Role of Advanced Gastrointestinal Endoscopy in the Comprehensive Management of Neuroendocrine Neoplasms
Simple Summary
Abstract
1. Introduction
2. Role of Endoscopy in the Diagnosis, Staging, and Management of Nets Based on Location
2.1. Esophagus
2.2. Stomach
2.3. Small Intestine
2.4. Appendix
2.5. Colon
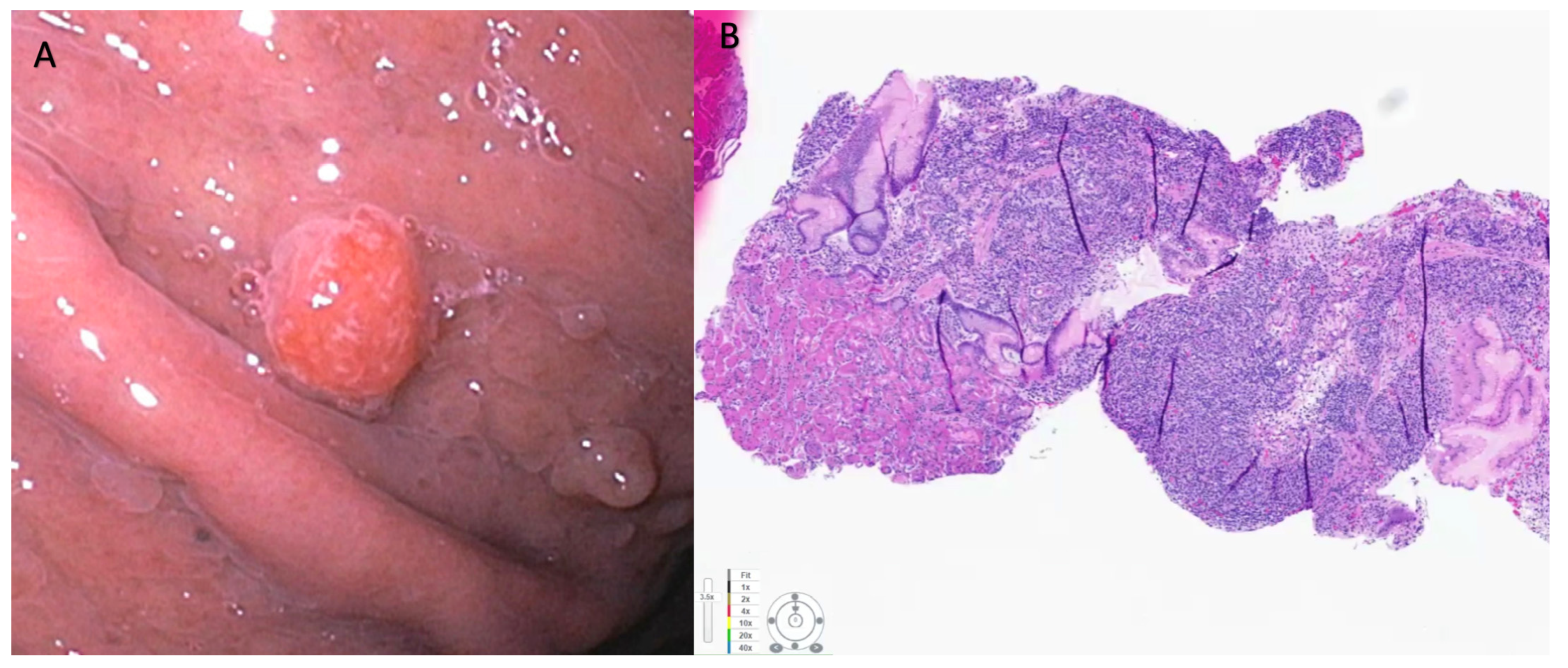
2.6. Rectum
2.7. Pancreas
2.8. Pulmonary
3. Limitations
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Oronsky, B.; Ma, P.C.; Morgensztern, D.; Carter, C.A. Nothing But NET: A Review of Neuroendocrine Tumors and Carcinomas. Neoplasia 2017, 19, 991–1002. [Google Scholar] [CrossRef]
- Shah, M.H.; Goldner, W.S.; Benson, A.B.; Bergsland, E.; Blaszkowsky, L.S.; Brock, P.; Chan, J.; Das, S.; Dickson, P.V.; Fanta, P.; et al. Neuroendocrine and Adrenal Tumors, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2021, 19, 839–868. [Google Scholar] [CrossRef]
- Dasari, A.; Shen, C.; Halperin, D.; Zhao, B.; Zhou, S.; Xu, Y.; Shih, T.; Yao, J.C. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients with Neuroendocrine Tumors in the United States. JAMA Oncol. 2017, 3, 1335–1342. [Google Scholar] [CrossRef]
- Nagtegaal, I.D.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, K.M.; Carneiro, F.; Cree, I.A. The 2019 WHO classification of tumours of the digestive system. Histopathology 2020, 76, 182–188. [Google Scholar] [CrossRef]
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, B.; Gustafsson, B.I.; Chan, A.; Svejda, B.; Kidd, M.; Modlin, I.M. The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol. Metab. Clin. N. Am. 2011, 40, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.G.; Lim, Y.J.; Park, S.J.; Jang, B.I.; Choi, S.R.; Kim, J.K.; Kim, Y.T.; Cho, J.Y.; Yang, C.H.; Chun, H.J.; et al. The clinical features and treatment modality of esophageal neuroendocrine tumors: A multicenter study in Korea. BMC Cancer 2014, 14, 569. [Google Scholar] [CrossRef] [PubMed]
- Deng, H.Y.; Ni, P.Z.; Wang, Y.C.; Wang, W.P.; Chen, L.Q. Neuroendocrine carcinoma of the esophagus: Clinical characteristics and prognostic evaluation of 49 cases with surgical resection. J. Thorac. Dis. 2016, 8, 1250–1256. [Google Scholar] [CrossRef] [PubMed]
- Giannetta, E.; Guarnotta, V.; Rota, F.; de Cicco, F.; Grillo, F.; Colao, A.; Faggiano, A. A rare rarity: Neuroendocrine tumor of the esophagus. Crit. Rev. Oncol. Hematol. 2019, 137, 92–107. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Wu, H.; Nie, L.; Shi, J.; Lebenthal, A.; Chen, J.; Sun, Q.; Yang, J.; Huang, L.; Ye, Q. Primary high-grade neuroendocrine carcinoma of the esophagus: A clinicopathologic and immunohistochemical study of 42 resection cases. Am. J. Surg. Pathol. 2013, 37, 467–483. [Google Scholar] [CrossRef]
- Kalemkerian, G.P. Staging and imaging of small cell lung cancer. Cancer Imaging 2012, 11, 253–258. [Google Scholar] [CrossRef]
- Ilett, E.E.; Langer, S.W.; Olsen, I.H.; Federspiel, B.; Kjær, A.; Knigge, U. Neuroendocrine Carcinomas of the Gastroenteropancreatic System: A Comprehensive Review. Diagnostics 2015, 5, 119–176. [Google Scholar] [CrossRef]
- Park, J.; Park, J.C.; Jo, J.H.; Kim, E.H.; Shin, S.K.; Lee, S.K.; Lee, Y.C. Prospective comparative study of endoscopic ultrasonography-guided fine-needle biopsy and unroofing biopsy. Dig. Liver Dis. 2019, 51, 831–836. [Google Scholar] [CrossRef] [PubMed]
- Zoundjiekpon, V.; Falt, P.; Fojtik, P.; Kundratova, E.; Mikolajek, O.; Hanousek, M.; Reiterova, K.; Ziak, D.; Bolek, M.; Tchibozo, A.; et al. Endosonography-Guided Fine-Needle Aspiration versus “Key-Hole Biopsy” in the diagnostics of upper gastrointestinal subepithelial tumors. A prospective randomized interventional study. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc. Czech Repub. 2020, 164, 63–70. [Google Scholar] [CrossRef]
- Sanaei, O.; Fernández-Esparrach, G.; De La Serna-Higuera, C.; Carrara, S.; Kumbhari, V.; El Zein, M.H.; Ismail, A.; Ginès, A.; Sendino, O.; Montenegro, A.; et al. EUS-guided 22-gauge fine needle biopsy versus single-incision with needle knife for the diagnosis of upper gastrointestinal subepithelial lesions: A randomized controlled trial. Endosc. Int. Open 2020, 8, E266–E273. [Google Scholar] [CrossRef] [PubMed]
- Giri, S.; Afzalpurkar, S.; Angadi, S.; Sundaram, S. Mucosal incision-assisted biopsy versus endoscopic ultrasound-assisted tissue acquisition for subepithelial lesions: A systematic review and meta-analysis. Clin. Endosc. 2022, 55, 615–625. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.S.; Park, S.J.; Park, M.I.; Moon, W.; Kim, H.H.; Lee, J.S.; Kim, B.J.; Ku, D.Y. Successful endoscopic mucosal resection of a low esophageal carcinoid tumor. Clin. Endosc. 2013, 46, 576–578. [Google Scholar] [CrossRef] [PubMed]
- Yagi, M.; Abe, Y.; Sasaki, Y.; Nomura, E.; Sato, T.; Iwano, D.; Yoshizawa, K.; Sakuta, K.; Kanno, N.; Nishise, S.; et al. Esophageal carcinoid tumor treated by endoscopic resection. Dig. Endosc. 2015, 27, 527–530. [Google Scholar] [CrossRef]
- Goto, O.; Uraoka, T.; Horii, J.; Yahagi, N. Expanding indications for ESD: Submucosal disease (SMT/carcinoid tumors). Gastrointest. Endosc. Clin. N. Am. 2014, 24, 169–181. [Google Scholar] [CrossRef]
- Li, Q.L.; Zhang, Y.Q.; Chen, W.F.; Xu, M.D.; Zhong, Y.S.; Ma, L.L.; Qin, W.Z.; Hu, J.W.; Cai, M.Y.; Yao, L.Q.; et al. Endoscopic submucosal dissection for foregut neuroendocrine tumors: An initial study. World J. Gastroenterol. 2012, 18, 5799–5806. [Google Scholar] [CrossRef]
- Shim, C.S.; Jung, I.S. Endoscopic removal of submucosal tumors: Preprocedure diagnosis, technical options, and results. Endoscopy 2005, 37, 646–654. [Google Scholar] [CrossRef] [PubMed]
- Gong, W.; Xiong, Y.; Zhi, F.; Liu, S.; Wang, A.; Jiang, B. Preliminary experience of endoscopic submucosal tunnel dissection for upper gastrointestinal submucosal tumors. Endoscopy 2012, 44, 231–235. [Google Scholar] [CrossRef]
- Deprez, P.H.; Moons, L.M.G.; O’Toole, D.; Gincul, R.; Seicean, A.; Pimentel-Nunes, P.; Fernández-Esparrach, G.; Polkowski, M.; Vieth, M.; Borbath, I.; et al. Endoscopic management of subepithelial lesions including neuroendocrine neoplasms: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2022, 54, 412–429. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.; Cai, H.; Cui, Y. Progress in the treatment of esophageal neuroendocrine carcinoma. Tumor Biol. 2017, 39, 1010428317711313. [Google Scholar] [CrossRef] [PubMed]
- Exarchou, K.; Howes, N.; Pritchard, D.M. Systematic review: Management of localised low-grade upper gastrointestinal neuroendocrine tumours. Aliment. Pharmacol. Ther. 2020, 51, 1247–1267. [Google Scholar] [CrossRef]
- Sato, Y. Endoscopic diagnosis and management of type I neuroendocrine tumors. World J. Gastrointest. Endosc. 2015, 7, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Delle Fave, G.; O’Toole, D.; Sundin, A.; Taal, B.; Ferolla, P.; Ramage, J.K.; Ferone, D.; Ito, T.; Weber, W.; Zheng-Pei, Z.; et al. ENETS Consensus Guidelines Update for Gastroduodenal Neuroendocrine Neoplasms. Neuroendocrinology 2016, 103, 119–124. [Google Scholar] [CrossRef]
- Wang, R.; Zheng-Pywell, R.; Chen, H.A.; Bibb, J.A.; Chen, H.; Rose, J.B. Management of Gastrointestinal Neuroendocrine Tumors. Clin. Med. Insights Endocrinol. Diabetes 2019, 12, 1179551419884058. [Google Scholar] [CrossRef]
- Chung, C.S.; Tsai, C.L.; Chu, Y.Y.; Chen, K.C.; Lin, J.C.; Chen, B.C.; Sun, W.C.; Yen, H.H.; Chen, C.Y.; Wu, I.C.; et al. Clinical features and outcomes of gastric neuroendocrine tumors after endoscopic diagnosis and treatment: A Digestive Endoscopy Society of Tawian (DEST). Medicine 2018, 97, e12101. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Takeuchi, M.; Hashimoto, S.; Mizuno, K.; Kobayashi, M.; Iwafuchi, M.; Narisawa, R.; Aoyagi, Y. Usefulness of endoscopic submucosal dissection for type I gastric carcinoid tumors compared with endoscopic mucosal resection. Hepatogastroenterology 2013, 60, 1524–1529. [Google Scholar]
- Jung, H.J.; Hong, S.J.; Han, J.P.; Kim, H.S.; Jeong, G.A.; Cho, G.S.; Kim, H.K.; Ko, B.M.; Lee, M.S. Long-term outcome of endoscopic and surgical resection for foregut neuroendocrine tumors. J. Dig. Dis. 2015, 16, 595–600. [Google Scholar] [CrossRef]
- Meier, B.; Schmidt, A.; Glaser, N.; Meining, A.; Walter, B.; Wannhoff, A.; Riecken, B.; Caca, K. Endoscopic full-thickness resection of gastric subepithelial tumors with the gFTRD-system: A prospective pilot study (RESET trial). Surg. Endosc. 2020, 34, 853–860. [Google Scholar] [CrossRef]
- Kim, S.J.; Kim, T.U.; Choi, C.W.; Kim, H.W.; Park, S.B.; Ryu, D.G. Underwater endoscopic mucosal resection of upper gastrointestinal subepithelial tumors: A case series pilot study (with video). Medicine 2022, 101, e31072. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, K.M.; Furukawa, M.; Jensen, R.T. Duodenal neuroendocrine tumors: Classification, functional syndromes, diagnosis and medical treatment. Best Pract. Res. Clin. Gastroenterol. 2005, 19, 675–697. [Google Scholar] [CrossRef] [PubMed]
- Randle, R.W.; Ahmed, S.; Newman, N.A.; Clark, C.J. Clinical outcomes for neuroendocrine tumors of the duodenum and ampulla of Vater: A population-based study. J. Gastrointest. Surg. 2014, 18, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Delle Fave, G.; Kwekkeboom, D.J.; Van Cutsem, E.; Rindi, G.; Kos-Kudla, B.; Knigge, U.; Sasano, H.; Tomassetti, P.; Salazar, R.; Ruszniewski, P. ENETS Consensus Guidelines for the management of patients with gastroduodenal neoplasms. Neuroendocrinology 2012, 95, 74–87. [Google Scholar] [CrossRef] [PubMed]
- Schmocker, R.K.; Wright, M.J.; Ding, D.; Javed, A.A.; Cameron, J.L.; Lafaro, K.; Burns, W.R.; He, J.; Wolfgang, C.L.; Burkhart, R.A. Duodenal, ampullary, and pancreatic neuroendocrine tumors: Oncologic outcomes are driven by tumor biology and tissue of origin. J. Surg. Oncol. 2021, 123, 416–424. [Google Scholar] [CrossRef] [PubMed]
- Fukasawa, H.; Tounou, S.; Nabetani, M.; Michida, T. Endoscopic Resection of Ampullary Neuroendocrine Tumor. Intern. Med. 2017, 56, 499–503. [Google Scholar] [CrossRef]
- Shimai, S.; Yamamoto, K.; Sofuni, A.; Tsuchiya, T.; Ishii, K.; Tanaka, R.; Tonozuka, R.; Honjo, M.; Mukai, S.; Fujita, M.; et al. Three Cases of Ampullary Neuroendocrine Tumor Treated by Endoscopic Papillectomy: A Case Report and Literature Review. Intern. Med. 2020, 59, 2369–2374. [Google Scholar] [CrossRef]
- Odabasi, M.; Yildiz, K.M.; Cengiz, E.; Hasan, A.H.; Gunay, E.; Ozkan, E.; Aktekin, A.; Kaya, B.; Muftuoglu, T.M. Treatment of ampullary neuroendocrine tumor by endoscopic snare papillectomy. Am. J. Case Rep. 2013, 14, 439–443. [Google Scholar] [CrossRef][Green Version]
- Gincul, R.; Ponchon, T.; Napoleon, B.; Scoazec, J.Y.; Guillaud, O.; Saurin, J.C.; Ciocirlan, M.; Lepilliez, V.; Pioche, M.; Lefort, C.; et al. Endoscopic treatment of sporadic small duodenal and ampullary neuroendocrine tumors. Endoscopy 2016, 48, 979–986. [Google Scholar] [CrossRef] [PubMed]
- Dogeas, E.; Cameron, J.L.; Wolfgang, C.L.; Hirose, K.; Hruban, R.H.; Makary, M.A.; Pawlik, T.A.; Choti, M.A. Duodenal and Ampullary Carcinoid Tumors: Size Predicts Necessity for Lymphadenectomy. J. Gastrointest. Surg. 2017, 21, 1262–1269. [Google Scholar] [CrossRef]
- Sato, Y.; Hashimoto, S.; Mizuno, K.; Takeuchi, M.; Terai, S. Management of gastric and duodenal neuroendocrine tumors. World J. Gastroenterol. 2016, 22, 6817–6828. [Google Scholar] [CrossRef] [PubMed]
- Kulke, M.H.; Shah, M.H.; Benson, A.B., 3rd; Bergsland, E.; Berlin, J.D.; Blaszkowsky, L.S.; Emerson, L.; Engstrom, P.F.; Fanta, P.; Giordano, T.; et al. Neuroendocrine tumors, version 1.2015. J. Natl. Compr. Cancer Netw. 2015, 13, 78–108. [Google Scholar] [CrossRef] [PubMed]
- Dasari, B.V.M.; Al-Shakhshir, S.; Pawlik, T.M.; Shah, T.; Marudanayagam, R.; Sutcliffe, R.P.; Mirza, D.F.; Muiesan, P.; Roberts, K.J.; Isaac, J. Outcomes of Surgical and Endoscopic Resection of Duodenal Neuroendocrine Tumours (NETs): A Systematic Review of the Literature. J. Gastrointest. Surg. 2018, 22, 1652–1658. [Google Scholar] [CrossRef]
- Brito, H.P.; Torres, I.T.; Turke, K.C.; Parada, A.A.; Waisberg, J.; Botelho, R.V. Comparison of endoscopic resection techniques for duodenal neuroendocrine tumors: Systematic review. Endosc. Int. Open 2021, 9, E1214–E1221. [Google Scholar] [CrossRef] [PubMed]
- Gopakumar, H.; Vohra, I.; Sharma, N.; Puli, S.R. Efficacy of self-assembling peptide in mitigating delayed bleeding after advanced endoscopic resection of gastrointestinal lesions. A meta-analysis. Endosc. Int. Open 2023, 11, E553–E560. [Google Scholar] [CrossRef]
- Hoteya, S.; Kaise, M.; Iizuka, T.; Ogawa, O.; Mitani, T.; Matsui, A.; Kikuchi, D.; Furuhata, T.; Yamashita, S.; Yamada, A.; et al. Delayed bleeding after endoscopic submucosal dissection for non-ampullary superficial duodenal neoplasias might be prevented by prophylactic endoscopic closure: Analysis of risk factors. Dig. Endosc. 2015, 27, 323–330. [Google Scholar] [CrossRef]
- Mori, H.; Shintaro, F.; Kobara, H.; Nishiyama, N.; Rafiq, K.; Kobayashi, M.; Nakatsu, T.; Miichi, N.; Suzuki, Y.; Masaki, T. Successful closing of duodenal ulcer after endoscopic submucosal dissection with over-the-scope clip to prevent delayed perforation. Dig. Endosc. 2013, 25, 459–461. [Google Scholar] [CrossRef]
- Tsujimoto, H.; Ichikura, T.; Nagao, S.; Sato, T.; Ono, S.; Aiko, S.; Hiraki, S.; Yaguchi, Y.; Sakamoto, N.; Tanimizu, T.; et al. Minimally invasive surgery for resection of duodenal carcinoid tumors: Endoscopic full-thickness resection under laparoscopic observation. Surg. Endosc. 2010, 24, 471–475. [Google Scholar] [CrossRef]
- Wang, S.C.; Parekh, J.R.; Zuraek, M.B.; Venook, A.P.; Bergsland, E.K.; Warren, R.S.; Nakakura, E.K. Identification of unknown primary tumors in patients with neuroendocrine liver metastases. Arch. Surg. 2010, 145, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Furnari, M.; Buda, A.; Delconte, G.; Citterio, D.; Voiosu, T.; Ballardini, G.; Cavallaro, F.; Savarino, E.; Mazzaferro, V.; Meroni, E. The role of wireless capsule endoscopy (WCE) in the detection of occult primary neuroendocrine tumors. J. Gastrointest. Liver Dis. 2017, 26, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Gangi, A.; Siegel, E.; Barmparas, G.; Lo, S.; Jamil, L.H.; Hendifar, A.; Nissen, N.N.; Wolin, E.M.; Amersi, F. Multifocality in Small Bowel Neuroendocrine Tumors. J. Gastrointest. Surg. 2018, 22, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Roggo, A.; Wood, W.C.; Ottinger, L.W. Carcinoid tumors of the appendix. Ann. Surg. 1993, 217, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Moertel, C.G.; Dockerty, M.B.; Judd, E.S. Carcinoid tumors of the vermiform appendix. Cancer 1968, 21, 270–278. [Google Scholar] [CrossRef]
- Boudreaux, J.P.; Klimstra, D.S.; Hassan, M.M.; Woltering, E.A.; Jensen, R.T.; Goldsmith, S.J.; Nutting, C.; Bushnell, D.L.; Caplin, M.E.; Yao, J.C. The NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: Well-differentiated neuroendocrine tumors of the Jejunum, Ileum, Appendix, and Cecum. Pancreas 2010, 39, 753–766. [Google Scholar] [CrossRef] [PubMed]
- Pavel, M.; Baudin, E.; Couvelard, A.; Krenning, E.; Öberg, K.; Steinmüller, T.; Anlauf, M.; Wiedenmann, B.; Salazar, R. ENETS Consensus Guidelines for the management of patients with liver and other distant metastases from neuroendocrine neoplasms of foregut, midgut, hindgut, and unknown primary. Neuroendocrinology 2012, 95, 157–176. [Google Scholar] [CrossRef]
- Heller, D.R.; Jean, R.A.; Luo, J.; Kurbatov, V.; Grisotti, G.; Jacobs, D.; Chiu, A.S.; Zhang, Y.; Khan, S.A. Practice Patterns and Guideline Non-Adherence in Surgical Management of Appendiceal Carcinoid Tumors. J. Am. Coll. Surg. 2019, 228, 839–851. [Google Scholar] [CrossRef]
- NCCN Guidelines. Available online: https://www.nccn,org/preofessionals/phyiciab_gls/pdf/neuroendocrine.pdf (accessed on 23 April 2023).
- Modlin, I.M.; Lye, K.D.; Kidd, M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer 2003, 97, 934–959. [Google Scholar] [CrossRef]
- Jetmore, A.B.; Ray, J.E.; Gathright, J.B., Jr.; McMullen, K.M.; Hicks, T.C.; Timmcke, A.E. Rectal carcinoids: The most frequent carcinoid tumor. Dis. Colon Rectum 1992, 35, 717–725. [Google Scholar] [CrossRef]
- Yao, J.C.; Hassan, M.; Phan, A.; Dagohoy, C.; Leary, C.; Mares, J.E.; Abdalla, E.K.; Fleming, J.B.; Vauthey, J.N.; Rashid, A.; et al. One hundred years after “carcinoid”: Epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J. Clin. Oncol. 2008, 26, 3063–3072. [Google Scholar] [CrossRef] [PubMed]
- Caplin, M.; Sundin, A.; Nillson, O.; Baum, R.P.; Klose, K.J.; Kelestimur, F.; Plöckinger, U.; Papotti, M.; Salazar, R.; Pascher, A. ENETS Consensus Guidelines for the management of patients with digestive neuroendocrine neoplasms: Colorectal neuroendocrine neoplasms. Neuroendocrinology 2012, 95, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Ramage, J.K.; De Herder, W.W.; Delle Fave, G.; Ferolla, P.; Ferone, D.; Ito, T.; Ruszniewski, P.; Sundin, A.; Weber, W.; Zheng-Pei, Z.; et al. ENETS Consensus Guidelines Update for Colorectal Neuroendocrine Neoplasms. Neuroendocrinology 2016, 103, 139–143. [Google Scholar] [CrossRef]
- Ploeckinger, U.; Kloeppel, G.; Wiedenmann, B.; Lohmann, R. The German NET-registry: An audit on the diagnosis and therapy of neuroendocrine tumors. Neuroendocrinology 2009, 90, 349–363. [Google Scholar] [CrossRef]
- Reumkens, A.; Sastrowijoto, P.; Grabsch, H.I.; Goudkade, D.; le Clercq, C.; Bakker, M.; Keulen, E.; de Ridder, R.; de Herder, W.W.; Winkens, B.; et al. Epidemiological, clinical and endoscopic characteristics of colorectal neuroendocrine neoplasms: A population-based study in the Netherlands. Endosc. Int. Open 2022, 10, E940–E951. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Yao, L.Q.; Xu, M.D.; Zhang, Y.Q.; Chen, W.F.; Shi, Q.; Cai, S.L.; Chen, Y.Y.; Xie, Y.H.; Ji, Y.; et al. Efficacy and Safety of Endoscopic Submucosal Dissection for Colorectal Carcinoids. Clin. Gastroenterol. Hepatol. 2016, 14, 575–581. [Google Scholar] [CrossRef]
- Sauer, M.; Hildenbrand, R.; Oyama, T.; Sido, B.; Yahagi, N.; Dumoulin, F.L. Endoscopic submucosal dissection for flat or sessile colorectal neoplasia >20 mm: A European single-center series of 182 cases. Endosc. Int. Open 2016, 4, E895–E900. [Google Scholar] [CrossRef]
- Takezawa, T.; Hayashi, Y.; Shinozaki, S.; Sagara, Y.; Okada, M.; Kobayashi, Y.; Sakamoto, H.; Miura, Y.; Sunada, K.; Lefor, A.K.; et al. The pocket-creation method facilitates colonic endoscopic submucosal dissection (with video). Gastrointest. Endosc. 2019, 89, 1045–1053. [Google Scholar] [CrossRef]
- Ismail, M.S.; Bahdi, F.; Mercado, M.O.; Habazi, R.; Alexander, A.; Prabhu, S.; John, S.; Kovvali, C.; Othman, M.O. ESD with double-balloon endoluminal intervention platform versus standard ESD for management of colon polyps. Endosc. Int. Open 2020, 8, E1273–E1279. [Google Scholar] [CrossRef]
- Ramos-Zabala, F.; García-Mayor, M.; Domínguez-Pino, A.; Alzina-Pérez, A.; Moreno-Almazán, L. Combination of immersion in saline solution, pocket-creation method, water-jet hydrodissection, and hybrid knife “probe mode” simplifies endoscopic submucosal dissection in giant rectal polyp. VideoGIE 2019, 4, 478–480. [Google Scholar] [CrossRef]
- Anthony, L.B.; Strosberg, J.R.; Klimstra, D.S.; Maples, W.J.; O’Dorisio, T.M.; Warner, R.R.; Wiseman, G.A.; Benson, A.B., 3rd; Pommier, R.F. The NANETS consensus guidelines for the diagnosis and management of gastrointestinal neuroendocrine tumors (nets): Well-differentiated nets of the distal colon and rectum. Pancreas 2010, 39, 767–774. [Google Scholar] [CrossRef]
- Gallo, C.; Rossi, R.E.; Cavalcoli, F.; Barbaro, F.; Boškoski, I.; Invernizzi, P.; Massironi, S. Rectal neuroendocrine tumors: Current advances in management, treatment, and surveillance. World J. Gastroenterol. 2022, 28, 1123–1138. [Google Scholar] [CrossRef]
- Veyre, F.; Lambin, T.; Fine, C.; Fenouil, T.; Rostain, F.; Walter, T.; Pioche, M. Endoscopic characterization of rectal neuroendocrine tumors with virtual chromoendoscopy: Differences between benign and malignant lesions. Endoscopy 2021, 53, E215–E216. [Google Scholar] [CrossRef]
- Brand, M.; Reimer, S.; Reibetanz, J.; Flemming, S.; Kornmann, M.; Meining, A. Endoscopic full thickness resection vs. transanal endoscopic microsurgery for local treatment of rectal neuroendocrine tumors - a retrospective analysis. Int. J. Color. Dis. 2021, 36, 971–976. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, J.H.; Lee, J.Y.; Chun, J.; Im, J.P.; Kim, J.S. Clinical outcomes of endoscopic mucosal resection for rectal neuroendocrine tumor. BMC Gastroenterol. 2018, 18, 77. [Google Scholar] [CrossRef] [PubMed]
- Moon, C.M.; Huh, K.C.; Jung, S.A.; Park, D.I.; Kim, W.H.; Jung, H.M.; Koh, S.J.; Kim, J.O.; Jung, Y.; Kim, K.O.; et al. Long-Term Clinical Outcomes of Rectal Neuroendocrine Tumors According to the Pathologic Status After Initial Endoscopic Resection: A KASID Multicenter Study. Am. J. Gastroenterol. 2016, 111, 1276–1285. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.G.; Goh, M.J.; Kim, E.R.; Hong, S.N.; Kim, T.J.; Chang, D.K.; Kim, Y.H. Recurrence pattern and surveillance strategy for rectal neuroendocrine tumors after endoscopic resection. J. Gastroenterol. Hepatol. 2021, 36, 968–973. [Google Scholar] [CrossRef] [PubMed]
- Bang, B.W.; Park, J.S.; Kim, H.K.; Shin, Y.W.; Kwon, K.S.; Kim, J.M. Endoscopic Resection for Small Rectal Neuroendocrine Tumors: Comparison of Endoscopic Submucosal Resection with Band Ligation and Endoscopic Submucosal Dissection. Gastroenterol. Res. Pract. 2016, 2016, 6198927. [Google Scholar] [CrossRef] [PubMed]
- Park, S.B.; Kim, H.W.; Kang, D.H.; Choi, C.W.; Kim, S.J.; Nam, H.S. Advantage of endoscopic mucosal resection with a cap for rectal neuroendocrine tumors. World J. Gastroenterol. 2015, 21, 9387–9393. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.C.; Zheng, K.; Zhao, S.; Wang, Z.N.; Xu, H.M.; Jiang, C.G. Efficacy and safety of modified endoscopic mucosal resection for rectal neuroendocrine tumors: A meta-analysis. Z. Gastroenterol. 2020, 58, 137–145. [Google Scholar] [CrossRef]
- Wang, X.; Xiang, L.; Li, A.; Han, Z.; Li, Y.; Wang, Y.; Guo, Y.; Zuang, K.; Yan, Q.; Zhong, J.; et al. Endoscopic submucosal dissection for the treatment of rectal carcinoid tumors 7–16 mm in diameter. Int. J. Color. Dis. 2015, 30, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.L.; Gan, R.Y.; Chen, Z.H.; Gao, R.Y.; Li, D.F.; Wang, L.S.; Yao, J. Endoscopic mucosal resection with double band ligation versus endoscopic submucosal dissection for small rectal neuroendocrine tumors. World J. Gastrointest. Surg. 2023, 15, 440–449. [Google Scholar] [CrossRef] [PubMed]
- Park, S.S.; Han, K.S.; Kim, B.; Chang Kim, B.; Hong, C.W.; Sohn, D.K.; Chang, H.J. Comparison of underwater endoscopic mucosal resection and endoscopic submucosal dissection of rectal neuroendocrine tumors (with videos). Gastrointest. Endosc. 2020, 91, 1164–1171.e1162. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.; Zhang, X.; Shi, Y.; Pei, Q. Endoscopic mucosal resection with suction vs. endoscopic submucosal dissection for small rectal neuroendocrine tumors: A meta-analysis. Scand. J. Gastroenterol. 2018, 53, 1139–1145. [Google Scholar] [CrossRef]
- Gleeson, F.C.; Levy, M.J.; Dozois, E.J.; Larson, D.W.; Wong Kee Song, L.M.; Boardman, L.A. Endoscopically identified well-differentiated rectal carcinoid tumors: Impact of tumor size on the natural history and outcomes. Gastrointest. Endosc. 2014, 80, 144–151. [Google Scholar] [CrossRef]
- Lie, J.J.; Yoon, H.M.; Karimuddin, A.A.; Raval, M.J.; Phang, P.T.; Ghuman, A.; Lee, L.H.; Stuart, H.; Brown, C.J. Management of rectal neuroendocrine tumours by transanal endoscopic microsurgery. Color. Dis. 2023, 25, 1026–1035. [Google Scholar] [CrossRef]
- de Mestier, L.; Lorenzo, D.; Fine, C.; Cros, J.; Hentic, O.; Walter, T.; Panis, Y.; Couvelard, A.; Cadiot, G.; Ruszniewski, P. Endoscopic, transanal, laparoscopic, and transabdominal management of rectal neuroendocrine tumors. Best Pract. Res. Clin. Endocrinol. Metab. 2019, 33, 101293. [Google Scholar] [CrossRef]
- Jin, R.; Bai, X.; Xu, T.; Wu, X.; Wang, Q.; Li, J. Comparison of the efficacy of endoscopic submucosal dissection and transanal endoscopic microsurgery in the treatment of rectal neuroendocrine tumors ≤ 2 cm. Front. Endocrinol. (Lausanne) 2022, 13, 1028275. [Google Scholar] [CrossRef]
- Park, S.S.; Kim, B.C.; Lee, D.E.; Han, K.S.; Kim, B.; Hong, C.W.; Sohn, D.K. Comparison of endoscopic submucosal dissection and transanal endoscopic microsurgery for T1 rectal neuroendocrine tumors: A propensity score-matched study. Gastrointest. Endosc. 2021, 94, 408–415.e402. [Google Scholar] [CrossRef]
- Meier, B.; Albrecht, H.; Wiedbrauck, T.; Schmidt, A.; Caca, K. Full-thickness resection of neuroendocrine tumors in the rectum. Endoscopy 2020, 52, 68–72. [Google Scholar] [CrossRef]
- Howe, J.R.; Merchant, N.B.; Conrad, C.; Keutgen, X.M.; Hallet, J.; Drebin, J.A.; Minter, R.M.; Lairmore, T.C.; Tseng, J.F.; Zeh, H.J.; et al. The North American Neuroendocrine Tumor Society Consensus Paper on the Surgical Management of Pancreatic Neuroendocrine Tumors. Pancreas 2020, 49, 1–33. [Google Scholar] [CrossRef] [PubMed]
- Leeds, J.S.; Nayar, M.K.; Bekkali, N.L.H.; Wilson, C.H.; Johnson, S.J.; Haugk, B.; Darne, A.; Oppong, K.W. Endoscopic ultrasound-guided fine-needle biopsy is superior to fine-needle aspiration in assessing pancreatic neuroendocrine tumors. Endosc. Int. Open 2019, 7, E1281–E1287. [Google Scholar] [CrossRef] [PubMed]
- Tacelli, M.; Bina, N.; Crinò, S.F.; Facciorusso, A.; Celsa, C.; Vanni, A.S.; Fantin, A.; Antonini, F.; Falconi, M.; Monica, F.; et al. Reliability of grading preoperative pancreatic neuroendocrine tumors on EUS specimens: A systematic review with meta-analysis of aggregate and individual data. Gastrointest. Endosc. 2022, 96, 898–908.e823. [Google Scholar] [CrossRef] [PubMed]
- Ghabi, E.M.; Habib, J.R.; Shoucair, S.; Javed, A.A.; Sham, J.; Burns, W.R.; Cameron, J.L.; Ali, S.Z.; Shin, E.J.; Arcidiacono, P.G.; et al. Detecting Somatic Mutations for Well-Differentiated Pancreatic Neuroendocrine Tumors in Endoscopic Ultrasound-Guided Fine Needle Aspiration with Next-Generation Sequencing. Ann. Surg. Oncol. 2023. [Google Scholar] [CrossRef]
- Mastrosimini, M.G.; Manfrin, E.; Remo, A.; De Bellis, M.; Parisi, A.; Pedron, S.; Luchini, C.; Brunelli, M.; Ammendola, S.; Bernardoni, L.; et al. Endoscopic ultrasound fine-needle biopsy to assess DAXX/ATRX expression and alternative lengthening of telomeres status in non-functional pancreatic neuroendocrine tumors. Pancreatology 2023, 23, 429–436. [Google Scholar] [CrossRef]
- Asokkumar, R.; Yung Ka, C.; Loh, T.; Kah Ling, L.; Gek San, T.; Ying, H.; Tan, D.; Khor, C.; Lim, T.; Soetikno, R. Comparison of tissue and molecular yield between fine-needle biopsy (FNB) and fine-needle aspiration (FNA): A randomized study. Endosc. Int. Open 2019, 7, E955–E963. [Google Scholar] [CrossRef]
- Partelli, S.; Muffatti, F.; Andreasi, V.; Giannone, F.; Rossi, G.; Palumbo, D.; Mapelli, P.; Schiavo Lena, M.; Arcidiacono, P.G.; De Cobelli, F.; et al. A Single-center Prospective Observational Study Investigating the Accuracy of Preoperative Diagnostic Procedures in the Assessment of Lymph Node Metastases in Nonfunctioning Pancreatic Neuroendocrine Tumors. Ann. Surg. 2022, 276, 921–928. [Google Scholar] [CrossRef] [PubMed]
- Franchellucci, G.; Andreozzi, M.; Carrara, S.; De Luca, L.; Auriemma, F.; Paduano, D.; Calabrese, F.; Facciorusso, A.; Poletti, V.; Zerbi, A.; et al. Contrast Enhanced EUS for Predicting Solid Pancreatic Neuroendocrine Tumor Grade and Aggressiveness. Diagnostics 2023, 13, 239. [Google Scholar] [CrossRef]
- Lakhtakia, S.; Seo, D.W. Endoscopic ultrasonography-guided tumor ablation. Dig. Endosc. 2017, 29, 486–494. [Google Scholar] [CrossRef]
- Rimbaş, M.; Horumbă, M.; Rizzatti, G.; Crinò, S.F.; Gasbarrini, A.; Costamagna, G.; Larghi, A. Interventional endoscopic ultrasound for pancreatic neuroendocrine neoplasms. Dig. Endosc. 2020, 32, 1031–1041. [Google Scholar] [CrossRef]
- Lee, L.C.; Grant, C.S.; Salomao, D.R.; Fletcher, J.G.; Takahashi, N.; Fidler, J.L.; Levy, M.J.; Huebner, M. Small, nonfunctioning, asymptomatic pancreatic neuroendocrine tumors (PNETs): Role for nonoperative management. Surgery 2012, 152, 965–974. [Google Scholar] [CrossRef]
- Sadot, E.; Reidy-Lagunes, D.L.; Tang, L.H.; Do, R.K.; Gonen, M.; D’Angelica, M.I.; DeMatteo, R.P.; Kingham, T.P.; Groot Koerkamp, B.; Untch, B.R.; et al. Observation versus Resection for Small Asymptomatic Pancreatic Neuroendocrine Tumors: A Matched Case-Control Study. Ann. Surg. Oncol. 2016, 23, 1361–1370. [Google Scholar] [CrossRef] [PubMed]
- Haynes, A.B.; Deshpande, V.; Ingkakul, T.; Vagefi, P.A.; Szymonifka, J.; Thayer, S.P.; Ferrone, C.R.; Wargo, J.A.; Warshaw, A.L.; Fernández-del Castillo, C. Implications of incidentally discovered, nonfunctioning pancreatic endocrine tumors: Short-term and long-term patient outcomes. Arch. Surg. 2011, 146, 534–538. [Google Scholar] [CrossRef] [PubMed]
- Toste, P.A.; Kadera, B.E.; Tatishchev, S.F.; Dawson, D.W.; Clerkin, B.M.; Muthusamy, R.; Watson, R.; Tomlinson, J.S.; Hines, O.J.; Reber, H.A.; et al. Nonfunctional pancreatic neuroendocrine tumors < 2 cm on preoperative imaging are associated with a low incidence of nodal metastasis and an excellent overall survival. J. Gastrointest. Surg. 2013, 17, 2105–2113. [Google Scholar] [CrossRef]
- Sallinen, V.J.; Le Large, T.Y.S.; Tieftrunk, E.; Galeev, S.; Kovalenko, Z.; Haugvik, S.P.; Antila, A.; Franklin, O.; Martinez-Moneo, E.; Robinson, S.M.; et al. Prognosis of sporadic resected small (≤2 cm) nonfunctional pancreatic neuroendocrine tumors—A multi-institutional study. HPB (Oxf.) 2018, 20, 251–259. [Google Scholar] [CrossRef]
- Singh, S.; Dey, C.; Kennecke, H.; Kocha, W.; Maroun, J.; Metrakos, P.; Mukhtar, T.; Pasieka, J.; Rayson, D.; Rowsell, C.; et al. Consensus Recommendations for the Diagnosis and Management of Pancreatic Neuroendocrine Tumors: Guidelines from a Canadian National Expert Group. Ann. Surg. Oncol. 2015, 22, 2685–2699. [Google Scholar] [CrossRef] [PubMed]
- El Sayed, G.; Frim, L.; Franklin, J.; McCrudden, R.; Gordon, C.; Al-Shamma, S.; Kiss, S.; Hegyi, P.; Erőss, B.; Hegyi, P.J. Endoscopic ultrasound-guided ethanol and radiofrequency ablation of pancreatic insulinomas: A systematic literature review. Ther. Adv. Gastroenterol. 2021, 14, 17562848211042171. [Google Scholar] [CrossRef]
- Crinò, S.F.; Napoleon, B.; Facciorusso, A.; Lakhtakia, S.; Borbath, I.; Caillol, F.; Do-Cong Pham, K.; Rizzatti, G.; Forti, E.; Palazzo, L.; et al. Endoscopic Ultrasound-guided Radiofrequency Ablation Versus Surgical Resection for Treatment of Pancreatic Insulinoma. Clin. Gastroenterol. Hepatol. 2023. [Google Scholar] [CrossRef]
- So, H.; Ko, S.W.; Shin, S.H.; Kim, E.H.; Son, J.; Ha, S.; Song, K.B.; Kim, H.J.; Kim, M.H.; Park, D.H. Comparison of EUS-guided ablation and surgical resection for nonfunctioning small pancreatic neuroendocrine tumors: A propensity score-matching study. Gastrointest. Endosc. 2022, 97, 741–751.e741. [Google Scholar] [CrossRef] [PubMed]
- Fink, G.; Krelbaum, T.; Yellin, A.; Bendayan, D.; Saute, M.; Glazer, M.; Kramer, M.R. Pulmonary carcinoid: Presentation, diagnosis, and outcome in 142 cases in Israel and review of 640 cases from the literature. Chest 2001, 119, 1647–1651. [Google Scholar] [CrossRef] [PubMed]
- Oberg, K. Diagnosis and treatment of carcinoid tumors. Expert Rev. Anticancer. Ther. 2003, 3, 863–877. [Google Scholar] [CrossRef] [PubMed]
- Piro, R.; Tonelli, R.; Taddei, S.; Marchioni, A.; Musci, G.; Clini, E.; Facciolongo, N. Atypical diagnosis for typical lung carcinoid. BMC Pulm. Med. 2019, 19, 168. [Google Scholar] [CrossRef] [PubMed]
- Mindaye, E.T.; Tesfaye, G.K. Bronchial carcinoid tumor: A case report. Int. J. Surg. Case Rep. 2020, 77, 349–352. [Google Scholar] [CrossRef]
- Singh, S.; Bergsland, E.K.; Card, C.M.; Hope, T.A.; Kunz, P.L.; Laidley, D.T.; Lawrence, B.; Leyden, S.; Metz, D.C.; Michael, M.; et al. Commonwealth Neuroendocrine Tumour Research Collaboration and the North American Neuroendocrine Tumor Society Guidelines for the Diagnosis and Management of Patients with Lung Neuroendocrine Tumors: An International Collaborative Endorsement and Update of the 2015 European Neuroendocrine Tumor Society Expert Consensus Guidelines. J. Thorac. Oncol. 2020, 15, 1577–1598. [Google Scholar] [CrossRef]
- Silvestri, G.A.; Gonzalez, A.V.; Jantz, M.A.; Margolis, M.L.; Gould, M.K.; Tanoue, L.T.; Harris, L.J.; Detterbeck, F.C. Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013, 143, e211S–e250S. [Google Scholar] [CrossRef] [PubMed]
- Vilmann, P.; Annema, J.; Clementsen, P. Endosonography in bronchopulmonary disease. Best Pract. Res. Clin. Gastroenterol. 2009, 23, 711–728. [Google Scholar] [CrossRef]
- Jue, T.L.; Sharaf, R.N.; Appalaneni, V.; Anderson, M.A.; Ben-Menachem, T.; Decker, G.A.; Fanelli, R.D.; Fukami, N.; Ikenberry, S.O.; Jain, R.; et al. Role of EUS for the evaluation of mediastinal adenopathy. Gastrointest. Endosc. 2011, 74, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Detterbeck, F.C.; Jantz, M.A.; Wallace, M.; Vansteenkiste, J.; Silvestri, G.A. Invasive mediastinal staging of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007, 132, 202s–220s. [Google Scholar] [CrossRef]
- Vilmann, P.; Clementsen, P.F.; Colella, S.; Siemsen, M.; De Leyn, P.; Dumonceau, J.M.; Herth, F.J.; Larghi, A.; Vazquez-Sequeiros, E.; Hassan, C.; et al. Combined endobronchial and oesophageal endosonography for the diagnosis and staging of lung cancer. European Society of Gastrointestinal Endoscopy (ESGE) Guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS). Endoscopy 2015, 47, 545–559. [Google Scholar] [CrossRef]
- Prasad, P.; Schmulewitz, N.; Patel, A.; Varadarajulu, S.; Wildi, S.M.; Roberts, S.; Tutuian, R.; King, P.; Hawes, R.H.; Hoffman, B.J.; et al. Detection of occult liver metastases during EUS for staging of malignancies. Gastrointest. Endosc. 2004, 59, 49–53. [Google Scholar] [CrossRef]
- DeWitt, J.; LeBlanc, J.; McHenry, L.; Ciaccia, D.; Imperiale, T.; Chappo, J.; Cramer, H.; McGreevy, K.; Chriswell, M.; Sherman, S. Endoscopic ultrasound-guided fine needle aspiration cytology of solid liver lesions: A large single-center experience. Am. J. Gastroenterol. 2003, 98, 1976–1981. [Google Scholar] [CrossRef] [PubMed]
- Giugliano, D.N.; Feinberg, A.E.; Sapci, I.; Ozgur, I.; Valente, M.A.; Steele, S.R.; Gorgun, E. The Learning Curve for Advanced Endoscopy for Colorectal Lesions: A Surgeon’s Experience at a High-Volume Center. Dis. Colon Rectum 2023. [Google Scholar] [CrossRef] [PubMed]
- Akintoye, E.; Kumar, N.; Aihara, H.; Nas, H.; Thompson, C.C. Colorectal endoscopic submucosal dissection: A systematic review and meta-analysis. Endosc. Int. Open 2016, 4, E1030–E1044. [Google Scholar] [CrossRef] [PubMed]


| Terminology | Differentiation | Grade | Mitotic Rate | Ki-67 Index |
|---|---|---|---|---|
| NET, GI | Well differentiated | Low | <2 | <3% |
| NET, G2 | Intermediate | 2–20 | 3–20% | |
| NET, G3 | High | >20 | >20% | |
| NEC, small-cell type (SCNEC) | Poorly differentiated | High | >20 | >20% |
| NEC, large-cell type (LCNEC) | >20 | >20% | ||
| MiNEN | Well or poorly differentiated | Variable | Variable | Variable |
| Location of NEN | Recommendation for Observation | Endoscopic Diagnostic and Therapeutic Techniques | Endoscopic Management Comments | ||
|---|---|---|---|---|---|
| Diagnostic and Staging Techniques | Therapeutic Interventions First Line | Therapeutic Interventions Second Line | |||
| Esophagus | Currently there are no treatment guidelines that specifically address esophageal NENs. Treatment choice should be based on assessment of tumor size, grade, stage, patient’s coexisting health conditions and local expertise | EGD ± NBI with biopsy EUS and CE-EUS EUS-FNA, FNB SINK MIAB | ESD | EMR Enucleation with SMT | Endoscopic resection recommended only for lesions < 1 cm with no suspicion for lymphovascular invasion |
| Stomach | Surveillance could be an option for Type-1 g-NENs < 1 cm. Treatment choice should be based on assessment of patient’s coexisting health conditions and local expertise. Observation is not favoured for Type-2 and Type-3 n-NENs. Local or limited excision can be considered, but must be tailored to the patient based on multidisciplinary evaluation at centers with expertise. | EGD ± NBI with biopsy, E-EUS EUS-FNA, FNB SINKMIAB | ESD | EMR EFTR Underwater EMR | Endoscopic resection recommended only for lesions < 2 cm with no suspicion for lymphovascular invasion |
| Small Intestine | Observation is not recommended for d-NENs or for NENs originating in the jejunum or ileum as they have a higher potential for an aggressive behaviour. Furthermore, endoscopic access to distal small bowel is limited and precludes effective surveillance. | EGD ± NBI with biopsy EUS EUS-FNA, FNB VCE Single or Double balloon enteroscopy | EMR (cap-assisted, underwater, ligation-assisted) ESDEFTR | No consensus. Based on local expertise, location and features of NEN | Endoscopic resection recommended only for lesions < 1 cm with no suspicion for lymphovascular invasion. NENs between 1 and 2 cm can be considered for endoscopic resection on a case-by-case basis. |
| Colon | Observation is not recommended. Small colonic NENs are often mistaken for hyperplastic polyps on colonoscopy and get resected using cold snare polypectomy. | Colonoscopy ± NBI with biopsy | EMR ESD ESD using DEIP | Endoscopic resection recommended only for lesions < 2 cm with no suspicion for lymphovascular invasion | |
| Rectum | Observation is not recommended as these are easily accessible to endoscopic resection. | Colonoscopy ± NBI with biopsy EUS EUS-FNA, FNB | EMR (ligation-assisted, hybrid, modified) ESD | EMR (cap-assisted, underwater, hybrid, modified) ESD EFTR | EMR is the preferred technique for removing rectal NENs < 10 mm in size, and ESD for lesions up to 20 mm. Transanal endoscopic microsurgery can also be an option for lesions> 10 mm but <20 mm. |
| Pancreas | Surveillance can be an acceptable strategy for asymptomatic patients with a pNETs < 1 cm. Decision to observe or resect an asymptomatic pNET 1–2 cm in size should be individualized based on patient age, co-morbidities and tumor behavior during surveillance. Well informed decision from the patient and access to dependable long-term follow-up will also be important factors to consider. | EUS-FNA, FNB | EUS-RFA EUS-EA | Endoscopic ablation techniques could be an effective treatment option for patients who would otherwise be considered for observation. One of the most important factor in the decision for observation instead of surgical resection is the relatively high morbidity and mortality associated with pancreatic surgeries. | |
| Location of NEN | NANETS Guidelines | ENETS Guidelines |
|---|---|---|
| Esophagus | No consensus. | No consensus. |
| Stomach | Type 1 <1 cm Surveillance or ER 1–2 cm Endoscopic surveillance every 3 years vs. ER >2 cm SR. ER can be considered if feasible on a case-by-case manner EUS recommended for NEN > 1 cm to assess depth of invasion Type 2 <1 cm Surveillance or ER 1–2 cm ER or SR >2 cm SR EUS recommended for NEN > 1 cm to assess depth of invasion Type 3 Surgical resection | EUS is recommended in tumors >1 cm Endoscopic resection in type 1 NEN larger than 1 cm. ESD and FTR are more effective to achieve R0 resection compared to EMR. Endoscopic resection may be considered for localized type III G1 gNETs ≤ 10 mm, and occasionally larger tumors with Ki-67 < 10% and <15 mm in diameter if the risks of surgical resection are high. |
| Small Intestine | No definite recommendations for ER in duodenal NENs, but guidelines state that ER is potentially appropriate for localized tumors <2 cm, if surgically feasible. Surgical resection with lymph node dissection and surgical full bowel examination to evaluate for lateral metastasis in NENs of jejunum, ileum and cecum. Appendiceal NEN <1 cm SR 1–2 cm SR/ Right hemicolectomy. >2 cm Right hemicolectomy | Biopsies to confirm the diagnosis and for grading EUS is recommended in tumours >1 cm Very small non-functioning tumors in D1 should be removed using ER Lesions of 5–10 mm (and up to 15 mm in some centers) can be removed endoscopically after imaging work-up, but risks are relatively high |
| Colorectum | <1 cm, ER 1–2 cm, ER or SR >2 cm, ER or SR | ≤10, ER is recommended and recurrence rates are low. ≥20 mm, SR using LAR or APR is recommended (after exclusion of unresectable distant metastases). 10–20 mm, MDT discussion about either endoscopic or surgical therapy. |
| Pancreas | EUS-FNA should be performed for diagnosis or when there is a question about tumor grade. Although FNA is most frequently performed, the addition of FNB can be performed where available. EUS should be performed to identify multifocal disease in MEN1 patients. EUS does not need to be performed to determine surgical resectability. | EUS for evaluation of all PNETS with EUS guided tissue sampling whenever possible. Guidelines mention that EUS directed ablation using ethanol injection or CT-guided RFA have all been successful for PNETS < 2 cm (insulinomas and MEN1), but no specific recommendations. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gopakumar, H.; Jahagirdar, V.; Koyi, J.; Dahiya, D.S.; Goyal, H.; Sharma, N.R.; Perisetti, A. Role of Advanced Gastrointestinal Endoscopy in the Comprehensive Management of Neuroendocrine Neoplasms. Cancers 2023, 15, 4175. https://doi.org/10.3390/cancers15164175
Gopakumar H, Jahagirdar V, Koyi J, Dahiya DS, Goyal H, Sharma NR, Perisetti A. Role of Advanced Gastrointestinal Endoscopy in the Comprehensive Management of Neuroendocrine Neoplasms. Cancers. 2023; 15(16):4175. https://doi.org/10.3390/cancers15164175
Chicago/Turabian StyleGopakumar, Harishankar, Vinay Jahagirdar, Jagadish Koyi, Dushyant Singh Dahiya, Hemant Goyal, Neil R. Sharma, and Abhilash Perisetti. 2023. "Role of Advanced Gastrointestinal Endoscopy in the Comprehensive Management of Neuroendocrine Neoplasms" Cancers 15, no. 16: 4175. https://doi.org/10.3390/cancers15164175
APA StyleGopakumar, H., Jahagirdar, V., Koyi, J., Dahiya, D. S., Goyal, H., Sharma, N. R., & Perisetti, A. (2023). Role of Advanced Gastrointestinal Endoscopy in the Comprehensive Management of Neuroendocrine Neoplasms. Cancers, 15(16), 4175. https://doi.org/10.3390/cancers15164175







