Haemostatic Gene Expression in Cancer-Related Immunothrombosis: Contribution for Venous Thromboembolism and Ovarian Tumour Behaviour
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Enrolment
2.2. Blood Sample Collection and Processing
2.3. Gene Selection
2.4. Total RNA Extraction
2.5. cDNA Synthesis
2.6. Gene Relative Quantification
2.7. Statistical Analysis
3. Results
3.1. Patients Characteristics
| Variable | n (%) |
|---|---|
| Age at OC diagnosis (years) * | 63.6 ± 12.0 |
| ≥64 | 27 (51.9) |
| Hormonal status at OC diagnosis | |
| Postmenopausal | 40 (76.9) |
| Baseline BMI (kg/m2) * | 26.8 ± 4.9 |
| ≥27.0 | 21 (40.4) |
| ECOG PS at OC diagnosis | |
| >1 | 7 (13.5) |
| Baseline haemoglobin levels (U/mL) * | 12.4 ± 1.4 |
| <12.4 | 25 (48.1) |
| Baseline platelet count (×109/L) ** | 296.0 [164.0; 572.0] |
| ≥296.0 | 25 (48.1) |
| Baseline leucocyte count (×109/L) * | 7.9 ± 2.3 |
| ≥7.9 | 25 (48.1) |
| Baseline neutrophil count (×109/L) * | 5.1 ± 2.1 |
| ≥5.1 | 25 (48.1) |
| Baseline monocyte count (×109/L) ** | 0.6 [0.3; 1.4] |
| ≥0.6 | 24 (46.2) |
| Baseline lymphocyte count (×109/L) ** | 1.5 [0.6; 4.3] |
| ≥1.5 | 24 (46.2) |
| Baseline PT (s) ** | 14.2 [11.4; 31.2] |
| ≥14.2 | 22 (42.3) |
| Baseline INR ** | 1.1 [1.0; 2.2] |
| ≥1.1 | 21 (40.4) |
| Baseline aPTT (s) * | 27.1 ± 2.4 |
| ≥27.1 | 21 (40.4) |
| KS | |
| ≥2 | 22 (42.3) |
| Platelet anti-aggregation therapy at OC diagnosis | 8 (15.4) |
| Anticoagulation therapy at OC diagnosis *** | 3 (5.8) |
| OC-related inherited mutations | 5 (9.6) |
| Tumour histology | |
| Serous | 44 (84.6) |
| Clear cell | 3 (5.8) |
| Endometroid | 1 (1.9) |
| Mixed | 2 (3.8) |
| Unusual | 2 (3.8) |
| Histological grade | |
| High | 49 (94.2) |
| FIGO stage # | |
| I/II | 10 (19.2) |
| III/IV | 42 (80.8) |
| Baseline CA-125 levels (U/mL) ** | 1067.0 [7.7; 10,184.0] |
| ≥1067 | 26 (50.0) |
| Upfront treatment | |
| Surgery and adjuvant chemotherapy | 23 (44.2) |
| Neoadjuvant chemotherapy and surgery | 2 (3.8) |
| Neoadjuvant chemotherapy, surgery and adjuvant chemotherapy | 14 (26.9) |
| Chemotherapy only | 13 (25.0) |
| Platinum sensitivity δ | 40 (76.9) |
| Maintenance therapy | |
| PARPi | 16 (30.8) |
| bevacizumab | 6 (11.5) |
3.2. Impact of VTE on Patients’ Prognosis
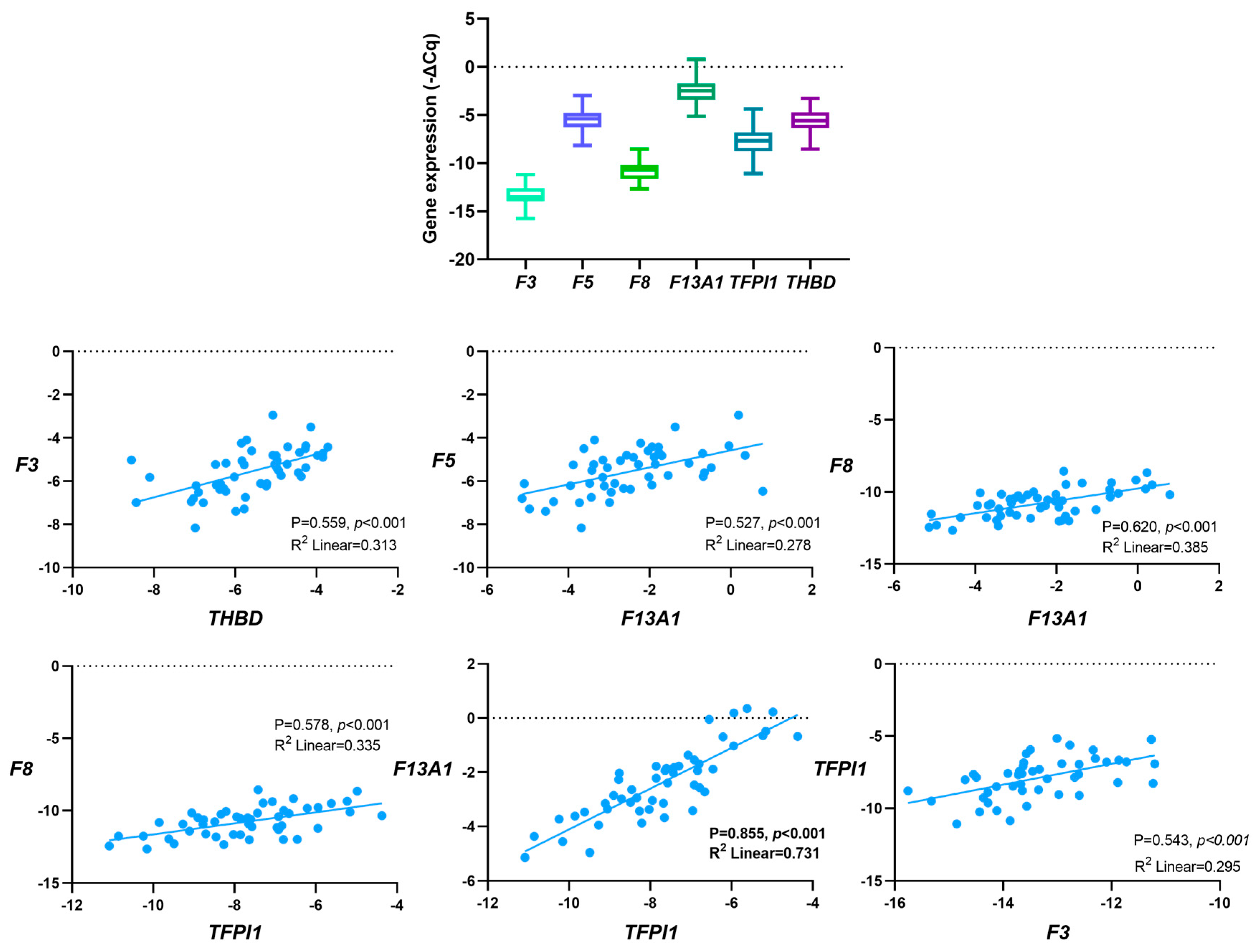
3.3. Correlation between Baseline Gene Expression
3.4. Baseline Gene Expression and Patients’ Characteristics
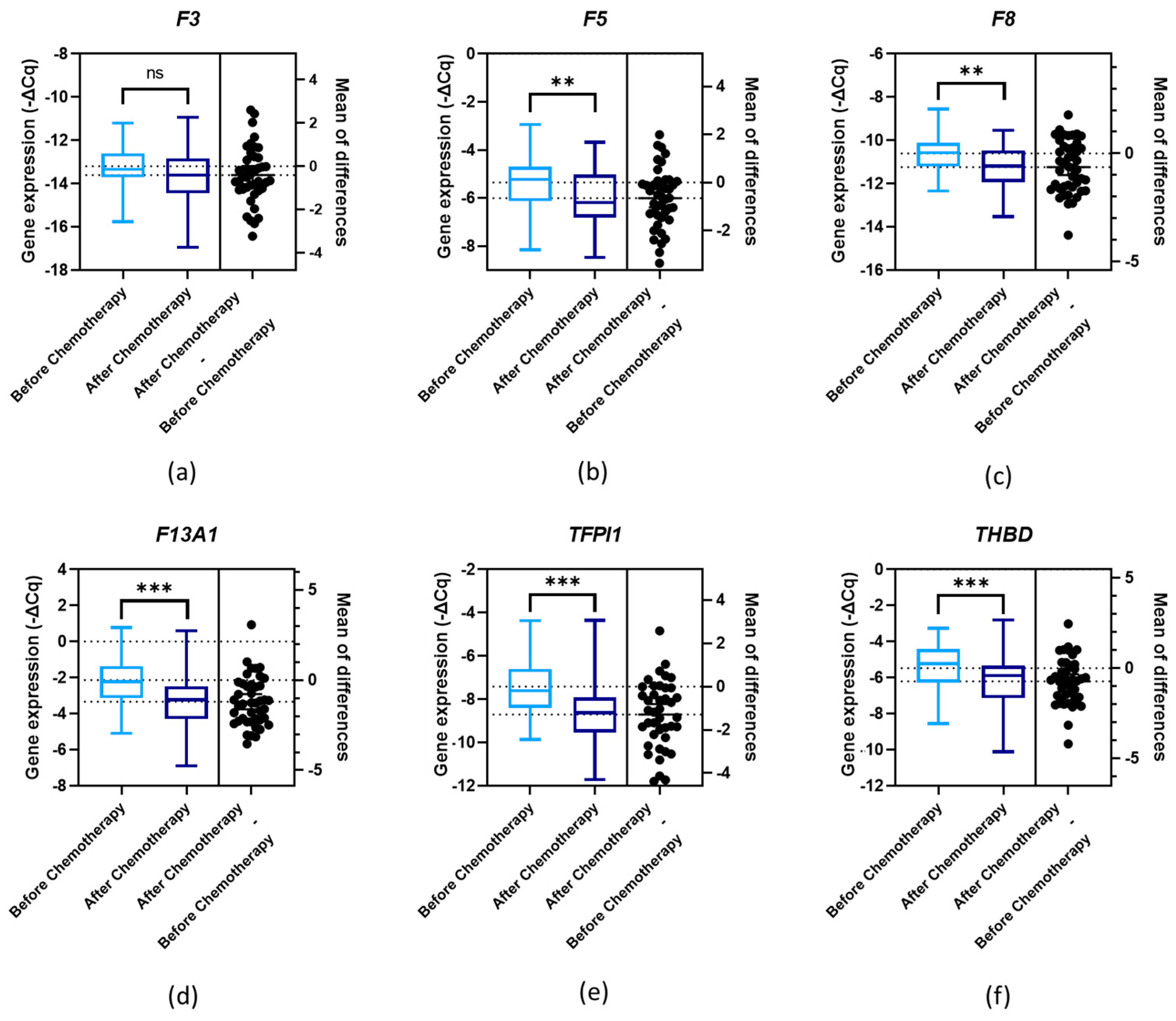
3.5. Gene Expression and First-Line Chemotherapy
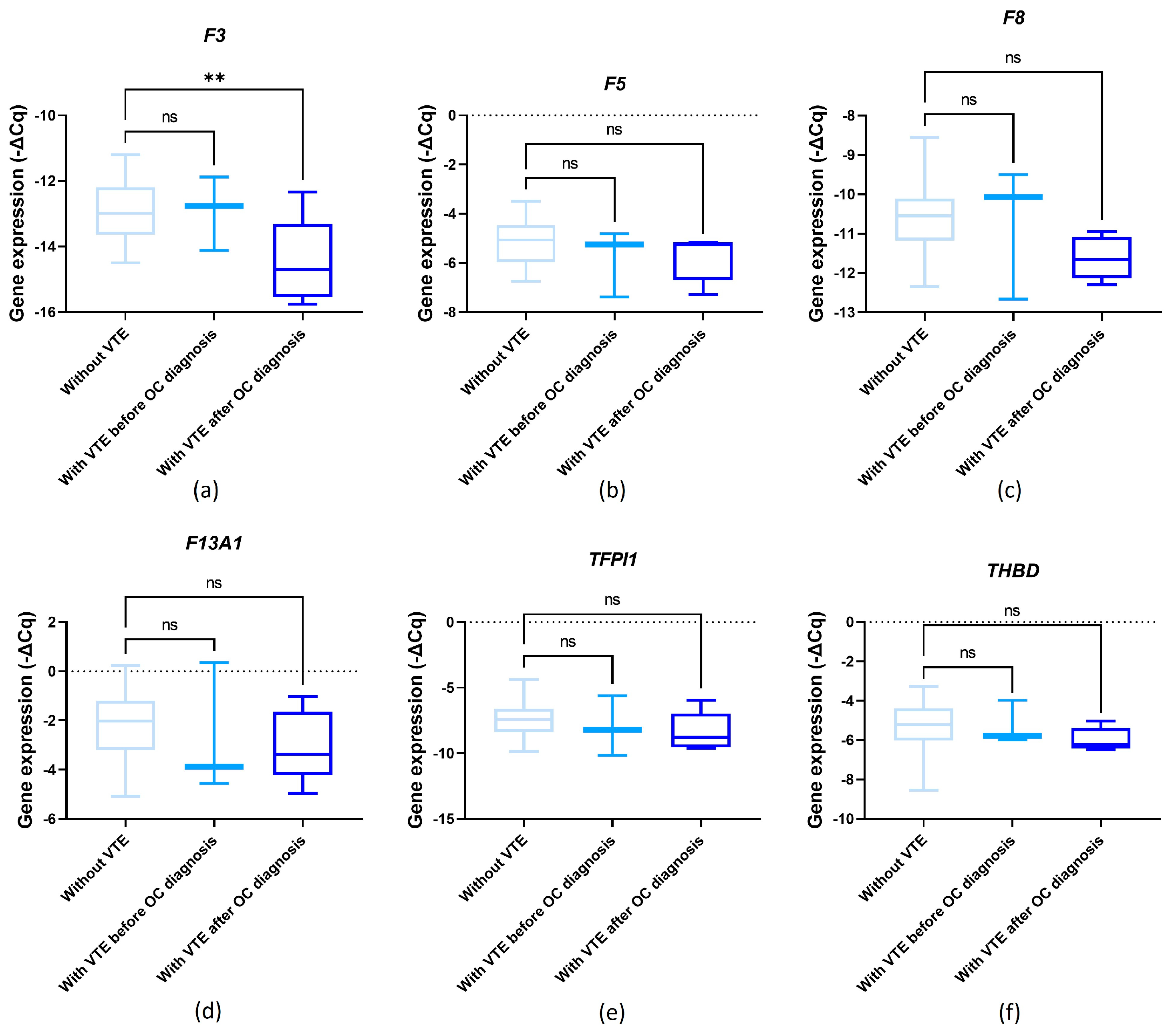
3.6. Baseline Gene Expression and OC-Related VTE
3.7. Impact of Baseline Gene Expression on Patients’ Prognosis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Ervik, M.; Lam, F.; Laversanne, M.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Today; International Agency for Research on Cancer: Lyon, France; Available online: https://gco.iarc.fr/today (accessed on 5 February 2024).
- Nag, S.; Aggarwal, S.; Rauthan, A.; Warrier, N. Maintenance therapy for newly diagnosed epithelial ovarian cancer—A review. J. Ovarian Res. 2022, 15, 88. [Google Scholar] [CrossRef]
- Tavares, V.; Marques, I.S.; Melo, I.G.d.; Assis, J.; Pereira, D.; Medeiros, R. Paradigm Shift: A Comprehensive Review of Ovarian Cancer Management in an Era of Advancements. Int. J. Mol. Sci. 2024, 25, 1845. [Google Scholar] [CrossRef]
- Oncul, S.; Cho, M.S. Interactions between platelets and tumor microenvironment components in ovarian cancer and their implications for treatment and clinical outcomes. Cancers 2023, 15, 1282. [Google Scholar] [CrossRef]
- Yousef, G.M.; Polymeris, M.-E.; Grass, L.; Soosaipillai, A.; Chan, P.-C.; Scorilas, A.; Borgono, C.; Harbeck, N.; Schmalfeldt, B.; Dorn, J. Human kallikrein 5: A potential novel serum biomarker for breast and ovarian cancer. Cancer Res. 2003, 63, 3958–3965. [Google Scholar]
- Kim, A.S.; Khorana, A.A.; McCrae, K.R. Mechanisms and biomarkers of cancer-associated thrombosis. Transl. Res. 2020, 225, 33–53. [Google Scholar] [CrossRef]
- Neto, B.V.; Tavares, V.; da Silva, J.B.; Liz-Pimenta, J.; Marques, I.S.; Salgado, L.; Carvalho, L.; Pereira, D.; Medeiros, R. Haemostatic gene variations in cervical cancer-associated venous thrombosis: Considerations for clinical strategies. J. Thromb. Thrombolysis 2024, 1–13. [Google Scholar] [CrossRef]
- Khorana, A.A.; Mackman, N.; Falanga, A.; Pabinger, I.; Noble, S.; Ageno, W.; Moik, F.; Lee, A.Y. Cancer-associated venous thromboembolism. Nat. Rev. Dis. Primers 2022, 8, 11. [Google Scholar] [CrossRef]
- Glassman, D.; Bateman, N.W.; Lee, S.; Zhao, L.; Yao, J.; Tan, Y.; Ivan, C.; Rangel, K.M.; Zhang, J.; Conrads, K.A. Molecular correlates of venous thromboembolism (VTE) in ovarian cancer. Cancers 2022, 14, 1496. [Google Scholar] [CrossRef]
- Liz-Pimenta, J.; Tavares, V.; Neto, B.V.; Santos, J.M.; Guedes, C.B.; Araújo, A.; Khorana, A.A.; Medeiros, R. Thrombosis and cachexia in cancer: Two partners in crime? Crit. Rev. Oncol./Hematol. 2023, 186, 103989. [Google Scholar] [CrossRef]
- Heestermans, M.; Poenou, G.; Duchez, A.-C.; Hamzeh-Cognasse, H.; Bertoletti, L.; Cognasse, F. Immunothrombosis and the role of platelets in venous thromboembolic diseases. Int. J. Mol. Sci. 2022, 23, 13176. [Google Scholar] [CrossRef]
- Palumbo, J.S. Crosstalk between hemostasis and immunity in cancer pathogenesis. Thromb. Res. 2022, 213, S3–S7. [Google Scholar] [CrossRef]
- Swystun, L.L.; Liaw, P.C. The role of leukocytes in thrombosis. Blood J. Am. Soc. Hematol. 2016, 128, 753–762. [Google Scholar] [CrossRef]
- Zhu, J.W.; Charkhchi, P.; Akbari, M.R. Potential clinical utility of liquid biopsies in ovarian cancer. Mol. Cancer 2022, 21, 114. [Google Scholar] [CrossRef]
- Gran, O.V.; Smith, E.N.; Brækkan, S.K.; Jensvoll, H.; Solomon, T.; Hindberg, K.; Wilsgaard, T.; Rosendaal, F.R.; Frazer, K.A.; Hansen, J.-B. Joint effects of cancer and variants in the factor 5 gene on the risk of venous thromboembolism. Haematologica 2016, 101, 1046. [Google Scholar] [CrossRef]
- Tavares, V.; Neto, B.V.; Marques, I.S.; Assis, J.; Pereira, D.; Medeiros, R. Cancer-associated thrombosis: What about microRNAs targeting the tissue factor coagulation pathway? Biochim. Biophys. Acta BBA-Rev. Cancer 2023, 1879, 189053. [Google Scholar] [CrossRef] [PubMed]
- Rondon, A.M.; Kroone, C.; Kapteijn, M.Y.; Versteeg, H.H.; Buijs, J.T. Role of tissue factor in tumor progression and cancer-associated thrombosis. Semin. Thromb. Hemost. 2019, 45, 396–412. [Google Scholar] [CrossRef]
- Girard, T.J.; Antunes, L.; Zhang, N.; Amrute, J.M.; Subramanian, R.; Eldem, I.; Remy, K.E.; Mazer, M.; Erlich, E.C.; Cruchaga, C. Peripheral blood mononuclear cell tissue factor (F3 gene) transcript levels and circulating extracellular vesicles are elevated in severe coronavirus 2019 (COVID-19) disease. J. Thromb. Haemost. 2023, 21, 629–638. [Google Scholar] [CrossRef]
- Panes, O.; Matus, V.; Sáez, C.G.; Quiroga, T.; Pereira, J.; Mezzano, D. Human platelets synthesize and express functional tissue factor. Blood J. Am. Soc. Hematol. 2007, 109, 5242–5250. [Google Scholar] [CrossRef]
- Dashty, M.; Akbarkhanzadeh, V.; Zeebregts, C.J.; Spek, C.A.; Sijbrands, E.J.; Peppelenbosch, M.P.; Rezaee, F. Characterization of coagulation factor synthesis in nine human primary cell types. Sci. Rep. 2012, 2, 787. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Kotagiri, P.; Lyons, P.A.; Al-Lamki, R.S.; Mescia, F.; Bergamaschi, L.; Turner, L.; Morgan, M.D.; Calero-Nieto, F.J.; Bach, K. Coagulation factor V is a T-cell inhibitor expressed by leukocytes in COVID-19. iScience 2022, 25, 103971. [Google Scholar] [CrossRef] [PubMed]
- Shahani, T.; Covens, K.; Lavend’Homme, R.; Jazouli, N.; Sokal, E.; Peerlinck, K.; Jacquemin, M. Human liver sinusoidal endothelial cells but not hepatocytes contain factor VIII. J. Thromb. Haemost. 2014, 12, 36–42. [Google Scholar] [CrossRef]
- Mazurkiewicz-Pisarek, A.; Płucienniczak, G.; Ciach, T.; Płucienniczak, A. The factor VIII protein and its function. Acta Biochim. Pol. 2016, 63, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Zanolini, D.; Merlin, S.; Feola, M.; Ranaldo, G.; Amoruso, A.; Gaidano, G.; Zaffaroni, M.; Ferrero, A.; Brunelleschi, S.; Valente, G. Extrahepatic sources of factor VIII potentially contribute to the coagulation cascade correcting the bleeding phenotype of mice with hemophilia A. Haematologica 2015, 100, 881. [Google Scholar] [CrossRef] [PubMed]
- Bugert, P.; Dugrillon, A.; Günaydin, A.; Eichler, H.; Klüter, H. Messenger RNA profiling of human platelets by microarray hybridization. Thromb. Haemost. 2003, 90, 738–748. [Google Scholar] [PubMed]
- Alshehri, F.S.; Whyte, C.S.; Mutch, N.J. Factor XIII-A: An indispensable “factor” in haemostasis and wound healing. Int. J. Mol. Sci. 2021, 22, 3055. [Google Scholar] [CrossRef] [PubMed]
- Songdej, N.; Del Carpio-cano, F.; Mao, G.; Wurtzel, J.; Goldfinger, L.; Lambert, M.P.; Rao, A.K. Transcription factor RUNX1 regulates factor FXIIIA subunit (F13A1) expression in megakaryocytic cells and platelet F13A1 expression is downregulated in RUNX1 haplodeficiency. Blood 2020, 136, 25–26. [Google Scholar] [CrossRef]
- Chinetti-Gbaguidi, G.; Copin, C.; Derudas, B.; Marx, N.; Eechkoute, J.; Staels, B. Peroxisome proliferator-activated receptor γ induces the expression of tissue factor pathway inhibitor-1 (TFPI-1) in human macrophages. PPAR Res. 2016, 2016, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Conway, E.M.; Nowakowski, B.; Steiner-Mosonyi, M. Human neutrophils synthesize thrombomodulin that does not promote thrombin-dependent protein C activation. Blood 1992, 80, 1254–1263. [Google Scholar] [CrossRef] [PubMed]
- Loghmani, H.; Conway, E.M. Exploring traditional and nontraditional roles for thrombomodulin. Blood J. Am. Soc. Hematol. 2018, 132, 148–158. [Google Scholar] [CrossRef] [PubMed]
- Vaiphei, S.T.; Keppen, J.; Nongrum, S.; Chaubey, R.; Kma, L.; Sharan, R. Evaluation of endogenous control gene(s) for gene expression studies in human blood exposed to 60 Co γ-rays ex vivo. J. Radiat. Res. 2015, 56, 177–185. [Google Scholar] [CrossRef]
- Davis, R.; Murgia, C.; Dordevic, A.L.; Bonham, M.P.; Huggins, C.E. Diurnal variation in gene expression of human peripheral blood mononuclear cells after eating a standard meal compared with a high protein meal: A cross-over study. Clin. Nutr. 2021, 40, 4349–4359. [Google Scholar] [CrossRef] [PubMed]
- Hazarika, A.; Nongkhlaw, B.; Mukhopadhyay, A. Identification of stable reference genes in peripheral blood mononuclear cells from type 2 diabetes mellitus patients. Sci. Rep. 2023, 13, 486. [Google Scholar] [CrossRef] [PubMed]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef] [PubMed]
- Berek, J.S.; Renz, M.; Kehoe, S.; Kumar, L.; Friedlander, M. Cancer of the ovary, fallopian tube, and peritoneum: 2021 update. Int. J. Gynecol. Obstet. 2021, 155, 61–85. [Google Scholar] [CrossRef] [PubMed]
- Tavares, V.; Pinto, R.; Assis, J.; Pereira, D.; Medeiros, R. Venous thromboembolism GWAS reported genetic makeup and the hallmarks of cancer: Linkage to ovarian tumour behaviour. Biochim. Biophys. Acta BBA-Rev. Cancer 2020, 1873, 188331. [Google Scholar] [CrossRef] [PubMed]
- Segal, B.H.; Giridharan, T.; Suzuki, S.; Khan, A.N.H.; Zsiros, E.; Emmons, T.R.; Yaffe, M.B.; Gankema, A.A.; Hoogeboom, M.; Goetschalckx, I. Neutrophil interactions with T cells, platelets, endothelial cells, and of course tumor cells. Immunol. Rev. 2023, 314, 13–35. [Google Scholar] [CrossRef] [PubMed]
- Castaño, M.; Tomás-Pérez, S.; González-Cantó, E.; Aghababyan, C.; Mascarós-Martínez, A.; Santonja, N.; Herreros-Pomares, A.; Oto, J.; Medina, P.; Götte, M. Neutrophil extracellular traps and cancer: Trapping our attention with their involvement in ovarian cancer. Int. J. Mol. Sci. 2023, 24, 5995. [Google Scholar] [CrossRef] [PubMed]
- Pankowska, K.A.; Będkowska, G.E.; Chociej-Stypułkowska, J.; Rusak, M.; Dąbrowska, M.; Osada, J. Crosstalk of immune cells and platelets in an ovarian cancer microenvironment and their prognostic significance. Int. J. Mol. Sci. 2023, 24, 9279. [Google Scholar] [CrossRef] [PubMed]
- Palta, S.; Saroa, R.; Palta, A. Overview of the coagulation system. Indian J. Anaesth. 2014, 58, 515–523. [Google Scholar] [CrossRef]
- Harrison, P.; Goodall, A.H. “Message in the platelet”–more than just vestigial mRNA! Platelets 2008, 19, 395–404. [Google Scholar] [CrossRef]
- Saadeh, F.A.; Norris, L.; O’Toole, S.; Gleeson, N. Venous thromboembolism in ovarian cancer: Incidence, risk factors and impact on survival. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 170, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Kahr, H.S.; Christiansen, O.B.; Grove, A.; Iyer, V.; Torp-Pedersen, C.; Knudsen, A.; Thorlacius-Ussing, O. Venous thromboembolism in epithelial ovarian cancer. A prospective cohort study. Thromb. Res. 2019, 181, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Salinaro, J.R.; McQuillen, K.; Stemple, M.; Boccaccio, R.; Ehrisman, J.; Lorenzo, A.M.; Havrilesky, L.; Secord, A.A.; Turner, V.G.; Moore, K.N.; et al. Incidence of venous thromboembolism among patients receiving neoadjuvant chemotherapy for advanced epithelial ovarian cancer. Int. J. Gynecol. Cancer 2020, 30, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Weeks, K.S.; Herbach, E.; McDonald, M.; Charlton, M.; Schweizer, M.L. Meta-Analysis of VTE Risk: Ovarian Cancer Patients by Stage, Histology, Cytoreduction, and Ascites at Diagnosis. Obs. Gynecol. Int. 2020, 2020, 2374716. [Google Scholar] [CrossRef] [PubMed]
- Basaran, D.; Boerner, T.; Suhner, J.; Sassine, D.; Liu, Y.; Grisham, R.N.; Tew, W.P.; Gardner, G.J.; Zivanovic, O.; Sonoda, Y.; et al. Risk of venous thromboembolism in ovarian cancer patients receiving neoadjuvant chemotherapy. Gynecol. Oncol. 2021, 163, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Oxley, S.G.; Achampong, Y.A.; Sambandan, N.; Hughes, D.J.; Thomas, M.; Lockley, M.; Olaitan, A. Venous thromboembolism in women with ovarian cancer undergoing neoadjuvant chemotherapy prior to cytoreductive surgery: A retrospective study. Acta Obstet. Gynecol. Scand. 2021, 100, 2091–2096. [Google Scholar] [CrossRef] [PubMed]
- Moufarrij, S.; Havrilesky, L.; Jewell, E.L. Universal thromboprophylaxis in ovarian cancer patients before and after surgery? Gynecol. Oncol. 2023, 176, A1–A2. [Google Scholar] [CrossRef] [PubMed]
- Connolly, G.C.; Khorana, A.A.; Kuderer, N.M.; Culakova, E.; Francis, C.W.; Lyman, G.H. Leukocytosis, thrombosis and early mortality in cancer patients initiating chemotherapy. Thromb. Res. 2010, 126, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Salazar, J.L.; Tirado, L.A.R.; Contreras, N.G.; Arrieta, O.; Gallardo, D.; Cesarman-Maus, G. Leukocytosis, but Not Thrombocytosis, May Constitute a Prothrombotic Pathway in Women with Ovarian Cancer: A Cohort Study. Blood 2018, 132, 1228. [Google Scholar] [CrossRef]
- Diaz, E.S.; Walts, A.E.; Karlan, B.Y.; Walsh, C.S. Venous thromboembolism during primary treatment of ovarian clear cell carcinoma is associated with decreased survival. Gynecol. Oncol. 2013, 131, 541–545. [Google Scholar] [CrossRef]
- Heath, O.M.; Van Beekhuizen, H.J.; Nama, V.; Kolomainen, D.; Nobbenhuis, M.A.; Ind, T.E.; Sohaib, S.A.; Lofts, F.J.; Heenan, S.; Gore, M. Venous thromboembolism at time of diagnosis of ovarian cancer: Survival differs in symptomatic and asymptomatic cases. Thromb. Res. 2016, 137, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Liz-Pimenta, J.; Tavares, V.; Gramaça, J.; Rato, J.; Menezes, M.; Baleiras, M.; Guedes, H.; Reis, J.; Guedes, C.; Gomes, R. Primary thromboprophylaxis in cancer outpatients–real-world evidence. J. Thromb. Thrombolysis 2024, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hisada, Y.; Mackman, N. Tissue factor and extracellular vesicles: Activation of coagulation and impact on survival in cancer. Cancers 2021, 13, 3839. [Google Scholar] [CrossRef] [PubMed]
- Unruh, D.; Horbinski, C. Beyond thrombosis: The impact of tissue factor signaling in cancer. J. Hematol. Oncol. 2020, 13, 93. [Google Scholar] [CrossRef]
- Hisada, Y.; Mackman, N. Tissue factor and cancer: Regulation, tumor growth, and metastasis. In Seminars in Thrombosis and Hemostasis; Thieme Medical Publishers: New York, NY, USA, 2019; pp. 385–395. [Google Scholar]
- Sachetto, A.T.; Mackman, N. Monocyte tissue factor expression: Lipopolysaccharide induction and roles in pathological activation of coagulation. Thromb. Haemost. 2023, 123, 1017–1033. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K.; Malviya, R. Coagulation and inflammation in cancer: Limitations and prospects for treatment. Biochim. Biophys. Acta BBA-Rev. Cancer 2022, 1877, 188727. [Google Scholar] [CrossRef]
- Gulley, D.; Teal, E.; Suvannasankha, A.; Chalasani, N.; Liangpunsakul, S. Deep vein thrombosis and pulmonary embolism in cirrhosis patients. Dig. Dis. Sci. 2008, 53, 3012–3017. [Google Scholar] [CrossRef] [PubMed]
- Tavares, V.; Pinto, R.; Assis, J.; Coelho, S.; Brandao, M.; Alves, S.; Pereira, D.; Medeiros, R. Implications of venous thromboembolism GWAS reported genetic makeup in the clinical outcome of ovarian cancer patients. Pharmacogenom. J. 2021, 21, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Marques, I.S.; Tavares, V.; Savva-Bordalo, J.; Rei, M.; Liz-Pimenta, J.; de Melo, I.G.; Assis, J.; Pereira, D.; Medeiros, R. Long Non-Coding RNAs: Bridging Cancer-Associated Thrombosis and Clinical Outcome of Ovarian Cancer Patients. Int. J. Mol. Sci. 2023, 25, 140. [Google Scholar] [CrossRef]
- Stojkovic, S.; Thulin, Å.; Hell, L.; Thaler, B.; Rauscher, S.; Baumgartner, J.; Gröger, M.; Ay, C.; Demyanets, S.; Neumayer, C. IL-33 stimulates the release of procoagulant microvesicles from human monocytes and differentially increases tissue factor in human monocyte subsets. Thromb. Haemost. 2017, 117, 1379–1390. [Google Scholar] [CrossRef]
- Osterud, B.; Bjorklid, E. Tissue factor in blood cells and endothelial cells. Front. Biosci.-Elite 2012, 4, 289–299. [Google Scholar] [CrossRef]
- McMichael, M.A. Overview of Hemostasis. In Schalm's Veterinary Hematology; Wiley: Hoboken, NJ, USA, 2022; pp. 763–786. [Google Scholar]
- Tabibian, S.; Shiravand, Y.; Shams, M.; Safa, M.; Gholami, M.S.; Heydari, F.; Ahmadi, A.; Rashidpanah, J.; Dorgalaleh, A. A comprehensive overview of coagulation factor V and congenital factor V deficiency. Semin. Thromb. Hemost. 2019, 45, 523–543. [Google Scholar] [CrossRef] [PubMed]
- Dahlbäck, B. Pro-and anticoagulant properties of factor V in pathogenesis of thrombosis and bleeding disorders. Int. J. Lab. Hematol. 2016, 38, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Tinholt, M.; Stavik, B.; Tekpli, X.; Garred, Ø.; Borgen, E.; Kristensen, V.; Sahlberg, K.K.; Sandset, P.M.; Iversen, N. Coagulation factor V is a marker of tumor-infiltrating immune cells in breast cancer. Oncoimmunology 2020, 9, 1824644. [Google Scholar] [CrossRef] [PubMed]
- Tinholt, M.; Garred, Ø.; Borgen, E.; Beraki, E.; Schlichting, E.; Kristensen, V.; Sahlberg, K.; Iversen, N. Subtype-specific clinical and prognostic relevance of tumor-expressed F5 and regulatory F5 variants in breast cancer: The CoCaV study. J. Thromb. Haemost. 2018, 16, 1347–1356. [Google Scholar] [CrossRef] [PubMed]
- Liang, H.P.H.; Kerschen, E.J.; Basu, S.; Hernandez, I.; Zogg, M.; Jia, S.; Hessner, M.J.; Toso, R.; Rezaie, A.R.; Fernández, J.A. Coagulation factor V mediates inhibition of tissue factor signaling by activated protein C in mice. Blood J. Am. Soc. Hematol. 2015, 126, 2415–2423. [Google Scholar] [CrossRef] [PubMed]
- Reddel, C.J.; Tan, C.W.; Chen, V.M. Thrombin generation and cancer: Contributors and consequences. Cancers 2019, 11, 100. [Google Scholar] [CrossRef]
- Bouchard, B.A.; Chapin, J.; Brummel-Ziedins, K.E.; Durda, P.; Key, N.S.; Tracy, P.B. Platelets and platelet-derived factor Va confer hemostatic competence in complete factor V deficiency. Blood J. Am. Soc. Hematol. 2015, 125, 3647–3650. [Google Scholar] [CrossRef]
- Rietveld, I.M.; Lijfering, W.M.; le Cessie, S.; Bos, M.H.; Rosendaal, F.R.; Reitsma, P.H.; Cannegieter, S.C. High levels of coagulation factors and venous thrombosis risk: Strongest association for factor VIII and von Willebrand factor. J. Thromb. Haemost. 2019, 17, 99–109. [Google Scholar] [CrossRef]
- Vormittag, R.; Simanek, R.; Ay, C.; Dunkler, D.; Quehenberger, P.; Marosi, C.; Zielinski, C.; Pabinger, I. High factor VIII levels independently predict venous thromboembolism in cancer patients: The cancer and thrombosis study. Arterioscler. Thromb. Vasc. Biol. 2009, 29, 2176–2181. [Google Scholar] [CrossRef]
- Rubio, V.E.C.; Pérez-Segura, P.; Muñoz, A.; Farré, A.L.; Ruiz, L.C.; Lorente, J.A. High plasma levels of soluble P-Selectin and Factor VIII predict venous thromboembolism in non-small cell lung cancer patients: The Thrombo-Nsclc risk score. Thromb. Res. 2020, 196, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Moik, F.; Posch, F.; Grilz, E.; Scheithauer, W.; Pabinger, I.; Prager, G.; Ay, C. Haemostatic biomarkers for prognosis and prediction of therapy response in patients with metastatic colorectal cancer. Thromb. Res. 2020, 187, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Albánez, S.; Ogiwara, K.; Michels, A.; Hopman, W.; Grabell, J.; James, P.; Lillicrap, D. Aging and ABO blood type influence von Willebrand factor and factor VIII levels through interrelated mechanisms. J. Thromb. Haemost. 2016, 14, 953–963. [Google Scholar] [CrossRef] [PubMed]
- Kiouptsi, K.; Reinhardt, C. Physiological roles of the von Willebrand factor-factor VIII interaction. In Vertebrate and Invertebrate Respiratory Proteins, Lipoproteins and Other Body Fluid Proteins; Springer: Berlin/Heidelberg, Germany, 2020; pp. 437–464. [Google Scholar]
- Walker, G.E.; Merlin, S.; Zanolini, D.; Vandoni, A.; Volpe, A.; Gaidano, G.; Valente, G.; Olivero, M.; Follenzi, A. Factor VIII as a potential player in cancer pathophysiology. J. Thromb. Haemost. 2022, 20, 648–660. [Google Scholar] [CrossRef] [PubMed]
- Khalilian, S.; Mohajer, Z.; Ghafouri-Fard, S. Factor VIII as a Novel Biomarker for Diagnosis, Prognosis, and Therapy Prediction in Human Cancer and Other Disorders. Avicenna J. Med. Biotechnol. 2023, 16, 68–80. [Google Scholar] [CrossRef] [PubMed]
- Parker, R.I.; Gralnick, H.R. Effect of aspirin on platelet-von Willebrand factor surface expression on thrombin and ADP-stimulated platelets. Blood 1989, 74, 2016–2021. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.E.; Roh, D.E.; Kim, Y.H. The impact of moderate-dose acetylsalicylic acid in the reduction of inflammatory cytokine and prevention of complication in acute phase of Kawasaki disease: The benefit of moderate-dose acetylsalicylic acid. Children 2020, 7, 185. [Google Scholar] [CrossRef] [PubMed]
- Byrnes, J.R.; Wolberg, A.S. Newly-recognized roles of factor XIII in thrombosis. In Seminars in Thrombosis and Hemostasis; Thieme Medical Publishers: New York, NY, USA, 2016; pp. 445–454. [Google Scholar]
- Bagoly, Z.; Koncz, Z.; Hársfalvi, J.; Muszbek, L. Factor XIII, clot structure, thrombosis. Thromb. Res. 2012, 129, 382–387. [Google Scholar] [CrossRef] [PubMed]
- Ichinose, A. Factor XIII is a key molecule at the intersection of coagulation and fibrinolysis as well as inflammation and infection control. Int. J. Hematol. 2012, 95, 362–370. [Google Scholar] [CrossRef]
- Lee, S.H.; Suh, I.B.; Lee, E.J.; Hur, G.Y.; Lee, S.Y.; Lee, S.Y.; Shin, C.; Shim, J.J.; In, K.H.; Kang, K.H. Relationships of coagulation factor XIII activity with cell-type and stage of non-small cell lung cancer. Yonsei Med. J. 2013, 54, 1394. [Google Scholar] [CrossRef]
- Sawai, Y.; Yamanaka, Y.; Nomura, S. Clinical significance of factor XIII activity and monocyte-derived microparticles in cancer patients. Vasc. Health Risk Manag. 2020, 16, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Fei, X.; Wang, H.; Yuan, W.; Wo, M.; Jiang, L. Tissue factor pathway inhibitor-1 is a valuable marker for the prediction of deep venous thrombosis and tumor metastasis in patients with lung cancer. BioMed Res. Int. 2017, 2017, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Englisch, C.; Moik, F.; Thaler, J.; Koder, S.; Preusser, M.; Pabinger, I.; Ay, C. Tissue factor pathway inhibitor is associated with risk of venous thromboembolism and all-cause mortality in patients with cancer. Hämostaseologie 2023, 43, S23. [Google Scholar]
- Amirkhosravi, A.; Meyer, T.; Amaya, M.; Davila, M.; Mousa, S.A.; Robson, T.; Francis, J.L. The role of tissue factor pathway inhibitor in tumor growth and metastasis. Semin. Thromb. Hemost. 2007, 33, 643–652. [Google Scholar] [PubMed]
- Watanabe-Kusunoki, K.; Nakazawa, D.; Ishizu, A.; Atsumi, T. Thrombomodulin as a physiological modulator of intravascular injury. Front. Immunol. 2020, 11, 575890. [Google Scholar] [CrossRef] [PubMed]
- Amiral, J.; Seghatchian, J. Revisiting the activated protein C-protein S-thrombomodulin ternary pathway: Impact of new understanding on its laboratory investigation. Transfus. Apher. Sci. 2019, 58, 538–544. [Google Scholar] [CrossRef] [PubMed]
- Piazza, G. Venous thromboembolism and cancer. Circulation 2013, 128, 2614–2618. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-M.; Wang, W.; Lee, J.-C.; Chiu, F.-H.; Wu, C.-T.; Tai, C.-J.; Wang, C.-K.; Tai, C.-J.; Huang, M.-T.; Chang, Y.-J. Thrombomodulin mediates the progression of epithelial ovarian cancer cells. Tumor Biol. 2013, 34, 3743–3751. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-J.; Cheng, Y.-W.; Lin, R.-K.; Huang, C.-C.; Chen, W.T.-L.; Ke, T.-W.; Wei, P.-L. Thrombomodulin influences the survival of patients with non-metastatic colorectal cancer through epithelial-to-mesenchymal transition (EMT). PLoS ONE 2016, 11, e0160550. [Google Scholar] [CrossRef]
- Zheng, N.; Huo, Z.; Zhang, B.; Meng, M.; Cao, Z.; Wang, Z.; Zhou, Q. Thrombomodulin reduces tumorigenic and metastatic potential of lung cancer cells by up-regulation of E-cadherin and down-regulation of N-cadherin expression. Biochem. Biophys. Res. Commun. 2016, 476, 252–259. [Google Scholar] [CrossRef]
- Sugano, H.; Shirai, Y.; Sato, S.; Hamatani, S.; Hamura, R.; Taniai, T.; Horiuchi, T.; Gocho, T.; Eto, K.; Ikegami, T. Thrombomodulin expression impacts the recurrence and long-term survival in pancreatic cancer. Ann. Gastroenterol. Surg. 2021, 5, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-Y.; Wei, P.-L.; Prince, G.S.H.; Batzorig, U.; Lee, C.-C.; Chang, Y.-J.; Hung, C.-S. The role of thrombomodulin in estrogen-receptor-positive breast cancer progression, metastasis, and curcumin sensitivity. Biomedicines 2023, 11, 1384. [Google Scholar] [CrossRef] [PubMed]


| Gene | Genomic Location | Main Source | Expression in Platelets and Immune Cells * |
|---|---|---|---|
| F3 | 1p21.3 | Extravascular tissue cells (pericytes, fibroblasts, smooth and epithelial cells) [17] | Monocytes [18] Platelets [19] |
| F5 | 1q24.2 | Hepatocytes [20] | Monocytes [18,20] Neutrophils [21] T cells [21] Platelets [20] |
| F8 | Xq28 | Liver sinusoidal endothelial cells [22] Hepatocytes [23] Megakaryocytes [24,25] | Monocytes [18] Macrophages [20] Platelets [25] |
| F13A1 | 6p25.1 | Cells of bone marrow and the mesenchymal lineage [26] | Monocytes [18,20] Macrophages [20] Platelets [20,27] |
| TFPI1 | 2q32.1 | Vascular endothelial cells [28] Platelets [18] | Monocytes [18] Macrophages [28] |
| THBD | 20p11.21 | Vascular endothelial cells [20] | Monocytes [18,20] Macrophages [20] Neutrophils [29] Dendritic cells [30] |
| Variable | aHR | 95% CI | p-Value | Event |
|---|---|---|---|---|
| F8 baseline expression (Low vs. high 1) | 2.54 | 1.15–5.58 | 0.021 | Risk of disease progression |
| Age at OC diagnosis (≥64 vs. <64 years 1) | 1.99 | 0.96–4.10 | 0.063 | |
| Metastatic disease (Yes vs. no 1) | 10.65 | 2.46–46.12 | 0.002 | |
| F8 baseline expression (Low vs. high 1) | 6.16 | 1.68–22.52 | 0.006 | Risk of death |
| Surgery (No vs. yes 1) | 2.64 | 0.77–9.10 | 0.124 | |
| Platinum sensitivity (Others vs. sensitive 1) | 13.72 | 3.35–56.22 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tavares, V.; Savva-Bordalo, J.; Rei, M.; Liz-Pimenta, J.; Assis, J.; Pereira, D.; Medeiros, R. Haemostatic Gene Expression in Cancer-Related Immunothrombosis: Contribution for Venous Thromboembolism and Ovarian Tumour Behaviour. Cancers 2024, 16, 2356. https://doi.org/10.3390/cancers16132356
Tavares V, Savva-Bordalo J, Rei M, Liz-Pimenta J, Assis J, Pereira D, Medeiros R. Haemostatic Gene Expression in Cancer-Related Immunothrombosis: Contribution for Venous Thromboembolism and Ovarian Tumour Behaviour. Cancers. 2024; 16(13):2356. https://doi.org/10.3390/cancers16132356
Chicago/Turabian StyleTavares, Valéria, Joana Savva-Bordalo, Mariana Rei, Joana Liz-Pimenta, Joana Assis, Deolinda Pereira, and Rui Medeiros. 2024. "Haemostatic Gene Expression in Cancer-Related Immunothrombosis: Contribution for Venous Thromboembolism and Ovarian Tumour Behaviour" Cancers 16, no. 13: 2356. https://doi.org/10.3390/cancers16132356






