High-Speed Videoendoscopy Enhances the Objective Assessment of Glottic Organic Lesions: A Case-Control Study with Multivariable Data-Mining Model Development
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Group
2.2. Equipment and Examination
2.3. Kymographic Analysis
2.4. Statistical Analysis
3. Results
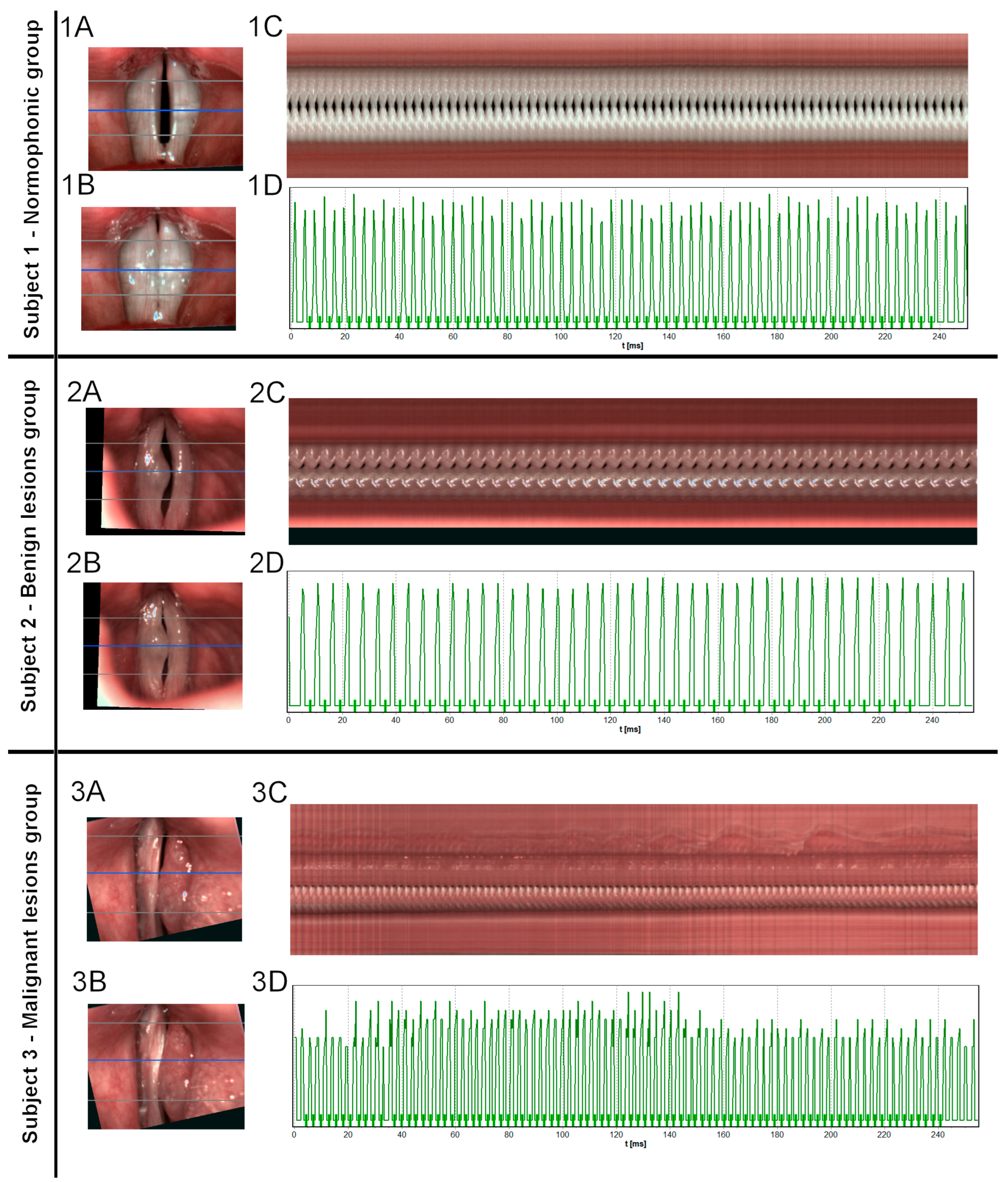
3.1. HSV Images
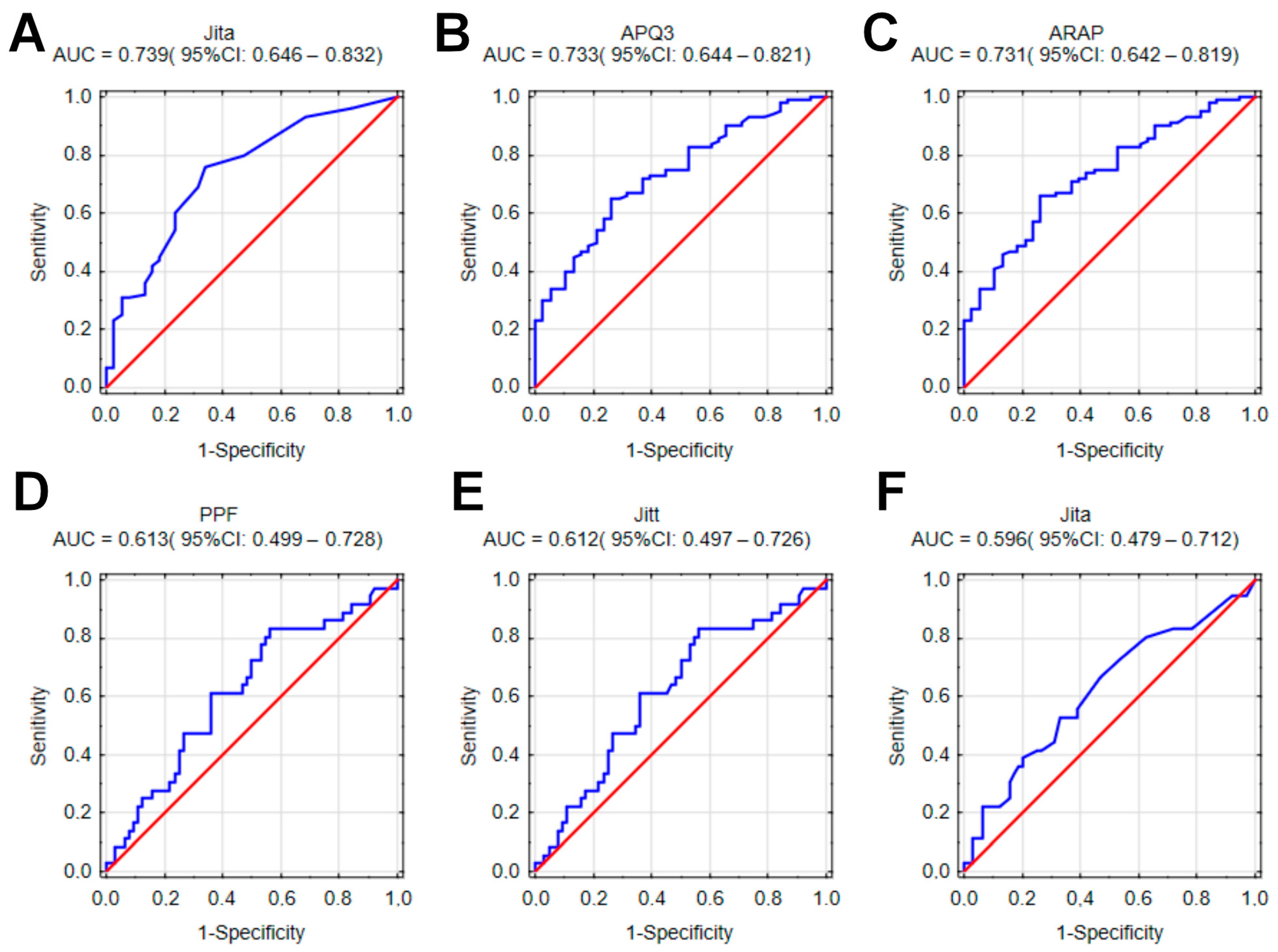
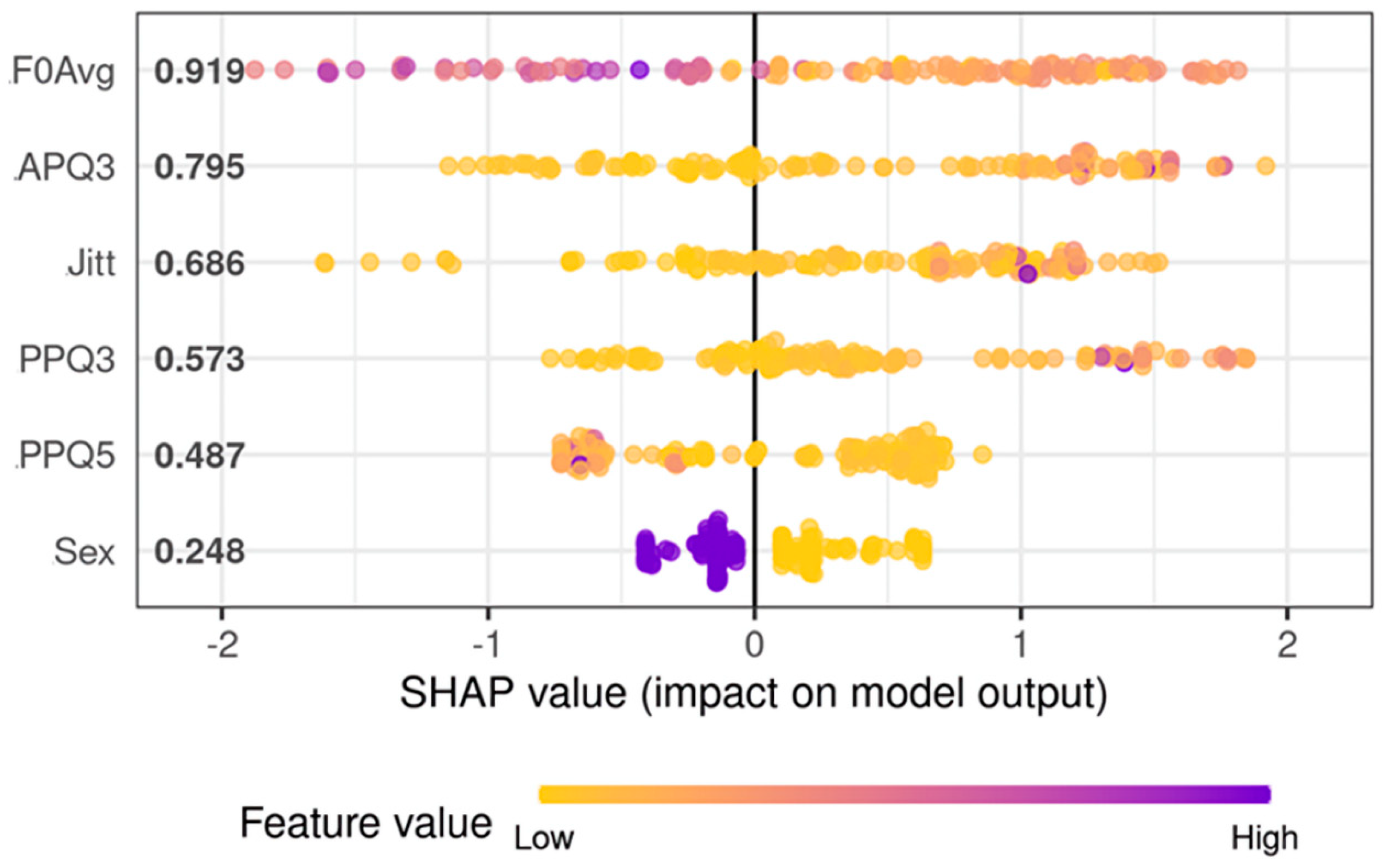
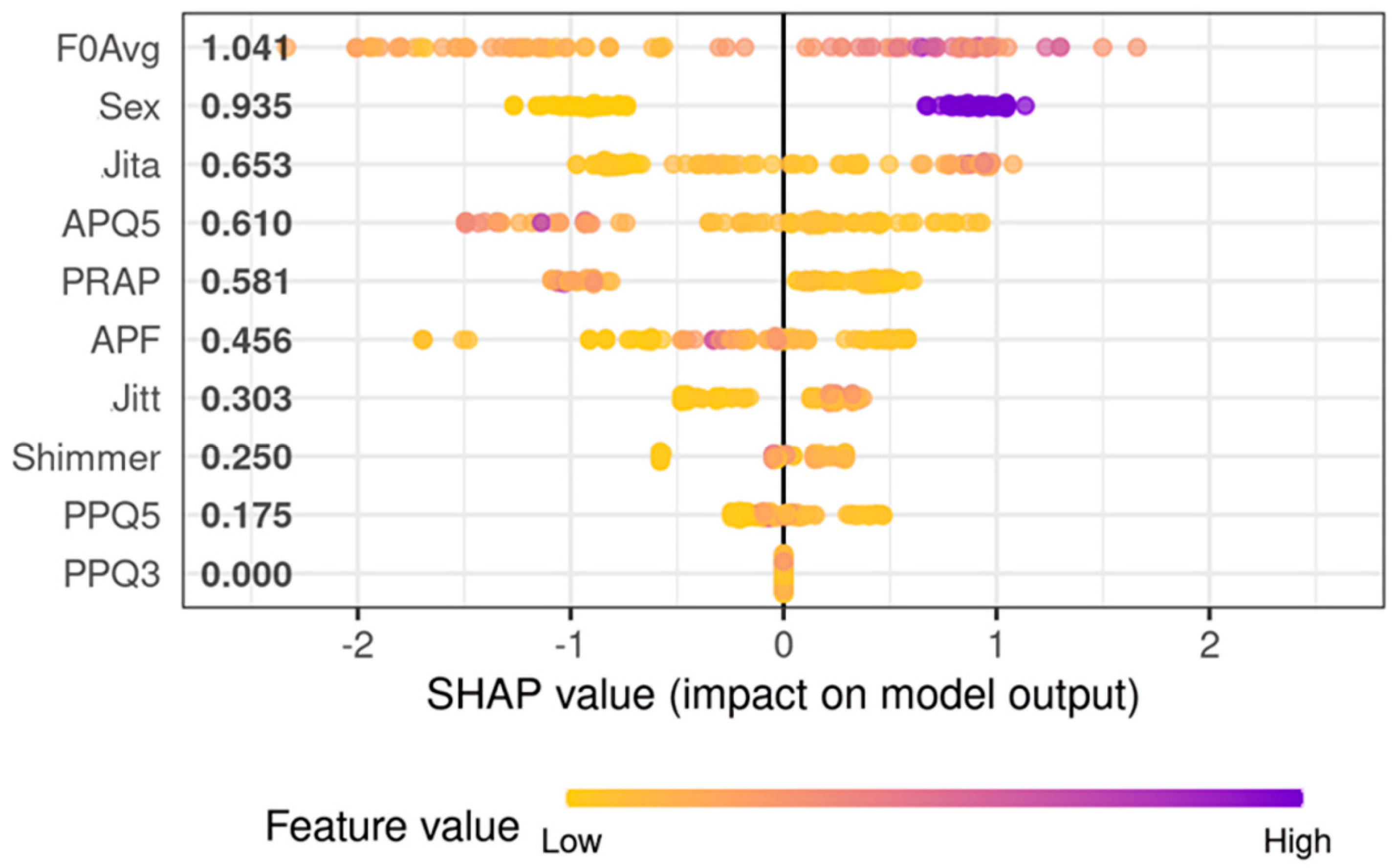
3.2. Objective Analysis—Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Phyland, D.; Miles, A. Occupational Voice Is a Work in Progress: Active Risk Management, Habilitation and Rehabilitation. Curr. Opin. Otolaryngol. Head. Neck Surg. 2019, 27, 439–447. [Google Scholar] [CrossRef] [PubMed]
- D’haeseleer, E.; Behlau, M.; Bruneel, L.; Meerschman, I.; Luyten, A.; Lambrecht, S.; Cassol, M.; Corthals, P.; Kryshtopava, M.; Wuyts, F.L.; et al. Factors Involved in Vocal Fatigue: A Pilot Study. Folia Phoniatr. Et. Logop. 2016, 68, 112–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jong, F.; Schutte, H. Principles of Physiology and Biomechanics of Voice: Aerodynamics of Voice. In Phoniatrics I Fundamentals—Voice Disorders—Disorders of Language and Hearing Development; am Zehnhoff-Dinnesen, A., Wiskirska-Woznica, B., Neumann, K., Nawka, T., Eds.; Springer: Berlin/Heidelberg, Germany, 2020; pp. 61–65. ISBN 978-3-662-46779-4. [Google Scholar]
- Woo, P. Objective Measures of Laryngeal Imaging: What Have We Learned Since Dr. Paul Moore. J. Voice 2014, 28, 69–81. [Google Scholar] [CrossRef] [PubMed]
- Niebudek-Bogusz, E.; Kopczynski, B.; Strumillo, P.; Morawska, J.; Wiktorowicz, J.; Sliwinska-Kowalska, M. Quantitative Assessment of Videolaryngostroboscopic Images in Patients with Glottic Pathologies. Logop. Phoniatr. Vocol 2017, 42, 73–83. [Google Scholar] [CrossRef]
- Rosen, C.A. Stroboscopy as a Research Instrument: Development of a Perceptual Evaluation Tool. Laryngoscope 2005, 115, 423–428. [Google Scholar] [CrossRef]
- Dejonckere, P.H.; Bradley, P.; Clemente, P.; Cornut, G.; Crevier-Buchman, L.; Friedrich, G.; van de Heyning, P.; Remacle, M.; Woisard, V. A Basic Protocol for Functional Assessment of Voice Pathology, Especially for Investigating the Efficacy of (Phonosurgical) Treatments and Evaluating New Assessment Techniques. Eur. Arch. Oto-Rhino-Laryngol. 2001, 258, 77–82. [Google Scholar] [CrossRef]
- Poburka, B.J.; Patel, R.R.; Bless, D.M. Voice-Vibratory Assessment with Laryngeal Imaging (VALI) Form: Reliability of Rating Stroboscopy and High-Speed Videoendoscopy. J. Voice 2017, 31, 513.e1–513.e14. [Google Scholar] [CrossRef]
- Schade, G.; Müller, F. High Speed Glottographic Diagnostics in Laryngology. HNO 2005, 53, 1085–1091. [Google Scholar] [CrossRef]
- Chao, S.; Song, S.A. Videostroboscopy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Woo, P. Objective Measures of Stroboscopy and High-Speed Video. Adv. Otorhinolaryngol. 2020, 85, 25–44. [Google Scholar] [CrossRef]
- Zacharias, S.R.C.; Deliyski, D.D.; Gerlach, T.T. Utility of Laryngeal High-Speed Videoendoscopy in Clinical Voice Assessment. J. Voice 2018, 32, 216–220. [Google Scholar] [CrossRef]
- Deliyski, D.D.; Powell, M.E.G.; Zacharias, S.R.C.; Gerlach, T.T.; de Alarcon, A. Experimental Investigation on Minimum Frame Rate Requirements of High-Speed Videoendoscopy for Clinical Voice Assessment. Biomed. Signal Process Control 2015, 17, 21–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schützenberger, A.; Kunduk, M.; Döllinger, M.; Alexiou, C.; Dubrovskiy, D.; Semmler, M.; Seger, A.; Bohr, C. Laryngeal High-Speed Videoendoscopy: Sensitivity of Objective Parameters towards Recording Frame Rate. Biomed. Res. Int. 2016, 2016, 4575437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohd Khairuddin, K.A.; Ahmad, K.; Mohd Ibrahim, H.; Yan, Y. Analysis Method for Laryngeal High-Speed Videoendoscopy: Development of the Criteria for the Measurement Input. J. Voice 2021, 35, 636–645. [Google Scholar] [CrossRef]
- Patel, R.R.; Liu, L.; Galatsanos, N.; Bless, D.M. Differential Vibratory Characteristics of Adductor Spasmodic Dysphonia and Muscle Tension Dysphonia on High-Speed Digital Imaging. Ann. Otol. Rhinol. Laryngol. 2011, 120, 21–32. [Google Scholar] [CrossRef]
- Warhurst, S.; McCabe, P.; Heard, R.; Yiu, E.; Wang, G.; Madill, C. Quantitative Measurement of Vocal Fold Vibration in Male Radio Performers and Healthy Controls Using High-Speed Videoendoscopy. PLoS ONE 2014, 9, e101128. [Google Scholar] [CrossRef] [Green Version]
- Powell, M.E.; Deliyski, D.D.; Zeitels, S.M.; Burns, J.A.; Hillman, R.E.; Gerlach, T.T.; Mehta, D.D. Efficacy of Videostroboscopy and High-Speed Videoendoscopy to Obtain Functional Outcomes From Perioperative Ratings in Patients with Vocal Fold Mass Lesions. J. Voice 2020, 34, 769–782. [Google Scholar] [CrossRef]
- Bohr, C.; Kräck, A.; Dubrovskiy, D.; Eysholdt, U.; Svec, J.; Psychogios, G.; Ziethe, A.; Döllinger, M. Spatiotemporal Analysis of High-Speed Videolaryngoscopic Imaging of Organic Pathologies in Males. J. Speech Lang. Hear. Res. 2014, 57, 1148–1161. [Google Scholar] [CrossRef]
- Tsutsumi, M.; Isotani, S.; Pimenta, R.A.; Dajer, M.E.; Hachiya, A.; Tsuji, D.H.; Tayama, N.; Yokonishi, H.; Imagawa, H.; Yamauchi, A.; et al. High-Speed Videolaryngoscopy: Quantitative Parameters of Glottal Area Waveforms and High-Speed Kymography in Healthy Individuals. J. Voice 2017, 31, 282–290. [Google Scholar] [CrossRef]
- Piazza, C.; Mangili, S.; del Bon, F.; Gritti, F.; Manfredi, C.; Nicolai, P.; Peretti, G. Quantitative Analysis of Videokymography in Normal and Pathological Vocal Folds: A Preliminary Study. Eur. Arch. Oto-Rhino-Laryngol. 2012, 269, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Yamauchi, A.; Yokonishi, H.; Imagawa, H.; Sakakibara, K.-I.; Nito, T.; Tayama, N.; Yamasoba, T. Quantification of Vocal Fold Vibration in Various Laryngeal Disorders Using High-Speed Digital Imaging. J. Voice 2016, 30, 205–214. [Google Scholar] [CrossRef]
- Powell, M.E.; Deliyski, D.D.; Hillman, R.E.; Zeitels, S.M.; Burns, J.A.; Mehta, D.D. Comparison of Videostroboscopy to Stroboscopy Derived from High-Speed Videoendoscopy for Evaluating Patients with Vocal Fold Mass Lesions. Am. J. Speech Lang. Pathol. 2016, 25, 576–589. [Google Scholar] [CrossRef] [PubMed]
- Naghibolhosseini, M.; Deliyski, D.D.; Zacharias, S.R.C.; de Alarcon, A.; Orlikoff, R.F. Temporal Segmentation for Laryngeal High-Speed Videoendoscopy in Connected Speech. J. Voice 2018, 32, 256.e1–256.e12. [Google Scholar] [CrossRef] [PubMed]
- Malinowski, J.; Niebudek-Bogusz, E.; Just, M.; Morawska, J.; Racino, A.; Hoffman, J.; Barańska, M.; Kowalczyk, M.M.; Pietruszewska, W. Laryngeal High-Speed Videoendoscopy with Laser Illumination: A Preliminary Report. Otolaryngol. Pol. 2021, 75, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Pietruszewska, W.; Just, M.; Morawska, J.; Malinowski, J.; Hoffman, J.; Racino, A.; Barańska, M.; Kowalczyk, M.; Niebudek-Bogusz, E. Comparative Analysis of High-Speed Videolaryngoscopy Images and Sound Data Simultaneously Acquired from Rigid and Flexible Laryngoscope: A Pilot Study. Sci. Rep. 2021, 11, 20480. [Google Scholar] [CrossRef]
- Fehling, M.K.; Grosch, F.; Schuster, M.E.; Schick, B.; Lohscheller, J. Fully Automatic Segmentation of Glottis and Vocal Folds in Endoscopic Laryngeal High-Speed Videos Using a Deep Convolutional LSTM Network. PLoS ONE 2020, 15, e0227791. [Google Scholar] [CrossRef] [Green Version]
- Lohscheller, J.; Švec, J.G.; Döllinger, M. Vocal Fold Vibration Amplitude, Open Quotient, Speed Quotient and Their Variability along Glottal Length: Kymographic Data from Normal Subjects. Logop. Phoniatr. Vocol. 2013, 38, 182–192. [Google Scholar] [CrossRef]
- Svec, J.G.; Sram, F. Videokymographic Examination of Voice. In Handbook of Voice Assessments; Ma, E., You, E., Eds.; Plural Publishing: San Diego, CA, USA, 2011; pp. 129–146. [Google Scholar]
- Bohr, C.; Kraeck, A.; Eysholdt, U.; Ziethe, A.; Döllinger, M. Quantitative Analysis of Organic Vocal Fold Pathologies in Females by High-Speed Endoscopy. Laryngoscope 2013, 123, 1686–1693. [Google Scholar] [CrossRef]
- Stawiski, K.; Kaszkowiak, M.; Mikulski, D.; Hogendorf, P.; Durczyński, A.; Strzelczyk, J.; Chowdhury, D.; Fendler, W. OmicSelector: Automatic Feature Selection and Deep Learning Modeling for Omic Experiments. bioRxiv 2022. [Google Scholar] [CrossRef]
- Rodríguez-Pérez, R.; Bajorath, J. Interpretation of Machine Learning Models Using Shapley Values: Application to Compound Potency and Multi-Target Activity Predictions. J. Comput. Aided Mol. Des. 2020, 34, 1013–1026. [Google Scholar] [CrossRef]
- Kist, A.M.; Gómez, P.; Dubrovskiy, D.; Schlegel, P.; Kunduk, M.; Echternach, M.; Patel, R.; Semmler, M.; Bohr, C.; Dürr, S.; et al. A Deep Learning Enhanced Novel Software Tool for Laryngeal Dynamics Analysis. J. Speech Lang. Hear. Res. 2021, 64, 1889–1903. [Google Scholar] [CrossRef]
- Kist, A.M.; Dürr, S.; Schützenberger, A.; Döllinger, M. OpenHSV: An Open Platform for Laryngeal High-Speed Videoendoscopy. Sci. Rep. 2021, 11, 13760. [Google Scholar] [CrossRef]
- Noordzij, J.P.; Woo, P. Glottal Area Waveform Analysis of Benign Vocal Fold Lesions before and after Surgery. Ann. Otol. Rhinol. Laryngol. 2000, 109, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Yamauchi, A.; Imagawa, H.; Yokonishi, H.; Sakakibara, K.-I.; Tayama, N. Multivariate Analysis of Vocal Fold Vibrations on Various Voice Disorders Using High-Speed Digital Imaging. Appl. Sci. 2021, 11, 6284. [Google Scholar] [CrossRef]
- Ikuma, T.; Kunduk, M.; McWhorter, A.J. Objective Quantification of Pre- and Postphonosurgery Vocal Fold Vibratory Characteristics Using High-Speed Videoendoscopy and a Harmonic Waveform Model. J. Speech Lang. Hear. Res. 2014, 57, 743–757. [Google Scholar] [CrossRef]
- Gandhi, S.; Bhatta, S.; Ganesuni, D.; Ghanpur, A.D.; Saindani, S.J. High-Speed Videolaryngoscopy in Early Glottic Carcinoma Patients Following Transoral CO2 LASER Cordectomy. Eur. Arch. Oto-Rhino-Laryngol. 2021, 278, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Andrade-Miranda, G.; Stylianou, Y.; Deliyski, D.D.; Godino-Llorente, J.I.; Henrich Bernardoni, N. Laryngeal Image Processing of Vocal Folds Motion. Appl. Sci. 2020, 10, 1556. [Google Scholar] [CrossRef] [Green Version]
- Schlegel, P.; Kniesburges, S.; Dürr, S.; Schützenberger, A.; Döllinger, M. Machine Learning Based Identification of Relevant Parameters for Functional Voice Disorders Derived from Endoscopic High-Speed Recordings. Sci. Rep. 2020, 10, 10517. [Google Scholar] [CrossRef]
- Demšar, J.; Zupan, B. Hands-on Training about Overfitting. PLoS Comput. Biol. 2021, 17, e1008671. [Google Scholar] [CrossRef]
- Shwartz-Ziv, R.; Armon, A. Tabular Data: Deep Learning Is Not All You Need. Inf. Fusion 2021, 81, 84–90. [Google Scholar] [CrossRef]
- Belle, V.; Papantonis, I. Principles and Practice of Explainable Machine Learning. Front. Big Data 2021, 4, 688969. [Google Scholar] [CrossRef]
- Kaluza, J.; Niebudek-Bogusz, E.; Malinowski, J.; Strumillo, P.; Pietruszewska, W. Assessment of Vocal Fold Stiffness by Means of High-Speed Videolaryngoscopy with Laryngotopography in Prediction of Early Glottic Malignancy: Preliminary Report. Cancers 2022, 14, 4697. [Google Scholar] [CrossRef] [PubMed]
- Nogal, P.; Buchwald, M.; Staśkiewicz, M.; Kupiński, S.; Pukacki, J.; Mazurek, C.; Jackowska, J.; Wierzbicka, M. Endoluminal Larynx Anatomy Model—towards Facilitating Deep Learning and Defining Standards for Medical Images Evaluation with Artificial Intelligence Algorithms. Otolaryngol. Pol. 2022, 76, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Hamzany, Y.; Shoffel-Havakuk, H.; Devons-Sberro, S.; Shteinberg, S.; Yaniv, D.; Mizrachi, A. Single Stage Transoral Laser Microsurgery for Early Glottic Cancer. Front. Oncol. 2018, 8, 298. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Group | Training Set (n = 99) | Testing Set (n = 39) |
|---|---|---|
| Normophonic subjects | 27 | 11 |
| Subjects with benign lesion | 45 | 19 |
| Subjects with malignant lesion | 27 | 9 |
| Parameter | Normophonic Subjects | Subjects with Benign Lesion | Subjects with Malignant Lesion | p-Value |
|---|---|---|---|---|
| F0Avg [Hz] | 259.04 ± 107.33 | 223.2 ± 78.04 | 224.77 ± 72.99 | p = 0.1700 |
| Jitt [%] | 1.3 ± 1.14 | 3 ± 3.99 | 4.26 ± 5.51 | p = 0.0002 |
| Jita [ms] | 0.06 ± 0.08 | 0.14 ± 0.2 | 0.21 ± 0.27 | p < 0.0001 |
| PPF [%] | 1.29 ± 1.1 | 2.96 ± 3.93 | 4.24 ± 5.42 | p = 0.0002 |
| PRAP [%] | 0.72 ± 0.64 | 1.71 ± 2.28 | 2.3 ± 3.18 | p = 0.0004 |
| PPQ3 [%] | 0.71 ± 0.62 | 1.69 ± 2.25 | 2.32 ± 3.21 | p = 0.0004 |
| PPQ5 [%] | 0.75 ± 0.73 | 1.74 ± 2.6 | 2.32 ±3.6 | p = 0.0008 |
| Shimmer [%] | 3.85 ± 3.55 | 10.21 ± 11.87 | 10.81 ± 5.14 | p = 0.0005 |
| APF [%] | 3.89 ± 3.62 | 10.78 ± 12.91 | 11.39 ± 14.87 | p = 0.0006 |
| ARAP [%] | 1.81 ± 1.63 | 5.5 ± 6.42 | 5.36 ± 6.93 | p = 0.0002 |
| APQ3 [%] | 1.82 ± 1.64 | 5.81 ± 6.95 | 5.57 ± 7.15 | p = 0.0001 |
| APQ5 [%] | 2.14 ± 2 | 6.29 ± 7.48 | 6.09 ± 8.02 | p = 0.0006 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malinowski, J.; Pietruszewska, W.; Stawiski, K.; Kowalczyk, M.; Barańska, M.; Rycerz, A.; Niebudek-Bogusz, E. High-Speed Videoendoscopy Enhances the Objective Assessment of Glottic Organic Lesions: A Case-Control Study with Multivariable Data-Mining Model Development. Cancers 2023, 15, 3716. https://doi.org/10.3390/cancers15143716
Malinowski J, Pietruszewska W, Stawiski K, Kowalczyk M, Barańska M, Rycerz A, Niebudek-Bogusz E. High-Speed Videoendoscopy Enhances the Objective Assessment of Glottic Organic Lesions: A Case-Control Study with Multivariable Data-Mining Model Development. Cancers. 2023; 15(14):3716. https://doi.org/10.3390/cancers15143716
Chicago/Turabian StyleMalinowski, Jakub, Wioletta Pietruszewska, Konrad Stawiski, Magdalena Kowalczyk, Magda Barańska, Aleksander Rycerz, and Ewa Niebudek-Bogusz. 2023. "High-Speed Videoendoscopy Enhances the Objective Assessment of Glottic Organic Lesions: A Case-Control Study with Multivariable Data-Mining Model Development" Cancers 15, no. 14: 3716. https://doi.org/10.3390/cancers15143716
APA StyleMalinowski, J., Pietruszewska, W., Stawiski, K., Kowalczyk, M., Barańska, M., Rycerz, A., & Niebudek-Bogusz, E. (2023). High-Speed Videoendoscopy Enhances the Objective Assessment of Glottic Organic Lesions: A Case-Control Study with Multivariable Data-Mining Model Development. Cancers, 15(14), 3716. https://doi.org/10.3390/cancers15143716







