Respiratory Tract Cancer Incidences across Industry Groups: A Nationwide Cohort Study with More Than 70 Million Person-Years of Follow-Up
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Cancers
2.3. Industrial Classification
2.4. Statistical Analysis
2.5. Ethics Statement
3. Results
4. Discussion
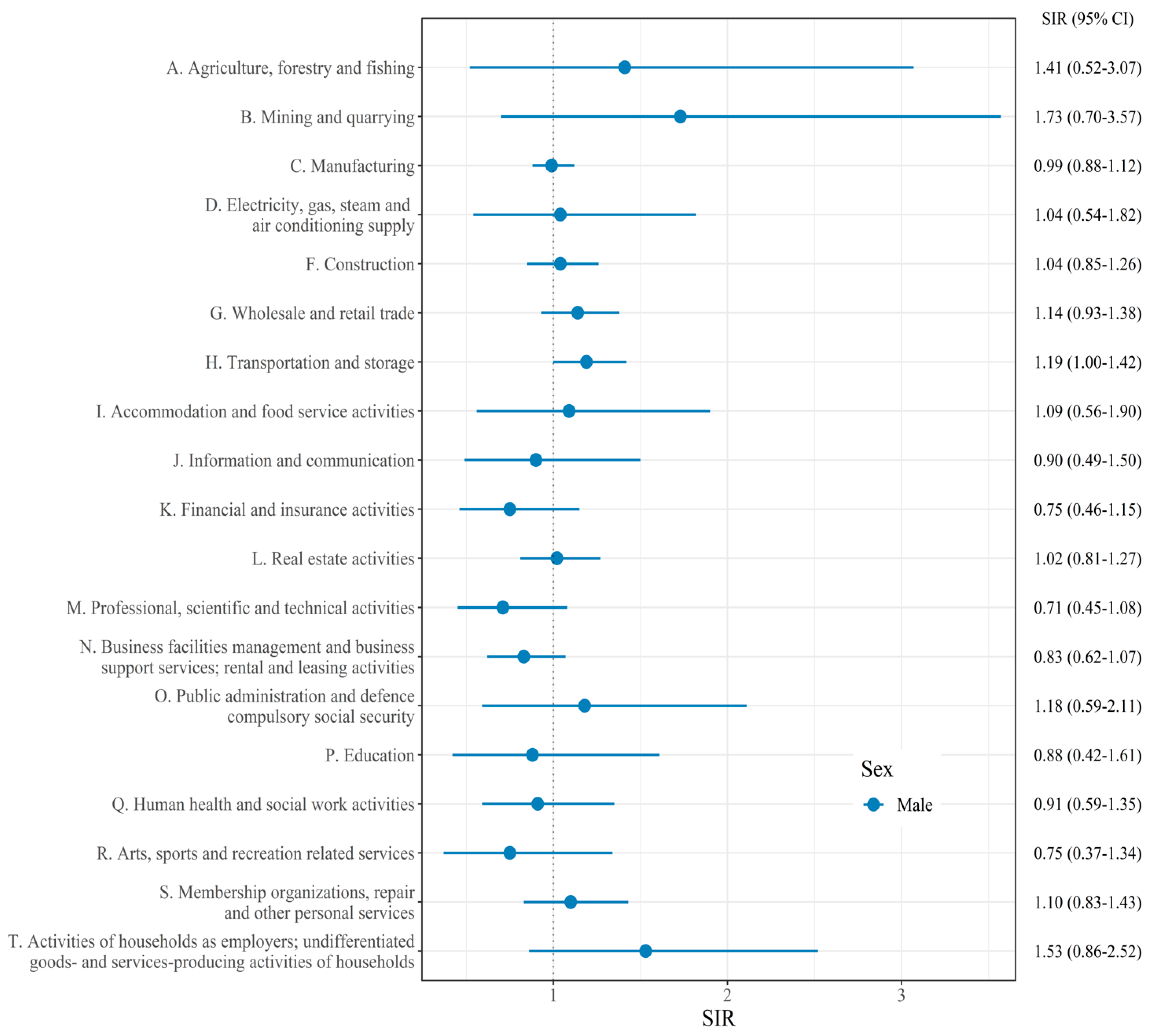
4.1. Laryngeal Cancer
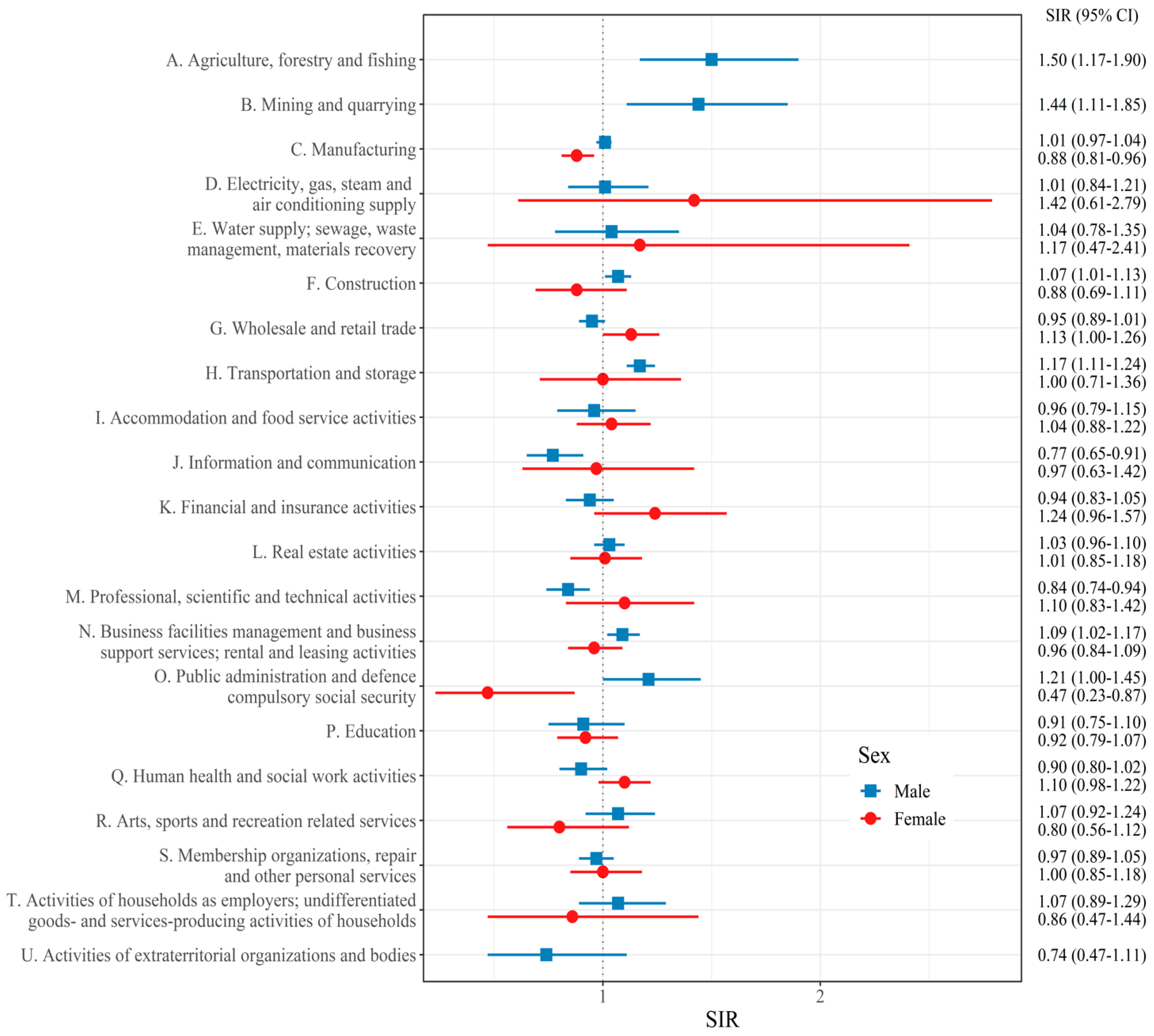
4.2. Lung Cancer
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2019 Respiratory Tract Cancers Collaborators. Global, regional, and national burden of respiratory tract cancers and associated risk factors from 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Respir. Med. 2021, 9, 1030–1049. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.J.; Won, Y.J.; Lee, J.J.; Jung, K.W.; Kim, H.J.; Kong, H.J.; Im, J.S.; Seo, H.G.; The Community of Population-Based Regional Cancer Registries. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2019. Cancer Res. Treat. 2022, 54, 330–344. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease Cancer Collaboration. Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2022, 8, 420–444. [Google Scholar] [CrossRef] [PubMed]
- Rushton, L.; Bagga, S.; Bevan, R.; Brown, T.P.; Cherrie, J.W.; Holmes, P.; Fortunato, L.; Slack, R.; Van Tongeren, M.; Young, C.; et al. Occupation and cancer in Britain. Br. J. Cancer 2010, 102, 1428–1437. [Google Scholar] [CrossRef]
- Loomis, D.; Guha, N.; Hall, A.L.; Straif, K. Identifying occupational carcinogens: An update from the IARC Monographs. Occup. Environ. Med. 2018, 75, 593–603. [Google Scholar] [CrossRef]
- Kogevinas, M.; Sala, M.; Boffetta, P.; Kazerouni, N.; Kromhout, H.; Hoar-Zahm, S. Cancer risk in the rubber industry: A review of the recent epidemiological evidence. Occup. Environ. Med. 1998, 55, 1–12. [Google Scholar] [CrossRef]
- Boniol, M.; Koechlin, A.; Boyle, P. Meta-analysis of occupational exposures in the rubber manufacturing industry and risk of cancer. Int. J. Epidemiol. 2017, 46, 1940–1947. [Google Scholar] [CrossRef]
- Cheol Seong, S.; Kim, Y.Y.; Khang, Y.H.; Heon Park, J.; Kang, H.J.; Lee, H.; Do, C.H.; Song, J.S.; Hyon Bang, J.; Ha, S.; et al. Data Resource Profile: The National Health Information Database of the National Health Insurance Service in South Korea. Int. J. Epidemiol. 2017, 46, 799–800. [Google Scholar] [CrossRef]
- Shin, D.W.; Cho, B.; Guallar, E. Korean national health insurance database. JAMA Intern. Med. 2016, 176, 138. [Google Scholar] [CrossRef]
- Statistics Korea. Korean Standard Industrial Classfication. Available online: https://kssc.kostat.go.kr:8443/ksscNew_web/ekssc/main/main.do# (accessed on 30 August 2022).
- de la Cour, C.D.; Munk, C.; Aalborg, G.L.; Kjaer, S.K. Base of tongue/tonsillar and laryngeal cancer in Denmark 1994-2018: Temporal trends in incidence according to education and age. Oral. Oncol. 2022, 128, 105832. [Google Scholar] [CrossRef]
- White, M.C.; Holman, D.M.; Boehm, J.E.; Peipins, L.A.; Grossman, M.; Henley, S.J. Age and cancer risk: A potentially modifiable relationship. Am. J. Prev. Med. 2014, 46, S7–S15. [Google Scholar] [CrossRef]
- Kim, H.R. Overview of asbestos issues in Korea. J. Korean Med. Sci. 2009, 24, 363–367. [Google Scholar] [CrossRef]
- Flanders, W.D.; Rothman, K.J. Occupational risk for laryngeal cancer. Am. J. Public Health 1982, 72, 369–372. [Google Scholar] [CrossRef]
- Laakkonen, A.; Kauppinen, T.; Pukkala, E. Cancer risk among Finnish food industry workers. Int. J. Cancer 2006, 118, 2567–2571. [Google Scholar] [CrossRef]
- Bayer, O.; Camara, R.; Zeissig, S.R.; Ressing, M.; Dietz, A.; Locati, L.D.; Ramroth, H.; Singer, S. Occupation and cancer of the larynx: A systematic review and meta-analysis. Eur. Arch. Otorhinolaryngol. 2016, 273, 9–20. [Google Scholar] [CrossRef]
- Elci, O.C.; Dosemeci, M.; Blair, A. Occupation and the risk of laryngeal cancer in Turkey. Scand. J. Work Environ. Health 2001, 27, 233–239. [Google Scholar] [CrossRef]
- Aronson, K.J.; Howe, G.R.; Carpenter, M.; Fair, M.E. Surveillance of potential associations between occupations and causes of death in Canada, 1965–1991. Occup. Environ. Med. 1999, 56, 265–269. [Google Scholar] [CrossRef]
- Elci, O.C.; Akpinar-Elci, M.; Blair, A.; Dosemeci, M. Risk of laryngeal cancer by occupational chemical exposure in Turkey. J. Occup. Environ. Med. 2003, 45, 1100–1106. [Google Scholar] [CrossRef]
- Paget-Bailly, S.; Cyr, D.; Luce, D. Occupational exposures and cancer of the larynx-systematic review and meta-analysis. J. Occup. Environ. Med. 2012, 54, 71–84. [Google Scholar] [CrossRef]
- Kim, H.B.; Shim, J.Y.; Park, B.; Lee, Y.J. Long-Term Exposure to Air Pollutants and Cancer Mortality: A Meta-Analysis of Cohort Studies. Int. J. Environ. Res. Public Health 2018, 15, 2608. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.; Xu, R.; Li, S.; Coelho, M.; Saldiva, P.H.N.; Sim, M.R.; Abramson, M.J.; Guo, Y. Associations between long-term exposure to PM2.5 and site-specific cancer mortality: A nationwide study in Brazil between 2010 and 2018. Environ. Pollut. 2022, 302, 119070. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Deng, W.; Liu, Y.; Zhao, W.; Liu, J.; Cao, Y.; Deng, J. Association between ambient air pollution and laryngeal neoplasms incidence in twelve major Chinese cities, 2006–2013. Environ. Sci. Pollut. Res. Int. 2020, 27, 39274–39282. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Kamal, R.; Ahamed, I.; Wagh, M.; Bihari, V.; Sathian, B.; Kesavachandran, C.N. PAH exposure-associated lung cancer: An updated meta-analysis. Occup. Med. 2018, 68, 255–261. [Google Scholar] [CrossRef]
- Cardis, E.; Vrijheid, M.; Blettner, M.; Gilbert, E.; Hakama, M.; Hill, C.; Howe, G.; Kaldor, J.; Muirhead, C.R.; Schubauer-Berigan, M.; et al. The 15-Country Collaborative Study of Cancer Risk among Radiation Workers in the Nuclear Industry: Estimates of radiation-related cancer risks. Radiat. Res. 2007, 167, 396–416. [Google Scholar] [CrossRef]
- Hancock, D.G.; Langley, M.E.; Chia, K.L.; Woodman, R.J.; Shanahan, E.M. Wood dust exposure and lung cancer risk: A meta-analysis. Occup. Environ. Med. 2015, 72, 889–898. [Google Scholar] [CrossRef]
- Li, L.; Jiang, M.; Li, X.; Zhou, B. Association between Coalmine Dust and Mortality Risk of Lung Cancer: A Meta-Analysis. Biomed. Res. Int. 2021, 2021, 6624799. [Google Scholar] [CrossRef]
- Lee, W.; Kang, M.Y.; Kim, J.; Lim, S.S.; Yoon, J.H. Cancer risk in road transportation workers: A national representative cohort study with 600,000 person-years of follow-up. Sci. Rep. 2020, 10, 11331. [Google Scholar] [CrossRef]
- Jung, J.K.H.; Feinstein, S.G.; Palma Lazgare, L.; Macleod, J.S.; Arrandale, V.H.; McLeod, C.B.; Peter, A.; Demers, P.A. Examining lung cancer risks across different industries and occupations in Ontario, Canada: The establishment of the Occupational Disease Surveillance System. Occup. Environ. Med. 2018, 75, 545–552. [Google Scholar] [CrossRef]
- Prideaux, B. The role of the transport system in destination development. Tour. Manag. 2000, 21, 53–63. [Google Scholar] [CrossRef]
- Ugelvig Petersen, K.; Pukkala, E.; Martinsen, J.I.; Lynge, E.; Tryggvadottir, L.; Weiderpass, E.; Kjaerheim, K.; Heikkinen, S.; Hansen, J. Cancer incidence among seafarers and fishermen in the Nordic countries. Scand. J. Work Environ. Health 2020, 46, 461–468. [Google Scholar] [CrossRef]
- Eguchi, H.; Wada, K.; Prieto-Merino, D.; Smith, D.R. Lung, gastric and colorectal cancer mortality by occupation and industry among working-aged men in Japan. Sci. Rep. 2017, 7, 43204. [Google Scholar] [CrossRef]
- Oldenburg, M.; Baur, X.; Schlaich, C. Occupational risks and challenges of seafaring. J. Occup. Health 2010, 52, 249–256. [Google Scholar] [CrossRef]
- Tual, S.; Lemarchand, C.; Boulanger, M.; Dalphin, J.C.; Rachet, B.; Marcotullio, E.; Velten, M.; Guizard, A.V.; Clin, B.; Baldi, I.; et al. Exposure to Farm Animals and Risk of Lung Cancer in the AGRICAN Cohort. Am. J. Epidemiol. 2017, 186, 463–472. [Google Scholar] [CrossRef]
- Peters, S.; Kromhout, H.; Olsson, A.C.; Wichmann, H.E.; Bruske, I.; Consonni, D.; Landi, M.T.; Caporaso, N.; Siemiatycki, J.; Richiardi, L.; et al. Occupational exposure to organic dust increases lung cancer risk in the general population. Thorax 2012, 67, 111–116. [Google Scholar] [CrossRef]
- Boulanger, M.; Tual, S.; Lemarchand, C.; Guizard, A.V.; Delafosse, P.; Marcotullio, E.; Pons, R.; Piel, C.; Pouchieu, C.; Baldi, I.; et al. Lung cancer risk and occupational exposures in crop farming: Results from the AGRIculture and CANcer (AGRICAN) cohort. Occup. Environ. Med. 2018, 75, 776–785. [Google Scholar] [CrossRef]
- Suraya, A.; Nowak, D.; Sulistomo, A.W.; Icksan, A.G.; Berger, U.; Syahruddin, E.; Bose-O’Reilly, S. Excess Risk of Lung Cancer Among Agriculture and Construction Workers in Indonesia. Ann. Glob. Health 2021, 87, 8. [Google Scholar] [CrossRef]
- Kim, B.; Park, E.Y.; Kim, J.; Park, E.; Oh, J.K.; Lim, M.K. Occupational Exposure to Pesticides and Lung Cancer Risk: A Propensity Score Analyses. Cancer Res. Treat. 2022, 54, 130–139. [Google Scholar] [CrossRef]
- Atramont, A.; Guida, F.; Mattei, F.; Matrat, M.; Cenee, S.; Sanchez, M.; Carton, M.; Menvielle, G.; Marrer, E.; Neri, M.; et al. Professional Cleaning Activities and Lung Cancer Risk Among Women: Results From the ICARE Study. J. Occup. Environ. Med. 2016, 58, 610–616. [Google Scholar] [CrossRef]
- Van den Borre, L.; Deboosere, P. Health risks in the cleaning industry: A Belgian census-linked mortality study (1991–2011). Int. Arch. Occup. Environ. Health 2018, 91, 13–21. [Google Scholar] [CrossRef]
- Bonner, M.R.; Freeman, L.E.; Hoppin, J.A.; Koutros, S.; Sandler, D.P.; Lynch, C.F.; Hines, C.J.; Thomas, K.; Blair, A.; Alavanja, M.C. Occupational Exposure to Pesticides and the Incidence of Lung Cancer in the Agricultural Health Study. Environ. Health Perspect. 2017, 125, 544–551. [Google Scholar] [CrossRef]
- Robinson, C.F.; Sullivan, P.A.; Li, J.; Walker, J.T. Occupational lung cancer in US women, 1984-1998. Am. J. Ind. Med. 2011, 54, 102–117. [Google Scholar] [CrossRef]
- Tse, L.A.; Yu, I.T.; Qiu, H.; Au, J.S.; Wang, X.R. Occupational risks and lung cancer burden for Chinese men: A population-based case-referent study. Cancer Causes Control. 2012, 23, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Corbin, M.; McLean, D.; Mannetje, A.; Dryson, E.; Walls, C.; McKenzie, F.; Maule, M.; Cheng, S.; Cunningham, C.; Kromhout, H.; et al. Lung cancer and occupation: A New Zealand cancer registry-based case-control study. Am. J. Ind. Med. 2011, 54, 89–101. [Google Scholar] [CrossRef] [PubMed]
- Lie, J.A.; Kjaerheim, K.; Tynes, T. Ionizing radiation exposure and cancer risk among Norwegian nurses. Eur. J. Cancer Prev. 2008, 17, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Schernhammer, E.S.; Feskanich, D.; Liang, G.; Han, J. Rotating night-shift work and lung cancer risk among female nurses in the United States. Am. J. Epidemiol. 2013, 178, 1434–1441. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.; Koh, D.H.; Choi, S.; Park, J.H.; Kim, H.C.; Lee, S.G.; Park, D. Estimates of the Prevalence, Intensity and the Number of Workers Exposed to Cigarette Smoking across Occupations and Industries in Korea. J. Korean Med. Sci. 2019, 34, e213. [Google Scholar] [CrossRef]
- Roswall, N.; Weiderpass, E. Alcohol as a risk factor for cancer: Existing evidence in a global perspective. J. Prev. Med. Public Health 2015, 48, 1–9. [Google Scholar] [CrossRef]
| Male | Female | |||
|---|---|---|---|---|
| N | % | N | % | |
| Total workers | 7,167,927 | 100 | 3,618,073 | 100 |
| Age | ||||
| 25–29 | 900,930 | 12.6 | 871,625 | 24.1 |
| 30–34 | 1,201,461 | 16.8 | 652,619 | 18.0 |
| 35–39 | 1,326,709 | 18.5 | 563,564 | 15.6 |
| 40–44 | 1,156,361 | 16.1 | 513,724 | 14.2 |
| 45–49 | 1,022,191 | 14.3 | 444,480 | 12.3 |
| 50–54 | 810,748 | 11.3 | 315,289 | 8.7 |
| 55–59 | 474,025 | 6.6 | 169,750 | 4.7 |
| 60–64 | 275,502 | 3.8 | 87,022 | 2.4 |
| Year | ||||
| 2009 | 7,167,927 | 100 | 3,618,073 | 100 |
| 2010 | 7,116,267 | 99.3 | 3,601,730 | 99.5 |
| 2011 | 7,076,872 | 98.7 | 3,590,469 | 99.2 |
| 2012 | 7,024,114 | 98.0 | 3,580,963 | 99.0 |
| 2013 | 6,970,061 | 97.2 | 3,571,713 | 98.7 |
| 2014 | 6,943,079 | 96.9 | 3,568,022 | 98.6 |
| 2015 | 6,925,839 | 96.6 | 3,565,209 | 98.5 |
| Larynx Cancer (C32) | Lung Cancer (C33, C34) | ||||||
|---|---|---|---|---|---|---|---|
| Person-Year | Cases | Incidence Rate (per 100,000) | Person-Year | Cases | Incidence Rate (per 100,000) | ||
| Total | 74,366,928 | 1150 | 1.54 | 71,872,786 | 15,013 | 20.08 | |
| Sex | Male | 49,253,195 | 1123 | 2.27 | 49,231,565 | 12,270 | 24.74 |
| Female | 25,113,734 | 27 | 0.11 | 25,107,016 | 2743 | 10.09 | |
| Age | 25–29 | 12,143,876 | 7 | 0.06 | 12,143,561 | 149 | 1.20 |
| 30–34 | 12,766,801 | 9 | 0.07 | 12,766,145 | 315 | 2.43 | |
| 35–39 | 13,035,008 | 37 | 0.28 | 13,033,646 | 656 | 4.98 | |
| 40–44 | 11,568,741 | 60 | 0.52 | 11,566,159 | 1232 | 10.55 | |
| 45–49 | 10,170,955 | 147 | 1.47 | 10,166,540 | 2172 | 21.13 | |
| 50–54 | 7,783,530 | 274 | 3.52 | 7,777,179 | 3297 | 41.94 | |
| 55–59 | 4,426,098 | 324 | 7.28 | 4,419,556 | 3694 | 82.66 | |
| 60–64 | 2,471,919 | 292 | 11.77 | 2,465,795 | 3626 | 145.98 | |
| KSIC Code | Industrial Classification (Group) | Cases | Person-Year | SIR (95% CI) |
|---|---|---|---|---|
| Male Workers | ||||
| 492 | Passenger land transport, except transport via railways | 21 | 308,510 | 1.65 (1.02–2.53) |
| KSIC Code | Industrial Classification (Group) | Cases | Person-Year | SIR (95% CI) |
|---|---|---|---|---|
| Male Workers | ||||
| 012 | Animal production | 19 | 36,266 | 1.72 (1.03–2.68) |
| 031 | Fishing | 21 | 33,588 | 1.70 (1.05–2.60) |
| 051 | Mining of coal and lignite | 43 | 68,719 | 1.69 (1.22–2.27) |
| 752 | Activities of travel agencies and tour operators and tourist assistance activities | 39 | 75,153 | 1.41 (1.00–1.93) |
| 742 | Cleaning and pest control services of building and industrial facilities | 139 | 169,980 | 1.23 (1.04–1.46) |
| 529 | Support activities for transportation | 1061 | 2,183,034 | 1.22 (1.15–1.30) |
| 412 | Heavy and civil engineering construction | 308 | 966,047 | 1.17 (1.05–1.31) |
| 682 | Real estate activities on a fee or contract basis | 407 | 563,482 | 1.11 (1.01–1.23) |
| Female workers | ||||
| 869 | Other human health activities | 11 | 41,399 | 2.08 (1.04–3.72) |
| 465 | Wholesale of machinery, equipment, and supplies | 22 | 118,943 | 1.88 (1.18–2.85) |
| 861 | Hospital activities | 70 | 637,586 | 1.29 (1.01–1.63) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baek, S.-U.; Lee, W.-R.; Yoo, K.-B.; Choi, J.-H.; Lee, K.-E.; Lee, W.; Yoon, J.-H. Respiratory Tract Cancer Incidences across Industry Groups: A Nationwide Cohort Study with More Than 70 Million Person-Years of Follow-Up. Cancers 2022, 14, 5219. https://doi.org/10.3390/cancers14215219
Baek S-U, Lee W-R, Yoo K-B, Choi J-H, Lee K-E, Lee W, Yoon J-H. Respiratory Tract Cancer Incidences across Industry Groups: A Nationwide Cohort Study with More Than 70 Million Person-Years of Follow-Up. Cancers. 2022; 14(21):5219. https://doi.org/10.3390/cancers14215219
Chicago/Turabian StyleBaek, Seong-Uk, Woo-Ri Lee, Ki-Bong Yoo, Jun-Hyeok Choi, Kyung-Eun Lee, Wanhyung Lee, and Jin-Ha Yoon. 2022. "Respiratory Tract Cancer Incidences across Industry Groups: A Nationwide Cohort Study with More Than 70 Million Person-Years of Follow-Up" Cancers 14, no. 21: 5219. https://doi.org/10.3390/cancers14215219
APA StyleBaek, S.-U., Lee, W.-R., Yoo, K.-B., Choi, J.-H., Lee, K.-E., Lee, W., & Yoon, J.-H. (2022). Respiratory Tract Cancer Incidences across Industry Groups: A Nationwide Cohort Study with More Than 70 Million Person-Years of Follow-Up. Cancers, 14(21), 5219. https://doi.org/10.3390/cancers14215219








