Risk-Stratified Therapy for Pediatric Acute Myeloid Leukemia
Abstract
:Simple Summary
Abstract
1. Introduction
2. Prognostic Factors and Risk Stratification in Pediatric AML
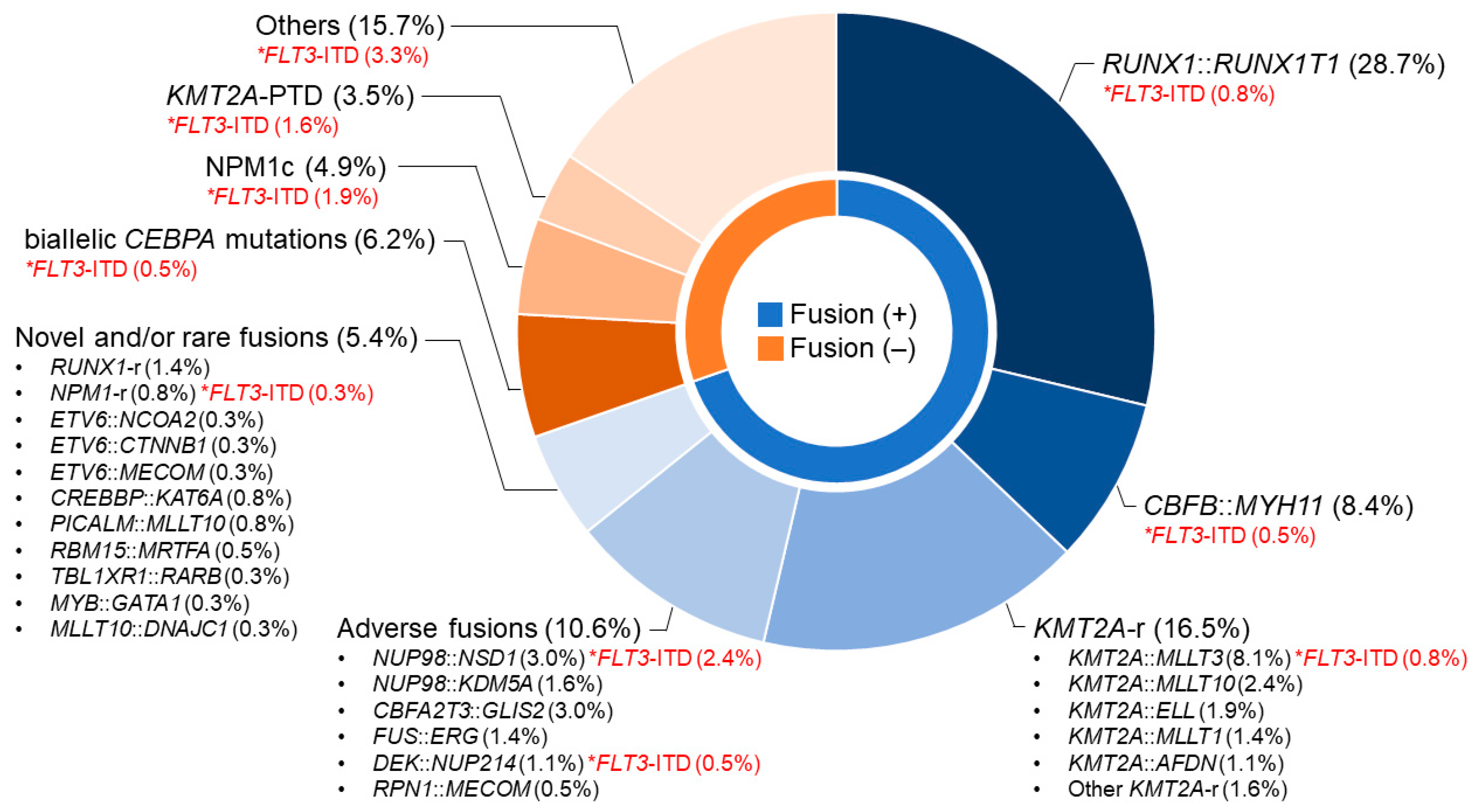
2.1. Leukemia-Specific Cytogenetics/Molecular Genetics
2.2. Treatment Response Including Measurable Residual Disease
2.3. Risk Stratification in Pediatric AML
3. Current Standard Therapy for Pediatric AML
3.1. Chemotherapy
3.2. Hematopoietic Stem Cell Transplantation
4. Novel Therapy for Pediatric AML
4.1. FLT3 Inhibitors
4.2. BCL2 Inhibitors
4.3. Menin Inhibitors
4.4. Others
5. Conclusions and Future Directions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Creutzig, U.; van den Heuvel-Eibrink, M.M.; Gibson, B.; Dworzak, M.N.; Adachi, S.; de Bont, E.; Harbott, J.; Hasle, H.; Johnston, D.; Kinoshita, A.; et al. Diagnosis and management of acute myeloid leukemia in children and adolescents: Recommendations from an international expert panel. Blood 2012, 120, 3187–3205. [Google Scholar] [CrossRef] [PubMed]
- Khoury, J.D.; Solary, E.; Abla, O.; Akkari, Y.; Alaggio, R.; Apperley, J.F.; Bejar, R.; Berti, E.; Busque, L.; Chan, J.K.C.; et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic Neoplasms. Leukemia 2022, 36, 1703–1719. [Google Scholar] [CrossRef] [PubMed]
- Pfister, S.M.; Reyes-Múgica, M.; Chan, J.K.; Hasle, H.; Lazar, A.J.; Rossi, S.; Ferrari, A.; Jarzembowski, J.A.; Pritchard-Jones, K.; Hill, D.A.; et al. A Summary of the Inaugural WHO Classification of Pediatric Tumors: Transitioning from the Optical into the Molecular Era. Cancer Discov. 2022, 12, 331–355. [Google Scholar] [CrossRef] [PubMed]
- Arber, D.A.; Orazi, A.; Hasserjian, R.P.; Borowitz, M.J.; Calvo, K.R.; Kvasnicka, H.-M.; Wang, S.A.; Bagg, A.; Barbui, T.; Branford, S.; et al. International Consensus Classification of Myeloid Neoplasms and Acute Leukemias: Integrating morphologic, clinical, and genomic data. Blood 2022, 140, 1200–1228. [Google Scholar] [CrossRef]
- Bolouri, H.; Farrar, J.E.; Triche, T., Jr.; Ries, R.E.; Lim, E.L.; Alonzo, T.A.; Ma, Y.; Moore, R.; Mungall, A.J.; Marra, M.A.; et al. The molecular landscape of pediatric acute myeloid leukemia reveals recurrent structural alterations and age-specific mutational interactions. Nat. Med. 2018, 24, 103–112. [Google Scholar] [CrossRef]
- Tomizawa, D.; Tawa, A.; Watanabe, T.; Saito, A.M.; Kudo, K.; Taga, T.; Iwamoto, S.; Shimada, A.; Terui, K.; Moritake, H.; et al. Excess treatment reduction including anthracyclines results in higher incidence of relapse in core binding factor acute myeloid leukemia in children. Leukemia 2013, 27, 2413–2416. [Google Scholar] [CrossRef]
- Hasegawa, D.; Tawa, A.; Tomizawa, D.; Watanabe, T.; Saito, A.M.; Kudo, K.; Taga, T.; Iwamoto, S.; Shimada, A.; Terui, K.; et al. Attempts to optimize postinduction treatment in childhood acute myeloid leukemia without core-binding factors: A report from the Japanese Pediatric Leukemia/Lymphoma Study Group (JPLSG). Pediatr. Blood Cancer 2020, 67, e28692. [Google Scholar] [CrossRef]
- Tomizawa, D.; Tanaka, S.; Hasegawa, D.; Iwamoto, S.; Hiramatsu, H.; Kiyokawa, N.; Miyachi, H.; Horibe, K.; Saito, A.M.; Taga, T.; et al. Evaluation of high-dose cytarabine in induction therapy for children with de novo acute myeloid leukemia: A study protocol of the Japan Children’s Cancer Group Multi-Center Seamless Phase II–III Randomized Trial (JPLSG AML-12). Jpn. J. Clin. Oncol. 2018, 48, 587–593. [Google Scholar] [CrossRef]
- Gamis, A.S.; Alonzo, T.A.; Meshinchi, S.; Sung, L.; Gerbing, R.B.; Raimondi, S.C.; Hirsch, B.A.; Kahwash, S.B.; Heerema-McKenney, A.; Winter, L.; et al. Gemtuzumab ozogamicin in children and adolescents with de novo acute myeloid leukemia improves event-free survival by reducing relapse risk: Results from the randomized phase III Children’s Oncology Group trial AAML0531. J. Clin. Oncol. 2014, 32, 3021–3032. [Google Scholar] [CrossRef]
- Aplenc, R.; Meshinchi, S.; Sung, L.; Alonzo, T.; Choi, J.; Fisher, B.; Gerbing, R.; Hirsch, B.; Horton, T.; Kahwash, S.; et al. Bortezomib with standard chemotherapy for children with acute myeloid leukemia does not improve treatment outcomes: A report from the Children’s Oncology Group. Haematologica 2020, 105, 1879–1886. [Google Scholar] [CrossRef]
- Rubnitz, J.E.; Inaba, H.; Dahl, G.; Ribeiro, R.C.; Bowman, W.P.; Taub, J.; Pounds, S.; Razzouk, B.I.; Lacayo, N.J.; Cao, X.; et al. Minimal residual disease-directed therapy for childhood acute myeloid leukaemia: Results of the AML02 multicentre trial. Lancet Oncol. 2010, 11, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Rubnitz, J.E.; Lacayo, N.J.; Inaba, H.; Heym, K.; Ribeiro, R.C.; Taub, J.; McNeer, J.; Degar, B.; Schiff, D.; Yeoh, A.E.-J.; et al. Clofarabine Can Replace Anthracyclines and Etoposide in Remission Induction Therapy for Childhood Acute Myeloid Leukemia: The AML08 Multicenter, Randomized Phase III Trial. J. Clin. Oncol. 2019, 37, 2072–2081. [Google Scholar] [CrossRef] [PubMed]
- Creutzig, U.; Zimmermann, M.; Bourquin, J.-P.; Dworzak, M.N.; Fleischhack, G.; Graf, N.; Klingebiel, T.; Kremens, B.; Lehrnbecher, T.; Von Neuhoff, C.; et al. Randomized trial comparing liposomal daunorubicin with idarubicin as induction for pediatric acute myeloid leukemia: Results from Study AML-BFM 2004. Blood 2013, 122, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Pession, A.; Masetti, R.; Rizzari, C.; Putti, M.C.; Casale, F.; Fagioli, F.; Luciani, M.; Nigro, L.L.; Menna, G.; Micalizzi, C.; et al. Results of the AIEOP AML 2002/01 multicenter prospective trial for the treatment of children with acute myeloid leukemia. Blood 2013, 122, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsson, J.; Forestier, E.; Heldrup, J.; Jahnukainen, K.; Jónsson, G.; Lausen, B.; Palle, J.; Zeller, B.; Hasle, H. Response-guided induction therapy in pediatric acute myeloid leukemia with excellent remission rate. J. Clin. Oncol. 2011, 29, 310–315. [Google Scholar] [CrossRef]
- De Moerloose, B.; Reedijk, A.; De Bock, G.H.; Lammens, T.; de Haas, V.; Denys, B.; Dedeken, L.; van den Heuvel-Eibrink, L.L.; te Loo, M.; Uyttebroeck, A.; et al. Response-guided chemotherapy for pediatric acute myeloid leukemia without hematopoietic stem cell transplantation in first complete remission: Results from protocol DB AML-01. Pediatr. Blood Cancer 2019, 66, e27605. [Google Scholar] [CrossRef]
- Petit, A.; Ducassou, S.; Leblanc, T.; Pasquet, M.; Rousseau, A.; Ragu, C.; Cachanado, M.; Nelken, B.; Bertrand, Y.; Michel, G.; et al. Maintenance Therapy With Interleukin-2 for Childhood AML: Results of ELAM02 Phase III Randomized Trial. Hemasphere 2018, 2, e159. [Google Scholar] [CrossRef]
- Rasche, M.; Zimmermann, M.; Borschel, L.; Bourquin, J.-P.; Dworzak, M.; Klingebiel, T.; Lehrnbecher, T.; Creutzig, U.; Klusmann, J.-H.; Reinhardt, D. Successes and challenges in the treatment of pediatric acute myeloid leukemia: A retrospective analysis of the AML-BFM trials from 1987 to 2012. Leukemia 2018, 32, 2167–2177. [Google Scholar] [CrossRef]
- Creutzig, U.; Kutny, M.A.; Barr, R.; Schlenk, R.F.; Ribeiro, R.C. Acute myelogenous leukemia in adolescents and young adults. Pediatr. Blood Cancer 2018, 65, e27089. [Google Scholar] [CrossRef]
- Aplenc, R.; Alonzo, T.A.; Gerbing, R.B.; Smith, F.O.; Meshinchi, S.; Ross, J.A.; Perentesis, J.; Woods, W.G.; Lange, B.J.; Davies, S.M. Ethnicity and survival in childhood acute myeloid leukemia: A report from the Children’s Oncology Group. Blood 2006, 108, 74–80. [Google Scholar] [CrossRef]
- Liu, T.; Rao, J.; Hu, W.; Cui, B.; Cai, J.; Liu, Y.; Sun, H.; Chen, X.; Tang, Y.; Chen, J.; et al. Distinct genomic landscape of Chinese pediatric acute myeloid leukemia impacts clinical risk classification. Nat. Commun. 2022, 13, 1640. [Google Scholar] [CrossRef] [PubMed]
- Shiba, N.; Yoshida, K.; Hara, Y.; Yamato, G.; Shiraishi, Y.; Matsuo, H.; Okuno, Y.; Chiba, K.; Tanaka, H.; Kaburagi, T.; et al. Transcriptome analysis offers a comprehensive illustration of the genetic background of pediatric acute myeloid leukemia. Blood Adv. 2019, 3, 3157–3169. [Google Scholar] [CrossRef] [PubMed]
- Harrison, C.J.; Hills, R.K.; Moorman, A.V.; Grimwade, D.J.; Hann, I.; Webb, D.K.; Wheatley, K.; de Graaf, S.S.; Berg, E.v.D.; Burnett, A.K.; et al. Cytogenetics of childhood acute myeloid leukemia: United Kingdom Medical Research Council Treatment trials AML 10 and 12. J. Clin. Oncol. 2010, 28, 2674–2681. [Google Scholar] [CrossRef]
- Balgobind, B.V.; Raimondi, S.C.; Harbott, J.; Zimmermann, M.; Alonzo, T.A.; Auvrignon, A.; Beverloo, H.B.; Chang, M.; Creutzig, U.; Dworzak, M.N.; et al. Novel prognostic subgroups in childhood 11q23/MLL-rearranged acute myeloid leukemia: Results of an international retrospective study. Blood 2009, 114, 2489–2496. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.; Larghero, P.; Lopes, B.A.; Burmeister, T.; Gröger, D.; Sutton, R.; Venn, N.C.; Cazzaniga, G.; Abascal, L.C.; Tsaur, G.; et al. The KMT2A recombinome of acute leukemias in 2023. Leukemia 2023, 37, 988–1005. [Google Scholar] [CrossRef]
- Coenen, E.A.; Zwaan, C.M.; Reinhardt, D.; Harrison, C.J.; Haas, O.A.; de Haas, V.; Mihál, V.; De Moerloose, B.; Jeison, M.; Rubnitz, J.E.; et al. Pediatric acute myeloid leukemia with t(8;16)(p11;p13), a distinct clinical and biological entity: A collaborative study by the International-Berlin-Frankfurt-Munster AML-study group. Blood 2013, 122, 2704–2713. [Google Scholar] [CrossRef]
- Sandahl, J.D.; Coenen, E.A.; Forestier, E.; Harbott, J.; Johansson, B.; Kerndrup, G.; Adachi, S.; Auvrignon, A.; Beverloo, H.B.; Cayuela, J.-M.; et al. t(6;9)(p22;q34)/DEK-NUP214-rearranged pediatric myeloid leukemia: An international study of 62 patients. Haematologica 2014, 99, 865–872. [Google Scholar] [CrossRef]
- Klein, K.; Kaspers, G.; Harrison, C.J.; Beverloo, H.B.; Reedijk, A.; Bongers, M.; Cloos, J.; Pession, A.; Reinhardt, D.; Zimmerman, M.; et al. Clinical Impact of Additional Cytogenetic Aberrations, cKIT and RAS Mutations, and Treatment Elements in Pediatric t(8;21)-AML: Results From an International Retrospective Study by the International Berlin-Frankfurt-Munster Study Group. J. Clin. Oncol. 2015, 33, 4247–4258. [Google Scholar] [CrossRef]
- Noort, S.; Zimmermann, M.; Reinhardt, D.; Cuccuini, W.; Pigazzi, M.; Smith, J.; Ries, R.E.; Alonzo, T.A.; Hirsch, B.; Tomizawa, D.; et al. Prognostic impact of t(16;21)(p11;q22) and t(16;21)(q24;q22) in pediatric AML: A retrospective study by the I-BFM Study Group. Blood 2018, 132, 1584–1592. [Google Scholar] [CrossRef]
- Hammer, A.S.B.; Juul-Dam, K.L.; Sandahl, J.D.; Abrahamsson, J.; Czogala, M.; Delabesse, E.; Haltrich, I.; Jahnukainen, K.; Kolb, E.A.; Kovács, G.T.; et al. Hypodiploidy has unfavorable impact on survival in pediatric acute myeloid leukemia: An I-BFM Study Group collaboration. Blood Adv. 2023, 7, 1045–1055. [Google Scholar] [CrossRef]
- Gruber, T.A.; Gedman, A.L.; Zhang, J.; Koss, C.S.; Marada, S.; Ta, H.Q.; Chen, S.-C.; Su, X.; Ogden, S.K.; Dang, J.; et al. An Inv(16)(p13.3q24.3)-encoded CBFA2T3-GLIS2 fusion protein defines an aggressive subtype of pediatric acute megakaryoblastic leukemia. Cancer Cell 2012, 22, 683–697. [Google Scholar] [CrossRef] [PubMed]
- de Rooij, J.D.; Hollink, I.H.; Arentsen-Peters, S.T.C.J.M.; Van Galen, J.F.; Berna Beverloo, H.; Baruchel, A.; Trka, J.; Reinhardt, D.; Sonneveld, E.; Zimmermann, M.; et al. NUP98/JARID1A is a novel recurrent abnormality in pediatric acute megakaryoblastic leukemia with a distinct HOX gene expression pattern. Leukemia 2013, 27, 2280–2288. [Google Scholar] [CrossRef] [PubMed]
- de Rooij, J.D.; Branstetter, C.; Ma, J.; Li, Y.; Walsh, M.P.; Cheng, J.; Obulkasim, A.; Dang, J.; Easton, J.; Verboon, L.J.; et al. Pediatric non-Down syndrome acute megakaryoblastic leukemia is characterized by distinct genomic subsets with varying outcomes. Nat. Genet. 2017, 49, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Meshinchi, S.; Alonzo, T.A.; Stirewalt, D.L.; Zwaan, M.; Zimmerman, M.; Reinhardt, D.; Kaspers, G.J.L.; Heerema, N.A.; Gerbing, R.; Lange, B.J.; et al. Clinical implications of FLT3 mutations in pediatric AML. Blood 2006, 108, 3654–3661. [Google Scholar] [CrossRef] [PubMed]
- Hollink, I.H.I.M.; Zwaan, C.M.; Zimmermann, M.; Arentsen-Peters, T.C.J.M.; Pieters, R.; Cloos, J.; Kaspers, G.J.L.; de Graaf, S.S.N.; Harbott, J.; Creutzig, U.; et al. Favorable prognostic impact of NPM1 gene mutations in childhood acute myeloid leukemia, with emphasis on cytogenetically normal AML. Leukemia 2009, 23, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Hollink, I.H.; van den Heuvel-Eibrink, M.M.; Arentsen-Peters, S.T.C.J.M.; Zimmermann, M.; Peeters, J.K.; Valk, P.J.; Balgobind, B.V.; Sonneveld, E.; Kaspers, G.J.; de Bont, E.S.; et al. Characterization of CEBPA mutations and promoter hypermethylation in pediatric acute myeloid leukemia. Haematologica 2011, 96, 384–392. [Google Scholar] [CrossRef] [PubMed]
- Tarlock, K.; Lamble, A.J.; Wang, Y.C.; Gerbing, R.B.; Ries, R.E.; Loken, M.R.; Brodersen, L.E.; Pardo, L.; Leonti, A.; Smith, J.L.; et al. CEBPA-bZip mutations are associated with favorable prognosis in de novo AML: A report from the Children’s Oncology Group. Blood 2021, 138, 1137–1147. [Google Scholar] [CrossRef]
- Dohner, H.; Weisdorf, D.J.; Bloomfield, C.D. Acute Myeloid Leukemia. N. Engl. J. Med. 2015, 373, 1136–1152. [Google Scholar] [CrossRef]
- Damm, F.; Thol, F.; Hollink, I.; Zimmermann, M.; Reinhardt, K.; van den Heuvel-Eibrink, M.M.; Zwaan, C.M.; de Haas, V.; Creutzig, U.; Klusmann, J.-H.; et al. Prevalence and prognostic value of IDH1 and IDH2 mutations in childhood AML: A study of the AML-BFM and DCOG study groups. Leukemia 2011, 25, 1704–1710. [Google Scholar] [CrossRef]
- Hollink, I.H.I.M.; Feng, Q.; Danen-van Oorschot, A.A.; Arentsen-Peters, S.T.C.J.M.; Verboon, L.J.; Zhang, P.; de Haas, V.; Reinhardt, D.; Creutzig, U.; Trka, J.; et al. Low frequency of DNMT3A mutations in pediatric AML, and the identification of the OCI-AML3 cell line as an in vitro model. Leukemia 2012, 26, 371–373. [Google Scholar] [CrossRef]
- Döhner, H.; Wei, A.H.; Appelbaum, F.R.; Craddock, C.; DiNardo, C.D.; Dombret, H.; Ebert, B.L.; Fenaux, P.; Godley, L.A.; Hasserjian, R.P.; et al. Diagnosis and management of AML in adults: 2022 recommendations from an international expert panel on behalf of the ELN. Blood 2022, 140, 1345–1377. [Google Scholar] [CrossRef] [PubMed]
- Cucchi, D.G.J.; Bachas, C.; Klein, K.; Huttenhuis, S.; Zwaan, C.M.; Ossenkoppele, G.J.; Janssen, J.M.W.M.; Kaspers, G.L.; Cloos, J. TP53 mutations and relevance of expression of TP53 pathway genes in paediatric acute myeloid leukaemia. Br. J. Haematol. 2020, 188, 736–739. [Google Scholar] [CrossRef]
- Hollink, I.H.; van den Heuvel-Eibrink, M.M.; Arentsen-Peters, S.T.; Pratcorona, M.; Abbas, S.; Kuipers, J.E.; van Galen, J.F.; Beverloo, H.B.; Sonneveld, E.; Kaspers, G.-J.J.L.; et al. NUP98/NSD1 characterizes a novel poor prognostic group in acute myeloid leukemia with a distinct HOX gene expression pattern. Blood 2011, 118, 3645–3656. [Google Scholar] [CrossRef] [PubMed]
- Bertrums, E.J.; Smith, J.L.; Harmon, L.; Ries, R.E.; Wang, Y.-C.J.; Alonzo, T.A.; Menssen, A.J.; Chisholm, K.M.; Leonti, A.R.; Tarlock, K.; et al. Comprehensive molecular and clinical characterization of NUP98 fusions in pediatric acute myeloid leukemia. Haematologica 2023, 108, 2044–2058. [Google Scholar] [CrossRef] [PubMed]
- Umeda, M.; Ma, J.; Huang, B.J.; Hagiwara, K.; Westover, T.; Abdelhamed, S.; Barajas, J.M.; Thomas, M.E.; Walsh, M.P.; Song, G.; et al. Integrated Genomic Analysis Identifies UBTF Tandem Duplications as a Recurrent Lesion in Pediatric Acute Myeloid Leukemia. Blood Cancer Discov. 2022, 3, 194–207. [Google Scholar] [CrossRef]
- Wheatley, K.; Burnett, A.K.; Goldstone, A.H.; Gray, R.G.; Hann, I.M.; Harrison, C.J.; Rees, J.K.H.; Stevens, R.F.; Walker, H. A simple, robust, validated and highly predictive index for the determination of risk-directed therapy in acute myeloid leukaemia derived from the MRC AML 10 trial. United Kingdom Medical Research Council’s Adult and Childhood Leukaemia Working Parties. Br. J. Haematol. 1999, 107, 69–79. [Google Scholar] [CrossRef]
- Gibson, B.E.S.; Webb, D.K.H.; Howman, A.J.; De Graaf, S.S.N.; Harrison, C.J.; Wheatley, K.; the United Kingdom Childhood Leukaemia Working Group and the Dutch Childhood Oncology Group. Results of a randomized trial in children with Acute Myeloid Leukaemia: Medical research council AML12 trial. Br. J. Haematol. 2011, 155, 366–376. [Google Scholar] [CrossRef]
- Creutzig, U.; Zimmermann, M.; Ritter, J.; Henze, G.; Graf, N.; Löffler, H.; Schellong, G. Definition of a standard-risk group in children with AML. Br. J. Haematol. 1999, 104, 630–639. [Google Scholar] [CrossRef]
- Inaba, H.; Coustan-Smith, E.; Cao, X.; Pounds, S.B.; Shurtleff, S.A.; Wang, K.Y.; Raimondi, S.C.; Onciu, M.; Jacobsen, J.; Ribeiro, R.C.; et al. Comparative analysis of different approaches to measure treatment response in acute myeloid leukemia. J. Clin. Oncol. 2012, 30, 3625–3632. [Google Scholar] [CrossRef]
- Heuser, M.; Freeman, S.D.; Ossenkoppele, G.J.; Buccisano, F.; Hourigan, C.S.; Ngai, L.L.; Tettero, J.M.; Bachas, C.; Baer, C.; Béné, M.C.; et al. 2021 Update Measurable Residual Disease in Acute Myeloid Leukemia: European LeukemiaNet Working Party Consensus Document. Blood 2021, 138, 2753–2767. [Google Scholar] [CrossRef]
- Coustan-Smith, E.; Ribeiro, R.C.; Rubnitz, J.E.; Razzouk, B.I.; Pui, C.-H.; Pounds, S.; Andreansky, M.; Behm, F.G.; Raimondi, S.C.; Shurtleff, S.A.; et al. Clinical significance of residual disease during treatment in childhood acute myeloid leukaemia. Br. J. Haematol. 2003, 123, 243–252. [Google Scholar] [CrossRef] [PubMed]
- Langebrake, C.; Creutzig, U.; Dworzak, M.; Hrusak, O.; Mejstrikova, E.; Griesinger, F.; Zimmermann, M.; Reinhardt, D. Residual disease monitoring in childhood acute myeloid leukemia by multiparameter flow cytometry: The MRD-AML-BFM Study Group. J. Clin. Oncol. 2006, 24, 3686–3692. [Google Scholar] [CrossRef] [PubMed]
- van der Velden, V.H.J.; van der Sluijs-Geling, A.; Gibson, B.E.S.; te Marvelde, J.G.; Hoogeveen, P.G.; Hop, W.C.J.; Wheatley, K.; Bierings, M.B.; Schuurhuis, G.J.; de Graaf, S.S.N.; et al. Clinical significance of flowcytometric minimal residual disease detection in pediatric acute myeloid leukemia patients treated according to the DCOG ANLL97/MRC AML12 protocol. Leukemia 2010, 24, 1599–1606. [Google Scholar] [CrossRef] [PubMed]
- Tierens, A.; Bjørklund, E.; Siitonen, S.; Marquart, H.V.; -Juergensen, G.W.; Pelliniemi, T.-T.; Forestier, E.; Hasle, H.; Jahnukainen, K.; Lausen, B.; et al. Residual disease detected by flow cytometry is an independent predictor of survival in childhood acute myeloid leukaemia; results of the NOPHO-AML 2004 study. Br. J. Haematol. 2016, 174, 600–609. [Google Scholar] [CrossRef] [PubMed]
- Buldini, B.; Rizzati, F.; Masetti, R.; Fagioli, F.; Menna, G.; Micalizzi, C.; Putti, M.C.; Rizzari, C.; Santoro, N.; Zecca, M.; et al. Prognostic significance of flow-cytometry evaluation of minimal residual disease in children with acute myeloid leukaemia treated according to the AIEOP-AML 2002/01 study protocol. Br. J. Haematol. 2017, 177, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Sievers, E.L.; Lange, B.J.; Alonzo, T.A.; Gerbing, R.B.; Bernstein, I.D.; Smith, F.O.; Arceci, R.J.; Woods, W.G.; Loken, M.R. Immunophenotypic evidence of leukemia after induction therapy predicts relapse: Results from a prospective Children’s Cancer Group study of 252 patients with acute myeloid leukemia. Blood 2003, 101, 3398–3406. [Google Scholar] [CrossRef]
- Loken, M.R.; Alonzo, T.A.; Pardo, L.; Gerbing, R.B.; Raimondi, S.C.; Hirsch, B.A.; Ho, P.A.; Franklin, J.; Cooper, T.M.; Gamis, A.S.; et al. Residual disease detected by multidimensional flow cytometry signifies high relapse risk in patients with de novo acute myeloid leukemia: A report from Children’s Oncology Group. Blood 2012, 120, 1581–1588. [Google Scholar] [CrossRef]
- Brodersen, L.E.; Gerbing, R.B.; Pardo, M.L.; Alonzo, T.A.; Paine, D.; Fritschle, W.; Hsu, F.-C.; Pollard, J.A.; Aplenc, R.; Kahwash, S.B.; et al. Morphologic remission status is limited compared to ΔN flow cytometry: A Children’s Oncology Group AAML0531 report. Blood Adv. 2020, 4, 5050–5061. [Google Scholar] [CrossRef]
- Tomizawa, D.; Yoshida, M.; Kondo, T.; Miyamura, T.; Taga, T.; Adachi, S.; Koh, K.; Noguchi, M.; Kakuda, H.; Watanabe, K.; et al. Allogeneic hematopoietic stem cell transplantation for children and adolescents with high-risk cytogenetic AML: Distinctly poor outcomes of FUS-ERG-positive cases. Bone Marrow Transplant. 2019, 54, 393–401. [Google Scholar] [CrossRef]
- Kigasawa, H. Progress of treatment of acute myeloid leukemia in children. Jpn. J. Pediatr. Hematol. 2000, 14, 288–297. [Google Scholar]
- Tsukimoto, I.; Tawa, A.; Horibe, K.; Tabuchi, K.; Kigasawa, H.; Tsuchida, M.; Yabe, H.; Nakayama, H.; Kudo, K.; Kobayashi, R.; et al. Risk-stratified therapy and the intensive use of cytarabine improves the outcome in childhood acute myeloid leukemia: The AML99 trial from the Japanese Childhood AML Cooperative Study Group. J. Clin. Oncol. 2009, 27, 4007–4013. [Google Scholar] [CrossRef] [PubMed]
- Tomizawa, D.; Tsujimoto, S.-I.; Tanaka, S.; Matsubayashi, J.; Aoki, T.; Iwamoto, S.; Hasegawa, D.; Nagai, K.; Nakashima, K.; Kawaguchi, K.; et al. A phase III clinical trial evaluating efficacy and safety of minimal residual disease-based risk stratification for children with acute myeloid leukemia, incorporating a randomized study of gemtuzumab ozogamicin in combination with post-induction chemotherapy for non-low-risk patients (JPLSG-AML-20). Jpn. J. Clin. Oncol. 2022, 52, 1225–1231. [Google Scholar]
- Becton, D.; Dahl, G.V.; Ravindranath, Y.; Chang, M.N.; Behm, F.G.; Raimondi, S.C.; Head, D.R.; Stine, K.C.; Lacayo, N.J.; Sikic, B.I.; et al. Randomized use of cyclosporin A (CsA) to modulate P-glycoprotein in children with AML in remission: Pediatric Oncology Group Study 9421. Blood 2006, 107, 1315–1324. [Google Scholar] [CrossRef] [PubMed]
- Creutzig, U.; Ritter, J.; Zimmermann, M.; Reinhardt, D.; Hermann, J.; Berthold, F.; Henze, G.; Jürgens, H.; Kabisch, H.; Havers, W.; et al. Improved treatment results in high-risk pediatric acute myeloid leukemia patients after intensification with high-dose cytarabine and mitoxantrone: Results of Study Acute Myeloid Leukemia-Berlin-Frankfurt-Munster 93. J. Clin. Oncol. 2001, 19, 2705–2713. [Google Scholar] [CrossRef] [PubMed]
- Creutzig, U.; Zimmermann, M.; Bourquin, J.-P.; Dworzak, M.N.; von Neuhoff, C.; Sander, A.; Schrauder, A.; Teigler-Schlegel, A.; Starý, J.; Corbacioglu, S.; et al. Second induction with high-dose cytarabine and mitoxantrone: Different impact on pediatric AML patients with t(8;21) and with inv(16). Blood 2011, 118, 5409–5415. [Google Scholar] [CrossRef] [PubMed]
- Creutzig, U.; Ritter, J.; Zimmermann, M.; Hermann, J.; Gadner, H.; Sawatzki, D.B.; Niemeyer, C.; Schwabe, D.; Selle, B.; Boos, J.; et al. Idarubicin improves blast cell clearance during induction therapy in children with AML: Results of study AML-BFM 93. AML-BFM Study Group. Leukemia 2001, 15, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Stevens, R.F.; Hann, I.M.; Wheatley, K.; Gray, R.G. Marked improvements in outcome with chemotherapy alone in paediatric acute myeloid leukemia: Results of the United Kingdom Medical Research Council’s 10th AML trial. MRC Childhood Leukaemia Working Party. Br. J. Haematol. 1998, 101, 130–140. [Google Scholar] [CrossRef]
- Getz, K.D.; Alonzo, T.A.; Sung, L.; Meshinchi, S.; Gerbing, R.B.; Raimondi, S.; Hirsch, B.; Loken, M.; Brodersen, L.E.; Kahwash, S.; et al. Cytarabine dose reduction in patients with low-risk acute myeloid leukemia: A report from the Children’s Oncology Group. Pediatr. Blood Cancer 2021, 69, e29313. [Google Scholar] [CrossRef]
- Hasle, H.; Abrahamsson, J.; Forestier, E.; Ha, S.-Y.; Heldrup, J.; Jahnukainen, K.; Jónsson, G.; Lausen, B.; Palle, J.; Zeller, B. Gemtuzumab ozogamicin as postconsolidation therapy does not prevent relapse in children with AML: Results from NOPHO-AML 2004. Blood 2012, 120, 978–984. [Google Scholar] [CrossRef]
- Perel, Y.; Auvrignon, A.; Leblanc, T.; Vannier, J.-P.; Michel, G.; Nelken, B.; Gandemer, V.; Schmitt, C.; Lamagnere, J.-P.; De Lumley, L.; et al. Impact of addition of maintenance therapy to intensive induction and consolidation chemotherapy for childhood acute myeloblastic leukemia: Results of a prospective randomized trial, LAME 89/91. Leucamie Aique Myeloide Enfant. J. Clin. Oncol. 2002, 20, 2774–2782. [Google Scholar] [CrossRef]
- Pollard, J.A.; Alonzo, T.A.; Gerbing, R.; Brown, P.; Fox, E.; Choi, J.; Fisher, B.; Hirsch, B.; Kahwash, S.; Getz, K.; et al. Sorafenib in Combination With Standard Chemotherapy for Children With High Allelic Ratio FLT3/ITD+ Acute Myeloid Leukemia: A Report From the Children’s Oncology Group Protocol AAML1031. J. Clin. Oncol. 2022, 40, 2023–2035. [Google Scholar] [CrossRef]
- Feijen, E.A.M.; Leisenring, W.M.; Stratton, K.L.; Ness, K.K.; van der Pal, H.J.H.; van Dalen, E.C.; Armstrong, G.T.; Aune, G.J.; Green, D.M.; Hudson, M.M.; et al. Derivation of Anthracycline and Anthraquinone Equivalence Ratios to Doxorubicin for Late-Onset Cardiotoxicity. JAMA Oncol. 2019, 5, 864–871. [Google Scholar] [CrossRef] [PubMed]
- Creutzig, U.; Dworzak, M.N.; Zimmermann, M.; Reinhardt, D.; Sramkova, L.; Bourquin, J.P.; Hasle, H.; Abrahamsson, J.; Kaspers, G.; van den Heuvel-Eibrink, M.M.; et al. Characteristics and outcome in patients with central nervous system involvement treated in European pediatric acute myeloid leukemia study groups. Pediatr. Blood Cancer 2017, 64, e26664. [Google Scholar] [CrossRef]
- Sauer, M.G.; Lang, P.J.; Albert, M.H.; Bader, P.; Creutzig, U.; Eyrich, M.; Greil, J.; Gruhn, B.; Holter, W.; Klingebiel, T.; et al. Hematopoietic stem cell transplantation for children with acute myeloid leukemia-results of the AML SCT-BFM 2007 trial. Leukemia 2020, 34, 613–624. [Google Scholar] [CrossRef] [PubMed]
- Tarlock, K.; Sulis, M.L.; Chewning, J.H.; Pollard, J.A.; Cooper, T.; Gamis, A.; Shenoy, S.; Kutny, M.; Horan, J.; Meshinchi, S.; et al. Hematopoietic Cell Transplantation in the Treatment of Pediatric Acute Myeloid Leukemia and Myelodysplastic Syndromes: Guidelines from the American Society of Transplantation and Cellular Therapy. Transplant. Cell. Ther. 2022, 28, 530–545. [Google Scholar] [CrossRef]
- Copelan, E.A.; Hamilton, B.K.; Avalos, B.; Ahn, K.W.; Bolwell, B.J.; Zhu, X.; Aljurf, M.; van Besien, K.; Bredeson, C.; Cahn, J.-Y.; et al. Better leukemia-free and overall survival in AML in first remission following cyclophosphamide in combination with busulfan compared with TBI. Blood 2013, 122, 3863–3870. [Google Scholar] [CrossRef] [PubMed]
- de Berranger, E.; Cousien, A.; Petit, A.; de Latour, R.P.; Galambrun, C.; Bertrand, Y.; Salmon, A.; Rialland, F.; Rohrlich, P.-S.; Vannier, J.-P.; et al. Impact on long-term OS of conditioning regimen in allogeneic BMT for children with AML in first CR: TBI+CY versus BU+CY: A report from the Societe Francaise de Greffe de Moelle et de Therapie Cellulaire. Bone Marrow Transplant. 2014, 49, 382–388. [Google Scholar] [CrossRef]
- Ishida, H.; Kato, M.; Kudo, K.; Taga, T.; Tomizawa, D.; Miyamura, T.; Goto, H.; Inagaki, J.; Koh, K.; Terui, K.; et al. Comparison of Outcomes for Pediatric Patients With Acute Myeloid Leukemia in Remission and Undergoing Allogeneic Hematopoietic Cell Transplantation With Myeloablative Conditioning Regimens Based on Either Intravenous Busulfan or Total Body Irradiation: A Report From the Japanese Society for Hematopoietic Cell Transplantation. Biol. Blood Marrow Transplant. 2015, 21, 2141–2147. [Google Scholar]
- Bitan, M.; He, W.; Zhang, M.-J.; Abdel-Azim, H.; Ayas, M.F.; Bielorai, B.; Carpenter, P.A.; Cairo, M.S.; Diaz, M.A.; Horan, J.T.; et al. Transplantation for children with acute myeloid leukemia: A comparison of outcomes with reduced intensity and myeloablative regimens. Blood 2014, 123, 1615–1620. [Google Scholar] [CrossRef]
- Ishida, H.; Adachi, S.; Hasegawa, D.; Okamoto, Y.; Goto, H.; Inagaki, J.; Inoue, M.; Koh, K.; Yabe, H.; Kawa, K.; et al. Comparison of a fludarabine and melphalan combination-based reduced toxicity conditioning with myeloablative conditioning by radiation and/or busulfan in acute myeloid leukemia in Japanese children and adolescents. Pediatr. Blood Cancer 2015, 62, 883–889. [Google Scholar] [CrossRef]
- Scott, B.L.; Pasquini, M.C.; Logan, B.R.; Wu, J.; Devine, S.M.; Porter, D.L.; Maziarz, R.T.; Warlick, E.D.; Fernandez, H.F.; Alyea, E.P.; et al. Myeloablative Versus Reduced-Intensity Hematopoietic Cell Transplantation for Acute Myeloid Leukemia and Myelodysplastic Syndromes. J. Clin. Oncol. 2017, 35, 1154–1161. [Google Scholar] [CrossRef] [PubMed]
- Stone, R.M.; Mandrekar, S.J.; Sanford, B.L.; Laumann, K.; Geyer, S.; Bloomfield, C.D.; Thiede, C.; Prior, T.W.; Döhner, K.; Marcucci, G.; et al. Midostaurin plus Chemotherapy for Acute Myeloid Leukemia with a FLT3 Mutation. N. Engl. J. Med. 2017, 377, 454–464. [Google Scholar] [CrossRef]
- Inaba, H.; Rubnitz, J.E.; Coustan-Smith, E.; Li, L.; Furmanski, B.D.; Mascara, G.P.; Heym, K.M.; Christensen, R.; Onciu, M.; Shurtleff, S.A.; et al. Phase I pharmacokinetic and pharmacodynamic study of the multikinase inhibitor sorafenib in combination with clofarabine and cytarabine in pediatric relapsed/refractory leukemia. J. Clin. Oncol. 2011, 29, 3293–3300. [Google Scholar] [CrossRef]
- Perl, A.E.; Martinelli, G.; Cortes, J.E.; Neubauer, A.; Berman, E.; Paolini, S.; Montesinos, P.; Baer, M.R.; Larson, R.A.; Ustun, C.; et al. Gilteritinib or Chemotherapy for Relapsed or Refractory FLT3-Mutated AML. N. Engl. J. Med. 2019, 381, 1728–1740. [Google Scholar] [CrossRef]
- Cortes, J.E.; Khaled, S.; Martinelli, G.; Perl, A.E.; Ganguly, S.; Russell, N.; Krämer, A.; Dombret, H.; Hogge, D.; Jonas, B.A.; et al. Quizartinib versus salvage chemotherapy in relapsed or refractory FLT3-ITD acute myeloid leukaemia (QuANTUM-R): A multicentre, randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2019, 20, 984–997. [Google Scholar] [CrossRef]
- Erba, H.P.; Montesinos, P.; Kim, H.J.; Patkowska, E.; Vrhovac, R.; Žák, P.; Wang, P.-N.; Mitov, T.; Hanyok, J.; Kamel, Y.M.; et al. Quizartinib plus chemotherapy in newly diagnosed patients with FLT3-internal-tandem-duplication-positive acute myeloid leukaemia (QuANTUM-First): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2023, 401, 1571–1583. [Google Scholar] [CrossRef] [PubMed]
- Dinardo, C.D.; Jonas, B.A.; Pullarkat, V.; Thirman, M.J.; Garcia, J.S.; Wei, A.H.; Konopleva, M.; Döhner, H.; Letai, A.; Fenaux, P.; et al. Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia. N. Engl. J. Med. 2020, 383, 617–629. [Google Scholar] [CrossRef] [PubMed]
- Wei, A.H.; Montesinos, P.; Ivanov, V.; DiNardo, C.D.; Novak, J.; Laribi, K.; Kim, I.; Stevens, D.A.; Fiedler, W.; Pagoni, M.; et al. Venetoclax plus LDAC for newly diagnosed AML ineligible for intensive chemotherapy: A phase 3 randomized placebo-controlled trial. Blood 2020, 135, 2137–2145. [Google Scholar] [CrossRef] [PubMed]
- Karol, S.E.; Alexander, T.B.; Budhraja, A.; Pounds, S.B.; Canavera, K.; Wang, L.; Wolf, J.; Klco, J.M.; Mead, P.E.; Das Gupta, S.; et al. Venetoclax in combination with cytarabine with or without idarubicin in children with relapsed or refractory acute myeloid leukaemia: A phase 1, dose-escalation study. Lancet Oncol. 2020, 21, 551–560. [Google Scholar] [CrossRef] [PubMed]
- van Weelderen, R.E.; Klein, K.; Harrison, C.J.; Jiang, Y.; Abrahamsson, J.; Arad-Cohen, N.; Bart-Delabesse, E.; Buldini, B.; De Moerloose, B.; Dworzak, M.N.; et al. Measurable Residual Disease and Fusion Partner Independently Predict Survival and Relapse Risk in Childhood KMT2A-Rearranged Acute Myeloid Leukemia: A Study by the International Berlin-Frankfurt-Münster Study Group. J. Clin. Oncol. 2023, 41, 2963–2974. [Google Scholar] [CrossRef]
- Krivtsov, A.V.; Evans, K.; Gadrey, J.Y.; Eschle, B.K.; Hatton, C.; Uckelmann, H.J.; Ross, K.N.; Perner, F.; Olsen, S.N.; Pritchard, T.; et al. A Menin-MLL Inhibitor Induces Specific Chromatin Changes and Eradicates Disease in Models of MLL-Rearranged Leukemia. Cancer Cell 2019, 36, 660–673.e11. [Google Scholar] [CrossRef] [PubMed]
- Issa, G.C.; Ravandi, F.; DiNardo, C.D.; Jabbour, E.; Kantarjian, H.M.; Andreeff, M. Therapeutic implications of menin inhibition in acute leukemias. Leukemia 2021, 35, 2482–2495. [Google Scholar] [CrossRef] [PubMed]
- Heikamp, E.B.; Henrich, J.A.; Perner, F.; Wong, E.M.; Hatton, C.; Wen, Y.; Barwe, S.P.; Gopalakrishnapillai, A.; Xu, H.; Uckelmann, H.J.; et al. The menin-MLL1 interaction is a molecular dependency in NUP98-rearranged AML. Blood 2022, 139, 894–906. [Google Scholar] [CrossRef] [PubMed]
- Issa, G.C.; Aldoss, I.; DiPersio, J.; Cuglievan, B.; Stone, R.; Arellano, M.; Thirman, M.J.; Patel, M.R.; Dickens, D.S.; Shenoy, S.; et al. The menin inhibitor revumenib in KMT2A-rearranged or NPM1-mutant leukaemia. Nature 2023, 615, 920–924. [Google Scholar] [CrossRef]
- Pearson, A.D.J.; Zwaan, C.M.; Kolb, E.A.; Karres, D.; Guillot, J.; Kim, S.Y.; Marshall, L.; Tasian, S.K.; Smith, M.; Cooper, T.; et al. Paediatric Strategy Forum for medicinal product development for acute myeloid leukaemia in children and adolescents: ACCELERATE in collaboration with the European Medicines Agency with participation of the Food and Drug Administration. Eur. J. Cancer 2020, 136, 116–129. [Google Scholar] [CrossRef] [PubMed]

| COG AAML1831 | MyeChild 01 | NOPHO-DBH AML 2012 | JPLSG AML-20 | |
|---|---|---|---|---|
| SR | Low Risk 1 (LR1)
| Standard risk (SR)
* Good-risk abnormalities
|
| Low risk (LR)
|
| HR |
|
|
|
† High-risk abnormalities:
|
| Treatment Factors | Summary | Specific Data |
|---|---|---|
| Induction chemotherapy | ||
| Cytarabine doses | Three randomized studies showed that there is not a clear impact of high-dose cytarabine in initial induction compared to low-dose or standard-dose cytarabine. High-dose cytarabine in the second induction may improve the outcome. | POG9421 [63] (n = 560): High-dose vs. standard-dose DAT in initial induction. No difference in CR and EFS. SJCRH AML02 [11] (n = 230): High-dose vs. low-dose ADE in initial induction. No difference in day 22 MRD, EFS, and OS. JPLSG AML-12 [8] (n = 324): High-dose vs. low-dose ECM in initial induction. No difference in end-of-induction MRD, EFS, and OS. Improved EFS for high-risk patients (n = 310) in AML-BFM93 by introducing HAM as a second induction [64]. Better RR, EFS, and OS with second induction HAM in t(8;21) patients (n = 78) in AML-BFM98 [65]. |
| Anthracyclines | Overall, there is no clear evidence for the best anthracyclines of choice. | MRC AML12 [47] (n = 504): MAE vs. ADE. Use of mitoxantrone showed decreased RR and improved DFS over daunorubicin use, but no difference in EFS and OS. AML-BFM93 [66] (n = 358): AIE vs. ADE. Better day 15 bone marrow blast reduction with idarubicin compared to daunorubicin, but no difference in EFS and DFS. AML-BFM2004 [13] (n = 521): ADxE (liposomal daunorubicin) vs. AIE (idarubicin). No difference in RR, EFS, and OS. |
| Addition of other cytotoxic drugs | No clear evidence of adding cytotoxic drugs to cytarabine/anthracycline induction. However, one randomized study showed the benefit of adding GO to initial induction and second consolidation courses. Clofarabine may spare the use of anthracyclines and etoposide. Some groups use fludarabine to enhance the effect of cytarabine (FLA). | MRC-AML10 [67] (n = 359): DAT (6-thioguanine) vs. ADE (etoposide). No difference in CR, RR, DFS, and OS. COG AAML1031 [10] (n = 1097): Randomization to add bortezomib to each standard chemotherapy course failed to improve EFS and OS. COG AAML0531 [9] (n = 1022): ADE + GO (3 mg/m2) vs. ADE. Improved EFS (but not OS) and reduced RR in GO arm. SJCRH AML08 [12] (n = 262): Clofarabine + HDAC vs. high-dose ADE. No difference in EFS and OS. DB-AML-01 [16] (n = 112): Patients with t(8;21) or day 15 marrow blasts ≥ 5% received FLA + liposomal daunorubicin as second induction. |
| Post-induction chemotherapy | ||
| Number of courses | A number of chemotherapy courses range from 4 to 6 (including induction) in recently conducted pediatric AML studies. Two retrospective analyses show benefit of an additional chemotherapy course for a subset of LR patients. | MRC-AML12 [47] (n = 270): 4 vs. 5 courses. No survival benefit for a 5th course of chemotherapy. Combined analysis of COG AAML0531 and AAML1031 studies [68] (n = 923) showed higher RR and lower DFS (but not OS) in a subset of LR patients who received 4 courses compared to those who received 5 courses. In the JPLSG AML-05 study [6] (n = 154), a reduction to 5 from 6 courses in the AML99 study (n = 89) resulted in increased RR in CBF-AML patients. |
| Addition of other cytotoxic drugs | No clear evidence of adding cytotoxic drugs to cytarabine/anthracycline chemotherapy. However, one randomized study showed the benefit of adding GO to initial induction and second consolidation courses. | COG AAML0531 [9] (n = 1022): MA + GO (3 mg/m2) vs. MA (second consolidation course). Improved EFS (but not OS) and reduced RR in GO arm. NOPHO-AML2004 [69] (n = 120): Addition of GO (5 mg/m2/dose on days 1 and 21) vs. no further therapy following the end of consolidation chemotherapies. No improvement in EFS and OS. COG AAML1031 [10] (n = 1097): Randomization to add bortezomib to each standard chemotherapy course failed to improve EFS and OS. |
| Maintenance therapy | No clear role of maintenance therapy. Major study groups no longer use maintenance therapy. | LAME89/91 [70] (n = 268): Maintenance therapy was introduced in LAME89 and randomized to receive or not receive maintenance in LAME91. No difference in EFS and OS. |
| Central nervous system-directed therapy | ||
| CNS-directed therapy | Most groups usually include intrathecal therapy (ITT) in every chemotherapy course, but it is not evidence-based. | Previous AML-BFM studies included prophylactic CNS irradiation, due to the BFM-AML87 study results that the patients without CNS irradiation showed an increase in marrow relapses (not CNS relapses) compared to irradiated patients, but stopped since 2009 [18]. |
| Study (Years of Accrual) | No. of Patients | Risk Group/ Treatment Arm | Cumulative Anthracycline Doses | No. (%) of Patients Treated with CR1 HSCT | EFS, % OS, % (Years) | References | |||
|---|---|---|---|---|---|---|---|---|---|
| Daunorubicin | Mitoxantrone | Idarubicin | Others | ||||||
| JPLSG AML-05 (2006–2010) | 443 | LR | – | 25 | 20 | – | 46 (10) | 54 (3) 73 (3) | Tomizawa et al., 2013 [6] Hasegawa et al., 2020 [7] |
| IR/HR | – | IR:55/HR40 | IR:20/HR:10 | – | |||||
| JPLSG AML-12 (2014–2018) | 359 | CBF SR | – | 40 | 20 | – | 40 (11) | 63.1 (3) 80.3 (3) | Tomizawa et al., 2018 [8] |
| nCBF-SR/HR | – | nCBF-SR:55 HR:40 | nCBF-SR:20 HR:10 | – | |||||
| COG AAML0531 (2006–2010) | 1022 | No HSCT | 300 | 48 | – | – | 157 (15) | 53.1 (3) * 69.4 (3) * | Gamis et al., 2014 [9] |
| HSCT | 300 | – | – | – | |||||
| COG AAML1031 (2011–2016) | 1097 | LR | 300 | 48 | – | – | 85 (8) | 45.9 (3) 65.4 (3) | Aplenc et al., 2020 [10] |
| HR | 300 | – | – | – | |||||
| SJCRH AML02 (2002–2008) | 230 | No HSCT | 300 | 20 * or 50 | – | – | 59 (26) | 63.0 (3) 71.1 (3) | Rubnitz et al., 2010 [11] |
| HSCT | 300 | – | – | – | |||||
| SJCRH AML08 (2008–2017) | 262 | HD-ADE | 300 | 36 | – | – | 81 (31) | 52.9 (3) ** 74.8 (3) ** | Rubnitz et al., 2019 [12] |
| Clo + Ara-C | 150 | 36 | – | – | |||||
| AML-BFM2004 (2004–2010) | 611 | ADxE | – | SR:20/HR:40 | 14 | DNX: 240 | NA | 55 (5) 74 (5) | Creutzig et al., 2013 [13] |
| AIE | – | SR:20/HR:40 | 50 | – | |||||
| AIEOP AML2002/01 (2002–2011) | 482 | – | – | 50 | 60 | – | 141 (29) | 55 (8) 68 (8) | Pession et al., 2013 [14] |
| NOPHO AML2004 (2004–2009) | 151 | – | – | 30 | 48 | – | 22 (15) | 57 (3) 69 (3) | Abrahamsson et al., 2011 [15] |
| DB-AML-01 (2010–2013) | 112 | AM | – | 30 | 36 | – | NA | 52.6 (3) 74.0 (3) | De Moerloose et al., 2019 [16] |
| FLA-DNX | – | – | 36 | DNX: 180 | |||||
| ELAM02 (2005–2011) | 438 | SR | 80 | 60 | – | AMSA: 300 | 119 (27) | 57 (4) 73 (4) | Petit et al., 2018 [17] |
| IR/HR | – | 60 | – | AMSA: 300 | |||||
| Trial (ClinicalTrials.gov Identifier) | Regimen | Key Eligibility | Phase (No. Patients) | Current Status |
|---|---|---|---|---|
| Novartis (NCT03591510) | Midostaurin + chemo | Children (3 mo–17 yo) FLT3-mutated AML | Phase 2 (n = 23) | Recruiting 33 sites: US, Austria, Czechia, Germany, Greece, Italy, Poland, Russia, Slovenia, Turkey, Jordan, Japan, Korea |
| COG AAML1831 (NCT04293562) | Gilteritinib + chemo | Children (2 yo–21 yo) FLT3-ITD (AR > 0.1)+ AML FLT3-TKD + AML | Phase 3 | Recruiting |
| Astellas (NCT04240002) | Gilteritinib + chemo | Children, AYA (6 mo–21 yo) r/r FLT3-ITD + AML | Phase 1/2 (n = 97) | Recruiting 19 sites: US, Canada, Germany, Italy, Spain, UK |
| Daiichi Sankyo/ITCC/COG (NCT03793478) | Quizartinib + chemo | Children, AYA (1 mo–21 yo) r/r FLT3-ITD + AML | Phase 1/2 (n = 65) | Recruiting 36 sites: US, Canada, Belgium, Denmark, France, Italy, Netherlands, Spain, Sweden, UK, Israel |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomizawa, D.; Tsujimoto, S.-I. Risk-Stratified Therapy for Pediatric Acute Myeloid Leukemia. Cancers 2023, 15, 4171. https://doi.org/10.3390/cancers15164171
Tomizawa D, Tsujimoto S-I. Risk-Stratified Therapy for Pediatric Acute Myeloid Leukemia. Cancers. 2023; 15(16):4171. https://doi.org/10.3390/cancers15164171
Chicago/Turabian StyleTomizawa, Daisuke, and Shin-Ichi Tsujimoto. 2023. "Risk-Stratified Therapy for Pediatric Acute Myeloid Leukemia" Cancers 15, no. 16: 4171. https://doi.org/10.3390/cancers15164171
APA StyleTomizawa, D., & Tsujimoto, S.-I. (2023). Risk-Stratified Therapy for Pediatric Acute Myeloid Leukemia. Cancers, 15(16), 4171. https://doi.org/10.3390/cancers15164171






