Treatment of Malignant Adnexal Tumors of the Skin: A 12-Year Perspective
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
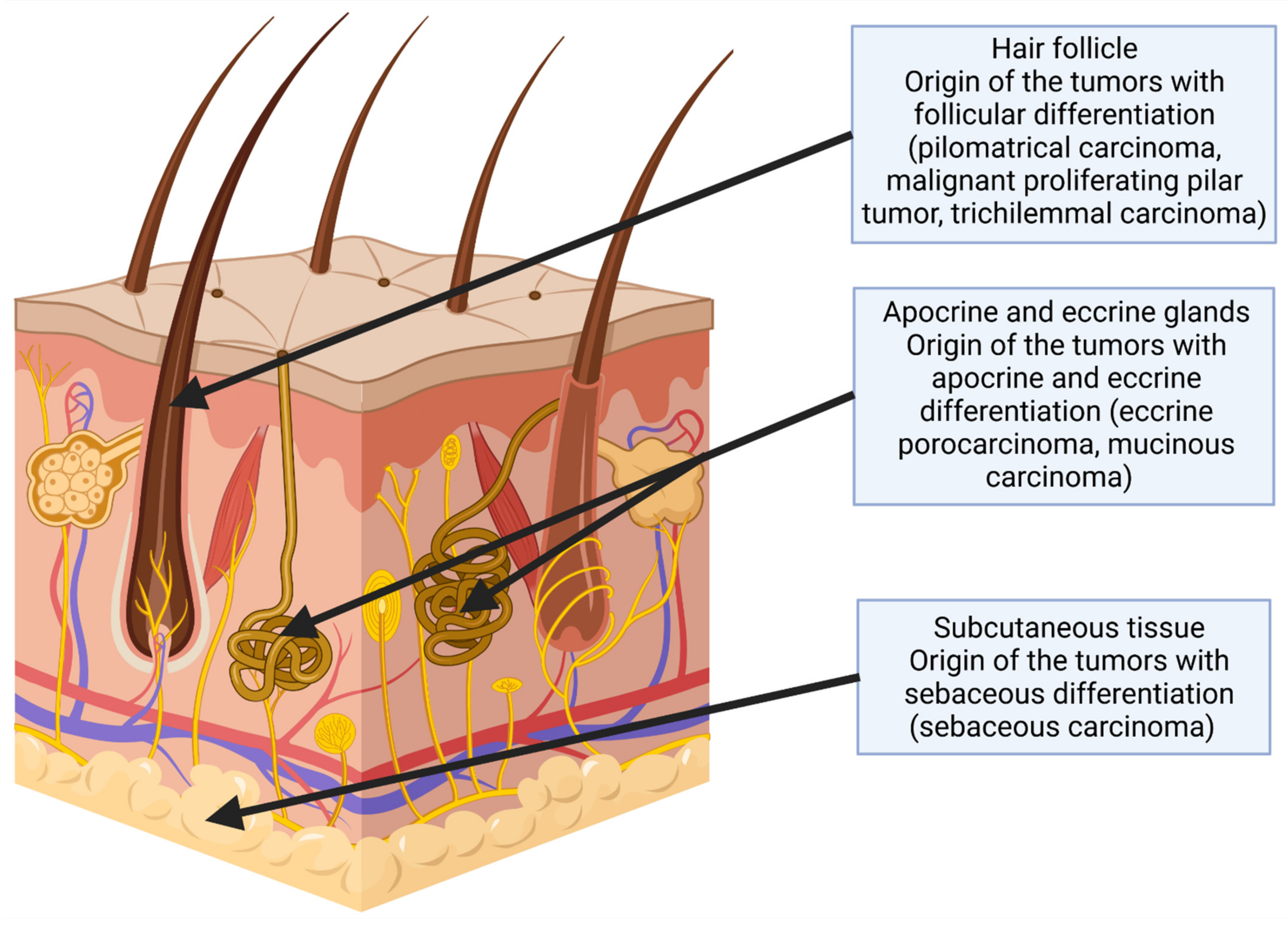
3.1. Tumors with Follicular Differentiation
3.1.1. Trichilemmal Carcinoma
3.1.2. Pilomatrix Carcinoma
3.1.3. Malignant Proliferating Pilar Tumor
3.2. Tumors with Sebaceous Differentiation
3.2.1. Sebaceous Carcinoma
First Case
Second Case
Third Case
Fourth Case
3.3. Tumors with Apocrine and Eccrine Differentiation
3.3.1. Eccrine Porocarcinoma
3.3.2. Mucinous Carcinoma
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stam, H.; Lohuis, P.J.; Zupan-Kajcovski, B.; Wouters, M.W.; van der Hage, J.A.; Visser, O. Increasing incidence and survival of a rare skin cancer in the Netherlands. A population-based study of 2220 cases of skin adnexal carcinoma. J. Surg. Oncol. 2013, 107, 822–827. [Google Scholar] [CrossRef] [PubMed]
- Mallone, S.; De Vries, E.; Guzzo, M.; Midena, E.; Verne, J.; Coebergh, J.W.; Marcos-Gragera, R.; Ardanaz, E.; Martinez, R.; Chirlaque, M.D.; et al. Descriptive epidemiology of malignant mucosal and uveal melanomas and adnexal skin carcinomas in Europe. Eur. J. Cancer 2012, 48, 1167–1175. [Google Scholar] [CrossRef] [PubMed]
- Busco, S.; Buzzoni, C.; Mallone, S.; Trama, A.; Castaing, M.; Bella, F.; Amodio, R.; Bizzoco, S.; Cassetti, T.; Cirilli, C.; et al. Italian cancer figures—Report 2015: The burden of rare cancers in Italy. Epidemiol. Prev. 2016, 40 (Suppl 2), 1–120. [Google Scholar] [PubMed]
- Płachta, I.; Kleibert, M.; Czarnecka, A.M.; Spałek, M.; Szumera-Ciećkiewicz, A.; Rutkowski, P. Current Diagnosis and Treatment Options for Cutaneous Adnexal Neoplasms with Follicular Differentiation. Int. J. Mol. Sci. 2021, 22, 4759. [Google Scholar] [CrossRef]
- Płachta, I.; Kleibert, M.; Czarnecka, A.M.; Spałek, M.; Szumera-Ciećkiewicz, A.; Rutkowski, P. Current Diagnosis and Treatment Options for Cutaneous Adnexal Neoplasms with Apocrine and Eccrine Differentiation. Int. J. Mol. Sci. 2021, 22, 5077. [Google Scholar] [CrossRef]
- Ogata, D.; Kiyohara, Y.; Yoshikawa, S.; Kasami, M. Treatment strategy for cutaneous apocrine carcinoma. Int. J. Clin. Oncol. 2014, 19, 712–715. [Google Scholar] [CrossRef]
- Ha, J.H.; Lee, C.; Lee, K.S.; Pak, C.-s.; Sun, C.-H.; Koh, Y.; Chang, H. The molecular pathogenesis of Trichilemmal carcinoma. BMC Cancer 2020, 20, 516. [Google Scholar] [CrossRef]
- Sassmannshausen, J.; Chaffins, M. Pilomatrix carcinoma: A report of a case arising from a previously excised pilomatrixoma and a review of the literature. J. Am. Acad. Dermatol. 2001, 44, 358–361. [Google Scholar] [CrossRef]
- Sawaya, J.L.; Khachemoune, A. Poroma: A review of eccrine, apocrine, and malignant forms. Int. J. Dermatol. 2014, 53, 1053–1061. [Google Scholar] [CrossRef]
- De Iuliis, F.; Amoroso, L.; Taglieri, L.; Vendittozzi, S.; Blasi, L.; Salerno, G.; Lanza, R.; Scarpa, S. Chemotherapy of rare skin adnexal tumors: A review of literature. Anticancer Res. 2014, 34, 5263–5268. [Google Scholar]
- Jones, C.; Twoon, M.; Ho, W.; Portelli, M.; Robertson, B.F.; Anderson, W. Pilomatrix carcinoma: 12-year experience and review of the literature. J. Cutan. Pathol. 2018, 45, 33–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Owen, J.L.; Kibbi, N.; Worley, B.; Kelm, R.C.; Wang, J.V.; Barker, C.A.; Behshad, R.; Bichakjian, C.K.; Bolotin, D.; Bordeaux, J.S.; et al. Sebaceous carcinoma: Evidence-based clinical practice guidelines. Lancet Oncol. 2019, 20, e699–e714. [Google Scholar] [CrossRef]
- O’Hare, A.M.; Cooper, P.H.; Parlette, H.L. Trichilemmomal carcinoma in a patient with Cowden’s disease (multiple hamartoma syndrome). J. Am. Acad. Dermatol. 1997, 36, 1021–1023. [Google Scholar] [CrossRef]
- Hamman, M.S.; Brian Jiang, S.I. Management of trichilemmal carcinoma: An update and comprehensive review of the literature. Dermatol. Surg. 2014, 40, 711–717. [Google Scholar]
- Kamil, Z.S.; Sachdeva, M.; Kwapis, J.; Ghazarian, D. Early Pilomatrix Carcinoma: A Case Report With Emphasis on Molecular Pathology and Review of the Literature. Cutis 2021, 108, E24–E28. [Google Scholar] [CrossRef]
- Rao, S.; Ramakrishnan, R.; Kamakshi, D.; Chakravarthi, S.; Sundaram, S.; Prathiba, D. Malignant proliferating trichilemmal tumour presenting early in life: An uncommon feature. J. Cutan. Aesthetic Surg. 2011, 4, 51–55. [Google Scholar] [CrossRef]
- Imko-Walczuk, B.; Krys, A.; Lizakowski, S.; Debska-Slizien, A.; Rutkowski, B.; Biernat, W.; Wojnarowska, F. Sebaceous carcinoma in patients receiving long-term immunosuppresive treatment: Case report and literature review. Transplant. Proc. 2014, 46, 2903–2907. [Google Scholar] [CrossRef]
- Shalin, S.C.; Lyle, S.; Calonje, E.; Lazar, A.J. Sebaceous neoplasia and the Muir-Torre syndrome: Important connections with clinical implications. Histopathology 2010, 56, 133–147. [Google Scholar] [CrossRef] [Green Version]
- Sargen, M.R.; Mai, Z.M.; Engels, E.A.; Goldstein, A.M.; Tucker, M.A.; Pfeiffer, R.M.; Cahoon, E.K. Ambient Ultraviolet Radiation and Sebaceous Carcinoma Incidence in the United States, 2000–2016. JNCI Cancer Spectr. 2020, 4, pkaa020. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, M.A.; Arslan, D.; Tatlı, A.M.; Uysal, M. Eccrine porocarcinoma: A case report and literature review. J. Clin. Exp. Investig. 2013, 4. [Google Scholar] [CrossRef]
- Chavez, A.; Linos, K.; Samie, F.H. Primary cutaneous mucinous carcinoma of the eyelid treated with Mohs surgery. JAAD Case Rep. 2015, 1, 85–87. [Google Scholar] [CrossRef]
- Blake, P.W.; Bradford, P.T.; Devesa, S.S.; Toro, J.R. Cutaneous appendageal carcinoma incidence and survival patterns in the United States: A population-based study. Arch. Dermatol. 2010, 146, 625–632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robson, A.; Greene, J.; Ansari, N.; Kim, B.; Seed, P.T.; McKee, P.H.; Calonje, E. Eccrine porocarcinoma (malignant eccrine poroma): A clinicopathologic study of 69 cases. Am. J. Surg. Pathol. 2001, 25, 710–720. [Google Scholar] [CrossRef] [PubMed]
- Harari, P.M.; Shimm, D.S.; Bangert, J.L.; Cassady, J.R. The role of radiotherapy in the treatment of malignant sweat gland neoplasms. Cancer 1990, 65, 1737–1740. [Google Scholar] [CrossRef]
- Brown, Z.; Riesco-Martinez, M.; Petrella, T. Treatment of primary cutaneous apocrine carcinoma of the scalp—Case and review of the literature. Glob. Dermatol. 2016, 3, 356–360. [Google Scholar] [CrossRef]
- Chamberlain, R.S.; Huber, K.; White, J.C.; Travaglino-Parda, R. Apocrine gland carcinoma of the axilla: Review of the literature and recommendations for treatment. Am. J. Clin. Oncol. 1999, 22, 131–135. [Google Scholar] [CrossRef]
- Sau, P.; Lupton, G.P.; Graham, J.H. Pilomatrix carcinoma. Cancer 1993, 71, 2491–2498. [Google Scholar] [CrossRef]
- Gould, E.; Kurzon, R.; Kowalczyk, A.P.; Saldana, M. Pilomatrix carcinoma with pulmonary metastasis. Report of a case. Cancer 1984, 54, 370–372. [Google Scholar] [CrossRef]
- Waqas, O.; Faisal, M.; Haider, I.; Amjad, A.; Jamshed, A.; Hussain, R. Retrospective study of rare cutaneous malignant adnexal tumors of the head and neck in a tertiary care cancer hospital: A case series. J. Med. Case Rep. 2017, 11, 67. [Google Scholar] [CrossRef] [Green Version]
- Gallant, J.-N.; Sewell, A.; Almodovar, K.; Wang, Q.; Dahlman, K.B.; Abramson, R.G.; Kapp, M.E.; Brown, B.T.; Boyd, K.L.; Gilbert, J.; et al. Genomic landscape of a metastatic malignant proliferating tricholemmal tumor and its response to PI3K inhibition. NPJ Precis. Oncol. 2019, 3, 5. [Google Scholar] [CrossRef]
- Ye, J.; Nappi, O.; Swanson, P.E.; Patterson, J.W.; Wick, M.R. Proliferating Pilar Tumors. Am. J. Clin. Pathol. 2004, 122, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Siddha, M.; Budrukkar, A.; Shet, T.; Deshpande, M.; Basu, A.; Patil, N.; Bhalavat, R. Malignant pilar tumor of the scalp: A case report and review of literature. J. Cancer Res. Ther. 2007, 3, 240–243. [Google Scholar] [PubMed]
- Zhuang, S.M.; Zhang, G.H.; Chen, W.K.; Chen, S.W.; Wang, L.P.; Li, H.; Song, M. Survival study and clinicopathological evaluation of trichilemmal carcinoma. Mol. Clin. Oncol. 2013, 1, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.; Zhu, H.G.; Wang, L.Z.; Zheng, J.W.; Chen, W.T.; Zhang, Z.; Dong, W.; Qu, W.; Wang, Y.A. Tricholemmal carcinoma of the head and neck region: A report of 15 cases. Oncol. Lett. 2014, 7, 423–426. [Google Scholar] [CrossRef] [Green Version]
- Topkan, E. Adjuvant radiotherapy in management of trichilemmal carcinoma of left nasal alae with positive surgical margins: A case report. Case Rep. Clin. Pathol. 2016, 3, 57–60. [Google Scholar] [CrossRef] [Green Version]
- Salih, A.M.; Kakamad, F.H.; Baba, H.O.; Salih, R.Q.; Hawbash, M.R.; Mohammed, S.H.; Othman, S.; Saeed, Y.A.; Habibullah, I.J.; Muhialdeen, A.S.; et al. Porocarcinoma; presentation and management, a meta-analysis of 453 cases. Ann. Med. Surg. 2017, 20, 74–79. [Google Scholar] [CrossRef]
- Kamalpour, L.; Brindise, R.T.; Nodzenski, M.; Bach, D.Q.; Veledar, E.; Alam, M. Primary cutaneous mucinous carcinoma: A systematic review and meta-analysis of outcomes after surgery. JAMA Dermatol. 2014, 150, 380–384. [Google Scholar] [CrossRef] [Green Version]
- Le, N.S.; Janik, S.; Liu, D.T.; Grasl, S.; Faisal, M.; Pammer, J.; Schickinger-Fischer, B.; Hamzavi, J.S.; Seemann, R.; Erovic, B.M. Eccrine porocarcinoma of the head and neck: Meta-analysis of 120 cases. Head Neck 2020, 42, 2644–2659. [Google Scholar] [CrossRef]
- Sokolenko, A.P.; Imyanitov, E.N. Molecular Diagnostics in Clinical Oncology. Front. Mol. Biosci. 2018, 5, 76. [Google Scholar] [CrossRef]
- Kazakov, D.V. Brooke-Spiegler Syndrome and Phenotypic Variants: An Update. Head Neck Pathol. 2016, 10, 125–130. [Google Scholar] [CrossRef]
- Pilarski, R.; Burt, R.; Kohlman, W.; Pho, L.; Shannon, K.M.; Swisher, E. Cowden syndrome and the PTEN hamartoma tumor syndrome: Systematic review and revised diagnostic criteria. J. Natl. Cancer Inst. 2013, 105, 1607–1616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- John, A.M.; Schwartz, R.A. Muir-Torre syndrome (MTS): An update and approach to diagnosis and management. J. Am. Acad. Dermatol. 2016, 74, 558–566. [Google Scholar] [CrossRef]
- Roberts, M.E.; Riegert-Johnson, D.L.; Thomas, B.C.; Rumilla, K.M.; Thomas, C.S.; Heckman, M.G.; Purcell, J.U.; Hanson, N.B.; Leppig, K.A.; Lim, J.; et al. A clinical scoring system to identify patients with sebaceous neoplasms at risk for the Muir-Torre variant of Lynch syndrome. Genet. Med. 2014, 16, 711–716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denisova, E.; Westphal, D.; Surowy, H.M.; Meier, F.; Hutter, B.; Reifenberger, J.; Rutten, A.; Schulz, A.; Sergon, M.; Ziemer, M.; et al. Whole-exome sequencing in eccrine porocarcinoma indicates promising therapeutic strategies. Cancer Gene Ther. 2021. [Google Scholar] [CrossRef] [PubMed]
- Ivan, D.; Prieto, V.G.; Esmaeli, B.; Wistuba, I.I.; Tang, X.; Lazar, A.J. Epidermal growth factor receptor (EGFR) expression in periocular and extraocular sebaceous carcinoma. J. Cutan. Pathol. 2010, 37, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Xu, Y. Unusual presentation of metastatic sebaceous carcinoma and its response to chemotherapy: Is genotyping a right answer for guiding chemotherapy in rare tumours? Curr. Oncol. 2015, 22, e316–e319. [Google Scholar] [CrossRef] [Green Version]
- Tetzlaff, M.T.; Singh, R.R.; Seviour, E.G.; Curry, J.L.; Hudgens, C.W.; Bell, D.; Wimmer, D.A.; Ning, J.; Czerniak, B.A.; Zhang, L.; et al. Next-generation sequencing identifies high frequency of mutations in potentially clinically actionable genes in sebaceous carcinoma. J. Pathol. 2016, 240, 84–95. [Google Scholar] [CrossRef]
- Domingo-Musibay, E.; Murugan, P.; Giubellino, A.; Sharma, S.; Steinberger, D.; Yuan, J.; Hunt, M.A.; Lou, E.; Miller, J.S. Near complete response to Pembrolizumab in microsatellite-stable metastatic sebaceous carcinoma. J. Immunother. Cancer 2018, 6, 58. [Google Scholar] [CrossRef]
- Kodali, S.; Tipirneni, E.; Gibson, P.C.; Cook, D.; Verschraegen, C.; Lane, K.A. Carboplatin and Pembrolizumab Chemoimmunotherapy Achieves Remission in Recurrent, Metastatic Sebaceous Carcinoma. Ophthalmic Plast. Reconstr. Surg. 2018, 34, e149–e151. [Google Scholar] [CrossRef]
- Lin, A.C.; Shriver, E.M. The Role of Pembrolizumab in the Treatment of Sebaceous Carcinoma. Int. Ophthalmol. Clin. 2020, 60, 39–46. [Google Scholar] [CrossRef]
- Lee, S.H.; Jung, Y.H.; Yoo, J.Y.; Park, H.J. A Case Report of Recurrent Metastatic Sebaceous Carcinoma Which Showed Favorable Response Tt Non-Fluorouracil Based Chemotherapy. Am. J. Case Rep. 2018, 19, 1192–1196. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.A.; Cioni, M.; Robson, A.; Bataille, V. Metastatic porocarcinoma achieving complete radiological and clinical response with pembrolizumab. BMJ Case Rep. 2019, 12, e228917. [Google Scholar] [CrossRef] [PubMed]
- Nash, J.W.; Barrett, T.L.; Kies, M.; Ross, M.I.; Sneige, N.; Diwan, A.H.; Lazar, A.J. Metastatic hidradenocarcinoma with demonstration of Her-2/neu gene amplification by fluorescence in situ hybridization: Potential treatment implications. J. Cutan. Pathol. 2007, 34, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Gauerke, S.; Driscoll, J.J. Hidradenocarcinomas: A brief review and future directions. Arch. Pathol. Lab. Med. 2010, 134, 781–785. [Google Scholar] [CrossRef]
- Hidaka, T.; Fujimura, T.; Watabe, A.; Hashimoto, A.; Haga, T.; Onami, K.; Mizuashi, M.; Aiba, S. Successful treatment of HER-2-positive metastatic apocrine carcinoma of the skin with lapatinib and capecitabine. Acta Derm. Venereol. 2012, 92, 654–655. [Google Scholar] [CrossRef]
- Portelli, F.; Salvati, L.; Projetto, E.; Gori, A.; Scarfì, F.; Trane, L.; Lo Russo, G.; Innocenti, A.; De Giorgi, V. A clinical, pathological and immunohistochemical series of 9 cases of primary cutaneous apocrine carcinomas of the head and neck. Australas. J. Dermatol. 2020, 61, e189–e195. [Google Scholar] [CrossRef]
- Requena, L.; Prieto, V.G.; Requena, C.; Sarasa, J.L.; Manzano, R.; Seco, M.; Rütten, A.; Kazakov, D.V.; Cerroni, L.; Kutzner, H. Primary signet-ring cell/histiocytoid carcinoma of the eyelid: A clinicopathologic study of 5 cases and review of the literature. Am. J. Surg. Pathol. 2011, 35, 378–391. [Google Scholar] [CrossRef]
- Philips, R.; Langston, L.; Hwang, H.; Vandergriff, T.; Trynosky, T.; Berlingeri-Ramos, A.C. Primary cutaneous histiocytoid carcinoma with distant metastasis. J. Cutan. Pathol. 2017, 44, 376–380. [Google Scholar] [CrossRef]
- Sakamoto, K.; Ito, T.; Tanioka, F.; Fukamizu, H.; Tokura, Y. Primary signet-ring cell/histiocytoid carcinoma of the eyelid expressing androgen receptors and treated with bicalutamide. J. Dermatol. 2017, 44, e230–e231. [Google Scholar] [CrossRef]
- Libertini, M.; Oneda, E.; Di Biasi, B.; Savelli, G.; Zaniboni, A. Cutaneous Adnexal Carcinoma with Apocrine Differentiation: A Challenging Diagnosis and Personalized Treatment with mTOR Inhibitor in a Very Rare Disease. Case Rep. Oncol. 2020, 13, 1091–1096. [Google Scholar] [CrossRef]
- Lepesant, P.; Crinquette, M.; Alkeraye, S.; Mirabel, X.; Dziwniel, V.; Cribier, B.; Mortier, L. Vismodegib induces significant clinical response in locally advanced trichoblastic carcinoma. Br. J. Dermatol. 2015, 173, 1059–1062. [Google Scholar] [CrossRef] [PubMed]
- Battistella, M.; Mateus, C.; Lassau, N.; Chami, L.; Boukoucha, M.; Duvillard, P.; Cribier, B.; Robert, C. Sunitinib efficacy in the treatment of metastatic skin adnexal carcinomas: Report of two patients with hidradenocarcinoma and trichoblastic carcinoma. J. Eur. Acad. Dermatol. Venereol. 2010, 24, 199–203. [Google Scholar] [CrossRef] [PubMed]



| Time after the Surgery (Months) | Follow-Up |
|---|---|
| 6 | US of the cervical lymph nodes |
| 12 | Chest X-ray, head and neck CT, CBC, thyroid hormone levels |
| 18 | Chest X-ray, US of cervical lymph nodes |
| 24 | Clinical evaluation |
| 30 | Chest X-ray, head and neck CT |
| 36 | Abdomen US |
| 42 | Chest X-ray, US of cervical lymph nodes |
| 48 | Clinical evaluation |
| 54 | Chest X-ray |
| 60 | Head, neck, and abdomen CT |
| Time after the surgery (months) | Follow-up |
| Tumor | Syndromes/Conditions that Potentially Increase the Risk | References |
|---|---|---|
| Trichilemmal carcinoma | UV and radiation exposure, pre-existing scars, Cowden syndrome, and immunosuppression | [13,14] |
| Pilomatrix carcinoma | UV exposure | [15] |
| Malignant proliferating pilar tumor | UV exposure | [16] |
| Sebaceous carcinoma | Muir–Torre syndrome, UV exposure, and immunosuppression | [17,18,19] |
| Eccrine porocarcinoma | Trauma, burning, radiotherapy, and immunosuppression, UV exposure, and AIDS | [20] |
| Mucinous carcinoma | UV and radiation exposure | [21] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kleibert, M.; Płachta, I.; Czarnecka, A.M.; Spałek, M.J.; Szumera-Ciećkiewicz, A.; Rutkowski, P. Treatment of Malignant Adnexal Tumors of the Skin: A 12-Year Perspective. Cancers 2022, 14, 998. https://doi.org/10.3390/cancers14040998
Kleibert M, Płachta I, Czarnecka AM, Spałek MJ, Szumera-Ciećkiewicz A, Rutkowski P. Treatment of Malignant Adnexal Tumors of the Skin: A 12-Year Perspective. Cancers. 2022; 14(4):998. https://doi.org/10.3390/cancers14040998
Chicago/Turabian StyleKleibert, Marcin, Iga Płachta, Anna M. Czarnecka, Mateusz J. Spałek, Anna Szumera-Ciećkiewicz, and Piotr Rutkowski. 2022. "Treatment of Malignant Adnexal Tumors of the Skin: A 12-Year Perspective" Cancers 14, no. 4: 998. https://doi.org/10.3390/cancers14040998
APA StyleKleibert, M., Płachta, I., Czarnecka, A. M., Spałek, M. J., Szumera-Ciećkiewicz, A., & Rutkowski, P. (2022). Treatment of Malignant Adnexal Tumors of the Skin: A 12-Year Perspective. Cancers, 14(4), 998. https://doi.org/10.3390/cancers14040998









