MRI Apparent Diffusion Coefficient (ADC) as a Biomarker of Tumour Response: Imaging-Pathology Correlation in Patients with Hepatic Metastases from Colorectal Cancer (EORTC 1423)
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
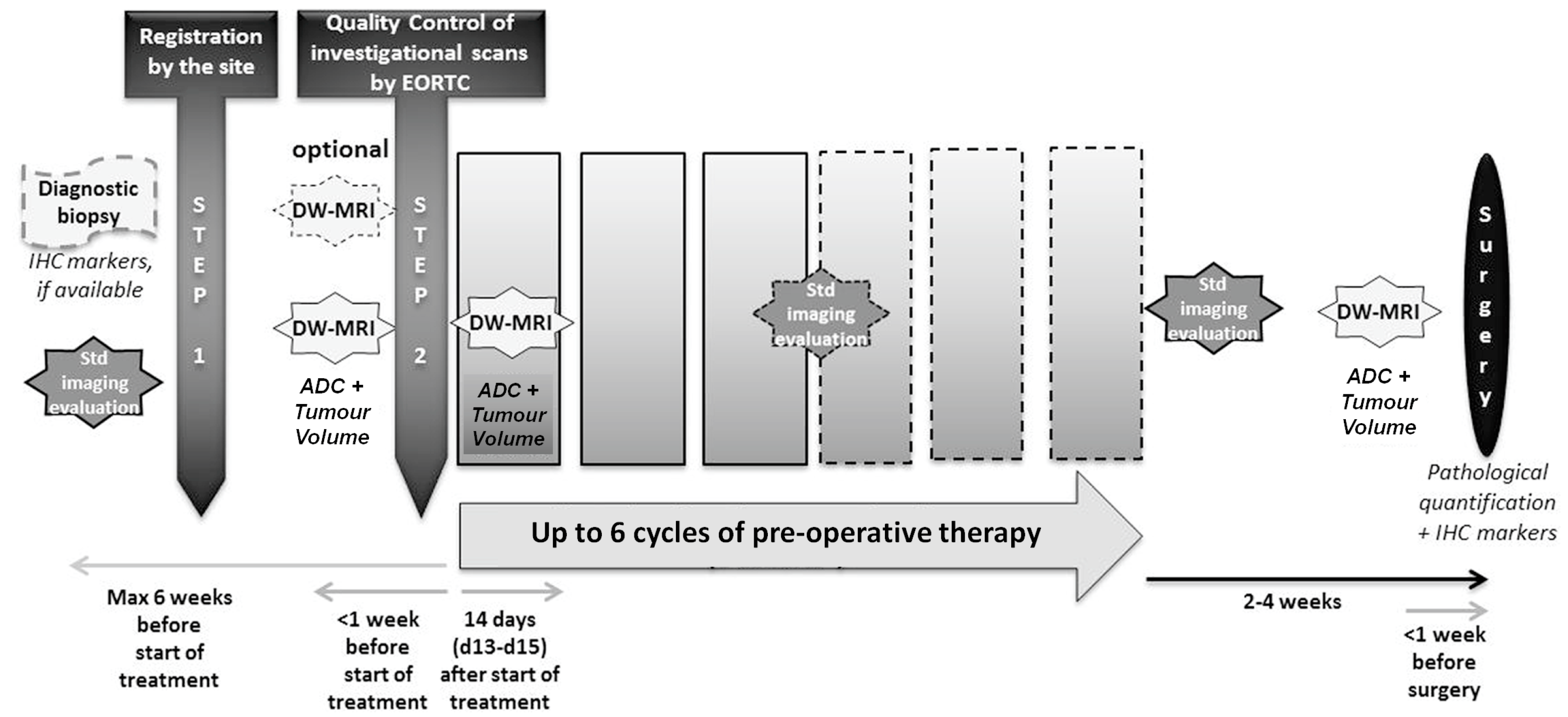
2.1. Trial Design
- To measure the variability of test–retest ADC measurements at baseline
- To correlate pre-operative (post-treatment) ADC measurement and TRG
- To correlate pre-operative (post-treatment) ADC measurement and tumour tissue cellularity/density, necrosis, and proliferation (Ki-67)
2.2. Image Handling
2.2.1. Quality Control (QC)
2.2.2. Scanning Protocol
2.2.3. Measurement of ADC
2.3. Histological Evaluation
2.4. Statistical Analysis
3. Results
3.1. Quality Control (QC)
3.2. Patient Demographics
3.3. Imaging Findings
3.4. Surgical Specimens and Pathology
3.5. Correlation between Imaging Biomarkers, Tumour Response Grade, and Histology
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Papaevangelou, E.; Almeida, G.S.; Jamin, Y.; Robinson, S.P.; deSouza, N.M. Diffusion-weighted MRI for imaging cell death after cytotoxic or apoptosis-inducing therapy. Br. J. Cancer 2015, 112, 1471–1479. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, J.P.; Aboagye, E.O.; Adams, J.E.; Aerts, H.J.; Barrington, S.F.; Beer, A.J.; Boellaard, R.; Bohndiek, S.E.; Brady, M.; Brown, G.; et al. Imaging biomarker roadmap for cancer studies. Nat. Rev. Clin. Oncol. 2017, 14, 169–186. [Google Scholar] [CrossRef] [PubMed]
- Stephen, R.M.; Jha, A.K.; Roe, D.J.; Trouard, T.P.; Galons, J.P.; Kupinski, M.A.; Frey, G.; Cui, H.; Squire, S.; Pagel, M.D.; et al. Diffusion MRI with Semi-Automated Segmentation Can Serve as a Restricted Predictive Biomarker of the Therapeutic Response of Liver Metastasis. Magn. Reson. Imaging 2015, 33, 1267–1273. [Google Scholar] [CrossRef]
- Oz, A.; Server, S.; Koyuncu Sokmen, B.; Namal, E.; Inan, N.; Balci, N.C. Intravoxel Incoherent Motion of Colon Cancer Liver Metastases for the Assessment of Response to Antiangiogenic Treatment: Results from a Pilot Study. Med. Princ. Pract. 2020, 29, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Deckers, F.; De Foer, B.; Van Mieghem, F.; Botelberge, T.; Weytjens, R.; Padhani, A.; Pouillon, M. Apparent diffusion coefficient measurements as very early predictive markers of response to chemotherapy in hepatic metastasis: A preliminary investigation of reproducibility and diagnostic value. J. Magn. Reson. Imaging 2014, 40, 448–456. [Google Scholar] [CrossRef]
- Donati, O.F.; Chong, D.; Nanz, D.; Boss, A.; Froehlich, J.M.; Andres, E.; Seifert, B.; Thoeny, H.C. Diffusion-weighted MR imaging of upper abdominal organs: Field strength and intervendor variability of apparent diffusion coefficients. Radiology 2014, 270, 454–463. [Google Scholar] [CrossRef]
- Pathak, R.; Tian, J.; Thacker, N.A.; Morris, D.M.; Ragheb, H.; Saunders, C.; Saunders, M.; Jackson, A. Considering tumour volume for motion corrected DWI of colorectal liver metastases increases sensitivity of ADC to detect treatment-induced changes. Sci. Rep. 2019, 9, 3828. [Google Scholar] [CrossRef]
- deSouza, N.M.; Winfield, J.M.; Waterton, J.C.; Weller, A.; Papoutsaki, M.V.; Doran, S.J.; Collins, D.J.; Fournier, L.; Sullivan, D.; Chenevert, T.; et al. Implementing diffusion-weighted MRI for body imaging in prospective multicentre trials: Current considerations and future perspectives. Eur. Radiol. 2018, 28, 1118–1131. [Google Scholar] [CrossRef]
- Jerome, N.P.; Papoutsaki, M.V.; Orton, M.R.; Parkes, H.G.; Winfield, J.M.; Boss, M.A.; Leach, M.O.; deSouza, N.M.; Collins, D.J. Development of a temperature-controlled phantom for magnetic resonance quality assurance of diffusion, dynamic, and relaxometry measurements. Med. Phys. 2016, 43, 2998–3007. [Google Scholar] [CrossRef]
- Hargreaves, B.; Sung, K.; Charles-Edwards, G. ADC Map Calculation. Available online: https://web.stanford.edu/~bah/software/ADCmap/ (accessed on 3 July 2023).
- Rubbia-Brandt, L.; Giostra, E.; Brezault, C.; Roth, A.D.; Andres, A.; Audard, V.; Sartoretti, P.; Dousset, B.; Majno, P.E.; Soubrane, O.; et al. Importance of histological tumor response assessment in predicting the outcome in patients with colorectal liver metastases treated with neo-adjuvant chemotherapy followed by liver surgery. Ann. Oncol. 2007, 18, 299–304. [Google Scholar] [CrossRef]
- Chang, H.H.; Leeper, W.R.; Chan, G.; Quan, D.; Driman, D.K. Infarct-like necrosis: A distinct form of necrosis seen in colorectal carcinoma liver metastases treated with perioperative chemotherapy. Am. J. Surg. Pathol. 2012, 36, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Padhani, A.R.; Liu, G.; Koh, D.M.; Chenevert, T.L.; Thoeny, H.C.; Takahara, T.; Dzik-Jurasz, A.; Ross, B.D.; Van Cauteren, M.; Collins, D.; et al. Diffusion-weighted magnetic resonance imaging as a cancer biomarker: Consensus and recommendations. Neoplasia 2009, 11, 102–125. [Google Scholar] [CrossRef] [PubMed]
- Schmeel, F.C. Variability in quantitative diffusion-weighted MR imaging (DWI) across different scanners and imaging sites: Is there a potential consensus that can help reducing the limits of expected bias? Eur. Radiol. 2019, 29, 2243–2245. [Google Scholar] [CrossRef] [PubMed]
- Winfield, J.M.; Wakefield, J.C.; Brenton, J.D.; AbdulJabbar, K.; Savio, A.; Freeman, S.; Pace, E.; Lutchman-Singh, K.; Vroobel, K.M.; Yuan, Y.; et al. Biomarkers for site-specific response to neoadjuvant chemotherapy in epithelial ovarian cancer: Relating MRI changes to tumour cell load and necrosis. Br. J. Cancer 2021, 124, 1130–1137. [Google Scholar] [CrossRef]
- Heijmen, L.; Ter Voert, E.E.; Nagtegaal, I.D.; Span, P.; Bussink, J.; Punt, C.J.; de Wilt, J.H.; Sweep, F.C.; Heerschap, A.; van Laarhoven, H.W. Diffusion-weighted MR imaging in liver metastases of colorectal cancer: Reproducibility and biological validation. Eur. Radiol. 2013, 23, 748–756. [Google Scholar] [CrossRef]
- Donati, F.; Boraschi, P.; Pacciardi, F.; Cervelli, R.; Castagna, M.; Urbani, L.; Falaschi, F.; Caramella, D. 3T diffusion-weighted MRI in the response assessment of colorectal liver metastases after chemotherapy: Correlation between ADC value and histological tumour regression grading. Eur. J. Radiol. 2017, 91, 57–65. [Google Scholar] [CrossRef]
- Boraschi, P.; Donati, F.; Cervelli, R.; Pacciardi, F.; Tarantini, G.; Castagna, M.; Urbani, L.; Lencioni, R. Colorectal liver metastases: ADC as an imaging biomarker of tumor behavior and therapeutic response. Eur. J. Radiol. 2021, 137, 109609. [Google Scholar] [CrossRef]
- Kim, J.H.; Joo, I.; Kim, T.Y.; Han, S.W.; Kim, Y.J.; Lee, J.M.; Han, J.K. Diffusion-Related MRI Parameters for Assessing Early Treatment Response of Liver Metastases to Cytotoxic Therapy in Colorectal Cancer. AJR Am. J. Roentgenol. 2016, 207, W26–W32. [Google Scholar] [CrossRef]
- Eriksson, S.; Bengtsson, J.; Toren, W.; Latt, J.; Andersson, R.; Sturesson, C. Changes in apparent diffusion coefficient and pathological response in colorectal liver metastases after preoperative chemotherapy. Acta Radiol. 2023, 64, 51–57. [Google Scholar] [CrossRef]
- Uutela, A.; Ovissi, A.; Hakkarainen, A.; Ristimaki, A.; Lundbom, N.; Kallio, R.; Soveri, L.M.; Salminen, T.; Algars, A.; Halonen, P.; et al. Treatment response of colorectal cancer liver metastases to neoadjuvant or conversion therapy: A prospective multicentre follow-up study using MRI, diffusion-weighted imaging and 1H-MR spectroscopy compared with histology (subgroup in the RAXO trial). ESMO Open 2021, 6, 100208. [Google Scholar] [CrossRef]
- Beckers, R.C.J.; Lambregts, D.M.J.; Lahaye, M.J.; Rao, S.X.; Kleinen, K.; Grootscholten, C.; Beets, G.L.; Beets-Tan, R.G.H.; Maas, M. Advanced imaging to predict response to chemotherapy in colorectal liver metastases—A systematic review. HPB 2018, 20, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Winfield, J.M.; Tunariu, N.; Rata, M.; Miyazaki, K.; Jerome, N.P.; Germuska, M.; Blackledge, M.D.; Collins, D.J.; de Bono, J.S.; Yap, T.A.; et al. Extracranial Soft-Tissue Tumors: Repeatability of Apparent Diffusion Coefficient Estimates from Diffusion-weighted MR Imaging. Radiology 2017, 284, 88–99. [Google Scholar] [CrossRef] [PubMed]
- Dale, B.M.; Braithwaite, A.C.; Boll, D.T.; Merkle, E.M. Field strength and diffusion encoding technique affect the apparent diffusion coefficient measurements in diffusion-weighted imaging of the abdomen. Investig. Radiol. 2010, 45, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Winfield, J.M.; Collins, D.J.; Priest, A.N.; Quest, R.A.; Glover, A.; Hunter, S.; Morgan, V.A.; Freeman, S.; Rockall, A.; deSouza, N.M. A framework for optimization of diffusion-weighted MRI protocols for large field-of-view abdominal-pelvic imaging in multicenter studies. Med. Phys. 2016, 43, 95. [Google Scholar] [CrossRef]
- Sedlaczek, O.L.; Kleesiek, J.; Gallagher, F.A.; Murray, J.; Prinz, S.; Perez-Lopez, R.; Sala, E.; Caramella, C.; Diffetock, S.; Lassau, N.; et al. Quantification and reduction of cross-vendor variation in multicenter DWI MR imaging: Results of the Cancer Core Europe imaging task force. Eur. Radiol. 2022, 32, 8617–8628. [Google Scholar] [CrossRef]
- Malyarenko, D.; Galban, C.J.; Londy, F.J.; Meyer, C.R.; Johnson, T.D.; Rehemtulla, A.; Ross, B.D.; Chenevert, T.L. Multi-system repeatability and reproducibility of apparent diffusion coefficient measurement using an ice-water phantom. J. Magn. Reson. Imaging 2013, 37, 1238–1246. [Google Scholar] [CrossRef]
- Asselin, M.C.; O’Connor, J.P.; Boellaard, R.; Thacker, N.A.; Jackson, A. Quantifying heterogeneity in human tumours using MRI and PET. Eur. J. Cancer 2012, 48, 447–455. [Google Scholar] [CrossRef]
- Winfield, J.M.; deSouza, N.M.; Priest, A.N.; Wakefield, J.C.; Hodgkin, C.; Freeman, S.; Orton, M.R.; Collins, D.J. Modelling DW-MRI data from primary and metastatic ovarian tumours. Eur. Radiol. 2015, 25, 2033–2040. [Google Scholar] [CrossRef]
- Miquel, M.E.; Scott, A.D.; Macdougall, N.D.; Boubertakh, R.; Bharwani, N.; Rockall, A.G. In vitro and in vivo repeatability of abdominal diffusion-weighted MRI. Br. J. Radiol. 2012, 85, 1507–1512. [Google Scholar] [CrossRef]
- Lu, T.L.; Meuli, R.A.; Marques-Vidal, P.M.; Bize, P.; Denys, A.; Schmidt, S. Interobserver and intraobserver variability of the apparent diffusion coefficient in treated malignant hepatic lesions on a 3.0T machine: Measurements in the whole lesion versus in the area with the most restricted diffusion. J. Magn. Reson. Imaging 2010, 32, 647–653. [Google Scholar] [CrossRef]
- Lambregts, D.M.; Maas, M.; Riedl, R.G.; Bakers, F.C.; Verwoerd, J.L.; Kessels, A.G.; Lammering, G.; Boetes, C.; Beets, G.L.; Beets-Tan, R.G. Value of ADC measurements for nodal staging after chemoradiation in locally advanced rectal cancer-a per lesion validation study. Eur. Radiol. 2011, 21, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Colagrande, S.; Pasquinelli, F.; Mazzoni, L.N.; Belli, G.; Virgili, G. MR-diffusion weighted imaging of healthy liver parenchyma: Repeatability and reproducibility of apparent diffusion coefficient measurement. J. Magn. Reson. Imaging 2010, 31, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Pathak, R.; Ragheb, H.; Thacker, N.A.; Morris, D.M.; Amiri, H.; Kuijer, J.; deSouza, N.M.; Heerschap, A.; Jackson, A. A data-driven statistical model that estimates measurement uncertainty improves interpretation of ADC reproducibility: A multi-site study of liver metastases. Sci. Rep. 2017, 7, 14084. [Google Scholar] [CrossRef] [PubMed]
- Nasu, K.; Kuroki, Y.; Sekiguchi, R.; Nawano, S. The effect of simultaneous use of respiratory triggering in diffusion-weighted imaging of the liver. Magn. Reson. Med. Sci. 2006, 5, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Ragheb, H.; Thacker, N.A.; Guyader, J.M.; Klein, S.; deSouza, N.M.; Jackson, A. The Accuracy of ADC Measurements in Liver Is Improved by a Tailored and Computationally Efficient Local-Rigid Registration Algorithm. PLoS ONE 2015, 10, e0132554. [Google Scholar] [CrossRef]
- Liu, L.H.; Zhou, G.F.; Lv, H.; Wang, Z.C.; Rao, S.X.; Zeng, M.S. Identifying response in colorectal liver metastases treated with bevacizumab: Development of RECIST by combining contrast-enhanced and diffusion-weighted MRI. Eur. Radiol. 2021, 31, 5640–5649. [Google Scholar] [CrossRef]
- Jepsen, D.N.M.; Hoeg, H.; Thagaard, J.; Walbech, J.S.; Gogenur, I.; Fiehn, A.K. Development of a method for digital assessment of tumor regression grade in patients with rectal cancer following neoadjuvant therapy. J. Pathol. Inform. 2022, 13, 100152. [Google Scholar] [CrossRef]
| Institution | Patients | MRI Scanners |
|---|---|---|
| Humanitas Unversity (Milan, Italy) | 10 | Phillips Achieva 1.5 T, Phillips Ingenia 1.5 T |
| Institut Bergonié (Bordeaux, France) | 5 | Siemens Aera 1.5 T |
| Universität Duisberg-Essen (Essen, Germany) | 4 | Siemens Aera 1.5 T |
| Universitari de Barcelona (Barcelona, Spain) | 3 | Siemens Aera 1.5 T |
| Hospital Universitari La Fe (Valencia, Spain) | 2 | GE Optima 360 3 T |
| Medizinische Universität Wien (Vienna, Austria) | 2 | Siemens Trio 3.0 T |
| Sapienza Università di Roma (Rome, Italy) | 2 | Siemens Avanto 1.5 T |
| Charité—Universitätsmedizin (Berlin, Germany) | 1 | Siemens Aera 1.5 T |
| Parameter | T1 and T2 Anatomical | Diffusion Weighted 1.5 T | Diffusion Weighted 3 T |
|---|---|---|---|
| FOV | 380 | 380 | 380 |
| Pixel Size | 1.5 × 1.5 mm | 3 × 3 mm | 3 × 3 mm |
| Slice Thickness | 5 mm | 5 mm | 5 mm |
| Slice gap | 0 | 0 | 0 |
| Respiratory Control | Breath holding if required | Free breathing | Free breathing |
| Acquisition matrix | 256 × 224 (87.5%) | 128 × 112 (87.5%) | 240 × 240 (87.5%) |
| Reconstruction matrix | 256 × 256 | 256 × 256 | 256 × 256 |
| Number of slices | 40 | 40 | 40 |
| Number of signal averages | 2 | 4 | 4 |
| TR ms | Site specific | ≥8000 | ≥5000 |
| TE ms | Site specific | minimum | minimum |
| Parallel imaging * | Site specific | yes | yes |
| Acceleration factor | Not specified | 2 | 2 |
| Diffusion gradient mode | Not applicable | 3 scan-trace | 3 scan-trace |
| Fat suppression | None | SPAIR | SPAIR |
| b-values s/mm2 | Not applicable | 100, 400, 800 | 150, 400, 800 |
| All Patients (N = 26) | Chemotherapy Alone (N = 18) | |
|---|---|---|
| N (%) | N (%) | |
| Site of the primary tumor | ||
| Colon cancer | 16 (61.5) | 12 (66.7) |
| Rectum cancer | 10 (38.5) | 6 (33.3) |
| Histological grade | ||
| GI | 3 (11.5) | 2 (11.1) |
| GII | 12 (46.2) | 7 (38.9) |
| GIII | 6 (23.1) | 4 (22.2) |
| Missing | 5 (19.2) | 5 (27.8) |
| TNM staging at first diagnosis | ||
| Stage I | 2 (7.7) | 0 (0.0) |
| Stage IIA | 4 (15.4) | 3 (16.7) |
| Stage IIB | 2 (7.7) | 1 (5.6) |
| Stage IIIB | 1 (3.8) | 1 (5.6) |
| Stage IVA | 16 (61.5) | 12 (66.7) |
| Stage IVB | 1 (3.8) | 1 (5.6) |
| All Patients | Patients Undergoing Surgery | ||||||
|---|---|---|---|---|---|---|---|
| Baseline | Day 14 | Within 1 Week before Surgery | Baseline | Day 14 | Within 1 Week before Surgery | ||
| ADC max (10−3 mm2/s) | No. lesions measured | 82 | 79 | 65 | 48 | 46 | 39 |
| Median | 2.0 | 2.1 | 2.0 | 2.1 | 2.2 | 1.9 | |
| Range | 1.1–4.1 | 1.1–4.1 | 1.3–4.1 | 1.1–4.1 | 1.1–4.1 | 1.3–4.1 | |
| Mean (SD) | 2.21 (0.73) | 2.23 (0.70) | 2.21 (0.72) | 2.24 (0.65) | 2.21 (0.61) | 2.08 (0.60) | |
| ADC mean (10−3 mm2/s) | No. lesions measured | 82 | 79 | 65 | 48 | 46 | 39 |
| Median | 1.0 | 1.1 | 1.1 | 1.0 | 1.1 | 1.1 | |
| Range | 0.7–2.7 | 0.7–2.6 | 0.4–2.6 | 0.7–2.7 | 0.7–2.6 | 0.8–2.5 | |
| Mean (SD) | 1.19 (0.45) | 1.24 (0.41) | 1.29 (0.45) | 1.16 (0.39) | 1.19 (0.36) | 1.20 (0.36) | |
| ΔADCmax | ΔADCmean | ||||
|---|---|---|---|---|---|
| All Patients N = 26 | Chemotherapy Alone N = 18 | All Patients N = 26 | Chemotherapy Alone N = 18 | ||
| ΔADCearly (%) | No. lesions measured | 79 | 56 | 79 | 56 |
| Median | −0.7 | 0.9 | 4.3 | 4.9 | |
| Range | −28.6–60.5 | −28.6–40.4 | −38.3–94.8 | −26.5–94.8 | |
| Mean (SD) | 1.90 (16.27) | 1.94 (15.29) | 5.43 (17.02) | 7.35 (16.51) | |
| ΔADClate (%) | No. lesions measured | 65 | 48 | 65 | 48 |
| Median | −1.5 | −1.2 | 7.6 | 6.4 | |
| Range | −50.8–61.8 | −50.8–61.8 | −64.1–116.2 | −64.1–116.2 | |
| Mean (SD) | −0.23 (21.28) | 0.41 (20.80) | 9.90 (23.65) | 9.07 (25.38) | |
| ΔADCmax | ΔADCmean | ||||
|---|---|---|---|---|---|
| All Surgical Patients (N = 23) | Chemotherapy Alone (N = 16) | All Surgical Patients (N = 23) | Chemotherapy Alone (N = 16) | ||
| ΔADCearly (%) | No. lesions measured | 46 | 33 | 46 | 33 |
| Median | −1.4 | −2.8 | 5.2 | 5.5 | |
| Range | −28.6–40.4 | −28.6–40.4 | −38.3–37.5 | −26.5–37.5 | |
| Mean (SD) | −0.70 (15.37) | −0.93 (15.59) | 2.82 (14.84) | 4.98 (11.65) | |
| ΔADClate (%) | No. lesions measured | 39 | 29 | 39 | 29 |
| Median | −6.8 | −6.8 | 4.0 | 2.2 | |
| Range | −50.8–61.8 | −50.8–61.8 | −18.6–54.5 | −16.1–44.8 | |
| Mean (SD) | −6.01 (21.44) | −6.76 (20.52) | 7.58 (18.71) | 6.01 (18.18) | |
| Total Surface Area of Lesion (mm2) | Total Surface Area of Fibrosis (%) | Total Surface Area of Necrosis (%) | Total Surface Area of Viable Tumour Cells (%) | Ratio Ki-67 Positive to Total Tumour | |
|---|---|---|---|---|---|
| Median | 180.0 | 37.5 | 20.0 | 32.1 | 0.2 |
| Range | 3.0–813.0 | 5.0–95.8 | 0.0–82.9 | 0.0–80.0 | 0.0–0.6 |
| Mean (SD) | 227.35 (195.29) | 42.42 (24.19) | 23.64 (21.37) | 33.94 (22.02) | 0.22 (0.17) |
| All Patients | Chemotherapy Only | ||||
|---|---|---|---|---|---|
| ADCmax (n = 39) | ADCmean (n = 39) | ADCmax (n = 29) | ADCmean (n = 29) | ||
| % viable tumour | Correlation | −0.404 | −0.222 | −0.411 | −0.280 |
| p-value | 0.776 | 0.976 | 0.732 | 0.916 | |
| % necrosis | Correlation | 0.005 | −0.384 | −0.132 | −0.632 |
| p-value | 1.00 | 1.00 | 1.00 | 1.00 | |
| % fibrosis | Correlation | 0.213 | 0.386 | 0.311 | 0.646 |
| p-value | 0.979 | 0.815 | 0.886 | 0.142 | |
| Ki-67 | Correlation | −0.115 | −0.329 | −0.238 | −0.459 |
| p-value | 0.996 | 0.901 | 0.946 | 0.625 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jackson, A.; Pathak, R.; deSouza, N.M.; Liu, Y.; Jacobs, B.K.M.; Litiere, S.; Urbanowicz-Nijaki, M.; Julie, C.; Chiti, A.; Theysohn, J.; et al. MRI Apparent Diffusion Coefficient (ADC) as a Biomarker of Tumour Response: Imaging-Pathology Correlation in Patients with Hepatic Metastases from Colorectal Cancer (EORTC 1423). Cancers 2023, 15, 3580. https://doi.org/10.3390/cancers15143580
Jackson A, Pathak R, deSouza NM, Liu Y, Jacobs BKM, Litiere S, Urbanowicz-Nijaki M, Julie C, Chiti A, Theysohn J, et al. MRI Apparent Diffusion Coefficient (ADC) as a Biomarker of Tumour Response: Imaging-Pathology Correlation in Patients with Hepatic Metastases from Colorectal Cancer (EORTC 1423). Cancers. 2023; 15(14):3580. https://doi.org/10.3390/cancers15143580
Chicago/Turabian StyleJackson, Alan, Ryan Pathak, Nandita M. deSouza, Yan Liu, Bart K. M. Jacobs, Saskia Litiere, Maria Urbanowicz-Nijaki, Catherine Julie, Arturo Chiti, Jens Theysohn, and et al. 2023. "MRI Apparent Diffusion Coefficient (ADC) as a Biomarker of Tumour Response: Imaging-Pathology Correlation in Patients with Hepatic Metastases from Colorectal Cancer (EORTC 1423)" Cancers 15, no. 14: 3580. https://doi.org/10.3390/cancers15143580
APA StyleJackson, A., Pathak, R., deSouza, N. M., Liu, Y., Jacobs, B. K. M., Litiere, S., Urbanowicz-Nijaki, M., Julie, C., Chiti, A., Theysohn, J., Ayuso, J. R., Stroobants, S., & Waterton, J. C. (2023). MRI Apparent Diffusion Coefficient (ADC) as a Biomarker of Tumour Response: Imaging-Pathology Correlation in Patients with Hepatic Metastases from Colorectal Cancer (EORTC 1423). Cancers, 15(14), 3580. https://doi.org/10.3390/cancers15143580







