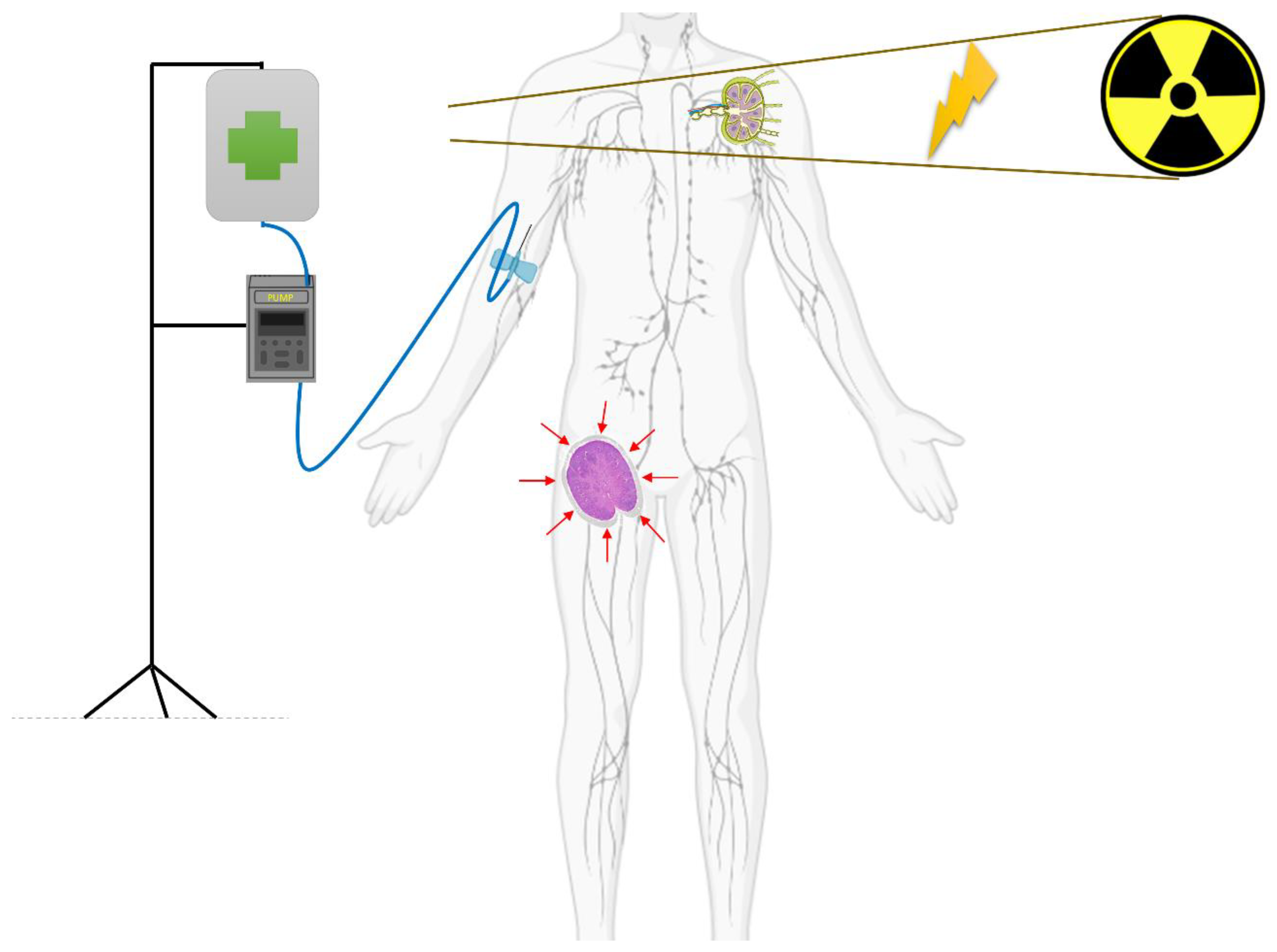
Novel Drugs and Radiotherapy in Relapsed Lymphomas: Abscopal Response and Beyond
Abstract
:Simple Summary
Abstract
1. Introduction: Radiation Therapy and Mechanisms of Immunomodulation
2. Radiotherapy and Checkpoint Inhibitors: Boosting the Abscopal Effect
3. Radiotherapy and Small-Molecule Inhibitors
4. Radiotherapy and Brentuximab Vedotin
5. Radiotherapy and CAR-T
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kostopoulos, N.; Bedgi, S.; Krimitza, E.; Costabile, F.; Paydar, I.; Kim, M.M.; LaRiviere, M.J.; Maity, A.; Schuster, S.; Plastaras, J.P.; et al. Radiation Therapy for Bridging and Improving CAR-T Cell Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2022, 114, S83–S84. [Google Scholar] [CrossRef]
- Zhu, M.; Yang, M.; Zhang, J.; Yin, Y.; Fan, X.; Zhang, Y.; Qin, S.; Zhang, H.; Yu, F. Immunogenic Cell Death Induction by Ionizing Radiation. Front. Immunol. 2021, 12, 705361. [Google Scholar] [CrossRef]
- Chao, M.P.; Jaiswal, S.; Weissman-Tsukamoto, R.; Alizadeh, A.A.; Gentles, A.J.; Volkmer, J.; Weiskopf, K.; Willingham, S.B.; Raveh, T.; Park, C.Y.; et al. Calreticulin is the dominant pro-phagocytic signal on multiple human cancers and is counterbalanced by CD47. Sci. Transl. Med. 2010, 2, 63ra94. [Google Scholar] [CrossRef]
- Zhang, Z.; Liu, X.; Chen, D.; Yu, J. Radiotherapy combined with immunotherapy: The dawn of cancer treatment. Signal Transduct. Target. Ther. 2022, 7, 258. [Google Scholar] [CrossRef]
- Liao, Y.; Liu, S.; Fu, S.; Wu, J. HMGB1 in Radiotherapy: A Two Headed Signal Regulating Tumor Radiosensitivity and Immunity. OncoTargets Ther. 2020, 13, 6859–6871. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.; Liang, H.; Xu, M.; Yang, X.; Burnette, B.; Arina, A.; Li, X.-D.; Mauceri, H.; Beckett, M.; Darga, T.; et al. STING-dependent Cytosolic DNA Sensing Promotes Radiation-induced Type I interferon-dependent Antitumor Immunity in Immunogenic Tumors. Immunity 2014, 41, 843–852. [Google Scholar] [CrossRef] [PubMed]
- Ngwa, W.; Irabor, O.C.; Schoenfeld, J.D.; Hesser, J.; Demaria, S.; Formenti, S.C. Using immunotherapy to boost the abscopal effect. Nat. Rev. Cancer 2018, 18, 313–322. [Google Scholar] [CrossRef]
- Baxevanis, C.N.; Gritzapis, A.D.; Voutsas, I.F.; Batsaki, P.; Goulielmaki, M.; Adamaki, M.; Zoumpourlis, V.; Fortis, S.P. T-Cell Repertoire in Tumor Radiation: The Emerging Frontier as a Radiotherapy Biomarker. Cancers 2022, 14, 2674. [Google Scholar] [CrossRef]
- Yu, N.; Wang, S.; Song, X.; Gao, L.; Li, W.; Yu, H.; Zhou, C.; Wang, Z.; Li, F.; Jiang, Q. Low-Dose Radiation Promotes Dendritic Cell Migration and IL-12 Production via the ATM/NF-KappaB Pathway. Radiat. Res. 2018, 189, 409–417. [Google Scholar] [CrossRef]
- Fang, X.; Guo, Z.; Liang, J.; Wen, J.; Liu, Y.; Guan, X.; Li, H. Neoantigens and their potential applications in tumor immunotherapy (Review). Oncol. Lett. 2022, 23, 88. [Google Scholar] [CrossRef]
- McLaughlin, M.; Patin, E.C.; Pedersen, M.; Wilkins, A.; Dillon, M.T.; Melcher, A.A.; Harrington, K.J. Inflammatory microenvironment remodelling by tumour cells after radiotherapy. Nat. Rev. Cancer 2020, 20, 203–217. [Google Scholar] [CrossRef] [PubMed]
- Burdak-Rothkamm, S.; Rothkamm, K. Radiation-induced bystander and systemic effects serve as a unifying model system for genotoxic stress responses. Mutat. Res. Rev. Mutat. Res. 2018, 778, 13–22. [Google Scholar] [CrossRef]
- Williamson, C.W.; Sherer, M.V.; Zamarin, D.; Sharabi, A.B.; Dyer, B.A.; Mell, L.K.; Mayadev, J.S. Immunotherapy and radiation therapy sequencing: State of the data on timing, efficacy, and safety. Cancer 2021, 127, 1553–1567. [Google Scholar] [CrossRef]
- Guerini, A.E.; Filippi, A.R.; Tucci, A.; Simontacchi, G.; Re, A.; Guaineri, A.; Morelli, V.; Borghetti, P.; Triggiani, L.; Pegurri, L.; et al. ‘Le Roi est mort, vive le Roi’: New Roles of Radiotherapy in the Treatment of Lymphomas in Combination With Immunotherapy. Clin. Lymphoma Myeloma Leuk. 2022, 22, e135–e148. [Google Scholar] [CrossRef] [PubMed]
- Bröckelmann, P.; Bühnen, I.; Zijlstra, J.; Fossa, A.; Meissner, J.; Mathas, S.; Rosenbrock, J.; Kobe, C.; Fuchs, M.; Plütschow, A.; et al. S203: Abscopal Effect of Radiotherapy and Nivolumab in Relapsed or Refractory Hodgkin Lymphoma: Pre-Planned Interim Analysis of the International GHSG Phase II Aern Trial. HemaSphere 2022, 6, 104–105. [Google Scholar] [CrossRef]
- Shree, T.; Haebe, S.; Czerwinski, D.K.; Eckhert, E.; Day, G.; Sathe, A.; Grimes, S.M.; Frank, M.J.; Maeda, L.S.; Alizadeh, A.A.; et al. Activating Immune Effectors and Dampening Immune Suppressors Generates Successful Therapeutic Cancer Vaccination in Patients with Lymphoma. Blood 2022, 140, 6450–6451. [Google Scholar] [CrossRef]
- Chen, D.S.; Mellman, I. Oncology meets immunology: The cancer-immunity cycle. Immunity 2013, 39, 543. [Google Scholar] [CrossRef]
- Yao, S.; Zhu, Y.; Chen, L. Advances in targeting cell surface signalling molecules for immune modulation. Nat. Rev. Drug Discov. 2013, 12, 130–146. [Google Scholar] [CrossRef]
- Motz, G.T.; Coukos, G. Deciphering and reversing tumor immune suppression. Immunity 2013, 39, 61–73. [Google Scholar] [CrossRef]
- Quail, D.F.; Joyce, J.A. Microenvironmental regulation of tumor progression and metastasis. Nat. Med. 2013, 19, 1423–1437. [Google Scholar] [CrossRef]
- Ishida, Y.; Agata, Y.; Shibahara, K.; Honjo, T. Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. EMBO J. 1992, 11, 3887–3895. [Google Scholar] [CrossRef] [PubMed]
- Yao, S.; Chen, L. Reviving exhausted T lymphocytes during chronic virus infection by B7-H1 blockade. Trends Mol. Med. 2006, 12, 244–246. [Google Scholar] [CrossRef] [PubMed]
- Butte, M.J.; Keir, M.E.; Phamduy, T.B.; Sharpe, A.H.; Freeman, G.J. Programmed death-1 ligand 1 interacts specifically with the B7-1 costimulatory molecule to inhibit T cell responses. Immunity 2007, 27, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Zou, W.; Chen, L. Inhibitory B7-family molecules in the tumour microenvironment. Nat. Rev. Immunol. 2008, 8, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Strome, S.E.; Salomao, D.R.; Tamura, H.; Hirano, F.; Flies, D.B.; Roche, P.C.; Lu, J.; Zhu, G.; Tamada, K.; et al. Tumor-associated B7-H1 promotes T-cell apoptosis: A potential mechanism of immune evasion. Nat. Med. 2002, 8, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Martelli, M.; Di Rocco, A.; Russo, E.; Perrone, S.; Foà, R. Primary mediastinal lymphoma: Diagnosis and treatment options. Expert Rev. Hematol. 2015, 8, 173–186. [Google Scholar] [CrossRef]
- Lee, J.Y.; Lee, H.T.; Shin, W.; Chae, J.; Choi, J.; Kim, S.H.; Lim, H.; Won Heo, T.; Park, K.Y.; Lee, Y.J.; et al. Structural basis of checkpoint blockade by monoclonal antibodies in cancer immunotherapy. Nat. Commun. 2016, 7, 13354. [Google Scholar] [CrossRef]
- Fessas, P.; Lee, H.; Ikemizu, S.; Janowitz, T. A molecular and preclinical comparison of the PD-1-targeted T-cell checkpoint inhibitors nivolumab and pembrolizumab. Semin. Oncol. 2017, 44, 136–140. [Google Scholar] [CrossRef]
- Younes, A.; Santoro, A.; Shipp, M.; Zinzani, P.L.; Timmerman, J.M.; Ansell, S.; Armand, P.; Fanale, M.; Ratanatharathorn, V.; Kuruvilla, J.; et al. Nivolumab for classical Hodgkin’s lymphoma after failure of both autologous stem-cell transplantation and brentuximab vedotin: A multicentre, multicohort, single-arm phase 2 trial. Lancet Oncol. 2016, 17, 1283–1294. [Google Scholar] [CrossRef]
- Kuruvilla, J.; Ramchandren, R.; Santoro, A.; Paszkiewicz-Kozik, E.; Gasiorowski, R.; Johnson, N.A.; Fogliatto, L.M.; Goncalves, I.; de Oliveira, J.S.R.; Buccheri, V.; et al. Pembrolizumab versus brentuximab vedotin in relapsed or refractory classical Hodgkin lymphoma (KEYNOTE-204): An interim analysis of a multicentre, randomised, open-label, phase 3 study. Lancet Oncol. 2021, 22, 512–524. [Google Scholar] [CrossRef]
- Armand, P.; Rodig, S.; Melnichenko, V.; Thieblemont, C.; Bouabdallah, K.; Tumyan, G.; Özcan, M.; Portino, S.; Fogliatto, L.; Caballero, M.D.; et al. Pembrolizumab in Relapsed or Refractory Primary Mediastinal Large B-Cell Lymphoma. J. Clin. Oncol. 2019, 37, 3291–3299. [Google Scholar] [CrossRef]
- Modi, D.; Potugari, B.; Uberti, J. Immunotherapy for Diffuse Large B-Cell Lymphoma: Current Landscape and Future Directions. Cancers 2021, 13, 5827. [Google Scholar] [CrossRef] [PubMed]
- Ansell, S.M.; Minnema, M.C.; Johnson, P.; Timmerman, J.M.; Armand, P.; Shipp, M.A.; Rodig, S.J.; Ligon, A.H.; Roemer, M.G.M.; Reddy, N.; et al. Nivolumab for relapsed/refractory diffuse large B-cell lymphoma in patients ineligible for or having failed autologous transplantation: A single-arm, phase II study. J. Clin. Oncol. 2019, 37, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Frigault, M.J.; Armand, P.; Redd, R.A.; Jeter, E.; Merryman, R.W.; Coleman, K.C.; Herrera, A.F.; Dahi, P.; Nieto, Y.; LaCasce, A.S.; et al. PD-1 blockade for diffuse large B-cell lymphoma after autologous stem cell transplantation. Blood Adv. 2020, 4, 122–126. [Google Scholar] [CrossRef] [PubMed]
- Ansell, S.M. The highs and lows of immune-checkpoint blockade in lymphoma. Cancer Immunol. Res. 2019, 7, 696–700. [Google Scholar] [CrossRef]
- Scott, D.W.; Gascoyne, R.D. The tumour microenvironment in B cell lymphomas. Nat. Rev. Cancer 2014, 14, 517–534. [Google Scholar] [CrossRef]
- Green, M.R.; Monti, S.; Rodig, S.J.; Juszczynski, P.; Currie, T.; O’Donnell, E.; Chapuy, B.; Takeyama, K.; Neuberg, D.; Golub, T.R.; et al. Integrative analysis reveals selective 9p24.1 amplification, increased PD-1 ligand expression, and further induction via JAK2 in nodular sclerosing Hodgkin lymphoma and primary mediastinal large B-cell lymphoma. Blood 2010, 116, 3268–3277. [Google Scholar] [CrossRef]
- Quéro, L.; Gilardin, L.; Fumagalli, I.; Martin, V.; Guillerm, S.; Bauduceau, O.; Kirova, Y.M.; Hennequin, C.; Brice, P. Anti-PD-1 immunotherapy in combination with sequential involved-site radiotherapy in heavily pretreated refractory Hodgkin lymphoma. Cancer/Radiothérapie 2019, 23, 132–137. [Google Scholar] [CrossRef] [PubMed]
- de Forceville, L.; Deau-Fischer, B.; Franchi, P.; Arsène-Henry, A.; Cassou Mounat, T.; Bouscary, D.; Kirova, Y.M. Radiotherapy in combination with nivolumab for relapsed/refractory classical Hodgkin lymphoma: About two cases. Cancer Radiother. 2019, 23, 232–239. [Google Scholar] [CrossRef]
- Lucchini, E.; Rusconi, C.; Levis, M.; Ricci, F.; Santoro, A.; Ricardi, U.; Volpetti, S.; Matrone, F.; di Russo, A.; Caizzi, M.; et al. Immune checkpoint inhibitors in combination with radiotherapy as salvage treatment for relapsed/refractory classical Hodgkin lymphoma: A retrospective analysis in 12 patients. Hematol. Rep. 2021, 13, 9080. [Google Scholar] [CrossRef]
- Bröckelmann, P.J.; Plütschow, A.; Greil, R.; Zijlstra, J.M.; Illidge, T.; Fosså, A.; Meissner, J.; Zimmermann, A.; Mathas, S.; Thol, F.; et al. Abscopal Effect of Radiotherapy and Nivolumab in Relapsed or Refractory Hodgkin Lymphoma (AERN): An International Multicenter Single-Arm Two-Stage Phase II GHSG Trial. Blood 2019, 134, 1547. [Google Scholar] [CrossRef]
- Pinnix, C.C.; Dabaja, B.S.; Gunther, J.R.; Fang, P.; Wu, S.; Ahmed, S.; Steiner, R.E.; Nair, R.; Strati, P.; Westin, J.; et al. Phase II Study of Pembrolizumab and Fractionated External Beam Radiotherapy in Patients with Relapsed and Refractory Large B-Cell Lymphoma. Blood 2022, 140, 3741–3743. [Google Scholar] [CrossRef]
- LaRiviere, M.J.; Vaziri, T.; Farwell, M.; Maity, A.; Paydar, I.; Schuster, S.J.; Dwivedy Nasta, S.; Chong, E.A.; Landsburg, D.J.; Plastaras, J.P.; et al. Low-Dose Radiation Therapy with Nivolumab in Patients with Relapsed/Refractory Hodgkin Lymphoma: Results of the Phase II Radvax Trial. Blood 2022, 140, 3726–3727. [Google Scholar] [CrossRef]
- Herrera, F.G.; Ronet, C.; Ochoa de Olza, M.; Barras, D.; Crespo, I.; Andreatta, M.; Corria-Osorio, J.; Spill, A.; Benedetti, F.; Genolet, R.; et al. Low-Dose Radiotherapy Reverses Tumor Immune Desertification and Resistance to Immunotherapy. Cancer Discov. 2022, 12, 108–133. [Google Scholar] [CrossRef] [PubMed]
- Brooks, E.D.; Chang, J.Y. Time to abandon single-site irradiation for inducing abscopal effects. Nat. Rev. Clin. Oncol. 2019, 16, 123–135. [Google Scholar] [CrossRef]
- Norbury, C.J.; Zhivotovsky, B. DNA damage-induced apoptosis. Oncogene 2004, 23, 2797–2808. [Google Scholar] [CrossRef]
- Punnoose, E.A.; Leverson, J.D.; Peale, F.; Boghaert, E.R.; Belmont, L.D.; Tan, N.; Young, A.; Mitten, M.; Ingalla, E.; Darbonne, W.C.; et al. Expression Profile of BCL-2, BCL-XL, and MCL-1 Predicts Pharmacological Response to the BCL-2 Selective Antagonist Venetoclax in Multiple Myeloma Models. Mol. Cancer Ther. 2016, 15, 1132–1144. [Google Scholar] [CrossRef] [PubMed]
- Bose, P.; Gandhi, V.; Konopleva, M. Pathways and mechanisms of venetoclax resistance. Leuk. Lymphoma 2017, 58, 1–17. [Google Scholar] [CrossRef]
- O’Steen, S.; Green, D.J.; Gopal, A.K.; Orozco, J.J.; Kenoyer, A.L.; Lin, Y.; Wilbur, D.S.; Hamlin, D.K.; Fisher, D.R.; Hylarides, M.D.; et al. Venetoclax Synergizes with Radiotherapy for Treatment of B-cell Lymphomas. Cancer Res. 2017, 77, 3885–3893. [Google Scholar] [CrossRef]
- Iqbal, J.; Neppalli, V.T.; Wright, G.; Dave, B.J.; Horsman, D.E.; Rosenwald, A.; Lynch, J.; Hans, C.P.; Weisenburger, D.D.; Greiner, T.C.; et al. BCL2 expression is a prognostic marker for the activated B-cell-like type of diffuse large B-cell lymphoma. J. Clin. Oncol. 2006, 24, 961–968. [Google Scholar] [CrossRef]
- Adams, C.M.; Mitra, R.; Gong, J.Z.; Eischen, C.M. Non-Hodgkin and Hodgkin lymphomas select for overexpression of BCLW. Clin. Cancer Res. 2017, 23, 7119–7129. [Google Scholar] [CrossRef]
- Ho, C.I.; Ballard, H.J.; Arscott, W.T.; Hughes, M.E.; Doucette, A.; Landsburg, D.J.; Dwivedy Nasta, S.; Gerson, J.N.; Maity, A.; Schuster, S.J.; et al. Concurrent Use of Novel Agents and Radiation Is Tolerated in Lymphoma Patients. Blood 2019, 134, 2905. [Google Scholar] [CrossRef]
- Ning, M.S.; Pinnix, C.C.; Chapman, B.V.; Gunther, J.R.; Milgrom, S.A.; Khoury, J.D.; Jain, P.; Chen, W.Y.; Oriabure, O.N.; Badillo, M.R.; et al. Low-dose radiation (4 Gy) with/without concurrent chemotherapy is highly effective for relapsed, refractory mantle cell lymphoma. Blood Adv. 2019, 3, 2035–2039. [Google Scholar] [CrossRef]
- Bohli, M.; Jaffel, H.; El Fida Noubbigh, G.; Tbessi, S.; Msadek, F.; Kochbati, L. Synergistic Effect and Tolerance of Concurrent Radiotherapy and Lenalidomide Use in Relapsing Mantle Cell Lymphoma: A Case Report. Perm. J. 2020, 24, 2026–2039. [Google Scholar] [CrossRef]
- Mancebo, S.E.; Smith, J.R.; Intlekofer, A.M.; Zelenetz, A.D.; Myskowski, P.L. Treatment Response of Cutaneous Mantle Cell Lymphoma to Ibrutinib and Radiotherapy. Clin. Lymphoma Myeloma Leuk. 2015, 15, e113–e115. [Google Scholar] [CrossRef]
- Chapuy, B.; Roemer, M.G.M.; Stewart, C.; Tan, Y.; Abo, R.P.; Zhang, L.; Dunford, A.J.; Meredith, D.M.; Thorner, A.R.; Jordanova, E.S.; et al. Targetable genetic features of primary testicular and primary central nervous system lymphomas. Blood 2016, 127, 869–881. [Google Scholar] [CrossRef] [PubMed]
- Wilson, W.H.; Young, R.M.; Schmitz, R.; Yang, Y.; Pittaluga, S.; Wright, G.; Lih, C.-J.; Williams, P.M.; Shaffer, A.L.; Gerecitano, J.; et al. Targeting B cell receptor signaling with ibrutinib in diffuse large B cell lymphoma. Nat. Med. 2015, 21, 922–926. [Google Scholar] [CrossRef] [PubMed]
- Lauer, E.M.; Waterhouse, M.; Braig, M.; Mutter, J.; Bleul, S.; Duque-Afonso, J.; Duyster, J.; Marks, R.; Reinacher, P.C.; Prinz, M.; et al. Ibrutinib in patients with relapsed/refractory central nervous system lymphoma: A retrospective single-centre analysis. Br. J. Haematol. 2020, 190, e110–e114. [Google Scholar] [CrossRef]
- Lewis, K.L.; Chin, C.K.; Manos, K.; Casey, J.; Hamad, N.; Crawford, J.; Ho, S.-J.; Issa, S.; Grigg, A.; Wood, P.; et al. Ibrutinib for central nervous system lymphoma: The Australasian Lymphoma Alliance/MD Anderson Cancer Center experience. Br. J. Haematol. 2021, 192, 1049–1053. [Google Scholar] [CrossRef] [PubMed]
- Lv, L.; Sun, X.; Wu, Y.; Cui, Q.; Chen, Y.; Liu, Y. Efficacy and Safety of Ibrutinib in Central Nervous System Lymphoma: A PRISMA-Compliant Single-Arm Meta-Analysis. Front. Oncol. 2021, 11, 707285. [Google Scholar] [CrossRef]
- Francisco, J.A.; Cerveny, C.G.; Meyer, D.L.; Mixan, B.J.; Klussman, K.; Chace, D.F.; Rejniak, S.X.; Gordon, K.A.; DeBlanc, R.; Toki, B.E.; et al. cAC10-vcMMAE, an anti-CD30-monomethyl auristatin E conjugate with potent and selective antitumor activity. Blood 2003, 102, 1458–1465. [Google Scholar] [CrossRef]
- Dürkop, H.; Latza, U.; Hummel, M.; Eitelbach, F.; Seed, B.; Stein, H. Molecular cloning and expression of a new member of the nerve growth factor receptor family that is characteristic for Hodgkin’s disease. Cell 1992, 68, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Falini, B.; Pileri, S.; Pizzolo, G.; Dürkop, H.; Flenghi, L.; Stirpe, F.; Martelli, M.F.; Stein, H. CD30 (Ki-1) molecule: A new cytokine receptor of the tumor necrosis factor receptor superfamily as a tool for diagnosis and immunotherapy. Blood 1995, 85, 1–14. [Google Scholar] [CrossRef]
- Matsumoto, K.; Terakawa, M.; Miura, K.; Fukuda, S.; Nakajima, T.; Saito, H. Extremely rapid and intense induction of apoptosis in human eosinophils by anti-CD30 antibody treatment in vitro. J. Immunol. 2004, 172, 2186–2193. [Google Scholar] [CrossRef] [PubMed]
- Sabattini, E.; Pizzi, M.; Tabanelli, V.; Baldin, P.; Sacchetti, C.S.; Agostinelli, C.; Zinzani, P.L.; Pileri, S.A. CD30 expression in peripheral T-cell lymphomas. Haematologica 2013, 98, e81–e82. [Google Scholar] [CrossRef]
- Federico, M.; Luminari, S.; Pellegrini, C.; Merli, F.; Pesce, E.A.; Chauvie, S.; Gandolfi, L.; Capodanno, I.; Salati, M.; Argnani, L.; et al. Brentuximab vedotin followed by ABVD +/− radiotherapy in patients with previously untreated Hodgkin lymphoma: Final results of a pilot phase II study. Haematologica 2016, 101, e139–e141. [Google Scholar] [CrossRef] [PubMed]
- Metzger, M.L.; Link, M.P.; Billett, A.L.; Flerlage, J.; Lucas, J.T.; Mandrell, B.N.; Ehrhardt, M.J.; Bhakta, N.; Yock, T.I.; Friedmann, A.M.; et al. Excellent Outcome for Pediatric Patients With High-Risk Hodgkin Lymphoma Treated With Brentuximab Vedotin and Risk-Adapted Residual Node Radiation. J. Clin. Oncol. 2021, 39, 2276–2283. [Google Scholar] [CrossRef]
- Kumar, A.; Casulo, C.; Advani, R.H.; Budde, E.; Barr, P.M.; Batlevi, C.L.; Caron, P.; Constine, L.S.; Dandapani, S.V.; Drill, E.; et al. Brentuximab Vedotin Combined With Chemotherapy in Patients With Newly Diagnosed Early-Stage, Unfavorable-Risk Hodgkin Lymphoma. J. Clin. Oncol. 2021, 39, 2257–2265. [Google Scholar] [CrossRef]
- Dozzo, M.; Zaja, F.; Volpetti, S.; Sperotto, A.; Magli, A.; Fanin, R. Brentuximab vedotin in combination with extended field radiotherapy as salvage treatment for primary refractory Hodgkin lymphoma. Am. J. Hematol. 2015, 90, E73. [Google Scholar] [CrossRef]
- Floyd, E.G.; Burns, T.F.; Linos, K.; LeBlanc, R.E.; Carter, J.B.; Jarvis, L.A.; Lansigan, F. Combined Modality Treatment With Brentuximab Vedotin and Radiation Therapy for Primary Cutaneous Anaplastic Large Cell Lymphoma: A Case Report. J. Hematol. 2019, 8, 132–136. [Google Scholar] [CrossRef]
- Wu, S.Y.; Fang, P.; Huen, A.O.; Iyer, S.P.; Nair, R.; Steiner, R.; Castillo, L.E.M.; Duvic, M.; Ahmed, S.; Jain, P.; et al. Concurrent Radiation Therapy With the Antibody-Drug Conjugates Brentuximab Vedotin and Polatuzumab Vedotin. Int. J. Radiat. Oncol. Biol. Phys. 2021, 111, e301. [Google Scholar] [CrossRef]
- Neelapu, S.S.; Locke, F.L.; Bartlett, N.L.; Lekakis, L.J.; Miklos, D.B.; Jacobson, C.A.; Braunschweig, I.; Oluwole, O.O.; Siddiqi, T.; Lin, Y.; et al. Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory Large B-Cell Lymphoma. N. Engl. J. Med. 2017, 377, 2531–2544. [Google Scholar] [CrossRef] [PubMed]
- Locke, F.L.; Miklos, D.B.; Jacobson, C.A.; Perales, M.-A.; Kersten, M.-J.; Oluwole, O.O.; Ghobadi, A.; Rapoport, A.P.; McGuirk, J.; Pagel, J.M.; et al. Axicabtagene Ciloleucel as Second-Line Therapy for Large B-Cell Lymphoma. N. Engl. J. Med. 2022, 386, 640–654. [Google Scholar] [CrossRef] [PubMed]
- Abramson, J.S.; Palomba, M.L.; Gordon, L.I.; Lunning, M.A.; Wang, M.; Arnason, J.; Mehta, A.; Purev, E.; Maloney, D.G.; Andreadis, C.; et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): A multicentre seamless design study. Lancet Lond. Engl. 2020, 396, 839–852. [Google Scholar] [CrossRef]
- Kamdar, M.; Solomon, S.R.; Arnason, J.; Johnston, P.B.; Glass, B.; Bachanova, V.; Ibrahimi, S.; Mielke, S.; Mutsaers, P.; Hernandez-Ilizaliturri, F.; et al. Lisocabtagene maraleucel versus standard of care with salvage chemotherapy followed by autologous stem cell transplantation as second-line treatment in patients with relapsed or refractory large B-cell lymphoma (TRANSFORM): Results from an interim analysis of an open-label, randomised, phase 3 trial. Lancet Lond. Engl. 2022, 399, 2294–2308. [Google Scholar] [CrossRef]
- Schuster, S.J.; Bishop, M.R.; Tam, C.S.; Waller, E.K.; Borchmann, P.; McGuirk, J.P.; Jäger, U.; Jaglowski, S.; Andreadis, C.; Westin, J.R.; et al. Tisagenlecleucel in Adult Relapsed or Refractory Diffuse Large B-Cell Lymphoma. N. Engl. J. Med. 2019, 380, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Beauford, S.S.; Kumari, A.; Garnett-Benson, C. Ionizing radiation modulates the phenotype and function of human CD4+ induced regulatory T cells. BMC Immunol. 2020, 21, 18. [Google Scholar] [CrossRef]
- DeSelm, C.; Palomba, M.L.; Yahalom, J.; Hamieh, M.; Eyquem, J.; Rajasekhar, V.K.; Sadelain, M. Low-Dose Radiation Conditioning Enables CAR T Cells to Mitigate Antigen Escape. Mol. Ther. J. Am. Soc. Gene Ther. 2018, 26, 2542–2552. [Google Scholar] [CrossRef]
- Klug, F.; Prakash, H.; Huber, P.E.; Seibel, T.; Bender, N.; Halama, N.; Pfirschke, C.; Voss, R.H.; Timke, C.; Umansky, L.; et al. Low-dose irradiation programs macrophage differentiation to an iNOS+/M1 phenotype that orchestrates effective T cell immunotherapy. Cancer Cell 2013, 24, 589–602. [Google Scholar] [CrossRef]
- Figura, N.B.; Sim, A.J.; Jain, M.D.; Chavez, J.C.; Robinson, T.J. Radiation therapy prior to CAR T-cell therapy in lymphoma: Impact on patient outcomes. Expert Rev. Hematol. 2022, 15, 1023–1030. [Google Scholar] [CrossRef]
- Nastoupil, L.J.; Jain, M.D.; Feng, L.; Spiegel, J.Y.; Ghobadi, A.; Lin, Y.; Dahiya, S.; Lunning, M.; Lekakis, L.; Reagan, P.; et al. Standard-of-Care Axicabtagene Ciloleucel for Relapsed or Refractory Large B-Cell Lymphoma: Results From the US Lymphoma CAR T Consortium. J. Clin. Oncol. 2020, 38, 3119–3128. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, C.A.; Hunter, B.D.; Redd, R.; Rodig, S.J.; Chen, P.-H.; Wright, K.; Lipschitz, M.; Ritz, J.; Kamihara, Y.; Armand, P.; et al. Axicabtagene Ciloleucel in the Non-Trial Setting: Outcomes and Correlates of Response, Resistance, and Toxicity. J. Clin. Oncol. 2020, 38, 3095–3106. [Google Scholar] [CrossRef]
- Dean, E.A.; Mhaskar, R.S.; Lu, H.; Mousa, M.S.; Krivenko, G.S.; Lazaryan, A.; Bachmeier, C.A.; Chavez, J.C.; Nishihori, T.; Davila, M.L.; et al. High metabolic tumor volume is associated with decreased efficacy of axicabtagene ciloleucel in large B-cell lymphoma. Blood Adv. 2020, 4, 3268–3276. [Google Scholar] [CrossRef]
- Jallouk, A.P.; Gouni, S.; Westin, J.; Feng, L.; Mistry, H.; Steiner, R.E.; James, J.; Noorani, M.; Horowitz, S.; Puebla-Osorio, N.; et al. Axicabtagene ciloleucel in relapsed or refractory large B-cell lymphoma patients in complete metabolic response. Haematologica 2022, 108. [Google Scholar] [CrossRef] [PubMed]
- Bishop, M.R.; Maziarz, R.T.; Waller, E.K.; Jäger, U.; Westin, J.R.; McGuirk, J.P.; Fleury, I.; Holte, H.; Borchmann, P.; Del Corral, C.; et al. Tisagenlecleucel in relapsed/refractory diffuse large B-cell lymphoma patients without measurable disease at infusion. Blood Adv. 2019, 3, 2230–2236. [Google Scholar] [CrossRef] [PubMed]
- Wudhikarn, K.; Alarcon Tomas, A.; Flynn, J.R.; Devlin, S.M.; Brower, J.; Bachanova, V.; Nastoupil, L.J.; McGuirk, J.P.; Maziarz, R.T.; Oluwole, O.O.; et al. Low toxicity and excellent outcomes in patients with DLBCL without residual lymphoma at the time of CD19 CAR T-cell therapy. Blood Adv. 2022. [CrossRef]
- Locke, F.L.; Rossi, J.M.; Neelapu, S.S.; Jacobson, C.A.; Miklos, D.B.; Ghobadi, A.; Oluwole, O.O.; Reagan, P.M.; Lekakis, L.J.; Lin, Y.; et al. Tumor burden, inflammation, and product attributes determine outcomes of axicabtagene ciloleucel in large B-cell lymphoma. Blood Adv. 2020, 4, 4898–4911. [Google Scholar] [CrossRef]
- Jain, M.D.; Zhao, H.; Wang, X.; Atkins, R.; Menges, M.; Reid, K.; Spitler, K.; Faramand, R.; Bachmeier, C.; Dean, E.A.; et al. Tumor interferon signaling and suppressive myeloid cells are associated with CAR T-cell failure in large B-cell lymphoma. Blood 2021, 137, 2621–2633. [Google Scholar] [CrossRef]
- Sim, A.J.; Jain, M.D.; Figura, N.B.; Chavez, J.C.; Shah, B.D.; Khimani, F.; Lazaryan, A.; Krivenko, G.; Davila, M.L.; Liu, H.D.; et al. Radiation Therapy as a Bridging Strategy for CAR T Cell Therapy With Axicabtagene Ciloleucel in Diffuse Large B-Cell Lymphoma. Int. J. Radiat. Oncol. Biol. Phys. 2019, 105, 1012–1021. [Google Scholar] [CrossRef]
- Wright, C.M.; LaRiviere, M.J.; Baron, J.A.; Uche, C.; Xiao, Y.; Arscott, W.T.; Anstadt, E.J.; Barsky, A.R.; Miller, D.; LaRose, M.I.; et al. Bridging Radiation Therapy Before Commercial Chimeric Antigen Receptor T-Cell Therapy for Relapsed or Refractory Aggressive B-Cell Lymphoma. Int. J. Radiat. Oncol. Biol. Phys. 2020, 108, 178–188. [Google Scholar] [CrossRef]
- Pinnix, C.C.; Gunther, J.R.; Dabaja, B.S.; Strati, P.; Fang, P.; Hawkins, M.C.; Adkins, S.; Westin, J.; Ahmed, S.; Fayad, L.; et al. Bridging therapy prior to axicabtagene ciloleucel for relapsed/refractory large B-cell lymphoma. Blood Adv. 2020, 4, 2871–2883. [Google Scholar] [CrossRef] [PubMed]
- Neelapu, S.S. CAR-T efficacy: Is conditioning the key? Blood 2019, 133, 1799–1800. [Google Scholar] [CrossRef]
- Ninomiya, S.; Narala, N.; Huye, L.; Yagyu, S.; Savoldo, B.; Dotti, G.; Heslop, H.E.; Brenner, M.K.; Rooney, C.M.; Ramos, C.A. Tumor indoleamine 2,3-dioxygenase (IDO) inhibits CD19-CAR T cells and is downregulated by lymphodepleting drugs. Blood 2015, 125, 3905–3916. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Finkelstein, S.E.; Klebanoff, C.A.; Antony, P.A.; Palmer, D.C.; Spiess, P.J.; Hwang, L.N.; Yu, Z.; Wrzesinski, C.; Heimann, D.M.; et al. Removal of homeostatic cytokine sinks by lymphodepletion enhances the efficacy of adoptively transferred tumor-specific CD8+ T cells. J. Exp. Med. 2005, 202, 907–912. [Google Scholar] [CrossRef] [PubMed]
- Kochenderfer, J.N.; Somerville, R.P.T.; Lu, T.; Shi, V.; Bot, A.; Rossi, J.; Xue, A.; Goff, S.L.; Yang, J.C.; Sherry, R.M.; et al. Lymphoma Remissions Caused by Anti-CD19 Chimeric Antigen Receptor T Cells Are Associated With High Serum Interleukin-15 Levels. J. Clin. Oncol. 2017, 35, 1803–1813. [Google Scholar] [CrossRef]
- Hirayama, A.V.; Gauthier, J.; Hay, K.A.; Voutsinas, J.M.; Wu, Q.; Gooley, T.; Li, D.; Cherian, S.; Chen, X.; Pender, B.S.; et al. The response to lymphodepletion impacts PFS in patients with aggressive non-Hodgkin lymphoma treated with CD19 CAR T cells. Blood 2019, 133, 1876–1887. [Google Scholar] [CrossRef]
- Strati, P.; Jallouk, A.P.; Sun, R.; Choi, J.; Das, K.; Cherng, H.-J.; Ahmed, S.; Lee, H.J.; Iyer, S.P.; Nair, R.; et al. Impact of conditioning chemotherapy on lymphocyte kinetics and outcomes in LBCL patients treated with CAR T-cell therapy. Leukemia 2022, 36, 2669–2677. [Google Scholar] [CrossRef]
- Strati, P.; Wierda, W.; Burger, J.; Ferrajoli, A.; Tam, C.; Lerner, S.; Keating, M.J.; O’Brien, S. Myelosuppression after frontline fludarabine, cyclophosphamide, and rituximab in patients with chronic lymphocytic leukemia: Analysis of persistent and new-onset cytopenia. Cancer 2013, 119, 3805–3811. [Google Scholar] [CrossRef]
- Strati, P.; Varma, A.; Adkins, S.; Nastoupil, L.J.; Westin, J.; Hagemeister, F.B.; Fowler, N.H.; Lee, H.J.; Fayad, L.E.; Samaniego, F.; et al. Hematopoietic recovery and immune reconstitution after axicabtagene ciloleucel in patients with large B-cell lymphoma. Haematologica 2021, 106, 2667–2672. [Google Scholar] [CrossRef]
- Rejeski, K.; Perez, A.; Sesques, P.; Hoster, E.; Berger, C.; Jentzsch, L.; Mougiakakos, D.; Frölich, L.; Ackermann, J.; Bücklein, V.; et al. CAR-HEMATOTOX: A model for CAR T-cell-related hematologic toxicity in relapsed/refractory large B-cell lymphoma. Blood 2021, 138, 2499–2513. [Google Scholar] [CrossRef]
- Jain, T.; Knezevic, A.; Pennisi, M.; Chen, Y.; Ruiz, J.D.; Purdon, T.J.; Devlin, S.M.; Smith, M.; Shah, G.L.; Halton, E.; et al. Hematopoietic recovery in patients receiving chimeric antigen receptor T-cell therapy for hematologic malignancies. Blood Adv. 2020, 4, 3776–3787. [Google Scholar] [CrossRef]
- Frank, M.J.; Hossain, N.M.; Bukhari, A.; Dean, E.; Spiegel, J.Y.; Claire, G.K.; Kirsch, I.; Jacob, A.P.; Mullins, C.D.; Lee, L.W.; et al. Monitoring of Circulating Tumor DNA Improves Early Relapse Detection After Axicabtagene Ciloleucel Infusion in Large B-Cell Lymphoma: Results of a Prospective Multi-Institutional Trial. J. Clin. Oncol. 2021, 39, 3034–3043. [Google Scholar] [CrossRef] [PubMed]
- Al Zaki, A.; Feng, L.; Watson, G.; Ahmed, S.A.; Mistry, H.; Nastoupil, L.J.; Hawkins, M.; Nair, R.; Iyer, S.P.; Lee, H.J.; et al. Day 30 SUVmax predicts progression in patients with lymphoma achieving PR/SD after CAR T-cell therapy. Blood Adv. 2022, 6, 2867–2871. [Google Scholar] [CrossRef] [PubMed]
- Kuhnl, A.; Roddie, C.; Kirkwood, A.A.; Menne, T.; Cuadrado, M.; Marzolini, M.A.V.; Osborne, W.; Sanderson, R.; O’Reilly, M.; Townsend, W.; et al. Early FDG-PET response predicts CAR-T failure in large B-cell lymphoma. Blood Adv. 2022, 6, 321–326. [Google Scholar] [CrossRef]
- Persky, D.O.; Unger, J.M.; Spier, C.M.; Stea, B.; LeBlanc, M.; McCarty, M.J.; Rimsza, L.M.; Fisher, R.I.; Miller, T.P. Southwest Oncology Group Phase II study of rituximab plus three cycles of CHOP and involved-field radiotherapy for patients with limited-stage aggressive B-cell lymphoma: Southwest Oncology Group study 0014. J. Clin. Oncol. 2008, 26, 2258–2263. [Google Scholar] [CrossRef] [PubMed]
- Stephens, D.M.; Li, H.; LeBlanc, M.L.; Puvvada, S.D.; Persky, D.; Friedberg, J.W.; Smith, S.M. Continued Risk of Relapse Independent of Treatment Modality in Limited-Stage Diffuse Large B-Cell Lymphoma: Final and Long-Term Analysis of Southwest Oncology Group Study S8736. J. Clin. Oncol. 2016, 34, 2997–3004. [Google Scholar] [CrossRef]
- Smith, E.L.; Mailankody, S.; Staehr, M.; Wang, X.; Senechal, B.; Purdon, T.J.; Daniyan, A.F.; Geyer, M.B.; Goldberg, A.D.; Mead, E.; et al. BCMA-Targeted CAR T-cell Therapy plus Radiotherapy for the Treatment of Refractory Myeloma Reveals Potential Synergy. Cancer Immunol. Res. 2019, 7, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Imber, B.S.; Sadelain, M.; DeSelm, C.; Batlevi, C.; Brentjens, R.J.; Dahi, P.B.; Giralt, S.; Park, J.H.; Sauter, C.; Scordo, M.; et al. Early experience using salvage radiotherapy for relapsed/refractory non-Hodgkin lymphomas after CD19 chimeric antigen receptor (CAR) T cell therapy. Br. J. Haematol. 2020, 190, 45–51. [Google Scholar] [CrossRef]
- Plaks, V.; Rossi, J.M.; Chou, J.; Wang, L.; Poddar, S.; Han, G.; Wang, Z.; Kuang, S.-Q.; Chu, F.; Davis, R.E.; et al. CD19 target evasion as a mechanism of relapse in large B-cell lymphoma treated with axicabtagene ciloleucel. Blood 2021, 138, 1081–1085. [Google Scholar] [CrossRef]
- Strati, P.; Neelapu, S.S. Chimeric Antigen Receptor-Engineered T Cell Therapy in Lymphoma. Curr. Oncol. Rep. 2019, 21, 38. [Google Scholar] [CrossRef]
- Perrone, S.; Lopedote, P.; Levis, M.; Di Rocco, A.; Smith, S.D. Management of relapsed or refractory large B-cell lymphoma in patients ineligible for CAR-T cell therapy. Expert Rev. Hematol. 2022, 15, 215–232. [Google Scholar] [CrossRef] [PubMed]
- Dickinson, M.J.; Carlo-Stella, C.; Morschhauser, F.; Bachy, E.; Corradini, P.; Iacoboni, G.; Khan, C.; Wróbel, T.; Offner, F.; Trněný, M.; et al. Glofitamab for Relapsed or Refractory Diffuse Large B-Cell Lymphoma. N. Engl. J. Med. 2022, 387, 2220–2231. [Google Scholar] [CrossRef] [PubMed]
- Demaria, S.; Ng, B.; Devitt, M.L.; Babb, J.S.; Kawashima, N.; Liebes, L.; Formenti, S.C. Ionizing radiation inhibition of distant untreated tumors (abscopal effect) is immune mediated. Int. J. Radiat. Oncol. Biol. Phys. 2004, 58, 862–870. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Auh, S.L.; Wang, Y.; Burnette, B.; Wang, Y.; Meng, Y.; Beckett, M.; Sharma, R.; Chin, R.; Tu, T.; et al. Therapeutic effects of ablative radiation on local tumor require CD8+ T cells: Changing strategies for cancer treatment. Blood 2009, 114, 589–595. [Google Scholar] [CrossRef]
- Dewan, M.Z.; Galloway, A.E.; Kawashima, N.; Dewyngaert, J.K.; Babb, J.S.; Formenti, S.C.; Demaria, S. Fractionated but not single-dose radiotherapy induces an immune-mediated abscopal effect when combined with anti-CTLA-4 antibody. Clin. Cancer Res. 2009, 15, 5379–5388. [Google Scholar] [CrossRef]
- Vanpouille-Box, C.; Alard, A.; Aryankalayil, M.J.; Sarfraz, Y.; Diamond, J.M.; Schneider, R.J.; Inghirami, G.; Coleman, C.N.; Formenti, S.C.; Demaria, S. DNA exonuclease Trex1 regulates radiotherapy-induced tumour immunogenicity. Nat. Commun. 2017, 8, 15618. [Google Scholar] [CrossRef]
- Daguenet, E.; Louati, S.; Wozny, A.-S.; Vial, N.; Gras, M.; Guy, J.-B.; Vallard, A.; Rodriguez-Lafrasse, C.; Magné, N. Radiation-induced bystander and abscopal effects: Important lessons from preclinical models. Br. J. Cancer 2020, 123, 339–348. [Google Scholar] [CrossRef]
- Potiron, V.A.; Abderrahmani, R.; Clément-Colmou, K.; Marionneau-Lambot, S.; Oullier, T.; Paris, F.; Supiot, S. Improved Functionality of the Vasculature during Conventionally Fractionated Radiation Therapy of Prostate Cancer. PLoS ONE 2013, 8, e84076. [Google Scholar] [CrossRef]
- Illidge, T.; Specht, L.; Yahalom, J.; Aleman, B.; Berthelsen, A.K.; Constine, L.; Dabaja, B.; Dharmarajan, K.; Ng, A.; Ricardi, U.; et al. Modern Radiation Therapy for Nodal Non-Hodgkin Lymphoma—Target Definition and Dose Guidelines From the International Lymphoma Radiation Oncology Group. Int. J. Radiat. Oncol. Biol. Phys. 2014, 89, 49–58. [Google Scholar] [CrossRef]
- Specht, L.; Yahalom, J.; Illidge, T.; Berthelsen, A.K.; Constine, L.S.; Eich, H.T.; Girinsky, T.; Hoppe, R.T.; Mauch, P.; Mikhaeel, N.G.; et al. Modern Radiation Therapy for Hodgkin Lymphoma: Field and Dose Guidelines From the International Lymphoma Radiation Oncology Group (ILROG). Int. J. Radiat. Oncol. Biol. Phys. 2014, 89, 854–862. [Google Scholar] [CrossRef]
- Coutu, B.; Kallam, A.; Lunning, M.; Bociek, G.; Bierman, P.; Vose, J.; Armitage, J.; Enke, C.A. Accelerated Fractionated Compared to Conventional Fractionated Salvage Radiation Therapy Improves Outcomes in Salvage Chemotherapy Refractory Diffuse Large B-Cell Lymphoma. Int. J. Radiat. Oncol. Biol. Phys. 2019, 105, S249–S250. [Google Scholar] [CrossRef]
- Young, K.H.; Baird, J.R.; Savage, T.; Cottam, B.; Friedman, D.; Bambina, S.; Messenheimer, D.J.; Fox, B.; Newell, P.; Bahjat, K.S.; et al. Optimizing Timing of Immunotherapy Improves Control of Tumors by Hypofractionated Radiation Therapy. PLoS ONE 2016, 11, e0157164. [Google Scholar] [CrossRef] [PubMed]
- Okumura, M.; Du, J.; Kageyama, S.-I.; Yamashita, R.; Hakozaki, Y.; Motegi, A.; Hojo, H.; Nakamura, M.; Hirano, Y.; Okuma, Y.; et al. Comprehensive screening for drugs that modify radiation-induced immune responses. Br. J. Cancer 2022, 126, 1815–1823. [Google Scholar] [CrossRef] [PubMed]
- Zanetti, G.; Astone, G.; Cappelli, L.; Chiu, W.; Cacciapuoti, M.T.; Kayembe, C.; Fiore, D.; Tam, W.; Scandura, J.; Di Giandomenico, S.; et al. Diffuse Large B Cell Pdtx in Humanized Mice Are Valuable Models to Study Host-Lymphoma Interactions and Immune-Modulating Agents. Blood 2021, 138, 2406. [Google Scholar] [CrossRef]
- Di Blasi, R.; Le Gouill, S.; Bachy, E.; Cartron, G.; Beauvais, D.; Le Bras, F.; Gros, F.-X.; Choquet, S.; Bories, P.; Feugier, P.; et al. Outcomes of patients with aggressive B-cell lymphoma after failure of anti-CD19 CAR T-cell therapy: A DESCAR-T analysis. Blood 2022, 140, 2584–2593. [Google Scholar] [CrossRef]
- Thieblemont, C.; Phillips, T.; Ghesquieres, H.; Cheah, C.Y.; Clausen, M.R.; Cunningham, D.; Do, Y.R.; Feldman, T.; Gasiorowski, R.; Jurczak, W.; et al. Epcoritamab, a Novel, Subcutaneous CD3xCD20 Bispecific T-Cell–Engaging Antibody, in Relapsed or Refractory Large B-Cell Lymphoma: Dose Expansion in a Phase I/II Trial. J. Clin. Oncol. 2023, 41, 2238–2247. [Google Scholar] [CrossRef]
- Harker-Murray, P.; Mauz-Körholz, C.; Leblanc, T.M.; Mascarin, M.; Michel, G.; Cooper, S.; Beishuizen, A.; Leger, K.J.; Amoroso, L.; Buffardi, S.; et al. Nivolumab, Brentuximab Vedotin, +/− Bendamustine For R/R Hodgkin Lymphoma in Children, Adolescents, and Young Adults. Blood 2022, 141, 2075–2084. [Google Scholar] [CrossRef]

| NCT Number | Disease (Previous Lines) | Treatment | Phase | Status |
|---|---|---|---|---|
| NCT04417166 | NK/T Cell Lymphoma (0) | Pembrolizumab + RT | II | Recruiting |
| NCT04827862 | NHL (≥2) | Pembrolizumab + Low-Dose RT | II | Recruiting |
| NCT03480334 | HL (≥1 anti-PD1 agent) | Nivolumab + RT | II | Recruiting [15] |
| NCT03179917 | HL (≥1) | Pembrolizumab + ISRT | II | Recruiting |
| NCT04962126 | FL (0) | Atezolizumab + Obinotuzumab +/− RT | II | Recruiting |
| NCT03210662 | NHL (≥1) | Pembrolizumab + EBRT | II | Recruiting |
| NCT03610061 | DLBCL or FL (≥1) | Durvalumab + RT | I | Active, not recruiting |
| NCT02927964 | FL, MZL, MCL | SD-101 + Ibrutinib + RT | I/II | Active, not recruiting [16] |
| NCT04365036 | ENKTL, nasal type (0) | Chemo-RT +/− Toripalimab | III | Recruiting |
| NCT04676789 | ENKTL, nasal type (0) | Sintilimab + PegAsp + RT | II | Not yet recruiting |
| NCT04366128 | ENKTL, nasal type (0) | Camrelizumab + PegAsp + Apatinib + RT | NA | Recruiting |
| NCT05477264 | ENKTL, nasal type (0) | Tislelizumab + RT | II | Not yet recruiting |
| NCT05149170 | ENKTL, nasal type (0) | Tislelizumab + RT | II | Recruiting |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perrone, S.; Lopedote, P.; De Sanctis, V.; Iamundo De Cumis, I.; Pulsoni, A.; Strati, P. Novel Drugs and Radiotherapy in Relapsed Lymphomas: Abscopal Response and Beyond. Cancers 2023, 15, 2751. https://doi.org/10.3390/cancers15102751
Perrone S, Lopedote P, De Sanctis V, Iamundo De Cumis I, Pulsoni A, Strati P. Novel Drugs and Radiotherapy in Relapsed Lymphomas: Abscopal Response and Beyond. Cancers. 2023; 15(10):2751. https://doi.org/10.3390/cancers15102751
Chicago/Turabian StylePerrone, Salvatore, Paolo Lopedote, Vitaliana De Sanctis, Ilenia Iamundo De Cumis, Alessandro Pulsoni, and Paolo Strati. 2023. "Novel Drugs and Radiotherapy in Relapsed Lymphomas: Abscopal Response and Beyond" Cancers 15, no. 10: 2751. https://doi.org/10.3390/cancers15102751
APA StylePerrone, S., Lopedote, P., De Sanctis, V., Iamundo De Cumis, I., Pulsoni, A., & Strati, P. (2023). Novel Drugs and Radiotherapy in Relapsed Lymphomas: Abscopal Response and Beyond. Cancers, 15(10), 2751. https://doi.org/10.3390/cancers15102751








