Radiotherapy for HER 2 Positive Brain Metastases: Urgent Need for a Paradigm Shift
Abstract
:Simple Summary
Abstract
1. Introduction
2. Brain Radiotherapy: Lessons from the Past and Novel Treatments
2.1. WBRT
2.2. SRS and Fractionated Stereotactic Radiotherapy (fSRT)
3. Combination of Brain RT with Systemic Therapy in the Treatment of BCBMs
3.1. Brain RT + Trastuzumab
3.2. Brain RT + Trastuzumab–Pertuzumab
| Authors | Study | Year | Population | Treatment | Outcome | Adverse Effects |
|---|---|---|---|---|---|---|
| Chargari et al. [42] | Retrospective | 2011 | - 31 patients |
| OR: 74.2% Clinical Response: 87.1% | RN / OTHER Related to WBRT: Grade 1 -Headache 8 (26%) -Nausea/vomiting 4 (13%) Related to trastuzumab Allergic-like reaction 2 (6.5%) Decrease in LVEF 3 (9.5%) |
| Miller et al. [43] | Retrospective | 2017 | - 187 patients (374 lesions) |
| OS Concurrent HER2 antibodies 17.9 months vs. local therapy alone 15.1 months (p = 0.04) | RN
|
| Ippolito E et al. [47] | Retrospective | 2021 | - 10 patients (32 lesions) |
| OR 68.7% iCB 100% DIF 4/10 patients (40.0%) Median OBMS 33.9 months (95%CI 24.1–43.6) Mean duration of PT treatment 27.9 months (range: 10.1–53.7 months) | RN
|
|
3.3. Brain RT + Lapatinib
3.4. Brain RT + TDM1
3.5. Limitations
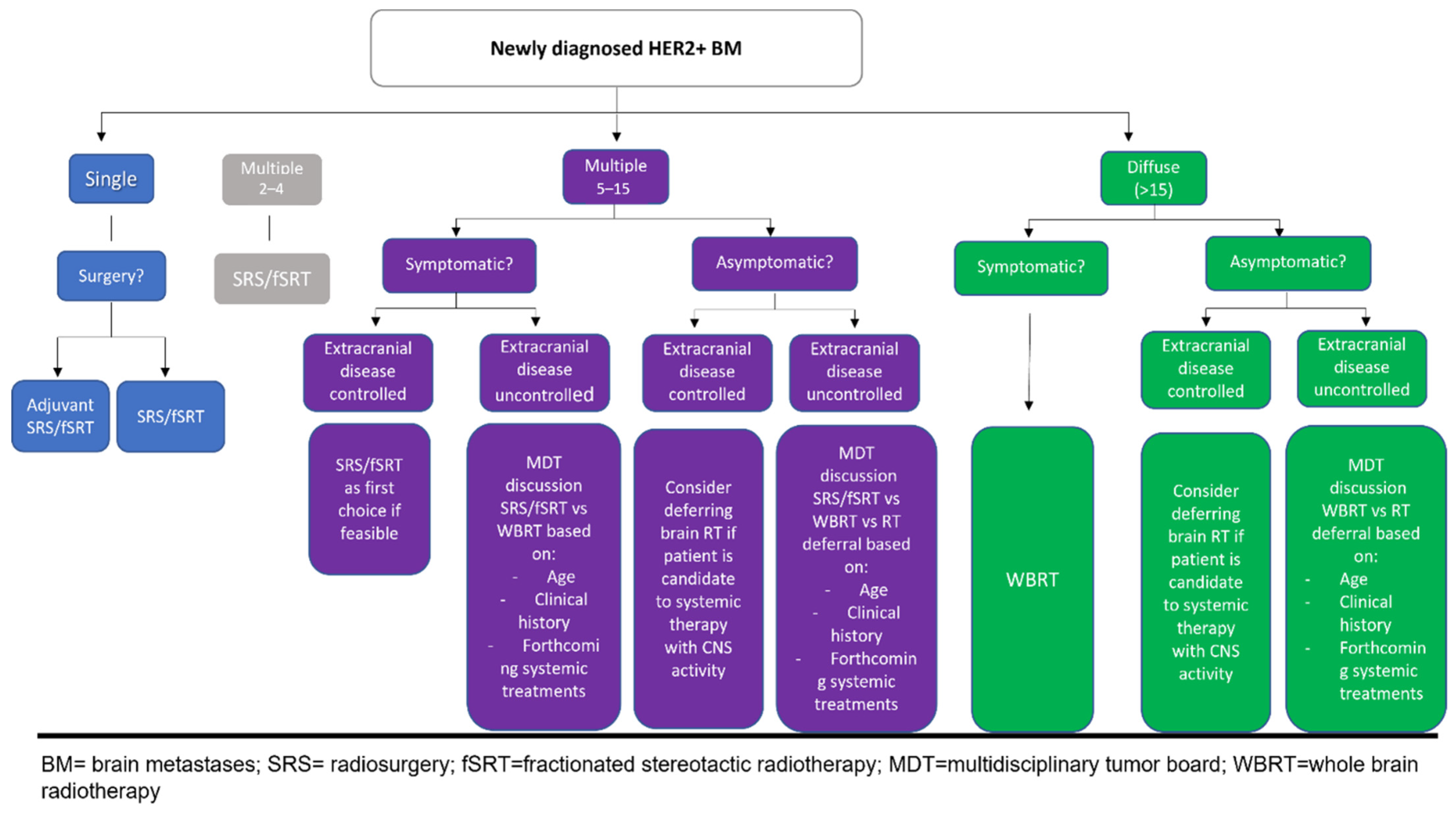
4. Future Developments: How the Therapeutic Algorithm Should Be Reshaped
4.1. When Should WBRT Be Delivered?
4.2. When Should SRS/fSRT Be Delivered?
4.3. When Can RT Deferral Be an Option?
4.4. How to Manage the Association of Systemic Therapy with Brain RT?
Author Contributions
Funding
Conflicts of Interest
References
- Sammons, S.; Van Swearingen, A.E.D.; Chung, C.; Anders, C.K. Advances in the management of breast cancer brain metastases. Neurooncol. Adv. 2021, 3 (Suppl. 5), v63–v74. [Google Scholar] [CrossRef] [PubMed]
- Yuan, P.; Gao, S.L. Management of breast cancer brain metastases: Focus on human epidermal growth factor receptor 2-positive breast cancer. Chronic Dis. Transl. Med. 2017, 3, 21–32. [Google Scholar] [CrossRef]
- Clayton, A.J.; Danson, S.; Jolly, S.; Ryder, W.D.; Burt, P.A.; Stewart, A.L.; Wilkinson, P.M.; Welch, R.S.; Magee, B.; Wilson, G.; et al. Incidence of cerebral metastases in patients treated with trastuzumab for metastatic breast cancer. Br. J. Cancer 2004, 91, 639–643. [Google Scholar] [CrossRef]
- Bendell, J.C.; Domchek, S.M.; Burstein, H.J.; Harris, L.; Younger, J.; Kuter, I.; Bunnell, C.; Rue, M.; Gelman, R.; Winer, E. Central nervous system metastases in women who receive trastuzumab-based therapy for metastatic breast carcinoma. Cancer 2003, 97, 2972–2977. [Google Scholar] [CrossRef] [PubMed]
- Stemmler, H.J.; Kahlert, S.; Siekiera, W.; Untch, M.; Heinrich, B.; Heinemann, V. Characteristics of patients with brain metastases receiving trastuzumab for HER2 overexpressing metastatic breast cancer. Breast 2006, 15, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Patchell, R.A.; Tibbs, P.A.; Walsh, J.W.; Dempsey, R.J.; Maruyama, Y.; Kryscio, R.J.; Markesbery, W.R.; Macdonald, J.S.; Young, B. A randomized trial of surgery in the treatment of single metastases to the brain. N. Engl. J. Med. 1990, 322, 494–500. [Google Scholar] [CrossRef] [PubMed]
- Vecht, C.J.; Haaxma-Reiche, H.; Noordijk, E.M.; Padberg, G.W.; Voormolen, J.H.; Hoekstra, F.H.; Tans, J.T.; Lambooij, N.; Metsaars, J.A.; Wattendorff, A.R.; et al. Treatment of single brain metastasis: Radiotherapy alone or combined with neurosurgery? Ann. Neurol. 1993, 33, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Mintz, A.H.; Kestle, J.; Rathbone, M.P.; Gaspar, L.; Hugenholtz, H.; Fisher, B.; Duncan, G.; Skingley, P.; Foster, G.; Levine, M. A randomized trial to assess the efficacy of surgery in addition to radiotherapy in patients with a single cerebral metastasis. Cancer 1996, 78, 1470–1476. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Serizawa, T.; Shuto, T.; Akabane, A.; Higuchi, Y.; Kawagishi, J.; Yamanaka, K.; Sato, Y.; Jokura, H.; Yomo, S.; et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): A multi-institutional prospective observational study. Lancet Oncol. 2014, 15, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Serizawa, T.; Higuchi, Y.; Sato, Y.; Kawagishi, J.; Yamanaka, K.; Shuto, T.; Akabane, A.; Jokura, H.; Yomo, S.; et al. A Multi-institutional Prospective Observational Study of Stereotactic Radiosurgery for Patients With Multiple Brain Metastases (JLGK0901 Study Update): Irradiation-related Complications and Long-term Maintenance of Mini-Mental State Examination Scores. Int. J. Radiat. Oncol. Biol. Phys. 2017, 99, 31–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stavrou, E.; Winer, E.P.; Lin, N.U. How we treat HER2-positive brain metastases. ESMO Open 2021, 6, 100256. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, H.; Shirato, H.; Tago, M.; Nakagawa, K.; Toyoda, T.; Hatano, K.; Kenjyo, M.; Oya, N.; Hirota, S.; Shioura, H.; et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: A randomized controlled trial. JAMA 2006, 295, 2483–2491. [Google Scholar] [CrossRef] [PubMed]
- Kocher, M.; Soffietti, R.; Abacioglu, U.; Villà, S.; Fauchon, F.; Baumert, B.G.; Fariselli, L.; Tzuk-Shina, T.; Kortmann, R.D.; Carrie, C.; et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: Results of the EORTC 22952-26001 study. J. Clin. Oncol. 2011, 29, 134–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chougule, P.; Burton-Williams, M.; Saris, S.; Zheng, Z.; Ponte, B.; Noren, G.; Alderson, L.; Friehs, G.; Wazer, D.; Epstein, M. Randomized treatment of brain metastasis with gamma knife radiosurgery, whole brain radiotherapy or both. Int. J. Radiat. Oncol. Biol. Phys. 2000, 48, 114. [Google Scholar] [CrossRef]
- Casanova, N.; Mazouni, Z.; Bieri, S.; Combescure, C.; Pica, A.; Weber, D.C. Whole brain radiotherapy with a conformational external beam radiation boost for lung cancer patients with 1-3 brain metastasis: A multi institutional study. Radiat. Oncol. 2010, 5, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weber, D.C.; Caparrotti, F.; Laouiti, M.; Malek, K. Simultaneous in-field boost for patients with 1 to 4 brain metastasis/es treated with volumetric modulated arc therapy: A prospective study on quality-of-life. Radiat. Oncol. 2011, 6, 79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruzzaniti, V.; Abate, A.; Pedrini, M.; Benassi, M.; Strigari, L. IsoBED: A tool for automatic calculation of biologically equivalent fractionation schedules in radiotherapy using IMRT with a simultaneous integrated boost (SIB) technique. J. Exp. Clin. Cancer Res. 2011, 30, 52. [Google Scholar] [CrossRef] [Green Version]
- Lin, B.; Huang, D.; Du, H.; Fan, J.; Zhang, Y.; Feng, G.; Gao, F.; Du, X.B. Whole-Brain Radiation Therapy With Simultaneous Integrated Boost Versus Whole-Brain Radiation Therapy Plus Stereotactic Radiosurgery for the Treatment of Brain Metastasis From Lung Cancer. Front. Oncol. 2021, 11, 631422. [Google Scholar] [CrossRef]
- Roman, D.D.; Sperduto, P.W. Neuropsychological effects of cranial radiation: Current knowledge and future directions. Int. J. Radiat. Oncol. Biol. Phys. 1995, 31, 983–998. [Google Scholar] [CrossRef] [PubMed]
- Soffietti, R.; Kocher, M.; Abacioglu, U.M.; Villa, S.; Fauchon, F.; Baumert, B.G.; Fariselli, L.; Tzuk-Shina, T.; Kortmann, R.D.; Carrie, C.; et al. A European Organisation for Research and Treatment of Cancer phase III trial of adjuvant whole-brain radiotherapy versus observation in patients with one to three brain metastases from solid tumors after surgical resection or radiosurgery: Quality-of-life results. J. Clin. Oncol. 2013, 31, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.L.; Wefel, J.S.; Hess, K.R.; Allen, P.K.; Lang, F.F.; Kornguth, D.G.; Arbuckle, R.B.; Swint, J.M.; Shiu, A.S.; Maor, M.H.; et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: A randomised controlled trial. Lancet Oncol. 2009, 10, 1037–1044. [Google Scholar] [CrossRef] [PubMed]
- Greene-Schloesser, D.; Moore, E.; Robbins, M.E. Molecular pathways: Radiation-induced cognitive impairment. Clin. Cancer Res. 2013, 19, 2294–2300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gondi, V.; Tomé, W.A.; Mehta, M.P. Why avoid the hippocampus? A comprehensive review. Radiother. Oncol. 2010, 97, 370–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, B.; Huang, Z.; Wu, S.; Shen, G.; Cha, L.; Meng, X.; Ding, L.; Wang, J.; Song, S. Incidence and relapse risk of intracranial metastases within the perihippocampal region in 314 patients with breast cancer. Radiother. Oncol. 2016, 118, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Gondi, V.; Pugh, S.L.; Tome, W.A.; Caine, C.; Corn, B.; Kanner, A.; Rowley, H.; Kundapur, V.; DeNittis, A.; Greenspoon, J.N.; et al. Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): A phase II multi-institutional trial. J. Clin. Oncol. 2014, 32, 3810–3816. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.D.; Gondi, V.; Pugh, S.; Tome, W.A.; Wefel, J.S.; Armstrong, T.S.; Bovi, J.A.; Robinson, C.; Konski, A.; Khuntia, D.; et al. Hippocampal Avoidance During Whole-Brain Radiotherapy Plus Memantine for Patients With Brain Metastases: Phase III Trial NRG Oncology CC001. J. Clin. Oncol. 2020, 38, 1019–1029. [Google Scholar] [CrossRef]
- Yang, W.C.; Chen, Y.F.; Yang, C.C.; Wu, P.F.; Chan, H.M.; Chen, J.L.; Chen, G.Y.; Cheng, J.C.; Kuo, S.H.; Hsu, F.M. Hippocampal avoidance whole-brain radiotherapy without memantine in preserving neurocognitive function for brain metastases: A phase II blinded randomized trial. Neuro Oncol. 2021, 23, 478–486, Erratum in Neuro Oncol. 2021, 23, 2125. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.D.; Pugh, S.; Laack, N.N.; Wefel, J.S.; Khuntia, D.; Meyers, C.; Choucair, A.; Fox, S.; Suh, J.H.; Roberge, D.; et al. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: A randomized, double-blind, placebo-controlled trial. Neuro Oncol. 2013, 15, 1429–1437. [Google Scholar] [CrossRef]
- Gutiérrez, A.N.; Westerly, D.C.; Tomé, W.A.; Jaradat, H.A.; Mackie, T.R.; Bentzen, S.M.; Khuntia, D.; Mehta, M.P. Whole brain radiotherapy with hippocampal avoidance and simultaneously integrated brain metastases boost: A planning study. Int. J. Radiat. Oncol. Biol. Phys. 2007, 69, 589–597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Westover, K.D.; Mendel, J.T.; Dan, T.; Kumar, K.; Gao, A.; Pulipparacharuv, S.; Iyengar, P.; Nedzi, L.; Hannan, R.; Anderson, J.; et al. Phase II trial of hippocampal-sparing whole brain irradiation with simultaneous integrated boost for metastatic cancer. Neuro Oncol. 2020, 22, 1831–1839. [Google Scholar] [CrossRef] [PubMed]
- Hall, E.J.; Brenner, D.J. The radiobiology of radiosurgery: Rationale for different treatment regimes for AVMs and malignancies. Int. J. Radiat. Oncol. Biol. Phys. 1993, 25, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Lupattelli, M.; Alì, E.; Ingrosso, G.; Saldi, S.; Fulcheri, C.; Borghesi, S.; Tarducci, R.; Aristei, C. Stereotactic Radiotherapy for Brain Metastases: Imaging Tools and Dosimetric Predictive Factors for Radionecrosis. J. Pers. Med. 2020, 10, 59. [Google Scholar] [CrossRef]
- Shaw, E.; Scott, C.; Souhami, L.; Dinapoli, R.; Kline, R.; Loeffler, J.; Farnan, N. Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: Final report of RTOG protocol 90-05. Int. J. Radiat. Oncol. Biol. Phys. 2000, 47, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Clark, G.M.; Popple, R.A.; Young, P.E.; Fiveash, J.B. Feasibility of single-isocenter volumetric modulated arc radiosurgery for treatment of multiple brain metastases. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.; Ford, E.C.; Smith, K.; Wong, J.; McNutt, T.R. A method for optimizing LINAC treatment geometry for volumetric modulated arc therapy of multiple brain metastases. Med. Phys. 2010, 37, 4146–4154. [Google Scholar] [CrossRef] [PubMed]
- Guckenberger, M.; Roesch, J.; Baier, K.; Sweeney, R.A.; Flentje, M. Dosimetric consequences of translational and rotational errors in frame-less image-guided radiosurgery. Radiat. Oncol. 2012, 7, 63. [Google Scholar] [CrossRef] [Green Version]
- Liang, K.; Lu, Y.; Jin, W.; Ang, K.K.; Milas, L.; Fan, Z. Sensitization of breast cancer cells to radiation by trastuzumab. Mol. Cancer Ther. 2003, 2, 1113–1120. [Google Scholar] [PubMed]
- Park, Y.H.; Park, M.J.; Ji, S.H.; Yi, S.Y.; Lim, D.H.; Nam, D.H.; Lee, J.I.; Park, W.; Choi, D.H.; Huh, S.J.; et al. Trastuzumab treatment improves brain metastasis outcomes through control and durable prolongation of systemic extracranial disease in HER2-overexpressing breast cancer patients. Br. J. Cancer 2009, 24, 100, 894–900. [Google Scholar] [CrossRef] [PubMed]
- Kurihara, H.; Hamada, A.; Yoshida, M.; Shimma, S.; Hashimoto, J.; Yonemori, K.; Tani, H.; Miyakita, Y.; Kanayama, Y.; Wada, Y.; et al. (64) Cu-DOTA-trastuzumab PET imaging and HER2 specificity of brain metastases in HER2-positive breast cancer patients. EJNMMI Res. 2015, 5, 8. [Google Scholar] [CrossRef] [Green Version]
- Chargari, C.; Idrissi, H.R.; Pierga, J.Y.; Bollet, M.A.; Diéras, V.; Campana, F.; Cottu, P.; Fourquet, A.; Kirova, Y.M. Preliminary results of whole brain radiotherapy with concurrent trastuzumab for treatment of brain metastases in breast cancer patients. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.A.; Kotecha, R.; Ahluwalia, M.S.; Mohammadi, A.M.; Chao, S.T.; Barnett, G.H.; Murphy, E.S.; Vogelbaum, M.A.; Angelov, L.; Peereboom, D.M.; et al. Overall survival and the response to radiotherapy among molecular subtypes of breast cancer brain metastases treated with targeted therapies. Cancer 2017, 123, 2283–2293. [Google Scholar] [CrossRef] [PubMed]
- Ulaner, G.A.; Lyashchenko, S.K.; Riedl, C.; Ruan, S.; Zanzonico, P.B.; Lake, D.; Jhaveri, K.; Zeglis, B.; Lewis, J.S.; O’Donoghue, J.A. First-in-Human Human Epidermal Growth Factor Receptor 2-Targeted Imaging Using 89Zr-Pertuzumab PET/CT: Dosimetry and Clinical Application in Patients with Breast Cancer. J. Nucl. Med. 2018, 59, 900–906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, N.U.; Kumthekar, P.; Sahebjam, S.; Ibrahim, N.; Fung, A.; Cheng, A.; Nicholas, A.; Wang, B.; Pegram, M. Pertuzumab (P) plus high-dose trastuzumab (H) for the treatment of central nervous system (CNS) progression after radiotherapy (RT) in patients (pts) with HER2-positive metastatic breast cancer (MBC): Primary efficacy analysis results from the phase II PATRICIA study. Cancer Res. 2020, 80, P1-18-03. [Google Scholar]
- Swain, S.M.; Baselga, J.; Miles, D.; Im, Y.H.; Quah, C.; Lee, L.F.; Cortés, J. Incidence of central nervous system metastases in patients with HER2-positive metastatic breast cancer treated with pertuzumab, trastuzumab, and docetaxel: Results from the randomized phase III study Cleopatra. Ann. Oncol. 2014, 25, 1116–1121. [Google Scholar] [CrossRef]
- Bergen, E.S.; Binter, A.; Starzer, A.M.; Heller, G.; Kiesel, B.; Tendl-Schulz, K.; Bago-Horvath, Z.; Furtner, J.; Leitner, J.; Exner, R.; et al. Favourable outcome of patients with breast cancer brain metastases treated with dual HER2 blockade of trastuzumab and pertuzumab. Ther. Adv. Med. Oncol. 2021, 13, 17588359211009002. [Google Scholar] [CrossRef]
- Ippolito, E.; Silipigni, S.; Matteucci, P.; Greco, C.; Pantano, F.; D’Auria, G.; Quattrocchi, C.C.; Floreno, B.; Fiore, M.; Gamucci, T.; et al. Stereotactic Radiation and Dual Human Epidermal Growth Factor Receptor 2 Blockade with Trastuzumab and Pertuzumab in the Treatment of Breast Cancer Brain Metastases: A Single Institution Series. Cancers 2022, 14, 303. [Google Scholar] [CrossRef]
- Saleem, A.; Searle, G.E.; Kenny, L.M.; Huiban, M.; Kozlowski, K.; Waldman, A.D.; Woodley, L.; Palmieri, C.; Lowdell, C.; Kaneko, T.; et al. Lapatinib access into normal brain and brain metastases in patients with Her-2 overexpressing breast cancer. EJNMMI Res. 2017, 5, 30, Erratum in EJNMMI Res. 2017, 7, 74. [Google Scholar] [CrossRef] [Green Version]
- Kennecke, H.; Yerushalmi, R.; Woods, R.; Cheang, M.C.; Voduc, D.; Speers, C.H.; Nielsen, T.O.; Gelmon, K. Metastatic behavior of breast cancer subtypes. J. Clin. Oncol. 2010, 28, 3271–3277. [Google Scholar] [CrossRef] [PubMed]
- Morikawa, A.; Peereboom, D.M.; Thorsheim, H.R.; Samala, R.; Balyan, R.; Murphy, C.G.; Lockman, P.R.; Simmons, A.; Weil, R.J.; Tabar, V.; et al. Capecitabine and lapatinib uptake in surgically resected brain metastases from metastatic breast cancer patients: A prospective study. Neuro Oncol. 2015, 17, 289–295, Erratum in Neuro Oncol. 2015, 17, 1423. [Google Scholar] [CrossRef] [Green Version]
- Bachelot, T.; Romieu, G.; Campone, M.; Diéras, V.; Cropet, C.; Dalenc, F.; Jimenez, M.; Le Rhun, E.; Pierga, J.Y.; Gonçalves, A.; et al. Lapatinib plus capecitabine in patients with previously untreated brain metastases from HER2-positive metastatic breast cancer (LANDSCAPE): A single-group phase 2 study. Lancet Oncol. 2013, 14, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.; Cho, B.J.; Choi, E.J.; Park, J.M.; Kim, D.H.; Kim, I.A. Radiosensitizing effect of lapatinib in human epidermal growth factor receptor 2-positive breast cancer cells. Oncotarget 2016, 7, 79089–79100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Angelini, P.D.; Zacarias Fluck, M.F.; Pedersen, K.; Parra-Palau, J.L.; Guiu, M.; Bernadó Morales, C.; Vicario, R.; Luque-García, A.; Navalpotro, N.P.; Giralt, J.; et al. Constitutive HER2 signaling promotes breast cancer metastasis through cellular senescence. Cancer Res. 2013, 73, 450–458, Erratum in Cancer Res. 2013, 73, 6095. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, N.U.; Freedman, R.A.; Ramakrishna, N.; Younger, J.; Storniolo, A.M.; Bellon, J.R.; Come, S.E.; Gelman, R.S.; Harris, G.J.; Henderson, M.A.; et al. A phase I study of lapatinib with whole brain radiotherapy in patients with Human Epidermal Growth Factor Receptor 2 (HER2)-positive breast cancer brain metastases. Breast Cancer Res. Treat. 2013, 142, 405–414. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.M.; Miller, J.A.; Kotecha, R.; Chao, S.T.; Ahluwalia, M.S.; Peereboom, D.M.; Mohammadi, A.M.; Barnett, G.H.; Murphy, E.S.; Vogelbaum, M.A.; et al. Stereotactic radiosurgery with concurrent HER2-directed therapy is associated with improved objective response for breast cancer brain metastasis. Neuro Oncol. 2019, 21, 659–668. [Google Scholar] [CrossRef] [PubMed]
- Parsai, S.; Miller, J.A.; Juloori, A.; Chao, S.T.; Kotecha, R.; Mohammadi, A.M.; Ahluwalia, M.S.; Murphy, E.S.; Barnett, G.H.; Vogelbaum, M.A.; et al. Stereotactic radiosurgery with concurrent lapatinib is associated with improved local control for HER2-positive breast cancer brain metastases. J. Neurosurg. 2019, 132, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Zhao, Z.; Arooj, S.; Zheng, T.; Liao, G. Lapatinib Plus Local Radiation Therapy for Brain Metastases From HER-2 Positive Breast Cancer Patients and Role of Trastuzumab: A Systematic Review and Meta-Analysis. Front. Oncol. 2020, 10, 576926. [Google Scholar] [CrossRef] [PubMed]
- Mignot, F.; Kirova, Y.; Verrelle, P.; Teulade-Fichou, M.P.; Megnin-Chanet, F. In vitro effects of Trastuzumab Emtansine (T-DM1) and concurrent irradiation on HER2-positive breast cancer cells. Cancer Radiother. 2021, 25, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, F.; Delaloge, S.; Barrios, C.H.; Wuerstlein, R.; Anton, A.; Brain, E.; Hatschek, T.; Kelly, C.M.; Peña-Murillo, C.; Yilmaz, M.; et al. Trastuzumab emtansine (T-DM1) in patients with HER2-positivemetastatic breast cancer and brain metastases: Exploratory final analysis of cohort 1 from KAMILLA, a single-arm phase IIIb clinical trials. Ann. Oncol. 2020, 10, 1350–1358. [Google Scholar] [CrossRef]
- Kowalczyk, L.; Bartsch, R.; Singer, C.F.; Farr, A. Adverse Events of Trastuzumab Emtansine (T-DM1) in the Treatment of HER2-Positive Breast Cancer Patients. Breast Care 2017, 12, 401–408. [Google Scholar] [CrossRef]
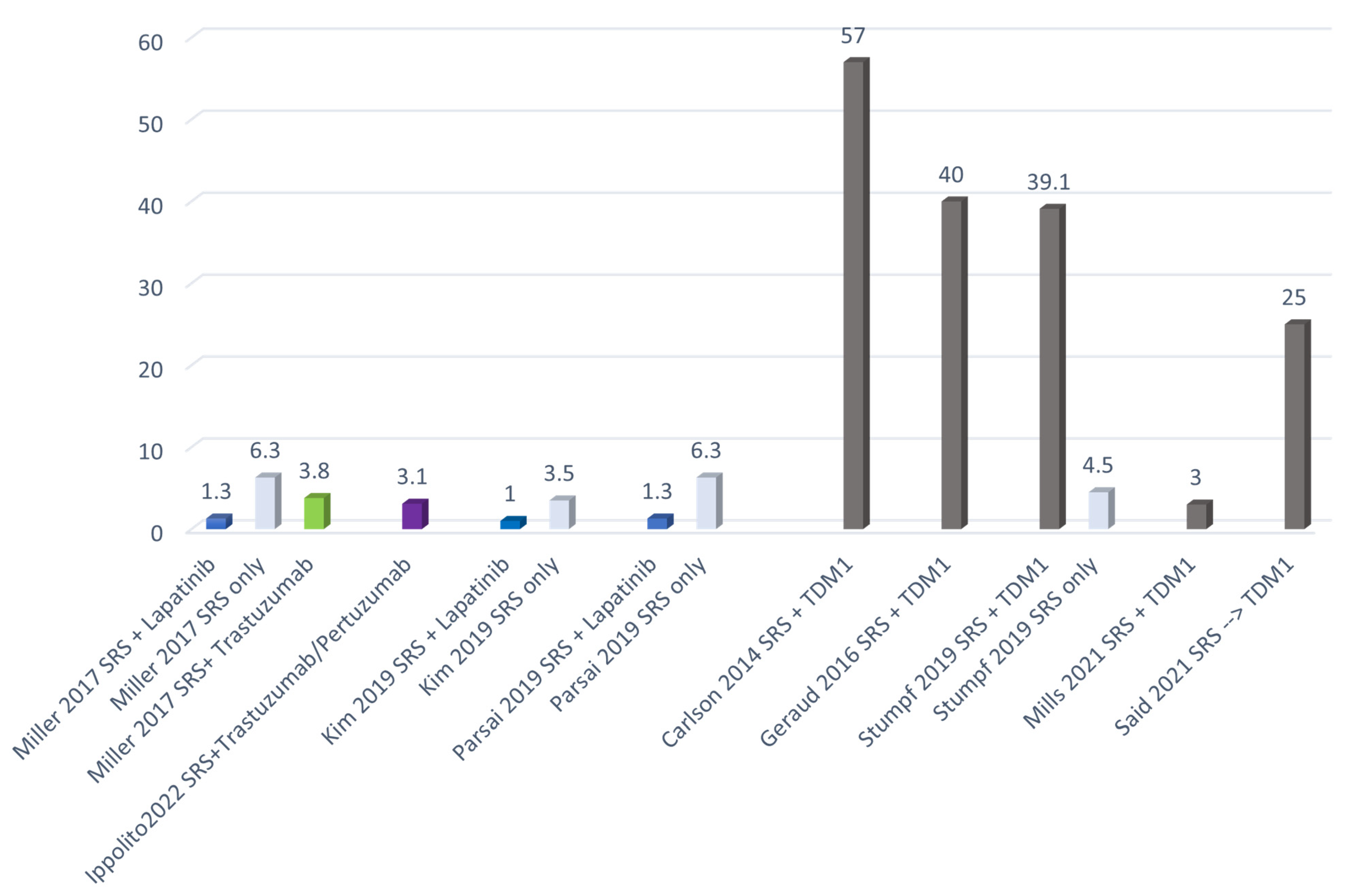
- Stumpf, P.K.; Cittelly, D.M.; Robin, T.P.; Carlson, J.A.; Stuhr, K.A.; Contreras-Zarate, M.J.; Lai, S.; Ormond, D.R.; Rusthoven, C.G.; Gaspar, L.E.; et al. Combination of Trastuzumab Emtansine and Stereotactic Radiosurgery Results in High Rates of Clinically Significant Radionecrosis and Dysregulation of Aquaporin-4. Clin. Cancer Res. 2019, 25, 3946–3953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mills, M.N.; Walker, C.; Thawani, C.; Naz, A.; Figura, N.B.; Kushchayev, S.; Etame, A.; Yu, H.M.; Robinson, T.J.; Liu, J.; et al. Trastuzumab Emtansine (T-DM1) and stereotactic radiation in the management of HER2+ breast cancer brain metastases. BMC Cancer 2021, 21, 223. [Google Scholar] [CrossRef] [PubMed]
- Id Said, B.; Chen, H.; Jerzak, K.; Myrehaug, S.D.; Tseng CLDetsky, J.; Husain, Z.A.; Sahgal, A.; Soliman, H. T-DM1 Increases the Risk of SRS-Induced Radiation Necrosis in Her2+ Breast Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2021, 111, e568. [Google Scholar] [CrossRef]
- Vogelbaum, M.A.; Brown, P.D.; Messersmith, H.; Brastianos, P.K.; Burri, S.; Cahill, D.; Dunn, I.F.; Gaspar, L.E.; Gatson, N.T.N.; Gondi, V.; et al. Treatment for Brain Metastases: ASCO-SNO-ASTRO Guideline. J. Clin. Oncol. 2021, 40, 452–516. [Google Scholar] [CrossRef] [PubMed]
- Gori, S.; Puglisi, F.; Moroso, S.; Fabi, A.; La Verde, N.; Frassoldati, A.; Tarenzi, E.; Garrone, O.; Vici, P.; Laudadio, L.; et al. The HERBA Study: A Retrospective Multi-Institutional Italian Study on Patients With Brain Metastases From HER2-Positive Breast Cancer. Clin. Breast Cancer 2019, 19, e501–e510. [Google Scholar] [CrossRef] [PubMed]
- Carlson, J.A.; Nooruddin, Z.; Rusthoven, C.; Elias, A.; Borges, V.F.; Diamond, J.R.; Kavanagh, B.; Kabos, P. Trastuzumab emtansine and stereotactic radiosurgery: An unexpected increase in clinically significant brain edema. Neuro Oncol. 2014, 16, 1006–1009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geraud, A.; Xu, H.P.; Beuzeboc, P.; Kirova, Y.M. Preliminary experience of the concurrent use of radiosurgery and T-DM1 for brain metastases in HER2-positive metastatic breast cancer. J. Neurooncol. 2017, 131, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Russillo, M.; Ferretti, G.; Vidiri, A.; Gasparro, S.; Cognetti, F.; Pellegrini, D.; Fabi, A. Impressive Long-term Response with Pertuzumab and Trastuzumab in HER2-positive Breast Cancer with Brain Metastasis. Vivo 2018, 32, 839–842. [Google Scholar] [CrossRef]
- Silipigni, S.; Ippolito, E.; Matteucci, P.; Santo, B.; Gangemi, E.; La Cesa, A.; Santini, D.; Greco, C.; Ramella, S. Repeated courses of radiation treatment in an HER2-positive breast cancer patient with diffuse brain metastases: A case report. Breast J. 2020, 26, 1370–1371. [Google Scholar] [CrossRef] [PubMed]


| Authors | Study | Year | Population | Treatment | Outcome | Adverse Effects |
|---|---|---|---|---|---|---|
| Lin et al. [55] | Phase I | 2013 | - 28 patients |
| ORR 79% 6 mPFS 46% at 6 months | RN / |
| Parsai et al. [57] | Retrospective | 2019 | - 126 patients (479 lesions) |
| LF - Concurrent lapatinib + SRS 12-month (5.7% vs. 15.1%, p < 0.01), 24-month (6.5% vs. 18.0%, p < 0.01) | RN - 1.3% cohort treated with lapatinib - SRS alone 6.3% (p< 0.01) |
| Kim et al. [56] | Retrospective | 2019 | - 84 patients (487 lesions) | SRS (18–24 Gy)+/−WBRT - 132 lesions (27%) SRS + lapatinib - 355 lesions (73%) only SRS | CR - Lapatinib + SRS 35% - Only SRS 11% (p = 0.008) OR - Lapatinib + SRS -100% - Only SRS - 70% (p < 0.001) | RN - SRS + lapatinib 1.0% - Only SRS 3.5% (p = 0.27) |
| M Khan et al. [58] | Review–meta-analysis | 2020 |
| 279 patients: lapatinib +/− anti-HER2 therapy - 610 patients: anti-HER2 therapy (mainly trastuzumab) - 227 patients: no anti-HER2 therapy | OS - Lapatinib-based therapy was associated with increase in OS (HR 0.63 p < 0.00001) LC significantly increased with concurrent lapatinib + SRS (HR 0.47 (0.33, 0.66), p = 0.0001) | RN Lower rate for concurrent lapatinib + SRS: - Miller: 1.3% vs. 6.3% (p 0.001) - Kim: 1% vs. 3.5% (p = 0.134) - Parsai: 1.3% vs. 6.3% (p = 0.001) |
| Authors | Study | Year | Population | Treatment | Outcome | Adverse Effects |
|---|---|---|---|---|---|---|
| Carlson J et al. [60] | Retrospective | 2014 | - 13 patients | 7/13 patients T-DM1 + SRS | NR | RN 57% (4/7) SRS + T-DM1 |
| Geraud A et al. [61] | Retrospective | 2017 | - 12 patients |
| SRS + Concurrent T-DM1 - OR 75% - PD 25% SRS + Sequential T-DM1 - OR 75% - PD 25% | RN - 33.3% (4/12) in the sequential group - 50% (2/4) in the concurrent group OTHER - Edema rate of 28.6% in the sequential group - Edema rate of 25% in the concurrent group |
| Stumpf PK et al. [62] | Retrospective | 2019 | -45 patients | TDM1 + RT: -23/45 (51.1%): -16 SRS/FSRT + Concurrent T-DM1: -7 SRS and sequential T-DM1 - Only SRS 22/45 -15 patients also received WBRT | NR | RN 10/45 (22.2%) clinically significant: - 9 of 23 (39.1%) patients received T-DM1 (3 sequential SRS, 6 concurrent SRS) - 1 of 22 (4.5%) patients did not receive T-DM1 |
| Mills MN et al. [63] | Retrospective | 2021 | - 16 patients (40 lesions) | RT: - 24 SRS (median dose 21 Gy) - 16 FSRT (median dose 25 Gy/3–5 fractions) T-DM1: - 19 RT + Concurrent T-DM1 - 11 RT and sequential T-DM1 - 10 T-DM1 and sequential RT | - 20 months LC 75% (SRS or FSRT) - 20 months DIC 50% (SRS or FSRT) - 20 months OS 67% (SRS or FSRT) and 79% (following BCBM diagnosis) | RN 1 patient (3%) OTHER: 45% G1–G2 Headaches and fatigue |
| Id Said B et al. [64] | Retrospective | 2021 | - 67 patients (223 lesions) | 21/67 patients (31.3%) SRS and sequential T-DM1 | / | RN - Post-SRS 1-year 6.7% (95% CI 2.7–10.7%) 2-year 15.2% (95% CI 9.2–21.3%) - SRS and sequential T-DM1 1- and 2-years 25.2% (95% CI 12.8–37.6%) |
| Clinicaltrials Identifier | Title | Phase | N° Patients | Treatment Arms | Endpoint |
|---|---|---|---|---|---|
| NCT05042791 | Pyrotinib Combined With Brain Radiotherapy in Breast Cancer Patients With BMs | 2 Randomized | 362 | Experimental: fSRT combined with pyrotinib and capecitabine Active Comparator: WBRT combined with pyrotinib and capecitabine | 1-year objective response rate of central nervous system |
| NCT04582968 | A Study of Pyrotinib Plus Capecitabine Combined With SRT in HER2+ MBC With BMs | I/II | 47 | fSRT or WBRT drug: pyrotinib combined with capecitabine pyrotinib, 400 mg once daily; capecitabine 1000 mg/m2 per day on day 1 through 14, every 21 days | 1. Safety and tolerability of pyrotinib plus capecitabine combined with brain radiotherapy 2. Intracranial local tumor control rate |
| WBRT Intent | Patient Category |
|---|---|
| Palliative | Patients with a life expectancy of less than 6 months |
| Increase intracranial control | Patients diagnosed with symptomatic diffuse BMs or multiple BMs (5–15) who are not suitable for SRS/fSRT. Multidisciplinary evaluation is recommended in this latter case for an accurate risk/benefit assessment in terms of disease control and neurocognitive side effects, with particular reference to age, patient preferences and therapeutic options to control extracranial disease |
| Increase intracranial control | Patients who rapidly progress (<6 months) after a first course of brain RT treatment or with associated systemic progression, with an evaluation of the therapeutic options available on the basis of the patient’s clinical history |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ippolito, E.; Silipigni, S.; Matteucci, P.; Greco, C.; Carrafiello, S.; Palumbo, V.; Tacconi, C.; Talocco, C.; Fiore, M.; D’Angelillo, R.M.; et al. Radiotherapy for HER 2 Positive Brain Metastases: Urgent Need for a Paradigm Shift. Cancers 2022, 14, 1514. https://doi.org/10.3390/cancers14061514
Ippolito E, Silipigni S, Matteucci P, Greco C, Carrafiello S, Palumbo V, Tacconi C, Talocco C, Fiore M, D’Angelillo RM, et al. Radiotherapy for HER 2 Positive Brain Metastases: Urgent Need for a Paradigm Shift. Cancers. 2022; 14(6):1514. https://doi.org/10.3390/cancers14061514
Chicago/Turabian StyleIppolito, Edy, Sonia Silipigni, Paolo Matteucci, Carlo Greco, Sofia Carrafiello, Vincenzo Palumbo, Claudia Tacconi, Claudia Talocco, Michele Fiore, Rolando Maria D’Angelillo, and et al. 2022. "Radiotherapy for HER 2 Positive Brain Metastases: Urgent Need for a Paradigm Shift" Cancers 14, no. 6: 1514. https://doi.org/10.3390/cancers14061514
APA StyleIppolito, E., Silipigni, S., Matteucci, P., Greco, C., Carrafiello, S., Palumbo, V., Tacconi, C., Talocco, C., Fiore, M., D’Angelillo, R. M., & Ramella, S. (2022). Radiotherapy for HER 2 Positive Brain Metastases: Urgent Need for a Paradigm Shift. Cancers, 14(6), 1514. https://doi.org/10.3390/cancers14061514







