The Potential Role of 3D In Vitro Acute Myeloid Leukemia Culture Models in Understanding Drug Resistance in Leukemia Stem Cells
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Overview of In Vitro 3D AML Models
3.1. Synthetic Scaffold-Based 3D Models (Table 1)
| Model | Niche Tested | Type of Scaffold | Important Findings |
|---|---|---|---|
| 3D stromal-based mode [14] | Stromal niche | Poly glycolic/Poly L-Lactic acid | 3D model can better identify chemoresistance and N-cadherin compared to 2D models and cells in suspension |
| 3D Static in vitro models [16] | Stromal niche | PU collagen-coated scaffold | The effect of glucose and oxygen levels on AML cell proliferation and adaptability was more pronounced in 3D models in contrast to 2D models |
| 3D triculture static models [15] | Vascular niche | PEG-heparin hydrogel | Chemoresistance was superior in 3D models when compared to 2D models or cells in suspension |
3.2. Biologic Scaffold-Based 3D Models (Table 2)
| Model | Niche Tested | Type of Scaffold | Important Findings |
|---|---|---|---|
| 3D biological scaffold-based static model [17] | ECM niche | Decellularized Wharton jelly matrix (DWJM) | 3D models demonstrated superior chemoresistance, ALDH + expression, N-cadherin expression |
| 3D- humanized scaffold-based static model [18] | Stromal niche | Hydroxyapatite and collagen | AML blasts alter MSC morphology and on the transcriptome level, 3D models exhibit a platform for testing dual chemotherapy |
3.3. Dynamic 3D In Vitro Models (Table 3)
| Model | Niche Tested | Type of Scaffold | Important Findings |
|---|---|---|---|
| Dynamic 3D (bioreactor) humanized model [20] | Vascular niche Stromal niche | Collagen and hydroxyapatite separately | Quiescence and superior chemoresistance in 3D models; highly customizable models which can recapitulate the stromal and vascular niche |
| Dynamic 3D (magnetic field-based) model [21] | Stromal niche | Magnetic hydrogel | The effect of chemotherapeutic agents on chemoresistance, metabolic profile, proliferation, and differentiation of both HPSC and AML cells |
4. Discussion
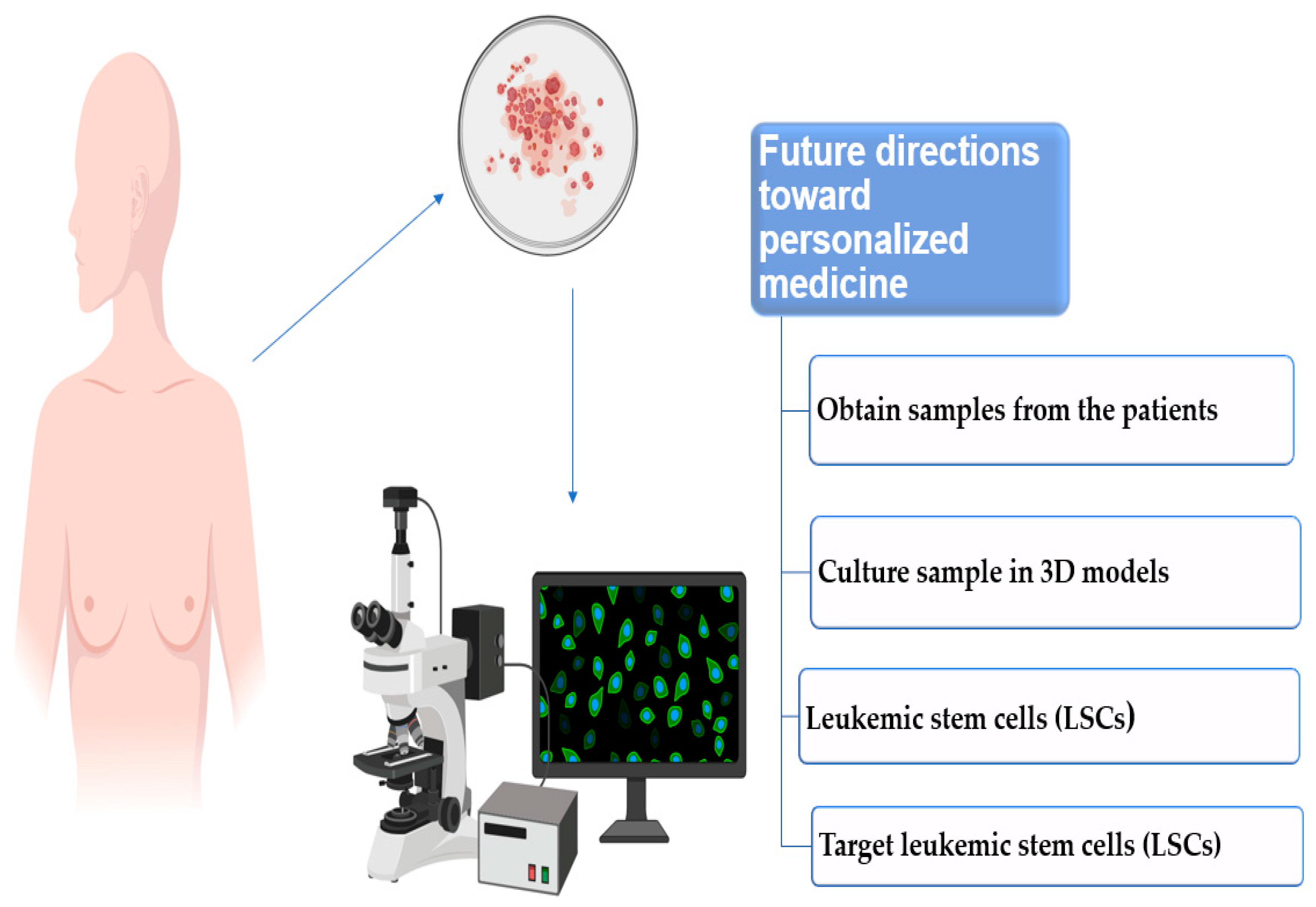
Future Directions toward Personalized Medicine
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Tallman, M.S.; Gilliland, D.G.; Rowe, J.M. Drug therapy for acute myeloid leukemia. Blood 2005, 106, 1154–1163. [Google Scholar] [CrossRef] [PubMed]
- Leopold, L.H.; Willemze, R. The Treatment of Acute Myeloid Leukemia in First Relapse: A Comprehensive Review of the Literature. Leuk. Lymphoma 2002, 43, 1715–1727. [Google Scholar] [CrossRef] [PubMed]
- Venditti, A.; Buccisano, F.; Del Poeta, G.; Maurillo, L.; Tamburini, A.; Cox, C.; Battaglia, A.; Catalano, G.; Del Moro, B.; Cudillo, L.; et al. Level of minimal residual disease after consolidation therapy predicts outcome in acute myeloid leukemia. Blood 2000, 96, 3948–3952. [Google Scholar] [CrossRef] [PubMed]
- Maurillo, L.; Buccisano, F.; del Principe, M.I.; DEL Poeta, G.; Spagnoli, A.; Panetta, P.; Ammatuna, E.; Neri, B.; Ottaviani, L.; Sarlo, C.; et al. Toward Optimization of Postremission Therapy for Residual Disease–Positive Patients with Acute Myeloid Leukemia. J. Clin. Oncol. 2008, 26, 4944–4951. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Short, N.J.; Zhou, S.; Fu, C.; Berry, D.A.; Walter, R.B.; Freeman, S.D.; Hourigan, C.S.; Huang, X.; Nogueras Gonzalez, G.; Hwang, H.; et al. Association of Measurable Residual Disease with Survival Outcomes in Patients with Acute Myeloid Leukemia: A Systematic Review and Meta-analysis. JAMA Oncol. 2020, 6, 1890–1899. [Google Scholar] [CrossRef]
- Van Gils, N.; Denkers, F.; Smit, L. Escape from Treatment; the Different Faces of Leukemic Stem Cells and Therapy Resistance in Acute Myeloid Leukemia. Front. Oncol. 2021, 11, 659253. [Google Scholar] [CrossRef]
- Feller, N.; Van Der Pol, M.A.; Van Stijn, A.; Weijers, G.W.D.; Westra, A.H.; Evertse, B.W.; Ossenkoppele, G.J.; Schuurhuis, G.J. MRD parameters using immunophenotypic detection methods are highly reliable in predicting survival in acute myeloid leukaemia. Leukemia 2004, 18, 1380–1390. [Google Scholar] [CrossRef] [PubMed]
- Van Rhenen, A.; Feller, N.; Kelder, A.; Westra, A.H.; Rombouts, E.; Zweegman, S.; van der Pol, M.A.; Waisfisz, Q.; Ossenkoppele, G.J.; Schuurhuis, G.J. High Stem Cell Frequency in Acute Myeloid Leukemia at Diagnosis Predicts High Minimal Residual Disease and Poor Survival. Clin. Cancer Res. 2005, 11, 6520–6527. [Google Scholar] [CrossRef] [Green Version]
- McCulloch, E.A. Stem cells in normal and leukemic hemopoiesis (Henry Stratton Lecture, 1982). Blood 1983, 62, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dick, J.E. Complexity of the human acute myeloid leukemia stem cell compartment: Implications for therapy. Biol. Blood Marrow Transplant. 2005, 11, 9–11. [Google Scholar] [CrossRef] [PubMed]
- Soto, C.A.; Celso, C.L.; Purton, L.E.; Frisch, B.J. From the niche to malignant hematopoiesis and back: Reciprocal interactions between leukemia and the bone marrow microenvironment. JBMR Plus 2021, 5, e10516. [Google Scholar] [CrossRef]
- Rashidi, A.; Uy, G.L. Targeting the Microenvironment in Acute Myeloid Leukemia. Curr. Hematol. Malign-Rep. 2015, 10, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Lund, A.; Yener, B.; Stegemann, J.P.; Plopper, G.E. The Natural and Engineered 3D Microenvironment as a Regulatory Cue During Stem Cell Fate Determination. Tissue Eng. Part B Rev. 2009, 15, 371–380. [Google Scholar] [CrossRef]
- Aljitawi, O.S.; Li, D.; Xiao, Y.; Zhang, D.; Ramachandran, K.; Stehno-Bittel, L.; Van Veldhuizen, P.; Lin, T.L.; Kambhampati, S.; Garimella, R. A novel three-dimensional stromal-based model for in vitro chemotherapy sensitivity testing of leukemia cells. Leuk. Lymphoma 2014, 55, 378–391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bray, L.J.; Binner, M.; Körner, Y.; von Bonin, M.; Bornhäuser, M.; Werner, C. A three-dimensional ex vivo tri-culture model mimics cell-cell interactions between acute myeloid leukemia and the vascular niche. Haematologica 2017, 102, 1215–1226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Velliou, E.G.; Dos Santos, S.B.; Papathanasiou, M.; Fuentes-Garí, M.; Misener, R.; Panoskaltsis, N.; Pistikopoulos, S.; Mantalaris, A. Towards unravelling the kinetics of an acute myeloid leukaemia model system under oxidative and starvation stress: A comparison between two- and three-dimensional cultures. Bioprocess Biosyst. Eng. 2015, 38, 1589–1600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, D.; Lin, T.L.; Lipe, B.; Hopkins, R.A.; Shinogle, H.; Aljitawi, O.S. A novel extracellular matrix-based leukemia model supports leukemia cells with stem cell-like characteristics. Leuk. Res. 2018, 72, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Borella, G.; Da Ros, A.; Borile, G.; Porcù, E.; Tregnago, C.; Benetton, M.; Marchetti, A.; Bisio, V.; Montini, B.; Michielotto, B.; et al. Targeting the plasticity of mesenchymal stromal cells to reroute the course of acute myeloid leukemia. Blood 2021, 138, 557–570. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, M.R.; Barata, D.; Teixeira, L.M.; Giselbrecht, S.; Reis, R.L.; Oliveira, J.M.; Truckenmüller, R.; Habibovic, P. Colorectal tumor-on-a-chip system: A 3D tool for precision onco-nanomedicine. Sci. Adv. 2019, 5, eaaw1317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García-García, A.; Klein, T.; Born, G.; Hilpert, M.; Scherberich, A.; Lengerke, C.; Skoda, R.C.; Bourgine, P.E.; Martin, I. Culturing patient-derived malignant hematopoietic stem cells in engineered and fully humanized 3D niches. Proc. Natl. Acad. Sci. USA 2021, 118, e2114227118. [Google Scholar] [CrossRef] [PubMed]
- Zippel, S.; Dilger, N.; Chatterjee, C.; Raic, A.; Brenner-Weiß, G.; Schadzek, P.; Rapp, B.E.; Lee-Thedieck, C. A parallelized, perfused 3D triculture model of leukemia for in vitro drug testing of chemotherapeutics. Biofabrication 2022, 14, 035011. [Google Scholar] [CrossRef] [PubMed]
- Chou, D.B.; Frismantas, V.; Milton, Y.; David, R.; Pop-Damkov, P.; Ferguson, D.; Macdonald, A.; Bölükbaşı, Ö.V.; Joyce, C.E.; Teixeira, L.S.M.; et al. On-chip recapitulation of clinical bone marrow toxicities and patient-specific pathophysiology. Nat. Biomed. Eng. 2020, 4, 394–406. [Google Scholar] [CrossRef] [PubMed]
- Sharipol, A.; Lesch, M.L.; Soto, C.A.; Frisch, B.J. Bone Marrow Microenvironment-On-Chip for Culture of Functional Hematopoietic Stem Cells. Front. Bioeng. Biotechnol. 2022, 10, 855777. [Google Scholar] [CrossRef]
- Scielzo, C.; Ghia, P. Modeling the Leukemia Microenviroment In Vitro. Front. Oncol. 2020, 10, 607608. [Google Scholar] [CrossRef]
- Baksh, D.; Yao, R.; Tuan, R.S. Comparison of Proliferative and Multilineage Differentiation Potential of Human Mesenchymal Stem Cells Derived from Umbilical Cord and Bone Marrow. Stem Cells 2007, 25, 1384–1392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, L.-L.; Liu, Y.; Yang, S.-G.; Zhao, Q.-J.; Wang, X.; Gong, W.; Han, Z.-B.; Xu, Z.-S.; Lu, Y.-X.; Liu, D.; et al. Isolation and characterization of human umbilical cord mesenchymal stem cells with hematopoiesis-supportive function and other potentials. Haematologica 2006, 91, 1017–1026. [Google Scholar]
- Valent, P. Targeting of leukemia-initiating cells to develop curative drug therapies: Straightforward but nontrivial concept. Curr. Cancer Drug Targets 2011, 11, 56–71. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Li, S. Survival regulation of leukemia stem cells. Cell. Mol. Life Sci. 2016, 73, 1039–1050. [Google Scholar] [CrossRef] [PubMed]
- Ye, H.; Adane, B.; Khan, N.; Sullivan, T.; Minhajuddin, M.; Gasparetto, M.; Stevens, B.; Pei, S.; Balys, M.; Ashton, J.M.; et al. Leukemic Stem Cells Evade Chemotherapy by Metabolic Adaptation to an Adipose Tissue Niche. Cell Stem Cell 2016, 19, 23–37. [Google Scholar] [CrossRef] [Green Version]
- Essers, M.A.G.; Trumpp, A. Targeting leukemic stem cells by breaking their dormancy. Mol. Oncol. 2010, 4, 443–450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nwajei, F.; Konopleva, M. The Bone Marrow Microenvironment as Niche Retreats for Hematopoietic and Leukemic Stem Cells. Adv. Hematol. 2013, 2013, 953982. [Google Scholar] [CrossRef] [PubMed]
- Naveiras, O.; Daley, G.Q. Stem cells and their niche: A matter of fate. Experientia 2006, 63, 760–766. [Google Scholar] [CrossRef] [PubMed]
- Dong-Feng, Z.; Ting, L.; Yong, Z.; Cheng, C.; Xi, Z.; Pei-Yan, K. The TPO/c-MPL Pathway in the Bone Marrow may Protect Leukemia Cells from Chemotherapy in AML Patients. Pathol. Oncol. Res. 2013, 20, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Al-Mawali, A.; Gillis, D.; Lewis, I. Immunoprofiling of leukemic stem cells CD34+/CD38-/CD123+ delineate FLT3/ITD-positive clones. J. Hematol. Oncol. 2016, 9, 61. [Google Scholar] [CrossRef] [Green Version]
- Hosen, N.; Park, C.Y.; Tatsumi, N.; Oji, Y.; Sugiyama, H.; Gramatzki, M.; Krensky, A.M.; Weissman, I.L. CD96 is a leukemic stem cell-specific marker in human acute myeloid leukemia. Proc. Natl. Acad. Sci. USA 2007, 104, 11008–11013. [Google Scholar] [CrossRef] [Green Version]
- Staal, F.J.; Clevers, H.C. WNT signalling and haematopoiesis: A WNT–WNT situation. Nat. Rev. Immunol. 2005, 5, 21–30. [Google Scholar] [CrossRef]
- Chan, W.-I.; Huntly, B. Leukemia Stem Cells in Acute Myeloid Leukemia. Semin. Oncol. 2008, 35, 326–335. [Google Scholar] [CrossRef]
- Lane, S.W.; Gilliland, D.G. Leukemia stem cells. Semin. Cancer Biol. 2010, 20, 71–76. [Google Scholar] [CrossRef]
- Döhner, H.; Weisdorf, D.J.; Bloomfield, C.D. Acute Myeloid Leukemia. N. Engl. J. Med. 2015, 373, 1136–1152. [Google Scholar] [CrossRef] [Green Version]
- Arfons, L.M.; Tomblyn, M.; Rocha, V.; Lazarus, H.M. Second hematopoietic stem cell transplantation in myeloid malignancies. Curr. Opin. Hematol. 2009, 16, 112–123. [Google Scholar] [CrossRef]
- Uwe, P.; Marc, B.; Christoph, S.; Claudia, R.; Gerhard, E.; Martin, B. Second donation of hematopoietic stem cells from unrelated donors for patients with relapse or graft failure after allogeneic transplantation. Haematologica 2008, 93, 1276–1278. [Google Scholar]
- Thol, F.; Ganser, A. Treatment of Relapsed Acute Myeloid Leukemia. Curr. Treat. Options Oncol. 2020, 21, 66. [Google Scholar] [CrossRef]
- Alhallak, K.; Sun, J.; Muz, B.; Jeske, A.; Yavner, J.; Bash, H.; Park, C.; Lubben, B.; Adebayo, O.; Achilefu, S.; et al. Nanoparticle T cell engagers for the treatment of acute myeloid leukemia. Oncotarget 2021, 12, 1878–1885. [Google Scholar] [CrossRef]
- He, S.Z.; Busfield, S.; Ritchie, D.S.; Hertzberg, M.S.; Durrant, S.; Lewis, I.D.; Marlton, P.; McLachlan, A.; Kerridge, I.; Bradstock, K.F.; et al. A Phase 1 study of the safety, pharmacokinetics and anti-leukemic activity of the anti-CD123 monoclonal antibody CSL360 in relapsed, refractory or high-risk acute myeloid leukemia. Leuk. Lymphoma 2014, 56, 1406–1415. [Google Scholar] [CrossRef]
- Cortes, J.E.; Smith, B.D.; Wang, E.S.; Merchant, A.; Oehler, V.G.; Arellano, M.; DeAngelo, D.J.; Pollyea, D.A.; Sekeres, M.A.; Robak, T.; et al. Glasdegib in combination with cytarabine and daunorubicin in patients with AML or high-risk MDS: Phase 2 study results. Am. J. Hematol. 2018, 93, 1301–1310. [Google Scholar] [CrossRef] [Green Version]
- Konopleva, M.; Pollyea, D.A.; Potluri, J.; Chyla, B.; Hogdal, L.; Busman, T.; McKeegan, E.; Salem, A.H.; Zhu, M.; Ricker, J.L.; et al. Efficacy and Biological Correlates of Response in a Phase II Study of Venetoclax Monotherapy in Patients with Acute Myelogenous Leukemia. Cancer Discov. 2016, 6, 1106–1117. [Google Scholar] [CrossRef] [Green Version]
- Ma, X.-Y.; Wei, L.; Lei, Z.; Chen, Y.; Ding, Z.; Chen, Z.-S. Recent progress on targeting leukemia stem cells. Drug Discov. Today 2021, 26, 1904–1913. [Google Scholar] [CrossRef]
- Uy, G.L.; Rettig, M.P.; Motabi, I.H.; McFarland, K.; Trinkaus, K.M.; Hladnik, L.M.; Kulkarni, S.; Abboud, C.N.; Cashen, A.F.; Stockerl-Goldstein, K.E.; et al. A phase 1/2 study of chemosensitization with the CXCR4 antagonist plerixafor in relapsed or refractory acute myeloid leukemia. Blood 2012, 119, 3917–3924. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Kaabneh, B.; Frisch, B.; Aljitawi, O.S. The Potential Role of 3D In Vitro Acute Myeloid Leukemia Culture Models in Understanding Drug Resistance in Leukemia Stem Cells. Cancers 2022, 14, 5252. https://doi.org/10.3390/cancers14215252
Al-Kaabneh B, Frisch B, Aljitawi OS. The Potential Role of 3D In Vitro Acute Myeloid Leukemia Culture Models in Understanding Drug Resistance in Leukemia Stem Cells. Cancers. 2022; 14(21):5252. https://doi.org/10.3390/cancers14215252
Chicago/Turabian StyleAl-Kaabneh, Basil, Benjamin Frisch, and Omar S. Aljitawi. 2022. "The Potential Role of 3D In Vitro Acute Myeloid Leukemia Culture Models in Understanding Drug Resistance in Leukemia Stem Cells" Cancers 14, no. 21: 5252. https://doi.org/10.3390/cancers14215252
APA StyleAl-Kaabneh, B., Frisch, B., & Aljitawi, O. S. (2022). The Potential Role of 3D In Vitro Acute Myeloid Leukemia Culture Models in Understanding Drug Resistance in Leukemia Stem Cells. Cancers, 14(21), 5252. https://doi.org/10.3390/cancers14215252







