Hepatocellular Carcinoma: Beyond the Border of Advanced Stage Therapy
Abstract
:Simple Summary
Abstract
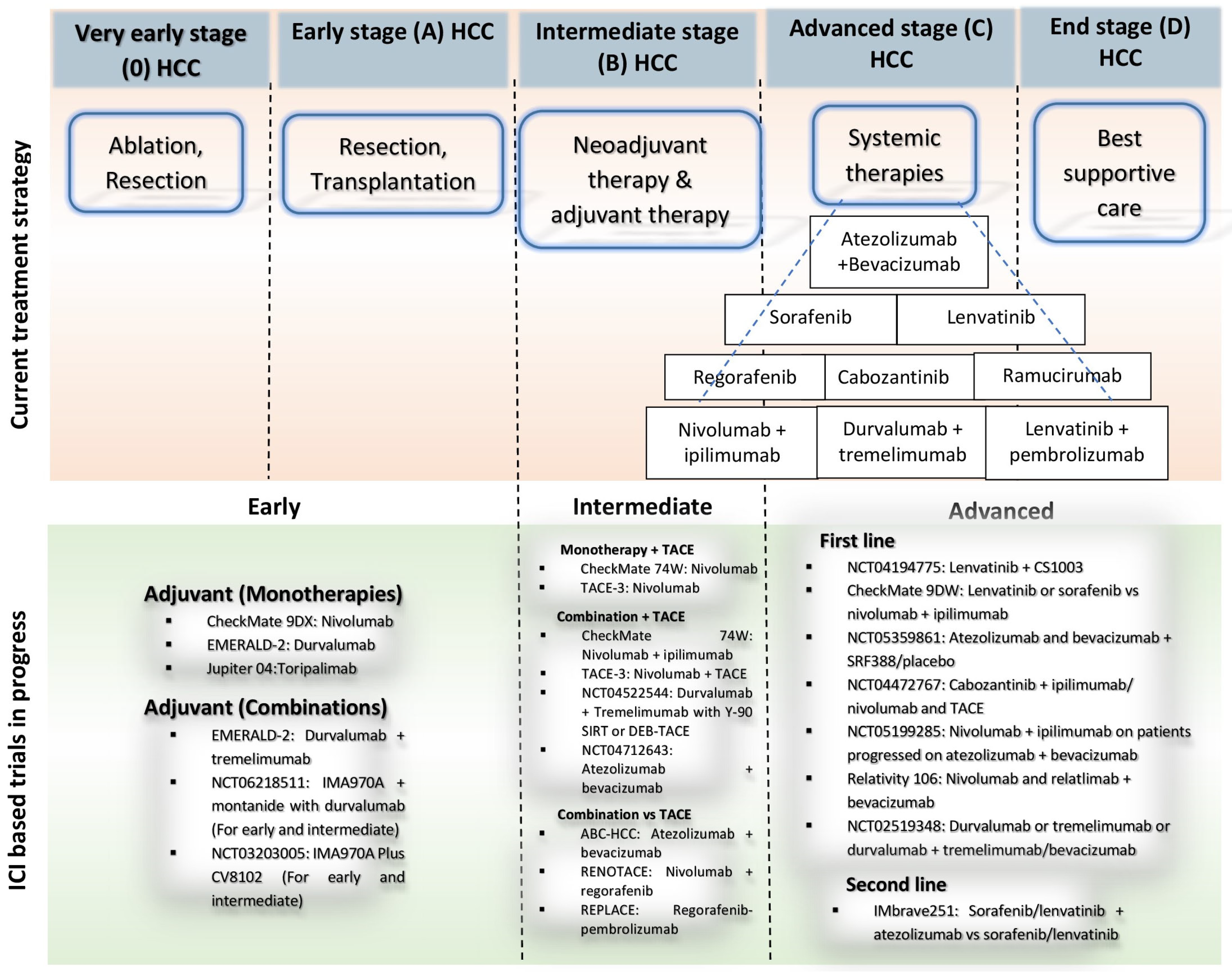
1. Introduction
2. Emerging Therapeutic Options for HCC Therapy
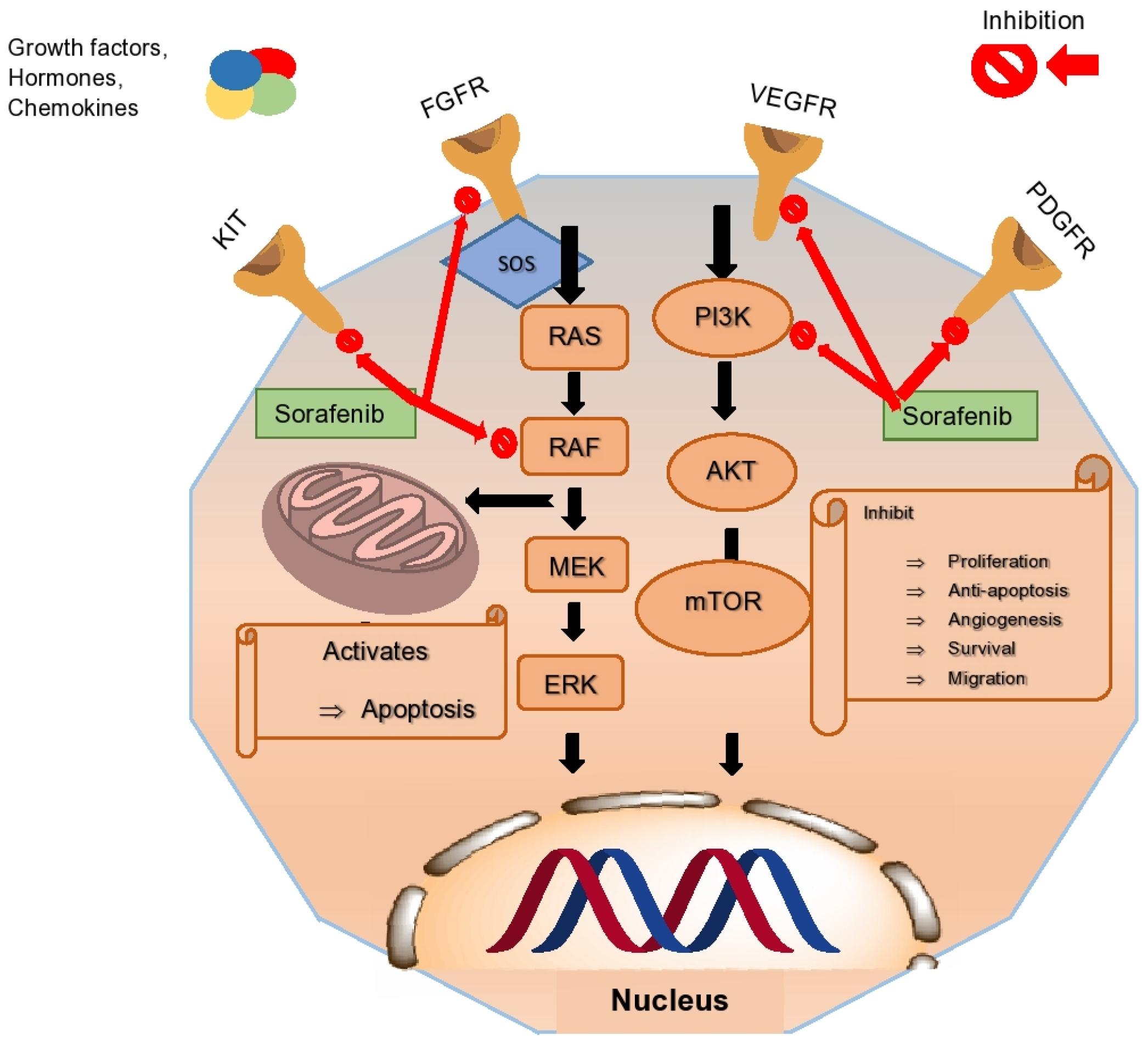
2.1. Multikinase Inhibitors
2.1.1. Sorafenib
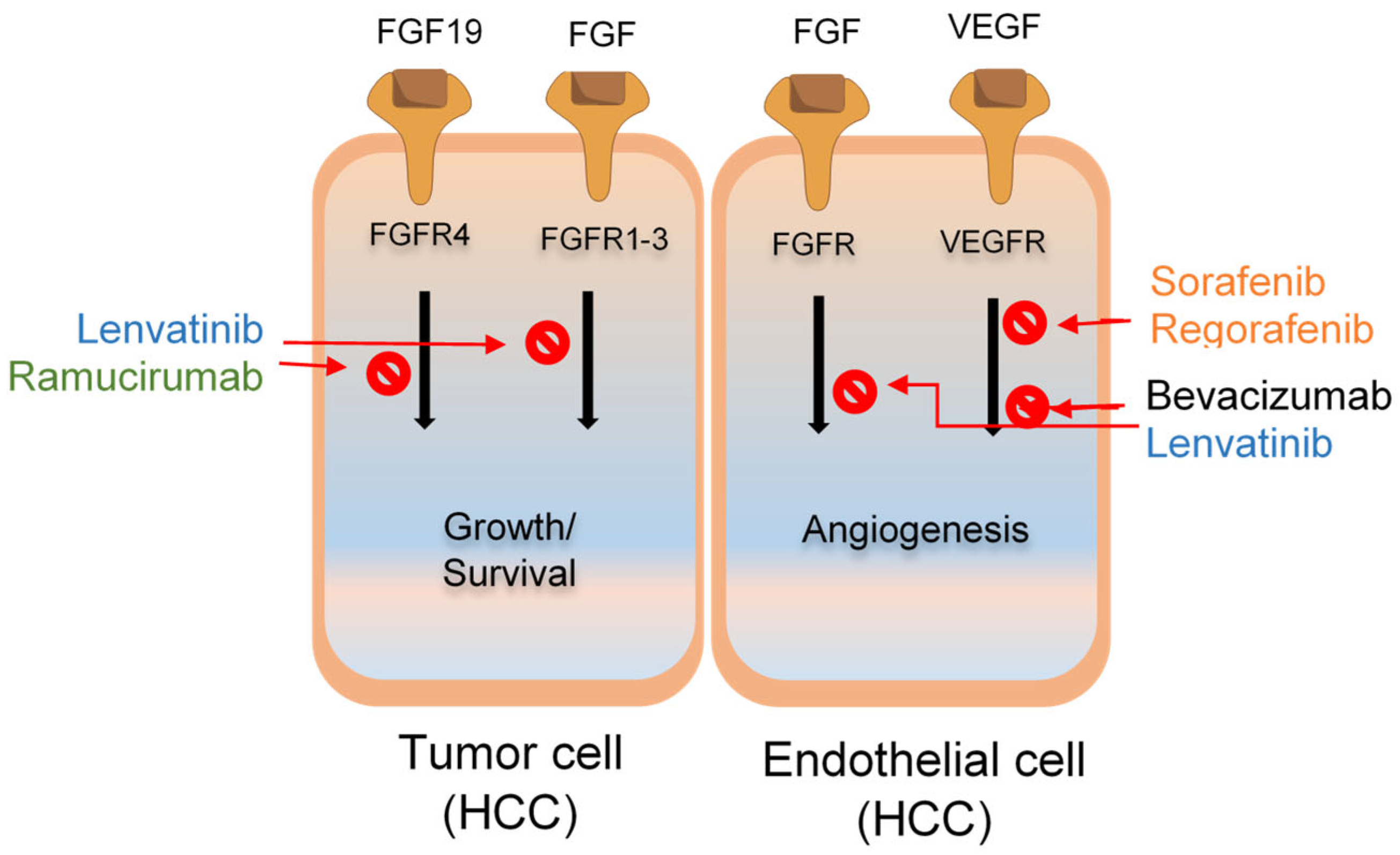
2.1.2. Lenvatinib
2.1.3. Regorafenib
2.2. Tyrosine Kinase Inhibitors
Cabozantinib
2.3. Angiogenesis Inhibitors
2.3.1. Ramucirumab
2.3.2. Atezolizumab and Bevacizumab
2.4. Immune Checkpoint Inhibitors (ICIs)
2.4.1. Nivolumab
2.4.2. Pembrolizumab
2.4.3. Nivolumab and Ipilimumab
2.4.4. Durvalumab and Tremelimumab
3. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Acharya, P.; Chouhan, K.; Weiskirchen, S.; Weiskirchen, R. Cellular mechanisms of liver fibrosis. Front. Pharmacol. 2021, 12, 671640. [Google Scholar] [CrossRef]
- Jiang, Y.; Que, W.; Zhu, P.; Li, X.-K. The role of diverse liver cells in liver transplantation tolerance. Front. Immunol. 2020, 11, 1203. [Google Scholar] [CrossRef] [PubMed]
- Flores, A.; Marrero, J.A. Emerging trends in hepatocellular carcinoma: Focus on diagnosis and therapeutics. Clin. Med. Insights Oncol. 2014, 8, CMO-S9926. [Google Scholar] [CrossRef] [PubMed]
- El-Serag, H.B.; Balakrishnan, M.; Natarajan, Y. Epidemiology and Risk Factors of Hepatocellular Carcinoma. J. Gastrointest. Oncol. 2024, 250–263. [Google Scholar]
- Couri, T.; Pillai, A. Goals and targets for personalized therapy for HCC. Hepatol. Int. 2019, 13, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.; Cho, K.; Shin, S.; Kim, D.Y.; Han, K.-H.; Ro, S.W. High risk of hepatocellular carcinoma development in fibrotic liver: Role of the hippo-YAP/TAZ signaling pathway. Int. J. Mol. Sci. 2019, 20, 581. [Google Scholar] [CrossRef] [PubMed]
- Ramadori, P.; Cubero, F.J.; Liedtke, C.; Trautwein, C.; Nevzorova, Y.A. Alcohol and hepatocellular carcinoma: Adding fuel to the flame. Cancer 2017, 9, 130. [Google Scholar] [CrossRef] [PubMed]
- Zuo, Q.; Park, N.H.; Lee, J.K.; Santaliz-Casiano, A.; Madak-Erdogan, Z. Navigating nonalcoholic fatty liver disease (NAFLD): Exploring the roles of estrogens, pharmacological and medical interventions, and life style. Steroid 2024, 203, 109330. [Google Scholar] [CrossRef] [PubMed]
- Benkerroum, N. Chronic and acute toxicities of aflatoxins: Mechanisms of action. Int. J. Environ. Health Res. 2020, 17, 423. [Google Scholar] [CrossRef]
- Jinjuvadia, R.; Patel, S.; Liangpunsakul, S. The association between metabolic syndrome and hepatocellular carcinoma: Systemic review and meta-analysis. J. Clin. Gastroenterol. 2014, 48, 172–177. [Google Scholar] [CrossRef]
- Hirai, M.; Kinugasa, H.; Nouso, K.; Yamamoto, S.; Terasawa, H.; Onishi, Y.; Oyama, A.; Adachi, T.; Wada, N.; Sakata, M. Prediction of the prognosis of advanced hepatocellular carcinoma by TERT promoter mutations in circulating tumor DNA. J. Gastroenterol. Hepatol. 2021, 36, 1118–1125. [Google Scholar] [CrossRef]
- Seto, W.-K.; Lo, Y.-R.; Pawlotsky, J.-M.; Yuen, M.-F. Chronic hepatitis B virus infection. Lancet 2018, 392, 2313–2324. [Google Scholar] [CrossRef] [PubMed]
- Bousali, M.; Papatheodoridis, G.; Paraskevis, D.; Karamitros, T. Hepatitis B virus DNA integration, chronic infections and hepatocellular carcinoma. Microorganisms 2021, 9, 1787. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.A. Biochemical and Molecular Role of Microorganisms in Disease Progression and Current Impact on Health Conditions. Saudi J. Pathol. Microbiol. 2021, 6, 156–162. [Google Scholar]
- Chen, Z.; Xie, H.; Hu, M.; Huang, T.; Hu, Y.; Sang, N.; Zhao, Y. Recent progress in treatment of hepatocellular carcinoma. Am. J. Cancer Res. 2020, 10, 2993. [Google Scholar]
- Luo, X.-Y.; Wu, K.-M.; He, X.-X. Advances in drug development for hepatocellular carcinoma: Clinical trials and potential therapeutic targets. J. Exp. Clin. Cancer Res. 2021, 40, 172. [Google Scholar] [CrossRef]
- Vitale, A.; Cabibbo, G.; Iavarone, M.; Viganò, L.; Pinato, D.J.; Ponziani, F.R.; Lai, Q.; Casadei-Gardini, A.; Celsa, C.; Galati, G. Personalised management of patients with hepatocellular carcinoma: A multiparametric therapeutic hierarchy concept. Lancet Oncol. 2023, 24, e312–e322. [Google Scholar] [CrossRef] [PubMed]
- Hsueh, K.-C.; Lee, T.-Y.; Kor, C.-T.; Chen, T.-M.; Chang, T.-M.; Yang, S.-F.; Hsieh, C.-B. The role of liver transplantation or resection for patients with early hepatocellular carcinoma. Tumor Biol. 2016, 37, 4193–4201. [Google Scholar] [CrossRef]
- Facciorusso, A.; Di Maso, M.; Muscatiello, N. Microwave ablation versus radiofrequency ablation for the treatment of hepatocellular carcinoma: A systematic review and meta-analysis. Int. J. Hyperthermia. 2016, 32, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Mourad, S.N.; De la Garza-Ramos, C.; Toskich, B.B. Radiation Segmentectomy for the Treatment of Hepatocellular Carcinoma: A Practical Review of Evidence. Cancer 2024, 16, 669. [Google Scholar] [CrossRef]
- Izzo, F.; Granata, V.; Grassi, R.; Fusco, R.; Palaia, R.; Delrio, P.; Carrafiello, G.; Azoulay, D.; Petrillo, A.; Curley, S.A. Radiofrequency ablation and microwave ablation in liver tumors: An update. Oncologist 2019, 24, e990–e1005. [Google Scholar] [CrossRef]
- Akateh, C.; Black, S.M.; Conteh, L.; Miller, E.D.; Noonan, A.; Elliott, E.; Pawlik, T.M.; Tsung, A.; Cloyd, J.M. Neoadjuvant and adjuvant treatment strategies for hepatocellular carcinoma. World J. Gastroenterol. 2019, 25, 3704. [Google Scholar] [CrossRef]
- Marron, T.U.; Fiel, M.I.; Hamon, P.; Fiaschi, N.; Kim, E.; Ward, S.C.; Zhao, Z.; Kim, J.; Kennedy, P.; Gunasekaran, G. Neoadjuvant cemiplimab for resectable hepatocellular carcinoma: A single-arm, open-label, phase 2 trial. Lancet Gastroenterol. Hepatol. 2022, 7, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Woei-A-Jin, F.S.H.; Weijl, N.I.; Burgmans, M.C.; Fariña Sarasqueta, A.; Tom van Wezel, J.; Wasser, M.N.; Coenraad, M.J.; Burggraaf, J.; Osanto, S. Neoadjuvant treatment with angiogenesis-inhibitor dovitinib prior to local therapy in hepatocellular carcinoma: A phase II study. Oncologist 2021, 26, 854–864. [Google Scholar] [CrossRef]
- Kaseb, A.O.; Vence, L.; Blando, J.; Yadav, S.S.; Ikoma, N.; Pestana, R.C.; Vauthey, J.N.; Allison, J.P.; Sharma, P. Immunologic correlates of pathologic complete response to preoperative immunotherapy in hepatocellular carcinoma. Cancer Immunol. Res. 2019, 7, 1390–1395. [Google Scholar] [CrossRef]
- Sansonno, D.; Lauletta, G.; Russi, S.; Conteduca, V.; Sansonno, L.; Dammacco, F. Transarterial chemoembolization plus sorafenib: A sequential therapeutic scheme for HCV-related intermediate-stage hepatocellular carcinoma: A randomized clinical trial. Oncologist 2012, 17, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Qin, S.; Chan, S.L.; Gu, S.; Bai, Y.; Ren, Z.; Lin, X.; Chen, Z.; Jia, W.; Jin, Y.; Guo, Y. Camrelizumab plus rivoceranib versus sorafenib as first-line therapy for unresectable hepatocellular carcinoma (CARES-310): A randomised, open-label, international phase 3 study. Lancet 2023, 402, 1133–1146. [Google Scholar] [CrossRef] [PubMed]
- Meriggi, F.; Graffeo, M. Clinical characterisation and management of the main treatment-induced toxicities in patients with hepatocellular carcinoma and cirrhosis. Cancer 2021, 13, 584. [Google Scholar] [CrossRef]
- Ramos-Casals, M.; Brahmer, J.R.; Callahan, M.K.; Flores-Chávez, A.; Keegan, N.; Khamashta, M.A.; Lambotte, O.; Mariette, X.; Prat, A.; Suárez-Almazor, M.E. Immune-related adverse events of checkpoint inhibitors. Nat. Rev. Dis. 2020, 6, 38. [Google Scholar] [CrossRef]
- Ghaziani, T.T.; Dhanasekaran, R. Recent progress in systemic therapy for hepatocellular cancer (HCC). Curr. Treat. Options Gastroenterol. 2021, 19, 351–368. [Google Scholar] [CrossRef]
- Sangro, B.; Chan, S.L.; Meyer, T.; Reig, M.; El-Khoueiry, A.; Galle, P.R. Diagnosis and management of toxicities of immune checkpoint inhibitors in hepatocellular carcinoma. J. Hepatol. 2020, 72, 320–341. [Google Scholar] [CrossRef] [PubMed]
- Munir, B.; Ahmed, B.; Kiran, S.; Jalal, F.; Zahoor, M.K.; Shehzadi, S.; Oranab, S.; Kamran, S.K.; Ghaffar, A. Sorafenib tosylate, Ribavirn and Sofosbuvir combination therapy for HCV virus infected patients with decompensated liver cancer. Pak. J. Pharm. Sci. 2017, 30, 2383–2387. [Google Scholar] [PubMed]
- Mushtaq, H.; Zarlashat, Y.; Ambreen, A.; Mujahid, M.; Kausar, S.; Shafqat, D. Reviewing advances in understanding and targeting the MAPK signaling pathway in hepatocellular carcinoma progression and therapeutics. Agrobiol. Rec. 2024, 15, 103–116. [Google Scholar]
- Matter, M.S.; Decaens, T.; Andersen, J.B.; Thorgeirsson, S.S. Targeting the mTOR pathway in hepatocellular carcinoma: Current state and future trends. J. Hepatol. 2014, 60, 855–865. [Google Scholar] [CrossRef]
- Ziogas, I.A.; Tsoulfas, G. Evolving role of Sorafenib in the management of hepatocellular carcinoma. World J. Clin. Oncol. 2017, 8, 203. [Google Scholar] [CrossRef] [PubMed]
- Zhai, B.; Sun, X.-Y. Mechanisms of resistance to sorafenib and the corresponding strategies in hepatocellular carcinoma. World J. Hepatol. 2013, 5, 345. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.-L.; Kang, Y.-K.; Chen, Z.; Tsao, C.-J.; Qin, S.; Kim, J.S.; Luo, R.; Feng, J.; Ye, S.; Yang, T.-S. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: A phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009, 10, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Cabral, L.K.D.; Tiribelli, C.; Sukowati, C.H. Sorafenib resistance in hepatocellular carcinoma: The relevance of genetic heterogeneity. Cancer 2020, 12, 1576. [Google Scholar] [CrossRef] [PubMed]
- Assenat, E.; Pageaux, G.-P.; Thézenas, S.; Peron, J.-M.; Bécouarn, Y.; Seitz, J.-F.; Merle, P.; Blanc, J.-F.; Bouché, O.; Ramdani, M. Sorafenib alone vs. sorafenib plus GEMOX as 1st-line treatment for advanced HCC: The phase II randomised PRODIGE 10 trial. Brit. J. Cancer 2019, 120, 896–902. [Google Scholar] [CrossRef]
- Abou-Alfa, G.K.; Shi, Q.; Knox, J.J.; Kaubisch, A.; Niedzwiecki, D.; Posey, J.; Tan, B.R.; Kavan, P.; Goel, R.; Lammers, P.E. Assessment of treatment with sorafenib plus doxorubicin vs sorafenib alone in patients with advanced hepatocellular carcinoma: Phase 3 CALGB 80802 randomized clinical trial. JAMA Oncol. 2019, 5, 1582–1588. [Google Scholar] [CrossRef]
- Islam, M.R.; Rahman, M.S.; Amin, M.A.; Alam, A.R.U.; Siddique, M.A.; Sultana, M.; Hossain, M.A. Evidence of combined effect of amino acid substitutions within G-H and B-C loops of VP1 conferring serological heterogeneity in foot-and-mouth disease virus serotype A. Transbound. Emerg. Dis. 2021, 68, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Matsuki, M.; Hoshi, T.; Yamamoto, Y.; Ikemori-Kawada, M.; Minoshima, Y.; Funahashi, Y.; Matsui, J. Lenvatinib inhibits angiogenesis and tumor fibroblast growth factor signaling pathways in human hepatocellular carcinoma models. Cancer Med. 2018, 7, 2641–2653. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Zhang, Y.-N.; Wang, K.-T.; Chen, L. Lenvatinib for hepatocellular carcinoma: From preclinical mechanisms to anti-cancer therapy. Biochim. Biophys. Acta 2020, 1874, 188391. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M. Lenvatinib may drastically change the treatment landscape of hepatocellular carcinoma. Liver Cancer 2018, 7, 1–19. [Google Scholar] [CrossRef]
- Guo, J.; Zhao, J.; Xu, Q.; Huang, D. Resistance of lenvatinib in hepatocellular carcinoma. Curr. Cancer Drug Targets 2022, 22, 865–878. [Google Scholar] [PubMed]
- Al-Salama, Z.T.; Syed, Y.Y.; Scott, L.J. Lenvatinib: A review in hepatocellular carcinoma. Drugs 2019, 79, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Facciorusso, A.; Tartaglia, N.; Villani, R.; Serviddio, G.; Ramai, D.; Mohan, B.P.; Chandan, S.; Abd El Aziz, M.A.; Evangelista, J.; Cotsoglou, C. Lenvatinib versus sorafenib as first-line therapy of advanced hepatocellular carcinoma: A systematic review and meta-analysis. Am. J. Transl. Res. 2021, 13, 2379. [Google Scholar] [PubMed]
- Qiao, Q.; Han, C.; Ye, S.; Li, J.; Shao, G.; Bai, Y.; Xu, A.; Sun, M.; Wang, W.; Wu, J. The efficacy and safety of cadonilimab combined with lenvatinib for first-line treatment of advanced hepatocellular carcinoma (COMPASSION-08): A phase Ib/II single-arm clinical trial. Front. Immunol. 2023, 14, 1238667. [Google Scholar] [CrossRef]
- Peng, Z.; Fan, W.; Zhu, B.; Wang, G.; Sun, J.; Xiao, C.; Huang, F.; Tang, R.; Cheng, Y.; Huang, Z. Lenvatinib combined with transarterial chemoembolization as first-line treatment for advanced hepatocellular carcinoma: A phase III, randomized clinical trial (LAUNCH). J. Clin. Oncol. 2023, 41, 117–127. [Google Scholar] [CrossRef]
- Kudo, M.; Finn, R.S.; Qin, S.; Han, K.-H.; Ikeda, K.; Piscaglia, F.; Baron, A.; Park, J.-W.; Han, G.; Jassem, J. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: A randomised phase 3 non-inferiority trial. Lancet 2018, 391, 1163–1173. [Google Scholar] [CrossRef]
- Finn, R.; Kudo, M.; Merle, P.; Meyer, T.; Qin, S.; Ikeda, M.; Xu, R.; Edeline, J.; Ryoo, B.; Ren, Z. LBA34 Primary results from the phase III LEAP-002 study: Lenvatinib plus pembrolizumab versus lenvatinib as first-line (1L) therapy for advanced hepatocellular carcinoma (aHCC). Ann. Oncol. 2022, 33, S1401. [Google Scholar] [CrossRef]
- Granito, A.; Forgione, A.; Marinelli, S.; Renzulli, M.; Ielasi, L.; Sansone, V.; Benevento, F.; Piscaglia, F.; Tovoli, F. Experience with regorafenib in the treatment of hepatocellular carcinoma. Therap. Adv. Gastroenterol. 2021, 14, 17562848211016959. [Google Scholar] [CrossRef] [PubMed]
- Heo, Y.-A.; Syed, Y.Y. Regorafenib: A review in hepatocellular carcinoma. Drugs 2018, 78, 951–958. [Google Scholar] [CrossRef] [PubMed]
- El-Hanboshy, S.M.; Helmy, M.W.; Abd-Alhaseeb, M.M. Catalpol synergistically potentiates the anti-tumour effects of regorafenib against hepatocellular carcinoma via dual inhibition of PI3K/Akt/mTOR/NF-κB and VEGF/VEGFR2 signaling pathways. Mol. Biol. Rep. 2021, 48, 7233–7242. [Google Scholar] [CrossRef] [PubMed]
- Moradi, M.; Mousavi, A.; Emamgholipour, Z.; Giovannini, J.; Moghimi, S.; Peytam, F.; Honarmand, A.; Bach, S.; Foroumadi, A. Quinazoline-based VEGFR-2 inhibitors as potential anti-angiogenic agents: A contemporary perspective of SAR and molecular docking studies. Eur. J. Med. Chem. 2023, 259, 115626. [Google Scholar] [CrossRef] [PubMed]
- Finn, R.S.; Merle, P.; Granito, A.; Huang, Y.-H.; Bodoky, G.; Pracht, M.; Yokosuka, O.; Rosmorduc, O.; Gerolami, R.; Caparello, C. Outcomes of sequential treatment with sorafenib followed by regorafenib for HCC: Additional analyses from the phase III RESORCE trial. J. Hepatol. 2018, 69, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Bruix, J.; Qin, S.; Merle, P.; Granito, A.; Huang, Y.-H.; Bodoky, G.; Pracht, M.; Yokosuka, O.; Rosmorduc, O.; Breder, V. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017, 389, 56–66. [Google Scholar] [CrossRef]
- Yoo, C.; Cheon, J.; Ryoo, B.-Y.; Ryu, M.-H.; Kim, H.-D.; Kim, K.-P.; Kang, B.; Chon, H.J.; Finn, R.S. Second-line regorafenib in patients (pts) with unresectable hepatocellular carcinoma (uHCC) after progression on first-line atezolizumab plus bevacizumab (Atezo-Bev): Phase 2 REGONEXT trial. Am. Soc. Clin. Oncol. 2024, 42, 477. [Google Scholar] [CrossRef]
- Ren, S.-H.; Cui, Z.-L.; Lang, M.-R.; Li, Q.; Zhang, W.; Fang, F.; Wu, Q.; Cui, Y.-L.; Li, H.-K.; Chen, P. Efficacy and safety of sequential therapy with sorafenib and regorafenib for advanced hepatocellular carcinoma: A two-center study in China. J. Gastrointest. Oncol. 2022, 13, 1266. [Google Scholar] [CrossRef]
- Chan, S.L.; Ryoo, B.-Y.; Mo, F.; Cheon, J.; Li, L.; Wong, K.H.; Yim, N.; Kim, H.; Yoo, C. A phase II clinical trial to study the use of cabozantinib (cabo) in patients with hepatocellular carcinoma (HCC) post immunotherapy treatment. Am. Soc. Clin. Oncol. 2023, 41, 571. [Google Scholar] [CrossRef]
- Zhu, A.X.; Park, J.O.; Ryoo, B.-Y.; Yen, C.-J.; Poon, R.; Pastorelli, D.; Blanc, J.-F.; Chung, H.C.; Baron, A.D.; Pfiffer, T.E.F. Ramucirumab versus placebo as second-line treatment in patients with advanced hepatocellular carcinoma following first-line therapy with sorafenib (REACH): A randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2015, 16, 859–870. [Google Scholar] [CrossRef] [PubMed]
- El-Khoueiry, A.B.; Yau, T.; Kang, Y.-K.; Kim, T.-Y.; Santoro, A.; Sangro, B.; Melero, I.; Kudo, M.; Hou, M.-M.; Matilla, A. Nivolumab (NIVO) plus ipilimumab (IPI) combination therapy in patients (Pts) with advanced hepatocellular carcinoma (aHCC): Long-term results from CheckMate 040. Am. Soc. Clin. Oncol. 2021, 39, 269. [Google Scholar] [CrossRef]
- Qin, S.; Chen, Z.; Fang, W.; Ren, Z.; Xu, R.; Ryoo, B.-Y.; Meng, Z.; Bai, Y.; Chen, X.; Liu, X. Pembrolizumab versus placebo as second-line therapy in patients from Asia with advanced hepatocellular carcinoma: A randomized, double-blind, phase III trial. J. Clin. Oncol. 2023, 41, 1434. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.-L.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Lim, H.Y.; Kudo, M.; Breder, V.; Merle, P. Updated efficacy and safety data from IMbrave150: Atezolizumab plus bevacizumab vs. sorafenib for unresectable hepatocellular carcinoma. J. Hepatol. 2022, 76, 862–873. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Qin, S.; Sun, H.-C. An open-label, multi-center phase IIIb study of durvalumab and tremelimumab as first-line treatment in patients with unresectable hepatocellular carcinoma (TREMENDOUS study). Am. Soc. Clin. Oncol. 2023, 41, TPS628. [Google Scholar] [CrossRef]
- Rimassa, L.; Kelley, R.K.; Meyer, T.; Ryoo, B.-Y.; Merle, P.; Park, J.-W.; Blanc, J.-F.; Lim, H.Y.; Tran, A.; Chan, Y.-W. Outcomes based on plasma biomarkers for the phase 3 CELESTIAL trial of cabozantinib versus placebo in advanced hepatocellular carcinoma. Liver Cancer 2022, 11, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Xia, M.; Jin, K.; Wang, S.; Wei, H.; Fan, C.; Wu, Y.; Li, X.; Li, X.; Li, G. Function of the c-Met receptor tyrosine kinase in carcinogenesis and associated therapeutic opportunities. Mol. Cancer 2018, 17, 45. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Rao, B.; Lou, J.; Li, J.; Liu, Z.; Li, A.; Cui, G.; Ren, Z.; Yu, Z. The function of the HGF/c-Met axis in hepatocellular carcinoma. Front. Cell Dev. Biol. 2020, 8, 55. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Q.; Chen, W.; Ren, M.; Wang, J.; Zhang, H.; Deng, D.Y.; Zhang, L.; Shang, C.; Chen, Y. Cabozantinib Suppresses Tumor Growth and Metastasis in Hepatocellular Carcinoma by a Dual Blockade of VEGFR2 and METAntitumor Activity of Cabozantinib in HCC. Clin. Cancer Res. 2014, 20, 2959–2970. [Google Scholar] [CrossRef]
- Liao, W.; Huang, J.; Hutton, D.; Zhu, G.; Wu, Q.; Wen, F.; Bai, L.; Li, Q. Cost-effectiveness analysis of cabozantinib as second-line therapy in advanced hepatocellular carcinoma. Liver Int. 2019, 39, 2408–2416. [Google Scholar] [CrossRef]
- Kelley, R.; Ryoo, B.-Y.; Merle, P.; Park, J.-W.; Bolondi, L.; Chan, S.L.; Lim, H.; Baron, A.D.; Parnis, F.; Knox, J. Second-line cabozantinib after sorafenib treatment for advanced hepatocellular carcinoma: A subgroup analysis of the phase 3 CELESTIAL trial. ESMO Open 2020, 5, e000714. [Google Scholar] [CrossRef] [PubMed]
- De Luca, E.; Marino, D.; Di Maio, M. Ramucirumab, a second-line option for patients with hepatocellular carcinoma: A review of the evidence. Cancer Manag. Res. 2020, 3721–3729. [Google Scholar] [CrossRef] [PubMed]
- Galle, P.R.; Foerster, F.; Kudo, M.; Chan, S.L.; Llovet, J.M.; Qin, S.; Schelman, W.R.; Chintharlapalli, S.; Abada, P.B.; Sherman, M. Biology and significance of alpha-fetoprotein in hepatocellular carcinoma. Liver Internat. 2019, 39, 2214–2229. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.M.; Singal, A.G.; Villanueva, A.; Finn, R.S.; Kudo, M.; Galle, P.R.; Ikeda, M.; Callies, S.; McGrath, L.M.; Wang, C. Prognostic and predictive factors in patients with advanced HCC and elevated alpha-fetoprotein treated with ramucirumab in two randomized phase III trials. Clin. Cancer Res. 2022, 28, 2297–2305. [Google Scholar] [CrossRef] [PubMed]
- Zhu, A.X.; Kang, Y.-K.; Yen, C.-J.; Finn, R.S.; Galle, P.R.; Llovet, J.M.; Assenat, E.; Brandi, G.; Pracht, M.; Lim, H.Y. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019, 20, 282–296. [Google Scholar] [CrossRef] [PubMed]
- Kasuya, K.; Kawamura, Y.; Kobayashi, M.; Shindoh, J.; Kobayashi, Y.; Kajiwara, A.; Iritani, S.; Fujiyama, S.; Hosaka, T.; Saitoh, S. Efficacy and safety of ramucirumab in patients with unresectable hepatocellular carcinoma with progression after treatment with lenvatinib. Intern. Med. 2021, 60, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Zhu, A.X.; Guan, Y.; Abbas, A.R.; Koeppen, H.; Lu, S.; Hsu, C.-H.; Lee, K.-H.; Lee, M.S.; He, A.R.; Mahipal, A. Abstract CT044: Genomic correlates of clinical benefits from atezolizumab combined with bevacizumab vs. atezolizumab alone in patients with advanced hepatocellular carcinoma (HCC). Cancer Res. 2020, 80, CT044. [Google Scholar] [CrossRef]
- Pishvaian, M.; Lee, M.; Ryoo, B.-Y.; Stein, S.; Lee, K.-H.; Verret, W.; Spahn, J.; Shao, H.; Liu, B.; Iizuka, K. Updated safety and clinical activity results from a phase Ib study of atezolizumab+ bevacizumab in hepatocellular carcinoma (HCC). Ann. Oncol. 2018, 29, viii718–viii719. [Google Scholar] [CrossRef]
- Finn, R.S.; Zhu, A.X. Targeting angiogenesis in hepatocellular carcinoma: Focus on VEGF and bevacizumab. Expert Rev. Anticancer Ther. 2009, 9, 503–509. [Google Scholar] [CrossRef]
- Garufi, C.; Mancuso, A. Hepatocellular Carcinoma Medical Therapy. In Hepatocellular Carcinoma; Springer: Berlin/Heidelberg, Germany, 2023; pp. 173–179. [Google Scholar]
- Kudo, M. Changing the treatment paradigm for hepatocellular carcinoma using atezolizumab plus bevacizumab combination therapy. Cancer 2021, 13, 5475. [Google Scholar] [CrossRef]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Tai, D.; Yip, C.; Choo, S.P.; Chew, V. Combinational immunotherapy for hepatocellular carcinoma: Radiotherapy, immune checkpoint blockade and beyond. Front. Immunol. 2020, 11, 568759. [Google Scholar] [CrossRef] [PubMed]
- Di Federico, A.; Rizzo, A.; Carloni, R.; De Giglio, A.; Bruno, R.; Ricci, D.; Brandi, G. Atezolizumab-bevacizumab plus Y-90 TARE for the treatment of hepatocellular carcinoma: Preclinical rationale and ongoing clinical trials. Expert. Opin. Investig. Drug 2022, 31, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Langhans, B.; Nischalke, H.D.; Krämer, B.; Dold, L.; Lutz, P.; Mohr, R.; Vogt, A.; Toma, M.; Eis-Hübinger, A.M.; Nattermann, J. Role of regulatory T cells and checkpoint inhibition in hepatocellular carcinoma. Cancer Immunol. Immunother. 2019, 68, 2055–2066. [Google Scholar] [CrossRef] [PubMed]
- Finkelmeier, F.; Waidmann, O.; Trojan, J. Nivolumab for the treatment of hepatocellular carcinoma. Expert Rev. Anticancer Ther. 2018, 18, 1169–1175. [Google Scholar] [CrossRef] [PubMed]
- Finkelmeier, F.; Canli, Ö.; Tal, A.; Pleli, T.; Trojan, J.; Schmidt, M.; Kronenberger, B.; Zeuzem, S.; Piiper, A.; Greten, F.R. High levels of the soluble programmed death-ligand (sPD-L1) identify hepatocellular carcinoma patients with a poor prognosis. Eur. J. Cancer 2016, 59, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Pang, K.; Shi, Z.-D.; Wei, L.-Y.; Dong, Y.; Ma, Y.-Y.; Wang, W.; Wang, G.-Y.; Cao, M.-Y.; Dong, J.-J.; Chen, Y.-A. Research progress of therapeutic effects and drug resistance of immunotherapy based on PD-1/PD-L1 blockade. Drug Resist. Updat. 2023, 66, 100907. [Google Scholar] [CrossRef]
- Shi, F.; Shi, M.; Zeng, Z.; Qi, R.Z.; Liu, Z.W.; Zhang, J.Y.; Yang, Y.P.; Tien, P.; Wang, F.S. PD-1 and PD-L1 upregulation promotes CD8+ T-cell apoptosis and postoperative recurrence in hepatocellular carcinoma patients. Int. J. Cancer 2011, 128, 887–896. [Google Scholar] [CrossRef]
- Zhang, C.-Y.; Liu, S.; Yang, M. Regulatory T cells and their associated factors in hepatocellular carcinoma development and therapy. World J. Gastroenterol. 2022, 28, 3346. [Google Scholar] [CrossRef]
- Kraehenbuehl, L.; Weng, C.-H.; Eghbali, S.; Wolchok, J.D.; Merghoub, T. Enhancing immunotherapy in cancer by targeting emerging immunomodulatory pathways. Nat. Rev. Clin. Oncol. 2022, 19, 37–50. [Google Scholar] [CrossRef]
- Yan, Y.; Zhang, L.; Zuo, Y.; Qian, H.; Liu, C. Immune checkpoint blockade in cancer immunotherapy: Mechanisms, clinical outcomes, and safety profiles of PD-1/PD-L1 inhibitors. Arch. Immunol. Ther. Exp. 2020, 68, 36. [Google Scholar] [CrossRef] [PubMed]
- Yau, T.; Park, J.; Finn, R.; Cheng, A.-L.; Mathurin, P.; Edeline, J.; Kudo, M.; Han, K.-H.; Harding, J.; Merle, P. CheckMate 459: A randomized, multi-center phase III study of nivolumab (NIVO) vs sorafenib (SOR) as first-line (1L) treatment in patients (pts) with advanced hepatocellular carcinoma (aHCC). Ann. Oncol. 2019, 30, v874–v875. [Google Scholar] [CrossRef]
- Pinato, D.J.; Cortellini, A.; Sukumaran, A.; Cole, T.; Pai, M.; Habib, N.; Spalding, D.; Sodergren, M.H.; Martinez, M.; Dhillon, T. PRIME-HCC: Phase Ib study of neoadjuvant ipilimumab and nivolumab prior to liver resection for hepatocellular carcinoma. BMC Cancer 2021, 21, 301. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M.; Ueshima, K.; Nakahira, S.; Nishida, N.; Ida, H.; Minami, Y.; Nakai, T.; Wada, H.; Kubo, S.; Ohkawa, K. Adjuvant nivolumab for hepatocellular carcinoma (HCC) after surgical resection (SR) or radiofrequency ablation (RFA)(NIVOLVE): A phase 2 prospective multicenter single-arm trial and exploratory biomarker analysis. J. Clin. Oncol. 2021, 39, 4070. [Google Scholar] [CrossRef]
- Kudo, M. Limited impact of anti-PD-1/PD-L1 monotherapy for hepatocellular carcinoma. Liver Cancer 2020, 9, 629–639. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.; Mao, J.; Liu, C.; Fu, H.; Guo, W.; Ding, G. Risk of adverse events in advanced hepatocellular carcinoma with immune checkpoint therapy: A systematic review and meta-analysis. Clin. Res. Hepatol. Gastroenterol. 2020, 44, 845–854. [Google Scholar] [CrossRef] [PubMed]
- Pinato, D.J.; Cole, T.; Bengsch, B.; Tait, P.; Sayed, A.A.; Abomeli, F.; Gramenitskaya, D.; Allara, E.; Thomas, R.; Ward, C. A phase Ib study of pembrolizumab following trans-arterial chemoembolization (TACE) in hepatocellular carcinoma (HCC): PETAL. Ann. Oncol. 2019, 30, v288. [Google Scholar] [CrossRef]
- Finn, R.S.; Ryoo, B.-Y.; Merle, P.; Bouattour, M.; Lim, H.; Breder, V.; Edeline, J.; Chao, Y.; Ogasawara, S.; Yau, T. Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240: A randomized, double-blind, phase III trial. J. Clin. Oncol. 2020, 38, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.M.; Kudo, M.; Cheng, A.-L.; Finn, R.S.; Galle, P.R.; Kaneko, S.; Meyer, T.; Qin, S.; Dutcus, C.E.; Chen, E. Lenvatinib (len) plus pembrolizumab (pembro) for the first-line treatment of patients (pts) with advanced hepatocellular carcinoma (HCC): Phase 3 LEAP-002 study. Am. Soc. Clin. Oncol. 2019, 37, TPS4152. [Google Scholar] [CrossRef]
- Akbulut, Z.; Aru, B.; Aydin, F.; Yanikkaya Demirel, G. Immune Checkpoint Inhibitors in The Treatment of Hepatocellular Carcinoma. Front. Immunol. 2024, 15, 1379622. [Google Scholar] [CrossRef]
- Kooshkaki, O.; Derakhshani, A.; Hosseinkhani, N.; Torabi, M.; Safaei, S.; Brunetti, O.; Racanelli, V.; Silvestris, N.; Baradaran, B. Combination of ipilimumab and nivolumab in cancers: From clinical practice to ongoing clinical trials. Int. J. Mol. Sci. 2020, 21, 4427. [Google Scholar] [CrossRef]
- Guardascione, M.; Toffoli, G. Immune checkpoint inhibitors as monotherapy or within a combinatorial strategy in advanced hepatocellular carcinoma. Int. J. Mol. Sci. 2020, 21, 6302. [Google Scholar] [CrossRef] [PubMed]
- Yau, T.; Kang, Y.-K.; Kim, T.-Y.; El-Khoueiry, A.B.; Santoro, A.; Sangro, B.; Melero, I.; Kudo, M.; Hou, M.-M.; Matilla, A. Efficacy and safety of nivolumab plus ipilimumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib: The CheckMate 040 randomized clinical trial. JAMA Oncol. 2020, 6, e204564. [Google Scholar] [CrossRef]
- Kaseb, A.O.; Tran Cao, H.S.; Mohamed, Y.I.; Qayyum, A.; Vence, L.M.; Blando, J.M.; Singh, S.; Lee, S.S.; Raghav, K.P.S.; Altameemi, L. Final results of a randomized, open label, perioperative phase II study evaluating nivolumab alone or nivolumab plus ipilimumab in patients with resectable HCC. Am. Soc. Clin. Oncol. 2020, 38, 4599. [Google Scholar] [CrossRef]
- Bhatt, A.; Wu, J. Immunotherapy for recurrent hepatocellular carcinoma. World J. Gastroenterol. 2023, 29, 2261. [Google Scholar] [CrossRef]
- Antonia, S.; Goldberg, S.B.; Balmanoukian, A.; Chaft, J.E.; Sanborn, R.E.; Gupta, A.; Narwal, R.; Steele, K.; Gu, Y.; Karakunnel, J.J. Safety and antitumour activity in a phase 1b study of combined checkpoint blockade with anti-PD-L1 (durvalumab) and anti-CTLA4 (tremelimumab) in non-small cell lung cancer. Lancet. Oncol. 2016, 17, 299. [Google Scholar] [CrossRef]
- Notohardjo, J.; van Pul, K.; Stam, A.; Chondronasiou, D.; Lougheed, S.; van den Tol, P.; Jooss, K.; Vuylsteke, R.; van den Eertwegh, A.; de Gruijl, T. 309 The role of tumor-draining lymph nodes in the tuning of systemic T cell immunity by CTLA-4 blockade is revealed by local delivery of tremelimumab in early-stage melanoma: Data from a Phase-I trial. BMJ Special. J. 2020, 8, A190. [Google Scholar]
- Ziogas, D.C.; Theocharopoulos, C.; Lialios, P.-P.; Foteinou, D.; Koumprentziotis, I.-A.; Xynos, G.; Gogas, H. Beyond CTLA-4 and PD-1 inhibition: Novel immune checkpoint molecules for melanoma treatment. Cancer 2023, 15, 2718. [Google Scholar] [CrossRef]
- De Toni, E.N.; Mayerle, J.; Oehrle, B.; Seidensticker, M.; Rimassa, L.; Ehmer, U.; Geier, A.; Reiter, F.P.; Ettrich, T.J.; Philipp, A.B. Sequential or up-front triple combination with durvalumab, tremelimumab, and bevacizumab for patients with unresectable hepatocellular carcinoma (HCC): MONTBLANC. Am. Soc. Clin. Oncol. 2024, 42, TPS574. [Google Scholar] [CrossRef]
- Buchalter, J.; Browne, I.; Mac Eochagain, C.; Flynn, C.; Carroll, H.K.; Galligan, M.; Bourke, M.; Lester-Grant, A.; Desmond, F.; Hoey, K. Tremelimumab (day 1 only) and durvalumab in combination with transarterial chemoemobilization (TACE) in patients with hepatocellular carcinoma (HCC). Am. Soc. Clin. Oncol. 2022, 40, 451. [Google Scholar] [CrossRef]



| Drugs | Commercial Name | Clinical ID | Phase | Targets | Mode of Action | Medium Overall Survival (Months) | Tumor-Associated Function | Specific Inhibited Pathway | Ref. |
|---|---|---|---|---|---|---|---|---|---|
| Sorafenib | Nexavar | NCT01015833 | III | RAF, VEGFR, PDGFR-β, TGF, IGF, FLT-3 | MKI | mOS 9.4 months | Immunoregulation, proliferation, angiogenesis | KIT, RET, FGFR1, VEGFR2/3, PDGFR-β | [40] |
| Lenvatinib | Lenvatinibvima | NCT01761266 | III | KIT, RET, PD-1, TGF, IGF, FGFR1-4, VEGFR1-3, PDGFR-α | MKI | mOS 13.6 months | Immunoregulation, proliferation, angiogenesis | KIT, RET, FGFR1–4, VEGFR1–3, PDGFR-α | [50] |
| Regorafenib | Stivarga | NCT01774344 | III | B-RAF, KIT, RET, TGF, IGF, FGFR1, VEGFR1-3, PDGFR-β | MKI | mOS 10.6 months | Immunoregulation, proliferation, angiogenesis | KIT, RET, VEGFR1–3, PDGFR-β | [57] |
| Cabozantinib | Cabozantinibmetyx and Cometriq | NCT04588051 | II | AXL, MET, TGF, IGF, VEGFR2 | TKI | mOS 9.9 months | Metastatic lesions, migration, angiogenesis | KIT, RET, AXL, MET, VEGFR2 | [60] |
| Ramucirumab | Cyramza | NCT01140347 | III | TGF, IGF, VEGFR2 | mAb | mOS 9.2 months | Immunoregulation, angiogenesis | VEGFR2 | [61] |
| Nivolumab + ipilimumab | Opdivo + Yervoy | NCT01658878 | II | PD-1 + CTLA-4 | Anti-PD-1 antibody + Anti-CTLA-4-antibody | mOS 22.2 months | Proliferation, angiogenesis, immunoregulation | PD-1, CTLA-4 pathway | [62] |
| Pembrolizumab | Keytruda | NCT03062358 | III | PD-1 | Anti-PD-1 anibody | mOS 14.6 months | Tumor regression, immune regulation | PD-1 | [63] |
| Atezolizumab + bevacizumab | Tecentriq + Avastin | NCT03434379 | III | PD-L1 + VEGF | Anti-PD-L1 antibody + Anti-VEGF-antibody | mOS of atezolizumab + bevacizumaba 19.2 months | Proliferation, metastasis, invasion, angiogenesis | PD-L1, VEGF | [64] |
| Durvalumab + tremelimumab | Imfinzi + Imjudo | CTR20222433 | III | PD-L1 + CTLA-4 | Anti-PD-L1 antibody + Anti-CTLA-4-antibody | N/A | Immunoregulation, proliferation, angiogenesis, necrosis | PD-L1, CTLA-4 | [65] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zarlashat, Y.; Abbas, S.; Ghaffar, A. Hepatocellular Carcinoma: Beyond the Border of Advanced Stage Therapy. Cancers 2024, 16, 2034. https://doi.org/10.3390/cancers16112034
Zarlashat Y, Abbas S, Ghaffar A. Hepatocellular Carcinoma: Beyond the Border of Advanced Stage Therapy. Cancers. 2024; 16(11):2034. https://doi.org/10.3390/cancers16112034
Chicago/Turabian StyleZarlashat, Yusra, Shakil Abbas, and Abdul Ghaffar. 2024. "Hepatocellular Carcinoma: Beyond the Border of Advanced Stage Therapy" Cancers 16, no. 11: 2034. https://doi.org/10.3390/cancers16112034





