Worldwide Burden, Risk Factors, and Temporal Trends of Ovarian Cancer: A Global Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Statistical Analysis
3. Results
3.1. Global Incidence of Ovarian Cancer in 2020
3.2. Global Mortality of Ovarian Cancer in 2020
3.3. Associations between Risk Factors and Incidence
3.4. Associations between Risk Factors and Mortality
3.5. Temporal Trends of Ovarian Cancer
3.6. Overall Incidence Trends of Ovarian Cancer
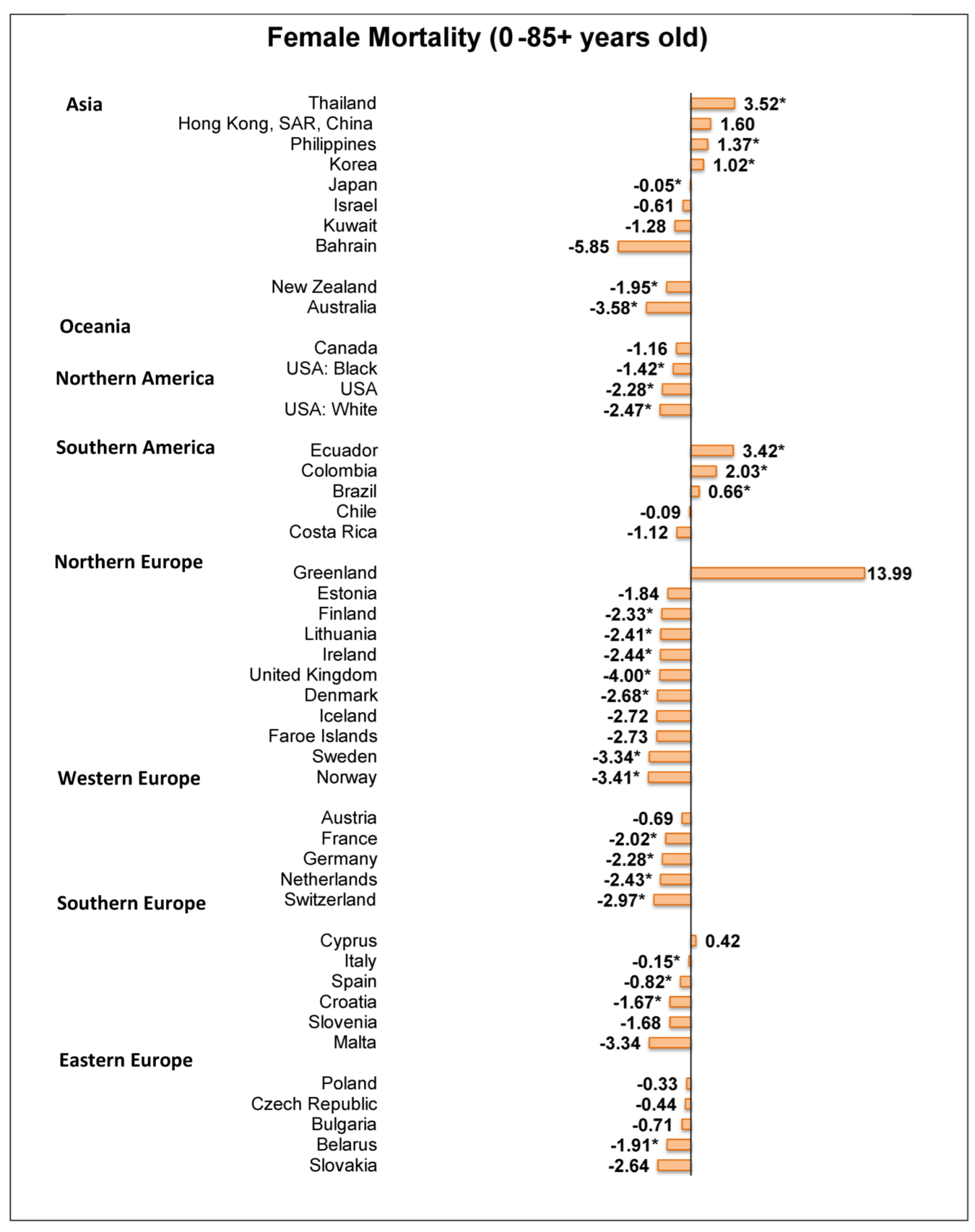
3.7. Overall Mortality Trends of Ovarian Cancer
3.8. Incidence Trends of Ovarian Cancer in Females Aged ≥ 50
3.9. Incidence Trends of Ovarian Cancer in Females Aged < 50
3.10. Incidence Trends of Ovarian Cancer in Females Aged < 40
4. Discussion
4.1. Summary of Main Findings
4.2. Explanation of Findings and Relationship with Literature
5. Limitation
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AAPC | Average annual percent change |
| APC | Annual percentage change |
| ASR | Age-standardized rates |
| CI | Confidence interval |
| CI5 | Cancer Incidence in Five Continents |
| GDP | Gross domestic products |
| GHDx | Global Health Data Exchange |
| HDI | Human Development Index |
| IARC | International Agency for Research on Cancer |
| NORDCAN | Nordic Cancer Registries |
| RR | Relative risk |
| SEER | Surveillance, Epidemiology, and End Results |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Jayson, G.C.; Kohn, E.C.; Kitchener, H.C.; Ledermann, J.A. Ovarian cancer. Lancet 2014, 384, 1376–1388. [Google Scholar] [CrossRef]
- Baldwin, L.A.; Huang, B.; Miller, R.W.; Tucker, T.; Goodrich, S.T.; Podzielinski, I.; DeSimone, C.P.; Ueland, F.R.; van Nagell, J.R.; Seamon, L.G. Ten-year relative survival for epithelial ovarian cancer. Obs. Gynecol. 2012, 120, 612–618. [Google Scholar] [CrossRef]
- Momenimovahed, Z.; Tiznobaik, A.; Taheri, S.; Salehiniya, H. Ovarian cancer in the world: Epidemiology and risk factors. Int. J. Womens Health 2019, 11, 287–299. [Google Scholar] [CrossRef] [Green Version]
- Salehi, F.; Dunfield, L.; Phillips, K.P.; Krewski, D.; Vanderhyden, B.C. Risk factors for ovarian cancer: An overview with emphasis on hormonal factors. J. Toxicol. Environ. Health B Crit. Rev. 2008, 11, 301–321. [Google Scholar] [CrossRef]
- Webb, P.M.; Jordan, S.J. Epidemiology of epithelial ovarian cancer. Best Pract. Res. Clin. Obstet. Gynaecol. 2017, 41, 3–14. [Google Scholar] [CrossRef] [Green Version]
- Torre, L.A.; Trabert, B.; DeSantis, C.E.; Miller, K.D.; Samimi, G.; Runowicz, C.D.; Gaudet, M.M.; Jemal, A.; Siegel, R.L. Ovarian cancer statistics, 2018. CA A Cancer J. Clin. 2018, 68, 284–296. [Google Scholar] [CrossRef]
- Wei, K.; Li, Y.; Zheng, R.; Zhang, S.; Liang, Z.; Cen, H.; Chen, W. Ovary cancer incidence and mortality in China, 2011. Chin. J. Cancer Res. 2015, 27, 38–43. [Google Scholar] [CrossRef]
- Zhang, Y.; Luo, G.; Li, M.; Guo, P.; Xiao, Y.; Ji, H.; Hao, Y. Global patterns and trends in ovarian cancer incidence: Age, period and birth cohort analysis. BMC Cancer 2019, 19, 984. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer; WHO. Data Visualization Tools for Exploring the Global Cancer Burden in 2020. 2020. Available online: https://gco.iarc.fr/today/home (accessed on 10 November 2021).
- Observatory, G.C. Fact Sheet: Brain, Central Nervous System. 2021. Available online: https://gco.iarc.fr/today/data/factsheets/cancers/31-Brain-central-nervous-system-fact-sheet.pdf (accessed on 15 July 2021).
- Global Health Data Exchange. Available online: https://ghdx.healthdata.org/ (accessed on 15 July 2021).
- Bray, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Zanetti, R.; Ferlay, J. Cancer Incidence in Five Continents, Vol. XI (Electronic Version) Lyon: International Agency for Research on Cancer. 2020. Available online: https://ci5.iarc.fr (accessed on 10 May 2020).
- World Health Organization. WHO Mortality Database. 2021. Available online: https://www.who.int/healthinfo/mortality_data/en/ (accessed on 10 May 2021).
- Danckert, B.F.J.; Engholm, G.; Hansen, H.L.; Johannesen, T.B.; Khan, S.; Køtlum, J.E.; Ólafsdóttir, E.; Schmidt, L.K.H.; Virtanen, A.; Storm, H.H. NORDCAN: Cancer Incidence, Mortality, Prevalence and Survival in the Nordic Countries, Version 8.2. (26 March 2019). Available online: https://www-dep.iarc.fr/NORDCAN/english/frame.asp (accessed on 10 May 2021).
- Engholm, G.; Ferlay, J.; Christensen, N.; Bray, F.; Gjerstorff, M.L.; Klint, A.; Kotlum, J.E.; Olafsdottir, E.; Pukkala, E.; Storm, H.H. NORDCAN—A Nordic tool for cancer information, planning, quality control and research. Acta. Oncol. 2010, 49, 725–736. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services, N.I.o.H. Surveillance, Epidemiology, and End Results (SEER) Program. 2020. Available online: https://seer.cancer.gov/about/ (accessed on 10 May 2021).
- WHO. International Statistical Classification of Diseases and Related Health Problems 10th Revision. 2019 Edition. Available online: https://icd.who.int/browse10/2019/en#/C53 (accessed on 21 July 2021).
- Arnold, M.; Sierra, M.S.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017, 66, 683–691. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.J.; Fay, M.P.; Feuer, E.J.; Midthune, D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2000, 19, 335–351. [Google Scholar] [CrossRef]
- Clegg, L.X.; Hankey, B.F.; Tiwari, R.; Feuer, E.J.; Edwards, B.K. Estimating average annual percent change in trend analysis. Stat. Med. 2009, 28, 3670–3682. [Google Scholar] [CrossRef] [Green Version]
- La Vecchia, C. Ovarian cancer: Epidemiology and risk factors. Eur. J. Cancer Prev. 2017, 26, 55–62. [Google Scholar] [CrossRef]
- Haier, J.; Sleeman, J.; Schäfers, J. Editorial series: Cancer care in low- and middle-income countries. Clin. Exp. Metastasis 2019, 36, 477–480. [Google Scholar] [CrossRef] [Green Version]
- Beral, V.; Gaitskell, K.; Hermon, C.; Moser, K.; Reeves, G.; Peto, R. Ovarian cancer and smoking: Individual participant meta-analysis including 28,114 women with ovarian cancer from 51 epidemiological studies. Lancet Oncol. 2012, 13, 946–956. [Google Scholar] [CrossRef]
- Chang, E.T.; Canchola, A.J.; Lee, V.S.; Clarke, C.A.; Purdie, D.M.; Reynolds, P.; Bernstein, L.; Stram, D.O.; Anton-Culver, H.; Deapen, D.; et al. Wine and other alcohol consumption and risk of ovarian cancer in the California Teachers Study cohort. Cancer Causes Control 2007, 18, 91–103. [Google Scholar] [CrossRef] [Green Version]
- Cottreau, C.M.; Ness, R.B.; Kriska, A.M. Physical activity and reduced risk of ovarian cancer. Obstet. Gynecol. 2000, 96, 609–614. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, T.T.; Zhao, J.J.; Qi, S.F.; Du, P.; Liu, D.W.; Tian, Q.B. The association between overweight, obesity and ovarian cancer: A meta-analysis. Jpn. J. Clin. Oncol. 2015, 45, 1107–1115. [Google Scholar] [CrossRef] [Green Version]
- Huang, J.; Huang, J.L.W.; Wang, J.; Chung, V.C.H.; Wong, M.C.S. Metabolic syndrome and risk of cancer in Chinese populations: A systematic review and meta-analysis in 57,260 individuals. Lancet 2018, 392, S15. [Google Scholar] [CrossRef]
- Ng, M.; Freeman, M.K.; Fleming, T.D.; Robinson, M.; Dwyer-Lindgren, L.; Thomson, B.; Wollum, A.; Sanman, E.; Wulf, S.; Lopez, A.D.; et al. Smoking Prevalence and Cigarette Consumption in 187 Countries, 1980–2012. JAMA 2014, 311, 183–192. [Google Scholar] [CrossRef] [Green Version]
- Bray, F.; Loos, A.H.; Tognazzo, S.; La Vecchia, C. Ovarian cancer in Europe: Cross-sectional trends in incidence and mortality in 28 countries, 1953–2000. Int. J. Cancer 2005, 113, 977–990. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Huang, J.; Wang, J.; Chan, P.S.F.; Lok, V.; Chen, X.; Leung, C.; Wang, H.H.X.; Lao, X.Q.; Zheng, Z.-J. Global, regional and time-trend prevalence of central obesity: A systematic review and meta-analysis of 13.2 million subjects. Eur. J. Epidemiol. 2020, 35, 673–683. [Google Scholar] [CrossRef]
- Wong, M.C.; Huang, J.; Pang, T.W.; Lok, V.; Chen, X.; Choi, P.; Wang, H.H.-X.; Zheng, Z.-J. Tu1007 Worldwide Incidence and Prevalence of Metabolic Syndrome: A Systematic Review and Meta-Analysis of 14.6 Million Individuals. Gastroenterology 2020, 158, S-1003. [Google Scholar] [CrossRef]
- Rosenberg, S.M.; Ruddy, K.J.; Tamimi, R.M.; Gelber, S.; Schapira, L.; Come, S.; Borges, V.F.; Larsen, B.; Garber, J.E.; Partridge, A.H. BRCA1 and BRCA2 Mutation Testing in Young Women with Breast Cancer. JAMA Oncol. 2016, 2, 730–736. [Google Scholar] [CrossRef] [Green Version]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, J.; Chan, W.C.; Ngai, C.H.; Lok, V.; Zhang, L.; Lucero-Prisno, D.E., III; Xu, W.; Zheng, Z.-J.; Elcarte, E.; Withers, M.; et al. Worldwide Burden, Risk Factors, and Temporal Trends of Ovarian Cancer: A Global Study. Cancers 2022, 14, 2230. https://doi.org/10.3390/cancers14092230
Huang J, Chan WC, Ngai CH, Lok V, Zhang L, Lucero-Prisno DE III, Xu W, Zheng Z-J, Elcarte E, Withers M, et al. Worldwide Burden, Risk Factors, and Temporal Trends of Ovarian Cancer: A Global Study. Cancers. 2022; 14(9):2230. https://doi.org/10.3390/cancers14092230
Chicago/Turabian StyleHuang, Junjie, Wing Chung Chan, Chun Ho Ngai, Veeleah Lok, Lin Zhang, Don Eliseo Lucero-Prisno, III, Wanghong Xu, Zhi-Jie Zheng, Edmar Elcarte, Mellissa Withers, and et al. 2022. "Worldwide Burden, Risk Factors, and Temporal Trends of Ovarian Cancer: A Global Study" Cancers 14, no. 9: 2230. https://doi.org/10.3390/cancers14092230
APA StyleHuang, J., Chan, W. C., Ngai, C. H., Lok, V., Zhang, L., Lucero-Prisno, D. E., III, Xu, W., Zheng, Z. -J., Elcarte, E., Withers, M., Wong, M. C. S., & on behalf of NCD Global Health Research Group of Association of Pacific Rim Universities (APRU). (2022). Worldwide Burden, Risk Factors, and Temporal Trends of Ovarian Cancer: A Global Study. Cancers, 14(9), 2230. https://doi.org/10.3390/cancers14092230










