The Changing Landscape of Thyroid Surgery during the COVID-19 Pandemic: A Four-Year Analysis in a University Hospital in Romania
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
- “Pre-COVID-19” (from 26 February 2019 to 25 February 2020);
- “C1” (COVID-19-first year, from 26 February 2020 to 25 February 2021);
- “C2” (COVID-19-s year, from 26 February 2021 to 25 February 2022);
- “C3” (COVID-19-third year, from 26 February 2022 to 25 February 2023).
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ahmad, A.; Mueller, C.; Tsamakis, K. COVID-19 pandemic: A public and global mental health opportunity for social transformation? BMJ 2020, 369, m1383. [Google Scholar] [CrossRef] [PubMed]
- Docea, A.O.; Tsatsakis, A.; Albulescu, D.; Cristea, O.; Zlatian, O.; Vinceti, M.; Moschos, S.A.; Tsoukalas, D.; Goumenou, M.; Drakoulis, N.; et al. A new threat from an old enemy: Re-emergence of coronavirus (Review). Int. J. Mol. Med. 2020, 45, 1631–1643. [Google Scholar] [CrossRef] [PubMed]
- Sjödin, H.; Wilder-Smith, A.; Osman, S.; Farooq, Z.; Rocklöv, J. Only strict quarantine measures can curb the coronavirus disease (COVID-19) outbreak in Italy, 2020. Eurosurveillance 2020, 25, 2000280. [Google Scholar] [CrossRef]
- Liang, W.; Guan, W.; Chen, R.; Wang, W.; Li, J.; Xu, K.; Li, C.; Ai, Q.; Lu, W.; Liang, H.; et al. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020, 21, 335–337. [Google Scholar] [CrossRef]
- Russ, G.; Leboulleux, S.; Leenhardt, L.; Hegedüs, L. Thyroid Incidentalomas: Epidemiology, Risk Stratification with Ultrasound and Workup. Eur. Thyroid J. 2014, 3, 154–163. [Google Scholar] [CrossRef]
- Pizzato, M.; Li, M.; Vignat, J.; Laversanne, M.; Singh, D.; La Vecchia, C.; Vaccarella, S. The epidemiological landscape of thyroid cancer worldwide: GLOBOCAN estimates for incidence and mortality rates in 2020. Lancet Diabetes Endocrinol. 2022, 10, 264–272. [Google Scholar] [CrossRef]
- Medas, F.; Ansaldo, G.L.; Avenia, N.; Basili, G.; Boniardi, M.; Bononi, M.; Bove, A.; Carcoforo, P.; Casaril, A.; Cavallaro, G.; et al. The THYCOVIT (Thyroid Surgery during COVID-19 pandemic in Italy) study: Results from a nationwide, multicentric, case-controlled study. Updat. Surg. 2021, 73, 1467–1475. [Google Scholar] [CrossRef]
- The National Institute of Public Health. Available online: https://insp.gov.ro/ (accessed on 22 April 2023).
- Onyeaka, H.; Anumudu, C.K.; Al-Sharify, Z.T.; Egele-Godswill, E.; Mbaegbu, P. COVID-19 pandemic: A review of the global lockdown and its far-reaching effects. Sci. Prog. 2021, 104, 368504211019854. [Google Scholar] [CrossRef]
- Gambardella, C.; Pagliuca, R.; Pomilla, G.; Gambardella, A. COVID-19 risk contagion: Organization and procedures in a South Italy geriatric oncology ward. J. Geriatr. Oncol. 2020, 11, 1187–1188. [Google Scholar] [CrossRef]
- Søreide, K.; Hallet, J.; Matthews, J.B.; Schnitzbauer, A.A.; Line, P.D.; Lai, P.B.S.; Otero, J.; Callegaro, D.; Warner, S.G.; Baxter, N.N.; et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br. J. Surg. 2020, 107, 1250–1261. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, A.; Pellino, G. COVID-19 pandemic: Perspectives on an unfolding crisis. Br. J. Surg. 2020, 107, 785–787. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, A.S.; Fernandes, B.; de Lange, M.; Lingsma, H.; Klazinga, N.; Kringos, D. Changes in the quality of cancer care as assessed through performance indicators during the first wave of the COVID-19 pandemic in 2020: A scoping review. BMC Health Serv. Res. 2022, 22, 786. [Google Scholar] [CrossRef] [PubMed]
- Pramono, L.A. COVID-19 and Thyroid Diseases: How the Pandemic Situation Affects Thyroid Disease Patients? J. ASEAN Fed. Endocr. Soc. 2020, 35, 155–157. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Oluyomi, A.; Woodard, L.; Raza, S.A.; Fahmideh, M.A.; El-Mubasher, O.; Byun, J.; Han, Y.; Amos, C.I.; Badr, H. Individual-Level Determinants of Lifestyle Behavioral Changes during COVID-19 Lockdown in the United States: Results of an Online Survey. Int. J. Environ. Res. Public Health 2021, 18, 4364. [Google Scholar] [CrossRef]
- Mogharab, V.; Ostovar, M.; Ruszkowski, J.; Hussain, S.Z.M.; Shrestha, R.; Yaqoob, U.; Aryanpoor, P.; Nikkhoo, A.M.; Heidari, P.; Jahromi, A.R.; et al. Global burden of the COVID-19 associated patient-related delay in emergency healthcare: A panel of systematic review and meta-analyses. Glob. Health 2022, 18, 58. [Google Scholar] [CrossRef]
- Tsang, V.H.M.; Gild, M.; Glover, A.; Clifton-Bligh, R.; Robinson, B.G. Thyroid cancer in the age of COVID-19. Endocr.-Relat. Cancer 2020, 27, R407–R416. [Google Scholar] [CrossRef]
- Vrachimis, A.; Iakovou, I.; Giannoula, E.; Giovanella, L. Endocrinology in the time of COVID-19: Management of thyroid nodules and cancer. Eur. J. Endocrinol. 2020, 183, G41–G48. [Google Scholar] [CrossRef]
- Baud, G.; Brunaud, L.; Lifante, J.-C.; Tresallet, C.; Sebag, F.; Bizard, J.-P.; Mathonnet, M.; Menegaux, F.; Caiazzo, R.; Mirallié, E.; et al. Endocrine surgery during and after the COVID-19 epidemic: Expert guidelines from AFCE. J. Visc. Surg. 2020, 157, S43–S49. [Google Scholar] [CrossRef]
- Nickel, B.; Miller, J.A.; Cvejic, E.; Gild, M.L.; Cope, D.; Dodd, R.; McCaffery, K.; Glover, A. Thyroid cancer clinicians’ views and experiences of delayed treatment during the COVID-19 pandemic: An international cross-sectional survey. ANZ J. Surg. 2021, 91, 2562–2564. [Google Scholar] [CrossRef]
- Stefanou, C.K.; Papathanakos, G.; Stefanou, S.K.; Tepelenis, K.; Kitsouli, A.; Barbouti, A.; Flindris, S.; Tsoumanis, P.; Kanavaros, P.; Kitsoulis, P. Thyroid surgery during the COVID-19 pandemic: Difficulties—How to improve. Innov. Surg. Sci. 2022, 7, 125–132. [Google Scholar] [CrossRef]
- Kim, S.H.; Min, E.; Hwang, Y.M.; Choi, Y.S.; Yi, J.W. Impact of COVID-19 Pandemic on Thyroid Surgery in a University Hospital in South Korea. Cancers 2022, 14, 4338. [Google Scholar] [CrossRef]
- American College of Surgeons, Corp-Author. COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures. Available online: https://www.facs.org/covid-19/clinical-guidance/triage (accessed on 17 March 2020).
- Ramakrishna, R.; Zadeh, G.; Sheehan, J.P.; Aghi, M.K. Inpatient and outpatient case prioritization for patients with neuro-oncologic disease amid the COVID-19 pandemic: General guidance for neuro-oncology practitioners from the AANS/CNS Tumor Section and Society for Neuro-Oncology. J. Neuro-Oncol. 2020, 147, 525–529. [Google Scholar] [CrossRef] [PubMed]
- Khorana, A.A.; Tullio, K.; Elson, P.; Pennell, N.A.; Grobmyer, S.R.; Kalady, M.F.; Raymond, D.; Abraham, J.; Klein, E.A.; Walsh, R.M.; et al. Time to initial cancer treatment in the United States and association with survival over time: An observational study. PLoS ONE 2019, 14, e0213209. [Google Scholar] [CrossRef]
- Reiners, C.; Wegscheider, K.; Schicha, H.; Theissen, P.; Vaupel, R.; Wrbitzky, R.; Schumm-Draeger, P.-M. Prevalence of Thyroid Disorders in the Working Population of Germany: Ultrasonography Screening in 96,278 Unselected Employees. Thyroid 2004, 14, 926–932. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.A.S.; Udelsman, R. Total thyroidectomy for differentiated thyroid cancer. J. Surg. Oncol. 2006, 94, 701–707. [Google Scholar] [CrossRef]
- Mulita, F.; Verras, G.-I.; Dafnomili, V.-D.; Tchabashvili, L.; Perdikaris, I.; Bousis, D.; Liolis, E.; Samaras, A.; Vafeiadis, V.; Delis, A.; et al. Thyroidectomy for the Management of Differentiated Thyroid Carcinoma and their Outcome on Early Postoperative Complications: A 6-year Single-Centre Retrospective Study. Chirurgia 2022, 117, 556–562. [Google Scholar] [CrossRef]
- Beninato, T.; Laird, A.M.; Graves, C.E.; Drake, F.T.; Alhefdhi, A.; Lee, J.A.; Kuo, J.H.; Grubbs, E.G.; Wang, T.S.; Pasieka, J.L.; et al. Impact of the COVID-19 pandemic on the practice of endocrine surgery. Am. J. Surg. 2022, 223, 670–675. [Google Scholar] [CrossRef]
- Mahajan, S.; Manjula, B.V.; Vaishnavi, R.; John, N.; Babu, B. Usefulness of The Bethesda System of Reporting Thyroid Cytopathology in Surgical Planning. Indian J. Otolaryngol. Head Neck Surg. 2022, 74, 2623–2628. [Google Scholar] [CrossRef]
- Mulita, F.; Plachouri, M.-K.; Liolis, E.; Vailas, M.; Panagopoulos, K.; Maroulis, I. Patient outcomes following surgical management of thyroid nodules classified as Bethesda category III (AUS/FLUS). Endokrynol. Polska 2021, 72, 143–144. [Google Scholar] [CrossRef] [PubMed]
- Ho, A.S.; Sarti, E.E.; Jain, K.S.; Wang, H.; Nixon, I.J.; Shaha, A.R.; Shah, J.P.; Kraus, D.H.; Ghossein, R.; Fish, S.A.; et al. Malignancy Rate in Thyroid Nodules Classified as Bethesda Category III (AUS/FLUS). Thyroid 2014, 24, 832–839. [Google Scholar] [CrossRef]
- Amit, M.; Rudnicki, Y.; Binenbaum, Y.; Msc, L.T.-L.; Cohen, J.T.; Gil, Z. Defining the outcome of patients with delayed diagnosis of differentiated thyroid cancer. Laryngoscope 2014, 124, 2837–2840. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Zhan, L.; Guo, L.; Yu, X.; Li, L.; Feng, H.; Yang, D.; Xu, Z.; Tu, Y.; Chen, C.; et al. More Aggressive Cancer Behaviour in Thyroid Cancer Patients in the Post-COVID-19 Pandemic Era: A Retrospective Study. Int. J. Gen. Med. 2021, 14, 7197–7206. [Google Scholar] [CrossRef] [PubMed]
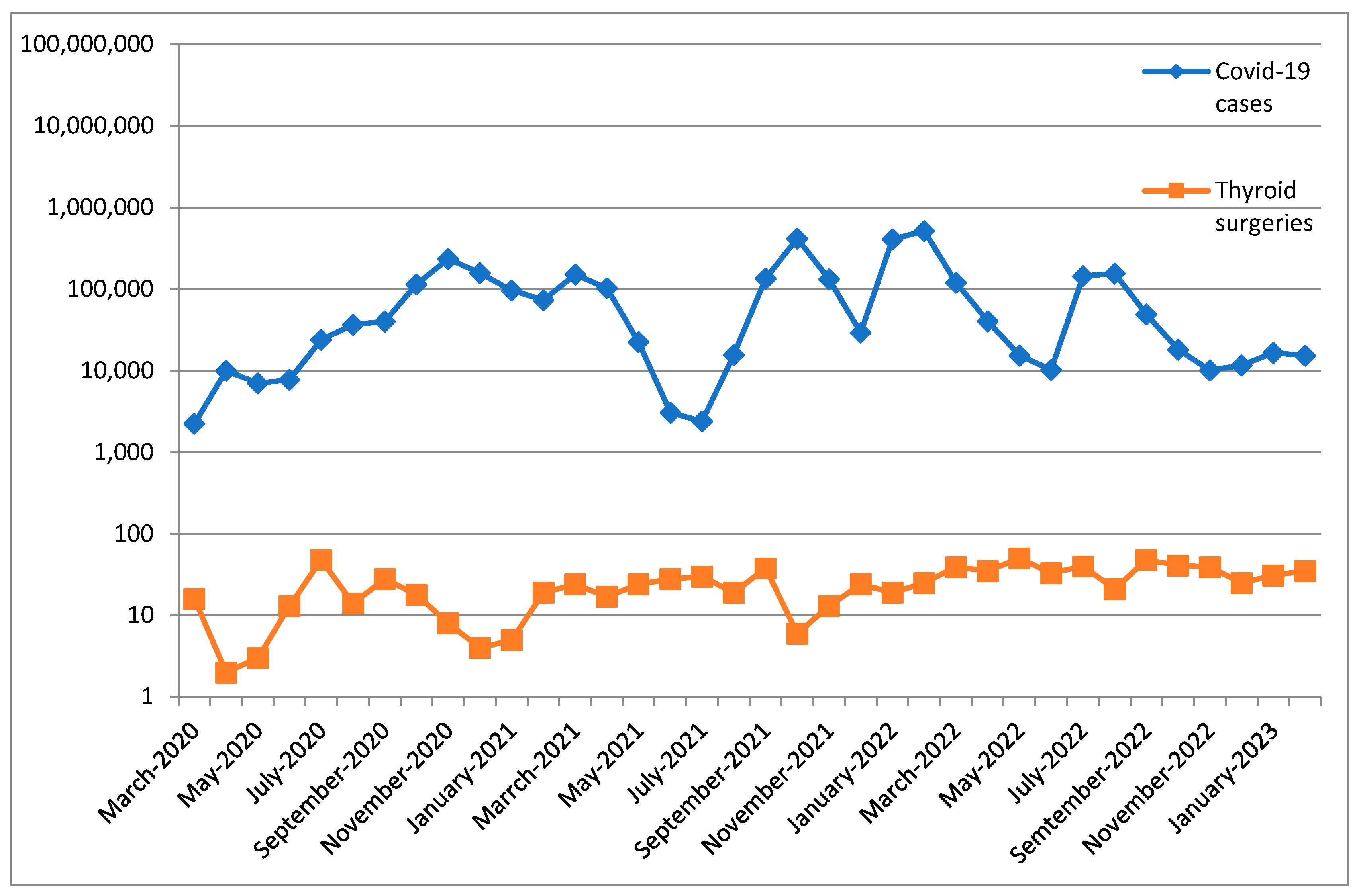
| Period | COVID-19 Cases | Thyroid Surgery | Spearman’s Rho | p |
|---|---|---|---|---|
| C1 (M ± SD) | 66,832.58 ± 72,069.597 | 14.83 ± 13.044 | 0.035 | 0.914 |
| C2 (M ± SD) | 160,957.75 ± 182,060.316 | 22.25 ± 8.292 | −0.314 | 0.320 |
| C3 (M ± SD) | 50,571.50 ± 55,781.587 | 36.42 ± 8.415 | 0.049 | 0.879 |
| Variables | Pre-COVID-19 N = 457 | C1 N = 178 | C2 N = 269 | C3 N = 435 | p |
|---|---|---|---|---|---|
| Age (years. M ± SD) | 52.88 ± 13.31 | 52.69 ± 13.56 | 53.38 ± 13.75 | 54.58 ± 12.91 | 0.206 |
| Gender | 0.425 | ||||
| Male | 48 (10.5%) | 26 (14.6%) | 30 (11.2%) | 57 (13.1%) | |
| Female | 409 (89.5%) | 152 (85.4%) | 239 (88.8%) | 378 (86.9%) | |
| Environment | 0.696 | ||||
| Urban | 286 (62.6%) | 116 (65.2%) | 171 (63.6%) | 263 (60.5%) | |
| Rural | 171 (37.4% | 62 (34.8%) | 98 (36.4%) | 172 (39.5%) | |
| Hospital stay (days. M ± SD) | 4.77 ± 2.34 | 4.63 ± 2.06 | 4.03 ± 2.27 | 4.08 ± 1.79 | <0.001 * |
| Preoperative stay (days. M ± SD) | 1.78 ± 1.48 | 1.90 ± 1.36 | 1.45 ± 0.99 | 1.48 ± 1.26 | <0.001 * |
| Postoperative stay (days. M ± SD) | 2.98 ± 1.57 | 2.73 ± 1.31 | 2.58 ± 1.93 | 2.60 ± 1.20 | <0.001 * |
| Duration of surgery (minutes. M ± SD) | 133.19 ± 45.66 | 140.02 ± 52.70 | 155.58 ± 61.19 | 161.63 ± 61.76 | <0.001 * |
| Type of surgery | 0.770 | ||||
| Total Thyroidectomy | 372 (81.4%) | 149 (83.7%) | 226 (84.0%) | 361 (83.0%) | |
| Lobectomy | 84 (18.4%) | 28 (15.7%) | 42 (15.6%) | 74 (17.0%) | |
| Completion surgery after initial lobectomy | 11 (12.9%) | 6 (21.4%) | 13 (31.0%) | 18 (24.7%) | 0.093 |
| Charlson index (M ± SD) | 3.11 ± 1.41 | 2.87 ± 1.14 | 2.95 ± 1.18 | 2.96 ± 1.12 | 0.099 |
| Pathologic Diagnosis | 0.140 | ||||
| Anaplastic cancer | 1 (0.2%) | 3 (1.7%) | 0 (0%) | 2 (0.5%) | |
| Medullary cancer | 2 (0.4%) | 1 (0.6%) | 4 (1.5%) | 7 (1.6%) | |
| Papillary cancer | 125 (27.5%) | 54 (30.3%) | 79 (29.6%) | 146 (33.6%) | |
| Follicular tumors ** | 324 (70.9%) | 119 (66.8%) | 184 (68.5%) | 280 (64.4%) | |
| Lymphoma | 1 (0.2%) | 0 (0%) | 1 (0.4%) | 0 (0%) |
| Variables | Pre-COVID-19 N = 307 | C1 N = 112 | C2 N = 172 | C3 N = 253 | p |
|---|---|---|---|---|---|
| Age (years. M ± SD) | 52.49 ± 13.37 | 52.03 ± 13.35 | 53.62 ± 14.09 | 53.9 ± 12.8 | 0.470 |
| Gender | 0.238 | ||||
| Male | 24 (7.8%) | 16 (14.3%) | 19 (11%) | 24 (9.5%) | |
| Female | 283 (92.2%) | 96 (85.7%) | 153 (89%) | 229 (90.5) | |
| Environment | 0.640 | ||||
| Urban | 188 (61.2%) | 75 (67%) | 112 (65.1%) | 156 (61.7%) | |
| Rural | 119 (38.8%) | 37 (33%) | 60 (34.9%) | 97 (38.3%) | |
| Hospital stay (days. M ± SD) | 4.62 ± 1.87 | 4.42 ± 1.75 | 3.95 ± 2.40 | 4.10 ± 1.88 | 0.001 * |
| Preoperative stay (days. M ± SD) | 1.67 ± 1.28 | 1.82 ± 1.24 | 1.37 ± 0.77 | 1.51 ± 1.37 | 0.007 * |
| Postoperative stay (days. M ± SD) | 2.94 ± 1.33 | 2.6 ± 1.15 | 2.58 ± 2.23 | 2.59 ± 1.16 | 0.012 * |
| Duration of surgery (minutes. M ± SD) | 133.62 ± 44.47 | 139.49 ± 52.72 | 153.41 ± 58.07 | 162.63 ± 57.02 | <0.001 * |
| Type of surgery | 0.699 | ||||
| Total Thyroidectomy | 242 (78.8%) | 89 (79.5%) | 140 (81.4%) | 209 (82.6%) | |
| Lobectomy | 65 (21.2%) | 23 (20.5%) | 32 (18.6%) | 44 (17.4%) | |
| Tumor size (cm. M ± SD) | 1.65 ± 0.91 | 2.20 ± 1.72 | 1.69 ± 0.93 | 1.85 ± 0.96 | <0.001 * |
| Variables | Pre-COVID-19 N = 125 | C1 N = 54 | C2 N = 79 | C3 N = 146 | p |
|---|---|---|---|---|---|
| Age (years. M ± SD) | 53.73 ± 12.40 | 53.46 ± 14.58 | 52.67 ± 12.87 | 56.14 ± 13.14 | 0.208 |
| Gender | 0.760 | ||||
| Male | 18 (14.4%) | 8 (14.8%) | 8 (10.1%) | 22 (15.1%) | |
| Female | 107 (85.6%) | 46 (85.2%) | 71 (89.9%) | 124 (84.9%) | |
| Environment | 0.452 | ||||
| Urban | 82 (65.6%) | 34 (63%) | 48 (60.8%) | 82 (56.2%) | |
| Rural | 43 (34.4%) | 20 (37%) | 31 (39.2%) | 64 (43.8%) | |
| Hospital stay (days. M ± SD) | 5.14 ± 3.15 | 4.69 ± 2.13 | 4.19 ± 2.11 | 3.91 ± 1.48 | <0.001 * |
| Preoperative stay (days. M ± SD) | 2.0 ± 1.86 | 1.87 ± 1.30 | 1.61 ± 1.29 | 1.39 ± 0.96 | 0.003 * |
| Postoperative stay (days. M ± SD) | 3.14 ± 2.09 | 2.81 ± 1.51 | 2.57 ± 1.26 | 2.52 ± 1.15 | 0.007 * |
| Duration of surgery (minutes. M ± SD) | 133.15 ± 46.85 | 130.0 ± 44.67 | 155.24 ± 62.96 | 160.72 ± 71.21 | <0.001 * |
| Tumor size (cm) | 0.870 | ||||
| ≤1 cm | 87 (70.2%) | 37 (68.5%) | 51 (64.6%) | 100 (68.5%) | |
| >1 cm | 37 (29.8%) | 17 (31.5%) | 28 (35.4%) | 46 (31.5%) | |
| Multifocality | 0.205 | ||||
| Single | 76 (60.8%) | 31 (57.4%) | 39 (49.4%) | 93 (63.7%) | |
| Multiple | 49 (39.2%) | 23 (42.6%) | 40 (50.6%) | 53 (36.3%) | |
| Capsular invasion | 0.127 | ||||
| Absent | 71 (56.8%) | 35 (64.8%) | 36 (45.6%) | 86 (58.9%) | |
| Present | 54 (43.2%) | 19 (35.2%) | 43 (54.4%) | 60 (41.1%) | |
| Vascular invasion | 0.193 | ||||
| Absent | 98 (78.4%) | 46 (85.2%) | 55 (69.6%) | 114 (78.1%) | |
| Present | 27 (21.6%) | 8 (14.8%) | 24 (30.4%) | 32 (21.9%) | |
| pT | 0.426 | ||||
| 1 | 93 (77.5%) | 48 (88.9%) | 70 (88.6%) | 113 (78.5%) | |
| 2 | 16 (13.3%) | 4 (7.4%) | 7 (8.9%) | 18 (12.5%) | |
| 3 | 11 (9.2%) | 2 (3.7%) | 2 (2.5%) | 12 (8.3%) | |
| 4 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.7%) | |
| pN | 0.282 | ||||
| 0 | 104 (86.7%) | 54 (100%) | 69 (87.3%) | 125 (86.8%) | |
| x | 7 (5.8%) | 0 (0%) | 4 (5.1%) | 5 (3.5%) | |
| 1a | 6 (5.0%) | 0 (0%) | 5 (6.3%) | 12 (8.3%) | |
| 1b | 3 (2.5%) | 0 (0%) | 1 (1.3%) | 2 (1.4%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feier, C.V.I.; Muntean, C.; Faur, A.M.; Blidari, A.; Contes, O.E.; Streinu, D.R.; Olariu, S. The Changing Landscape of Thyroid Surgery during the COVID-19 Pandemic: A Four-Year Analysis in a University Hospital in Romania. Cancers 2023, 15, 3032. https://doi.org/10.3390/cancers15113032
Feier CVI, Muntean C, Faur AM, Blidari A, Contes OE, Streinu DR, Olariu S. The Changing Landscape of Thyroid Surgery during the COVID-19 Pandemic: A Four-Year Analysis in a University Hospital in Romania. Cancers. 2023; 15(11):3032. https://doi.org/10.3390/cancers15113032
Chicago/Turabian StyleFeier, Catalin Vladut Ionut, Calin Muntean, Alaviana Monique Faur, Andiana Blidari, Oana Elena Contes, Diana Raluca Streinu, and Sorin Olariu. 2023. "The Changing Landscape of Thyroid Surgery during the COVID-19 Pandemic: A Four-Year Analysis in a University Hospital in Romania" Cancers 15, no. 11: 3032. https://doi.org/10.3390/cancers15113032
APA StyleFeier, C. V. I., Muntean, C., Faur, A. M., Blidari, A., Contes, O. E., Streinu, D. R., & Olariu, S. (2023). The Changing Landscape of Thyroid Surgery during the COVID-19 Pandemic: A Four-Year Analysis in a University Hospital in Romania. Cancers, 15(11), 3032. https://doi.org/10.3390/cancers15113032






