Effectiveness of Colorectal Cancer (CRC) Screening on All-Cause and CRC-Specific Mortality Reduction: A Systematic Review and Meta-Analysis
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Search Strategies
2.2. Study Selection and Data Extraction
2.3. Quality Assessment for RCTs and Simulation Models
2.4. Data Synthesis and Analysis
3. Results
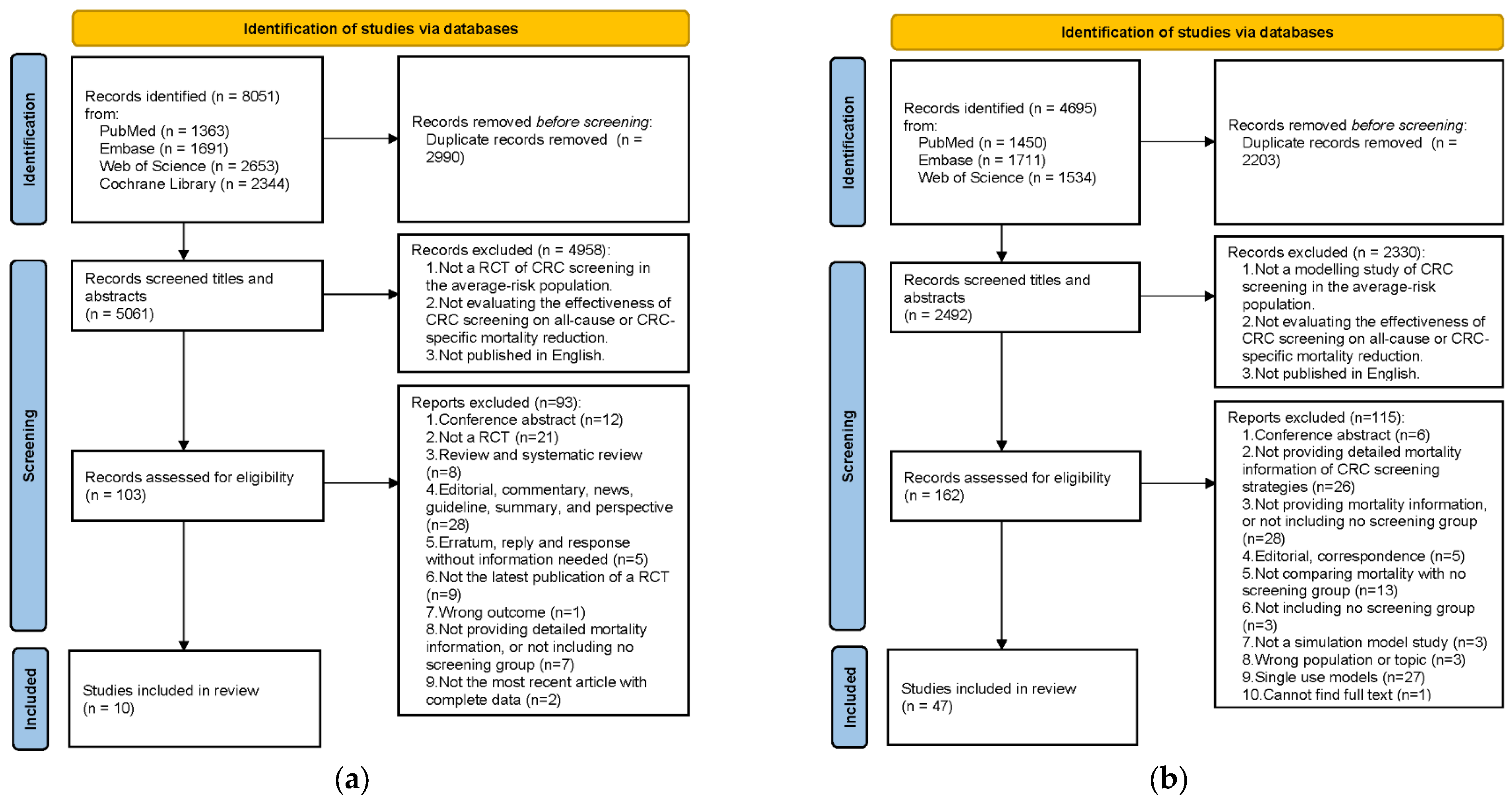
3.1. Literature Search
3.2. RCTs
3.2.1. Quality Assessment
3.2.2. Study Characteristics
3.2.3. Synthesis Results of CRC-Specific and All-Cause MR
3.2.4. Subgroup Analysis
3.3. Simulation Models
3.3.1. Study Characteristics and Quality Assessment
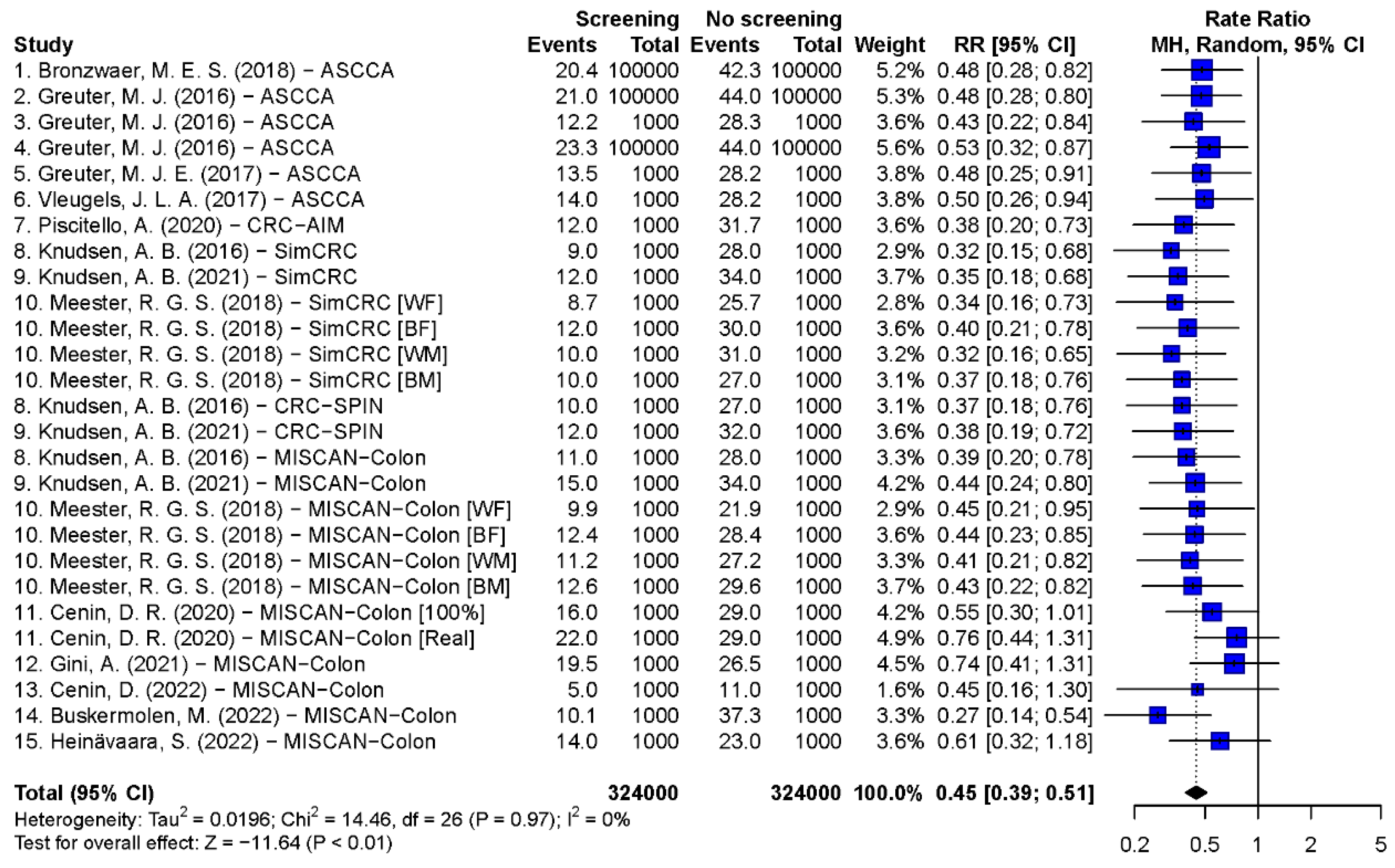
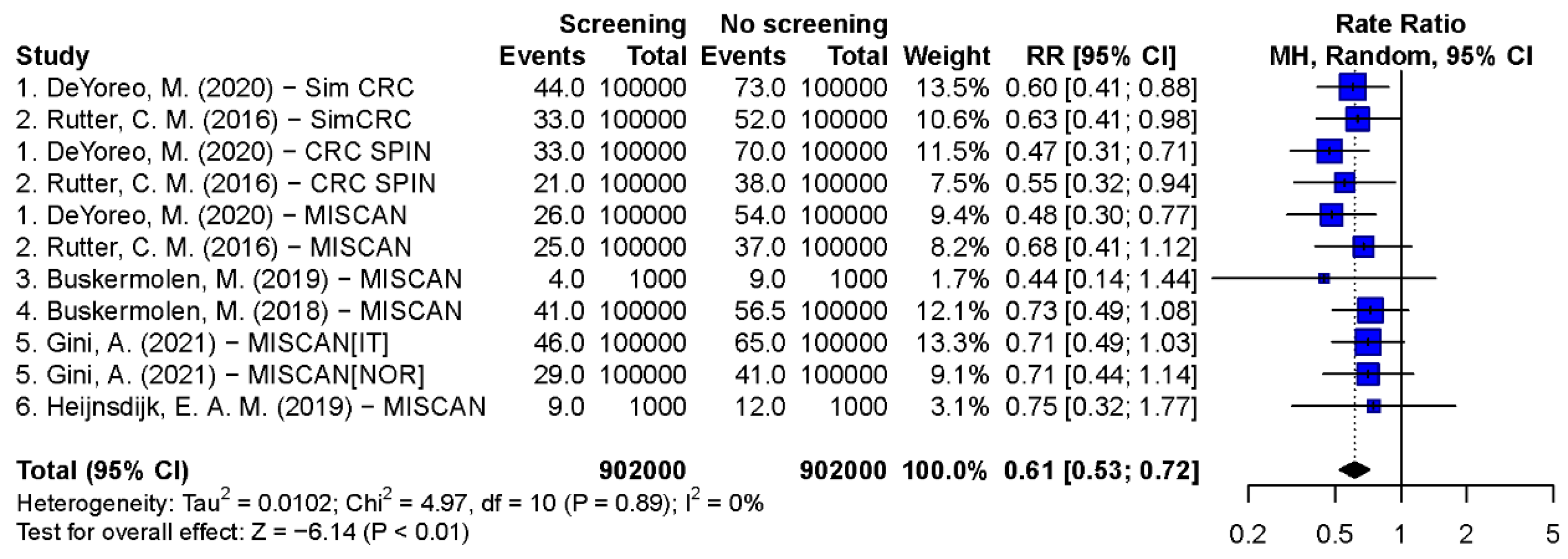
3.3.2. Synthesis Results of CRC-Specific and All-Cause MR
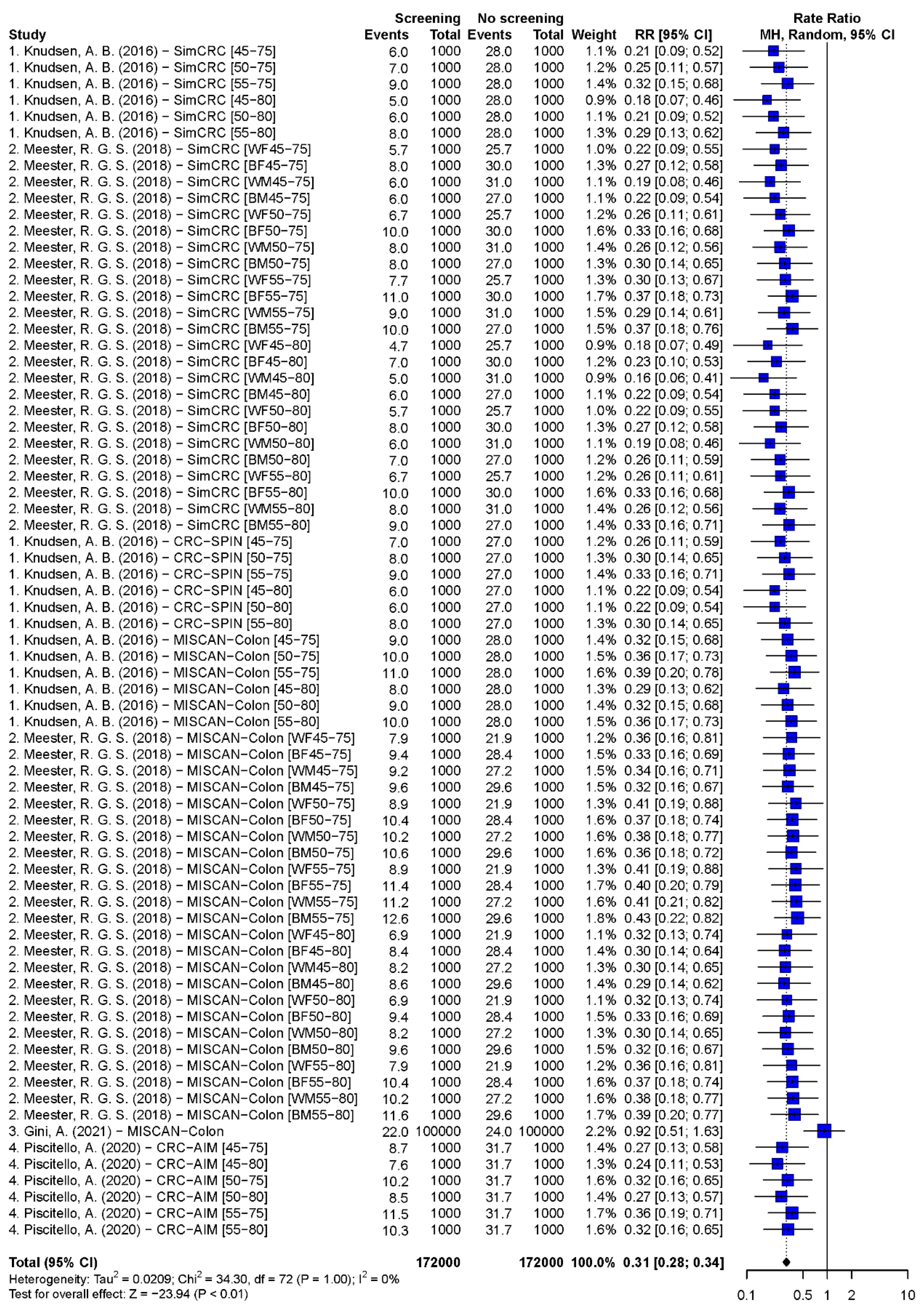
3.3.3. Subgroup Analysis
3.3.4. The Comparison of Model Studies and RCTs
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Agency for Research on Cancer. GLOBOCAN 2020. Available online: https://gco.iarc.fr/today/online-analysis-pie?v=2020&mode=cancer&mode_population=continents&population=900&populations=900&key=total&sex=0&cancer=39&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&nb_items=7&group_cancer=1&include_nmsc=1&include_nmsc_other=1&half_pie=0&donut=0 (accessed on 10 February 2023).
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Allemani, C.; Matsuda, T.; Di Carlo, V.; Harewood, R.; Matz, M.; Niksic, M.; Bonaventure, A.; Valkov, M.; Johnson, C.J.; Esteve, J.; et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): Analysis of individual records for 37,513,025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 2018, 391, 1023–1075. [Google Scholar] [CrossRef] [PubMed]
- International Agency for Research on Cancer. Colorectal cancer screening. In IARC Handbooks of Cancer Prevention; International Agency for Research on Cancer: Lyon, France, 2019; Volume 17, p. 300. [Google Scholar]
- Greuter, M.J.; Xu, X.M.; Lew, J.B.; Dekker, E.; Kuipers, E.J.; Canfell, K.; Meijer, G.A.; Coupe, V.M. Modeling the Adenoma and Serrated pathway to Colorectal CAncer (ASCCA). Risk Anal. 2014, 34, 889–910. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.D.; Oh, T.J.; Chung, T.H.; Jang, H.W.; Kim, Y.N.; An, S.; Kim, N.K. Early detection of colorectal cancer based on presence of methylated syndecan-2 (SDC2) in stool DNA. Clin. Epigenetics 2019, 11, 51. [Google Scholar] [CrossRef]
- American Cancer Society. Can Colorectal Polyps and Cancer Be Found Early? Available online: https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/detection.html (accessed on 10 February 2023).
- Bevan, R.; Rutter, M.D. Colorectal Cancer Screening-Who, How, and When? Clin. Endosc. 2018, 51, 37–49. [Google Scholar] [CrossRef]
- World Health Organization. Cancer Control: Module 3: Early Detection; WHO Press: Geneva, Switzerland, 2007; p. 50. [Google Scholar]
- Fisher, D.A.; Saoud, L.; Hassmiller Lich, K.; Fendrick, A.M.; Ozbay, A.B.; Borah, B.J.; Matney, M.; Parton, M.; Limburg, P.J. Impact of screening and follow-up colonoscopy adenoma sensitivity on colorectal cancer screening outcomes in the CRC-AIM microsimulation model. Cancer Med. 2021, 10, 2855–2864. [Google Scholar] [CrossRef] [PubMed]
- Goede, S.L.; Rabeneck, L.; van Ballegooijen, M.; Zauber, A.G.; Paszat, L.F.; Hoch, J.S.; Yong, J.H.; Kroep, S.; Tinmouth, J.; Lansdorp-Vogelaar, I. Harms, benefits and costs of fecal immunochemical testing versus guaiac fecal occult blood testing for colorectal cancer screening. PLoS ONE 2017, 12, e0172864. [Google Scholar] [CrossRef]
- Greuter, M.J.E.; de Klerk, C.M.; Meijer, G.A.; Dekker, E.; Coupe, V.M.H. Screening for Colorectal Cancer with Fecal Immunochemical Testing with and without Postpolypectomy Surveillance Colonoscopy: A Cost-Effectiveness Analysis. Ann. Intern. Med. 2017, 167, 544–554. [Google Scholar] [CrossRef]
- Lew, J.B.; St John, D.J.B.; Macrae, F.A.; Emery, J.D.; Ee, H.C.; Jenkins, M.A.; He, E.; Grogan, P.; Caruana, M.; Greuter, M.J.E.; et al. Benefits, Harms, and Cost-Effectiveness of Potential Age Extensions to the National Bowel Cancer Screening Program in Australia. Cancer Epidemiol. Biomark. Prev. 2018, 27, 1450–1461. [Google Scholar] [CrossRef]
- Naber, S.K.; Knudsen, A.B.; Zauber, A.G.; Rutter, C.M.; Fischer, S.E.; Pabiniak, C.J.; Soto, B.; Kuntz, K.M.; Lansdorp-Vogelaar, I. Cost-effectiveness of a multitarget stool DNA test for colorectal cancer screening of Medicare beneficiaries. PLoS ONE 2019, 14, e0220234. [Google Scholar] [CrossRef]
- Brenner, H.; Stock, C.; Hoffmeister, M. Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: Systematic review and meta-analysis of randomised controlled trials and observational studies. BMJ 2014, 348, g2467. [Google Scholar] [CrossRef] [PubMed]
- Elmunzer, B.J.; Hayward, R.A.; Schoenfeld, P.S.; Saini, S.D.; Deshpande, A.; Waljee, A.K. Effect of flexible sigmoidoscopy-based screening on incidence and mortality of colorectal cancer: A systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2012, 9, e1001352. [Google Scholar] [CrossRef]
- Elmunzer, B.J.; Singal, A.G.; Sussman, J.B.; Deshpande, A.R.; Sussman, D.A.; Conte, M.L.; Dwamena, B.A.; Rogers, M.A.; Schoenfeld, P.S.; Inadomi, J.M.; et al. Comparing the effectiveness of competing tests for reducing colorectal cancer mortality: A network meta-analysis. Gastrointest. Endosc. 2015, 81, 700–709.e3. [Google Scholar] [CrossRef]
- Zhang, J.; Cheng, Z.; Ma, Y.; He, C.; Lu, Y.; Zhao, Y.; Chang, X.; Zhang, Y.; Bai, Y.; Cheng, N. Effectiveness of Screening Modalities in Colorectal Cancer: A Network Meta-Analysis. Clin. Color. Cancer 2017, 16, 252–263. [Google Scholar] [CrossRef]
- Bronzwaer, M.E.S.; Greuter, M.J.E.; Bleijenberg, A.G.C.; JEG, I.J.; Dekker, E.; Coupe, V.M.H. Impact of differences in adenoma and proximal serrated polyp detection rate on the long-term effectiveness of FIT-based colorectal cancer screening. BMC Cancer 2018, 18, 465. [Google Scholar] [CrossRef]
- Buskermolen, M.; Cenin, D.R.; Helsingen, L.M.; Guyatt, G.; Vandvik, P.O.; Haug, U.; Bretthauer, M.; Lansdorp-Vogelaar, I. Colorectal cancer screening with faecal immunochemical testing, sigmoidoscopy or colonoscopy: A microsimulation modelling study. BMJ 2019, 367, l5383. [Google Scholar] [CrossRef]
- Buskermolen, M.; Gini, A.; Naber, S.K.; Toes-Zoutendijk, E.; de Koning, H.J.; Lansdorp-Vogelaar, I. Modeling in Colorectal Cancer Screening: Assessing External and Predictive Validity of MISCAN-Colon Microsimulation Model Using NORCCAP Trial Results. Med. Decis. Mak. 2018, 38, 917–929. [Google Scholar] [CrossRef] [PubMed]
- Cenin, D.R.; Naber, S.K.; de Weerdt, A.C.; Jenkins, M.A.; Preen, D.B.; Ee, H.C.; O’Leary, P.C.; Lansdorp-Vogelaar, I. Cost-Effectiveness of Personalized Screening for Colorectal Cancer Based on Polygenic Risk and Family History. Cancer Epidemiol. Biomark. Prev. 2020, 29, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Deibel, A.; Deng, L.; Cheng, C.Y.; Schlander, M.; Ran, T.; Lang, B.; Krupka, N.; Beerenwinkel, N.; Rogler, G.; Wiest, R.; et al. Evaluating key characteristics of ideal colorectal cancer screening modalities: The microsimulation approach. Gastrointest. Endosc. 2021, 94, 379–390.e7. [Google Scholar] [CrossRef]
- DeYoreo, M.; Lansdorp-Vogelaar, I.; Knudsen, A.B.; Kuntz, K.M.; Zauber, A.G.; Rutter, C.M. Validation of Colorectal Cancer Models on Long-term Outcomes from a Randomized Controlled Trial. Med. Decis. Mak. 2020, 40, 1034–1040. [Google Scholar] [CrossRef]
- Gini, A.; Buskermolen, M.; Senore, C.; Anttila, A.; Novak Mlakar, D.; Veerus, P.; Csanadi, M.; Jansen, E.E.L.; Zielonke, N.; Heinavaara, S.; et al. Development and Validation of Three Regional Microsimulation Models for Predicting Colorectal Cancer Screening Benefits in Europe. MDM Policy Pract. 2021, 6, 2381468320984974. [Google Scholar] [CrossRef]
- Greuter, M.J.; Berkhof, J.; Canfell, K.; Lew, J.B.; Dekker, E.; Coupe, V.M. Resilience of a FIT screening programme against screening fatigue: A modelling study. BMC Public Health 2016, 16, 1009. [Google Scholar] [CrossRef] [PubMed]
- Greuter, M.J.; Berkhof, J.; Fijneman, R.J.; Demirel, E.; Lew, J.B.; Meijer, G.A.; Stoker, J.; Coupe, V.M. The potential of imaging techniques as a screening tool for colorectal cancer: A cost-effectiveness analysis. Br. J. Radiol. 2016, 89, 20150910. [Google Scholar] [CrossRef]
- Greuter, M.J.; Demirel, E.; Lew, J.B.; Berkhof, J.; Xu, X.M.; Canfell, K.; Dekker, E.; Meijer, G.A.; Coupe, V.M. Long-Term Impact of the Dutch Colorectal Cancer Screening Program on Cancer Incidence and Mortality-Model-Based Exploration of the Serrated Pathway. Cancer Epidemiol. Biomark. Prev. 2016, 25, 135–144. [Google Scholar] [CrossRef]
- Heijnsdijk, E.A.M.; Csanadi, M.; Gini, A.; Ten Haaf, K.; Bendes, R.; Anttila, A.; Senore, C.; de Koning, H.J. All-cause mortality versus cancer-specific mortality as outcome in cancer screening trials: A review and modeling study. Cancer Med. 2019, 8, 6127–6138. [Google Scholar] [CrossRef] [PubMed]
- Knudsen, A.B.; Rutter, C.M.; Peterse, E.F.P.; Lietz, A.P.; Seguin, C.L.; Meester, R.G.S.; Perdue, L.A.; Lin, J.S.; Siegel, R.L.; Doria-Rose, V.P.; et al. Colorectal Cancer Screening: An Updated Modeling Study for the US Preventive Services Task Force. JAMA 2021, 325, 1998–2011. [Google Scholar] [CrossRef] [PubMed]
- Knudsen, A.B.; Zauber, A.G.; Rutter, C.M.; Naber, S.K.; Doria-Rose, V.P.; Pabiniak, C.; Johanson, C.; Fischer, S.E.; Lansdorp-Vogelaar, I.; Kuntz, K.M. Estimation of Benefits, Burden, and Harms of Colorectal Cancer Screening Strategies: Modeling Study for the US Preventive Services Task Force. JAMA 2016, 315, 2595–2609. [Google Scholar] [CrossRef]
- Ladabaum, U.; Mannalithara, A.; Meester, R.G.S.; Gupta, S.; Schoen, R.E. Cost-Effectiveness and National Effects of Initiating Colorectal Cancer Screening for Average-Risk Persons at Age 45 Years Instead of 50 Years. Gastroenterology 2019, 157, 137–148. [Google Scholar] [CrossRef]
- Lew, J.B.; St John, D.J.B.; Macrae, F.A.; Emery, J.D.; Ee, H.C.; Jenkins, M.A.; He, E.; Grogan, P.; Caruana, M.; Sarfati, D.; et al. Evaluation of the benefits, harms and cost-effectiveness of potential alternatives to iFOBT testing for colorectal cancer screening in Australia. Int. J. Cancer 2018, 143, 269–282. [Google Scholar] [CrossRef]
- Lew, J.B.; St John, D.J.B.; Xu, X.M.; Greuter, M.J.E.; Caruana, M.; Cenin, D.R.; He, E.; Saville, M.; Grogan, P.; Coupe, V.M.H.; et al. Long-term evaluation of benefits, harms, and cost-effectiveness of the National Bowel Cancer Screening Program in Australia: A modelling study. Lancet Public Health 2017, 2, e331–e340. [Google Scholar] [CrossRef]
- Meester, R.G.S.; Doubeni, C.A.; Zauber, A.G.; van Ballegooijen, M.; Corley, D.A.; Lansdorp-Vogelaar, I. Impact of adenoma detection on the benefit of faecal testing vs. colonoscopy for colorectal cancer. Int. J. Cancer 2017, 141, 2359–2367. [Google Scholar] [CrossRef]
- Meester, R.G.S.; Peterse, E.F.P.; Knudsen, A.B.; de Weerdt, A.C.; Chen, J.C.; Lietz, A.P.; Dwyer, A.; Ahnen, D.J.; Siegel, R.L.; Smith, R.A.; et al. Optimizing colorectal cancer screening by race and sex: Microsimulation analysis II to inform the American Cancer Society colorectal cancer screening guideline. Cancer 2018, 124, 2974–2985. [Google Scholar] [CrossRef]
- Meulen, M.P.V.; Kapidzic, A.; Leerdam, M.E.V.; van der Steen, A.; Kuipers, E.J.; Spaander, M.C.W.; de Koning, H.J.; Hol, L.; Lansdorp-Vogelaar, I. Do Men and Women Need to Be Screened Differently with Fecal Immunochemical Testing? A Cost-Effectiveness Analysis. Cancer Epidemiol. Biomark. Prev. 2017, 26, 1328–1336. [Google Scholar] [CrossRef] [PubMed]
- Peterse, E.F.P.; Meester, R.G.S.; de Jonge, L.; Omidvari, A.H.; Alarid-Escudero, F.; Knudsen, A.B.; Zauber, A.G.; Lansdorp-Vogelaar, I. Comparing the Cost-Effectiveness of Innovative Colorectal Cancer Screening Tests. J. Natl. Cancer Inst. 2021, 113, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Peterse, E.F.P.; Meester, R.G.S.; Siegel, R.L.; Chen, J.C.; Dwyer, A.; Ahnen, D.J.; Smith, R.A.; Zauber, A.G.; Lansdorp-Vogelaar, I. The impact of the rising colorectal cancer incidence in young adults on the optimal age to start screening: Microsimulation analysis I to inform the American Cancer Society colorectal cancer screening guideline. Cancer 2018, 124, 2964–2973. [Google Scholar] [CrossRef]
- Piscitello, A.; Saoud, L.; Fendrick, A.M.; Borah, B.J.; Hassmiller Lich, K.; Matney, M.; Ozbay, A.B.; Parton, M.; Limburg, P.J. Estimating the impact of differential adherence on the comparative effectiveness of stool-based colorectal cancer screening using the CRC-AIM microsimulation model. PLoS ONE 2020, 15, e0244431. [Google Scholar] [CrossRef] [PubMed]
- Prakash, M.K.; Lang, B.; Heinrich, H.; Valli, P.V.; Bauerfeind, P.; Sonnenberg, A.; Beerenwinkel, N.; Misselwitz, B. CMOST: An open-source framework for the microsimulation of colorectal cancer screening strategies. BMC Med. Inform. Decis. Mak. 2017, 17, 80. [Google Scholar] [CrossRef]
- Rutter, C.M.; Knudsen, A.B.; Marsh, T.L.; Doria-Rose, V.P.; Johnson, E.; Pabiniak, C.; Kuntz, K.M.; van Ballegooijen, M.; Zauber, A.G.; Lansdorp-Vogelaar, I. Validation of Models Used to Inform Colorectal Cancer Screening Guidelines: Accuracy and Implications. Med. Decis. Mak. 2016, 36, 604–614. [Google Scholar] [CrossRef]
- Vleugels, J.L.A.; Greuter, M.J.E.; Hazewinkel, Y.; Coupe, V.M.H.; Dekker, E. Implementation of an optical diagnosis strategy saves costs and does not impair clinical outcomes of a fecal immunochemical test-based colorectal cancer screening program. Endosc. Int. Open 2017, 5, E1197–E1207. [Google Scholar] [CrossRef]
- Fisher, D.A.; Karlitz, J.J.; Jeyakumar, S.; Smith, N.; Limburg, P.; Lieberman, D.; Fendrick, A.M. Real-world cost-effectiveness of stool-based colorectal cancer screening in a Medicare population. J. Med. Econ. 2021, 24, 654–664. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Koleva-Kolarova, R.G.; Zhan, Z.; Greuter, M.J.; Feenstra, T.L.; De Bock, G.H. Simulation models in population breast cancer screening: A systematic review. Breast 2015, 24, 354–363. [Google Scholar] [CrossRef] [PubMed]
- Atkin, W.; Wooldrage, K.; Parkin, D.M.; Kralj-Hans, I.; MacRae, E.; Shah, U.; Duffy, S.; Cross, A.J. Long term effects of once-only flexible sigmoidoscopy screening after 17 years of follow-up: The UK Flexible Sigmoidoscopy Screening randomised controlled trial. Lancet 2017, 389, 1299–1311. [Google Scholar] [CrossRef] [PubMed]
- Scholefield, J.H.; Moss, S.M.; Mangham, C.M.; Whynes, D.K.; Hardcastle, J.D. Nottingham trial of faecal occult blood testing for colorectal cancer: A 20-year follow-up. Gut 2012, 61, 1036–1040. [Google Scholar] [CrossRef]
- Senore, C.; Riggi, E.; Armaroli, P.; Bonelli, L.; Sciallero, S.; Zappa, M.; Arrigoni, A.; Casella, C.; Crosta, C.; Falcini, F.; et al. Long-Term Follow-up of the Italian Flexible Sigmoidoscopy Screening Trial. Ann. Intern. Med. 2022, 175, 36–45. [Google Scholar] [CrossRef]
- Shaukat, A.; Kaalby, L.; Baatrup, G.; Kronborg, O.; Duval, S.; Shyne, M.; Mandel, J.S.; Church, T.R. Effects of Screening Compliance on Long-term Reductions in All-Cause and Colorectal Cancer Mortality. Clin. Gastroenterol. Hepatol. 2021, 19, 967–975.e2. [Google Scholar] [CrossRef]
- Shaukat, A.; Mongin, S.J.; Geisser, M.S.; Lederle, F.A.; Bond, J.H.; Mandel, J.S.; Church, T.R. Long-term mortality after screening for colorectal cancer. N. Engl. J. Med. 2013, 369, 1106–1114. [Google Scholar] [CrossRef]
- Holme, O.; Loberg, M.; Kalager, M.; Bretthauer, M.; Hernan, M.A.; Aas, E.; Eide, T.J.; Skovlund, E.; Lekven, J.; Schneede, J.; et al. Long-Term Effectiveness of Sigmoidoscopy Screening on Colorectal Cancer Incidence and Mortality in Women and Men: A Randomized Trial. Ann. Intern. Med. 2018, 168, 775–782. [Google Scholar] [CrossRef]
- Lindholm, E.; Brevinge, H.; Haglind, E. Survival benefit in a randomized clinical trial of faecal occult blood screening for colorectal cancer. Br. J. Surg. 2008, 95, 1029–1036. [Google Scholar] [CrossRef]
- Pinsky, P.F.; Miller, E.A.; Zhu, C.S.; Prorok, P.C. Overall mortality in men and women in the randomized Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. J. Med. Screen. 2019, 26, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Pitkaniemi, J.; Seppa, K.; Hakama, M.; Malminiemi, O.; Palva, T.; Vuoristo, M.S.; Jarvinen, H.; Paimela, H.; Pikkarainen, P.; Anttila, A.; et al. Effectiveness of screening for colorectal cancer with a faecal occult-blood test, in Finland. BMJ Open Gastroenterol. 2015, 2, e000034. [Google Scholar] [CrossRef]
- Thiis-Evensen, E.; Kalager, M.; Bretthauer, M.; Hoff, G. Long-term effectiveness of endoscopic screening on incidence and mortality of colorectal cancer: A randomized trial. United Eur. Gastroenterol. J. 2013, 1, 162–168. [Google Scholar] [CrossRef]
- Babela, R.; Orsagh, A.; Ricova, J.; Lansdorp-Vogelaar, I.; Csanadi, M.; De Koning, H.; Reckova, M. Cost-effectiveness of colorectal cancer screening in Slovakia. Eur. J. Cancer Prev. 2021, 31, 415–421. [Google Scholar] [CrossRef]
- Buskermolen, M.; Naber, S.K.; Toes-Zoutendijk, E.; van der Meulen, M.P.; van Grevenstein, W.M.U.; van Leerdam, M.E.; Spaander, M.C.W.; Lansdorp-Vogelaar, I. Impact of surgical versus endoscopic management of complex nonmalignant polyps in a colorectal cancer screening program. Endoscopy 2022, 54, 871–880. [Google Scholar] [CrossRef] [PubMed]
- Cenin, D.; Li, P.; Wang, J.; de Jonge, L.; Yan, B.; Tao, S.; Lansdorp-Vogelaar, I. Optimising colorectal cancer screening in Shanghai, China: A modelling study. BMJ Open 2022, 12, e048156. [Google Scholar] [CrossRef] [PubMed]
- Csanadi, M.; Gini, A.; Koning, H.; Szeles, G.; Pitter, J.G.; Oroszi, B.; Pataki, P.; Fadgyas-Freyler, P.; Korponai, G.; Voko, Z.; et al. Modeling costs and benefits of the organized colorectal cancer screening programme and its potential future improvements in Hungary. J. Med. Screen. 2021, 28, 268–276. [Google Scholar] [CrossRef] [PubMed]
- Gini, A.; van Ravesteyn, N.T.; Jansen, E.E.L.; Heijnsdijk, E.A.M.; Senore, C.; Anttila, A.; Novak Mlakar, D.; Veerus, P.; Csanadi, M.; Zielonke, N.; et al. The EU-TOPIA evaluation tool: An online modelling-based tool for informing breast, cervical, and colorectal cancer screening decisions in Europe. Prev. Med. Rep. 2021, 22, 101392. [Google Scholar] [CrossRef]
- Heinavaara, S.; Gini, A.; Sarkeala, T.; Anttila, A.; de Koning, H.; Lansdorp-Vogelaar, I. Optimizing screening with faecal immunochemical test for both sexes—Cost-effectiveness analysis from Finland. Prev. Med. 2022, 157, 106990. [Google Scholar] [CrossRef] [PubMed]
- Naber, S.K.; Almadi, M.A.; Guyatt, G.; Xie, F.; Lansdorp-Vogelaar, I. Cost-effectiveness analysis of colorectal cancer screening in a low incidence country: The case of Saudi Arabia. Saudi J. Gastroenterol. 2021, 27, 208–216. [Google Scholar] [CrossRef]
- Naber, S.K.; Kundu, S.; Kuntz, K.M.; Dotson, W.D.; Williams, M.S.; Zauber, A.G.; Calonge, N.; Zallen, D.T.; Ganiats, T.G.; Webber, E.M.; et al. Cost-Effectiveness of Risk-Stratified Colorectal Cancer Screening Based on Polygenic Risk: Current Status and Future Potential. JNCI Cancer Spectr. 2020, 4, pkz086. [Google Scholar] [CrossRef]
- van der Meulen, M.P.; Lansdorp-Vogelaar, I.; Goede, S.L.; Kuipers, E.J.; Dekker, E.; Stoker, J.; van Ballegooijen, M. Colorectal Cancer: Cost-effectiveness of Colonoscopy versus CT Colonography Screening with Participation Rates and Costs. Radiology 2018, 287, 901–911. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; de Jonge, L.; Cenin, D.R.; Li, P.; Tao, S.; Yang, C.; Yan, B.; Lansdorp-Vogelaar, I. Cost-effectiveness analysis of colorectal cancer screening in Shanghai, China: A modelling study. Prev. Med. Rep. 2022, 29, 101891. [Google Scholar] [CrossRef] [PubMed]
- Fisher, D.A.; Saoud, L.; Finney Rutten, L.J.; Ozbay, A.B.; Brooks, D.; Limburg, P.J. Lowering the colorectal cancer screening age improves predicted outcomes in a microsimulation model. Curr. Med. Res. Opin. 2021, 37, 1005–1010. [Google Scholar] [CrossRef]
- Karlitz, J.J.; Fendrick, A.M.; Bhatt, J.; Coronado, G.D.; Jeyakumar, S.; Smith, N.J.; Plescia, M.; Brooks, D.; Limburg, P.; Lieberman, D. Cost-Effectiveness of Outreach Strategies for Stool-Based Colorectal Cancer Screening in a Medicaid Population. Popul. Health Manag. 2022, 25, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Ladabaum, U.; Mannalithara, A. Comparative Effectiveness and Cost Effectiveness of a Multitarget Stool DNA Test to Screen for Colorectal Neoplasia. Gastroenterology 2016, 151, 427–439.e6. [Google Scholar] [CrossRef]
- Ladabaum, U.; Mannalithara, A.; Brill, J.V.; Levin, Z.; Bundorf, K.M. Contrasting Effectiveness and Cost-Effectiveness of Colorectal Cancer Screening Under Commercial Insurance vs. Medicare. Am. J. Gastroenterol. 2018, 113, 1836–1847. [Google Scholar] [CrossRef]
- Ladabaum, U.; Mannalithara, A.; Mitani, A.; Desai, M. Clinical and Economic Impact of Tailoring Screening to Predicted Colorectal Cancer Risk: A Decision Analytic Modeling Study. Cancer Epidemiol. Biomark. Prev. 2020, 29, 318–328. [Google Scholar] [CrossRef]
- Chen, C.; Stock, C.; Hoffmeister, M.; Brenner, H. Optimal age for screening colonoscopy: A modeling study. Gastrointest. Endosc. 2019, 89, 1017–1025.e12. [Google Scholar] [CrossRef]
- Heisser, T.; Hoffmeister, M.; Brenner, H. Model based evaluation of long-term efficacy of existing and alternative colorectal cancer screening offers: A case study for Germany. Int. J. Cancer 2022, 150, 1471–1480. [Google Scholar] [CrossRef]
- Lew, J.B.; Feletto, E.; Worthington, J.; Roder, D.; Canuto, K.; Miller, C.; D’Onise, K.; Canfell, K. The potential for tailored screening to reduce bowel cancer mortality for Aboriginal and Torres Strait Islander peoples in Australia: Modelling study. J. Cancer Policy 2022, 32, 100325. [Google Scholar] [CrossRef] [PubMed]
- Helsingen, L.M.; Vandvik, P.O.; Jodal, H.C.; Agoritsas, T.; Lytvyn, L.; Anderson, J.C.; Auer, R.; Murphy, S.B.; Almadi, M.A.; Corley, D.A.; et al. Colorectal cancer screening with faecal immunochemical testing, sigmoidoscopy or colonoscopy: A clinical practice guideline. BMJ 2019, 367, l5515. [Google Scholar] [CrossRef] [PubMed]
- Powell, K.; Prasad, V. Colorectal cancer screening at a younger age: Pitfalls in the model-based recommendation of the USPSTF. BMJ Evid. Based Med. 2022, 27, 206–208. [Google Scholar] [CrossRef]
- Choi, K.S.; Lee, H.Y.; Jun, J.K.; Shin, A.; Park, E.C. Adherence to follow-up after a positive fecal occult blood test in an organized colorectal cancer screening program in Korea, 2004–2008. J. Gastroenterol. Hepatol. 2012, 27, 1070–1077. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick-Lewis, D.; Ali, M.U.; Warren, R.; Kenny, M.; Sherifali, D.; Raina, P. Screening for Colorectal Cancer: A Systematic Review and Meta-Analysis. Clin. Color. Cancer 2016, 15, 298–313. [Google Scholar] [CrossRef]
- Jodal, H.C.; Helsingen, L.M.; Anderson, J.C.; Lytvyn, L.; Vandvik, P.O.; Emilsson, L. Colorectal cancer screening with faecal testing, sigmoidoscopy or colonoscopy: A systematic review and network meta-analysis. BMJ Open 2019, 9, e032773. [Google Scholar] [CrossRef]
- Patel, S.S.; Kilgore, M.L. Cost Effectiveness of Colorectal Cancer Screening Strategies. Cancer Control. 2015, 22, 248–258. [Google Scholar] [CrossRef] [PubMed]
- Ran, T.; Cheng, C.Y.; Misselwitz, B.; Brenner, H.; Ubels, J.; Schlander, M. Cost-Effectiveness of Colorectal Cancer Screening Strategies-A Systematic Review. Clin. Gastroenterol. Hepatol. 2019, 17, 1969–1981.e15. [Google Scholar] [CrossRef]
- Zhong, G.C.; Sun, W.P.; Wan, L.; Hu, J.J.; Hao, F.B. Efficacy and cost-effectiveness of fecal immunochemical test versus colonoscopy in colorectal cancer screening: A systematic review and meta-analysis. Gastrointest. Endosc. 2020, 91, 684–697.e15. [Google Scholar] [CrossRef]
- Zauber, A.G.; Winawer, S.J.; O’Brien, M.J.; Lansdorp-Vogelaar, I.; van Ballegooijen, M.; Hankey, B.F.; Shi, W.; Bond, J.H.; Schapiro, M.; Panish, J.F.; et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N. Engl. J. Med. 2012, 366, 687–696. [Google Scholar] [CrossRef]
- Lin, J.S.; Piper, M.A.; Perdue, L.A.; Rutter, C.; Webber, E.M.; O’Connor, E.; Smith, N.; Whitlock, E.P. Screening for Colorectal Cancer: A Systematic Review for the U.S. Preventive Services Task Force; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2016. [Google Scholar]
- Whitlock, E.P.; Lin, J.S.; Liles, E.; Beil, T.L.; Fu, R. Screening for colorectal cancer: A targeted, updated systematic review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2008, 149, 638–658. [Google Scholar] [CrossRef]
- Wu, W.; Huang, J.; Yang, Y.; Gu, K.; Luu, H.N.; Tan, S.; Yang, C.; Fu, J.; Bao, P.; Ying, T.; et al. Adherence to colonoscopy in cascade screening of colorectal cancer: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2022, 37, 620–631. [Google Scholar] [CrossRef] [PubMed]
- Ponti, A.; Anttila, A.; Ronco, G.; Senore, C.; Basu, P.; Segnan, N.; Tomatis, M. Against Cancer. In Cancer Screening in the European Union. Report on the Implementation of the Council Recommendation on Cancer Screening; European Commission: Brussels, Belgium, 2017; p. 333. [Google Scholar]
- World Health Organization. Comprehensive Cervical Cancer Control: A Guide to Essential Practice, 2nd ed.; WHO Press: Geneva, Switzerland, 2014; p. 364. [Google Scholar]
- Jandorf, L.; Braschi, C.; Ernstoff, E.; Wong, C.R.; Thelemaque, L.; Winkel, G.; Thompson, H.S.; Redd, W.H.; Itzkowitz, S.H. Culturally targeted patient navigation for increasing african americans’ adherence to screening colonoscopy: A randomized clinical trial. Cancer Epidemiol. Biomark. Prev. 2013, 22, 1577–1587. [Google Scholar] [CrossRef]
- Jensen, J.D.; King, A.J.; Carcioppolo, N.; Krakow, M.; Samadder, N.J.; Morgan, S. Comparing tailored and narrative worksite interventions at increasing colonoscopy adherence in adults 50–75: A randomized controlled trial. Soc. Sci. Med. 2014, 104, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Ling, B.S.; Schoen, R.E.; Trauth, J.M.; Wahed, A.S.; Eury, T.; Simak, D.M.; Solano, F.X.; Weissfeld, J.L. Physicians encouraging colorectal screening: A randomized controlled trial of enhanced office and patient management on compliance with colorectal cancer screening. Arch. Intern. Med. 2009, 169, 47–55. [Google Scholar] [CrossRef]
- Myers, R.E.; Sifri, R.; Daskalakis, C.; DiCarlo, M.; Geethakumari, P.R.; Cocroft, J.; Minnick, C.; Brisbon, N.; Vernon, S.W. Increasing colon cancer screening in primary care among African Americans. J. Natl. Cancer Inst. 2014, 106, dju344. [Google Scholar] [CrossRef] [PubMed]
- Carter, J.L.; Coletti, R.J.; Harris, R.P. Quantifying and monitoring overdiagnosis in cancer screening: A systematic review of methods. BMJ 2015, 350, g7773. [Google Scholar] [CrossRef]
- Eddy, D.M.; Hollingworth, W.; Caro, J.J.; Tsevat, J.; McDonald, K.M.; Wong, J.B.; ISPOR-SMDM Modeling Good Research Practices Task Force. Model transparency and validation: A report of the ISPOR-SMDM Modeling Good Research Practices Task Force-7. Med. Decis. Mak. 2012, 32, 733–743. [Google Scholar] [CrossRef]
| Study | Program | Intervention | Age | Screening Years | Follow-Up Time (Years) | Total No. of Participants | Total No. of Screening Group | Adherence Rate in Screening Group (%) | Total No. of Control Group | Results of Compliance-Adjusted |
|---|---|---|---|---|---|---|---|---|---|---|
| A Shaukat US, 2013 [52] | Minnesota Colon Cancer Control Study | Annual or biennial gFOBT | 50–80 | 1976–1992 | 30.0 | 46,551 | 31,157 | 90.0 | 15,394 | All-cause and CRC-specific |
| A Shaukat Finland, 2021 [51] | Funen Fecal Occult Blood Trial | Biennial gFOBT | 45–75 | 1985–2002 | 30.0 | 61,933 | 30,966 | 66.8 | 30,964 | All-cause and CRC-specific |
| E Lindholm Sweden, 2008 [54] | Goteborg FOBT Trial | 2–3 times gFOBT | 60–64 | 1982–1995 | Mean 15.5/8.7 a | 68,308 | 34,144 | 70.0 | 34,164 | N/A |
| J H Scholefield UK, 2012 [49] | Nottingham Trial | Biennial gFOBT | 45–74 | 1981–1991 | Median 19.5 | 151,975 | 76,056 | 57.0 | 75,919 | CRC-specific |
| J Pitkäniemi Finland, 2015 [56] | Finnish FOBT Screening Programme | Biennial gFOBT | 60–69 | 2004–2012 | Median 4.5 | 360,492 | 180,210 | 68.8 | 180,282 | N/A |
| E Thiis-Evensen Norway, 2013 [57] | Telemark Polyp Study | Single FS | 50–59 | 1983–1996 | 26.0 | 799 | 400 | 81.0 | 399 | N/A |
| C Senore Italy, 2022 [50] | SCORE Trial | Single FS | 55–64 | 1995–1999 | Median 18.8 | 34,272 | 17,136 | 57.8 | 17,136 | All-cause and CRC-specific |
| Ø Holme Norway, 2018 [53] | NORCCAP | Single FS with or without FOBT | 50–64 | 1999–2001 | Median 14.8 | 98,678 | 20,552 | 63.1 | 78,126 | N/A |
| P F Pinsky US, 2019 [55] | PLCO Cancer Screening | FS at baseline and at year 3 or 5 | 55–74 | 1993–2001 | Median 17.0 | 154,887 | 77,443 | 86.6 | 77,444 | N/A |
| W Atkin UK, 2017 [48] | UKFSST | Single FS | 55–64 | 1994–1999 | Median 17.0 | 170,034 | 57,098 | 71.1 | 112,936 | All-cause and CRC-specific |
| Studies | Screening Group | Control Group | All-Cause Mortality Rate Ratio (95 CI%) b | CRC-Specific Mortality Rate Ratio (95 CI%) b | ||||
|---|---|---|---|---|---|---|---|---|
| All-Cause Deaths | CRC-Specific Deaths | Total Person-Years of Observation | All-Cause Deaths | CRC-Specific Deaths | Total Person-Years of Observation | |||
| FOBT | ||||||||
| A Shaukat 2013 [52] | 22,076 | 437 | 951,047 | 10,944 | 295 | 469,897 | 1.00 (0.97, 1.02) | 0.73 (0.63, 0.85) |
| A Shaukat 2021 [51] | 22,474 | 786 | 605,023 | 22,535 | 851 | 603,953 | 1.00 (0.98, 1.01) | 0.92 (0.84, 1.02) |
| E Lindholm 2008 [54] | 10,591 | 252 | 471,072 | 10,432 | 300 | 471,980 | 1.02 (0.99, 1.04) | 0.84 (0.71, 1.00) |
| J H Scholefield 2012 [49] | 40,681 | 1176 | 1,296,712 | 40,550 | 1300 | 1,296,614 | 1.00 (0.99, 1.02) | 0.90 (0.84, 0.98) |
| J Pitkäniemi 2015 [56] | 8000 | 170 | 805,480 | 7963 | 164 | 805,693 | 1.00 (0.97, 1.04) | 1.04 (0.84, 1.28) |
| Meta-analysis: | ||||||||
| No. of studies | 5 | 5 | ||||||
| Pooled estimate | 1.00 (0.99, 1.01) | 0.88 (0.80, 0.96) | ||||||
| Test for overall effect: P | 0.65 | 0.005 | ||||||
| Heterogeneity: I2 (%)/Tau2/P | 0/0.00/0.74 | 59/0.01/0.04 | ||||||
| FS | ||||||||
| E Thiis-Evensen 2013 [57] | 188 | 1 | 8441 | 151 | 7 | 8997 | 1.33 (1.07, 1.64) | 0.15 (0.02, 1.24) |
| C Senore 2022 [50] | 3062 | 122 | 296,730 | 3155 | 157 | 295,013 | 0.96 (0.92, 1.01) | 0.77 (0.61, 0.98) |
| P F Pinsky 2019 [55] | 22,562 | 416 | 1,234,900 | 22,652 | 546 | 1,222,450 | 0.99 (0.97, 1.00) | 0.75 (0.66, 0.86) |
| W Atkin 2017 [48] | 13,279 | 353 | 902,198 | 26,409 | 996 | 1,780,738 | 0.99 (0.97, 1.01) | 0.70 (0.62, 0.79) |
| Ø Holme 2018 [53] | 3809 | 122 | 291,075 | 13,433 | 530 | 1,114,581 | 1.09 (1.05, 1.13) | 0.88 (0.72, 1.07) |
| Meta-analysis: | ||||||||
| No. of studies | 5 | 5 | ||||||
| Pooled estimate | 1.02 (0.97, 1.06) | 0.76 (0.68, 0.84) | ||||||
| Test for overall effect: P | 0.46 | <0.001 | ||||||
| Heterogeneity: I2 (%)/Tau2/P | 88/0.00/<0.001 | 35/0.00/0.19 | ||||||
| Model | Study No. | Study | Simulate Population | Screening Age | Simulation Period/Follow-Up Time (Years) | Adherence Rate in Screening Group (%) | CRC Mortality of No Screening Group | CRC Mortality of Screening Group |
|---|---|---|---|---|---|---|---|---|
| ASCCA | 1 | Bronzwaer, M. E. S. (2018) [19] | Dutch | 55–75 | 2014–2044 | 73% (FIT)/92% (FIT-positive CS) | 42.3/100,000 | 20.4/100,000 |
| 2 | Greuter, M. J. (2016) [26] | Dutch | 55–75 | 2014–2044 (30 years) | 63% (FIT)/82% (FIT-positive CS) | 44.0/100,000 | 21.0/100,000 | |
| 3 | Greuter, M. J. (2016) [27] | Dutch | 55–75 | Lifetime (11 rounds) | 63% (FIT)/96% (FIT-positive CS) | 28.3/1000 | 12.2/1000 | |
| 4 | Greuter, M. J. (2016) [28] | Dutch | 55–75 | 2014–2044 (30 years) | 63% (FIT)/96% (FIT-positive CS) | 44.0/100,000 | 23.3/100,000 | |
| 5 | Greuter, M. J. E. (2017) [12] | Dutch | 55–75 | Lifetime | 72.6% (FIT)/92% (FIT-positive and Surveillance CS) | 28.2/1000 | 13.5/1000 | |
| 6 | Vleugels, J. L. A. (2017) [43] | Dutch | 55–75 | Lifetime | 73% (FIT)/92% (FIT-positive CS) | 28.2/1000 | 14.0/1000 | |
| CRC-AIM | 7 | Piscitello, A. (2020) [40] | US | 55–75 | Lifetime | 100% | 31.7/1000 | 12.0/1000 |
| SimCRC | 8 | Knudsen, A. B. (2016) [31] | US | 55–75 | Lifetime | 100% | 28.0/1000 | 9.0/1000 |
| 9 | Knudsen, A. B. (2021) [30] | US | 55–75 | Lifetime | 100% | 34.0/1000 | 12.0/1000 | |
| 10 | Meester, R. G. S. (2018) [36] | US White Female | 55–75 | Lifetime | 100% | 25.7/1000 | 8.7/1000 | |
| US Black Female | 55–75 | Lifetime | 100% | 30.0/1000 | 12.0/1000 | |||
| US White Male | 55–75 | Lifetime | 100% | 31.0/1000 | 10.0/1000 | |||
| US Black Male | 55–75 | Lifetime | 100% | 27.0/1000 | 10.0/1000 | |||
| CRC-SPIN | 8 | Knudsen, A. B. (2016) [31] | US | 55–75 | Lifetime | 100% | 27.0/1000 | 10.0/1000 |
| 9 | Knudsen, A. B. (2021) [30] | US | 55–75 | Lifetime | 100% | 32.0/1000 | 12.0/1000 | |
| MISCAN-Colon | 8 | Knudsen, A. B. (2016) [31] | US | 55–75 | Lifetime | 100% | 28.0/1000 | 11.0/1000 |
| 9 | Knudsen, A. B. (2021) [30] | US | 55–75 | Lifetime | 100% | 34.0/1000 | 15.0/1000 | |
| 10 | Meester, R. G. S. (2018) [36] | US White Female | 55–75 | Lifetime | 100% | 21.9/1000 | 9.9/1000 | |
| US Black Female | 55–75 | Lifetime | 100% | 28.4/1000 | 12.4/1000 | |||
| US White Male | 55–75 | Lifetime | 100% | 27.2/1000 | 11.2/1000 | |||
| US Black Male | 55–75 | Lifetime | 100% | 29.6/1000 | 12.6/1000 | |||
| 11 | Cenin, D. R. (2020) [22] | Australian | 54–74 | Lifetime 40–100 | 100% | 29.0/1000 | 16.0/1000 | |
| Australian | 54–74 | Lifetime 40–100 | Realistic adherence | 29.0/1000 | 22.0/1000 | |||
| 12 | Gini, A. (2021) [62] | Dutch | 55–75 | 2018–2050 | 71.3% | 26.5/1000 | 19.5/1000 | |
| 13 | Cenin, D. (2022) [60] | Chinese | 55–75 | Lifetime | 100% | 11.0/1000 | 5.0/1000 | |
| 14 | Buskermolen, M. (2022) [59] | Dutch | 55–75 | Lifetime | 72.4% | 37.3/1000 | 10.1/1000 | |
| 15 | Heinävaara, S. (2022) [63] | Finnish | 55–74 | Lifetime | 100% | 23.0/1000 | 14.0/1000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, S.; Schrijvers, J.J.A.; Greuter, M.J.W.; Kats-Ugurlu, G.; Lu, W.; de Bock, G.H. Effectiveness of Colorectal Cancer (CRC) Screening on All-Cause and CRC-Specific Mortality Reduction: A Systematic Review and Meta-Analysis. Cancers 2023, 15, 1948. https://doi.org/10.3390/cancers15071948
Zheng S, Schrijvers JJA, Greuter MJW, Kats-Ugurlu G, Lu W, de Bock GH. Effectiveness of Colorectal Cancer (CRC) Screening on All-Cause and CRC-Specific Mortality Reduction: A Systematic Review and Meta-Analysis. Cancers. 2023; 15(7):1948. https://doi.org/10.3390/cancers15071948
Chicago/Turabian StyleZheng, Senshuang, Jelle J. A. Schrijvers, Marcel J. W. Greuter, Gürsah Kats-Ugurlu, Wenli Lu, and Geertruida H. de Bock. 2023. "Effectiveness of Colorectal Cancer (CRC) Screening on All-Cause and CRC-Specific Mortality Reduction: A Systematic Review and Meta-Analysis" Cancers 15, no. 7: 1948. https://doi.org/10.3390/cancers15071948
APA StyleZheng, S., Schrijvers, J. J. A., Greuter, M. J. W., Kats-Ugurlu, G., Lu, W., & de Bock, G. H. (2023). Effectiveness of Colorectal Cancer (CRC) Screening on All-Cause and CRC-Specific Mortality Reduction: A Systematic Review and Meta-Analysis. Cancers, 15(7), 1948. https://doi.org/10.3390/cancers15071948







