Diagnostic Performance of 18F-Choline Positron Emission Tomography/Contrast-Enhanced Computed Tomography in Adenoma Detection in Primary Hyperparathyroidism after Inconclusive Imaging: A Retrospective Study of 215 Patients
Abstract
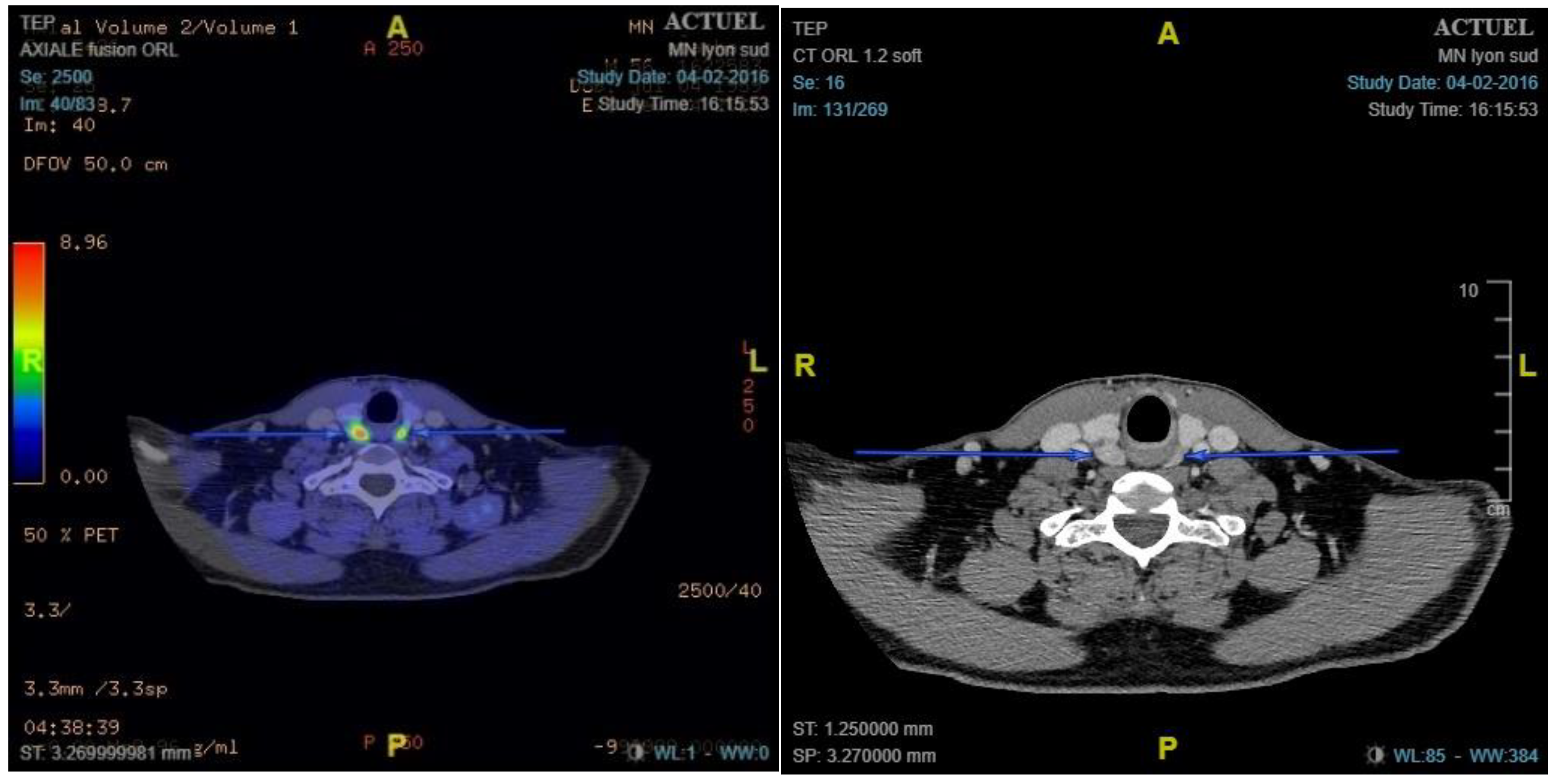
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. Measurements
2.2.1. General Measurements
- Demographic data: sex, age, body mass index (BMI)
- Medical background: hypertension, diabetes, osteoporosis, nephrolithiasis, multiple endocrine neoplasia (MEN), HRPT2 mutation, and persistent or recurrent hyperparathyroidism
- Surgical background: thyroid surgery or parathyroid surgery
2.2.2. Preoperative Measurements
- Biological findings: calcium level (mmol/L) and PTH level (expressed as the PTH/normal PTH ratio due to differences in normal ranges among laboratories)
- Preoperative 18F-choline PET/ceCT data: lesion location, number of lesions, lesion size, and maximum standardised uptake value (SUVmax)
2.2.3. Perioperative Findings
2.2.4. Histological Findings
2.2.5. Follow-Up
2.3. Protocols
2.3.1. 18F-Choline PET/ceCT Protocol
2.3.2. Surgical Protocol
2.4. Data Interpretation and Statistics
2.4.1. Diagnostic Performances
- True positive (TP): a removed gland leading to cure with pathological findings on histological examination.
- False positive (FP): a removed gland not leading to cure but with normal findings on histological examination.
- False negative (FN): a removed gland not considered pathological on 18F-choline PET/ceCT but its removal leads to cure with pathological findings on histological examination.
- True negative (TN): glands not considered pathological on 18F-choline PET/ceCT or during surgical exploration.
2.4.2. Correlation between 18F-Choline PET/ceCT and Surgical Findings
- Removed glands with different locations on 18F-choline PET/ceCT and during a surgical examination
- Removed glands not described as pathological on 18F-choline PET/ceCT but showing pathological findings on histological examination
- Removed glands described as pathological on 18F-choline PET/ceCT but without pathological findings during surgical and/or histological examination
2.4.3. Statistics
3. Results
3.1. Population Characteristics
3.2. Surgical Results
3.3. 18F-Choline PET/ceCT Results and Performances
3.4. Correlation between 18F-Choline PET/ceCT and Surgical Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spanu, A.; Schillaci, O.; Piras, B.; Madeddu, G. SPECT/CT in hyperparathyroidism. Clin. Transl. Imaging 2014, 2, 537–555. [Google Scholar] [CrossRef][Green Version]
- Udelsman, R. Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann. Surg. 2002, 235, 665–670, discussion 670–672. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.F.; Sebag, F.; Cherenko, M.; Ippolito, G.; Taieb, D.; Vaillant, J. Endoscopic parathyroidectomy: Why and when? World J. Surg. 2008, 32, 2509–2515. [Google Scholar] [CrossRef] [PubMed]
- Bergenfelz, A.; Lindblom, P.; Tibblin, S.; Westerdahl, J. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: A prospective randomized controlled trial. Ann. Surg. 2002, 236, 543–551. [Google Scholar] [CrossRef] [PubMed]
- Schneider, D.F.; Mazeh, H.; Sippel, R.S.; Chen, H. Is minimally invasive parathyroidectomy associated with greater recurrence compared to bilateral exploration? Analysis of more than 1000 cases. Surgery 2012, 152, 1008–1015. [Google Scholar] [CrossRef]
- Norman, J.; Lopez, J.; Politz, D. Abandoning unilateral parathyroidectomy: Why we reversed our position after 15,000 parathyroid operations. J. Am. Coll Surg. 2012, 214, 260–269. [Google Scholar] [CrossRef]
- Huppert, B.J.; Reading, C.C. Parathyroid sonography: Imaging and intervention. J. Clin. Ultrasound 2007, 35, 144–155. [Google Scholar] [CrossRef]
- Aspinall, S.R.; Nicholson, S.; Bliss, R.D.; Lennard, T.W.J. The impact of surgeon-based ultrasonography for parathyroid disease on a British endocrine surgical practice. Ann. R Coll. Surg. Engl. 2012, 94, 17–22. [Google Scholar] [CrossRef]
- Sample, W.F.; Mitchell, S.P.; Bledsoe, R.C. Parathyroid ultrasonography. Radiology 1978, 127, 485–490. [Google Scholar] [CrossRef]
- Biertho, L.D.; Kim, C.; Wu, H.S.; Unger, P.; Inabnet, W.B. Relationship between sestamibi uptake, parathyroid hormone assay, and nuclear morphology in primary hyperparathyroidism. J. Am. Coll Surg. 2004, 199, 229–233. [Google Scholar] [CrossRef]
- Ruda, J.M.; Hollenbeak, C.S.; Stack, B.C. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol. Head Neck. Surg. 2005, 132, 359–372. [Google Scholar] [CrossRef] [PubMed]
- Ghafoor, S.; Burger, I.A.; Vargas, A.H. Multimodality imaging of prostate cancer. J. Nucl. Med. 2019, 60, 1350–1358. [Google Scholar] [CrossRef] [PubMed]
- Talbot, J.N.; Fartoux, L.; Balogova, S.; Nataf, V.; Kerrou, K.; Gutman, F.; Huchet, V.; Ancel, D.; Grange, J.-D.; Rosmorduc, O. Detection of hepatocellular carcinoma with PET/CT: A prospective comparison of 18F-fluorocholine and 18F-FDG in patients with cirrhosis or chronic liver disease. J. Nucl. Med. 2010, 51, 1699–1706. [Google Scholar] [CrossRef] [PubMed]
- Quak, E.; Lheureux, S.; Reznik, Y.; Bardet, S.; Aide, N. F18-choline, a novel PET tracer for parathyroid adenoma? J. Clin. Endocrinol. Metab 2013, 98, 3111–3112. [Google Scholar] [CrossRef]
- Mapelli, P.; Busnardo, E.; Magnani, P.; Freschi, M.; Picchio, M.; Gianolli, L.; Messa, C. Incidental finding of parathyroid adenoma with 11C-choline PET/CT. Clin. Nucl. Med. 2012, 37, 593–595. [Google Scholar] [CrossRef]
- Beheshti, M.; Hehenwarter, L.; Paymani, Z.; Rendl, G.; Imamovic, L.; Rettenbacher, R.; Tsybrovskyy, O.; Langsteger, W.; Pirich, C. 18F-Fluorocholine PET/CT in the assessment of primary hyperparathyroidism compared with 99mTc-MIBI or 99mTc-tetrofosmin SPECT/CT: A prospective dual-centre study in 100 patients. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 1762–1771. [Google Scholar] [CrossRef]
- Huber, G.F.; Hüllner, M.; Schmid, C.; Brunner, A.; Sah, B.; Vetter, D.; Kaufmann, P.A.; von Schulthess, G.K. Benefit of 18F-fluorocholine PET imaging in parathyroid surgery. Eur. Radiol. 2018, 28, 2700–2707. [Google Scholar] [CrossRef]
- Fischli, S.; Suter-Widmer, I.; Nguyen, B.T.; Müller, W.; Metzger, J.; Strobel, K.; Grunig, H.; Henzen, G. The significance of 18F-fluorocholine-PET/CT as localizing imaging technique in patients with primary hyperparathyroidism and negative conventional imaging. Front Endocrinol. 2017, 8, 380. [Google Scholar] [CrossRef]
- Orevi, M.; Freedman, N.; Mishani, E.; Bocher, M.; Jacobson, O.; Krausz, Y. Localization of parathyroid adenoma by 11C-choline PET/CT: Preliminary results. Clin. Nucl. Med. 2014, 39, 1033–1038. [Google Scholar] [CrossRef]
- Michaud, L.; Burgess, A.; Huchet, V.; Lefèvre, M.; Tassart, M.; Ohnona, J.; Kerrou, K.; Balogova, S.; Talbot, J.-N.; Perie, S. Is 18F-fluorocholine-positron emission tomography/computerized tomography a new imaging tool for detecting hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism? J. Clin. Endocrinol. Metab 2014, 99, 4531–4536. [Google Scholar] [CrossRef]
- Kluijfhout, W.P.; Vorselaars, W.M.C.M.; van den Berk, S.A.M.; Vriens, M.R.; Borel Rinkes, I.H.M.; Valk, G.D.; van Dalen, T.; de Klerk, J.M.H.; de Keizer, B. Fluorine-18 fluorocholine PET-CT localizes hyperparathyroidism in patients with inconclusive conventional imaging: A multicenter study from the Netherlands. Nucl. Med. Commun. 2016, 37, 1246–1252. [Google Scholar] [CrossRef] [PubMed]
- Quak, E.; Blanchard, D.; Houdu, B.; Le Roux, Y.; Ciappuccini, R.; Lireux, B.; de Raucourt, D.; Grellard, J.-M.; Licaj, I.; Bardet, S.; et al. F18-choline PET/CT guided surgery in primary hyperparathyroidism when ultrasound and MIBI SPECT/CT are negative or inconclusive: The APACH1 study. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 658–666. [Google Scholar] [CrossRef] [PubMed]
- Broos, W.A.M.; van der Zant, F.M.; Knol, R.J.J.; Wondergem, M. Choline PET/CT in parathyroid imaging: A systematic review. Nucl. Med. Commun. 2019, 40, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Lee, S.W.; Jeong, S.Y.; Pak, K.; Kim, K. Diagnostic performance of F-18 fluorocholine PET/CT for parathyroid localization in hyperparathyroidism: A systematic review and meta-analysis. Horm. Cancer 2018, 9, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Lezaic, L.; Rep, S.; Sever, M.J.; Kocjan, T.; Hocevar, M.; Fettich, J. 18F-fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: A pilot study. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 2083–2089. [Google Scholar] [CrossRef]
- Hamidi, M.; Sullivan, M.; Hunter, G.; Hamberg, L.; Cho, N.L.; Gawande, A.A.; Doherty, G.M.; Moore, F.D., Jr.; Nehs, M.A. 4D-CT is superior to ultrasound and sestamibi for localizing recurrent parathyroid disease. Ann. Surg. Oncol. 2018, 25, 1403–1409. [Google Scholar] [CrossRef]
- Amadou, C.; Bera, G.; Ezziane, M.; Chami, L.; Delbot, T.; Rouxel, A.; Leban, M.; Herve, G.; Menegaux, F.; Leenhardt, L. 18F-fluorocholine PET/CT and parathyroid 4D computed tomography for primary hyperparathyroidism: The challenge of reoperative patients. World J. Surg. 2019, 43, 1232–1242. [Google Scholar] [CrossRef]
- Griffith, B.; Chaudhary, H.; Mahmood, G.; Carlin, A.M.; Peterson, E.; Singer, M.; Patel, S.C. Accuracy of 2-phase parathyroid CT for the preoperative localization of parathyroid adenomas in primary hyperparathyroidism. AJNR Am. J. Neuroradiol. 2015, 36, 2373–2379. [Google Scholar] [CrossRef]
- Day, K.M.; Elsayed, M.; Beland, M.D.; Monchik, J.M. The utility of 4-dimensional computed tomography for preoperative localization of primary hyperparathyroidism in patients not localized by sestamibi or ultrasonography. Surgery 2015, 157, 534–539. [Google Scholar] [CrossRef]
- Meilstrup, J.W. Ultrasound examination of the parathyroid glands. Otolaryngol Clin. North Am. 2004, 37, 763–778, ix. [Google Scholar] [CrossRef]
- Gritzmann, N.; Koischwitz, D.; Rettenbacher, T. Sonography of the thyroid and parathyroid glands. Radiol. Clin. North Am. 2000, 38, 1131–1145, xii. [Google Scholar] [CrossRef]
- Quak, E.; Lasne Cardon, A.; Ciappuccini, R.; Lasnon, C.; Bastit, V.; Le Henaff, V.; Lireux, B.; Foucras, G.; Jaudet, C.; Berchi, C.; et al. Upfront F18-choline PET/CT versus Tc99m-sestaMIBI SPECT/CT guided surgery in primary hyperparathyroidism: The randomized phase III diagnostic trial APACH2. BMC Endocr. Disord 2021, 21, 3. [Google Scholar] [CrossRef] [PubMed]





| Characteristics | Mean (Standard Deviation) or Number (Proportion) | Range |
|---|---|---|
| Age (years) (n = 215) | 62 (14.2) | (18–87) |
| Sex (n = 215) | ||
| Male | 52 (24%) | |
| Female | 163 (76%) | |
| BMI (kg/m2) (n = 215) | 26.2 (6.0) | (13.9–51.3) |
| Hypertension (n = 215) | 81 (38%) | |
| Osteoporosis (n = 215) | 84 (39%) | |
| Fractures (n = 215) | 27 (13%) | |
| Nephrolithiasis (n = 215) | 63 (29%) | |
| Previous cervical surgery (n = 215) | ||
| Thyroidectomy | ||
| Partial | 7 (3.3%) | |
| Total | 7 (3.3%) | |
| Parathyroidectomy | ||
| Minimally invasive | 7 (3.3%) | |
| SBPE | 23 (11%) | |
| Preoperative markers | ||
| Calcium (mmol/L) (n = 215) | 2.77 (0.19) | (2.28–3.64) |
| PTH (normal ratio) (n = 208) | 2.18 (1.00) | (0.61–19.80) |
| Postoperative markers, day 1 | ||
| Calcium (mmol/L) (n = 214) | 2.38 (0.196) | (1.930–3.120) |
| PTH (ng/L) (n = 201) | 13.9 (10.8) | (4.0–65.0) |
| PTH (normal ratio) (n = 200) | 0.35 (0.26) | (0.10–1.94) |
| Postoperative markers, week 6 | ||
| Calcium (mmol/L) (n = 209) | 2.370 (0.141) | (1.190–2.910) |
| PTH (normal ratio) (n = 195) | 0.917 (0.472) | (0.280–4.630) |
| Surgical approach (n = 215) | ||
| Minimally invasive | 52 (24%) | |
| SBPE | 163 (76%) | |
| Surgical complications (n = 215) | ||
| Hypocalcaemia | 7 (3.4%) | |
| Recurrent laryngeal nerve palsy | 6 (2.9%) | |
| Superficial hematoma | 1 (0.4%) | |
| Cure rate at 6 weeks (n = 210) | 202 (95%) |
| TP | TN | FP | FN | Se | Sp | PPV | NPV | |
|---|---|---|---|---|---|---|---|---|
| Per lesion | 219 | 592 | 21 | 28 | 88.6% | 96.6% | 91.4% | 95.4% |
| Per patient | 164 | 21 | 25 | 86.8% | 88.6% |
| Well Correlated (n = 220) | Uncorrelated (n = 49) | p | Test | |
|---|---|---|---|---|
| Age (years) | 62.0 ± 14.3 | 61.5 ± 13.6 | 0.83 | Welch |
| BMI (kg/m²) | 26.2 ± 6.2 | 26.5 ± 6.0 | 0.77 | Welch |
| Sex | ||||
| Male | 51 (23%) | 12 (24%) | 0.84 | χ2 |
| Female | 169 (77%) | 37 (76%) | ||
| Hypertension | 86 (39%) | 17 (35%) | 0.57 | χ2 |
| Diabetes | 14 (6.4%) | 2 (4.1%) | 0.74 | Fisher |
| Osteoporosis | 87 (40%) | 18 (37%) | 0.72 | χ2 |
| Fractures | 28 (13.0%) | 3 (6.1%) | 0.19 | |
| Nephrolithiasis | 63 (29%) | 15 (31%) | 0.78 | χ2 |
| Previous cervical surgery | ||||
| Thyroidectomy | 0.81 | Fisher | ||
| Partial | 7 (3.3%) | 2 (4.0%) | ||
| Total | 8 (3.6%) | 1 (2.0%) | ||
| Parathyroidectomy | ||||
| Minimally invasive | 4 (1.8%) | 3 (6.1%) | 0.093 | Fisher |
| SBPE | 20 (9.1%) | 7 (14.0%) | ||
| Recurring disease | 16 (7.3%) | 7 (14.0%) | 0.16 | Fisher |
| Persisting disease | 8 (3.6%) | 3 (6.1%) | ||
| Preoperative markers | ||||
| Calcium (mmol/L) | 2.76 ± 0.21 | 2.77 ± 0.18 | 0.67 | Welch |
| PTH (normal ratio) | 2.27 ± 2.18 | 1.95 ± 0.95 | 0.12 | Welch |
| Surgeon | ||||
| JCL | 147 (67%) | 36 (75%) | 0.27 | χ2 |
| LM | 73 (33%) | 12 (25%) | ||
| Surgical approach | ||||
| Minimally invasive | 52 (24%) | 0 (0%) | <0.001 | χ2 |
| SBPE | 168 (76%) | 49 (100%) | ||
| PET data | ||||
| Size (mm) | 12.20 ± 7.61 | 3.90 ± 6.02 | <0.001 | Welch |
| SUVmax | 4.25 ± 2.25 | 1.55 ± 2.00 | <0.001 | Welch |
| Number of lesions | ||||
| 0 | 0 (0%) | 13 (27%) | <0.001 | Fisher |
| 1 | 162 (74%) | 22 (45%) | ||
| >1 | 58 (26%) | 14 (29%) | ||
| Cure rate | 212 (97%) | 43 (91%) | 0.081 | Fisher |
| Variables | OR (95% CI) | p | Variables | OR (95% CI) | p | Variables | OR (95% CI) | p |
|---|---|---|---|---|---|---|---|---|
| SUVmax of lesion | 0.379 (0.281, 0.510) | <0.001 | Size of lesion | 0.703 (0.631, 0.785) | <0.001 | Number of lesions | 0.151 (0.039, 0.497) | <0.01 |
| Osteoporosis | 0.854 (0.347, 2.10) | 0.73 | - | 1.430 (0.578, 3.56) | 0.44 | - | 0.851 (0.312, 2.210) | 0.74 |
| Calcium level | 1.140 (0.187, 6.96) | 0.89 | - | 1.390 (0.158, 12.2) | 0.77 | - | 0.885 (0.665, 1.150) | 0.38 |
| PTH ratio | 1.060 (0.741, 1.53) | 0.74 | - | 0.986 (0.593, 1.64) | 0.96 | - | 0.784 (0.436, 1.150) | 0.35 |
| Age | 0.989 (0.958, 1.02) | 0.47 | - | 0.985 (0.953, 1.02) | 0.37 | - | 0.991 (0.960, 1.020) | 0.56 |
| BMI | 0.984 (0.928, 1.04) | 0.60 | - | 1.050 (0.983, 1.12) | 0.15 | - | 0.999 (0.921, 1.080) | 0.99 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benjamin, J.; Maillard, L.; Morelec, I.; Got, P.; Borson-Chazot, F.; Lifante, J.-C. Diagnostic Performance of 18F-Choline Positron Emission Tomography/Contrast-Enhanced Computed Tomography in Adenoma Detection in Primary Hyperparathyroidism after Inconclusive Imaging: A Retrospective Study of 215 Patients. Cancers 2022, 14, 2029. https://doi.org/10.3390/cancers14082029
Benjamin J, Maillard L, Morelec I, Got P, Borson-Chazot F, Lifante J-C. Diagnostic Performance of 18F-Choline Positron Emission Tomography/Contrast-Enhanced Computed Tomography in Adenoma Detection in Primary Hyperparathyroidism after Inconclusive Imaging: A Retrospective Study of 215 Patients. Cancers. 2022; 14(8):2029. https://doi.org/10.3390/cancers14082029
Chicago/Turabian StyleBenjamin, Johan, Laure Maillard, Isabelle Morelec, Philippe Got, Françoise Borson-Chazot, and Jean-Christophe Lifante. 2022. "Diagnostic Performance of 18F-Choline Positron Emission Tomography/Contrast-Enhanced Computed Tomography in Adenoma Detection in Primary Hyperparathyroidism after Inconclusive Imaging: A Retrospective Study of 215 Patients" Cancers 14, no. 8: 2029. https://doi.org/10.3390/cancers14082029
APA StyleBenjamin, J., Maillard, L., Morelec, I., Got, P., Borson-Chazot, F., & Lifante, J.-C. (2022). Diagnostic Performance of 18F-Choline Positron Emission Tomography/Contrast-Enhanced Computed Tomography in Adenoma Detection in Primary Hyperparathyroidism after Inconclusive Imaging: A Retrospective Study of 215 Patients. Cancers, 14(8), 2029. https://doi.org/10.3390/cancers14082029







