Real-World Study: A Powerful Tool for Malignant Tumor Research in General Surgery
Abstract
Simple Summary
Abstract
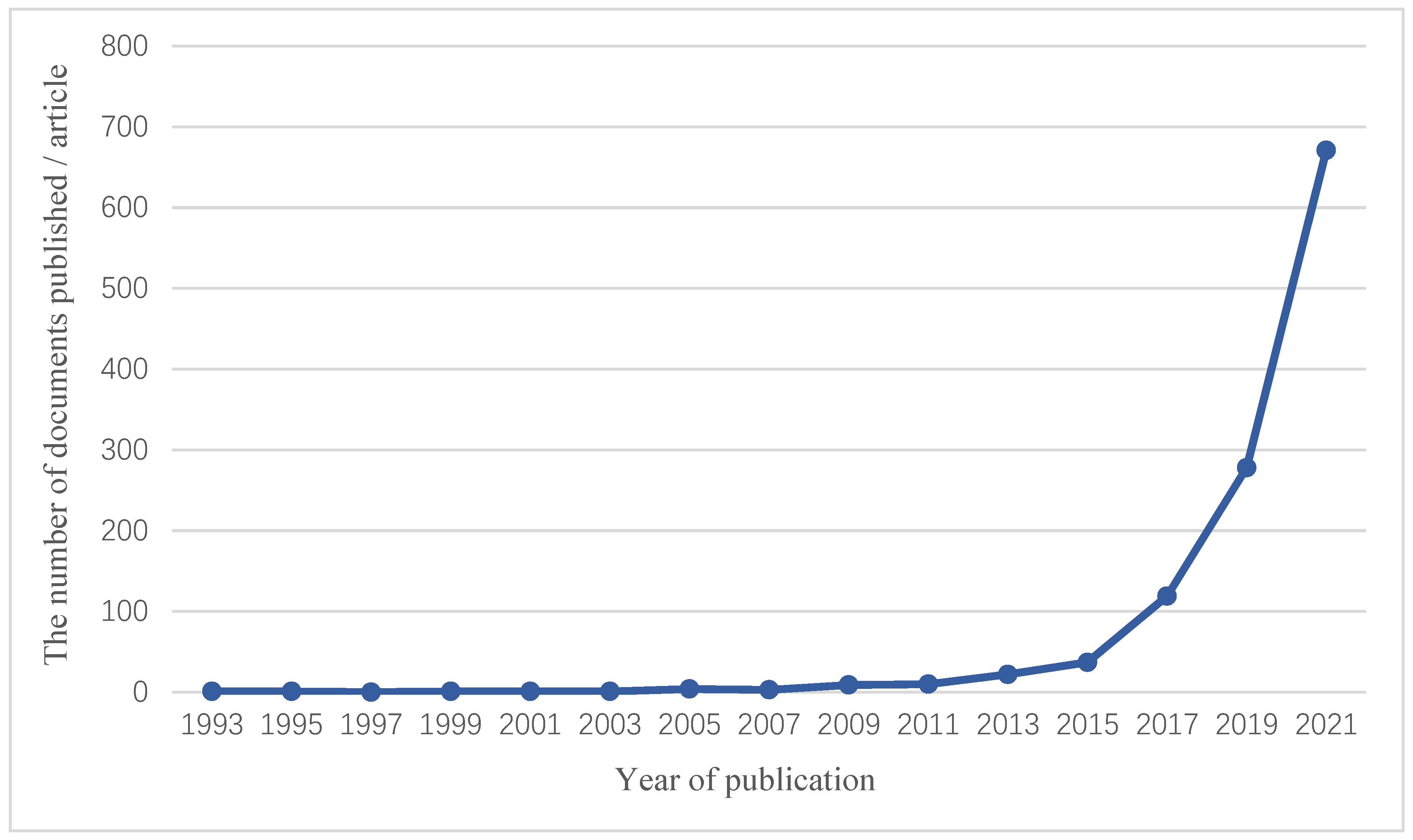
1. Introduction
2. RCT and RWS
3. Breast Cancer (BC)
4. Hepatocellular Carcinoma (HCC)
5. Colorectal Cancer (CRC)
6. Gastric Cancer (GC)
7. Issues and Prospects
8. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Ford, I.; Norrie, J. Pragmatic Trials. N. Engl. J. Med. 2016, 375, 454–463. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, N.M.; Sproul, L.E.; Mulcahy, W.S. Large prospective study of ramipril in patients with hypertension. CARE Investigators. Clin. Ther. 1993, 15, 810–818. [Google Scholar] [PubMed]
- Sun, X.; Tan, J.; Tang, L.; Guo, J.J.; Li, X. Real world evidence: Experience and lessons from China. BMJ 2018, 360, j5262. [Google Scholar] [CrossRef] [PubMed]
- Freemantle, N.; Strack, T. Real-world effectiveness of new medicines should be evaluated by appropriately designed clinical trials. J. Clin. Epidemiol. 2010, 63, 1053–1058. [Google Scholar] [CrossRef]
- Thorpe, K.E.; Zwarenstein, M.; Oxman, A.D.; Treweek, S.; Furberg, C.D.; Altman, D.G.; Tunis, S.; Bergel, E.; Harvey, I.; Magid, D.J.; et al. A pragmatic-explanatory continuum indicator summary (PRECIS): A tool to help trial designers. Can. Med Assoc. J. 2009, 180, E47–E57. [Google Scholar] [CrossRef]
- Sherman, R.E.; Anderson, S.A.; Dal Pan, G.J.; Gray, G.W.; Gross, T.; Hunter, N.L.; LaVange, L.; Marinac-Dabic, D.; Marks, P.W.; Robb, M.A. Real-World Evidence—What Is It and What Can It Tell Us? N. Engl. J. Med. 2016, 375, 2293–2297. [Google Scholar] [CrossRef]
- Makady, A.; de Boer, A.; Hillege, H.; Klungel, O.; Gorttsch, W.; on behalf of GetReal Work Package 1. What Is Real-World Data? A Review of Definitions Based on Literature and Stakeholder Interviews. Value Health 2017, 20, 858–865. [Google Scholar] [CrossRef]
- Sox, H.C.; Lewis, R.J. Pragmatic Trials: Practical Answers to “Real World” Questions. JAMA 2016, 316, 1205–1206. [Google Scholar] [CrossRef]
- Aljunid, S.M.; Srithamrongsawat, S.; Chen, W.; Bae, S.J.; Pwu, R.-F.; Ikeda, S.; Xu, L. Health-care data collecting, sharing, and using in Thailand, China mainland, South Korea, Taiwan, Japan, and Malaysia. Value Health 2012, 15, S132–S138. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2018. CA Cancer J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef]
- Chang, J.; Clark, G.M.; Allred, D.C.; Mohsin, S.; Chamness, G.; Elledge, R.M. Survival of patients with metastatic breast carcinoma: Importance of prognostic markers of the primary tumor. Cancer 2003, 97, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F.; Senkus, E.; Costa, A.; Papadopoulos, E.; Aapro, M.; André, F.; Harbeck, N.; Aguilar Lopez, B.; Barrios, C.H.; Bergh, J.; et al. 4th ESO-ESMO International Consensus Guidelines for Advanced Breast Cancer (ABC 4). Ann. Oncol. 2018, 29, 1634–1657. [Google Scholar] [CrossRef] [PubMed]
- Lei, W.; Li, H.; Song, G.; Zhang, R.; Ran, R.; Yan, Y.; Di, L.; Jiang, H. Efficacy and Safety of Fulvestrant 500mg in Hormone-receptor Positive Human Epidermal Receptor 2 Negative Advanced Breast Cancer: A Real-world Study in China. J. Cancer 2020, 11, 6612–6622. [Google Scholar] [CrossRef] [PubMed]
- Beachler, D.C.; de Luise, C.; Jamal-Allial, A.; Yin, R.; Taylor, D.H.; Suzuki, A.; Lewis, J.H.; Freston, J.W.; Lanes, S. Real-world safety of palbociclib in breast cancer patients in the United States: A new user cohort study. BMC Cancer 2021, 21, 97. [Google Scholar] [CrossRef]
- Davie, A.; Carter, G.C.; Rider, A.; Pike, J.; Lewis, K.; Bailey, A.; Price, G.L.; Ringeisen, F.; Pivot, X. Real-world patient-reported outcomes of women receiving initial endocrine-based therapy for HR+/HER2- advanced breast cancer in five European countries. BMC Cancer 2020, 20, 855. [Google Scholar] [CrossRef]
- Basile, D.; Gerratana, L.; Corvaja, C.; Pelizzari, G.; Franceschin, G.; Bertoli, E.; Palmero, L.; Zara, D.; Alberti, M.; Buriolla, S.; et al. First- and second-line treatment strategies for hormone-receptor (HR)-positive HER2-negative metastatic breast cancer: A real-world study. Breast 2021, 57, 104–112. [Google Scholar] [CrossRef]
- Zhao, Y.; Li, Y.; Gong, C.; Xie, Y.; Zhang, J.; Wang, L.; Cao, J.; Tao, Z.; Wang, B.; Hu, X. Optimal duration of prior endocrine therapy predicts the efficacy of Fulvestrant in a real-world study for patients with hormone receptor-positive and HER2-negative advanced breast cancer. Cancer Med. 2020, 9, 8821–8831. [Google Scholar] [CrossRef]
- Batra, A.; Hannouf, M.B.; Alsafar, N.; Lupichuk, S. Four cycles of docetaxel and cyclophosphamide as adjuvant chemotherapy in node negative breast cancer: A real-world study. Breast 2020, 54, 1–7. [Google Scholar] [CrossRef]
- Guo, J.; Li, Q.; Zhang, P.; Yuan, P.; Wang, J.; Ma, F.; Fan, Y.; Cai, R.; Luo, Y.; Li, Q.; et al. Trastuzumab plus adjuvant chemotherapy for human epidermal growth factor receptor 2 (HER2)-positive early-stage breast cancer: A real-world retrospective study in Chinese patients. Chin. J. Cancer Res. 2019, 31, 759–770. [Google Scholar] [CrossRef]
- Cameron, D.; Piccart-Gebhart, M.J.; Gelber, R.D.; Procter, M.; Goldhirsch, A.; de Azambuja, E.; Castro, G., Jr.; Untch, M.; Smith, I.; Gianni, L.; et al. 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: Final analysis of the HERceptin Adjuvant (HERA) trial. Lancet 2017, 389, 1195–1205. [Google Scholar] [CrossRef]
- Lambertini, M.; Pondé, N.F.; Solinas, C.; De Azambuja, E. Adjuvant trastuzumab: A 10-year overview of its benefit. Expert Rev. Anticancer Ther. 2017, 17, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Bian, L.; Wang, T.; Zhang, S.; Li, J.; Xu, F.; Jiang, Z. Effectiveness of second-line anti-HER2 treatment in HER2-positive metastatic breast cancer patients previously treated with trastuzumab: A real-world study. Chin. J. Cancer Res. 2020, 32, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Gui, X.; Li, H.; Yan, Y.; Zhang, R. Efficacy of lapatinib combined with capecitabine in patients with HER2-positive metastatic breast cancer in a real-world study. Oncol. Lett. 2020, 20, 378. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Luo, X.; Du, Q.; Li, H.; Liu, H.-Y.; Yu, B.; Zhai, Q. Efficacy and safety of lapatinib in Chinese breast cancer patients: A real-world study. Ann. Transl. Med. 2020, 8, 240. [Google Scholar] [CrossRef] [PubMed]
- Hardy-Werbin, M.; Quiroga, V.; Cirauqui, B.; Romeo, M.; Felip, E.; Teruel, I.; Garcia, J.J.; Erasun, C.; España, S.; Cucurull, M.; et al. Real-world data on T-DM1 efficacy—Results of a single-center retrospective study of HER2-positive breast cancer patients. Sci. Rep. 2019, 9, 12760. [Google Scholar] [CrossRef] [PubMed]
- Lidbrink, E.; Chmielowska, E.; Otremba, B.; Bouhlel, A.; Lauer, S.; Hermoso, M.L.; Nüesch, E.; Shing, M.; Misra, V. A real-world study of cardiac events in > 3700 patients with HER2-positive early breast cancer treated with trastuzumab: Final analysis of the OHERA study. Breast Cancer Res. Treat. 2019, 174, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Ward, M.; Harnett, J.; Bell, T.J.; Mardekian, J. Risk Factors of QTc Prolongation in Women with Hormone Receptor-positive/Human Epidermal Growth Factor Receptor 2-negative Metastatic Breast Cancer: A Retrospective Analysis of Health Care Claims Data. Clin. Ther. 2019, 41, 494–504.e1. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, D.J.; Chen, Q.T.; Anwar, M.; Xie, N.; Ouyang, Q.C.; Fan, P.Z.; Qian, L.Y.; Chen, G.N.; Zhou, E.X.; Guo, L.; et al. The Efficacy of Pyrotinib as a Third- or Higher-Line Treatment in HER2-Positive Metastatic Breast Cancer Patients Exposed to Lapatinib Compared to Lapatinib-Naive Patients: A Real-World Study. Front. Pharmacol. 2021, 12, 682568. [Google Scholar] [CrossRef]
- Zhang, L.; Wu, X.; Zhou, J.; Zhu, M.; Yu, H.; Zhang, Y.; Zhao, Y.; Han, Z.; Guo, Y.; Guan, X.; et al. Pyrotinib in the Treatment of Women with HER2-Positive Advanced Breast Cancer: A Multicenter, Prospective, Real-World Study. Front. Oncol. 2021, 11, 699323. [Google Scholar] [CrossRef]
- Li, F.; Xu, F.; Li, J.; Wang, T.; Bian, L.; Zhang, S.; Jiang, Z. Pyrotinib versus trastuzumab emtansine for HER2-positive metastatic breast cancer after previous trastuzumab and lapatinib treatment: A real-world study. Ann. Transl. Med. 2021, 9, 103. [Google Scholar] [CrossRef]
- Anwar, M.; Chen, Q.; Ouyang, D.; Wang, S.; Xie, N.; Ouyang, Q.; Fan, P.; Qian, L.; Chen, G.; Zhou, E.; et al. Pyrotinib Treatment in Patients with HER2-positive Metastatic Breast Cancer and Brain Metastasis: Exploratory Final Analysis of Real-World, Multicenter Data. Clin. Cancer Res. 2021, 27, 4634–4641. [Google Scholar] [CrossRef] [PubMed]
- Niu, L.; Lv, H.; Zhang, M.; Zeng, H.; Wang, L.; Cui, S.; Liu, Z.; Yan, M. Clinical diagnosis and treatment of breast cancer with brain metastases and establishment of a prognostic model: A 10-year, single-center, real-world study of 559 cases. Ann. Transl. Med. 2021, 9, 1331. [Google Scholar] [CrossRef] [PubMed]
- Xie, N.; Tian, C.; Wu, H.; Yang, X.; Liu, L.; Li, J.; Xiao, H.; Gao, J.; Lu, J.; Hu, X.; et al. FGFR aberrations increase the risk of brain metastases and predict poor prognosis in metastatic breast cancer patients. Ther. Adv. Med. Oncol. 2020, 12, 1758835920915305. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Bian, X.; Liu, Z.; Wang, X.; Song, X.; Zhao, W.; Liu, Y.; Yu, Z. Effectiveness and safety of pyrotinib-based therapy in patients with HER2-positive metastatic breast cancer: A real-world retrospective study. Cancer Med. 2021, 10, 8352–8364. [Google Scholar] [CrossRef]
- Denkert, C.; Liedtke, C.; Tutt, A.; von Minckwitz, G. Molecular alterations in triple-negative breast cancer—The road to new treatment strategies. Lancet 2017, 389, 2430–2442. [Google Scholar] [CrossRef]
- Chen, Y.; Guan, Y.; Wang, J.; Ma, F.; Luo, Y.; Chen, S.; Zhang, P.; Li, Q.; Cai, R.; Li, Q. Platinum-based chemotherapy in advanced triple-negative breast cancer: A multicenter real-world study in China. Int. J. Cancer 2020, 147, 3490–3499. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Li, L.; Zhang, S.; Zhu, W.; Yang, S.; Di, G.; Ma, X.; Yang, H. Efficacy of Neoadjuvant Chemotherapy with Epirubicin and Cyclophosphamide and Weekly Paclitaxel and Trastuzumab in Human Epidermal Growth Factor Receptor 2-Positive Breast Carcinoma: A Real-World Study. Biomed. Res. Int. 2020, 2020, 3208391. [Google Scholar] [CrossRef]
- O’Brien, M.E.; Wigler, N.; Inbar, M.; Rosso, R.; Grischke, E.; Santoro, A.; Catane, R.; Kieback, D.G.; Tomczak, P.; Ackland, S.P. Reduced cardiotoxicity and comparable efficacy in a phase III trial of pegylated liposomal doxorubicin HCl (CAELYX/Doxil) versus conventional doxorubicin for first-line treatment of metastatic breast cancer. Ann. Oncol. 2004, 15, 440–449. [Google Scholar] [CrossRef]
- Zhang, J.; Jiang, H.; Bao, G.; Zhang, G.; Wang, H.; Wang, X. Effectiveness and safety of pegylated liposomal doxorubicin versus epirubicin as neoadjuvant or adjuvant chemotherapy for breast cancer: A real-world study. BMC Cancer 2021, 21, 1301. [Google Scholar] [CrossRef]
- Chen, R.; Li, S.; Li, Y.; Zhu, Q.; Shi, X.; Xu, L.; Xu, Y.; Zhang, W.; Huang, X.; Wang, J.; et al. Can axillary surgery be omitted in patients with breast pathologic complete response after neoadjuvant systemic therapy for breast cancer? A real-world retrospective study in China. J. Cancer Res. Clin. Oncol. 2021, 147, 3495–3501. [Google Scholar] [CrossRef]
- Ai, X.; Liao, X.; Li, J.; Tang, P.; Jiang, J. Clinical Outcomes of N3 Breast Cancer: A Real-World Study of a Single Institution and the US Surveillance, Epidemiology, and End Results (SEER) Database. Cancer Manag. Res. 2020, 12, 5331–5343. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.; Fu, X.; Xu, S.; Qiu, P.; Lv, Z.; Xu, Y.; Zhang, Q. Quantification of Ki67 Change as a Valid Prognostic Indicator of Luminal B Type Breast Cancer After Neoadjuvant Therapy. Pathol. Oncol. Res. 2021, 27, 1609972. [Google Scholar] [CrossRef] [PubMed]
- O’Shaughnessy, J.; Robert, N.; Annavarapu, S.; Zhou, J.; Sussell, J.; Cheng, A.; Fung, A. Recurrence rates in patients with HER2+ breast cancer who achieved a pathological complete response after neoadjuvant pertuzumab plus trastuzumab followed by adjuvant trastuzumab: A real-world evidence study. Breast Cancer Res. Treat. 2021, 187, 903–913. [Google Scholar] [CrossRef]
- Schad, F.; Thronicke, A.; Von Trott, P.; Oei, S.L. Analysis of Changes in Cancer-Related Fatigue of Breast Cancer Patients Receiving an Integrative Medicine Program. Integr. Cancer Ther. 2020, 19, 1534735420963780. [Google Scholar] [CrossRef]
- Oei, S.L.; Thronicke, A.; Matthes, H.; Schad, F. Evaluation of the effects of integrative non-pharmacological interventions on the internal coherence and resilience of breast cancer patients. Support. Care Cancer 2021, 29, 1413–1421. [Google Scholar] [CrossRef]
- Zhang, X.; Yang, L.; Liu, S.; Li, H.; Li, Q.; Cheng, Y.; Wang, N.; Ji, J. Evaluation of Different Breast Cancer Screening Strategies for High-Risk Women in Beijing, China: A Real-World Population-Based Study. Front. Oncol. 2021, 11, 776848. [Google Scholar] [CrossRef]
- Bonotto, M.; Basile, D.; Gerratana, L.; Bartoletti, M.; Lisanti, C.; Pelizzari, G.; Vitale, M.G.; Fanotto, V.; Poletto, E.; Minisini, A.M.; et al. Clinico-radiological monitoring strategies in patients with metastatic breast cancer: A real-world study. Future Oncol. 2020, 16, 2059–2073. [Google Scholar] [CrossRef]
- Llovet, J.M.; Ricci, S.; Mazzaferro, V.; Hilgard, P.; Gane, E.; Blanc, J.F.; De Oliveira, A.C.; Santoro, A.; Raoul, J.L.; Forner, A.; et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 2008, 359, 378–390. [Google Scholar] [CrossRef]
- Cheng, A.-L.; Kang, Y.-K.; Chen, Z.; Tsao, C.-J.; Qin, S.; Kim, J.S.; Luo, R.; Feng, J.; Ye, S.; Yang, T.-S.; et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: A phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009, 10, 25–34. [Google Scholar] [CrossRef]
- Hanzel, J.; Bozic, T.K.; Stabuc, B.; Jansa, R. Sorafenib for the treatment of hepatocellular carcinoma: A single-centre real-world study. Radiol. Oncol. 2020, 54, 233–236. [Google Scholar] [CrossRef]
- Díaz-González, Á.; Sanduzzi-Zamparelli, M.; da Fonseca, L.G.; Di Costanzo, G.G.; Alves, R.; Iavarone, M.; Leal, C.; Sacco, R.; Matilla, A.M.; Hernández-Guerra, M.; et al. International and multicenter real-world study of sorafenib-treated patients with hepatocellular carcinoma under dialysis. Liver Int. 2020, 40, 1467–1476. [Google Scholar] [CrossRef] [PubMed]
- Marquardt, J.U.; Saborowski, A.; Czauderna, C.; Vogel, A. The Changing Landscape of Systemic Treatment of Advanced Hepatocellular Carcinoma: New Targeted Agents and Immunotherapies. Target Oncol. 2019, 14, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Sung, P.S.; Yang, H.; Lee, S.K.; Nam, H.C.; Yoo, S.H.; Lee, H.L.; Kim, H.Y.; Lee, S.W.; Kwon, J.H.; et al. A Real-World Comparative Analysis of Lenvatinib and Sorafenib as a Salvage Therapy for Transarterial Treatments in Unresectable HCC. J. Clin. Med. 2020, 9, 4121. [Google Scholar] [CrossRef]
- Wang, D.-X.; Yang, X.; Lin, J.-Z.; Bai, Y.; Long, J.-Y.; Yang, X.-B.; Seery, S.; Zhao, H.-T. Efficacy and safety of lenvatinib for patients with advanced hepatocellular carcinoma: A retrospective, real-world study conducted in China. World J. Gastroenterol. 2020, 26, 4465–4478. [Google Scholar] [CrossRef]
- Cheon, J.; Chon, H.J.; Bang, Y.; Park, N.H.; Shin, J.W.; Kim, K.M.; Lee, H.C.; Lee, J.; Yoo, C.; Ryoo, B.-Y. Real-World Efficacy and Safety of Lenvatinib in Korean Patients with Advanced Hepatocellular Carcinoma: A Multicenter Retrospective Analysis. Liver Cancer 2020, 9, 613–624. [Google Scholar] [CrossRef]
- Zhu, Y.; Sun, P.; Wang, K.; Xiao, S.; Cheng, Y.; Li, X.; Wang, B.; Li, J.; Yu, W.; Cheng, Y. Efficacy and safety of lenvatinib monotreatment and lenvatinib-based combination therapy for patients with unresectable hepatocellular carcinoma: A retrospective, real-world study in China. Cancer Cell Int. 2021, 21, 503. [Google Scholar] [CrossRef]
- Tomonari, T.; Sato, Y.; Tanaka, H.; Tanaka, T.; Taniguchi, T.; Sogabe, M.; Okamoto, K.; Miyamoto, H.; Muguruma, N.; Takayama, T. Sorafenib as second-line treatment option after failure of lenvatinib in patients with unresectable hepatocellular carcinoma. JGH Open 2020, 4, 1135–1139. [Google Scholar] [CrossRef]
- Bruix, J.; Qin, S.; Merle, P.; Granito, A.; Huang, Y.-H.; Bodoky, G.; Pracht, M.; Yokosuka, O.; Rosmorduc, O.; Breder, V.; et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017, 389, 56–66. [Google Scholar] [CrossRef]
- Hsu, P.; Cheng, T.; Chuang, S.; Chang, W.; Liang, P.; Hsu, C.; Wei, Y.; Jang, T.; Yeh, M.; Lin, Y.; et al. Regorafenib for Taiwanese patients with unresectable hepatocellular carcinoma after sorafenib failure: Impact of alpha-fetoprotein levels. Cancer Med. 2022, 11, 104–116. [Google Scholar] [CrossRef]
- Han, Y.; Cao, G.; Sun, B.; Wang, J.; Yan, D.; Xu, H.; Shi, Q.; Liu, Z.; Zhi, W.; Xu, L.; et al. Regorafenib combined with transarterial chemoembolization for unresectable hepatocellular carcinoma: A real-world study. BMC Gastroenterol. 2021, 21, 393. [Google Scholar] [CrossRef]
- Llovet, J.M.; Brú, C.; Bruix, J. Prognosis of hepatocellular carcinoma: The BCLC staging classification. Semin. Liver Dis. 1999, 19, 329–338. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Sun, H.; Li, F.; Yang, H.; Lou, M.; Wang, S.; Wu, C. Efficacy and safety of raltitrexed-based transcatheter arterial chemoembolization for intermediate and advanced hepatocellular carcinoma: A multicenter real-world study. Hepatol. Res. 2021, 51, 1153–1163. [Google Scholar] [CrossRef]
- Lu, L.; Zheng, P.; Wu, Z.; Chen, X. Hepatic Resection Versus Transarterial Chemoembolization for Intermediate-Stage Hepatocellular Carcinoma: A Cohort Study. Front. Oncol. 2021, 11, 618937. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Ke, Q.; Deng, M.; Huang, X.; Zeng, J.; Liu, H.; Yang, Y.; Zeng, Y.; Zhou, W.; Liu, J. Adjuvant transarterial chemoembolization for patients with hepatocellular carcinoma after radical hepatectomy: A real world study. Scand. J. Gastroenterol. 2019, 54, 1403–1411. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.-J.; Gao, S.; Zhu, X.; Guo, J.-H.; Kou, F.-X.; Liu, S.-X.; Zhang, X.; Wang, X.-D.; Cao, G.; Chen, H.; et al. Real-world study of hepatic artery infusion chemotherapy combined with anti-PD-1 immunotherapy and tyrosine kinase inhibitors for advanced hepatocellular carcinoma. Immunotherapy 2021, 13, 1395–1405. [Google Scholar] [PubMed]
- Ji, Y.; Zhu, J.; Zhu, L.; Zhu, Y.; Zhao, H. High-Intensity Focused Ultrasound Ablation for Unresectable Primary and Metastatic Liver Cancer: Real-World Research in a Chinese Tertiary Center With 275 Cases. Front. Oncol. 2020, 10, 519164. [Google Scholar] [CrossRef]
- Hatanaka, T.; Naganuma, A.; Shibasaki, M.; Kohga, T.; Arai, Y.; Nagashima, T.; Ueno, T.; Namikawa, M.; Saito, S.; Hoshino, T.; et al. The Role of the Albumin-Bilirubin Score for Predicting the Outcomes in Japanese Patients with Advanced Hepatocellular Carcinoma Treated with Ramucirumab: A Real-World Study. Oncology 2021, 99, 203–214. [Google Scholar] [CrossRef]
- Zhu, G.; Wang, W.; Liu, Q.; Chen, D.; Wen, L. A Real-World Study of Prognosis of N0M0 Hepatocellular Carcinoma with Hepatic Resection Based on SEER Database. Gastroenterol. Res. Pract. 2020, 2020, 2357840. [Google Scholar] [CrossRef]
- Benson, A.B.; Venook, A.P.; Al-Hawary, M.M.; Cederquist, L.; Chen, Y.-J.; Ciombor, K.K.; Cohen, S.; Cooper, H.S.; Deming, D.; Engstrom, P.F.; et al. NCCN Guidelines Insights: Colon Cancer, Version 2.2018. J. Natl. Compr. Cancer Netw. 2018, 16, 359–369. [Google Scholar]
- François, E.; Mineur, L.; Deplanque, G.; Laplaige, P.; Smith, D.; Gourgou, S.; Tanang, A.; Ionescu-Goga, M.; Veerabudun, K.; Lelarge, Y.; et al. Efficacy and Safety of Bevacizumab Combined with First-Line Chemotherapy in Elderly (≥75 Years) Patients with Metastatic Colorectal Cancer: A Real-World Study. Clin. Color. Cancer 2020, 19, e100–e109. [Google Scholar] [CrossRef]
- Akdeniz, N.; Küçüköner, M.; Kaplan, M.A.; Urakçı, Z.; Sezgin, Y.; Karhan, O.; Işıkdoğan, A. Survival impact of optimal treatment for elderly patients with colorectal cancer: A real world study. Indian J. Cancer 2021, 58, 539–544. [Google Scholar]
- Guo, Y.; Zheng, T.; Zhang, C.; Zhang, Y. A Study of the S-1 or Capecitabine as First-line Regimen in Patients with Metastatic Colorectal Cancer: A Real World Study. J. Cancer 2020, 11, 1839–1845. [Google Scholar] [CrossRef]
- Yuan, M.; Wang, Z.; Zhao, Y.; Feng, T.; Lv, W.; Zhong, H. Cetuximab Can Be an Effective and Low-Toxicity Maintenance Treatment Drug in Patients with Metastatic Colorectal Cancer: A Real-World Study of Zhejiang Cancer Hospital. Front. Pharmacol. 2021, 12, 632076. [Google Scholar] [CrossRef]
- Lamy, F.-X.; Batech, M.; Boutmy, E.; Ronga, P.; Salim, S.; Pescott, C.P. Comparative effectiveness of weekly versus every-2-weeks cetuximab in metastatic colorectal cancer in a US-insured population. J. Comp. Eff. Res. 2020, 9, 1117–1129. [Google Scholar] [CrossRef]
- Cheung, W.Y.; Kavan, P.; Dolley, A. Quality of life in a real-world study of patients with metastatic colorectal cancer treated with trifluridine/tipiracil. Curr. Oncol. 2020, 27, e451–e458. [Google Scholar] [CrossRef]
- Xu, J.; Ma, T.; Ye, Y.; Pan, Z.; Lu, D.; Pan, F.; Peng, W.; Sun, G. Surgery on primary tumor shows survival benefit in selected stage IV colon cancer patients: A real-world study based on SEER database. J. Cancer 2020, 11, 3567–3579. [Google Scholar] [CrossRef]
- Chen, P.-J.; Li, T.-L.; Sun, T.-T.; Willis, V.C.; Roebuck, M.C.; Bravata, D.M.; Liu, X.-Z.; Arriaga, Y.E.; Dankwa-Mullan, I.; Wu, A.-W. Clinical Decision Support for High-Risk Stage II Colon Cancer: A Real-World Study of Treatment Concordance and Survival. Dis. Colon. Rectum 2020, 63, 1383–1392. [Google Scholar] [CrossRef]
- Abdel-Rahman, O.; Tang, P.A.; Koski, S. Hospitalizations among early-stage colon cancer patients receiving adjuvant chemotherapy: A real-world study. Int. J. Colorectal. Dis. 2021, 36, 1905–1913. [Google Scholar] [CrossRef]
- Martínez-Lago, N.; Fernández-Montes, A.; Covela, M.; Brozos, E.M.; De la Cámara, J.; Méndez Méndez, J.C.; Jorge-Fernández, M.; Cousillas Castiñeiras, A.; Reboredo, C.; Arias Ron, D.; et al. Effect of antiangiogenic-based treatment and systemic inflammatory factors on outcomes in patients with BRAF v600-mutated metastatic colorectal cancer: A real-world study in Spain. BMC Cancer 2021, 21, 64. [Google Scholar] [CrossRef]
- García-Alfonso, P.; García-González, G.; Gallego, I.; Peligros, M.I.; Ortega, L.; Pérez-Solero, G.T.; Sandoval, C.; Martin, A.M.; Codesido, M.B.; Ferrándiz, A.C.; et al. Prognostic value of molecular biomarkers in patients with metastatic colorectal cancer: A real-world study. Clin. Transl. Oncol. 2021, 23, 122–129. [Google Scholar] [CrossRef]
- Mo, S.; Cai, X.; Zhou, Z.; Li, Y.; Hu, X.; Ma, X.; Zhang, L.; Cai, S.; Peng, J. Nomograms for predicting specific distant metastatic sites and overall survival of colorectal cancer patients: A large population-based real-world study. Clin. Transl. Med. 2020, 10, 169–181. [Google Scholar] [CrossRef]
- Du, Y.; Cao, Q.; Jiang, C.; Liang, H.; Ning, Z.; Ji, C.; Wang, J.; Zhou, C.; Jiang, Z.; Yu, C.; et al. Effectiveness and safety of low-dose apatinib in advanced gastric cancer: A real-world study. Cancer Med. 2020, 9, 5008–5014. [Google Scholar] [CrossRef]
- Wang, X.; Yu, J.; Yang, M.; Liu, L.; Gao, J.; Ren, Y.; Zhang, R.; Zhong, D.; Du, N.; Fu, Z.; et al. Safety and effectiveness of apatinib in patients with previously treated metastatic gastric cancer: A sub-analysis from the real-world study of apatinib for gastric cancer treatment (AHEAD-G202). Am. J. Cancer Res. 2020, 10, 987–996. [Google Scholar]
- Peng, W.; Zhang, F.; Wang, Z.; Li, D.; He, Y.; Ning, Z.; Sheng, L.; Wang, J.; Xia, X.; Yu, C.; et al. Large Scale, Multicenter, Prospective Study of Apatinib in Advanced Gastric Cancer: A Real-World Study from China. Cancer Manag. Res. 2020, 12, 6977–6985. [Google Scholar] [CrossRef]
- Zheng, X.-H.; Zhang, W.; Yang, L.; Du, C.-X.; Li, N.; Xing, G.-S.; Tian, Y.-T.; Xie, Y.-B. Role of D2 gastrectomy in gastric cancer with clinical para-aortic lymph node metastasis. World J. Gastroenterol. 2019, 25, 2338–2353. [Google Scholar] [CrossRef]
- Xu, W.; Wang, L.; Yan, C.; He, C.; Lu, S.; Ni, Z.; Hua, Z.; Zhu, Z.; Sah, B.K.; Yang, Z.; et al. Neoadjuvant Chemotherapy Versus Direct Surgery for Locally Advanced Gastric Cancer with Serosal Invasion (cT4NxM0): A Propensity Score-Matched Analysis. Front. Oncol. 2021, 11, 718556. [Google Scholar]
- Yu, S.; Wang, Y.; Cheng, X.; Lv, M.; Cui, Y.; Li, W.; Yu, Y.; Li, Q.; Liu, T. Prognosis of Adjuvant SOX vs XELOX Chemotherapy for Gastric Cancer After D2 Gastrectomy in Chinese Patients. Cancer Manag. Res. 2020, 12, 10091–10101. [Google Scholar] [CrossRef]
- Cheng, X.; Yu, S.; Wang, Y.; Cui, Y.; Li, W.; Yu, Y.; Tang, C.; Jiang, H.; Ji, Y.; Sun, Y.; et al. The role of oxaliplatin in the adjuvant setting of different Lauren’s type of gastric adenocarcinoma after D2 gastrectomy: A real-world study. Gastric Cancer 2019, 22, 587–597. [Google Scholar]
- Saif, M.; Makrilia, N.; Zalonis, A.; Merikas, M.; Syrigos, K. Gastric cancer in the elderly: An overview. Eur. J. Surg. Oncol. 2010, 36, 709–717. [Google Scholar]
- Wang, X.; Zhao, J.; Fairweather, M.; Yang, T.; Sun, Y.; Wang, J. Optimal treatment for elderly patients with resectable proximal gastric carcinoma: A real world study based on National Cancer Database. BMC Cancer 2019, 19, 1079. [Google Scholar]
- Zhao, L.; Li, J.; Bai, C.; Nie, Y.; Lin, G. Multi-Modality Treatment for Patients with Metastatic Gastric Cancer: A Real-World Study in China. Front. Oncol. 2019, 9, 1155. [Google Scholar] [CrossRef]
- Huang, T.; Luo, X.; Wu, B.; Peng, P.; Dai, Y.; Hu, G.; Qiu, H.; Yuan, X. Pyrotinib enhances the radiosensitivity of HER2-overexpressing gastric and breast cancer cells. Oncol. Rep. 2020, 44, 2634–2644. [Google Scholar] [CrossRef]
- Su, R.-Y.; Ling, S.-B.; Shan, Q.-N.; Wei, X.-Y.; Wang, R.; Jia, C.-K.; Zhuang, L.; Shen, T.; Ding, L.-M.; Xu, Z.-D.; et al. Efficacy and safety of sirolimus early conversion protocol in liver transplant patients with hepatocellular carcinoma: A single-arm, multicenter, prospective study. Hepatobiliary Pancreat. Dis. Int. 2022, 21, 106–112. [Google Scholar] [CrossRef]
| Comparison Catalogue | RCT | RWS |
|---|---|---|
| Research environment | Ideal experimental conditions | Real clinical environment |
| Research and design | Randomized controlled trial | Observational study |
| Research object | Strict screening | Unrestricted condition |
| Number of samples | Usually small | Usually larger |
| Intervention measures | Strict intervention | No intervention |
| Compliance | Poor | Good |
| Interfering factors | Less | More |
| Cost input and extrapolation | Large cost input and poor extrapolation | Low cost input and good extrapolation |
| Disease | Drug | Sample Size/Example | Research Type | Year | References |
|---|---|---|---|---|---|
| BC | Fulvestrant | 303 | Treatment | 2020 | [11] |
| Palbociclib | 2445 | Treatment | 2021 | [12] | |
| Lapatinib | 92 | Treatment | 2020 | [21] | |
| Lapatinib | 112 | Treatment | 2020 | [22] | |
| T-DM1 | 15 | Treatment | 2019 | [23] | |
| Pyrotinib | 94 | Treatment | 2021 | [24] | |
| Pyrotinib | 141 | Treatment | 2021 | [25] | |
| Pyrotinib | 105 | Treatment | 2021 | [26] | |
| Pyrotinib | 168 | Treatment | 2021 | [27] | |
| Pyrotinib | 218 | Treatment | 2021 | [29] | |
| PLD | 1213 | Treatment | 2021 | [32] | |
| Trastuzumab | 3733 | Treatment | 2019 | [33] | |
| Pertuzumab | 217 | Prognosis | 2021 | [41] | |
| HCC | Sorafenib | 115 | Treatment | 2020 | [48] |
| Sorafenib | 6156 | Treatment | 2020 | [49] | |
| lenvatinib | 98 | Treatment | 2020 | [51] | |
| lenvatinib | 54 | Treatment | 2020 | [52] | |
| lenvatinib | 92 | Treatment | 2020 | [53] | |
| Sorafenib | 13 | Treatment | 2020 | [55] | |
| Regorafenib | 86 | Treatment | 2022 | [57] | |
| Regorafenib | 38 | Treatment | 2021 | [58] | |
| Ramucirumab | 16 | Prognosis | 2021 | [65] | |
| CRC | Bevacizumab | 402 | Treatment | 2020 | [68] |
| S-1 | 1367 | Treatment | 2020 | [70] | |
| Cetuximab | 177 | Treatment | 2021 | [71] | |
| Cetuximab | 2943 | Treatment | 2020 | [72] | |
| FTD/TPI | 105 | Treatment | 2020 | [73] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, L.; Li, H.; Wang, T.; Wang, R.; Cheng, L.; Wang, G. Real-World Study: A Powerful Tool for Malignant Tumor Research in General Surgery. Cancers 2022, 14, 5408. https://doi.org/10.3390/cancers14215408
Zhang L, Li H, Wang T, Wang R, Cheng L, Wang G. Real-World Study: A Powerful Tool for Malignant Tumor Research in General Surgery. Cancers. 2022; 14(21):5408. https://doi.org/10.3390/cancers14215408
Chicago/Turabian StyleZhang, Liang, He Li, TianFu Wang, RuiXin Wang, Long Cheng, and Gang Wang. 2022. "Real-World Study: A Powerful Tool for Malignant Tumor Research in General Surgery" Cancers 14, no. 21: 5408. https://doi.org/10.3390/cancers14215408
APA StyleZhang, L., Li, H., Wang, T., Wang, R., Cheng, L., & Wang, G. (2022). Real-World Study: A Powerful Tool for Malignant Tumor Research in General Surgery. Cancers, 14(21), 5408. https://doi.org/10.3390/cancers14215408






