Mucosal Melanoma Clinical Management and Prognostic Implications: A Retrospective Cohort Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Statistical Analysis
3. Results
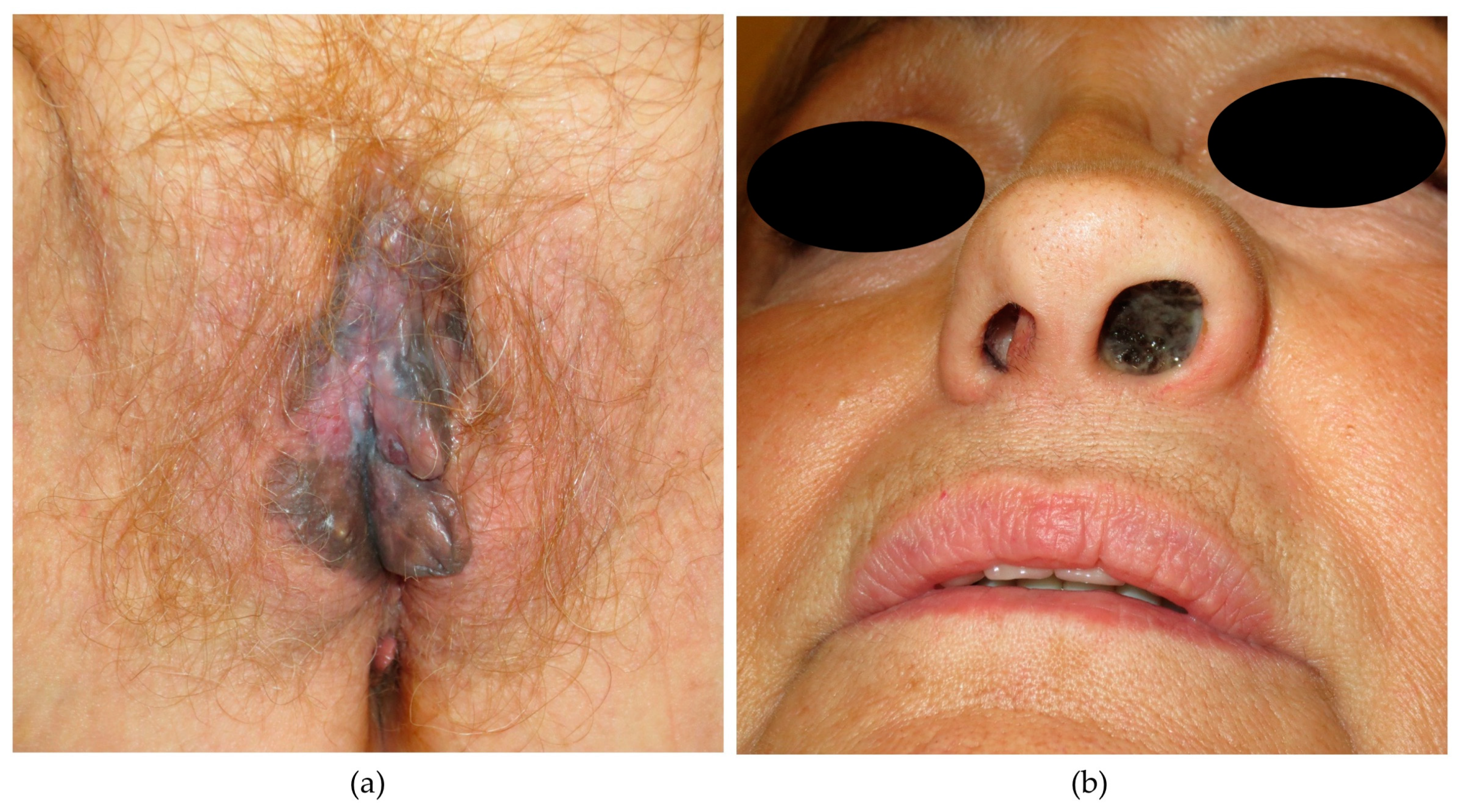
3.1. Characteristics of Patients and Tumors at Baseline
3.2. Breslow and Staging
3.3. Mutations
3.4. Management
3.5. Survival Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MM | mucosal melanoma |
| CM | cutaneous melanoma |
| Inh | Inhibitor |
| RT | Radiotherapy |
| SLNB | selective sentinel lymph node biopsy |
| PET | positron emission tomography |
| CT | computerized tomography |
| MRI | magnetic resonance imaging |
| OS | overall survival |
References
- Olla, D.; Neumeister, M.W. Mucosal Melanoma. Clin. Plast. Surg. 2021, 48, 707–711. [Google Scholar] [PubMed]
- Mihajlovic, M.; Vlajkovic, S.; Jovanovic, P.; Stefanovic, V. Primary mucosal melanomas: A comprehensive review. Int. J. Clin. Exp. Pathol. 2012, 5, 739–753. [Google Scholar] [PubMed]
- Tacastacas, J.D.; Bray, J.; Cohen, Y.K.; Arbesman, J.; Kim, J.; Koon, H.B.; Honda, K.; Cooper, K.D.; Gerstenblith, M.R. Update on primary mucosal melanoma. J. Am. Acad. Dermatol. 2014, 71, 366–375. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.E.; Karnell, L.H.; Menck, H.R. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: A summary of 84,836 cases from the past decade. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer 1998, 83, 1664–1678. [Google Scholar] [CrossRef]
- Ballester, R.; de Unamuno, B.; Navarro, M.; Botella, R. Actualización en melanoma mucoso. Actas Dermo-Sifiliográficas 2015, 106, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Patrick, R.J.; Fenske, N.A.; Messina, J.L. Primary mucosal melanoma. J. Am. Acad. Dermatol. 2007, 56, 828–834. [Google Scholar] [CrossRef] [PubMed]
- Postow, M.A.; Hamid, O.; Carvajal, R.D. Mucosal melanoma: Pathogenesis, clinical behavior, and management. Curr. Oncol. Rep. 2012, 14, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Rawson, R.V.; Wilmott, J.S.; Scolyer, R.A. Mucosal Melanoma: A Review Emphasizing the Molecular Landscape and Implications for Diagnosis and Management. Surg. Pathol. Clin. 2021, 14, 293–307. [Google Scholar] [CrossRef]
- Placa, M.L.; Ambretti, S.; Bonvicini, F.; Venturoli, S.; Bianchi, T.; Varotti, C.; Zerbini, M.; Musiani, M. Presence of high-risk mucosal human papillomavirus genotypes in primary melanoma and in acquired dysplastic melanocytic naevi. Br. J. Dermatol. 2005, 152, 909–914. [Google Scholar] [CrossRef]
- Lundberg, R.; Brytting, M.; Dahlgren, L.; Kanter-Lewensohn, L.; Schloss, L.; Dalianis, T.; Ragnarsson-Olding, B. Human herpes virus DNA is rarely detected in non-UV light-associated primary malignant melanomas of mucous membranes. Anticancer Res. 2006, 26, 3627–3631. [Google Scholar]
- Giraud, G.; Ramqvist, T.; Ragnarsson-Olding, B.; Dalianis, T. DNA from BK virus and JC virus and from KI, WU, and MC polyomaviruses as well as from simian virus 40 is not detected in non-UV-light-associated primary malignant melanomas of mucous membranes. J. Clin. Microbiol. 2008, 46, 3595–3598. [Google Scholar] [CrossRef] [PubMed]
- Holmstrom, M.; Lund, V.J. Malignant melanomas of the nasal cavity after occupational exposure to formaldehyde. Br. J. Ind. Med. 1991, 48, 9–11. [Google Scholar] [CrossRef] [PubMed]
- Axéll, T.; Hedin, C.A. Epidemiologic study of excessive oral melanin pigmentation with special reference to the influence of tobacco habits. Scand. J. Dent. Res. 1982, 90, 434–442. [Google Scholar] [PubMed]
- Yde, S.S.; Sjoegren, P.; Heje, M.; Stolle, L.B. Mucosal Melanoma: A Literature Review. Curr. Oncol. Rep. 2018, 20, 28. [Google Scholar] [CrossRef] [PubMed]
- Curtin, J.A.; Busam, K.; Pinkel, D.; Bastian, B.C. Somatic activation of KIT in distinct subtypes of melanoma. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2006, 24, 4340–4346. [Google Scholar] [CrossRef] [PubMed]
- Beadling, C.; Jacobson-Dunlop, E.; Hodi, F.S.; Le, C.; Warrick, A.; Patterson, J.; Town, A.; Harlow, A.; Cruz, F., III; Azar, S.; et al. KIT gene mutations and copy number in melanoma subtypes. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2008, 14, 6821–6828. [Google Scholar] [CrossRef]
- Spencer, K.R.; Mehnert, J.M. Mucosal Melanoma: Epidemiology, Biology and Treatment. Cancer Treat. Res. 2016, 167, 295–320. [Google Scholar]
- Sutherland, C.M.; Chmiel, J.S.; Henson, D.E.; Winchester, D.P. Patient characteristics, methods of diagnosis, and treatment of mucous membrane melanoma in the United States of America. J. Am. Coll. Surg. 1994, 179, 561–566. [Google Scholar]
- Pandey, M.; Mathew, A.; Abraham, E.K.; Ahamed, I.M.; Nair, K.M. Primary malignant melanoma of the mucous membranes. Eur. J. Surg. Oncol. Br. Assoc. Surg. Oncol. 1998, 24, 303–307. [Google Scholar] [CrossRef]
- Locoregional Mucosal Melanoma: Epidemiology, Clinical Diagnosis, and Treatment—UpToDate [Internet]. Available online: https://www.uptodate.com/contents/locoregional-mucosal-melanoma-epidemiology-clinical-diagnosis-and-treatment?source=mostViewed_widget (accessed on 6 September 2023).
- Heppt, M.V.; Roesch, A.; Weide, B.; Gutzmer, R.; Meier, F.; Loquai, C.; Kähler, K.C.; Gesierich, A.; Meissner, M.; von Bubnoff, D.; et al. Prognostic factors and treatment outcomes in 444 patients with mucosal melanoma. Eur. J. Cancer Oxf. Engl. 2017, 81, 36–44. [Google Scholar] [CrossRef]
- Goldemberg, D.C.; Thuler, L.C.S.; de Melo, A.C. An Update on Mucosal Melanoma: Future Directions. Acta Dermatovenerol. Croat. ADC 2019, 27, 11–115. [Google Scholar] [PubMed]
- Mao, L.; Qi, Z.; Zhang, L.; Guo, J.; Si, L. Immunotherapy in Acral and Mucosal Melanoma: Current Status and Future Directions. Front. Immunol. 2021, 12, 680407. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, C.C.; Wu, X.C.; Jemal, A.; Martin, H.J.; Roche, L.M.; Chen, V.W. Incidence of noncutaneous melanomas in the U.S. Cancer 2005, 103, 1000–1007. [Google Scholar] [CrossRef] [PubMed]
- Cui, C.; Lian, B.; Zhou, L.; Song, X.; Zhang, X.; Wu, D.; Chi, Z.; Si, L.; Sheng, X.; Kong, Y.; et al. Multifactorial Analysis of Prognostic Factors and Survival Rates Among 706 Mucosal Melanoma Patients. Ann. Surg. Oncol. 2018, 25, 2184–2192. [Google Scholar] [CrossRef] [PubMed]
- Altieri, L.; Eguchi, M.; Peng, D.H.; Cockburn, M. Predictors of mucosal melanoma survival in a population-based setting. J. Am. Acad. Dermatol. 2019, 81, 136–142.e2. [Google Scholar] [CrossRef] [PubMed]
- Weinstock, M.A. Malignant melanoma of the vulva and vagina in the United States: Patterns of incidence and population-based estimates of survival. Am. J. Obstet. Gynecol. 1994, 171, 1225–1230. [Google Scholar] [CrossRef] [PubMed]
- Verschraegen, C.F.; Benjapibal, M.; Supakarapongkul, W.; Levy, L.B.; Ross, M.; Atkinson, E.N.; Bodurka-Bevers, D.; Kavanagh, J.J.; Kudelka, A.P.; Legha, S.S. Vulvar melanoma at the M. D. Anderson Cancer Center: 25 years later. Int. J. Gynecol. Cancer Off. J. Int. Gynecol. Cancer Soc. 2001, 11, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Lian, B.; Cui, C.L.; Zhou, L.; Song, X.; Zhang, X.S.; Wu, D.; Si, L.; Chi, Z.H.; Sheng, X.N.; Mao, L.L.; et al. The natural history and patterns of metastases from mucosal melanoma: An analysis of 706 prospectively-followed patients. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2017, 28, 868–873. [Google Scholar] [CrossRef]
- Ottaviano, M.; Giunta, E.F.; Marandino, L.; Tortora, M.; Attademo, L.; Bosso, D.; Cardalesi, C.; Fabbrocini, A.; Rosanova, M.; Silvestri, A.; et al. Anorectal and Genital Mucosal Melanoma: Diagnostic Challenges, Current Knowledge and Therapeutic Opportunities of Rare Melanomas. Biomedicines 2022, 10, 150. [Google Scholar] [CrossRef]
- Carvajal, R.D.; Spencer, S.A.; Lydiatt, W. Mucosal melanoma: A clinically and biologically unique disease entity. J. Natl. Compr. Cancer Netw. 2012, 10, 345–356. [Google Scholar] [CrossRef]
- Femiano, F.; Lanza, A.; Buonaiuto, C.; Gombos, F.; Di Spirito, F.; Cirillo, N. Oral malignant melanoma: A review of the literature. J. Oral. Pathol. Med. Off. Publ. Int. Assoc. Oral. Pathol. Am. Acad. Oral. Pathol. 2008, 37, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Jing, G.; Wu, Y.; Song, H.; Ren, G.; Wang, R.; Guo, W. Primary Malignant Melanoma of the Lip: A Report of 48 Cases. J. Oral. Maxillofac. Surg. Off. J. Am. Assoc. Oral. Maxillofac. Surg. 2015, 73, 2232–2240. [Google Scholar] [CrossRef] [PubMed]
- Eng, V.A.; David, S.P.; Li, S.; Ally, M.S.; Stefanick, M.; Tang, J.Y. The association between cigarette smoking, cancer screening, and cancer stage: A prospective study of the women’s health initiative observational cohort. BMJ Open 2020, 10, e037945. [Google Scholar] [CrossRef] [PubMed]
- Kuk, D.; Shoushtari, A.N.; Barker, C.A.; Panageas, K.S.; Munhoz, R.R.; Momtaz, P.; Ariyan, C.E.; Brady, M.S.; Coit, D.G.; Bogatch, K.; et al. Prognosis of Mucosal, Uveal, Acral, Nonacral Cutaneous, and Unknown Primary Melanoma from the Time of First Metastasis. Oncologist 2016, 21, 848–854. [Google Scholar] [CrossRef]
- Patel, S.G.; Prasad, M.L.; Escrig, M.; Singh, B.; Shaha, A.R.; Kraus, D.H.; Boyle, J.O.; Huvos, A.G.; Busam, K.; Shah, J.P. Primary mucosal malignant melanoma of the head and neck. Head Neck 2002, 24, 247–257. [Google Scholar] [CrossRef]
- Yeh, J.J.; Shia, J.; Hwu, W.J.; Busam, K.J.; Paty, P.B.; Guillem, J.G.; Coit, D.G.; Wong, W.D.; Weiser, M.R. The role of abdominoperineal resection as surgical therapy for anorectal melanoma. Ann. Surg. 2006, 244, 1012–1017. [Google Scholar] [CrossRef]
- Tcheung, W.J.; Selim, M.A.; Herndon, J.E.; Abernethy, A.P.; Nelson, K.C. Clinicopathologic study of 85 cases of melanoma of the female genitalia. J. Am. Acad. Dermatol. 2012, 67, 598–605. [Google Scholar] [CrossRef]
- Chen, F.; Zhang, Q.; Wang, Y.; Wang, S.; Feng, S.; Qi, L.; Li, X.; Ding, C. KIT, NRAS, BRAF and FMNL2 mutations in oral mucosal melanoma and a systematic review of the literature. Oncol. Lett. 2018, 15, 9786–9792. [Google Scholar] [CrossRef]
- Mori, T.; Izumi, T.; Doi, R.; Kamimura, A.; Takai, S.; Teramoto, Y.; Nakamura, Y. Immune checkpoint inhibitor-based therapy for advanced acral and mucosal melanoma. Exp. Dermatol. 2023, 32, 276–289. [Google Scholar] [CrossRef]
- Zhang, S.; Zhang, J.; Guo, J.; Si, L.; Bai, X. Evolving Treatment Approaches to Mucosal Melanoma. Curr. Oncol. Rep. 2022, 24, 1261–1271. [Google Scholar] [CrossRef]
- Thuaire, A.; Nicot, R.; Boileau, M.; Raoul, G.; Descarpentries, C.; Mouawad, F.; Germain, N.; Mortier, L.; Schlund, M. Oral mucosal melanoma—A systematic review. J. Stomatol. Oral. Maxillofac. Surg. 2022, 123, e425–e432. [Google Scholar] [CrossRef] [PubMed]
- Seetharamu, N.; Ott, P.A.; Pavlick, A.C. Mucosal melanomas: A case-based review of the literature. Oncologist 2010, 15, 772–781. [Google Scholar] [CrossRef] [PubMed]
- Grant-Freemantle, M.C.; Lane O’Neill, B.; Clover, A.J.P. The effectiveness of radiotherapy in the treatment of head and neck mucosal melanoma: Systematic review and meta-analysis. Head Neck 2021, 43, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Breik, O.; Sim, F.; Wong, T.; Nastri, A.; Iseli, T.A.; Wiesenfeld, D. Survival Outcomes of Mucosal Melanoma in the Head and Neck: Case Series and Review of Current Treatment Guidelines. J. Oral. Maxillofac. Surg. Off. J. Am. Assoc. Oral. Maxillofac. Surg. 2016, 74, 1859–1871. [Google Scholar] [CrossRef]
- Ma, Y.; Xia, R.; Ma, X.; Judson-Torres, R.L.; Zeng, H. Mucosal Melanoma: Pathological Evolution, Pathway Dependency and Targeted Therapy. Front. Oncol. 2021, 11, 702287. [Google Scholar] [CrossRef]

| Anorectal * (N = 8) | Head and Neck (N = 10) | Vulvovaginal (N = 17) | Total (N = 35) | p-Value | |
|---|---|---|---|---|---|
| Sex | <0.001 | ||||
| Female | 2 (25.0%) | 3 (30.0%) | 17 (100.0%) | 22 (62.9%) | |
| Male | 6 (75.0%) | 7 (70.0%) | 0 (0.0%) | 13 (37.1%) | |
| Age at diagnosis, years | 0.912 | ||||
| Median (Q1, Q3) | 67.5 (59.8, 82.2) | 72.0 (64.5, 80.2) | 68.0 (58.0, 82.0) | 70.0 (60.5, 82.0) | |
| Smoking, ever | 0.173 | ||||
| No | 1 (14.3%) | 5 (55.6%) | 9 (56.2%) | 15 (46.9%) | |
| Yes | 6 (85.7%) | 4 (44.4%) | 7 (43.8%) | 17 (53.1%) | |
| Unknown | 1 | 1 | 1 | 3 | |
| Immunosuppression | 0.126 | ||||
| No | 8 (100.0%) | 8 (80.0%) | 17 (100.0%) | 33 (94.3%) | |
| Yes | 0 (0.0%) | 2 (20.0%) | 0 (0.0%) | 2 (5.7%) | |
| Disease Stage | 0.567 | ||||
| Localized | 2 (25.0%) | 3 (30.0%) | 6 (35.3%) | 11 (31.4%) | |
| Nodal | 2 (25.0%) | 4 (40.0%) | 7 (41.2%) | 13 (37.1%) | |
| Distant | 4 (50.0%) | 3 (30.0%) | 4 (23.5%) | 11 (31.4%) | |
| Breslow depth, mm | 0.324 | ||||
| Median (Q1, Q3) | 10.5 (5.2, 15.0) | 3.0 (1.5, 6.0) | 5.2 (2.5, 8.7) | 5.5 (2.9, 9.0) | |
| Unknown | 4 | 7 | 5 | 16 | |
| Breslow depth, mm | 0.503 | ||||
| Unknown | 4 | 7 | 5 | 16 | |
| <5 mm | 1 (25.0%) | 2 (66.7%) | 4 (33.3%) | 7 (36.8%) | |
| ≥5 mm | 3 (75.0%) | 1 (33.3%) | 8 (66.7%) | 12 (63.2%) | |
| BRAF mutations | 0.784 | ||||
| No | 8 (100.0%) | 8 (88.9%) | 14 (87.5%) | 30 (90.9%) | |
| Yes | 0 (0.0%) | 1 (11.1%) | 2 (12.5%) | 3 (9.1%) | |
| Unknown | 0 | 1 | 1 | 2 | |
| Nodal involvement | 0.625 | ||||
| No | 2 (25.0%) | 5 (50.0%) | 8 (47.1%) | 15 (42.9%) | |
| Yes | 6 (75.0%) | 5 (50.0%) | 9 (52.9%) | 20 (57.1%) | |
| Nodal status assessment technique | 0.628 | ||||
| CT | 1 (16.7%) | 0 (0.0%) | 3 (33.3%) | 4 (20.0%) | |
| MRI | 2 (33.3%) | 1 (20.0%) | 1 (11.1%) | 4 (20.0%) | |
| PET/CT | 3 (50.0%) | 2 (40.0%) | 4 (44.4%) | 9 (45.0%) | |
| SLNB | 0 (0.0%) | 2 (40.0%) | 1 (11.1%) | 3 (15.0%) | |
| Unknown | 2 | 5 | 8 | 15 | |
| Metastasis | 0.453 | ||||
| No | 4 (50.0%) | 7 (70.0%) | 13 (76.5%) | 24 (68.6%) | |
| Yes | 4 (50.0%) | 3 (30.0%) | 4 (23.5%) | 11 (31.4%) | |
| Surgical resection | 0.796 | ||||
| No | 3 (37.5%) | 2 (20.0%) | 5 (29.4%) | 10 (28.6%) | |
| Yes | 5 (62.5%) | 8 (80.0%) | 12 (70.6%) | 25 (71.4%) | |
| Radiotherapy | 0.867 | ||||
| No | 7 (87.5%) | 7 (70.0%) | 13 (76.5%) | 27 (77.1%) | |
| Yes | 1 (12.5%) | 3 (30.0%) | 4 (23.5%) | 8 (22.9%) | |
| Systemic therapy | 0.710 | ||||
| No | 2 (25.0%) | 3 (30.0%) | 7 (41.2%) | 12 (34.3%) | |
| Yes | 6 (75.0%) | 7 (70.0%) | 10 (58.8%) | 23 (65.7%) | |
| Number of systemic treatment lines | 0.935 | ||||
| Median (Q1, Q3) | 1.0 (0.8, 1.2) | 1.0 (0.2, 2.0) | 1.0 (0.0, 3.0) | 1.0 (0.0, 2.0) | |
| Follow-up/survival time, months | 0.095 | ||||
| Median (Q1, Q3) | 12.5 (6.5, 20.8) | 14.0 (6.8, 21.8) | 28.0 (19.0, 55.0) | 21.0 (8.0, 35.0) | |
| Death | 0.247 | ||||
| No | 3 (37.5%) | 1 (10.0%) | 7 (41.2%) | 11 (31.4%) | |
| Yes | 5 (62.5%) | 9 (90.0%) | 10 (58.8%) | 24 (68.6%) |
| Anatomical Site | Treatments Received | ||||
|---|---|---|---|---|---|
| Surgery | RT | Systemic Treatment | |||
| First Line | Second Line | Third Line | |||
| Vulvovaginal | 12/17 (70.6%) | 4/17 (23.5%) | 10/17 (58.9%) Anti-PD-1: 3 (30%) Chemotherapy **: 2 (20%) Anti-PD-1 + LAG-3 inh: 2 (20%) BRAF inh + MEK inh: 1 (10%) Interferon: 1 (10%) Anti-PD-1 + IDO inh: 1 (10%) | 7/17 (41.1%) Anti-CTLA-4: 3 (42.8%) Anti-PD-1: 2 (28.6%) Chemotherapy **: 1 (14.3%) Anti-PD-1 + Anti-CTLA-4: 1 (14.3%) | 5/17 (29.4%) Anti-CTLA-4: 2 (40%) Chemotherapy **: 1 (20%) Pan-RAF inh: 1 (20%) Tyrosine kinase inh (imatinib): 1 (20%) |
| Anorectal *** | 5/8 (62.5%) | 1/8 (12.5%) | 6/8 (75%) Anti-PD-1: 2 (25%) Clinical trial *: 2 (25%) Chemotherapy **: 1 (12.5%) Anti-PD-1 + anti-CTLA-4: 1 (12.5%) | 2/8 (25%) Anti-CTLA-4: 2 (100%) | 0/8 (0%) |
| Head and neck | 8/10 (80%) | 3/10 (30%) | 7/10 (70%) Anti-PD-1: 3 (42.8%) Chemotherapy **: 1 (14.3%) BRAF inh + MEK inh: 1 (14.3%) Anti-PD-1 + LAG-3 inh: 1 (14.3%) Anti-PD-1 + anti-CTLA-4: 1 (14.3%) | 4/10 (40%) Chemotherapy **: 1 (25%) Anti-PD-1: 1 (25%) Anti-CTLA-4: 1 (25%) Clinical trial *: 1 (25%) | 1/10 (10%) Clinical trial *: 1 (100%) |
| Total | 25/35 (71.4%) | 8/35 (22.9%) | 23/35 (65.7%) Anti-PD-1: 8 (34.8%) Chemotherapy **: 4 (17.4%) Anti-PD-1 + LAG-3 inh: 3 (13%) BRAF inh + MEK inh: 2 (8.7%) Clinical trial *: 2 (8.7%) Anti-PD-1 + anti-CTLA-4: 2 (8.7%) Interferon: 1 (4.3%) Anti-PD-1 + IDO inh: 1 (4.3%) | 13/35 (37.1%) Anti-CTLA-4: 6 (46.2%) Anti-PD-1: 3 (23.1%) Chemotherapy **: 2 (15.4%) Anti-PD-1 + anti-CTLA-4: 1 (7.7%) Clinical trial *: 1 (7.7%) | 6/35 (17.1%) Anti-CTLA-4: 2 (33.3%) Chemotherapy **: 1 (16.7%) Pan-RAF inh: 1 (16.7%) Tyrosine kinase inh (imatinib): 1 (16.7%) Clinical trial: 1 (16.7%) |
| Crude Model | Model 1 * | Model 2 ** | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | HR 1 | 95% CI 1 | p-Value | HR 1 | 95% CI 1 | p-Value | HR1 | 95% CI 1 | p-Value |
| Age at diagnosis, 10 y | 0.93 | (0.69, 1.27) | 0.7 | 0.95 | (0.70, 1.29) | 0.7 | 1.41 | (0.93, 2.12) | 0.093 |
| Sex | 0.12 | 0.13 | 0.083 | ||||||
| Female | 1.00 | — | 1.00 | — | 1.00 | — | |||
| Male | 1.94 | (0.85, 4.43) | 0.12 | 1.92 | (0.84, 4.39) | 0.12 | 2.16 | (0.92, 5.05) | 0.076 |
| Anatomical site | 0.15 | 0.5 | 0.7 | ||||||
| Anorectal *** | 1.00 | — | 1.00 | — | 1.00 | — | |||
| Head and Neck | 1.09 | (0.36, 3.34) | 0.9 | 1.10 | (0.35, 3.48) | 0.9 | 1.53 | (0.44, 5.29) | 0.5 |
| Vulvovaginal | 0.47 | (0.15, 1.43) | 0.2 | 0.50 | (0.11, 2.39) | 0.4 | 1.07 | (0.22, 5.31) | >0.9 |
| Surgical resection | 0.044 | 0.013 | 0.2 | ||||||
| No | 1.00 | — | 1.00 | — | 1.00 | — | |||
| Yes | 0.37 | (0.15, 0.93) | 0.035 | 0.25 | (0.08, 0.74) | 0.012 | 0.44 | (0.12, 1.57) | 0.2 |
| Breslow depth, mm | 1.35 | (1.12, 1.63) | <0.001 | 1.47 | (1.14, 1.89) | <0.001 | 1.51 | (1.13, 2.01) | <0.001 |
| Nodal Involvement | 0.008 | <0.001 | |||||||
| No | 1.00 | — | 1.00 | — | |||||
| Yes | 3.23 | (1.29, 8.07) | 0.012 | 7.02 | (2.30, 21.5) | <0.001 | |||
| Metastasis | 0.021 | 0.018 | |||||||
| No | 1.00 | — | 1.00 | — | |||||
| Yes | 3.04 | (1.22, 7.59) | 0.017 | 3.61 | (1.24, 10.5) | 0.018 | |||
| Disease stage | 0.009 | 0.002 | |||||||
| Localized | 1.00 | — | 1.00 | — | |||||
| Nodal | 3.13 | (0.98, 10.0) | 0.055 | 4.92 | (1.41, 17.1) | 0.012 | |||
| Distant | 6.47 | (1.79, 23.5) | 0.004 | 13.2 | (2.82, 62.0) | 0.001 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clavero-Rovira, L.; Gómez-Tomás, Á.; Bassas-Freixas, P.; Bodet, D.; Ferrer, B.; Hernández-Losa, J.; Muñoz-Couselo, E.; Pérez-Benavente, A.; García-Patos, V.; Ferrándiz-Pulido, C. Mucosal Melanoma Clinical Management and Prognostic Implications: A Retrospective Cohort Study. Cancers 2024, 16, 227. https://doi.org/10.3390/cancers16010227
Clavero-Rovira L, Gómez-Tomás Á, Bassas-Freixas P, Bodet D, Ferrer B, Hernández-Losa J, Muñoz-Couselo E, Pérez-Benavente A, García-Patos V, Ferrándiz-Pulido C. Mucosal Melanoma Clinical Management and Prognostic Implications: A Retrospective Cohort Study. Cancers. 2024; 16(1):227. https://doi.org/10.3390/cancers16010227
Chicago/Turabian StyleClavero-Rovira, Laia, Álvaro Gómez-Tomás, Patricia Bassas-Freixas, Domingo Bodet, Berta Ferrer, Javier Hernández-Losa, Eva Muñoz-Couselo, Assumpció Pérez-Benavente, Vicente García-Patos, and Carla Ferrándiz-Pulido. 2024. "Mucosal Melanoma Clinical Management and Prognostic Implications: A Retrospective Cohort Study" Cancers 16, no. 1: 227. https://doi.org/10.3390/cancers16010227
APA StyleClavero-Rovira, L., Gómez-Tomás, Á., Bassas-Freixas, P., Bodet, D., Ferrer, B., Hernández-Losa, J., Muñoz-Couselo, E., Pérez-Benavente, A., García-Patos, V., & Ferrándiz-Pulido, C. (2024). Mucosal Melanoma Clinical Management and Prognostic Implications: A Retrospective Cohort Study. Cancers, 16(1), 227. https://doi.org/10.3390/cancers16010227






