Immune Checkpoint Inhibitors and the Kidney: A Focus on Diagnosis and Management for Personalised Medicine
Abstract
:Simple Summary
Abstract
1. Introduction
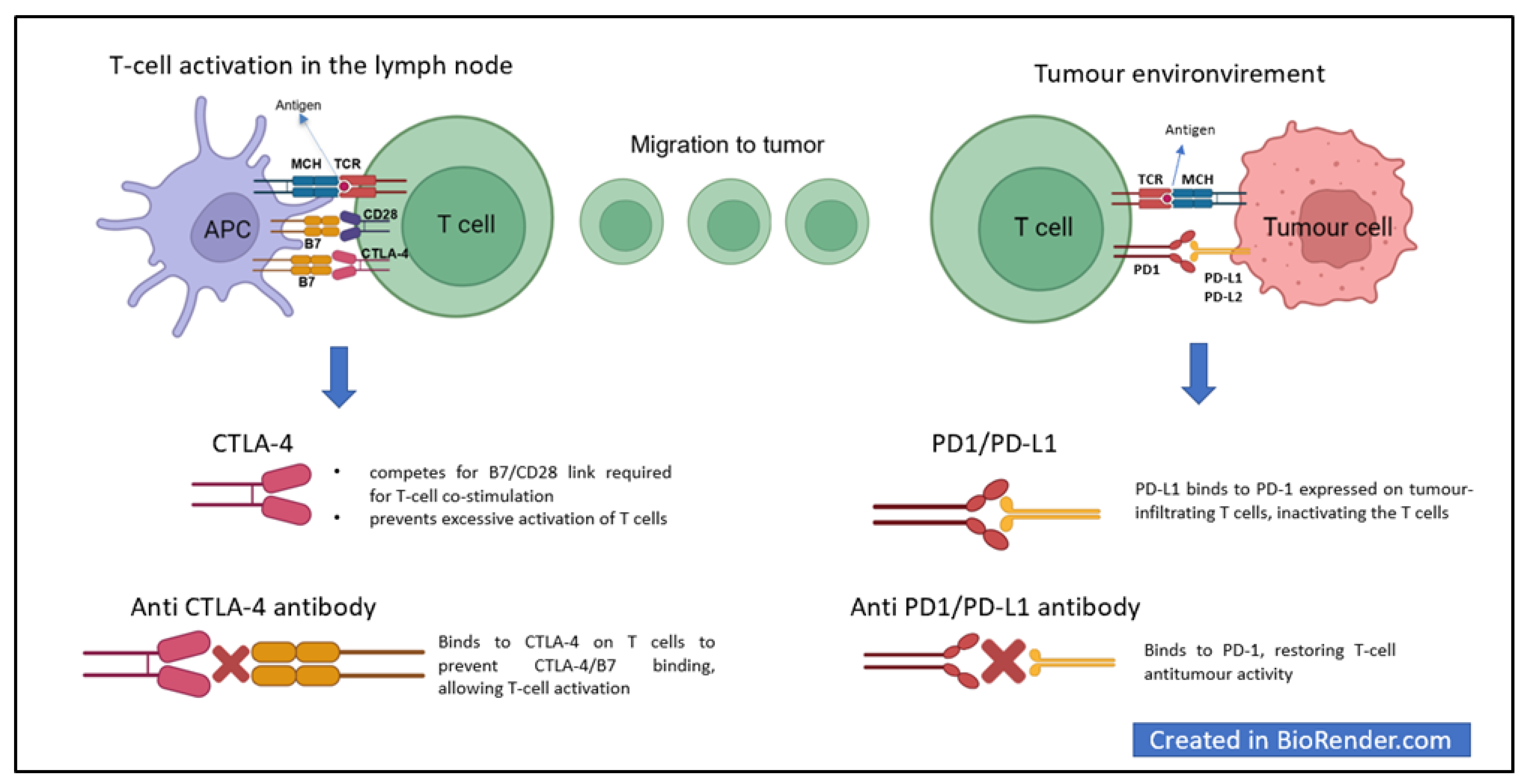
2. Immune Checkpoints and Cancer
3. ICI
4. Immune-Related Adverse Events
5. Immune-Related Renal Adverse Events
6. Mechanisms of Kidney Damage from Immune Checkpoint Inhibitors
7. Clinical and Instrumental Exams Used in Clinical Practice to Aid in Diagnosis
8. Indications for Kidney Biopsy, ICI Discontinuation, and the Start of Immunosuppressive Therapies
9. Recovery from ICI-Mediated irAEs
10. ICIs in Patients with Chronic Kidney Disease and Renal Replacement Therapy
11. ICIs in Patients with Pre-existent Autoimmune Glomerulonephritis
12. Suggested Nephrology–Oncology Approach
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Janeway, C. Immunobiology: The Immune System in Health and Disease, 6th ed.; Garland Science: New York, NY, USA, 2005; Volume xxiii, 823p. [Google Scholar]
- Boudreau, J.E.; Bonehill, A.; Thielemans, K.; Wan, Y. Engineering dendritic cells to enhance cancer immunotherapy. Mol. Ther. 2011, 19, 841–853. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vesely, M.D.; Schreiber, R.D. Cancer immunoediting: Antigens, mechanisms, and implications to cancer immunotherapy. Ann. N. Y. Acad. Sci. 2013, 1284, 1–5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adachi, K.; Tamada, K. Immune checkpoint blockade opens an avenue of cancer immunotherapy with a potent clinical efficacy. Cancer Sci. 2015, 106, 945–950. [Google Scholar] [CrossRef] [Green Version]
- Vesely, M.D.; Kershaw, M.H.; Schreiber, R.D.; Smyth, M.J. Natural innate and adaptive immunity to cancer. Annu. Rev. Immunol. 2011, 29, 235–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drake, C.G.; Jaffee, E.; Pardoll, D.M. Mechanisms of immune evasion by tumors. Adv Immunol. 2006, 90, 51–81. [Google Scholar] [PubMed]
- Martins, F.; Sofiya, L.; Sykiotis, G.P.; Lamine, F.; Maillard, M.; Fraga, M.; Shabafrouz, K.; Ribi, C.; Cairoli, A.; Guex-Crosier, Y.; et al. Adverse effects of immune-checkpoint inhibitors: Epidemiology, management and surveillance. Nat. Rev. Clin. Oncol. 2019, 16, 563–580. [Google Scholar] [CrossRef] [PubMed]
- Martin, K.; Schreiner, J.; Zippelius, A. Modulation of APC Function and Anti-Tumor Immunity by Anti-Cancer Drugs. Front. Immunol. 2015, 6, 501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsushita, H.; Vesely, M.D.; Koboldt, D.C.; Rickert, C.G.; Uppaluri, R.; Magrini, V.J.; Arthur, C.D.; White, J.M.; Chen, Y.S.; Shea, L.K.; et al. Cancer exome analysis reveals a T-cell-dependent mechanism of cancer immunoediting. Nature 2012, 482, 400–404. [Google Scholar] [CrossRef] [Green Version]
- Waldman, A.D.; Fritz, J.M.; Lenardo, M.J. A guide to cancer immunotherapy: From T cell basic science to clinical practice. Nat. Rev. Immunol. 2020, 20, 651–668. [Google Scholar] [CrossRef]
- Sprangers, B.; Leaf, D.E.; Porta, C.; Soler, M.J.; Perazella, M.A. Diagnosis and management of immune checkpoint inhibitor-associated acute kidney injury. Nat. Rev. Nephrol. 2022, 18, 794–805. [Google Scholar] [CrossRef]
- Leach, D.R.; Krummel, M.F.; Allison, J.P. Enhancement of antitumor immunity by CTLA-4 blockade. Science 1996, 271, 1734–1736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pardoll, D.M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer 2012, 12, 252–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hodi, F.S.; O’Day, S.J.; McDermott, D.F.; Weber, R.W.; Sosman, J.A.; Haanen, J.B.; Gonzalez, R.; Robert, C.; Schadendorf, D.; Hassel, J.C.; et al. Improved survival with ipilimumab in patients with metastatic melanoma. N. Engl. J. Med. 2010, 363, 711–723. [Google Scholar] [CrossRef]
- Peggs, K.S.; Quezada, S.A.; Chambers, C.A.; Korman, A.J.; Allison, J.P. Blockade of CTLA-4 on both effector and regulatory T cell compartments contributes to the antitumor activity of anti-CTLA-4 antibodies. J. Exp. Med. 2009, 206, 1717–1725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Helissey, C.; Vicier, C.; Champiat, S. The development of immunotherapy in older adults: New treatments, new toxicities? J. Geriatr. Oncol. 2016, 7, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Postow, M.A.; Sidlow, R.; Hellmann, M.D. Immune-Related Adverse Events Associated with Immune Checkpoint Blockade. N. Engl. J. Med. 2018, 378, 158–168. [Google Scholar] [CrossRef] [PubMed]
- Esfahani, K.; Elkrief, A.; Calabrese, C.; Lapointe, R.; Hudson, M.; Routy, B.; Miller, W.H., Jr.; Calabrese, L. Moving towards personalized treatments of immune-related adverse events. Nat. Rev. Clin. Oncol. 2020, 17, 504–515. [Google Scholar] [CrossRef] [PubMed]
- Perazella, M.A.; Shirali, A.C. Immune checkpoint inhibitor nephrotoxicity: What do we know and what should we do? Kidney Int. 2020, 97, 62–74. [Google Scholar] [CrossRef]
- Song, P.; Zhang, D.; Cui, X.; Zhang, L. Meta-analysis of immune-related adverse events of immune checkpoint inhibitor therapy in cancer patients. Thorac. Cancer 2020, 11, 2406–2430. [Google Scholar] [CrossRef]
- Nigro, O.; Pinotti, G.; De Galitiis, F.; Di Pietro, F.R.; Giusti, R.; Filetti, M.; Bersanelli, M.; Lazzarin, A.; Bordi, P.; Catino, A.; et al. Late immune-related adverse events in long-term responders to PD-1/PD-L1 checkpoint inhibitors: A multicentre study. Eur. J. Cancer 2020, 134, 19–28. [Google Scholar] [CrossRef]
- Wanchoo, R.; Karam, S.; Uppal, N.N.; Barta, V.S.; Deray, G.; Devoe, C.; Launay-Vacher, V.; Jhaveri, K.D.; on behalf of Cancer and Kidney International Network Workgroup on Immune Checkpoint Inhibitors. Adverse Renal Effects of Immune Checkpoint Inhibitors: A Narrative Review. Am. J. Nephrol. 2017, 45, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Perazella, M.A. Checkmate: Kidney injury associated with targeted cancer immunotherapy. Kidney Int. 2016, 90, 474–476. [Google Scholar] [CrossRef] [PubMed]
- Seethapathy, H.; Zhao, S.; Strohbehn, I.A.; Lee, M.; Chute, D.F.; Bates, H.; Molina, G.E.; Zubiri, L.; Gupta, S.; Motwani, S.; et al. Incidence and Clinical Features of Immune-Related Acute Kidney Injury in Patients Receiving Programmed Cell Death Ligand-1 Inhibitors. Kidney Int. Rep. 2020, 5, 1700–1705. [Google Scholar] [CrossRef] [PubMed]
- Sorah, J.D.; Rose, T.L.; Radhakrishna, R.; Derebail, V.K.; Milowsky, M.I. Incidence and Prediction of Immune Checkpoint Inhibitor-related Nephrotoxicity. J. Immunother. 2021, 44, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Seethapathy, H.; Zhao, S.; Chute, D.F.; Zubiri, L.; Oppong, Y.; Strohbehn, I.; Cortazar, F.B.; Leaf, D.E.; Mooradian, M.J.; Villani, A.-C.; et al. The Incidence, Causes, and Risk Factors of Acute Kidney Injury in Patients Receiving Immune Checkpoint Inhibitors. Clin. J. Am. Soc. Nephrol. 2019, 14, 1692–1700. [Google Scholar] [CrossRef]
- Meraz-Muñoz, A.; Amir, E.; Ng, P.; Avila-Casado, C.; Ragobar, C.; Chan, C.; Kim, J.; Wald, R.; Kitchlu, A. Acute kidney injury associated with immune checkpoint inhibitor therapy: Incidence, risk factors and outcomes. J. Immunother. Cancer 2020, 8, e000467. [Google Scholar] [CrossRef]
- García-Carro, C.; Bolufer, M.; Bury, R.; Castañeda, Z.; Muñoz, E.; Felip, E.; Lorente, D.; Carreras, M.J.; Gabaldon, A.; Agraz, I.; et al. Acute kidney injury as a risk factor for mortality in oncological patients receiving checkpoint inhibitors. Nephrol. Dial. Transplant. 2022, 37, 887–894. [Google Scholar] [CrossRef]
- Weber, J.S.; D’Angelo, S.P.; Minor, D.; Hodi, F.S.; Gutzmer, R.; Neyns, B.; Hoeller, C.; Khushalani, N.; Miller, W.H., Jr.; Lao, C.D.; et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): A randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015, 16, 375–384. [Google Scholar] [CrossRef]
- Oleas, D.; Bolufer, M.; Agraz, I.; Felip, E.; Munoz, E.; Gabaldon, A.; Bury, R.; Espinel, E.; Serón, D.; García-Carro, C.; et al. Acute interstitial nephritis associated with immune checkpoint inhibitors: A single-centre experience. Clin. Kidney J. 2021, 14, 1364–1370. [Google Scholar] [CrossRef] [Green Version]
- Kellum, J.A.; Lameire, N.; on behalf of the KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: A KDIGO summary (Part 1). Crit. Care 2013, 17, 204. [Google Scholar] [CrossRef] [Green Version]
- Gupta, S.; Cortazar, F.B.; Riella, L.V.; Leaf, D.E. Immune Checkpoint Inhibitor Nephrotoxicity: Update 2020. Kidney360 2020, 1, 130–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freites-Martinez, A.; Santana, N.; Arias-Santiago, S.; Viera, A. Using the Common Terminology Criteria for Adverse Events (CTCAE—Version 5.0) to Evaluate the Severity of Adverse Events of Anticancer Therapies. Actas Dermosifiliogr. (Engl. Ed.) 2021, 112, 90–92. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Valenzuela, L.; Draibe, J.; Fulladosa, X.; Gomà, M.; Gómez, F.; Antón, P.; Cruzado, J.; Torras, J. Acute Tubulointerstitial Nephritis in Clinical Oncology: A Comprehensive Review. Int. J. Mol. Sci. 2021, 22, 2326. [Google Scholar] [CrossRef] [PubMed]
- Manohar, S.; Ghamrawi, R.; Chengappa, M.; Goksu, B.N.B.; Kottschade, L.; Finnes, H.; Dronca, R.; Leventakos, K.; Herrmann, J.; Herrman, S. Acute Interstitial Nephritis and Checkpoint Inhibitor Therapy: Single Center Experience of Management and Drug Rechallenge. Kidney360 2020, 1, 16–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, S.; Short, S.A.P.; Sise, M.E.; Prosek, J.M.; Madhavan, S.M.; Soler, M.J.; Ostermann, M.; Herrmann, S.M.; Abudayyeh, A.; Anand, S.; et al. Acute kidney injury in patients treated with immune checkpoint inhibitors. J. Immunother. Cancer 2021, 9, e003467. [Google Scholar] [CrossRef]
- Kitchlu, A.; Jhaveri, K.D.; Wadhwani, S.; Deshpande, P.; Harel, Z.; Kishibe, T.; Henriksen, K.; Wanchoo, R. A Systematic Review of Immune Checkpoint Inhibitor-Associated Glomerular Disease. Kidney Int. Rep. 2021, 6, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Izzedine, H.; Mathian, A.; Albiges, L.; Champiat, S.; Brocheriou, I. Association of thrombotic microangiopathy with atezolizumab therapy in cancer patients. Eur. J. Cancer 2021, 149, 34–36. [Google Scholar] [CrossRef]
- Badra, S.; Ruchi, R.; Zeng, X.; Gordan, L.; Shah, C.V. Immune checkpoint inhibitor associated renally limited thrombotic microangiopathy—A clinical dilemma. Eur. J. Cancer 2022, 169, 126–130. [Google Scholar] [CrossRef]
- Gallan, A.J.; Alexander, E.; Reid, P.; Kutuby, F.; Chang, A.; Henriksen, K.J. Renal Vasculitis and Pauci-immune Glomerulonephritis Associated With Immune Checkpoint Inhibitors. Am. J. Kidney Dis. 2019, 74, 853–856. [Google Scholar] [CrossRef]
- Sise, M.E.; Seethapathy, H.; Reynolds, K.L. Diagnosis and Management of Immune Checkpoint Inhibitor-Associated Renal Toxicity: Illustrative Case and Review. Oncologist 2019, 24, 735–742. [Google Scholar] [CrossRef] [Green Version]
- Cortazar, F.B.; Marrone, K.A.; Troxell, M.L.; Ralto, K.M.; Hoenig, M.P.; Brahmer, J.R.; Le, D.T.; Lipson, E.J.; Glezerman, I.G.; Wolchok, J.; et al. Clinicopathological features of acute kidney injury associated with immune checkpoint inhibitors. Kidney Int. 2016, 90, 638–647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tian, R.; Liang, J.; Li, R.; Zhou, X. Acute Kidney Injury Induced by Immune Checkpoint Inhibitors. Kidney Dis. 2022, 8, 190–201. [Google Scholar] [CrossRef] [PubMed]
- Cortazar, F.B.; Kibbelaar, Z.A.; Glezerman, I.G.; Abudayyeh, A.; Mamlouk, O.; Motwani, S.S.; Murakami, N.; Herrmann, S.M.; Manohar, S.; Shirali, A.C.; et al. Clinical Features and Outcomes of Immune Checkpoint Inhibitor-Associated AKI: A Multicenter Study. J. Am. Soc. Nephrol. 2020, 31, 435–446. [Google Scholar] [CrossRef] [PubMed]
- Hultin, S.; Nahar, K.; Menzies, A.M.; Long, G.V.; Fernando, S.L.; Atkinson, V.; Cebon, J.; Wong, M.G. Histological diagnosis of immune checkpoint inhibitor induced acute renal injury in patients with metastatic melanoma: A retrospective case series report. BMC Nephrol. 2020, 21, 391. [Google Scholar] [CrossRef] [PubMed]
- Mamlouk, O.; Selamet, U.; Machado, S.; Abdelrahim, M.; Glass, W.F.; Tchakarov, A.; Gaber, L.; Lahoti, A.; Workeneh, B.; Chen, S.; et al. Nephrotoxicity of immune checkpoint inhibitors beyond tubulointerstitial nephritis: Single-center experience. J. Immunother. Cancer 2019, 7, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seethapathy, H.; Rusibamayila, N.; Chute, D.F.; Lee, M.; Strohbehn, I.; Zubiri, L.; Faje, A.T.; Reynolds, K.L.; Jhaveri, K.D.; Sise, M.E. Hyponatremia and other electrolyte abnormalities in patients receiving immune checkpoint inhibitors. Nephrol. Dial. Transplant. 2021, 36, 2241–2247. [Google Scholar] [CrossRef]
- Tinawi, M.; Bastani, B. Nephrotoxicity of Immune Checkpoint Inhibitors: Acute Kidney Injury and Beyond. Cureus 2020, 12, e12204. [Google Scholar] [CrossRef]
- Herrmann, S.M.; Perazella, M.A. Immune Checkpoint Inhibitors and Immune-Related Adverse Renal Events. Kidney Int. Rep. 2020, 5, 1139–1148. [Google Scholar] [CrossRef]
- Paschou, S.A.; Kassi, E.; Psaltopoulou, T. Hyponatraemia in patients on immune checkpoint inhibitors. Ther. Adv. Endocrinol. Metab. 2022, 13, 20420188221136755. [Google Scholar] [CrossRef]
- Cui, K.; Wang, Z.; Zhang, Q.; Zhang, X. Immune checkpoint inhibitors and adrenal insufficiency: A large-sample case series study. Ann. Transl. Med. 2022, 10, 251. [Google Scholar] [CrossRef]
- du Payrat, J.A.; Cugnet-Anceau, C.; Maillet, D.; Levy, M.; Raverot, G.; Disse, E.; Borson-Chazot, F. Checkpoint inhibitors-induced hypophysitis. Bull. Cancer 2020, 107, 490–498. [Google Scholar] [CrossRef]
- Ruggeri, R.M.; Campennì, A.; Giuffrida, G.; Trimboli, P.; Giovanella, L.; Trimarchi, F.; Cannavò, S. Endocrine and metabolic adverse effects of immune checkpoint inhibitors: An overview (what endocrinologists should know). J. Endocrinol. Investig. 2019, 42, 745–756. [Google Scholar] [CrossRef] [PubMed]
- Charmetant, X.; Teuma, C.; Lake, J.; Dijoud, F.; Frochot, V.; Deeb, A. A new expression of immune checkpoint inhibitors’ renal toxicity: When distal tubular acidosis precedes creatinine elevation. Clin. Kidney J. 2020, 13, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Franzin, R.; Netti, G.S.; Spadaccino, F.; Porta, C.; Gesualdo, L.; Stallone, G.; Castellano, G.; Ranieri, E. The Use of Immune Checkpoint Inhibitors in Oncology and the Occurrence of AKI: Where Do We Stand? Front. Immunol. 2020, 11, 574271. [Google Scholar] [CrossRef]
- Schneider, B.J.; Naidoo, J.; Santomasso, B.D.; Lacchetti, C.; Adkins, S.; Anadkat, M.; Atkins, M.B.; Brassil, K.J.; Caterino, J.M.; Chau, I.; et al. Management of Immune-Related Adverse Events in Patients Treated With Immune Checkpoint Inhibitor Therapy: ASCO Guideline Update. J. Clin. Oncol. 2021, 39, 4073–4126. [Google Scholar] [CrossRef]
- Thompson, J.A.; Schneider, B.J.; Brahmer, J.; Andrews, S.; Armand, P.; Bhatia, S.; Budde, L.E.; Costa, L.; Davies, M.; Dunnington, D.; et al. NCCN Guidelines Insights: Management of Immunotherapy-Related Toxicities, Version 1.2020. J. Natl. Compr. Cancer Netw. 2020, 18, 230–241. [Google Scholar] [CrossRef] [Green Version]
- Brahmer, J.R.; Abu-Sbeih, H.; Ascierto, P.A.; Brufsky, J.; Cappelli, L.C.; Cortazar, F.B.; Gerber, D.E.; Hamad, L.; Hansen, E.; Johnson, D.B.; et al. Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immune checkpoint inhibitor-related adverse events. J. Immunother. Cancer 2021, 9, e002435. [Google Scholar] [CrossRef]
- Haanen, J.; Obeid, M.; Spain, L.; Carbonnel, F.; Wang, Y.; Robert, C.; Lyon, A.; Wick, W.; Kostine, M.; Peters, S.; et al. Management of toxicities from immunotherapy: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2022, 33, 1217–1238. [Google Scholar] [CrossRef] [PubMed]
- Associazione Italiana Oncologia Medica. Gestione Della Tossicita’ da Immunoterapia 2021. Available online: https://www.aiom.it/linee-guida-aiom-2021-gestione-della-tossicita-da-immunoterapia/ (accessed on 23 January 2023).
- von Itzstein, M.S.; Khan, S.; Gerber, D.E. Investigational Biomarkers for Checkpoint Inhibitor Immune-Related Adverse Event Prediction and Diagnosis. Clin. Chem. 2020, 66, 779–793. [Google Scholar] [CrossRef] [PubMed]
- Moledina, D.G.; Wilson, F.P.; Pober, J.S.; Perazella, M.A.; Singh, N.; Luciano, R.L.; Obeid, W.; Lin, H.; Kuperman, M.; Moeckel, G.W.; et al. Urine TNF-alpha and IL-9 for clinical diagnosis of acute interstitial nephritis. JCI Insight 2019, 4, e127456. [Google Scholar] [CrossRef] [Green Version]
- Bhaumik, S.K.; Kher, V.; Arora, P.; Rai, P.K.; Singhal, M.; Gupta, A.; Pandey, R.; Sharma, R.K. Evaluation of clinical and histological prognostic markers in drug-induced acute interstitial nephritis. Ren. Fail. 1996, 18, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Qualls, D.; Seethapathy, H.; Bates, H.; Tajmir, S.; Heidari, P.; Endres, P.; Reynolds, K.; Lawrence, D.; Sise, M. Positron emission tomography as an adjuvant diagnostic test in the evaluation of checkpoint inhibitor-associated acute interstitial nephritis. J. Immunother. Cancer 2019, 7, 356. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Zhang, J.; Xu, L.; Yang, H.; Liang, N.; Zhang, L.; Zhang, F.; Zhang, X. Safety and Efficacy of the Rechallenge of Immune Checkpoint Inhibitors After Immune-Related Adverse Events in Patients With Cancer: A Systemic Review and Meta-Analysis. Front. Immunol. 2021, 12, 730320. [Google Scholar] [CrossRef] [PubMed]
- Mroue, A.; Moujaess, E.; Kourie, H.R.; Azar, H.; Finianos, S.; Chelala, D. Exploring the knowledge gap of immune checkpoint inhibitors in chronic renal failure: A systematic review of the literature. Crit. Rev. Oncol. Hematol. 2021, 157, 103169. [Google Scholar] [CrossRef] [PubMed]
- Vitale, M.G.; Baldessari, C.; Milella, M.; Buti, S.; Militello, A.M.; Di Girolamo, S.; Fornarini, G.; Perri, G.; Basso, U.; Maruzzo, M.; et al. Immunotherapy in Dialysis-Dependent Cancer Patients: Our Experience in Patients With Metastatic Renal Cell Carcinoma and a Review of the Literature. Clin. Genitourin. Cancer 2019, 17, e903–e908. [Google Scholar] [CrossRef]
- Cheun, H.; Kim, M.; Lee, H.; Oh, K.H.; Keam, B. Safety and efficacy of immune checkpoint inhibitors for end-stage renal disease patients undergoing dialysis: A retrospective case series and literature review. Investig. N. Drugs 2019, 37, 579–583. [Google Scholar] [CrossRef]
- Strohbehn, I.A.; Lee, M.; Seethapathy, H.; Chute, D.; Rahma, O.; Guidon, A.; Neilan, T.G.; Zlotoff, D.A.; Okin, D.; Rengarajan, M.; et al. Safety and Efficacy of Immune Checkpoint Inhibitors in Patients on Dialysis: A Retrospective Case Series. Am. J. Kidney Dis. 2020, 76, 299–302. [Google Scholar] [CrossRef]
- Abdel-Wahab, N.; Safa, H.; Abudayyeh, A.; Johnson, D.H.; Trinh, V.A.; Zobniw, C.M.; Lin, H.; Wong, M.; Abdelrahim, M.; Gaber, A.O.; et al. Checkpoint inhibitor therapy for cancer in solid organ transplantation recipients: An institutional experience and a systematic review of the literature. J. Immunother. Cancer 2019, 7, 106. [Google Scholar] [CrossRef] [Green Version]
- Abdel-Wahab, N.; Shah, M.; Lopez-Olivo, M.A.; Suarez-Almazor, M.E. Use of Immune Checkpoint Inhibitors in the Treatment of Patients With Cancer and Preexisting Autoimmune Disease. Ann. Intern. Med. 2018, 169, 133–134. [Google Scholar] [CrossRef]
- Tison, A.; Quéré, G.; Misery, L.; Funck-Brentano, E.; Danlos, F.; Routier, E.; Robert, C.; Loriot, Y.; Lambotte, O.; Bonniaud, B.; et al. Safety and Efficacy of Immune Checkpoint Inhibitors in Patients With Cancer and Preexisting Autoimmune Disease: A Nationwide, Multicenter Cohort Study. Arthritis Rheumatol. 2019, 71, 2100–2111. [Google Scholar] [CrossRef]
- Kennedy, L.C.; Bhatia, S.; Thompson, J.A.; Grivas, P. Preexisting Autoimmune Disease: Implications for Immune Checkpoint Inhibitor Therapy in Solid Tumors. J. Natl. Compr. Cancer Netw. 2019, 17, 750–757. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, J.S.; Wang, D.Y.; Mamlouk, O.; Glass, W.F.; Abdelrahim, M.; Yee, C.; Abudayyeh, A. Immune checkpoint inhibitor associated reactivation of primary membranous nephropathy responsive to rituximab. J. Immunother. Cancer 2020, 8, e001287. [Google Scholar] [CrossRef] [PubMed]
- Murakami, N.; Mulvaney, P.; Danesh, M.; Abudayyeh, A.; Diab, A.; Abdel-Wahab, N.; Abdelrahim, M.; Khairallah, P.; Shirazian, S.; Kukla, A.; et al. A multi-center study on safety and efficacy of immune checkpoint inhibitors in cancer patients with kidney transplant. Kidney Int. 2021, 100, 196–205. [Google Scholar] [CrossRef]
- Champiat, S.; Lambotte, O.; Barreau, E.; Belkhir, R.; Berdelou, A.; Carbonnel, F.; Cauquil, C.; Chanson, P.; Collins, M.; Durrbach, A.; et al. Management of immune checkpoint blockade dysimmune toxicities: A collaborative position paper. Ann. Oncol. 2016, 27, 559–574. [Google Scholar] [CrossRef] [PubMed]
- Zheng, K.; Qiu, W.; Wang, H.; Si, X.; Zhang, X.; Zhang, L.; Li, X. Clinical recommendations on diagnosis and treatment of immune checkpoint inhibitor-induced renal immune-related adverse events. Thorac. Cancer 2020, 11, 1746–1751. [Google Scholar] [CrossRef] [Green Version]
- Perazella, M.A.; Sprangers, B. Checkpoint inhibitor therapy-associated acute kidney injury: Time to move on to evidence-based recommendations. Clin. Kidney J. 2021, 14, 1301–1306. [Google Scholar] [CrossRef] [PubMed]
- Bermejo, S.; Bolufer, M.; Riveiro-Barciela, M.; Soler, M.J. Immunotherapy and the Spectrum of Kidney Disease: Should We Individualize the Treatment? Front. Med. 2022, 9, 906565. [Google Scholar] [CrossRef]



| Type of irAEs | Any Grade Toxicity (% of Patients) | Grade 3–4 Toxicity (% of Patients) |
|---|---|---|
| SKIN (rash, pruritus, psoriasis, vitiligo, DRESS, Stevens-Johnson syndrome) | 13–50 | <3 |
| GASTROINTESTINAL (diarrhoea, colitis, ileitis, pancreatitis) | 16–54 | 1–11 |
| LIVER (hepatitis) | 5–10 | 1–2 |
| ENDOCRINE (hyper or hypothyroidism, hypophysitis, adrenal insufficiency, diabetes) | 5–21 | 0 |
| RESPIRATORY (pneumonitis, pleuritis, sarcoid-like granulomatosis) | 20–30 | 1–9 |
| CARDIOVASCULAR (myocarditis, pericarditis, vasculitis) | <1 | 0 |
| NEUROLOGIC (Neuropathy, Guillain-Barrè syndrome, myelopathy, meningitis, encephalitis, myasthenia) | 1–4 | 0 |
| EYE (uveitis, conjunctivitis, scleritis, episcleritis, blepharitis, retinitis) | <1 | 0 |
| RENAL (ATIN, glomerulonephritis, tubular acidosis, electrolytes alterations) | 1–29 | 2 |
| BLOOD (haemolyticanaemia, thrombocytopenia, neutropenia, haemophilia) | <1 | 0 |
| RHEUMATIC (polymyalgia rheumatica, psoriatic arthritis, seronegative-polyarthritis, dermatomyositis, myositis) | 2–12 | <1 (myositis) |
| KDIGO | ||
|---|---|---|
| Stage | Serum Creatinine | Diuresis |
| 1 | 1.5–1.9 × baseline or increase ≥ 0.3 mg/dL within 48 h | <0.5 mL/kg/h for 6–12 h |
| 2 | 2–2.9 × baseline | <0.5 mL/kg/h for >12 h |
| 3 | 3 × baseline or increase ≥ 4 mg/dL within 48 h or initiation of RRT or in patients < 18 years old, decreased eGFR < 35 mL/min/1.73 m2 | <0.3 mL/kg/h for >24 h or anuria for ≥ 12 h |
| CTCAE 3.0 | CTCAE 5.0 | |
|---|---|---|
| Grade | Serum Creatinine | Indications |
| 1 | 1–1.5 × ULN | - |
| 2 | 1.5–3 × ULN | - |
| 3 | >3 × ULN | Hospitalisation |
| 4 | >6 × ULN | Dialysis |
| General Management | Supportive Care; Withdraw Nephrotoxic Medication; Evaluate Other Causes | ||||
|---|---|---|---|---|---|
| Grade 1 | Grade 2 | Grade 3–4 | |||
| ASCO [56] | ICI therapy | Consider temporarily withholding | Temporarily withhold. | If there is a strong suspicion of AKI-ICI, permanently discontinue | |
| Treatment | Follow-up | Start prednisone or equivalent 0.5–1 mg/kg/d | Start 1–2 mg/kg/d prednisone or equivalent | ||
| Response | Improvement (to grade 1) | Follow-up | Wean CS over 4 weeks | ||
| Worsening | Treat as grade 2 | Treat as grade 3 | Consider additional immunosuppressors (such as MMF ° or infliximab *) | ||
| Nephrological consul | Consult nephrologist | ||||
| Kidney biopsy | Kidney biopsy should be discouraged with strong suspicions of ICI-related renal damage until steroid treatment has been attempted | ||||
| NCCN [57] | ICI therapy | Consider temporarily withholding | Withhold ICI | Withhold ICI | |
| Treatment | Follow-up | Start prednisone 0.5–1 mg/kg/d | Start prednisone/methylprednisolone 1–2 mg/kg/d Consider hospitalization | ||
| Response | Improvement (to grade 1) | Follow-up | |||
| Worsening | Prednisone/methylprednisolone 1–2 mg/kg/d | If kidney injury remains > G2 after 4–6 weeks of steroids, consider other immunosuppressors (such as MMF ° or infliximab *) | |||
| Nephrological consul | Consult nephrologist if not improved within 2 weeks | Consult nephrologist | |||
| Kidney biopsy | Consider renal biopsy, if feasible, prior to starting steroids | ||||
| SITC [58] | ICI therapy | Consider temporarily withholding ICI | Withhold ICI | ||
| Treatment | Start steroid therapy | ||||
| Response | Improvement (to grade 1) | ||||
| Worsening | Consider other immunosuppressors (such as MMF ° or infliximab *) | ||||
| Nephrological consul | For progressive or persistent AKI grade 1 | Consult nephrologist | |||
| Kidney biopsy | In the suspicion of renal damage that is not ICI-related | ||||
| ESMO [59] | ICI therapy | Continue ICI | Continue ICI if not attributed to an irAE. | Withhold ICI | |
| Treatment | Start 0.5–1 mg/kg/d prednisolone if attributed to an irAE. | ||||
| Response | Improvement (to grade 1) | Wean CS over 4 weeks | Wean corticosteroid over 4–12 weeks | ||
| Worsening | Treat as grade 2 | Treat as grade 3 | Start prednisolone 1 mg/kg/d or pulse dose methylprednisolone 250–500 mg for 3 days | ||
| Nephrological consult | Consult nephrologist | ||||
| Kidney biopsy | Early consideration of renal biopsy | ||||
| AIOM [60] | ICI therapy | Continue ICI | Discontinue ICI | Permanent discontinue ICI | |
| Treatment | Prednisone 0.5–1 mg/kg/d | Prednisone 1–2 mg/kg/d | |||
| Response | Improvement (to grade 1) | Wean corticosteroid over at least 4 weeks | |||
| Worsening | Start 1–2 mg/kg/d prednisone | Additional immunosuppressor not indicated | |||
| Nephrological consult | Not indicated | ||||
| Kidney biopsy | Not indicated | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longhitano, E.; Muscolino, P.; Lo Re, C.; Ferrara, S.A.; Cernaro, V.; Gembillo, G.; Tessitore, D.; Speranza, D.; Figura, F.; Santarpia, M.; et al. Immune Checkpoint Inhibitors and the Kidney: A Focus on Diagnosis and Management for Personalised Medicine. Cancers 2023, 15, 1891. https://doi.org/10.3390/cancers15061891
Longhitano E, Muscolino P, Lo Re C, Ferrara SA, Cernaro V, Gembillo G, Tessitore D, Speranza D, Figura F, Santarpia M, et al. Immune Checkpoint Inhibitors and the Kidney: A Focus on Diagnosis and Management for Personalised Medicine. Cancers. 2023; 15(6):1891. https://doi.org/10.3390/cancers15061891
Chicago/Turabian StyleLonghitano, Elisa, Paola Muscolino, Claudia Lo Re, Serena Ausilia Ferrara, Valeria Cernaro, Guido Gembillo, Dalila Tessitore, Desirèe Speranza, Francesco Figura, Mariacarmela Santarpia, and et al. 2023. "Immune Checkpoint Inhibitors and the Kidney: A Focus on Diagnosis and Management for Personalised Medicine" Cancers 15, no. 6: 1891. https://doi.org/10.3390/cancers15061891
APA StyleLonghitano, E., Muscolino, P., Lo Re, C., Ferrara, S. A., Cernaro, V., Gembillo, G., Tessitore, D., Speranza, D., Figura, F., Santarpia, M., Silvestris, N., Santoro, D., & Franchina, T. (2023). Immune Checkpoint Inhibitors and the Kidney: A Focus on Diagnosis and Management for Personalised Medicine. Cancers, 15(6), 1891. https://doi.org/10.3390/cancers15061891









