LGL Clonal Expansion and Unexplained Cytopenia: Two Clues Don’t Make an Evidence
Abstract
Simple Summary
Abstract
1. Introduction
2. Detection and Characterization of LGL Clones
3. Large Granular Lymphocytes Leukemia: From Phenotypic to Genetic Heterogeneity
4. T-LGLL and NK-LGLL Diagnosis: Stringent Criteria and Recommended Analyses
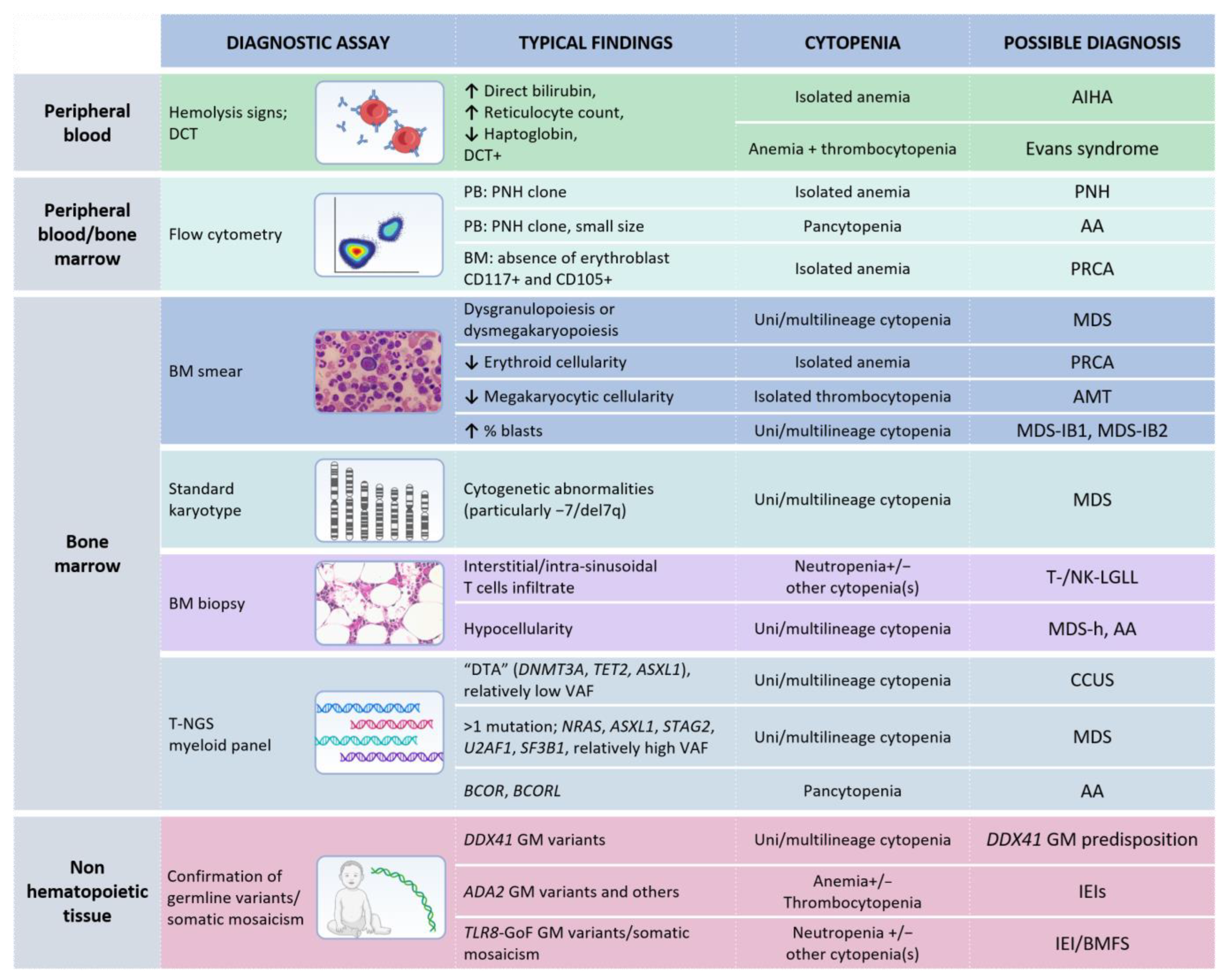
5. LGLL-Related Cytopenias
6. The Boundaries between LGLL and Autoimmunity in the Pathogenesis of Cytopenia
7. The Origin of Cytopenia(s): Is the LGL Clonal Expansion the Culprit?
8. LGL Clones as a Clue in the Differential Diagnosis of Cytopenic Patients
8.1. Bone Marrow Smear and Biopsy
8.2. Bone Marrow/Peripheral Blood Flow Cytometry
8.3. Bone Marrow Conventional Karyotyping and Myeloid Gene Mutation Analysis
8.4. The Landscape of Germline Immune-Hematological Disorders
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lamy, T.; Moignet, A.; Loughran, T.P. LGL Leukemia: From Pathogenesis to Treatment. Blood 2017, 129, 1082–1094. [Google Scholar] [CrossRef] [PubMed]
- Zawit, M.; Bahaj, W.; Gurnari, C.; Maciejewski, J. Large Granular Lymphocytic Leukemia: From Immunopathogenesis to Treatment of Refractory Disease. Cancers 2021, 13, 4418. [Google Scholar] [CrossRef]
- Gurnari, C.; Yeaney, G.A.; Kalinowski, M.; Cotta, C.V.; Maciejewski, J.P. T-Cell Large Granular Lymphocytic Leukemia Associated with Inclusion Body Myositis. Int. J. Lab. Hematol. 2022, 44, 27–28. [Google Scholar] [CrossRef] [PubMed]
- Gurnari, C.; Durrani, J.; Pagliuca, S.; Kishtagari, A.; Awada, H.; Kerr, C.M.; Adema, V.; Kongkiatkamon, S.; Lichtin, A.E.; Patel, B.J.; et al. Novel Invariant Features of Good Syndrome. Leukemia 2021, 35, 1792–1796. [Google Scholar] [CrossRef] [PubMed]
- Durrani, J.; Awada, H.; Kishtagari, A.; Visconte, V.; Kerr, C.; Adema, V.; Nagata, Y.; Kuzmanovic, T.; Hong, S.; Patel, B.; et al. Large Granular Lymphocytic Leukemia Coexists with Myeloid Clones and Myelodysplastic Syndrome. Leukemia 2020, 34, 957–962. [Google Scholar] [CrossRef]
- Moignet, A.; Lamy, T. Latest Advances in the Diagnosis and Treatment of Large Granular Lymphocytic Leukemia. Am. Soc. Clin. Oncol. Educ. Book 2018, 38, 616–625. [Google Scholar] [CrossRef]
- Zhang, D.; Loughran, T.P., Jr. Large Granular Lymphocytic Leukemia: Molecular Pathogenesis, Clinical Manifestations, and Treatment. Hematol. Am. Soc. Hematol. Educ. Program 2012, 2012, 652–659. [Google Scholar] [CrossRef]
- Huuhtanen, J.; Bhattacharya, D.; Lönnberg, T.; Kankainen, M.; Kerr, C.; Theodoropoulos, J.; Rajala, H.; Gurnari, C.; Kasanen, T.; Braun, T.; et al. Single-Cell Characterization of Leukemic and Non-Leukemic Immune Repertoires in CD8 T-Cell Large Granular Lymphocytic Leukemia. Nat. Commun. 2022, 13, 1981. [Google Scholar] [CrossRef]
- Cheon, H.; Dziewulska, K.H.; Moosic, K.B.; Olson, K.C.; Gru, A.A.; Feith, D.J.; Loughran, T.P., Jr. Advances in the Diagnosis and Treatment of Large Granular Lymphocytic Leukemia. Curr. Hematol. Malig. Rep. 2020, 15, 103–112. [Google Scholar] [CrossRef]
- Steinway, S.N.; LeBlanc, F.; Loughran, T.P., Jr. The Pathogenesis and Treatment of Large Granular Lymphocyte Leukemia. Blood Rev. 2014, 28, 87–94. [Google Scholar] [CrossRef]
- Ishida, F.; Ko, Y.H.; Kim, W.S.; Suzumiya, J.; Isobe, Y.; Oshimi, K.; Nakamura, S.; Suzuki, R. Aggressive Natural Killer Cell Leukemia: Therapeutic Potential of L-Asparaginase and Allogeneic Hematopoietic Stem Cell Transplantation. Cancer Sci. 2012, 103, 1079–1083. [Google Scholar] [CrossRef] [PubMed]
- Zambello, R.; Semenzato, G. Natural Killer Receptors in Patients with Lymphoproliferative Diseases of Granular Lymphocytes. Semin. Hematol. 2003, 40, 201–212. [Google Scholar] [CrossRef]
- Barilà, G.; Calabretto, G.; Teramo, A.; Vicenzetto, C.; Gasparini, V.R.; Semenzato, G.; Zambello, R. T Cell Large Granular Lymphocyte Leukemia and Chronic NK Lymphocytosis. Best Pract. Res. Clin. Haematol. 2019, 32, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Clemente, M.J.; Wlodarski, M.W.; Makishima, H.; Viny, A.D.; Bretschneider, I.; Shaik, M.; Bejanyan, N.; Lichtin, A.E.; Hsi, E.D.; Paquette, R.L.; et al. Clonal Drift Demonstrates Unexpected Dynamics of the T-Cell Repertoire in T-Large Granular Lymphocyte Leukemia. Blood 2011, 118, 4384–4393. [Google Scholar] [CrossRef]
- Clemente, M.J.; Przychodzen, B.; Jerez, A.; Dienes, B.E.; Afable, M.G.; Husseinzadeh, H.; Rajala, H.L.M.; Wlodarski, M.W.; Mustjoki, S.; Maciejewski, J.P. Deep Sequencing of the T-Cell Receptor Repertoire in CD8+ T-Large Granular Lymphocyte Leukemia Identifies Signature Landscapes. Blood 2013, 122, 4077–4085. [Google Scholar] [CrossRef]
- Lima, M.; Almeida, J.; Santos, A.H.; dos Anjos Teixeira, M.; Alguero, M.C.; Queirós, M.L.; Balanzategui, A.; Justiça, B.; Gonzalez, M.; San Miguel, J.F.; et al. Immunophenotypic Analysis of the TCR-Vbeta Repertoire in 98 Persistent Expansions of CD3(+)/TCR-Alphabeta(+) Large Granular Lymphocytes: Utility in Assessing Clonality and Insights into the Pathogenesis of the Disease. Am. J. Pathol. 2001, 159, 1861–1868. [Google Scholar] [CrossRef]
- Muñoz-García, N.; Morán-Plata, F.J.; Villamor, N.; Lima, M.; Barrena, S.; Mateos, S.; Caldas, C.; van Dongen, J.J.M.; Orfao, A.; Almeida, J. High-Sensitive TRBC1-Based Flow Cytometric Assessment of T-Cell Clonality in Tαβ-Large Granular Lymphocytic Leukemia. Cancers 2022, 14, 408. [Google Scholar] [CrossRef]
- Zambello, R.; Falco, M.; Della Chiesa, M.; Trentin, L.; Carollo, D.; Castriconi, R.; Cannas, G.; Carlomagno, S.; Cabrelle, A.; Lamy, T.; et al. Expression and Function of KIR and Natural Cytotoxicity Receptors in NK-Type Lymphoproliferative Diseases of Granular Lymphocytes. Blood 2003, 102, 1797–1805. [Google Scholar] [CrossRef]
- Bárcena, P.; Jara-Acevedo, M.; Tabernero, M.D.; López, A.; Sánchez, M.L.; García-Montero, A.C.; Muñoz-García, N.; Vidriales, M.B.; Paiva, A.; Lecrevisse, Q.; et al. Phenotypic Profile of Expanded NK Cells in Chronic Lymphoproliferative Disorders: A Surrogate Marker for NK-Cell Clonality. Oncotarget 2015, 6, 42938–42951. [Google Scholar] [CrossRef]
- Alaggio, R.; Amador, C.; Anagnostopoulos, I.; Attygalle, A.D.; de Araujo, I.B.O.; Berti, E.; Bhagat, G.; Borges, A.M.; Boyer, D.; Calaminici, M.; et al. The 5th Edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia 2022, 36, 1720–1748. [Google Scholar] [CrossRef]
- Matutes, E. The 2017 WHO Update on Mature T- and Natural Killer (NK) Cell Neoplasms. Int. J. Lab. Hematol. 2018, 40 (Suppl. 1), 97–103. [Google Scholar] [CrossRef] [PubMed]
- Ishida, F. Aggressive NK-Cell Leukemia. Front. Pediatr. 2018, 6, 292. [Google Scholar] [CrossRef] [PubMed]
- Lima, M.; Almeida, J.; Dos Anjos Teixeira, M.; del Carmen Alguero, M.; Santos, A.H.; Balanzategui, A.; Queirós, M.L.; Bárcena, P.; Izarra, A.; Fonseca, S.; et al. TCRalphabeta+/CD4+ Large Granular Lymphocytosis: A New Clonal T-Cell Lymphoproliferative Disorder. Am. J. Pathol. 2003, 163, 763–771. [Google Scholar] [CrossRef]
- Barilà, G.; Teramo, A.; Calabretto, G.; Vicenzetto, C.; Gasparini, V.R.; Pavan, L.; Leoncin, M.; Vedovato, S.; Frigo, A.C.; Facco, M.; et al. Stat3 Mutations Impact on Overall Survival in Large Granular Lymphocyte Leukemia: A Single-Center Experience of 205 Patients. Leukemia 2020, 34, 1116–1124. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.V.; Zhang, R.; Loughran, T.P., Jr. Never Say Die: Survival Signaling in Large Granular Lymphocyte Leukemia. Clin. Lymphoma Myeloma 2009, 9 (Suppl. 3), S244–S253. [Google Scholar] [CrossRef] [PubMed]
- Koskela, H.L.M.; Eldfors, S.; Ellonen, P.; van Adrichem, A.J.; Kuusanmäki, H.; Andersson, E.I.; Lagström, S.; Clemente, M.J.; Olson, T.; Jalkanen, S.E.; et al. Somatic STAT3 Mutations in Large Granular Lymphocytic Leukemia. N. Engl. J. Med. 2012, 366, 1905–1913. [Google Scholar] [CrossRef]
- Mariotti, B.; Calabretto, G.; Rossato, M.; Teramo, A.; Castellucci, M.; Barilà, G.; Leoncin, M.; Vicenzetto, C.; Facco, M.; Semenzato, G.; et al. Identification of a miR-Fas Ligand Axis in the Development of Neutropenia in T Large Granular Lymphocyte Leukemia. Haematologica 2020, 105, 1351–1360. [Google Scholar] [CrossRef]
- Teramo, A.; Barilà, G.; Calabretto, G.; Vicenzetto, C.; Gasparini, V.R.; Semenzato, G.; Zambello, R. Insights Into Genetic Landscape of Large Granular Lymphocyte Leukemia. Front. Oncol. 2020, 10, 152. [Google Scholar] [CrossRef]
- Teramo, A.; Barilà, G.; Calabretto, G.; Ercolin, C.; Lamy, T.; Moignet, A.; Roussel, M.; Pastoret, C.; Leoncin, M.; Gattazzo, C.; et al. STAT3 Mutation Impacts Biological and Clinical Features of T-LGL Leukemia. Oncotarget 2017, 8, 61876–61889. [Google Scholar] [CrossRef]
- Teramo, A.; Binatti, A.; Ciabatti, E.; Schiavoni, G.; Tarrini, G.; Barilà, G.; Calabretto, G.; Vicenzetto, C.; Gasparini, V.R.; Facco, M.; et al. Defining TCRγδ Lymphoproliferative Disorders by Combined Immunophenotypic and Molecular Evaluation. Nat. Commun. 2022, 13, 3298. [Google Scholar] [CrossRef]
- Barilà, G.; Grassi, A.; Cheon, H.; Teramo, A.; Calabretto, G.; Chahal, J.; Vicenzetto, C.; Almeida, J.; Shemo, B.; Min, S.; et al. Tγδ LGL leukemia identifies a subset with more symptomatic disease: Analysis of an international cohort of 137 patients. Blood 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Rajala, H.L.M.; Eldfors, S.; Kuusanmäki, H.; van Adrichem, A.J.; Olson, T.; Lagström, S.; Andersson, E.I.; Jerez, A.; Clemente, M.J.; Yan, Y.; et al. Discovery of Somatic STAT5b Mutations in Large Granular Lymphocytic Leukemia. Blood 2013, 121, 4541–4550. [Google Scholar] [CrossRef] [PubMed]
- Barilà, G.; Teramo, A.; Calabretto, G.; Ercolin, C.; Boscaro, E.; Trimarco, V.; Carraro, S.; Leoncin, M.; Vicenzetto, C.; Cabrelle, A.; et al. Dominant Cytotoxic NK Cell Subset within CLPD-NK Patients Identifies a More Aggressive NK Cell Proliferation. Blood Cancer J. 2018, 8, 51. [Google Scholar] [CrossRef] [PubMed]
- Gasparini, V.R.; Binatti, A.; Coppe, A.; Teramo, A.; Vicenzetto, C.; Calabretto, G.; Barilà, G.; Barizza, A.; Giussani, E.; Facco, M.; et al. A High Definition Picture of Somatic Mutations in Chronic Lymphoproliferative Disorder of Natural Killer Cells. Blood Cancer J. 2020, 10, 42. [Google Scholar] [CrossRef]
- Shi, M.; Olteanu, H.; Jevremovic, D.; He, R.; Viswanatha, D.; Corley, H.; Horna, P. T-Cell Clones of Uncertain Significance Are Highly Prevalent and Show Close Resemblance to T-Cell Large Granular Lymphocytic Leukemia. Implications for Laboratory Diagnostics. Mod. Pathol. 2020, 33, 2046–2057. [Google Scholar] [CrossRef]
- Dhodapkar, M.V.; Li, C.Y.; Lust, J.A.; Tefferi, A.; Phyliky, R.L. Clinical Spectrum of Clonal Proliferations of T-Large Granular Lymphocytes: A T-Cell Clonopathy of Undetermined Significance? Blood 1994, 84, 1620–1627. [Google Scholar] [CrossRef]
- Evans, H.L.; Burks, E.; Viswanatha, D.; Larson, R.S. Utility of Immunohistochemistry in Bone Marrow Evaluation of T-Lineage Large Granular Lymphocyte Leukemia. Hum. Pathol. 2000, 31, 1266–1273. [Google Scholar] [CrossRef]
- Morice, W.G.; Kurtin, P.J.; Tefferi, A.; Hanson, C.A. Distinct Bone Marrow Findings in T-Cell Granular Lymphocytic Leukemia Revealed by Paraffin Section Immunoperoxidase Stains for CD8, TIA-1, and Granzyme B. Blood 2002, 99, 268–274. [Google Scholar] [CrossRef]
- Osuji, N.; Beiske, K.; Randen, U.; Matutes, E.; Tjonnfjord, G.; Catovsky, D.; Wotherspoon, A. Characteristic Appearances of the Bone Marrow in T-Cell Large Granular Lymphocyte Leukaemia. Histopathology 2007, 50, 547–554. [Google Scholar] [CrossRef]
- Mailloux, A.W.; Zhang, L.; Moscinski, L.; Bennett, J.M.; Yang, L.; Yoder, S.J.; Bloom, G.; Wei, C.; Wei, S.; Sokol, L.; et al. Fibrosis and Subsequent Cytopenias Are Associated with Basic Fibroblast Growth Factor-Deficient Pluripotent Mesenchymal Stromal Cells in Large Granular Lymphocyte Leukemia. J. Immunol. 2013, 191, 3578–3593. [Google Scholar] [CrossRef]
- Pastoret, C.; Desmots, F.; Drillet, G.; Le Gallou, S.; Boulland, M.-L.; Thannberger, A.; Doncker, A.-V.; Salaun, V.; Damaj, G.L.; Veyrat-Masson, R.; et al. Linking the KIR Phenotype with STAT3 and TET2 Mutations to Identify Chronic Lymphoproliferative Disorders of NK Cells. Blood 2021, 137, 3237–3250. [Google Scholar] [CrossRef] [PubMed]
- Baer, C.; Kimura, S.; Rana, M.S.; Kleist, A.B.; Flerlage, T.; Feith, D.J.; Chockley, P.; Walter, W.; Meggendorfer, M.; Olson, T.L.; et al. CCL22 Mutations Drive Natural Killer Cell Lymphoproliferative Disease by Deregulating Microenvironmental Crosstalk. Nat. Genet. 2022, 54, 637–648. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, D.; Teramo, A.; Gasparini, V.R.; Huuhtanen, J.; Kim, D.; Theodoropoulos, J.; Schiavoni, G.; Barilà, G.; Vicenzetto, C.; Calabretto, G.; et al. Identification of Novel STAT5B Mutations and Characterization of TCRβ Signatures in CD4+ T-Cell Large Granular Lymphocyte Leukemia. Blood Cancer J. 2022, 12, 31. [Google Scholar] [CrossRef] [PubMed]
- Semenzato, G.; Zambello, R. Interrogating Molecular Genetics to Refine LGLL Classification. Blood 2022, 139, 3002–3004. [Google Scholar] [CrossRef] [PubMed]
- Semenzato, G.; Pandolfi, F.; Chisesi, T.; De Rossi, G.; Pizzolo, G.; Zambello, R.; Trentin, L.; Agostini, C.; Dini, E.; Vespignani, M.; et al. The Lymphoproliferative Disease of Granular Lymphocytes. A Heterogeneous Disorder Ranging from Indolent to Aggressive Conditions. Cancer 1987, 60, 2971–2978. [Google Scholar] [CrossRef]
- Mohan, S.R.; Maciejewski, J.P. Diagnosis and Therapy of Neutropenia in Large Granular Lymphocyte Leukemia. Curr. Opin. Hematol. 2009, 16, 27–34. [Google Scholar] [CrossRef]
- Pontikoglou, C.; Kalpadakis, C.; Papadaki, H.A. Pathophysiologic Mechanisms and Management of Neutropenia Associated with Large Granular Lymphocytic Leukemia. Expert Rev. Hematol. 2011, 4, 317–328. [Google Scholar] [CrossRef]
- Calabretto, G.; Teramo, A.; Barilà, G.; Vicenzetto, C.; Gasparini, V.R.; Semenzato, G.; Zambello, R. Neutropenia and Large Granular Lymphocyte Leukemia: From Pathogenesis to Therapeutic Options. Cells 2021, 10, 2800. [Google Scholar] [CrossRef]
- Bareau, B.; Rey, J.; Hamidou, M.; Donadieu, J.; Morcet, J.; Reman, O.; Schleinitz, N.; Tournilhac, O.; Roussel, M.; Fest, T.; et al. Analysis of a French Cohort of Patients with Large Granular Lymphocyte Leukemia: A Report on 229 Cases. Haematologica 2010, 95, 1534–1541. [Google Scholar] [CrossRef]
- Sanikommu, S.R.; Clemente, M.J.; Chomczynski, P.; Afable, M.G., 2nd; Jerez, A.; Thota, S.; Patel, B.; Hirsch, C.; Nazha, A.; Desamito, J.; et al. Clinical Features and Treatment Outcomes in Large Granular Lymphocytic Leukemia (LGLL). Leuk. Lymphoma 2018, 59, 416–422. [Google Scholar] [CrossRef]
- Dong, N.; Castillo Tokumori, F.; Isenalumhe, L.; Zhang, Y.; Tandon, A.; Knepper, T.C.; Mo, Q.; Shao, H.; Zhang, L.; Sokol, L. Large Granular Lymphocytic Leukemia—A Retrospective Study of 319 Cases. Am. J. Hematol. 2021, 96, 772–780. [Google Scholar] [CrossRef] [PubMed]
- Rivero, A.; Mozas, P.; Jiménez, L.; López-Guerra, M.; Colomer, D.; Bataller, A.; Correa, J.; Rivas-Delgado, A.; Bastidas, G.; Baumann, T.; et al. Clinicobiological Characteristics and Outcomes of Patients with T-Cell Large Granular Lymphocytic Leukemia and Chronic Lymphoproliferative Disorder of Natural Killer Cells from a Single Institution. Cancers 2021, 13, 3900. [Google Scholar] [CrossRef] [PubMed]
- Salama, Y.; Zhao, F.; Oliveira, J.L.; Yuan, J.; Jevremovic, D.; Go, R.S.; Ding, W.; Parikh, S.A.; Shah, M.V.; Hampel, P.J.; et al. Isolated Anemia in Patients with Large Granular Lymphocytic Leukemia (LGLL). Blood Cancer J. 2022, 12, 30. [Google Scholar] [CrossRef] [PubMed]
- Semenzato, G.; Teramo, A.; Calabretto, G.; Gasparini, V.R.; Zambello, R. All that glitters is not LGL Leukemia. Leukemia, 2022; Online ahead of print. [Google Scholar] [CrossRef]
- Sun, H.; Wei, S.; Yang, L. Dysfunction of Immune System in the Development of Large Granular Lymphocyte Leukemia. Hematology 2019, 24, 139–147. [Google Scholar] [CrossRef]
- Gazitt, T.; Loughran, T.P., Jr. Chronic Neutropenia in LGL Leukemia and Rheumatoid Arthritis. Hematol. Am. Soc. Hematol. Educ. Program 2017, 2017, 181–186. [Google Scholar] [CrossRef]
- Liu, X.; Loughran, T.P. The Spectrum of Large Granular Lymphocyte Leukemia and Felty’s Syndrome. Curr. Opin. Hematol. 2011, 18, 254–259. [Google Scholar] [CrossRef]
- Moosic, K.B.; Ananth, K.; Andrade, F.; Feith, D.J.; Darrah, E.; Loughran, T.P., Jr. Intersection Between Large Granular Lymphocyte Leukemia and Rheumatoid Arthritis. Front. Oncol. 2022, 12, 869205. [Google Scholar] [CrossRef]
- Burks, E.J.; Loughran, T.P., Jr. Pathogenesis of Neutropenia in Large Granular Lymphocyte Leukemia and Felty Syndrome. Blood Rev. 2006, 20, 245–266. [Google Scholar] [CrossRef]
- Pflug, N.; Littauer, A.; Beverungen, D.; Sretenovic, A.; Wahnschaffe, L.; Braun, T.; Dechow, A.; Jungherz, D.; Otte, M.; Monecke, A.; et al. Case Report: Large Granular Lymphocyte Leukemia (LGLL)-A Case Series of Challenging Presentations. Front. Oncol. 2021, 11, 775313. [Google Scholar] [CrossRef]
- Alfano, G.; Ferrari, A.; Fontana, F.; Damiano, F.; Solazzo, A.; Mori, G.; Cappelli, G. Hemolytic Anemia as Presentation of T-Cell Large Granular Lymphocytic Leukemia After Kidney Transplantation: A Case Report. Transplant. Proc. 2020, 52, 1617–1618. [Google Scholar] [CrossRef] [PubMed]
- Gentile, T.C.; Loughran, T.P., Jr. Resolution of Autoimmune Hemolytic Anemia Following Splenectomy in CD3+ Large Granular Lymphocyte Leukemia. Leuk. Lymphoma 1996, 23, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Gurnari, C.; Maciejewski, J.P. How I Manage Acquired Pure Red Cell Aplasia in Adults. Blood 2021, 137, 2001–2009. [Google Scholar] [CrossRef] [PubMed]
- Bockorny, B.; Dasanu, C.A. Autoimmune Manifestations in Large Granular Lymphocyte Leukemia. Clin. Lymphoma Myeloma Leuk. 2012, 12, 400–405. [Google Scholar] [CrossRef]
- Osuji, N.; Matutes, E.; Catovsky, D.; Lampert, I.; Wotherspoon, A. Histopathology of the Spleen in T-Cell Large Granular Lymphocyte Leukemia and T-Cell Prolymphocytic Leukemia: A Comparative Review. Am. J. Surg. Pathol. 2005, 29, 935–941. [Google Scholar] [CrossRef]
- Ergas, D.; Tsimanis, A.; Shtalrid, M.; Duskin, C.; Berrebi, A. T-γ Large Granular Lymphocyte Leukemia Associated with Amegakaryocytic Thrombocytopenic Purpura, Sjögren’s Syndrome, and Polyglandular Autoimmune Syndrome Type II, with Subsequent Development of Pure Red Cell Aplasia. Am. J. Hematol. 2002, 69, 132–134. [Google Scholar] [CrossRef]
- Lai, D.W.; Loughran, T.P., Jr.; Maciejewski, J.P.; Sasu, S.; Song, S.X.; Epling-Burnette, P.K.; Paquette, R.L. Acquired Amegakaryocytic Thrombocytopenia and Pure Red Cell Aplasia Associated with an Occult Large Granular Lymphocyte Leukemia. Leuk. Res. 2008, 32, 823–827. [Google Scholar] [CrossRef]
- Fattizzo, B.; Bellani, V.; Pasquale, R.; Giannotta, J.A.; Barcellini, W. Large Granular Lymphocyte Expansion in Myeloid Diseases and Bone Marrow Failure Syndromes: Whoever Seeks Finds. Front. Oncol. 2021, 11, 748610. [Google Scholar] [CrossRef]
- Komrokji, R.S.; Ali, N.A.; Sallman, D.; Padron, E.; Lancet, J.; Sokol, L.; Varnadoe, C.; Burnette, P.K.; List, A. Characterization of Myelodysplastic Syndromes (MDS) with T-Cell Large Granular Lymphocyte Proliferations (LGL). Leukemia 2020, 34, 3097–3099. [Google Scholar] [CrossRef]
- Nyland, S.B.; Krissinger, D.J.; Clemente, M.J.; Irby, R.B.; Baab, K.T.; Jarbadan, N.R.; Sokol, L.; Schaefer, E.; Liao, J.; Cuthbertson, D.; et al. Seroreactivity to LGL Leukemia-Specific Epitopes in Aplastic Anemia, Myelodysplastic Syndrome and Paroxysmal Nocturnal Hemoglobinuria: Results of a Bone Marrow Failure Consortium Study. Leuk. Res. 2012, 36, 581–587. [Google Scholar] [CrossRef]
- Raess, P.W.; Cascio, M.J.; Fan, G.; Press, R.; Druker, B.J.; Brewer, D.; Spurgeon, S.E. Concurrent STAT3, DNMT3A, and TET2 Mutations in T-LGL Leukemia with Molecularly Distinct Clonal Hematopoiesis of Indeterminate Potential. Am. J. Hematol. 2017, 92, E6–E8. [Google Scholar] [CrossRef] [PubMed]
- Isabelle, C.; Boles, A.; Chakravarti, N.; Porcu, P.; Brammer, J.; Mishra, A. Cytokines in the Pathogenesis of Large Granular Lymphocytic Leukemia. Front. Oncol. 2022, 12, 849917. [Google Scholar] [CrossRef] [PubMed]
- Calabretto, G.; Attardi, E.; Teramo, A.; Trimarco, V.; Carraro, S.; Mossuto, S.; Barilà, G.; Vicenzetto, C.; Gasparini, V.R.; Crugnola, M.; et al. Hypocellular Myelodysplastic Syndromes (h-MDS): From Clinical Description to Immunological Characterization in the Italian Multi-Center Experience. Leukemia 2022, 36, 1947–1950. [Google Scholar] [CrossRef]
- Cazzola, M. Myelodysplastic Syndromes. Reply. N. Engl. J. Med. 2020, 383, 2590. [Google Scholar] [CrossRef]
- Arber, D.A.; Orazi, A.; Hasserjian, R.; Thiele, J.; Borowitz, M.J.; Le Beau, M.M.; Bloomfield, C.D.; Cazzola, M.; Vardiman, J.W. The 2016 Revision to the World Health Organization Classification of Myeloid Neoplasms and Acute Leukemia. Blood 2016, 127, 2391–2405. [Google Scholar] [CrossRef]
- Fattizzo, B.; Serpenti, F.; Barcellini, W.; Caprioli, C. Hypoplastic Myelodysplastic Syndromes: Just an Overlap Syndrome? Cancers 2021, 13, 132. [Google Scholar] [CrossRef]
- Zhang, H.-F.; Huang, Z.-D.; Wu, X.-R.; Li, Q.; Yu, Z.-F. Comparison of T Lymphocyte Subsets in Aplastic Anemia and Hypoplastic Myelodysplastic Syndromes. Life Sci. 2017, 189, 71–75. [Google Scholar] [CrossRef]
- Ogata, K.; Della Porta, M.G.; Malcovati, L.; Picone, C.; Yokose, N.; Matsuda, A.; Yamashita, T.; Tamura, H.; Tsukada, J.; Dan, K.; et al. Diagnostic Utility of Flow Cytometry in Myelodysplastic Syndromes: A Prospective Validation Study in Low-Risk Patients with Normal Karyotype. Blood 2008, 112, 3634. [Google Scholar] [CrossRef]
- Mathis, S.; Chapuis, N.; Debord, C.; Rouquette, A.; Radford-Weiss, I.; Park, S.; Dreyfus, F.; Lacombe, C.; Béné, M.C.; Kosmider, O.; et al. Flow Cytometric Detection of Dyserythropoiesis: A Sensitive and Powerful Diagnostic Tool for Myelodysplastic Syndromes. Leukemia 2013, 27, 1981–1987. [Google Scholar] [CrossRef]
- Jerez, J.; Ocqueteau, M. Immunophenotype of Erythroid Precursors in Patient with Pure Red Cell Aplasia (PRCA): Utility of Analysis of Erythroid Maturation. Ann. Hematol. Oncol. 2021, 8, 1346. [Google Scholar]
- Gurnari, C.; Graham, A.C.; Efanov, A.; Pagliuca, S.; Durrani, J.; Awada, H.; Patel, B.J.; Lichtin, A.E.; Visconte, V.; Sekeres, M.A.; et al. Frequency and Perturbations of Various Peripheral Blood Cell Populations before and after Eculizumab Treatment in Paroxysmal Nocturnal Hemoglobinuria. Blood Cells Mol. Dis. 2021, 87, 102528. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.K.; Pati, H.P.; Tejomurtula, A.P.; Seth, T. PNH Clone Assessment by Flow Cytometry and Its Clinical Correlation in PNH and Aplastic Anemia. J. Hematop. 2010, 3, 137–143. [Google Scholar] [CrossRef]
- Bono, E.; McLornan, D.; Travaglino, E.; Gandhi, S.; Gallì, A.; Khan, A.A.; Kulasekararaj, A.G.; Boveri, E.; Raj, K.; Elena, C.; et al. Clinical, Histopathological and Molecular Characterization of Hypoplastic Myelodysplastic Syndrome. Leukemia 2019, 33, 2495–2505. [Google Scholar] [CrossRef]
- Voso, M.T.; Gurnari, C. Have We Reached a Molecular Era in Myelodysplastic Syndromes? Hematol. Am. Soc. Hematol. Educ. Program 2021, 2021, 418–427. [Google Scholar] [CrossRef]
- DeZern, A.E.; Malcovati, L.; Ebert, B.L. CHIP, CCUS, and Other Acronyms: Definition, Implications, and Impact on Practice. Am. Soc. Clin. Oncol. Educ. Book 2019, 39, 400–410. [Google Scholar] [CrossRef]
- Jerez, A.; Clemente, M.J.; Makishima, H.; Rajala, H.; Gómez-Seguí, I.; Olson, T.; McGraw, K.; Przychodzen, B.; Kulasekararaj, A.; Afable, M.; et al. STAT3 Mutations Indicate the Presence of Subclinical T-Cell Clones in a Subset of Aplastic Anemia and Myelodysplastic Syndrome Patients. Blood 2013, 122, 2453–2459. [Google Scholar] [CrossRef]
- Ai, K.; Li, M.; Wu, P.; Deng, C.; Huang, X.; Ling, W.; Xu, R.; Geng, S.; Sun, Q.; Weng, J.; et al. Concurrence of Myelodysplastic Syndromes and Large Granular Lymphocyte Leukemia: Clinicopathological Features, Mutational Profile and Gene Ontology Analysis in a Single Center. Am. J. Cancer Res. 2021, 11, 1616–1631. [Google Scholar]
- Yoshizato, T.; Dumitriu, B.; Hosokawa, K.; Makishima, H.; Yoshida, K.; Townsley, D.; Sato-Otsubo, A.; Sato, Y.; Liu, D.; Suzuki, H.; et al. Somatic Mutations and Clonal Hematopoiesis in Aplastic Anemia. N. Engl. J. Med. 2015, 373, 35–47. [Google Scholar] [CrossRef]
- Gurnari, C.; Pagliuca, S.; Prata, P.H.; Galimard, J.-E.; Catto, L.F.B.; Larcher, L.; Sebert, M.; Allain, V.; Patel, B.J.; Durmaz, A.; et al. Clinical and Molecular Determinants of Clonal Evolution in Aplastic Anemia and Paroxysmal Nocturnal Hemoglobinuria. J. Clin. Oncol. 2022, 138, JCO2200710. [Google Scholar] [CrossRef]
- Goyal, T.; Tu, Z.J.; Wang, Z.; Cook, J.R. Clinical and Pathologic Spectrum of DDX41-Mutated Hematolymphoid Neoplasms. Am. J. Clin. Pathol. 2021, 156, 829–838. [Google Scholar] [CrossRef]
- Pilania, R.K.; Banday, A.Z.; Sharma, S.; Kumrah, R.; Joshi, V.; Loganathan, S.; Dhaliwal, M.; Jindal, A.K.; Vignesh, P.; Suri, D.; et al. Deficiency of Human Adenosine Deaminase Type 2—A Diagnostic Conundrum for the Hematologist. Front. Immunol. 2022, 13, 869570. [Google Scholar] [CrossRef] [PubMed]
- Dorjbal, B.; Stinson, J.R.; Ma, C.A.; Weinreich, M.A.; Miraghazadeh, B.; Hartberger, J.M.; Frey-Jakobs, S.; Weidinger, S.; Moebus, L.; Franke, A.; et al. Hypomorphic Caspase Activation and Recruitment Domain 11 (CARD11) Mutations Associated with Diverse Immunologic Phenotypes with or without Atopic Disease. J. Allergy Clin. Immunol. 2019, 143, 1482–1495. [Google Scholar] [CrossRef] [PubMed]
- Rajpurkar, M.; Buck, S.; Lafferty, J.; Wakeling, E.; Ravindranath, Y.; Savaşan, S. Acquired Pure Red Cell Aplasia and Acquired Amegakaryocytic Thrombocytopenia Associated With Clonal Expansion of T-Cell Large Granular Lymphocytes in a Patient With Lipopolysaccharide-Responsive Beige-like Anchor (LRBA) Protein Deficiency. J. Pediatr. Hematol./Oncol. 2019, 41, e542–e545. [Google Scholar] [CrossRef] [PubMed]
- Aluri, J.; Bach, A.; Kaviany, S.; Chiquetto Paracatu, L.; Kitcharoensakkul, M.; Walkiewicz, M.A.; Putnam, C.D.; Shinawi, M.; Saucier, N.; Rizzi, E.M.; et al. Immunodeficiency and Bone Marrow Failure with Mosaic and Germline TLR8 Gain of Function. Blood 2021, 137, 2450–2462. [Google Scholar] [CrossRef] [PubMed]
- Bleesing, J. Gain-of-Function Defects in Toll-like Receptor 8 Shed Light on the Interface between Immune System and Bone Marrow Failure Disorders. Front. Immunol. 2022, 13, 935321. [Google Scholar] [CrossRef]
- Wehr, C.; Houet, L.; Unger, S.; Kindle, G.; Goldacker, S.; Grimbacher, B.; de Oteyza, A.C.G.; Marks, R.; Pfeifer, D.; Nieters, A.; et al. Altered Spectrum of Lymphoid Neoplasms in a Single-Center Cohort of Common Variable Immunodeficiency with Immune Dysregulation. J. Clin. Immunol. 2021, 41, 1250–1265. [Google Scholar] [CrossRef]
- Kitchen, B.J.; Boxer, L.A. Large Granular Lymphocyte Leukemia (LGL) in a Child with Hyper IgM Syndrome and Autoimmune Hemolytic Anemia. Pediatr. Blood Cancer 2008, 50, 142–145. [Google Scholar] [CrossRef]
- Attardi, E.; Di Cesare, S.; Amodio, D.; Giancotta, C.; Cotugno, N.; Cifaldi, C.; Chiriaco, M.; Palma, P.; Finocchi, A.; Di Matteo, G.; et al. Phenotypical T Cell Differentiation Analysis: A Diagnostic and Predictive Tool in the Study of Primary Immunodeficiencies. Front. Immunol. 2019, 10, 2735. [Google Scholar] [CrossRef]
- Schiavo, E.; Martini, B.; Attardi, E.; Consonni, F.; Ciullini Mannurita, S.; Coniglio, M.L.; Tellini, M.; Chiocca, E.; Fotzi, I.; Luti, L.; et al. Autoimmune Cytopenias and Dysregulated Immunophenotype Act as Warning Signs of Inborn Errors of Immunity: Results From a Prospective Study. Front. Immunol. 2021, 12, 790455. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calabretto, G.; Attardi, E.; Gurnari, C.; Semenzato, G.; Voso, M.T.; Zambello, R. LGL Clonal Expansion and Unexplained Cytopenia: Two Clues Don’t Make an Evidence. Cancers 2022, 14, 5236. https://doi.org/10.3390/cancers14215236
Calabretto G, Attardi E, Gurnari C, Semenzato G, Voso MT, Zambello R. LGL Clonal Expansion and Unexplained Cytopenia: Two Clues Don’t Make an Evidence. Cancers. 2022; 14(21):5236. https://doi.org/10.3390/cancers14215236
Chicago/Turabian StyleCalabretto, Giulia, Enrico Attardi, Carmelo Gurnari, Gianpietro Semenzato, Maria Teresa Voso, and Renato Zambello. 2022. "LGL Clonal Expansion and Unexplained Cytopenia: Two Clues Don’t Make an Evidence" Cancers 14, no. 21: 5236. https://doi.org/10.3390/cancers14215236
APA StyleCalabretto, G., Attardi, E., Gurnari, C., Semenzato, G., Voso, M. T., & Zambello, R. (2022). LGL Clonal Expansion and Unexplained Cytopenia: Two Clues Don’t Make an Evidence. Cancers, 14(21), 5236. https://doi.org/10.3390/cancers14215236







