glioma: A systematic review of neurocognitive functioning prior to anti-tumor treatment. J. Neuro-Oncol. 2017, 134, 9–18. [Google Scholar] [CrossRef]
- Dayani, F.; Young, J.S.; Bonte, A.; Chang, E.F.; Theodosopoulos, P.; McDermott, M.W.; Berger, M.S.; Aghi, M.K. Safety and outcomes of resection of butterfly glioblastoma. Neurosurg. Focus 2018, 44, E4. [Google Scholar] [CrossRef]
- Tunthanathip, T.; Ratanalert, S.; Sae-Heng, S.; Oearsakul, T. Butterfly Tumor of the Corpus Callosum: Clinical Characteristics, Diagnosis, and Survival Analysis. J. Neurosci. Rural Pract. 2017, 8, S57. [Google Scholar] [CrossRef]
- Colman, H. Potential survival benefit of resection in butterfly glioblastoma. Neurosurg. Focus 2018, 44, E5. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. Available online: https://www.bmj.com/content/372/bmj.n71 (accessed on 14 April 2021). [CrossRef]
- Chan, K.; Bhandari, M. Three-minute critical appraisal of a case series article. Indian J. Orthop. 2011, 45, 103. [Google Scholar] [CrossRef]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629. [Google Scholar] [CrossRef] [Green Version]
- Altman, D.G.; Bland, J.M. How to obtain the confidence interval from a P value. BMJ 2011, 343, d2090. [Google Scholar] [CrossRef] [Green Version]
- Der Simonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franco, P.; Delev, D.; Cipriani, D.; Neidert, N.; Kellner, E.; Masalha, W.; Mercas, B.; Mader, I.; Reinacher, P.; Weyerbrock, A.; et al. Surgery for IDH1/2 wild-type glioma invading the corpus callosum. Acta Neurochir. 2021, 163, 937–945. [Google Scholar] [CrossRef] [PubMed]
- Boaro, A.; Kavouridis, V.K.; Siddi, F.; Mezzalira, E.; Harary, M.; Iorgulescu, J.B.; Reardon, D.A.; Smith, T.R. Improved outcomes associated with maximal extent of resection for butterfly glioblastoma: Insights from institutional and national data. Acta Neurochir. 2021, 163, 1883–1894. [Google Scholar] [CrossRef] [PubMed]
- Opoku-Darko, M.; Amuah, J.E.; Kelly, J.J.P. Surgical Resection of Anterior and Posterior Butterfly Glioblastoma. World Neurosurg. 2018, 110, e612–e620. [Google Scholar] [CrossRef]
- Hall, B.J.; Maleyko, I.; Brodbelt, A.; Jenkinson, M.D.; Chavredakis, E. The utility of surgery in butterfly glioblastoma: A case-control study. J. Clin. Oncol. 2019, 37, e13529. [Google Scholar] [CrossRef]
- Chojak, R.; Koźba-Gosztyła, M.; Słychan, K.; Gajos, D.; Kotas, M.; Tyliszczak, M.; Czapiga, B. Impact of surgical resection of butterfly glioblastoma on survival: A meta-analysis based on comparative studies. Sci. Rep. 2021, 11, 13934. [Google Scholar] [CrossRef]
- Burks, J.D.; Bonney, P.A.; Conner, A.K.; Glenn, C.A.; Briggs, R.G.; Battiste, J.D.; McCoy, T.; O’Donoghue, D.L.; Wu, D.H.; Sughrue, M.E. A method for safely resecting anterior butterfly gliomas: The surgical anatomy of the default mode network and the relevance of its preservation. J. Neurosurg. 2016, 126, 1795–1811. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Reference | Country | Study Design | Study Period | Sample Size | Male Sex (%) | Mean Age (Years) | |
|---|---|---|---|---|---|---|---|
| Resection | Biopsy | ||||||
| Dziurzynski, 2012 | USA | Case series | 2000–2010 | 11 | 12 | 48% | 56.3 |
| Chaichana, 2014 | USA | Case series | 2007–2012 | 29 | 19 | 52% | NR |
| Dayani, 2018 | USA, Ireland | Case series | 2004–2014 | 14 | 25 | 59% | 57.8 |
| OpokuDarko, 2018 | Canada | Case series | 2004–2016 | 9 | 20 | 62% | 59.8 |
| Hall, 2019 | UK | Case control | 2011–2017 | 37 * | 64.9% | 62.7 * | |
| Franco, 2020 | Germany | Case series | 2005–2017 | 25 | 30 | 61.8% | 64 |
| Boaro, 2021 | USA, Italy | Case series | 2008–2018 | 26 | 36 | 51.6% | 64.3 |
| Resection | Biopsy | |
|---|---|---|
| Mean pre-operative tumor volume in cm3 | 48.9 | 44.1 |
| IDH1/2 Mutation% (n/N) | 1.59% (1/63) | 2.63% (2/76) |
| MGMT Methylation% (n/N) | 34.4% (21/61) | 34.8% (24/69) |
| Mean age *, years | 58.3 | 62.8 |
| Sex (% Male) * | 57.3% | 65.2% |
| Reference | Receipt of Adjuvant Therapy (%) | Overall Survival (Median Months) | Extent of Resection (Median) | |
|---|---|---|---|---|
| Chemotherapy | Radiation | |||
| Dziurzynski, 2012 | 39.10% | 52.20% | 5.9 | 100% |
| Chaichana, 2014 | NR | NR | NR | 61.4% |
| Dayani, 2018 | 43.60% | 12.80% | 3.2 | 83.04% |
| OpokuDarko, 2018 | NR | NR | 3.3 | NR |
| Boaro, 2021 | 71.00% | 75.80% | 8.7 | 72.30% |
| Hall, 2019 | NR | NR | 3.3 | NR |
| Franco, 2020 | 52.5% | 34.6% | 8.3 | NR |
| Complication | All | Surgery Subgroup | N of Studies | Biopsy Subgroup | N of Studies | Surgery vs. Biopsy p-Value |
|---|---|---|---|---|---|---|
| Motor | 7% (2%, 20%) | 11% (4%, 27%) | 5 | 1.3% (0%, 100%) | 3 | 0.33 |
| Speech and Language | 8% (4%, 15%) | 11% (5%, 22%) | 5 | 4% (0.3%, 37%) | 3 | 0.15 |
| Visuospatial | 0.4% (0%, 29%) | 1.59% (0.02%, 51.8%) | 5 | 0% (0%, 100%) | 3 | >0.99 |
| Cognition | 0.5% (0.01%, 30%) | 2% (0.04%, 49%) | 5 | 0% (0%, 100%) | 3 | >0.99 |
| Seizures | 10% (0.01%, 99%) | NR | NR | NR | NR | NR |
| Hydrocephalus | 7.4% (1.3%, 33%) | 7.84% (0.01%, 98%) | 2 | 7% (2%, 23%) | 1 | 0.85 |
| Total | 21% (14%, 31%) | 28% (18–41%) | 5 | 13% (4%, 37%) | 3 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chawla, S.; Kavouridis, V.K.; Boaro, A.; Korde, R.; Amaral Medeiros, S.; Edrees, H.; Mezzalira, E.; Sala, F.; Mekary, R.A.; Smith, T.R. Surgery vs. Biopsy in the Treatment of Butterfly Glioblastoma: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 314. https://doi.org/10.3390/cancers14020314
Chawla S, Kavouridis VK, Boaro A, Korde R, Amaral Medeiros S, Edrees H, Mezzalira E, Sala F, Mekary RA, Smith TR. Surgery vs. Biopsy in the Treatment of Butterfly Glioblastoma: A Systematic Review and Meta-Analysis. Cancers. 2022; 14(2):314. https://doi.org/10.3390/cancers14020314
Chicago/Turabian StyleChawla, Shreya, Vasileios K. Kavouridis, Alessandro Boaro, Rasika Korde, Sofia Amaral Medeiros, Heba Edrees, Elisabetta Mezzalira, Francesco Sala, Rania A. Mekary, and Timothy R. Smith. 2022. "Surgery vs. Biopsy in the Treatment of Butterfly Glioblastoma: A Systematic Review and Meta-Analysis" Cancers 14, no. 2: 314. https://doi.org/10.3390/cancers14020314
APA StyleChawla, S., Kavouridis, V. K., Boaro, A., Korde, R., Amaral Medeiros, S., Edrees, H., Mezzalira, E., Sala, F., Mekary, R. A., & Smith, T. R. (2022). Surgery vs. Biopsy in the Treatment of Butterfly Glioblastoma: A Systematic Review and Meta-Analysis. Cancers, 14(2), 314. https://doi.org/10.3390/cancers14020314






