Boron Neutron Capture Therapy Followed by Image-Guided Intensity-Modulated Radiotherapy for Locally Recurrent Head and Neck Cancer: A Prospective Phase I/II Trial
Abstract
:Simple Summary
Abstract
1. Background
2. Materials and Methods
2.1. Study Design and Objectives
2.2. Inclusion and Exclusion Criteria
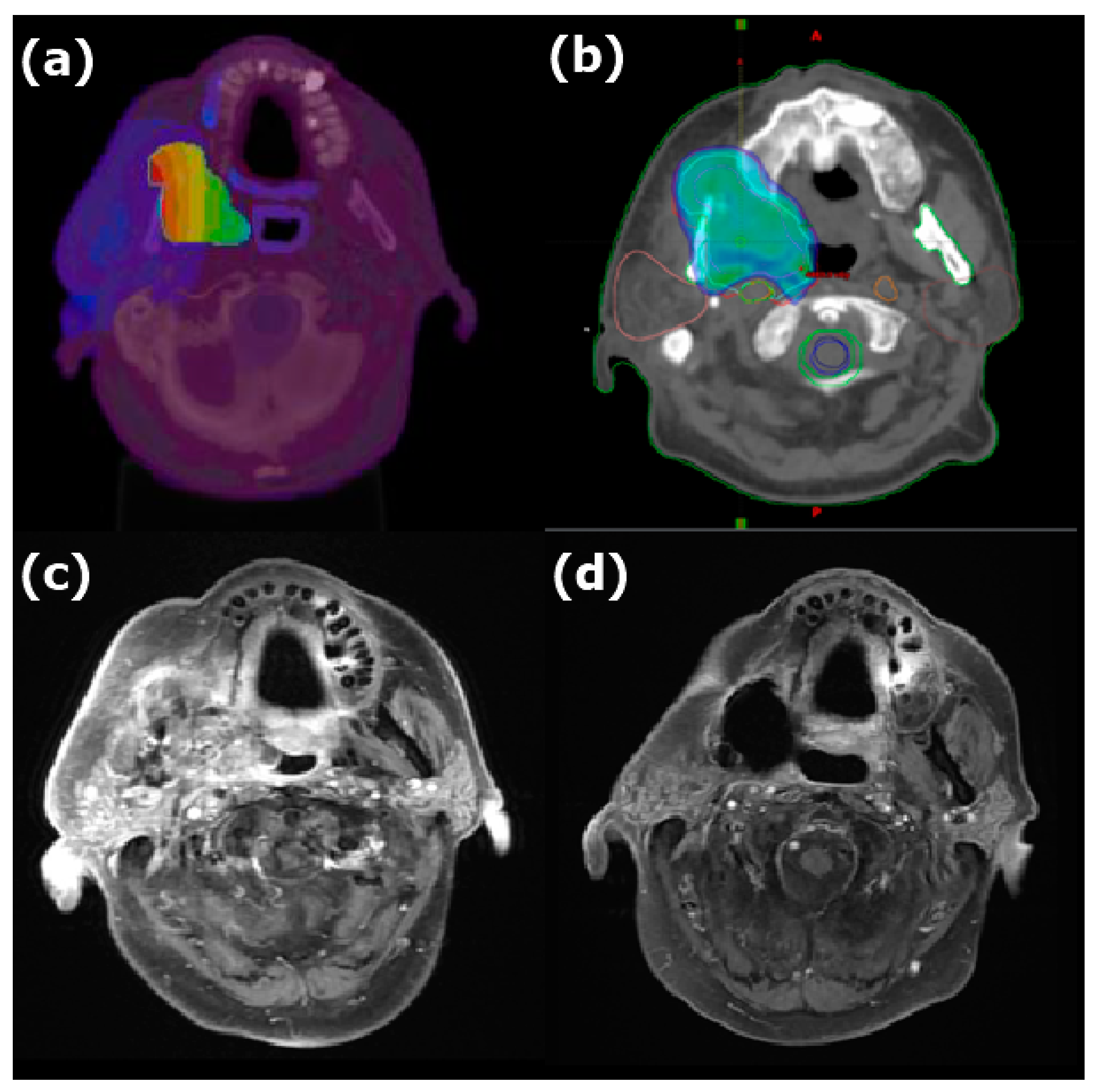
2.3. Imaging Studies
2.4. Treatment Planning for BNCT
2.5. Treatment Planning for IG-IMRT
2.6. BNCT and IG-IMRT Administration
2.7. Follow-Up
2.8. Criteria for Response and Toxicity Evaluation
2.9. Statistical Analysis
3. Results
3.1. Participant Accrual and Tumor Characteristics
3.2. Radiation Dose Delivered
3.3. Efficacy
3.4. Toxicity
3.5. Failure Pattern
3.6. Other Therapies Administered after Combined Treatment or BNCT Alone
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BNCT | Boron neutron capture therapy |
| IG-IMRT | Image-guided intensity-modulated radiotherapy |
| HNC | Head and neck cancer |
| BPA | Boronophenylalanine |
| THOR | Tsing Hua Open-Pool Reactor |
| CTV | Clinical target volume |
| PTV | Planning target volume |
| GTV | Gross tumor volume |
| RECIST | Response Evaluation Criteria in Solid Tumors |
References
- Sulman, E.P.; Schwartz, D.L.; Le, T.T.; Ang, K.K.; Morrison, W.H.; Rosenthal, D.I.; Ahamad, A.; Kies, M.; Glisson, B.; Weber, R.; et al. IMRT reirradiation of head and neck cancer-disease control and morbidity outcomes. Int. J. Radiat. Oncol. Biol. Phys. 2009, 73, 399–409. [Google Scholar] [CrossRef] [PubMed]
- Bots, W.T.; van den Bosch, S.; Zwijnenburg, E.M.; Dijkema, T.; van den Broek, G.B.; Weijs, W.L.; Verhoef, L.C.; Kaanders, J.H. Reirradiation of head and neck cancer: Long-term disease control and toxicity. Head Neck 2017, 39, 1122–1130. [Google Scholar] [CrossRef] [PubMed]
- Zwicker, F.; Roeder, F.; Hauswald, H.; Thieke, C.; Timke, C.; Schlegel, W.; Debus, J.; Münter, M.W.; Huber, P.E. Reirradiation with intensity-modulated radiotherapy in recurrent head and neck cancer. Head Neck 2011, 33, 1695–1702. [Google Scholar] [CrossRef] [PubMed]
- Ahlawat, P.; Rawat, S.; Kakria, A.; Devnani, B.; Wahi, I.K.; Simson, D.K. Reirradiation with IMRT for recurrent head and neck cancer: A single-institutional report on disease control, survival, and toxicity. Rep. Pract. Oncol. Radiother. 2017, 22, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Barth, R.F.; HVicente, M.; Harling, O.K.; Kiger, W.S.; Riley, K.J.; Binns, P.J.; Wagner, F.M.; Suzuki, M.; Aihara, T.; Kato, I.; et al. Current status of boron neutron capture therapy of high grade gliomas and recurrent head and neck cancer. Radiat. Oncol. 2012, 7, 146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aihara, T.; Hiratsuka, J.; Morita, N.; Uno, M.; Sakurai, Y.; Maruhashi, A.; Ono, K.; Harada, T. First clinical case of boron neutron capture therapy for head and neck malignancies using 18F-BPA PET. Head Neck 2006, 28, 850–855. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, M.; Sakurai, Y.; Nagata, K.; Kinashi, Y.; Masunaga, S.; Ono, K.; Maruhashi, A.; Kato, I.; Fuwa, N.; Hiratsuka, J.; et al. Impact of intra-arterial administration of boron compounds on dose-volume histograms in boron neutron capture therapy for recurrent head-and-neck tumors. Int. J. Radiat. Oncol. Biol. Phys. 2006, 66, 1523–1527. [Google Scholar] [CrossRef] [PubMed]
- Kankaanranta, L.; Seppälä, T.; Koivunoro, H.; Saarilahti, K.; Atula, T.; Collan, J.; Salli, E.; Kortesniemi, M.; Uusi-Simola, J.; Välimäki, P.; et al. Boron neutron capture therapy in the treatment of locally recurred head and neck cancer. Int. J. Radiat. Oncol. Biol. Phys. 2007, 69, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.H.; Liu, Y.W.H.; Chou, F.I.; Liu, H.M.; Peir, J.J.; Liu, Y.H.; Huang, Y.S.; Wang, L.W.; Chen, Y.W.; Yen, S.H.; et al. The overview and prospects of BNCT facility at Tsing Hua Open-pool reactor. Appl. Radiat. Isot. 2020, 161, 109143. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.W.; Chen, Y.W.; Ho, C.Y.; Liu, Y.W.H.; Chou, F.I.; Liu, Y.H.; Liu, H.M.; Peir, J.J.; Jiang, S.H.; Chang, C.W.; et al. Fractionated boron neutron capture therapy in locally recurrent head and neck cancer: A prospective phase I/II trial. Int. J. Radiat. Oncol. Biol. Phys. 2016, 95, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Kankaanranta, L.; Seppälä, T.; Koivunoro, H.; Saarilahti, K.; Atula, T.; Collan, J.; Salli, E.; Kortesniemi, M.; Uusi-Simola, J.; Välimäki, P.; et al. Boron neutron capture therapy in the treatment of locally recurred head-and-neck cancer: Final analysis of a phase I/II trial. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, e67–e75. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.M.; Farwell, D.G.; Luu, Q.; Cheng, S.; Donald, P.J.; Purdy, J.A. Prospective trial of high-dose reirradiation using daily image guidance with intensity-modulated radiotherapy for recurrent and second primary head-and-neck cancer. Int. J. Radiat. Oncol. Biol. Phys. 2011, 80, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.; Yoo, E.J.; Kim, J.Y.; Han, C.W.; Kim, K.J.; Kay, C.S. Re-irradiation of unresectable recurrent head and neck cancer: Using Helical Tomotherapy as image-guided intensity-modulated radiotherapy. Radiat. Oncol. J. 2013, 31, 206–215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, H.S.; Liu, Y.W.; Lee, C.Y.; Lin, T.Y.; Hsu, F.Y. Verification of the accuracy of BNCT treatment planning system THORplan. Appl. Radiat. Isot. 2009, 67, S122–S125. [Google Scholar] [CrossRef] [PubMed]
- International Commission on Radiation Units and Measurements. ICRU Report 46, Photon, Electron, Proton, and Neutron Interaction Data for Body Tissues; International Committee on Radiation Units and Measurements: Bethesda, MD, USA, 1992. [Google Scholar]
- Coderre, J.A.; Morris, G.M. The radiation biology of boron neutron capture therapy. Radiat Res. 1999, 151, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Yoshino, K.; Suzuki, A.; Mori, Y.; Kakihana, H.; Honda, C.; Mishima, Y.; Kobayashi, T.; Kanda, K. Improvement of solubility of p-boronophenylalanine by complex formation with monosaccharides. Strahlenther. Onkol. 1989, 165, 127–129. [Google Scholar] [PubMed]
- Joensuu, H.; Kankaanranta, L.; Seppälä, T.; Auterinen, I.; Kallio, M.; Kulvik, M.; Laakso, J.; Vähätalo, J.; Kortesniemi, M.; Kotiluoto, P.; et al. Boron neutron capture therapy of brain tumors: Clinical trials at the finnish facility using boronophenylalanine. J. Neuro-Oncol. 2003, 62, 123–134. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.C.; Chuang, K.S.; Hsueh Liu, Y.W.; Lin, T.Y.; Teng, Y.C.; Wang, L.W. A comparison of dose distributions in gross tumor volume between boron neutron capture therapy alone and combined boron neutron capture therapy plus intensity modulation radiation therapy for head and neck cancer. PLoS ONE 2019, 14, e0210626. [Google Scholar] [CrossRef] [PubMed]
- Hirose, K.; Konno, A.; Hiratsuka, J.; Yoshimoto, S.; Kato, T.; Ono, K.; Otsuki, N.; Hatazawa, J.; Tanaka, H.; Takayama, K.; et al. Boron neutron capture therapy using cyclotron-based epithermal neutron source and borofalan (10B) for recurrent or locally advanced head and neck cancer (JHN002): An open-label phase II trial. Radiother. Oncol. 2021, 155, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, M.; Kato, I.; Aihara, T.; Hiratsuka, J.; Yoshimura, K.; Niimi, M.; Kimura, Y.; Ariyoshi, Y.; Haginomori, S.I.; Sakurai, Y.; et al. Boron neutron capture therapy outcomes for advanced or recurrent head and neck cancer. J. Radiat. Res. 2014, 55, 146–153. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | n (%) | Median (Range) |
|---|---|---|
| Patient | ||
| Gender | ||
| Male | 10 (71) | |
| Female | 4 (29) | |
| Age (y) | 57 (40, 78) | |
| Surgery before BNCT | ||
| Yes | 8 (57) | |
| No | 6 (43) | |
| Prior cumulative RT dose (Gy) | 68 (60, 102) | |
| Time from prior RT to BNCT (mo) | 23 (8, 108) | |
| Tumor | ||
| Primary site | ||
| Oral cavity | 7 (50) | |
| Nasopharynx | 2 (14) | |
| Oropharynx | 2 (14) | |
| Hypopharynx | 1 (7) | |
| Parotid gland | 1 (7) | |
| Mandible | 1 (7) | |
| Pathology | ||
| SCC | 10 (71) | |
| Other carcinoma * | 3 (21) | |
| Sarcoma | 1 (7) | |
| Volume (cc) | 13.5 (3.1, 368) | |
| Recurrent T stage | ||
| rT0 | 1 (7) | |
| rT1 | 0 (0) | |
| rT2 | 1 (7) | |
| rT3 | 6 (43) | |
| rT4 | 6 (43) | |
| Recurrent N stage | ||
| rN0 | 9 (64) | |
| rN1 | 2 (14) | |
| rN2 | 3 (21) | |
| rN3 | 0 (0) |
| Parameters | Median (Minimum, Maximum) |
|---|---|
| BNCT | |
| BPA T/N ratio by PET | 3.0 (2.5,3.6) |
| Irradiation time (min) | 21.0 (16.7, 27.0) |
| Average equivalent tumor dose (Gy (Eq)) | 21.6 (10.7, 32.3) |
| Average tumor physical dose (Gy) | 6.1 (3.4, 9.8) |
| Maximum mucosa physical dose (Gy) | 4.9 (3.0, 6.1) |
| Interval between BNCT and IG-IMRT (days) | 30 (26, 39) |
| IG-IMRT | |
| Total prescription dose | 46.8 (41.4,53) |
| Total fractions | 25 (23, 28) |
| Adverse Effects | None (n) | Grades 1–2 (n) | Grade 3 (n) | Grade 4 (n) | Not Available |
|---|---|---|---|---|---|
| Mucositis | 0 | 14 | 0 | 0 | 0 |
| Radiation dermatitis | 0 | 14 | 0 | 0 | 0 |
| Alopecia | 0 | 14 | 0 | 0 | 0 |
| Dysphagia | 3 | 6 | 2 | 0 | 3 |
| Tumor pain | 3 | 8 | 3 | 0 | 0 |
| Hemorrhage | 10 | 3 | 0 | 1 | 0 |
| Infection (soft tissue) | 5 | 6 | 2 | 0 | 1 |
| Edema (H&N) | 10 | 3 | 1 | 0 | 0 |
| Edema (laryngeal) | 13 | 0 | 0 | 1 | 0 |
| Otitis | 12 | 2 | 0 | 0 | 0 |
| Nausea or vomiting | 9 | 5 | 0 | 0 | 0 |
| Trismus | 12 | 2 | 0 | 0 | 0 |
| Adverse Effects | None (n) | Grades 1–2 (n) | Grade 3 (n) | Grade 4 (n) |
|---|---|---|---|---|
| Osteoradionecrosis | 8 | 3 | 1 | 0 |
| Soft tissue necrosis | 4 | 6 | 2 | 0 |
| Hemorrhage | 11 | 0 | 0 | 1 |
| Cranial neuropathy | 9 | 1 | 2 | 0 |
| Dysphagia | 6 | 5 | 1 | 0 |
| Pain | 2 | 8 | 2 | 0 |
| Skin ulceration | 7 | 1 | 4 | 0 |
| Alopecia | 12 | 0 | 0 | 0 |
| Impaired hearing | 11 | 1 | 0 | 0 |
| Otitis | 9 | 2 | 1 | 0 |
| Xerostomia | 8 | 4 | 0 | 0 |
| Edema (H&N) | 10 | 2 | 0 | 0 |
| Trismus | 8 | 3 | 1 | 0 |
| Infection | 4 | 7 | 1 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, L.-W.; Liu, Y.-W.H.; Chu, P.-Y.; Liu, H.-M.; Peir, J.-J.; Lin, K.-H.; Huang, W.-S.; Lo, W.-L.; Lee, J.-C.; Lin, T.-Y.; et al. Boron Neutron Capture Therapy Followed by Image-Guided Intensity-Modulated Radiotherapy for Locally Recurrent Head and Neck Cancer: A Prospective Phase I/II Trial. Cancers 2023, 15, 2762. https://doi.org/10.3390/cancers15102762
Wang L-W, Liu Y-WH, Chu P-Y, Liu H-M, Peir J-J, Lin K-H, Huang W-S, Lo W-L, Lee J-C, Lin T-Y, et al. Boron Neutron Capture Therapy Followed by Image-Guided Intensity-Modulated Radiotherapy for Locally Recurrent Head and Neck Cancer: A Prospective Phase I/II Trial. Cancers. 2023; 15(10):2762. https://doi.org/10.3390/cancers15102762
Chicago/Turabian StyleWang, Ling-Wei, Yen-Wan Hsueh Liu, Pen-Yuan Chu, Hong-Ming Liu, Jinn-Jer Peir, Ko-Han Lin, Wen-Sheng Huang, Wen-Liang Lo, Jia-Cheng Lee, Tzung-Yi Lin, and et al. 2023. "Boron Neutron Capture Therapy Followed by Image-Guided Intensity-Modulated Radiotherapy for Locally Recurrent Head and Neck Cancer: A Prospective Phase I/II Trial" Cancers 15, no. 10: 2762. https://doi.org/10.3390/cancers15102762






