11p15 Epimutations in Pediatric Embryonic Tumors: Insights from a Methylome Analysis
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Eligibility and Sample Collection
2.2. Determining Tumor Methylation Status via EPIC Beadchip Arrays
2.3. Determining Tumor Methylation Status via MS-MLPA
2.4. Determining CfDNA Methylation Status via Digital PCR (dPCR)
3. Results
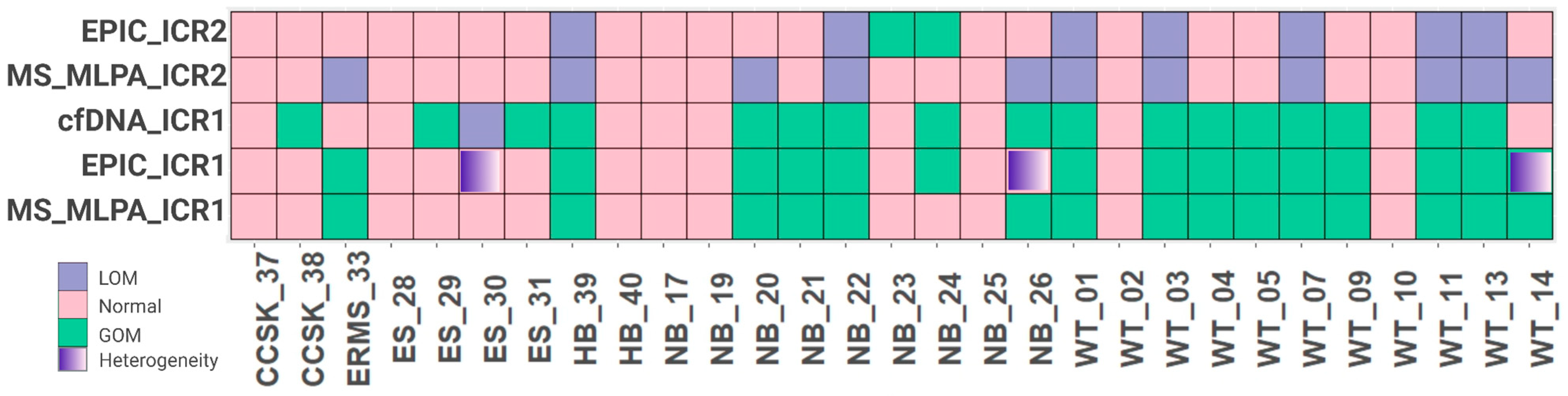
3.1. The Characterization of Methylation Status in ICR1 and ICR2, Located at the 11p15 Region in Embryonic Tumors
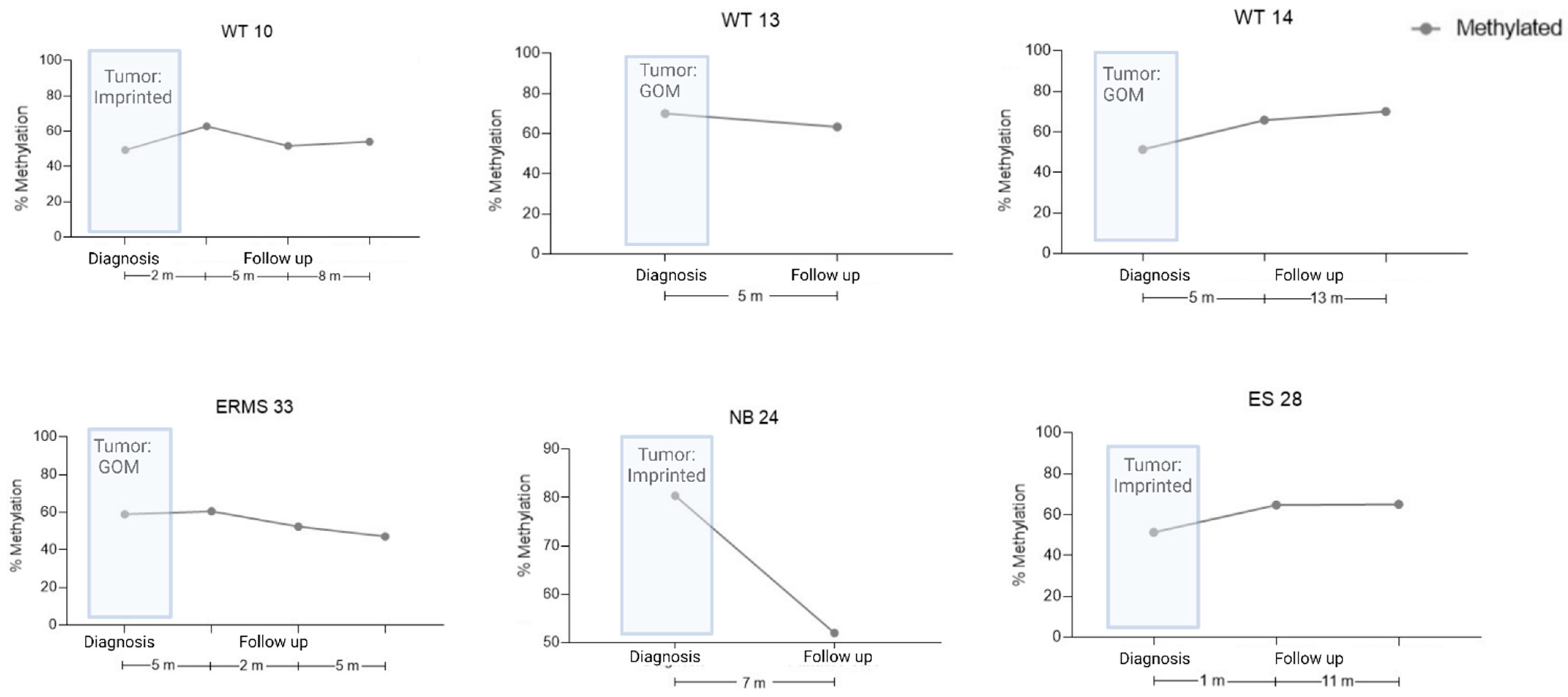
3.2. ICR1 Methylation Status Is Detectable at the cfDNA at Diagnosis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feinberg, A.P.; Ohlsson, R.; Henikoff, S. The epigenetic progenitor origin of human cancer. Nat. Rev. Genet. 2006, 7, 21–33. [Google Scholar] [CrossRef]
- Zhang, X.; Sjöblom, T. Targeting Loss of Heterozygosity: A Novel Paradigm for Cancer Therapy. Pharmaceuticals 2021, 14, 57. [Google Scholar] [CrossRef] [PubMed]
- Reik, W.; Walter, J. Genomic imprinting: Parental influence on the genome. Nat. Rev. Genet. 2001, 2, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Ishida, M.; Moore, G.E. The role of imprinted genes in humans. Mol. Asp. Med. 2013, 34, 826–840. [Google Scholar] [CrossRef] [PubMed]
- Rainier, S.; Johnson, L.A.; Dobry, C.J.; Ping, A.J.; Grundy, P.E.; Feinberg, A.P. Relaxation of imprinted genes in human cancer. Nature 1993, 362, 747–749. [Google Scholar] [CrossRef] [PubMed]
- Jelinic, P.; Shaw, P. Loss of imprinting and cancer. J. Pathol. 2007, 211, 261–268. [Google Scholar] [CrossRef]
- Charlton, J.; Williams, R.D.; Sebire, N.J.; Popov, S.; Vujanic, G.; Chagtai, T.; Alcaide-German, M.; Morris, T.; Butcher, L.M.; Guilhamon, P.; et al. Comparative methylome analysis identifies new tumour subtypes and biomarkers for transformation of nephrogenic rests into Wilms tumour. Genome Med. 2015, 7, 11. [Google Scholar] [CrossRef]
- MacFarland, S.P.; Duffy, K.A.; Bhatti, T.R.; Bagatell, R.; Balamuth, N.J.; Brodeur, G.M.; Ganguly, A.; Mattei, P.A.; Surrey, L.F.; Balis, F.M.; et al. Diagnosis of Beckwith-Wiedemann syndrome in children presenting with Wilms tumor. Pediatr. Blood Cancer 2018, 65, e27296. [Google Scholar] [CrossRef]
- Eggermann, T.; Maher, E.R.; Kratz, C.P.; Prawitt, D. Molecular Basis of Beckwith–Wiedemann Syndrome Spectrum with Associated Tumors and Consequences for Clinical Practice. Cancers 2022, 14, 3083. [Google Scholar] [CrossRef]
- Fiala, E.M.; Ortiz, M.V.; Kennedy, J.A.; Glodzik, D.; Fleischut, M.H.; Duffy, K.A.; Hathaway, E.R.; Heaton, T.; Gerstle, J.T.; Steinherz, P.; et al. 11p15.5 epimutations in children with Wilms tumor and hepatoblastoma detected in peripheral blood. Cancer 2020, 126, 3114–3121. [Google Scholar] [CrossRef]
- Stoltze, U.K.; Hildonen, M.; Hansen, T.V.O.; Foss-Skiftesvik, J.; Byrjalsen, A.; Lundsgaard, M.; Pignata, L.; Grønskov, K.; Tumer, Z.; Schmiegelow, K.; et al. Germline (epi)genetics reveals high predisposition in females: A 5-year, nationwide, prospective Wilms tumour cohort. J. Med. Genet. 2023. [Google Scholar] [CrossRef] [PubMed]
- Brioude, F.; Kalish, J.M.; Mussa, A.; Foster, A.C.; Bliek, J.; Ferrero, G.B.; Boonen, S.E.; Cole, T.; Baker, R.; Bertoletti, M.; et al. Clinical and molecular diagnosis, screening and management of Beckwith–Wiedemann syndrome: An international consensus statement. Nat. Rev. Endocrinol. 2018, 14, 229–249. [Google Scholar] [CrossRef] [PubMed]
- Charlton, J.; Williams, R.D.; Weeks, M.; Sebire, N.J.; Popov, S.; Vujanic, G.; Mifsud, W.; Alcaide-German, M.; Butcher, L.M.; Beck, S.; et al. Methylome analysis identifies a Wilms tumor epigenetic biomarker detectable in blood. Genome Biol. 2014, 15, 434. [Google Scholar] [CrossRef] [PubMed]
- Scott, R.H.; Murray, A.; Baskcomb, L.; Turnbull, C.; Loveday, C.; Al-Saadi, R.; Williams, R.; Breatnach, F.; Gerrard, M.; Hale, J.; et al. Stratification of Wilms tumor by genetic and epigenetic analysis. Oncotarget 2012, 3, 327–335. [Google Scholar] [CrossRef]
- Anderson, J.; Gordon, A.; McManus, A.; Shipley, J.; Pritchard-Jones, K. Disruption of Imprinted Genes at Chromosome Region 11p15.5 in Paediatric Rhabdomyosarcoma. Neoplasia 1999, 1, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Adam, G.; Cui, H.; Sandstedt, B.; Ohlsson, R.; Ekström, T.J. Expression, promoter usage and parental imprinting status of insulin-like growth factor II (IGF2) in human hepatoblastoma: Uncoupling of IGF2 and H19 imprinting. Oncogene 1995, 11, 221–229. [Google Scholar] [PubMed]
- Rumbajan, J.M.; Maeda, T.; Souzaki, R.; Mitsui, K.; Higashimoto, K.; Nakabayashi, K.; Yatsuki, H.; Nishioka, K.; Harada, R.; Aoki, S.; et al. Comprehensive analyses of imprinted differentially methylated regions reveal epigenetic and genetic characteristics in hepatoblastoma. BMC Cancer 2013, 13, 608. [Google Scholar] [CrossRef]
- Kurahashi, H.; Oue, T.; Akagi, K.; Fukuzawa, M.; Okada, A.; Tawa, A.; Okada, S.; Nishisho, I. Allelic status on 1p and 11p15 in neuroblastoma and benign ganglioneuroma. Int. J. Oncol. 1995, 6, 669–674. [Google Scholar] [CrossRef]
- Gröbner, S.N.; Worst, B.C.; Weischenfeldt, J.; Buchhalter, I.; Kleinheinz, K.; Rudneva, V.A.; Johann, P.D.; Balasubramanian, G.P.; Segura-Wang, M.; Brabetz, S.; et al. The landscape of genomic alterations across childhood cancers. Nature 2018, 555, 321–327. [Google Scholar] [CrossRef]
- Ma, X.; Liu, Y.; Liu, Y.; Alexandrov, L.B.; Edmonson, M.N.; Gawad, C.; Zhou, X.; Li, Y.; Rusch, M.C.; Easton, J.; et al. Pan-cancer genome and transcriptome analyses of 1699 paediatric leukaemias and solid tumours. Nature 2018, 555, 371–376. [Google Scholar] [CrossRef]
- van Zogchel, L.M.J.; Lak, N.S.M.; Verhagen, O.J.H.M.; Tissoudali, A.; Gussmalla Nuru, M.; Gelineau, N.U.; Zappeij-Kannengieter, L.; Javadi, A.; Zijtregtop, E.A.M.; Merks, J.H.M.; et al. Novel Circulating Hypermethylated RASSF1A ddPCR for Liquid Biopsies in Patients with Pediatric Solid Tumors. JCO Precis. Oncol. 2021, 5, 1738–1748. [Google Scholar] [CrossRef]
- Ruas, J.S.; Silva, F.L.T.; Euzébio, M.F.; Biazon, T.O.; Daiggi, C.M.M.; Nava, D.; Franco, M.T.; Cardinalli, I.A.; Cassone, A.E.; Pereira, L.H.; et al. Somatic Copy Number Alteration in Circulating Tumor DNA for Monitoring of Pediatric Patients with Cancer. Biomedicines 2023, 11, 1082. [Google Scholar] [CrossRef] [PubMed]
- Aryee, M.J.; Jaffe, A.E.; Corrada-Bravo, H.; Ladd-Acosta, C.; Feinberg, A.P.; Hansen, K.D.; Irizarry, R.A. Minfi: A flexible and comprehensive Bioconductor package for the analysis of Infinium DNA methylation microarrays. Bioinformatics 2014, 30, 1363–1369. [Google Scholar] [CrossRef] [PubMed]
- Fortin, J.-P.; Labbe, A.; Lemire, M.; Zanke, B.W.; Hudson, T.J.; Fertig, E.J.; Greenwood, C.M.; Hansen, K.D. Functional normalization of 450k methylation array data improves replication in large cancer studies. Genome Biol. 2014, 15, 503. [Google Scholar] [CrossRef]
- Suzuki, R.; Shimodaira, H. Pvclust: An R package for assessing the uncertainty in hierarchical clustering. Bioinformatics 2006, 22, 1540–1542. [Google Scholar] [CrossRef]
- Coffa, J.; Van De Wiel, M.A.; Diosdado, B.; Carvalho, B.; Schouten, J.; Meijer, G.A. MLPAnalyzer: Data analysis tool for reliable automated normalization of MLPA fragment data. Cell Oncol. 2008, 30, 323–335. [Google Scholar] [CrossRef]
- Scott, R.H.; Douglas, J.; Baskcomb, L.; Nygren, A.O.; Birch, J.M.; Cole, T.; Cormier-Daire, V.; Eastwood, D.M.; Garciaminaur, S.; Lupunzina, P.; et al. Methylation-specific multiplex ligation-dependent probe amplification (MS-MLPA) robustly detects and distinguishes 11p15 abnormalities associated with overgrowth and growth retardation. J. Med. Genet. 2008, 45, 106–113. [Google Scholar] [CrossRef]
- Coffee, B.; Muralidharan, K.; Highsmith, W.E.; Lapunzina, P.; Warren, S.T. Molecular diagnosis of Beckwith-Wiedemann Syndrome using quantitative methylation-sensitive polymerase chain reaction. Anesth. Analg. 2006, 8, 628–634. [Google Scholar] [CrossRef]
- Alharbi, M.; Mobark, N.; Bashawri, Y.; Abu Safieh, L.; Alowayn, A.; Aljelaify, R.; AlSaeed, M.; Almutairi, A.; Alqubaishi, F.; AlSolme, E.; et al. Methylation Profiling of Medulloblastoma in a Clinical Setting Permits Sub-classification and Reveals New Outcome Predictions. Front. Neurol. 2020, 11, 167. [Google Scholar] [CrossRef]
- Brzezinski, J.; Choufani, S.; Romao, R.; Shuman, C.; Chen, H.; Cunanan, J.; Bagli, D.; Grant, R.; Lorenzo, A.; Weksberg, R. Clinically and biologically relevant subgroups of Wilms tumour defined by genomic and epigenomic analyses. Br. J. Cancer 2021, 124, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Romani, M.; Pistillo, M.P.; Banelli, B. Epigenetic Targeting of Glioblastoma. Front. Oncol. 2018, 8, 448. [Google Scholar] [CrossRef]
- Roussel, M.F.; Stripay, J.L. Epigenetic Drivers in Pediatric Medulloblastoma. Cerebellum 2018, 17, 28–36. [Google Scholar] [CrossRef]
- Maschietto, M.; Rodrigues, T.C.; Kashiwabara, A.Y.; de Araujo, É.S.S.; Aguiar, T.F.M.; da Costa, C.M.L.; da Cunha, I.W.; Vasques, L.d.R.; Cypriano, M.; Brentani, H.; et al. DNA methylation landscape of hepatoblastomas reveals arrest at early stages of liver differentiation and cancer-related alterations. Oncotarget 2017, 8, 97871–97889. [Google Scholar] [CrossRef]
- Capper, D.; Jones, D.T.W.; Sill, M.; Hovestadt, V.; Schrimpf, D.; Sturm, D.; Koelsche, C.; Sahm, F.; Chavez, L.; Reuss, D.E.; et al. DNA methylation-based classification of central nervous system tumours. Nature 2018, 555, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Koelsche, C.; Schrimpf, D.; Stichel, D.; Sill, M.; Sahm, F.; Reuss, D.E.; Blattner, M.; Worst, B.; Heilig, C.E.; Beck, K.; et al. Sarcoma classification by DNA methylation profiling. Nat. Commun. 2021, 12, 498. [Google Scholar] [CrossRef] [PubMed]
- Tüysüz, B.; Bozlak, S.; Alkaya, D.U.; Ocak, S.; Kasap, B.; Çifçi, E.S.; Seker, A.; Bayhan, I.A.; Apak, H. Investigation of 11p15.5 Methylation Defects Associated with Beckwith-Wiedemann Spectrum and Embryonic Tumor Risk in Lateralized Overgrowth Patients. Cancers 2023, 15, 1872. [Google Scholar] [CrossRef]
- Maschietto, M.; Charlton, J.; Perotti, D.; Radice, P.; Geller, J.I.; Pritchard-Jones, K.; Weeks, M. The IGF signalling pathway in Wilms tumours—A report from the ENCCA Renal Tumours Biology-driven drug development workshop. Oncotarget 2014, 5, 8014–8026. [Google Scholar] [CrossRef]
- Mussa, A.; Molinatto, C.; Baldassarre, G.; Riberi, E.; Russo, S.; Larizza, L.; Riccio, A.; Ferrero, G.B. Cancer Risk in Beckwith-Wiedemann Syndrome: A Systematic Review and Meta-Analysis Outlining a Novel (Epi)Genotype Specific Histotype Targeted Screening Protocol. J. Pediatr. 2016, 176, 142–149.e1. [Google Scholar] [CrossRef] [PubMed]
- Spreafico, F.; Fernandez, C.V.; Brok, J.; Nakata, K.; Vujanic, G.; Geller, J.I.; Gessler, M.; Maschietto, M.; Behjati, S.; Polanco, A.; et al. Wilms tumour. Nat. Rev. Dis. Prim. 2021, 7, 75. [Google Scholar] [CrossRef]
- Schuster, A.E.; Schneider, D.T.; Fritsch, M.K.; Grundy, P.; Perlman, E.J. Genetic and Genetic Expression Analyses of Clear Cell Sarcoma of the Kidney. Lab. Investig. 2003, 83, 1293–1299. [Google Scholar] [CrossRef] [PubMed]
- Abbou, S.D.; Shulman, D.S.; Dubois, S.G.; Crompton, B.D. Assessment of circulating tumor DNA in pediatric solid tumors: The promise of liquid biopsies. HHS Public Access Pediatr. Blood Cancer 2019, 66, e27595. [Google Scholar] [CrossRef] [PubMed]
- van Zogchel, L.M.J.; van Wezel, E.M.; van Wijk, J.; Stutterheim, J.; Bruins, W.S.C.; Zappeij-Kannegieter, L.; Slager, T.J.E.; Schumacher-Kuckelkorn, R.; Verly, I.R.N.; van der Schoot, C.E.; et al. Hypermethylated RASSF1A as Circulating Tumor DNA Marker for Disease Monitoring in Neuroblastoma. JCO Precis. Oncol. 2020, 4, 291–306. [Google Scholar] [CrossRef] [PubMed]
- Stuppia, L.; Antonucci, I.; Palka, G.; Gatta, V. Use of the MLPA Assay in the Molecular Diagnosis of Gene Copy Number Alterations in Human Genetic Diseases. Int. J. Mol. Sci. 2012, 13, 3245–3276. [Google Scholar] [CrossRef] [PubMed]

| Tumor Type | Characterized Tumors (n) | Tumors with ICR1 LOM | Tumors with ICR1 GOM | Tumors with ICR2 LOM |
|---|---|---|---|---|
| Atypical teratoid rhabdoid tumor | 2 | 0 | 0 | 0 |
| Clear cell sarcoma of the kidney | 2 | 0 | 0 | 0 |
| Diffuse midline gliomas H3 K27-altered * | 3 | 0 | 1 (3.3%) | 0 |
| Embryonal rhabdomyosarcoma | 4 | 0 | 4 (100%) | 3 (75%) |
| Ewing sarcoma | 17 | 0 | 0 | 0 |
| Ganglioneuroblastoma | 1 | 0 | 0 | 0 |
| Hepatoblastoma | 3 | 0 | 2 (67.3%) | 2 (67.3%) |
| Medulloblastoma, unclassified | 8 | 3 (37.5%) | 0 | 0 |
| Medulloblastoma_G34 * | 12 | 7 (58.3%) | 1 (8.33%) | 1 (8.33%) |
| Medulloblastoma_SHH * | 4 | 1 (25%) | 1 (25%) | 0 |
| Medulloblastoma_WNT * | 5 | 1 (20%) | 1 (20%) | 0 |
| Neuroblastoma | 16 | 0 | 7 (43.75%) | 1 (6.25%) |
| Osteoblastoma | 1 | 0 | 0 | 0 |
| Pineoblastoma_FOXR2 * | 1 | 1 (100%) | 0 | 0 |
| Pineoblastoma_GRP1A * | 1 | 1 (100%) | 0 | 0 |
| Pleomorphic xanthoastrocytoma * | 1 | 0 | 0 | 0 |
| Rhabdomyosarcoma | 1 | 0 | 1 (100%) | 0 |
| Wilms tumor | 17 | 0 | 14 (82.35%) | 7 (41.17%) |
| Comparison | Sensitivity (%) | Specificity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) |
|---|---|---|---|---|
| ICR1 Technical (EPIC/MS-MLPA) | 93.3 | 92.9 | 93.3 | 92.9 |
| ICR2 Technical (EPIC/MS-MLPA) | 63.6 | 88.9 | 77.8 | 80 |
| ICR1 Biological (MS-MLPA/cfDNA) | 86.7 | 64.3 | 72.2 | 81.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, F.L.T.; Ruas, J.S.; Euzébio, M.F.; Hoffmann, I.L.; Junqueira, T.; Tedeschi, H.; Pereira, L.H.; Cassone, A.E.; Cardinalli, I.A.; Seidinger, A.L.; et al. 11p15 Epimutations in Pediatric Embryonic Tumors: Insights from a Methylome Analysis. Cancers 2023, 15, 4256. https://doi.org/10.3390/cancers15174256
Silva FLT, Ruas JS, Euzébio MF, Hoffmann IL, Junqueira T, Tedeschi H, Pereira LH, Cassone AE, Cardinalli IA, Seidinger AL, et al. 11p15 Epimutations in Pediatric Embryonic Tumors: Insights from a Methylome Analysis. Cancers. 2023; 15(17):4256. https://doi.org/10.3390/cancers15174256
Chicago/Turabian StyleSilva, Felipe Luz Torres, Juliana Silveira Ruas, Mayara Ferreira Euzébio, Iva Loureiro Hoffmann, Thais Junqueira, Helder Tedeschi, Luiz Henrique Pereira, Alejandro Enzo Cassone, Izilda Aparecida Cardinalli, Ana Luiza Seidinger, and et al. 2023. "11p15 Epimutations in Pediatric Embryonic Tumors: Insights from a Methylome Analysis" Cancers 15, no. 17: 4256. https://doi.org/10.3390/cancers15174256






