Carbohydrate, Lipid, and Apolipoprotein Biomarkers in Blood and Risk of Thyroid Cancer: Findings from the AMORIS Cohort
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
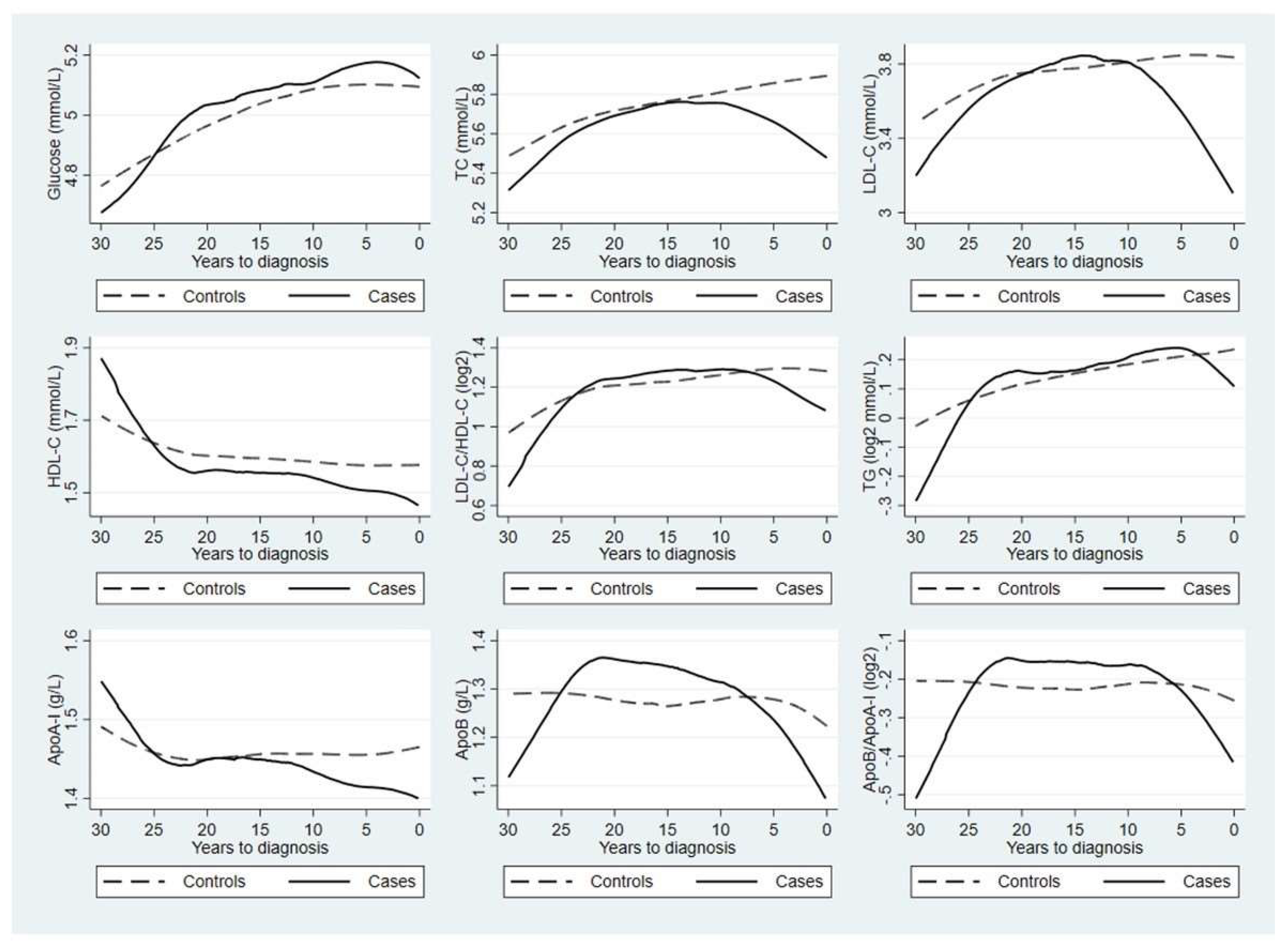
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Cancer Epidemiology and Prevention, 4th ed.; Oxford University Press: Oxford, UK, 2018; pp. 839–860.
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
- Coelho, R.G.; Fortunato, R.S.; Carvalho, D.P. Metabolic Reprogramming in Thyroid Carcinoma. Front. Oncol. 2018, 8, 82. [Google Scholar] [CrossRef]
- Heydarzadeh, S.; Moshtaghie, A.A.; Daneshpoor, M.; Hedayati, M. Regulators of glucose uptake in thyroid cancer cell lines. Cell Commun. Signal. 2020, 18, 83. [Google Scholar] [CrossRef]
- Wen, S.; Luo, Y.; Wu, W.; Zhang, T.; Yang, Y.; Ji, Q.; Wu, Y.; Shi, R.; Ma, B.; Xu, M.; et al. Identification of lipid metabolism-related genes as prognostic indicators in papillary thyroid cancer. Acta Biochim. Biophys. Sin. 2021, 53, 1579–1589. [Google Scholar] [CrossRef]
- von Roemeling, C.A.; Copland, J.A. Targeting lipid metabolism for the treatment of anaplastic thyroid carcinoma. Expert Opin. Targets 2016, 20, 159–166. [Google Scholar] [CrossRef]
- Park, J.H.; Cho, H.S.; Yoon, J.H. Thyroid Cancer in Patients with Metabolic Syndrome or Its Components: A Nationwide Population-Based Cohort Study. Cancers 2022, 14, 4106. [Google Scholar] [CrossRef]
- Alkurt, E.G.; Şahin, F.; Tutan, B.; Canal, K.; Turhan, V.B. The relationship between papillary thyroid cancer and triglyceride/glucose index, which is an indicator of insulin resistance. Eur. Rev. Med. Pharm. Sci. 2022, 26, 6114–6120. [Google Scholar] [CrossRef]
- Fussey, J.M.; Beaumont, R.N.; Wood, A.R.; Vaidya, B.; Smith, J.; Tyrrell, J. Does obesity cause thyroid cancer? A Mendelian randomization study. J. Clin. Endocrinol. Metab. 2020, 105, e2398–e2407. [Google Scholar] [CrossRef]
- Park, J.H.; Choi, M.; Kim, J.H.; Kim, J.; Han, K.; Kim, B.; Kim, D.H.; Park, Y.G. Metabolic Syndrome and the Risk of Thyroid Cancer: A Nationwide Population-Based Cohort Study. Thyroid 2020, 30, 1496–1504. [Google Scholar] [CrossRef]
- Hu, M.J.; Zhang, C.; Liang, L.; Wang, S.Y.; Zheng, X.C.; Zhang, Q.; Jiang, C.X.; Zhong, Q.; Huang, F. Fasting serum glucose, thyroid-stimulating hormone, and thyroid hormones and risk of papillary thyroid cancer: A case-control study. Head Neck 2019, 41, 2277–2284. [Google Scholar] [CrossRef]
- Kim, M.-H.; Huh, J.-Y.; Lim, D.-J.; Kang, M.-I. Does the risk of metabolic syndrome increase in thyroid cancer survivors? Thyroid 2017, 27, 936–943. [Google Scholar] [CrossRef]
- Bae, M.J.; Kim, S.S.; Kim, W.J.; Yi, Y.S.; Jeon, Y.K.; Kim, B.H.; Lee, B.J.; Lee, J.C.; Kim, I.J.; Wang, S.G. High prevalence of papillary thyroid cancer in Korean women with insulin resistance. Head Neck 2016, 38, 66–71. [Google Scholar] [CrossRef]
- Balkan, F.; Onal, E.D.; Usluogullari, A.; Tuzun, D.; Ozdemir, D.; Inancli, S.S.; Ersoy, R.; Cakir, B. Is there any association between insulin resistance and thyroid cancer?: A case control study. Endocrine 2014, 45, 55–60. [Google Scholar] [CrossRef]
- Han, J.M.; Kim, T.Y.; Jeon, M.J.; Yim, J.H.; Kim, W.G.; Song, D.E.; Hong, S.J.; Bae, S.J.; Kim, H.K.; Shin, M.H.; et al. Obesity is a risk factor for thyroid cancer in a large, ultrasonographically screened population. Eur. J. Endocrinol. 2013, 168, 879–886. [Google Scholar] [CrossRef]
- Almquist, M.; Johansen, D.; Björge, T.; Ulmer, H.; Lindkvist, B.; Stocks, T.; Hallmans, G.; Engeland, A.; Rapp, K.; Jonsson, H.; et al. Metabolic factors and risk of thyroid cancer in the Metabolic syndrome and Cancer project (Me-Can). Cancer Causes Control 2011, 22, 743–751. [Google Scholar] [CrossRef]
- Giusti, M.; Mortara, L.; Degrandi, R.; Cecoli, F.; Mussap, M.; Rodriguez, G.; Ferone, D.; Minuto, F. Metabolic and cardiovascular risk in patients with a history of differentiated thyroid carcinoma: A case-controlled cohort study. Thyroid Res. 2008, 1, 2. [Google Scholar] [CrossRef]
- Rapp, K.; Schroeder, J.; Klenk, J.; Ulmer, H.; Concin, H.; Diem, G.; Oberaigner, W.; Weiland, S. Fasting blood glucose and cancer risk in a cohort of more than 140,000 adults in Austria. Diabetologia 2006, 49, 945–952. [Google Scholar] [CrossRef]
- Xu, H.; Pang, Y.; Li, X.; Zha, B.; He, T.; Ding, H. Monocyte to high-density lipoprotein cholesterol ratio as an independent risk factor for papillary thyroid carcinoma. J. Clin. Lab. Anal. 2021, 35, e24014. [Google Scholar] [CrossRef]
- Zhao, J.; Tian, Y.; Yao, J.; Gu, H.; Zhang, R.; Wang, H.; Liao, L.; Dong, J. Hypercholesterolemia Is an Associated Factor for Risk of Differentiated Thyroid Cancer in Chinese Population. Front. Oncol. 2020, 10, 508126. [Google Scholar] [CrossRef]
- Chrisoulidou, A.; Pazaitou-Panayiotou, K.; Georgiou, E.; Boudina, M.; Lytras, K.; Iakovou, I.; Vainas, I.; Kaltsas, G. The hypothalamic-pituitary-adrenal axis in women with differentiated thyroid cancer. Endocr. Res. 2010, 35, 137–143. [Google Scholar] [CrossRef]
- Tulinius, H.; Sigfússon, N.; Sigvaldason, H.; Bjarnadóttir, K.; Tryggvadóttir, L. Risk factors for malignant diseases: A cohort study on a population of 22,946 Icelanders. Cancer Epidemiol. Biomark. Prev. 1997, 6, 863–873. [Google Scholar]
- Li, D.; Zhou, L.; Ma, C.; Chen, W.; Zhang, Y.; Yu, S.; Wang, D.; Zou, Y.; Wu, J.; Qiu, L. Comparative analysis of the serum proteome profiles of thyroid cancer: An initial focus on the lipid profile. Oncol. Lett. 2019, 18, 3349–3357. [Google Scholar] [CrossRef]
- Revilla, G.; Pons, M.P.; Baila-Rueda, L.; García-León, A.; Santos, D.; Cenarro, A.; Magalhaes, M.; Blanco, R.M.; Moral, A.; Ignacio Pérez, J.; et al. Cholesterol and 27-hydroxycholesterol promote thyroid carcinoma aggressiveness. Sci. Rep. 2019, 9, 10260. [Google Scholar] [CrossRef]
- Abiaka, C.; Al-Awadi, F.; Al-Sayer, H.; Gulshan, S.; Behbehani, A.; Farghally, M.; Simbeye, A. Serum antioxidant and cholesterol levels in patients with different types of cancer. J. Clin. Lab. Anal. 2001, 15, 324–330. [Google Scholar] [CrossRef]
- Borena, W.; Stocks, T.; Jonsson, H.; Strohmaier, S.; Nagel, G.; Bjørge, T.; Manjer, J.; Hallmans, G.; Selmer, R.; Almquist, M.; et al. Serum triglycerides and cancer risk in the metabolic syndrome and cancer (Me-Can) collaborative study. Cancer Causes Control 2011, 22, 291–299. [Google Scholar] [CrossRef]
- Ulmer, H.; Borena, W.; Rapp, K.; Klenk, J.; Strasak, A.; Diem, G.; Concin, H.; Nagel, G. Serum triglyceride concentrations and cancer risk in a large cohort study in Austria. Br. J. Cancer 2009, 101, 1202–1206. [Google Scholar] [CrossRef]
- Kim, J.; Kim, M.K.; Baek, K.H.; Song, K.H.; Han, K.; Kwon, H.S. Repeated Low High-Density Lipoprotein Cholesterol and the Risk of Thyroid Cancer: A Nationwide Population- Based Study in Korea. Endocrinol. Metab. 2022, 37, 303–311. [Google Scholar] [CrossRef]
- Walldius, G.; Malmström, H.; Jungner, I.; de Faire, U.; Lambe, M.; Van Hemelrijck, M.; Hammar, N. Cohort Profile: The AMORIS cohort. Int. J. Epidemiol. 2017, 46, 1103–1103i. [Google Scholar] [CrossRef]
- Walldius, G.; Jungner, I.; Holme, I.; Aastveit, A.H.; Kolar, W.; Steiner, E. High apolipoprotein B, low apolipoprotein A-I, and improvement in the prediction of fatal myocardial infarction (AMORIS study): A prospective study. Lancet 2001, 358, 2026–2033. [Google Scholar] [CrossRef]
- Talmud, P.J.; Hawe, E.; Miller, G.J.; Humphries, S.E. Nonfasting apolipoprotein B and triglyceride levels as a useful predictor of coronary heart disease risk in middle-aged UK men. Arterioscler. Thromb. Vasc. Biol. 2002, 22, 1918–1923. [Google Scholar] [CrossRef] [PubMed]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Barlow, L.; Westergren, K.; Holmberg, L.; Talbäck, M. The completeness of the Swedish Cancer Register: A sample survey for year 1998. Acta Oncol. 2009, 48, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.F.; Svedberg, P.; Olén, O.; Bruze, G.; Neovius, M. The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur. J. Epidemiol. 2019, 34, 423–437. [Google Scholar] [CrossRef]
- Lubin, J.H.; Gail, M.H. Biased selection of controls for case-control analyses of cohort studies. Biometrics 1984, 40, 63–75. [Google Scholar] [CrossRef]
- Kuzu, O.F.; Noory, M.A.; Robertson, G.P. The Role of Cholesterol in Cancer. Cancer Res. 2016, 76, 2063–2070. [Google Scholar] [CrossRef]
- Chiesa, S.T.; Charakida, M. High-Density Lipoprotein Function and Dysfunction in Health and Disease. Cardiovasc. Drugs 2019, 33, 207–219. [Google Scholar] [CrossRef]
- Pedersen, K.M.; Colak, Y.; Bojesen, S.E.; Nordestgaard, B.G. Low high-density lipoprotein and increased risk of several cancers: 2 population-based cohort studies including 116,728 individuals. J. Hematol. Oncol. 2020, 13, 129. [Google Scholar] [CrossRef]
- Pirro, M.; Ricciuti, B.; Rader, D.J.; Catapano, A.L.; Sahebkar, A.; Banach, M. High density lipoprotein cholesterol and cancer: Marker or causative? Prog. Lipid Res. 2018, 71, 54–69. [Google Scholar] [CrossRef]
- Mason, R.L.; Hunt, H.M.; Hurxthal, L. Blood cholesterol values in hyperthyroidism and hypothyroidism-their significance. N. Engl. J. Med. 1930, 203, 1273–1278. [Google Scholar] [CrossRef]
- Duntas, L.H.; Brenta, G. A Renewed Focus on the Association between Thyroid Hormones and Lipid Metabolism. Front. Endocrinol. 2018, 9, 511. [Google Scholar] [CrossRef] [PubMed]
- Canaris, G.J.; Manowitz, N.R.; Mayor, G.; Ridgway, E.C. The Colorado thyroid disease prevalence study. Arch. Intern. Med. 2000, 160, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Tagami, T.; Kimura, H.; Ohtani, S.; Tanaka, T.; Tanaka, T.; Hata, S.; Saito, M.; Miyazaki, Y.; Araki, R.; Tanaka, M.; et al. Multi-center study on the prevalence of hypothyroidism in patients with hypercholesterolemia. Endocr. J. 2011, 58, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Lalami, Y.; Awada, A. Recurrent thyroid cancer: A molecular-based therapeutic breakthrough. Curr. Opin. Oncol. 2011, 23, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Kitahara, C.; Sosa, J. The changing incidence of thyroid cancer. Nat. Rev. Endocrinol. 2016, 12, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Kotwal, A.; Cortes, T.; Genere, N.; Hamidi, O.; Jasim, S.; Newman, C.; Prokop, L.; Murad, M.; Alahdab, F. Treatment of Thyroid Dysfunction and Serum Lipids: A Systematic Review and Meta-analysis. J. Clin. Endocrinol. Metab. 2020, 105, dgaa672. [Google Scholar] [CrossRef]
| Study; Country | Biomarker; Outcome | Study Design | Sample Size | Result |
|---|---|---|---|---|
| Glucose | ||||
| Park et al. (2022) [8]; Korea | Hyperglycemia; relative risk (RR) of thyroid cancer | Cohort with 6 years of follow-up | 4,658,473 participants with 47,325 cases of thyroid cancer | Male: RR = 0.99 (95%CI: 0.96–1.03) Female: RR = 1.03 (95%CI: 1.01–1.06) |
| Alkurt et al. (2022) [9]; Turkey | Glucose; mean difference between groups | Cross-sectional study | 254 patients with papillary thyroid cancer and 128 controls | 112.98 mg/dL among controls vs. 143.05 mg/dL among patients with thyroid cancer (p for difference: <0.001) |
| Fussey et al. (2020) [10]; UK | Serum glucose; odds ratio (OR) of thyroid cancer | Cross-sectional study | 425 individuals with thyroid cancer and 310,176 controls | OR = 0.97 (95%CI: 0.83–1.14) per standard deviation (SD) increase |
| Park et al. (2020) [11]; Korea | Fasting plasma glucose; hazard ratio (HR) of thyroid cancer | Nationwide cohort with 7.2 years of follow-up | 9,890,917 participants with 77,133 cases of thyroid cancer | HR = 0.99 (95%CI: 0.97–1.00) per unit increase |
| Hu et al. (2019) [12]; China | Fasting serum glucose; odds ratio (OR) of thyroid cancer | Case-control study | 320 cases with papillary thyroid cancer and 329 controls | Association between increasing level and higher risk of thyroid cancer (p for trend: 0.01) |
| Kim et al. (2017) [13]; Korea | Fasting plasma glucose ≥100 mg/dL; difference in prevalence between groups | Cross-sectional study | 34,347 individuals including 155 individuals with prevalent thyroid cancer | p for difference: 0.435 |
| Bae et al. (2016) [14]; Korea | Fasting glucose; mean difference between groups | Case-control study | 735 patients with thyroid cancer and 537 controls | 91.5 mg/dL among cases vs. 87.9 mg/dL among controls; p for difference: <0.01 |
| Balkan et al. (2014) [15]; Turkey | Fasting plasma glucose; mean difference between groups | Case-control study | 41 cases with thyroid cancer and 41 age- and gender-matched controls | 93.4 mg/dL among cases vs. 90.8 mg/dL among controls; p for difference: >0.05 |
| Han et al. (2013) [16]; Korea | Glucose; mean difference between groups | Cross-sectional study | 15,068 participants including 267 cases of thyroid cancer | Male: 100 mg/dL among cases vs. 101 mg/dL among controls; p for difference: 0.664 Female: 98.5 mg/dL among cases vs. 95.0 mg/dL among controls; p for difference: 0.066 |
| Almquist et al. (2011) [17]; Norway, Austria, and Sweden | Glucose; relative risk (RR) of thyroid cancer | Cohort with 12.0 years of follow-up | 578,700 participants with 388 incident cases of thyroid cancer | Male: Increased risk per quintile increase; p for trend: 0.08 Female: Decreased risk per quintile increase; p for trend: 0.02 |
| Giusti et al. (2008) [18]; Italy | Glucose; mean difference between groups | Case-control study | 106 cases with thyroid cancer and 87 controls | 4.7 mmol/L among cases vs. 4.9 mmol/L among controls; p for difference: ns |
| Rapp et al. (2006) [19]; Austria | Glucose; hazard ratio (HR) of thyroid cancer | Cohort with 8.4 years of follow-up | 140,813 participants with 70 incident cases of thyroid cancer | Increasing risk of thyroid cancer with increasing level; p for trend: 0.02 |
| Xu et al. (2021) [20]; China | Fasting plasma glucose; mean difference between groups | Case-control study | 372 patients with thyroid cancer and 651 controls with benign thyroid nodule | 4.72 mmol/L among cases vs. 5.06 mmol/L among controls; p for difference: 0.530 |
| Zhao et al. (2020) [21]; China | Fasting plasma glucose; mean difference between groups | Case-control study | 2021 patients with thyroid cancer and 1727 patients with benign thyroid nodules | 5.18 mmol/L among cases vs. 5.21 mmol/L among controls; p for difference: 0.174 |
| Chrisoulidou et al. (2011) [22]; Greece | Glucose area under the curve; mean difference between groups | Case-control study | 16 women with thyroid cancer and 14 controls | 557 among cases vs. 772 among controls; p for difference: ns |
| Tulinius et al. (1997) [23]; Iceland | Glucose 90 min; relative risk (RR) of thyroid cancer | Cohort | 22,946 participants with 83 incident cases of thyroid cancer | Female: RR = 1.12 (95%CI: 1.06–1.19) per unit increase |
| Total cholesterol | ||||
| Bae et al. (2016) [14]; Korea | Total cholesterol; mean difference between groups | Case-control study | 735 patients with thyroid cancer and 537 controls | 194.5 mg/dL among cases vs. 200.5 mg/dL among controls; p for difference: 0.005 |
| Xu et al. (2021) [20]; China | Total cholesterol; mean difference between groups | Case-control study | 372 patients with thyroid cancer and 651 controls with benign thyroid nodule | 4.56 mmol/L among cases vs. 4.60 mmol/L among controls; p for difference: 0.588 |
| Zhao et al. (2020) [21]; China | Total cholesterol; mean difference between groups | Case-control study | 2021 patients with thyroid cancer and 1727 patients with benign thyroid nodules | 4.67 mmol/L among cases vs. 4.67 mmol/L among controls; p for difference: <0.001 (?) |
| Li et al. (2019) [24]; China | Total cholesterol; mean difference between groups | Case-control study | 1717 cases of thyroid cancer and 2158 healthy controls | Men: 4.49 mmol/L among cases vs. 4.63 mmol/L among controls; p for difference: 0.040 Women: 4.65 mmol/L among cases vs. 4.78 mmol/L among controls; p for difference: 0.002 |
| Revilla et al. (2019) [25]; Spain | Cholesterol; mean difference between groups | Cross-sectional study | 27 patients with benign thyroid tumor; 43 patients with low/intermediate thyroid cancer; 12 patients with high-risk thyroid cancer; and 7 patients with poorly differentiated and anaplastic thyroid carcinoma | Lower level among patients with high-risk thyroid cancer and patients with PDTC/ATC, compared to patients with BTT; p for difference: <0.05 |
| Han et al. (2013) [16]; Korea | Cholesterol; mean difference between groups | Cross-sectional study | 15,068 participants including 267 cases of thyroid cancer | Male: 193.3 mg/dL among cases vs. 191.6 mg/dL among controls; p for difference: 0.533; Female: 192.8 mg/dL among cases vs. 193.6 mg/dL among controls; p for difference: 0.798 |
| Almquist et al. (2011) [17]; Norway, Austria, and Sweden | Cholesterol; relative risk (RR) of thyroid cancer | Cohort with 12.0 years of follow-up | 578,700 participants with 388 incident cases of thyroid cancer | Male: No altered risk per quintile increase; p for trend: 0.65 Female: No altered risk per quintile increase; p for trend: 0.38 |
| Giusti et al. (2008) [18]; Italy | Cholesterol; mean difference between groups | Case-control study | 106 cases with thyroid cancer and 87 controls | 5.36 mmol/L among cases vs. 5.51 mmol/L among controls; p for difference: ns |
| Abiaka et al. (2001) [26]; Kuwait | Cholesterol; mean difference between groups | Case-control study | 14 cases with thyroid cancer and 100 controls | 4.4 mM among cases vs. 4.4 mM among controls; p for difference: ns |
| Chrisoulidou et al. (2011) [22]; Greece | Total cholesterol; mean difference between groups | Case-control study | 16 women with thyroid cancer and 14 controls | 182 mg/dL among cases vs. 173 mg/dL among controls; p for difference: ns |
| Triglycerides | ||||
| Alkurt et al. (2022) [9]; Turkey | Triglycerides; mean difference between groups | Cross-sectional study | 254 patients with papillary thyroid cancer and 128 controls | 144.21 mg/dL among controls vs. 152.24 mg/dL among patients with thyroid cancer (p for difference: 0.691) |
| Park et al. (2022) [8]; Korea | Hypertriglyceridemia: relative risk (RR) of thyroid cancer | Cohort with 6 years of follow-up | 4,658,473 participants with 47,325 cases of thyroid cancer | Male: RR = 1.02 (95%CI: 0.99–1.06) Female: RR = 1.06 (95%CI: 1.04–1.09) |
| Fussey et al. (2020) [10]; UK | Serum triglycerides; odds ratio (OR) of thyroid cancer | Cross-sectional study | 425 individuals with thyroid cancer and 310,176 controls | OR = 1.06 (95%CI: 0.93–1.20) per SD increase |
| Park et al. (2020) [11]; Korea | Triglycerides; hazard ratio (HR) of thyroid cancer | Nationwide cohort with 7.2 years of follow-up | 9,890,917 participants with 77,133 cases of thyroid cancer | HR = 0.96 (95%CI: 0.95–0.98) per unit increase |
| Zhao et al. (2020) [21]; China | Triglycerides; mean difference between groups | Case-control study | 2021 patients with thyroid cancer and 1727 patients with benign thyroid nodules | 1.16 mmol/L among cases vs. 1.04 mmol/L among controls; p for difference: 0.001 |
| Revilla et al. (2019) [25]; Span | Triglycerides; mean difference between groups | Cross-sectional study | 27 patients with benign thyroid tumor; 43 patients with low/intermediate thyroid cancer; 12 patients with high-risk thyroid cancer; and 7 patients with poorly differentiated and anaplastic thyroid carcinoma | Lower level among patients with high-risk thyroid cancer, compared to patients with BTT; p for difference: <0.01 |
| Li et al. (2019) [24]; China | Triglycerides; mean difference between groups | Case-control study | 1717 cases of thyroid cancer and 2158 healthy controls | Men: 1.51 mmol/L among cases vs. 1.52 mmol/L among controls; p for difference: 0.632 Women: 1.10 mmol/L among cases vs. 0.99 mmol/L among controls; p for difference: <0.001 |
| Kim et al. (2017) [13]; Korea | Triglycerides ≥150 mg/dL; difference in prevalence between groups | Cross-sectional study | 34,347 individuals including 155 individuals with prevalent thyroid cancer | p for difference: 0.517 |
| Balkan et al. (2014) [15]; Turkey | Triglycerides; mean difference between groups | Case-control study | 41 cases with thyroid cancer and 41 age- and gender-matched controls | 132.5 mg/dL among cases vs. 123.8 mg/dL among controls; p for difference: >0.05 |
| Han et al. (2013) [16]; Korea | Triglycerides; mean difference between groups | Cross-sectional study | 15,068 participants including 267 cases of thyroid cancer | Male: 139 mg/dL among cases vs. 130 mg/dL among controls; p for difference: 0.650 Female: 90 mg/dL among cases vs. 92 mg/dL among controls; p for difference: 0.159 |
| Borena et al. (2011) [27]; Norway, Austria, and Sweden | Serum triglycerides; relative risk (RR) of thyroid cancer | Cohort with 13.4 years of follow-up | 514,097 participants including 131 incident cases of thyroid cancer | Men: RR = 1.53 (95%CI: 0.80–2.89) per log unit increase Women: RR = 0.98 (95%CI: 0.60–1.63) per log unit increase |
| Chrisoulidou et al. (2011) [22]; Greece | Triglycerides; mean difference between groups | Case-control study | 16 women with thyroid cancer and 14 controls | 80 mg/dL among cases vs. 120 mg/dL among controls; p for difference: ns |
| Almquist et al. (2011) [17]; Norway, Austria, and Sweden | Triglycerides; relative risk (RR) of thyroid cancer | Cohort with 12.0 years of follow-up | 578,700 participants with 388 incident cases of thyroid cancer | Male: No altered risk per quintile increase; p for trend: 0.28 Female: No altered risk per quintile increase; p for trend: 0.46 |
| Ulmer et al. (2009) [28]; Austria | Serum triglycerides; relative risk (RR) of thyroid cancer | Cohort with 10.6 years of follow-up | 156,153 participants with 101 incident cases of thyroid cancer | Comparing highest to lowest quartile: RR = 1.96 (95%CI: 1.00–3.84) |
| Giusti et al. (2008) [18]; Italy | Triglycerides; mean difference between groups | Case-control study | 106 cases with thyroid cancer and 87 controls | 1.26 mmol/L among cases vs. 1.21 mmol/L among controls; p for difference: ns |
| Tulinius et al. (1997) [23]; Iceland | Triglycerides; relative risk (RR) of thyroid cancer | Cohort | 22,946 participants with 83 incident cases of thyroid cancer | Male: RR = 1.46 (95%CI: 1.12–1.91) per unit increase |
| LDL-C | ||||
| Xu et al. (2021) [20]; China | LDL-C; mean difference between groups | Case-control study | 372 patients with thyroid cancer and 651 controls with benign thyroid nodule | 2.93 mmol/L among cases vs. 2.97 mmol/L among controls; p for difference: 0.567 |
| Zhao et al. (2020) [21]; China | LDL-C; mean difference between groups | Case-control study | 2021 patients with thyroid cancer and 1727 patients with benign thyroid nodules | 2.71 mmol/L among cases vs. 2.69 mmol/L among controls; p for difference: 0.125 |
| Fussey et al. (2020) [10]; UK | Serum LDL-C; odds ratio (OR) of thyroid cancer | Cross-sectional study | 425 individuals with thyroid cancer and 310,176 controls | OR = 1.00 (95%CI: 0.87–1.05) per SD increase |
| Revilla et al. (2019) [25]; Spain | LDL-C; mean difference between groups | Cross-sectional study | 27 patients with benign thyroid tumor; 43 patients with low/intermediate thyroid cancer; 12 patients with high-risk thyroid cancer; and 7 patients with poorly differentiated and anaplastic thyroid carcinoma | Lower level among patients with PDTC/ATC, compared to patients with BTT; p for difference: <0.05 |
| Li et al. (2019) [24]; China | LDL-C; mean difference between groups | Case-control study | 1717 cases of thyroid cancer and 2158 healthy controls | Men: 2.66 mmol/L among cases vs. 2.74 mmol/L among controls; p for difference: 0.119 Women: 2.67 mmol/L among cases vs. 2.75 mmol/L among controls; p for difference: 0.025 |
| Balkan et al. (2014) [15]; Turkey | LDL-C; mean difference between groups | Case-control study | 41 cases with thyroid cancer and 41 age- and gender-matched controls | 122.7 mg/dL among cases vs. 112.6 mg/dL among controls; p for difference: >0.05 |
| Giusti et al. (2008) [18]; Italy | LDL-C; mean difference between groups | Case-control study | 106 cases with thyroid cancer and 87 controls | 3.11 mmol/L among cases vs. 2.93 mmol/L among controls; p for difference: ns |
| Chrisoulidou et al. (2011) [22]; Greece | LDL-C; mean difference between groups | Case-control study | 16 women with thyroid cancer and 14 controls | 88 mg/dL among cases vs. 98 mg/dL among controls; p for difference: ns |
| HDL-C | ||||
| Kim et al. (2022) [29]; Korea | Number of times a low HDL-C (<40 mg/dL for men and <50 mg/dL for women) was identified; hazard ratio (HR) of thyroid cancer | Cohort with 8 years of follow-up | 3,134,278 participants with 16,129 incident cases of thyroid cancer | Increasing number of times associated with an increasing risk of thyroid cancer; p for trend: <0.001 |
| Park et al. (2022) [8]; Korea | Low HDL-C; relative risk (RR) of thyroid cancer | Cohort with 6 years of follow-up | 4,658,473 participants with 47,325 incident cases of thyroid cancer | Male: RR = 1.27 (95%CI: 1.21–1.34) Female: RR = 1.19 (95%CI: 1.16–1.22) |
| Xu et al. (2021) [20], China | HDL-C; mean difference between groups | Case-control study | 372 patients with thyroid cancer and 651 controls with benign thyroid nodule | 1.32 mmol/L among cases vs. 1.39 mmol/L among controls; p for difference: 0.017 |
| Zhao et al. (2020) [21]; China | HDL-C; mean difference between groups | Case-control study | 2021 patients with thyroid cancer and 1727 patients with benign thyroid nodules | 1.28 mmol/L among cases vs. 1.34 mmol/L among controls; p for difference: 0.017 |
| Fussey et al. (2020) [10]; UK | Serum HDL-C; odds ratio (OR) of thyroid cancer | Cross-sectional study | 425 individuals with thyroid cancer and 310,176 controls | OR = 0.68 (95%CI: 0.45–1.00) per SD increase |
| Park et al. (2020) [11]; Korea | Low HDL-C; hazard ratio (HR) of thyroid cancer | Nationwide cohort with 7.2 years of follow-up | 9,890,917 participants with 77,133 incident cases of thyroid cancer | HR = 1.17 (95%CI: 1.15–1.19) |
| Revilla et al. (2019) [25]; Spain | Cholesterol; mean difference between groups | Cross-sectional study | 27 patients with benign thyroid tumor; 43 patients with low/intermediate thyroid cancer; 12 patients with high-risk thyroid cancer; and 7 patients with poorly differentiated and anaplastic thyroid carcinoma | No difference |
| Li et al. (2019) [24]; China | Total cholesterol; mean difference between groups | Case-control study | 1717 cases of thyroid cancer and 2158 healthy controls | Men: 1.02 mmol/L among cases vs. 1.02 mmol/L among controls; p for difference: 0.472 Women: 1.22 mmol/L among cases vs. 1.32 mmol/L among controls; p for difference: <0.001 |
| Kim et al. (2017) [13]; Korea | HDL-C <40 mg/dL in men or <50 mg/dL in women; difference in prevalence between groups | Cross-sectional study | 34,347 individuals including 155 individuals with prevalent thyroid cancer | p for difference: 0.135 |
| Balkan et al. (2014) [15]; Turkey | HDL-C; mean difference between groups | Case-control study | 41 cases with thyroid cancer and 41 age- and gender-matched controls | 52.4 mg/dL among cases vs. 51.6 mg/dL among controls; p for difference: >0.05 |
| Giusti et al. (2008) [18]; Italy | HDL-C; mean difference between groups | Case-control study | 106 cases with thyroid cancer and 87 controls | 1.71 mmol/L among cases vs. 2.04 mmol/L among controls; p for difference: 0.01 |
| Chrisoulidou et al. (2011) [22]; Greece | HDL-C; mean difference between groups | Case-control study | 16 women with thyroid cancer and 14 controls | 53 mg/dL among cases vs. 50 mg/dL among controls; p for difference: ns |
| LDL-C/HDL-C | ||||
| Li et al. (2019) [24]; China | LDL-C/HDL-C; mean difference between groups | Case-control study | 1717 cases of thyroid cancer and 2158 healthy controls | Men: 2.69 among cases vs. 2.65 among controls; p for difference: 0.671 Women: 2.22 among cases vs. 2.11 among controls; p for difference: 0.036 |
| ApoA-I | ||||
| Li et al. (2019) [24]; China | ApoA-I; mean difference between groups | Case-control study | 1717 cases of thyroid cancer and 2158 healthy controls | Men: 1.25 g/L among cases vs. 1.24 g/L among controls; p for difference: 0.475 Women: 1.38 g/L among cases vs. 1.42 g/L among controls; p for difference: 0.01 |
| ApoB | ||||
| Revilla et al. (2019) [25]; Spain | ApoB; mean difference between groups | Cross-sectional study | 27 patients with benign thyroid tumor; 43 patients with low/intermediate thyroid cancer; 12 patients with high-risk thyroid cancer; and 7 patients with poorly differentiated and anaplastic thyroid carcinoma | Lower level among patients with high-risk thyroid cancer (p for difference: <0.01) and patients with PDTC/ATC (p for difference: <0.05), compared to patients with BTT |
| Li et al. (2019) [24]; China | ApoB; mean difference between groups | Case-control study | 1717 cases of thyroid cancer and 2158 healthy controls | Men: 0.93 g/L among cases vs. 0.96 g/L among controls; p for difference: 0.021 Women: 0.89 g/L among cases vs. 0.89 g/L among controls; p for difference: 0.527 |
| ApoB/ApoA-1 | ||||
| Li et al. (2019) [24]; China | ApoB/ApoA-1; mean difference between groups | Case-control study | 1717 cases of thyroid cancer and 2158 healthy controls | Men: 0.76 among cases vs. 0.78 among controls; p for difference: 0.001 Women: 0.65 among cases vs. 0.64 among controls; p for difference: 0.242 |
| Characteristics | Male (N = 301,669) | Female (N = 259,719) |
|---|---|---|
| Age at first blood sampling, mean (SD) | 44.4 (13.2) | 45.8 (14.7) |
| Country of birth, N (%) | ||
| Sweden | 262,281 (86.9%) | 218,170 (84.0%) |
| Other Nordic countries | 16,025 (5.3%) | 19,851 (7.6%) |
| Other or unknown | 23,363 (7.7%) | 21,698 (8.4%) |
| Occupational status | ||
| Employed | 270,750 (89.8%) | 215,366 (82.9%) |
| Unemployed or unknown | 30,919 (10.2%) | 44,353 (17.1%) |
| Biomarkers of carbohydrate metabolism, mean (SD) | ||
| Glucose in mmol/L (N = 535,733) | 5.11 (1.38) | 4.85 (1.15) |
| Biomarkers of lipid metabolism, mean (SD) | ||
| TC in mmol/L (N = 556,849) | 5.60 (1.15) | 5.57 (1.18) |
| LDL-C in mmol/L (N = 229,824) | 3.75 (1.06) | 3.61 (1.14) |
| HDL-C in mmol/L (N = 229,434) | 1.38 (0.41) | 1.70 (0.43) |
| LDL-C/HDL-C ratio a (N = 229,140) | 1.46 (0.73) | 1.06 (0.66) |
| TG in mmol/L (N = 556,347) | 1.51 (1.16) | 1.12 (0.73) |
| Biomarkers of apolipoprotein metabolism, mean (SD) | ||
| ApoA-I in g/L (N = 202,661) | 1.36 (0.21) | 1.51 (0.24) |
| ApoB in g/L (N = 190,013) | 1.30 (0.36) | 1.20 (0.36) |
| ApoB/ApoA-I ratio a (N = 180,096) | −0.10 (0.46) | −0.37 (0.49) |
| Biomarker | Entire Cohort | Male | Female | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N of Cases | IR | HR (95%CI) a | N of Cases | IR | HR (95%CI) a | N of Cases | IR | HR (95%CI) a | |
| Carbohydrate metabolism | |||||||||
| Glucose | 596 | 5.4 | 1.05 (0.97–1.15) | 220 | 3.7 | 1.06 (0.94–1.19) | 376 | 7.3 | 1.04 (0.93–1.18) |
| Lipid metabolism | |||||||||
| TC | 623 | 5.4 | 0.91 (0.82–0.99) | 227 | 3.7 | 0.93 (0.80–1.08) | 396 | 7.4 | 0.90 (0.79–1.01) |
| LDL-C | 247 | 5.6 | 0.93 (0.81–1.07) | 87 | 3.4 | 0.84 (0.66–1.07) | 160 | 8.3 | 1.00 (0.84–1.19) |
| HDL-C | 245 | 5.5 | 0.86 (0.75–0.99) | 86 | 3.4 | 0.82 (0.64–1.03) | 159 | 8.3 | 0.89 (0.75–1.05) |
| LDL-C/HDL-C b | 245 | 5.5 | 1.03 (0.91–1.18) | 86 | 3.4 | 1.02 (0.84–1.25) | 159 | 8.3 | 1.06 (0.88–1.27) |
| TG b | 623 | 5.4 | 1.05 (0.96–1.14) | 227 | 3.7 | 1.04 (0.91–1.19) | 396 | 7.4 | 1.06 (0.94–1.19) |
| Apolipoprotein metabolism | |||||||||
| ApoA-I | 216 | 5.5 | 0.94 (0.81–1.08) | 77 | 3.4 | 0.91 (0.70–1.18) | 139 | 8.2 | 0.95 (0.80–1.13) |
| ApoB | 192 | 5.2 | 1.12 (0.96–1.30) | 71 | 3.4 | 1.14 (0.90–1.44) | 121 | 7.6 | 1.11 (0.91–1.35) |
| ApoB/ApoA-I b | 190 | 5.5 | 1.12 (0.96–1.31) | 70 | 3.5 | 1.13 (0.87–1.47) | 120 | 8.1 | 1.13 (0.93–1.37) |
| Biomarker | N of Cases | IR | HR (95%CI) a |
|---|---|---|---|
| High glucose (≥4.80 mmol/L) | |||
| No | 294 | 5.4 | 1.0 (ref) |
| Yes | 302 | 5.3 | 1.01 (0.86–1.20) |
| High TC (≥5.50 mmol/L) | |||
| No | 320 | 5.5 | 1.0 (ref) |
| Yes | 303 | 5.4 | 0.88 (0.74–1.04) |
| High LDL-C (≥3.60 mmol/L) | |||
| No | 131 | 5.7 | 1.0 (ref) |
| Yes | 116 | 5.4 | 0.93 (0.71–1.22) |
| High HDL-C (≥1.51 mmol/L) | |||
| No | 117 | 5.4 | 1.0 (ref) |
| Yes | 128 | 5.7 | 0.77 (0.59–1.01) |
| High LDL-C/HDL-C (≥2.41) | |||
| No | 135 | 5.8 | 1.0 (ref) |
| Yes | 110 | 5.2 | 1.08 (0.82–1.41) |
| High TG (≥1.10 mmol/L) | |||
| No | 331 | 5.6 | 1.0 (ref) |
| Yes | 292 | 5.3 | 1.04 (0.88–1.22) |
| High ApoA-I (≥1.41 g/L) | |||
| No | 107 | 5.3 | 1.0 (ref) |
| Yes | 109 | 5.6 | 0.82 (0.62–1.08) |
| High ApoB (≥1.21 g/L) | |||
| No | 100 | 5.3 | 1.0 (ref) |
| Yes | 92 | 5.2 | 1.06 (0.78–1.44) |
| High ApoB/ApoA-I (≥0.87) | |||
| No | 98 | 5.5 | 1.0 (ref) |
| Yes | 92 | 5.5 | 1.22 (0.90–1.66) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xiao, X.; Huang, Y.; Sadeghi, F.; Feychting, M.; Hammar, N.; Fang, F.; Zhang, Z.; Liu, Q. Carbohydrate, Lipid, and Apolipoprotein Biomarkers in Blood and Risk of Thyroid Cancer: Findings from the AMORIS Cohort. Cancers 2023, 15, 520. https://doi.org/10.3390/cancers15020520
Xiao X, Huang Y, Sadeghi F, Feychting M, Hammar N, Fang F, Zhang Z, Liu Q. Carbohydrate, Lipid, and Apolipoprotein Biomarkers in Blood and Risk of Thyroid Cancer: Findings from the AMORIS Cohort. Cancers. 2023; 15(2):520. https://doi.org/10.3390/cancers15020520
Chicago/Turabian StyleXiao, Xue, Yi Huang, Fetemeh Sadeghi, Maria Feychting, Niklas Hammar, Fang Fang, Zhe Zhang, and Qianwei Liu. 2023. "Carbohydrate, Lipid, and Apolipoprotein Biomarkers in Blood and Risk of Thyroid Cancer: Findings from the AMORIS Cohort" Cancers 15, no. 2: 520. https://doi.org/10.3390/cancers15020520
APA StyleXiao, X., Huang, Y., Sadeghi, F., Feychting, M., Hammar, N., Fang, F., Zhang, Z., & Liu, Q. (2023). Carbohydrate, Lipid, and Apolipoprotein Biomarkers in Blood and Risk of Thyroid Cancer: Findings from the AMORIS Cohort. Cancers, 15(2), 520. https://doi.org/10.3390/cancers15020520





