Leukemia Cutis—The Current View on Pathogenesis, Diagnosis, and Treatment
Simple Summary
Abstract
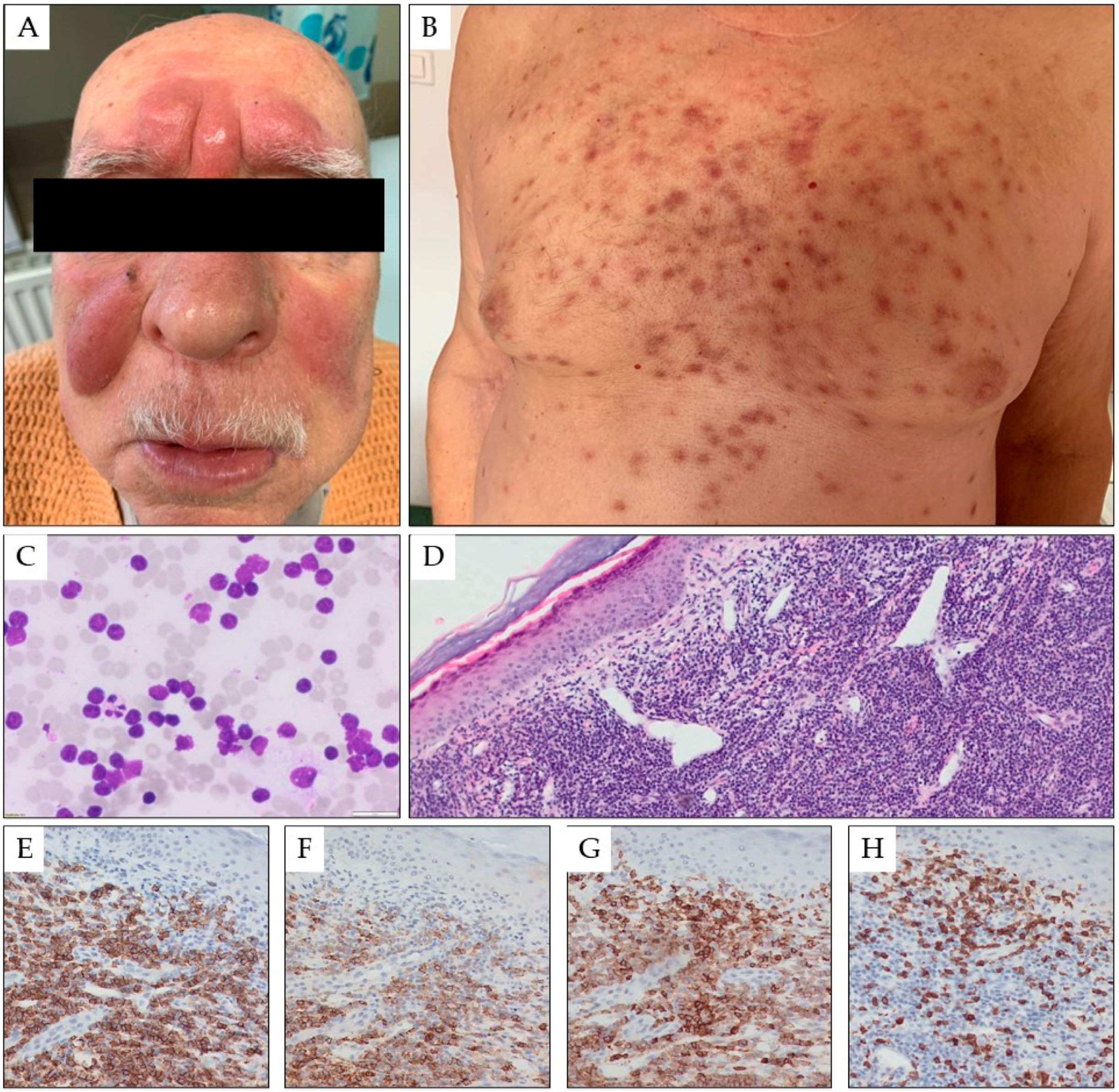
1. Introduction
2. Pathogenesis
3. Diagnosis
4. Prognosis
5. Treatment
6. Characteristics of Leukemia Cutis in Different Subtypes of Leukemia
6.1. Chronic Lymphocytic Leukemia
6.2. Hairy Cell Leukemia
6.3. T Cell Prolymphocytic Leukemia
6.4. Acute Lymphoblastic Leukemia
6.5. Acute Myeloid Leukemia
6.6. Chronic Neutrophilic Leukemia
6.7. Chronic Myelomonocytic Leukaemia
6.8. Chronic Myeloid Leukemia
7. Leukemia Cutis in Children
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Su, W.D.; Buechner, S.; Li, C.-Y. Clinicopathologic correlations in leukemia cutis. J. Am. Acad. Dermatol. 1984, 11, 121–128. [Google Scholar]
- Wagner, G.; Fenchel, K.; Back, W.; Schulz, A.; Sachse, M.M. Leukemia cutis—Epidemiology, clinical presentation, and differential diagnoses. J. Dtsch. Dermatol. Ges. 2012, 10, 27–36. [Google Scholar] [CrossRef]
- Yook, H.J.; Son, J.H.; Kim, Y.H.; Han, J.H.; Lee, J.H.; Park, Y.M.; Chung, N.G.; Kim, H.J.; Bang, C.H. Leukaemia Cutis: Clinical Features and Outcomes of 56 Patients. Acta Derm. Venereol. 2022, 102, adv00647. [Google Scholar] [CrossRef]
- Jang, K.A.; Chi, D.H.; Choi, J.H.; Sung, K.J.; Moon, K.C.; Koh, J.K. Leukemia cutis:a clinico-pathologic study of 23 patients. Korean J. Dermatol. 2000, 38, 15–22. [Google Scholar]
- Chang, Y.W.; Lee, C.H.; Tseng, H.C. Leukemia cutis in a medical center in southern Taiwan: A retrospective study of 42 patients. J. Formos. Med. Assoc. 2021, 120 Pt 1, 226–233. [Google Scholar] [CrossRef]
- Ratnam, K.V.; Khor, C.J.; Su, W.P. Leukemia cutis. Dermatol. Clin. 1994, 12, 419–431. [Google Scholar] [CrossRef] [PubMed]
- Cho-Vega, J.H.; Medeiros, L.J.; Prieto, V.G.; Vega, F. Leukemia cutis. Am. J. Clin. Pathol. 2008, 129, 130–142. [Google Scholar] [CrossRef]
- Parsi, M.; Go, M.S.; Ahmed, A. Leukemia Cutis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK541136/ (accessed on 16 February 2023).
- Zhang, I.H.; Zane, L.T.; Braun, B.S.; Maize, J., Jr.; Zoger, S.; Loh, M.L. Congenital leukemia cutis with subsequent development of leukemia. J. Am. Acad. Dermatol. 2006, 54 (Suppl. S2), S22–S27. [Google Scholar] [CrossRef] [PubMed]
- Monopoux, F.; Lacour, J.P.; Hatchuel, Y.; Hofman, P.; Raynaund, S.; Sudaka, I.; Ortonne, J.P.; Mariani, R. Congenital leukemia cutis preceeding monoblastic leukaemia by 3 months. Pediatr. Dermatol. 1996, 13, 472–476. [Google Scholar] [CrossRef]
- Resnik, K.S.; Brod, B.B. Leukemia cutis in congenital leukemia: Analysis and review of the world literature with report of an additional case. Arch. Dermatol. 1993, 129, 1301–1306. [Google Scholar] [CrossRef]
- Kaddu, S.; Zenahlik, P.; Beham-Schmid, C.; Kerl, H.; Cerroni, L. Specific cutaneous infiltrates in patients with myelogenous leukemia: A clinicopathologic study of 26 patients with assessment of diagnostic criteria. J. Am. Acad. Dermatol. 1999, 40 Pt 1, 966–978. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.S.; Kim, H.S.; Park, H.J.; Lee, J.Y.; Kim, H.O.; Cho, B.K.; Park, Y.M. Clinical characteristics of 75 patients with leukemia cutis. J. Korean Med. Sci. 2013, 28, 614–619. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Leborans, L.; Victoria-Martinez, A.M.; Torregrosa-Calatayud, J.L.; Alegre de Miquel, V. Leukemia cutis: A report of 17 cases and a review of the literature. Actas Dermosifiliogr. 2016, 107, e65e69. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Wang, Y.; Lian, C.G.; Hu, N.; Jin, H.; Liu, Y. Clinical and pathological features of myeloid leukemia cutis. An. Bras. Dermatol. 2018, 93, 216–221. [Google Scholar] [CrossRef]
- Watson, K.M.; Mufti, G.; Salisbury, J.R.; du Vivier, A.W.; Creamer, D. Spectrum of clinical presentation, treatment and prognosis in a series of eight patients with leukaemia cutis. Clin. Exp. Dermatol. 2006, 31, 218–221. [Google Scholar] [CrossRef]
- Osmola, M.; Gierej, B.; Kłosowicz, A.; Waszczuk-Gajda, A.; Basak, G.W.; Jędrzejczak, W.W.; Jurczyszyn, A.; Ziarkiewicz-Wróblewska, B. Leukaemia cutis for clinicians, a literature review. Postepy Dermatol. Alergol. 2021, 38, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Li, A.W.; Yin, E.S.; Stahl, M.; Kim, T.K.; Panse, G.; Zeidan, A.M.; Leventhal, J.S. The skin as a window to the blood: Cutaneous manifestations of myeloid malignancies. Blood Rev. 2017, 31, 370–388. [Google Scholar] [CrossRef]
- Bakst, R.; Powers, A.; Yahalom, J. Diagnostic and therapeutic considerations for extramedullary leukemia. Curr. Oncol. Rep. 2020, 22, 75. [Google Scholar] [CrossRef]
- Tomasini, C.; Quaglino, P.; Novelli, M.; Fierro, M.T. “Aleukemic” granulomatous leukemia cutis. Am. J. Dermatopathol. 1998, 20, 417–421. [Google Scholar] [CrossRef]
- Haidari, W.; Strowd, L.C. Clinical characterization of leukemia cutis presentation. Cutis 2019, 104, 326–330. [Google Scholar]
- Seckin, D.; Senol, A.; Gurbuz, O.; Demirkesen, C. Leukemic vasculitis: An unusual manifestation of leukemia cutis. J. Am. Acad. Dermatol. 2009, 61, 519–521. [Google Scholar] [CrossRef]
- Mansoori, P.; Taheri, A.; O’Neill, S.S.; Sangueza, O.P. T-lymphoblastic leukemia/lymphoma with annular skin rash and epidermotropism. Am. J. Dermatopathol. 2018, 40, 676–678. [Google Scholar] [CrossRef]
- Cañueto, J.; Meseguer-Yebra, C.; Román-Curto, C.; Santos-Briz, A.; Fernández-López, E.; Fraile, C.; Unamuno, P. Leukemic vasculitis: A rare pattern of leukemia cutis. J. Cutan. Pathol. 2011, 38, 360–364. [Google Scholar] [CrossRef] [PubMed]
- Nohria, A.; Criscito, M.C.; Weston, G.K.; Kim, R.H.; Lo Sicco, K.I.; Femia, A.N.; Hejazi, E.Z.; Milam, E.C. Profound leukemia cutis in a patient with relapsed T-cell acute lymphoblastic leukemia. JAAD Case Rep. 2021, 18, 51–53. [Google Scholar] [CrossRef]
- Lee, J.I.; Park, H.J.; Oh, S.T.; Lee, J.Y.; Cho, B.K. A case of leukemia cutis at the site of a prior catheter insertion. Ann. Dermatol. 2009, 21, 193–196. [Google Scholar] [CrossRef] [PubMed]
- Obi, C.; Holler, P.; Pugliese, D.; Abraham, R.; Xu, X.; Sobanko, J.; Rosenbach, M.; Wanat, K.A. Leukemia labialis: A rare presentation of leukemia cutis limited to the lips. J. Am. Acad. Dermatol. 2012, 67, e146–e147. [Google Scholar] [CrossRef] [PubMed]
- Grunwald, M.R.; McDonnell, M.H.; Induru, R.; Gerber, J.M. Cutaneous manifestations in leukemia patients. Semin. Oncol. 2016, 43, 359–365. [Google Scholar] [CrossRef]
- Fadilah, S.A.; Alawiyah, A.A.; Amir, M.A.; Cheong, S.K. Leukaemia cutis presenting as leonine facies. Med. J. Malays. 2003, 58, 102–104. [Google Scholar]
- Souza, P.K.; Amorim, R.O.; Sousa, L.S.; Batista, M.D. Dermatological manifestations of hematologic neoplasms. Part I: Secondary specific skin lesions. An. Bras. Dermatol. 2023, 98, 5–12. [Google Scholar] [CrossRef]
- Wang, S.-M.; Park, S.-S.; Park, S.-H.; Kim, N.-Y.; Kang, D.W.; Na, H.-R.; Lee, J.W.; Han, S.; Lim, H.K. Pre-transplant depression decreased overall survival of patients receiving allogeneic hematopoietic stem cell transplantation: A nationwide cohort study. Sci. Rep. 2020, 10, 15265. [Google Scholar] [CrossRef]
- Massoud, C.M.; Trivedi, L.; Kappius, R.; Maize JCSr Elston, D.M.; Metcalf, J.S. Varicella zoster virus presenting as lower extremity ulcers and an atypical myeloid infiltrate. JAAD Case Rep. 2020, 7, 68–70. [Google Scholar] [CrossRef] [PubMed]
- Patel, L.M.; Maghari, A.; Schwartz, R.A.; Kapila, R.; Morgan, A.J.; Lambert, W.C. Myeloid leukemia cutis in the setting of myelodysplastic syndrome: A crucial dermatological diagnosis. Int. J. Dermatol. 2012, 51, 383–388. [Google Scholar] [CrossRef]
- Zweegman, S.; Vermeer, M.H.; Bekkink, M.W.; van der Valk, P.; Nanayakkara, P.; Ossenkoppele, G.J. Leukaemia cutis: Clinical features and treatment strategies. Haematologica 2002, 87, ECR13. [Google Scholar] [PubMed]
- Sambasivan, A.; Keely, K.; Mandel, K.; Johnston, D.L. Leukemia cutis: An unusual rash in a child. CMAJ 2010, 182, 171–173. [Google Scholar] [CrossRef]
- Wong, T.Y.; Suster, S.; Bouffard, D.; Flynn, S.D.; Johnson, R.A.; Barnhill, R.L.; Mihm, M.C. Histologic spectrum of cutaneous involvement in patients with myelogenous leukemia including the neutrophilic dermatoses. Int. J. Dermatol. 1995, 34, 323e9. [Google Scholar] [CrossRef]
- Paydaş, S.; Zorludemir, S. Leukaemia cutis and leukaemic vasculitis. Br. J. Dermatol. 2000, 143, 773–779. [Google Scholar] [CrossRef]
- Cerroni, L.; Zenahlik, P.; Höfler, G.; Kaddu, S.; Smolle, J.; Kerl, H. Specific cutaneous infiltrates of B-cell chronic lymphocytic leukemia: A clinicopathologic and prognostic study of 42 patients. Am. J. Surg. Pathol. 1996, 20, 1000–1010. [Google Scholar] [CrossRef]
- Rao, A.G.; Danturty, I. Leukemia cutis. Indian J. Dermatol. 2012, 57, 504. [Google Scholar] [CrossRef] [PubMed]
- Elsayad, K.; Oertel, M.; Haverkamp, U.; Eich, H.T. The effectiveness of radiotherapy for leukemia cutis. J. Cancer Res. Clin. Oncol. 2017, 143, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.H.; Tien, H.J.; Yu, Y.B.; Wu, Y.H.; Shueng, P.W.; Lu, Y.F.; Wang, S.-Y.; Wang, L.-Y. Simultaneous integrated boost with helical arc radiotherapy of total skin (HEARTS) to treat cutaneous manifestations of advanced, therapy-refractory cutaneous lymphoma and leukemia—Dosimetry comparison of different regimens and clinical application. Radiat. Oncol. 2019, 14, 17. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Eichhorst, B.; Robak, T.; Montserrat, E.; Ghia, P.; Niemann, C.U.; Kater, A.P.; Gregor, M.; Cymbalista, F.; Buske, C.; Hillmen, P.; et al. Chronic lymphocytic leukaemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2021, 32, 23–33. [Google Scholar] [CrossRef]
- Hallek, M.; Cheson, B.D.; Catovsky, D.; Caligaris-Cappio, F.; Dighiero, G.; Döhner, H.; Hillmen, P.; Keating, M.; Montserrat, E.; Chiorazzi, N.; et al. iwCLL guidelines for diagnosis, indications for treatment, response assessment, and supportive management of CLL. Blood 2018, 131, 2745–2760. [Google Scholar] [CrossRef]
- Robak, E.; Robak, T. Skin lesions in chronic lymphocytic leukemia. Leuk. Lymphoma 2007, 48, 855–865. [Google Scholar] [CrossRef] [PubMed]
- Raufi, A.; Alsharedi, M.; Khelfa, Y.; Griswold, D.C.; Lebowicz, Y. Leukemia cutis in a patient with chronic lymphocytic leukemia presenting as bilateral helical nodules. SAGE Open Med. Case Rep. 2016, 4, 2050313X16683624. [Google Scholar] [CrossRef] [PubMed]
- Pedreira-García, W.M.; Nieves, D.; Montesinos-Cartagena, M.; Cortés, C.A.; Cáceres-Perkins, W.; Rabelo-Cartagena, J. Leukemia cutis as the initial manifestation of chronic lymphocytic leukemia progression. Cureus 2022, 14, e33013. [Google Scholar] [CrossRef] [PubMed]
- Thiesen, I.; Wehkamp, U.; Brüggemann, M.; Ritgen, M.; Murga Penas, E.M.; Klapper, W.; Oschlies, I. Skin involvement by chronic lymphocytic leukaemia is frequently associated with unrelated neoplastic or inflammatory cutaneous disease and is not indicative of general disease progression. Br. J. Dermatol. 2019, 180, 227–228. [Google Scholar] [CrossRef]
- Fried, L.J.; Criscito, M.C.; Stevenson, M.L.; Pomeranz, M.K. Chronic lymphocytic leukemia and the skin: Implications for the dermatologist. Int. J. Dermatol. 2022, 61, 519–531. [Google Scholar] [CrossRef]
- Morozova, E.A.; Olisova, O.Y.; Nikitin, E.A. Cutaneous manifestations of B-cell chronic lymphocytic leukemia. Int. J. Hematol. 2020, 112, 459–465. [Google Scholar] [CrossRef]
- Cerroni, L.; Hofler, G.; Bck, B.; Wolf, P.; Maier, G.; Kerl, H. Specific cutaneous infiltrates of B-cell chronic lymphocytic leukemia (B-CLL) at sites typical for Borrelia burgdorferi infection. J. Cutan. Pathol. 2002, 29, 142–147. [Google Scholar] [CrossRef]
- Robak, E.; Robak, T.; Biernat, W.; Bartkowiak, J.; Krykowski, E. Successful treatment of leukaemia cutis with cladribine in a patient with B-cell chronic lymphocytic leukaemia. Br. J. Dermatol. 2002, 147, 775–780. [Google Scholar] [CrossRef]
- Greenwood, R.; Barker, D.J.; Tring, F.C.; Parapia, L.; Reid, M.; Scott, C.S.; Lauder, I. Clinical and immunohistological characterization of cutaneous lesions in chronic lymphocytic leukaemia. Br. J. Dermatol. 1985, 113, 447–453. [Google Scholar] [CrossRef] [PubMed]
- Ziemer, M.; Bornkessel, A.; Hahnfeld, S.; Weyers, W. “Specific” cutaneous infiltrate of B-cell chronic lymphocytic leukemia at the site of a florid herpes simplex infection. J. Cutan. Pathol. 2005, 32, 581–584. [Google Scholar] [CrossRef]
- Aberer, W.; Zonzits, E.; Soyer, H.P.; Kerl, H. Postzosterische spezifische Hautinfiltrate bei chronischer lymphatischer Leukämie [Post-zoster-specific skin infiltrates in chronic lymphatic leukemia]. Hautarzt Z. Dermatol. 1990, 41, 455–457. [Google Scholar]
- Aldapt, M.B.; Yassin, M. Leukemia cutis as an early presentation or relapsing manifestation of chronic lymphocytic leukemia (CLL). Acta Biomed. 2021, 92, e2021192. [Google Scholar]
- Colburn, D.E.; Welch, M.A.; Giles, F.J. Skin infiltration with chronic lymphocytic leukemia is consistent with a good prognosis. Hematology 2002, 7, 187–188. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kaddu, S.; Smolle, J.; Cerroni, L.; Kerl, H. Prognostic evaluation of specific cutaneous infiltrates in B-chronic lymphocytic leukemia. J. Cutan. Pathol. 1996, 23, 487–494. [Google Scholar] [CrossRef]
- Robak, P.; Robak, T. Immunotherapy combinations for chronic lymphocytic leukemia: Advantages and disadvantages. Expert Opin. Biol. Ther. 2023, 23, 21–35. [Google Scholar] [CrossRef]
- Robak, T.; Witkowska, M.; Smolewski, P. The role of Bruton’s kinase inhibitors in chronic lymphocytic leukemia: Current status and future directions. Cancers 2022, 14, 771. [Google Scholar] [CrossRef]
- Robak, E.; Jesionek-Kupnicka, D.; Stelmach, P.; Kupnicki, P.; Szataniak, M.; Robak, T. Leukemia cutis in accelerated chronic lymphocytic leukemia: Successful treatment with venetoclax and rituximab. Ann. Hematol. 2022, 101, 1387–1392. [Google Scholar] [CrossRef]
- Bakst, R.; Yahalom, J. Radiation therapy for leukemia cutis. Pract. Radiat. Oncol. 2011, 1, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Sainsbury, D.C.; Allison, K.P.; Muir, T. Electrochemotherapy treatment of a recalcitrant earlobe keloid scar with chronic lymphocytic leukaemia infiltration. J. Plast. Reconstr. Aesthet. Surg. 2010, 63, e733–e736. [Google Scholar] [CrossRef] [PubMed]
- Robak, T.; Matutes, E.; Catovsky, D.; Zinzani, P.L.; Buske, C. Hairy cell leukaemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2015, 26 (Suppl. S5), v100–v107. [Google Scholar] [CrossRef] [PubMed]
- Puła, A.; Robak, T. Hairy cell leukemia: A brief update on current knowledge and treatment prospects. Curr. Opin. Oncol. 2021, 33, 412–419. [Google Scholar] [CrossRef]
- Tiacci, E.; Schiavoni, G.; Forconi, F.; Santi, A.; Trentin, L.; Ambrosetti, A.; Cecchini, D.; Sozzi, E.; di Celle, P.F.; Di Bello, C.; et al. Simple genetic diagnosis of hairy cell leukemia by sensitive detection of the BRAF-V600E mutation. Blood 2012, 119, 192–195. [Google Scholar] [CrossRef]
- Robak, E.; Jesionek-Kupnicka, D.; Robak, T. Skin changes in hairy cell leukemia. Ann. Hematol. 2021, 100, 615–625. [Google Scholar] [CrossRef]
- Fino, P.; Fioramonti, P.; Onesti, M.G.; Passaretti, D.; Scuderi, N. Skin metastasis in patient with hairy cell leukemia: Case report and review of literature. In Vivo 2012, 26, 311–314. [Google Scholar]
- Yetgin, S.; Olcay, L.; Yenicesu, I.; Oner, A.F.; Cağlar, M. Relapse in hairy cell leukemia due to isolated nodular skin infiltration. Pediatr. Hematol. Oncol. 2001, 18, 415–417. [Google Scholar] [CrossRef]
- Colović, N.; Perunicić, M.; Jurisić, V.; Colović, M. Specific skin lesions in hairy cell leukemia at presentation: Case report and review of literature. Med. Oncol. 2010, 27, 559–561. [Google Scholar] [CrossRef]
- Arai, E.; Ikeda, S.; Itoh, S.; Katayama, I. Specific skin lesions as the presenting symptom of hairy cell leukemia. Am. J. Clin. Pathol. 1988, 90, 459–464. [Google Scholar] [CrossRef]
- Bilsland, D.; Shahriari, S.; Douglas, W.S.; Chaudhuri, A.K.; Todd, W.T. Transient leukaemia cutis in hairy-cell leukaemia. Clin. Exp. Dermatol. 1991, 16, 207–209. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, D.M.; Sun, N.C.J.; Mena, R.; Moss, R. Cutaneous lesions in hairy cell leukemia. Case report and review of the literature. Arch Dermatol. 1983, 119, 322–325. [Google Scholar] [CrossRef]
- Fressoldati, A.; Lamparelli, T.; Federico, M.; Annino, L.; Capnist, G.; Pagnucco, G.; Dini, E.; Resegotti, L.; Damasio, E.E.; Silingardi, V. Hairy cell leukemia: A clinical review based on 725 cases of the Italian Cooperative Group (ICGHCL). Leuk. Lymphoma 1994, 13, 307–316. [Google Scholar] [CrossRef]
- Finan, M.C.; Su, W.P.; Li, C.Y. Cutaneous findings in hairy cell leukemia. J. Am. Acad. Dermatol. 1998, 11 Pt 1, 788–797. [Google Scholar] [CrossRef] [PubMed]
- Ergene, U.; Ozbalcı, D.; Işisağ, A. Hairy cell leukemia and cutaneous involvement. Transfus. Apher. Sci. 2012, 46, 231–232. [Google Scholar] [CrossRef] [PubMed]
- Robak, T.; Robak, P. Refractory and relapsed hairy-cell leukemia (HCL): Casting light on promising experimental drugs in clinical trials. Expert Opin. Investig. Drugs 2023, 32, 311–324. [Google Scholar] [CrossRef]
- Catovsky, D.; Ralfkiaer, E.; Muller-Hermelink, H.K. T-cell prolymphocytic leukaemia. In Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues; Jaffe, E.S., Harris, N.L., Stein, H., Vardiman, J.W., Eds.; World Health Organization Classification of Tumours: Lyon, France; IARC Press: Geneva, Switzerland, 2001; pp. 195–198. [Google Scholar]
- Laribi, K.; Lemaire, P.; Sandrini, J.; de Materre, A.B. Advances in the understanding and management of T-cell prolymphocytic leukemia. Oncotarget 2017, 8, 104664–104686. [Google Scholar] [CrossRef]
- Jain, P.; Aoki, E.; Keating, M.; Wierda, W.G.; O’Brien, S.; Gonzalez, G.N.; Ferrajoli, A.; Jain, N.; Thompson, P.A.; Jabbour, E.; et al. Characteristics, outcomes, prognostic factors and treatment of patients with T-cell prolymphocytic leukemia (T-PLL). Ann. Oncol. 2017, 28, 1554–1559. [Google Scholar] [CrossRef]
- Serra, A.; Estrach, M.T.; Martí, R.; Villamor, N.; Rafel, M.; Montserrat, E. Cutaneous involvement as the first manifestation in a case of T-cell prolymphocytic leukaemia. Acta Derm. Venereol. 1998, 78, 198–200. [Google Scholar]
- Wasifuddin, M.; Sabzposh, H.; Sun, L.; Wu, R.; Wang, J.C. Recurrence of T-cell prolymphocytic leukemia with a rare presentation as diffuse generalized skin lesion. J. Investig. Med. High Impact. Case Rep. 2023, 11, 23247096231176223. [Google Scholar] [CrossRef]
- Ventre, M.O.; Bacelieri, R.E.; Lazarchick, J.; Pollack, R.B.; Metcalf, J.S. Cutaneous presentation of T-cell prolymphocytic leukemia. Cutis 2013, 91, 87–91. [Google Scholar]
- Dearden, C.E. T-cell prolymphocytic leukemia. Clin. Lymphoma Myeloma 2009, 9 (Suppl. S3), S239–S243. [Google Scholar] [CrossRef]
- Jeong, K.H.; Lew, B.L.; Sim, W.Y. Generalized leukaemia cutis from a small cell variant of T-cell prolymphocytic leukaemia presenting with exfoliative dermatitis. Acta Derm. Venereol. 2009, 89, 509–512. [Google Scholar] [CrossRef] [PubMed]
- Kaminska, E.C.; Yu, Z.; Kress, J.; Petronic-Rosic, V.; Soltani, K. Erythematous eruption with marked conjunctival injection—Quiz case. Diagnosis: Leukemia cutis with conjunctival involvement in the setting of T-cell prolymphocytic leukemia (T-PLL). Arch. Dermatol. 2012, 148, 1199. [Google Scholar] [CrossRef]
- Mallett, R.B.; Matutes, E.; Catovsky, D.; Maclennan, K.; Mortimer, P.S.; Holden, C.A. Cutaneous infiltration in T-cell prolymphocytic leukaemia. Br. J. Dermatol. 1995, 132, 263–266. [Google Scholar] [CrossRef] [PubMed]
- Magro, C.M.; Morrison, C.D.; Heerema, N.; Porcu, P.; Sroa, N.; Deng, A.C. T-cell prolymphocytic leukemia: An aggressiveT-cell malignancy with frequent cutaneous tropism. J. Am. Acad. Dermatol. 2006, 55, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Volk, J.R.; Kjeldsberg, C.R.; Eyre, H.J.; Marty, J. T-cell prolymphocytic leukemia. Clinical and immunology characterization. Cancer 1983, 52, 2049–2054. [Google Scholar] [CrossRef]
- Leckey, B.D., Jr.; Kheterpal, M.K.; Selim, M.A.; Al-Rohil, R.N. Cutaneous involvement by T-cell prolymphocytic leukemia presenting as livedoid vasculopathy. J. Cutan. Pathol. 2021, 48, 975–979. [Google Scholar] [CrossRef]
- Hsi, A.C.; Robirds, D.H.; Luo, J.; Kreisel, F.H.; Frater, J.L.; Nguyen, T.T. T-cell prolymphocytic leukemia frequently shows cutaneous involvement and is associated with gains of MYC, loss of ATM, and TCL1A rearrangement. Am. J. Surg. Pathol. 2014, 38, 1468–1483. [Google Scholar] [CrossRef]
- Shumilov, E.; Hasenkamp, J.; Szuszies, C.J.; Koch, R.; Wulf, G.G. Patterns of late relapse after allogeneic hematopoietic stem cell transplantation in patients with T-cell prolymphocytic leukemia. Acta Haematol. 2021, 144, 105–110. [Google Scholar] [CrossRef]
- Matutes, E.; Brito-Babapulle, V.; Swansbury, J.; Ellis, J.; Morilla, R.; Dearden, C.; Sempere, A.; Catovsky, D. Clinical and laboratory features of 78 cases of T-prolymphocytic leukemia. Blood 1991, 78, 3269–3274. [Google Scholar] [CrossRef] [PubMed]
- Paul, S.; Kantarjian, H.; Jabbour, E.J. Adult acute lymphoblastic leukemia. Mayo Clin. Proc. 2016, 91, 1645–1666. [Google Scholar] [CrossRef] [PubMed]
- Terwilliger, T.; Abdul-Hay, M. Acute lymphoblastic leukemia: A comprehensive review and 2017 update. Blood Cancer J. 2017, 7, e577. [Google Scholar] [CrossRef] [PubMed]
- Rafei, H.; Kantarjian, H.M.; Jabbour, E.J. Recent advances in the treatment of acute lymphoblastic leukemia. Leuk. Lymphoma 2019, 60, 2606–2621. [Google Scholar] [CrossRef] [PubMed]
- Jabbour, E.; O’Brien, S.; Konopleva, M.; Kantarjian, H. New insights into the pathophysiology and therapy of adult acute lymphoblastic leukemia. Cancer 2015, 121, 2517–2528. [Google Scholar] [CrossRef]
- Singh, S.; Taneja, N.; Kaul, S.; Arava, S.; Bhari, N. Aleukemic leukemia cutis mimicking urticaria pigmentosa in a patient of T-cell acute lymphoblastic leukemia. Indian J. Dermatol. Venereol. Leprol. 2020, 86, 105. [Google Scholar] [PubMed]
- Jiang, X.; Wang, W.; Zhang, M. Leukemia Cutis: An unusual presentation of acute lymphoblastic leukemia in a child. Indian J. Dermatol. 2015, 60, 636. [Google Scholar]
- Yin, Y.T.; Tseng, J.H.; Liu, Y.L.; Miser, J.S.; Chen, S.H. Neonatal acute lymphoblastic leukemia (MLL-AF9) with leukemia cutis. Pediatr. Neonatol. 2021, 62, 676–678. [Google Scholar] [CrossRef]
- Arora, P.; Sinha, N.; Malhotra, P.; Kumar, V.; Shastri, A.; Yadav, K. T-cell acute lymphoblastic leukemia with a rare chromosomal translocation presenting as leukemia cutis. Int. J. Dermatol. 2022, 61, e120–e123. [Google Scholar] [CrossRef]
- Obiozor, C.; Ganguly, S.; Fraga, G.R. Leukemia cutis with lymphoglandular bodies: A clue to acute lymphoblastic leukemia cutis. Dermatol. Online J. 2015, 21. [Google Scholar] [CrossRef]
- Afzal, A.; Mingola, P.; Farooque, U.; Shabih, S.; Thomas, C.A. B-cell acute lymphoblastic leukemia presenting as leukemia cutis: A case report. Cureus 2020, 12, e11032. [Google Scholar] [CrossRef]
- Ansell, L.H.; Mehta, J.; Cotliar, J. Recurrent aleukemic leukemia cutis in a patient with pre-B-cell acute lymphoblastic leukemia. J. Clin. Oncol. 2013, 31, e353–e355. [Google Scholar] [CrossRef] [PubMed]
- Campuzano-García, A.E.; Torres-Álvarez, B.; Castanedo-Cázares, J.P. Leukemia cutis in a patient with pre-B-cell acute lymphoblastic leukemia. JAAD Case Rep. 2015, 6, 364–367. [Google Scholar] [CrossRef][Green Version]
- Lee, E.; Park, H.J.; Cho, B.K.; Lee, J.Y.; Lee, S. Leukemia cutis as early relapse of T-cell acute lymphoblastic leukemia. Int. J. Dermatol. 2010, 49, 335–337. [Google Scholar] [CrossRef] [PubMed]
- Andriescu, E.C.; Coughlin, C.C.; Cheng, C.E.; Prajapati, V.H.; Huang, J.T.; Schmidt, B.A.; Degar, B.A.; Aplenc, R.; Pillai, V.; Yan, A.C.; et al. Pediatric leukemia cutis: A case series. Pediatr. Dermatol. 2019, 36, 658–663. [Google Scholar] [CrossRef] [PubMed]
- Najem, N.; Zadeh, V.B.; Badawi, M.; Kumar, R.; Al-Otaibi, S.; Al-Abdulrazzaq, A. Aleukemic leukemia cutis in a child preceding T-cell acute lymphoblastic leukemia. Pediatr. Dermatol. 2011, 28, 535–537. [Google Scholar] [CrossRef]
- Chao, S.C.; Lee, J.Y.; Tsao, C.J. Leukemia cutis in acute lymphocytic leukemia masquerading as viral exanthem. J. Dermatol. 1999, 26, 216–219. [Google Scholar] [CrossRef]
- Roberts, I.; Fordham, N.J.; Rao, A.; Bain, B.J. Neonatal leukaemia. Br. J. Haematol. 2018, 182, 170–184. [Google Scholar] [CrossRef]
- Zhang, B.; Wang, T. Leukemia cutis in T-cell acute lymphoblastic leukemia: A 3-year follow-up case report. Ann. Palliat. Med. 2023, 12, 200–204. [Google Scholar] [CrossRef]
- Schlegel, S.; Hamm, H.; Reichel, A.; Kneitz, H.; Ernestus, K.; Andres, O.; Wiegering, V.G.; Eyrich, M.; Wölfl, M.; Schlegel, P.-G. Neonatal acute lymphoblastic leukemia with t(9;11) translocation presenting as blueberry muffin baby: Successful treatment by ALL-bfm induction therapy, allogeneic stem cell transplantation from an unrelated donor, and PCR-MRD-guided post-transplant follow-up. Am. J. Case Rep. 2020, 21, e927153. [Google Scholar]
- Agis, H.; Weltermann, A.; Fonatsch, C.; Haas, O.; Mitterbauer, G.; Müllauer, L.; Schreiber, S.; Schwarzinger, I.; Juretzka, W.; Valent, P.; et al. A comparative study on demographic, haematological and cytogeentic findings and prognosis in acute myeloid leukaemia with or without leukemia cutis. Ann. Hematol. 2002, 81, 90–95. [Google Scholar] [CrossRef]
- Khieu, M.; Beauvais, A.; Matz, R.; Bersabe, A.; Brown, P.; Brown, A.; Fillman, E.; Hall, J. Aleukemic myeloid leukemia cutis with a kikuchi disease-like inflammatory pattern in myelodysplastic syndrome. South. Med. J. 2017, 110, 308–313. [Google Scholar] [CrossRef]
- Koizumi, H.; Kumakiri, M.; Ishizuka, M.; Ohkawara, A.; Okabe, S. Leukemia cutis in acute myelomonocytic leukemia: Infiltration to minor traumas and scars. J. Dermatol. 1991, 18, 281–285. [Google Scholar] [CrossRef]
- Kubonishi, I.; Seto, M.; Murata, N.; Kamioka, M.; Taguchi, H.; Miyoshi, I. Translocation (10;11) (p13;q13) and MLL rearrangement in a case of AML (M5a) with aggressive leukemia cutis. Cancer Genet. Cytogenet. 1998, 104 (Suppl. S1), 28–31. [Google Scholar] [CrossRef] [PubMed]
- Baer, M.R.; Barcos, M.; Farrell, H.; Raza, A.; Preisler, H.D. Acute myelogenous leukemia with leukemia cutis. Eighteen cases seen between 1969 and 1986. Cancer 1989, 63, 2192–2200. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.Y.; Wong, K.M.; Bosenberg, M.; McKee, P.H.; Haynes, H.A. Myelogenous leukemia cutis resembling stasis dermatitis. J. Am. Acad. Dermatol. 2003, 49, 128–129. [Google Scholar] [CrossRef]
- Wang, C.X.; Pusic, I.; Anadkat, M.J. Association of leukemia cutis with survival in acute myeloid leukemia. JAMA Dermatol. 2019, 155, 826–832. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Escanamé, M.; Zuriel, D.; Tee, S.I.; Fried, I.; Massone, C.; Cerroni, L. Cutaneous infiltrates of acute myelogenous leukemia simulating inflammatory dermatoses. Am. J. Dermatopathol. 2013, 35, 419–424. [Google Scholar] [CrossRef]
- Koc, Y.; Miller, K.B.; Schenkein, D.P.; Daoust, P.; Sprague, K.; Berkman, E. Extramedullary tumors of myeloid blasts in adults as a pattern of relapse following allogeneic bone marrow transplantation. Cancer 1999, 85, 608–615. [Google Scholar] [CrossRef]
- Mandal, A.P.; Das, R.; Sengupta, M.; Chatterjee, U. Leukemia cutis—A case of cutaneous manifestation of acute monoblastic leukemia. J. Cancer Res. Ther. 2023, 19, 826–828. [Google Scholar] [CrossRef]
- Aguilera, S.B.; Zarraga, M.; Rosen, L. Leukemia cutis in a patient with acute myelogenous leukemia: A case report and review of the literature. Cutis 2010, 85, 31–36. [Google Scholar]
- Hobbs, L.K.; Carr, P.C.; Gru, A.A.; Flowers, R.H. Case and review: Cutaneous involvement by chronic neutrophilic leukemia vs Sweet syndrome—A diagnostic dilemma. J. Cutan. Pathol. 2021, 48, 644–649. [Google Scholar] [CrossRef]
- Thomopoulos, T.P.; Symeonidis, A.; Kourakli, A.; Papageorgiou, S.G.; Pappa, V. Chronic neutrophilic leukemia: A comprehensive review of clinical characteristics, genetic landscape and management. Front. Oncol. 2022, 12, 891961. [Google Scholar] [CrossRef] [PubMed]
- Szuber, N.; Tefferi, A. Chronic neutrophilic leukemia: New science and new diagnostic criteria. Blood Cancer J. 2018, 8, 19. [Google Scholar] [CrossRef] [PubMed]
- Coombs, L.A. Chronic neutrophilic leukemia: A case report of a rare myeloproliferative neoplasm with a CSF3R mutation. J. Adv. Pract. Oncol. 2019, 10, 853–857. [Google Scholar]
- Maxson, J.E.; Gotlib, J.; Pollyea, D.A.; Fleischman, A.G.; Agarwal, A.; Eide, C.A.; Bottomly, D.; Wilmot, B.; McWeeney, S.K.; Tognon, C.E.; et al. OhOncogenic CSF3R mutations in chronic neutrophilic leukemia and atypical CML. N. Engl. J. Med. 2013, 368, 1781–1790. [Google Scholar] [CrossRef]
- Kwon, O.; Park, J.; Chung, H.; Park, K.D. Leukemia cutis in chronic neutrophilic leukemia associated with colony stimulating Factor 3 receptor mutation: Clinical severity paralleled with hematologic abnormality. Ann. Dermatol. 2019, 31, 673–677. [Google Scholar] [CrossRef]
- Zhou, Y.; Duan, R.; Yao, J.; Qin, M.; Deng, J.; Xu, Z.; Wu, R. Skin Rash as the First Manifestation of Pediatric Chronic Neutrophilic Leukemia. J. Rare Dis. 2022, 1, 413–419. [Google Scholar]
- Castanet, J.; Lacour, J.P.; Garnier, G.; Perrin, C.; Taillan, B.; Fuzibet, J.G.; Ortonne, J.P. Neutrophilic dermatosis associated with chronic neutrophilic leukemia. J. Am. Acad. Dermatol. 1993, 29, 290–292. [Google Scholar] [CrossRef]
- Zhou, Y.B.; Yao, J.F.; Xu, Z.G.; Wu, R.H. Case report: Leukemia cutis as the first manifestation of chronic neutrophilic leukemia in a 6-year-old girl. Front. Pediatr. 2022, 10, 972224. [Google Scholar] [CrossRef] [PubMed]
- Willard, R.J.; Turiansky, G.W.; Genest, G.P.; Davis, B.J.; Diehl, L.F. Leukemia cutis in a patient with chronic neutrophilic leukemia. J. Am. Acad. Dermatol. 2001, 44, 365–369. [Google Scholar] [CrossRef]
- Patnaik, M.M.; Tefferi, A. Chronic myelomonocytic leukemia: 2022 update on diagnosis, risk stratification, and management. Am. J. Hematol. 2022, 97, 352–372. [Google Scholar] [CrossRef]
- Qiao, Y.; Jian, J.; Deng, L.; Tian, H.; Liu, B. Leukaemia cutis as a specific skin involvement in chronic myelomonocytic leukaemia and review of the literature: Acknowledgments. Transl. Cancer Res. 2020, 9, 4988–4998. [Google Scholar] [CrossRef]
- Cronin, D.M.; George, T.I.; Sundram, U.N. An updated approach to the diagnosis of myeloid leukemia cutis. Am. J. Clin. Pathol. 2009, 132, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Vitte, F.; Fabiani, B.; Bénet, C.; Dalac, S.; Balme, B.; Delattre, C.; Vergier, B.; Beylot-Barry, M.; Vignon-Pennamen, D.; Ortonne, N.; et al. Specific skin lesions in chronic myelomonocytic leukemia: A spectrum of myelomonocytic and dendritic cell proliferations: A study of 42 cases. Am. J. Surg. Pathol. 2012, 36, 1302–1316. [Google Scholar] [CrossRef] [PubMed]
- Mathew, R.A.; Bennett, J.M.; Liu, J.J.; Komrokji, R.S.; Lancet, J.E.; Naghashpour, M.; Messina, J.L.; List, A.F.; Moscinski, L.C.; Zhang, L. Cutaneous manifestations in CMML: Indication of disease acceleration or transformation to AML and review of the literature. Leuk. Res. 2012, 36, 72–80. [Google Scholar] [CrossRef]
- Duguid, J.K.; Mackie, M.J.; McVerry, B.A. Skin infiltration associated with chronic myelomonocytic leukaemia. Br. J. Haematol. 1983, 53, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Eubanks, S.W.; Patterson, J.W. Subacute myelomonocytic leukemia—An unusual skin manifestation. J. Am. Acad. Dermatol. 1983, 9, 581–584. [Google Scholar] [CrossRef]
- Török, L.; Lueff, S.; Garay, G.; Tápai, M. Monocytic aleukemic leukemia cutis. J. Eur. Acad. Dermatol. Venereol. 1999, 13, 54–58. [Google Scholar] [CrossRef]
- Loghavi, S.; Curry, J.L.; Garcia-Manero, G.; Patel, K.P.; Xu, J.; Khoury, J.D.; Torres-Cabala, C.A.; Nagarajan, P.; Aung, P.P.; Gibson, B.R.; et al. Chronic myelomonocytic leukemia masquerading as cutaneous indeterminate dendritic cell tumor: Expanding the spectrum of skin lesions in chronic myelomonocytic leukemia. J. Cutan. Pathol. 2017, 44, 1075–1079. [Google Scholar] [CrossRef]
- Alfonso, A.; Montalban-Bravo, G.; Garcia-Manero, G. Current management of patients with chronic myelomonocytic leukemia. Curr. Opin. Oncol. 2017, 29, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Goldman, J.M.; Melo, J.V. Chronic myeloid leukemia—Advances in biology and new approaches to treatment. N. Engl. J. Med. 2003, 349, 1451–1464. [Google Scholar] [CrossRef]
- Tarantini, F.; Anelli, L.; Ingravallo, G.; Attolico, I.; Zagaria, A.; Russo Rossi, A.; Lospalluti, L.; Bufano, T.; Zanframundo, G.; Maiorano, E.; et al. Skin lesions in chronic myeloid leukemia patients during dasatinib treatment. Cancer Manag. Res. 2019, 11, 7991–7996. [Google Scholar] [CrossRef]
- Afroz, S.; Ayub, M.; Joshi, U.; Mahapatra, E.; Mba, B. Leukemia cutis: A rare presentation in chronic myeloid leukemia mas-querading as cellulitis. In Proceedings of the Hospital Medicine, Orlando, FL, USA, 8–11 April 2018; Abstract 431. Available online: https://shmabstracts.org/abstract/leukemia-cutis-a-rare-presentation-in-chronic-myeloid-leukemia-masquerading-as-cellulitis/ (accessed on 8 September 2023).
- Qi, J.; Zhang, F.; Liu, Y.; Yao, J.; Xu, Y.; He, H. Extramedullary blast crisis of chronic myelogenous leukemia with a skin lesion: A case report and literature review. Am. J. Dermatopathol. 2021, 43, 450–453. [Google Scholar] [CrossRef] [PubMed]
- Zelman, B.; Bode-Omoleye, O.; Muhlbauer, A.; Agidi, A.; Mafee, M.; Velankar, M.; Mirza, K.; Speiser, J.; Mudaliar, K. Chronic myeloid leukemia-leukemia cutis mimicking a neutrophilic panniculitis-like leukemia cutis: Report of a rare case. J. Cutan. Pathol. 2021, 48, 1277–1281. [Google Scholar] [CrossRef] [PubMed]
- Singhal, M.; Singh, S.; Kumar, R.; Raina, V. Extensive cutaneous manifestations: Presenting feature of chronic myelocytic leukemia in second blast crisis. Indian J. Dermatol. 2010, 55, 265–267. [Google Scholar] [CrossRef] [PubMed]
- Naher, S.; Hoque, M.M. Leukaemia cutis in a patient with chronic myeloid leukaemia with blast crisis. J. Med. 2023, 24, 65–66. [Google Scholar] [CrossRef]
- Joshi, K.; Panchal, H.; Parikh, S.; Modi, G.; Talele, A.; Anand, A.; Uparkar, U.; Joshi, N.; Khatawani, I. Aleukemic leukemia cutis presenting as a sole sign of relapsed paediatric acute lymphoblastic leukemia. Indian J. Hematol. Blood Transfus. 2016, 32 (Suppl. S1), 46–49. [Google Scholar] [CrossRef]
- Available online: https://www.leukaemiacare.org.uk/support-and-information/latest-from-leukaemia-care/blog/leukaemia-cutis/ (accessed on 27 April 2023).
- Torrelo, A.; Madero, L.; Mediero, I.G.; Bano, A.; Zambrano, A. Aleukemic congenital leukemia cutis. Pediatr. Dermatol. 2004, 21, 458–461. [Google Scholar] [CrossRef]
- Bacchetta, J.; Douvillez, B.; Warin, L.; Girard, S.; Pagès, M.P.; Rebaud, P.; Bertrand, Y. Leucémie aiguë néonatale et Blueberry Muffin syndrome: À propos d’un cas spontanément régressif [Blueberry Muffin Baby and spontaneous remission of neonatal leukaemia]. Arch. Pediatr. 2008, 15, 1315–1319. [Google Scholar] [CrossRef]
- Gru, A.A.; Coughlin, C.C.; Schapiro, M.L.; Lombardi, M.; Martin, A.; Bayliss, S.J.; Frater, J.; Dehner, L.P. Pediatric aleukemic leukemia cutis: Report of 3 cases and review of the literature. Am. J. Dermatopathol. 2015, 37, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Godínez-Chaparro, J.A.; Valencia-Herrera, A.M.; Duarte-Abdala, M.R.; Mena-Cedillos, C.A.; Toledo-Bahena, M.E. Leukemia cutis and other dermatological findings in pediatric patients with acute myeloid leukemia. Bol. Med. Hosp. Infant. Mex. 2021, 78, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Gouache, E.; Greze, V.; Strullu, M.; Saultier, P.; Fenneteau, O.; Gandemer, V.; Ragu, C.; Auvrignon, A.; Boutroux, H.; Lapillonne, H.; et al. Leukemia cutis in childhood acute myeloid leukemia: Epidemiological, clinical, biological, and prognostic characteristics of patients included in the ELAM02 study. Hemasphere 2018, 2, e141. [Google Scholar] [CrossRef] [PubMed]
- Michel, G.; Boulad, F.; Small, T.N.; Black, P.; Heller, G.; Castro-Malaspina, H.; Childs, B.; Gillio, A.; Papadopoulos, E.; Young, J.; et al. Risk of extramedullary relapse following allogeneic bone marrow transplantation for acute myelogenous leukemia with leukemia cutis. Bone Marrow Transplant. 1997, 20, 107–112. [Google Scholar] [CrossRef]
- Millot, F.; Robert, A.; Bertrand, Y.; Mechinaud, F.; Laureys, G.; Ferster, A.; Brock, P.; Rohrlich, P.; Mazingue, F.; Plantaz, D.; et al. Cutaneous involvement in children with acute lymphoblastic leukemia or lymphoblastic lymphoma. The Children’s Leukemia Cooperative Group of the European Organization of Research and Treatment of Cancer (EORTC). Pediatrics 1997, 100, 60–64. [Google Scholar] [CrossRef]
- Brown, P.; Pieters, R.; Biondi, A. How I treat infant leukemia. Blood 2019, 133, 205–214. [Google Scholar] [CrossRef]
- Górecki, M.; Kozioł, I.; Kopystecka, A.; Budzyńska, J.; Zawitkowska, J.; Lejman, M. Updates in KMT2A gene rearrangement in pediatric acute lymphoblastic leukemia. Biomedicines 2023, 11, 821. [Google Scholar] [CrossRef]



| Authors/Reference | No. of Patients | Clinical Characteristics | Time from Leukemia Diagnosis to LC Development | Survival from LC Diagnosis | |||||
|---|---|---|---|---|---|---|---|---|---|
| Total | AML | ALL | CML | CLL | Other | ||||
| Su et al., 1984 [1] | 42 | 20 | 3 | 3 | 16 | 0 | Multiple papules and nodules (60%), infiltrative plaques (26%), macules, nodules, ulcers | LC after systemic leukemia—23 mo. (55%), before—3 mo. (7%), concomitant 16 mo. (38%) | 10–60 mo. (range) |
| Yook et al., 2022 [3] | 56 | 40 | 8 | 3 | 2 | MDS-3 | Plaques (28%), papules (27%), patches (18%), nodules (16%) | 12.3 mo. (mean) | 5.4 mo. (mean) |
| Kaddu et al., 1999 [12] | 26 | 17 | 0 | 9 | 0 | 0 | Solitary or multiple reddish to violaceous papules, plaques, and nodules (17 pts.) generalized erythematous maculopapular eruption (9 pts.) | 0 to 13 mo. in AML pts. (range), 36–72 months (mean of 52.4 mo.) in CML pts. | AML 1–25 mo. (range), CML 3–17 mo. (range) |
| Chang et al., 2021 [5] | 42 | 24 | 3 | 1 | 1 | MDS-8, ALL-5 | Papules (38%), nodules (29%), plaques (16%), ulcers (10%) | 16.3 mo. (mean) | 7.2 mo. (median) |
| Kang et al., 2013 [13] | 75 | 49 | 18 | 7 | 0 | MDS-1 | Nodules (33%), papules (30%), and plaques (17%) | 16.2 mo. (mean) in 58 pts. after systemic leukemia diagnosis, 2.3 mo. (mean) in 4 pts. LC before systemic leukemia diagnosis, 13 pts. concurrent diagnosis with systemic leukemia | 8.3 mo. (median) |
| Martinez-Leborans et al., 2016 [14] | 17 | 12 | 0 | 4 | 1 | 0 | Nodules (7 pts.), papules (5 pts.), erythematous-violaceous plaques (4 pts.) | aleukemic LC—5 pts. | 7 pts. died during the first year |
| Li et al., 2018 [15] | 10 | 9 | 0 | 0 | 0 | CMML-1 | Generalized papules or nodules (5 pts), localized masses (5 pts). | 4–72 mo. in 7 pts. after systemic leukemia diagnosis | 6 pts. died within 2–12 mo. |
| Watson et al., 2006 [16] | 8 | 5 | 0 | 2 | 1 | 0 | Erythematous papules (75%), nodules and plaques | 2–114 mo. (range); 2 pts. at presentation | 14 mo. (median) and 3–39 mo. (range) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Robak, E.; Braun, M.; Robak, T. Leukemia Cutis—The Current View on Pathogenesis, Diagnosis, and Treatment. Cancers 2023, 15, 5393. https://doi.org/10.3390/cancers15225393
Robak E, Braun M, Robak T. Leukemia Cutis—The Current View on Pathogenesis, Diagnosis, and Treatment. Cancers. 2023; 15(22):5393. https://doi.org/10.3390/cancers15225393
Chicago/Turabian StyleRobak, Ewa, Marcin Braun, and Tadeusz Robak. 2023. "Leukemia Cutis—The Current View on Pathogenesis, Diagnosis, and Treatment" Cancers 15, no. 22: 5393. https://doi.org/10.3390/cancers15225393
APA StyleRobak, E., Braun, M., & Robak, T. (2023). Leukemia Cutis—The Current View on Pathogenesis, Diagnosis, and Treatment. Cancers, 15(22), 5393. https://doi.org/10.3390/cancers15225393







