The Prospective Association between Early Life Growth and Breast Density in Young Adult Women
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants and Recruitment
2.2. Exclusion Criteria
2.3. Measuring Breast Density Using OBS
2.4. Measuring Breast Density Using DXA
2.5. Statistical Analyses
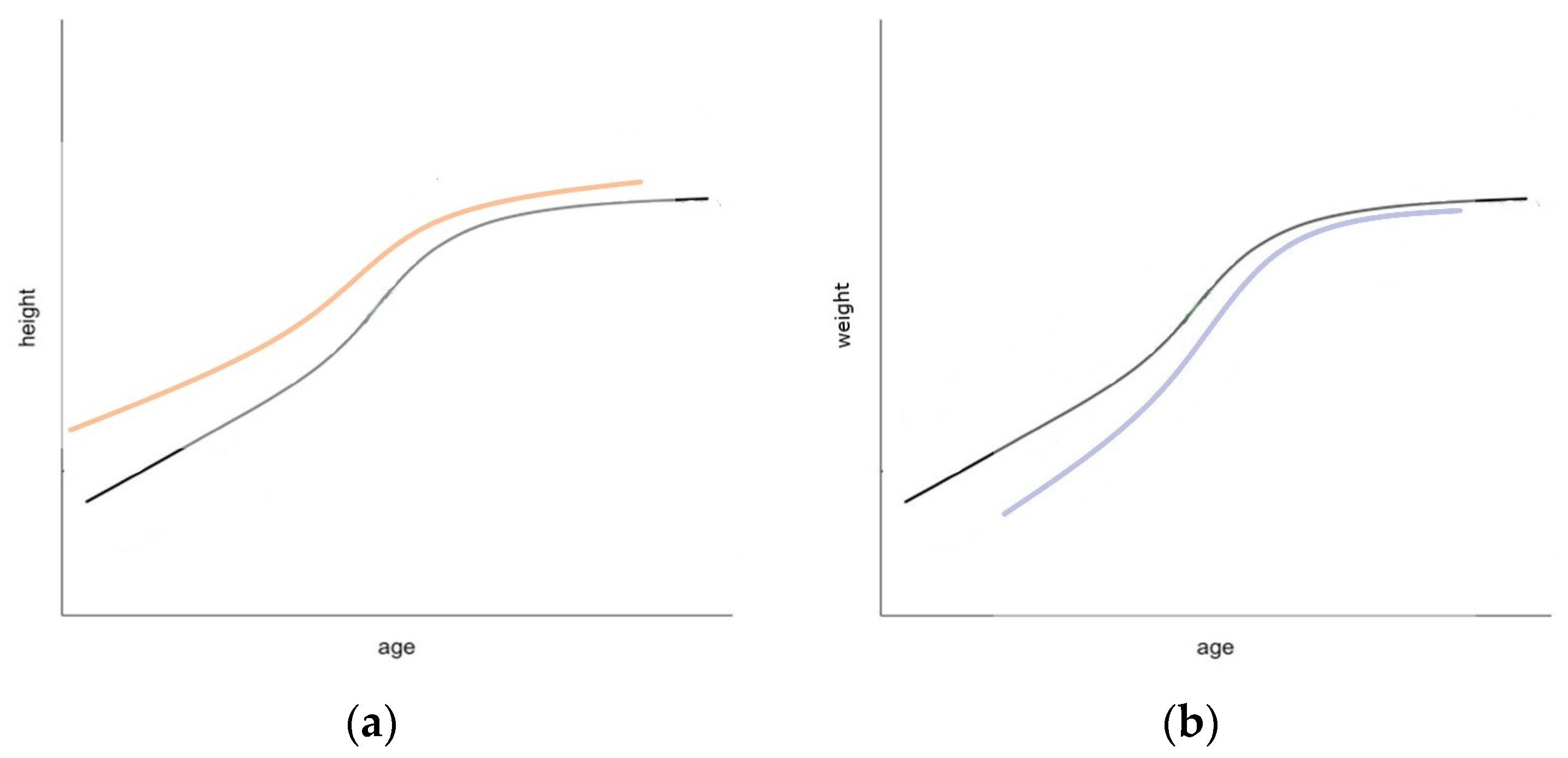
2.6. Growth Curve Analysis
2.7. Associations between Growth Curves and Breast Density Measures
3. Results
3.1. Height
3.2. Weight
3.3. BMI
| OBS (β, 95% CI) | DXA (β, 95% CI) | |||||
|---|---|---|---|---|---|---|
| %Water + Collagen 1 | %Water 2 | %Lipid 2 | %FGV 1 | FGV 3 (cm3) | NFGV 1 (cm3) | |
| Height Size (cm) | 0.20 (0.03, 0.38) * | 0.17 (0.04, 0.31) ** | −0.19 (−0.42, 0.03) | 0.02 (0.00, 0.04) | 0.03 (−0.05, 0.10) | −0.08 (−0.17, 0.00) |
| Height Timing (year) | −3.00 (−5.20, −0.68) ** | −2.70 (−4.50, −0.92) ** | 3.50 (0.56, 6.40) ** | −0.02 (−0.32, 0.28) | 0.31 (−0.68, 1.30) | 0.28 (−0.91,1.50) |
| Height Velocity | −23.00 (−38.0, −7.50) ** | −21.00 (−33.0, −9.50) *** | 27.00 (7.10, 46.00) ** | −0.32 (−2.5, 1.90) | 1.10 (−6.10, 8.40) | 3.60 (−5.20, 12.00) |
| Weight Size 4 (kg) | 0.11 ( −0.12, 0.35) | 0.08 (−0.09, 0.26) | −0.11 (−0.40, 0.18) | 0.00 (−0.02, 0.03) | −0.10 (−0.19, −0.02) ** | −0.12 (−0.22, −0.02) ** |
| Weight Velocity 4 | −2.00 (−15.00, 11.00) | 1.10(−9.00, 11.00) | 4.90 (−12.00, 21.00) | 1.10 (−0.39, 2.60) | 5.90 (0.96, 11.00) * | 0.33 (−5.60, 6.20) |
| Weight Timing 5 (year) | −0.36 (−2.70, 1.90) | −0.01 (−1.80, 1.80) | 1.10 (−1.80, 4.00) | 0.21 (−0.05, 0.48) | 1.00 (0.18, 1.90) ** | 0.09 (−0.94, 1.10) |
| BMI Size | 0.33 (−0.18, 0.84) | 0.26 (−0.13, 0.65) | −0.28 (−0.92, 0.36) | 0.01 (−0.05, 0.07) | −0.23 (−0.42, −0.04) ** | −0.32 (−0.55, −0.09) ** |
| BMI Velocity | −1.20 (−6.80, 4.50) | 1.40 (−2.90, 5.80) | 2.70 (−4.40, 9.80) | 0.59 (−0.09, 1.30) | 2.00 (−0.24, 4.20) | −0.74 (−3.40, 1.90) |
4. Discussion
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boyd, N.F.; Rommens, J.M.; Vogt, K.; Lee, V.; Hopper, J.L.; Yaffe, M.J.; Paterson, A.D. Mammographic breast density as an intermediate phenotype for breast cancer. Lancet Oncol. 2005, 6, 798–808. [Google Scholar] [CrossRef]
- McCormack, V.A.; Dos Santos Silva, I. Breast Density and Parenchymal Patterns as Markers of Breast Cancer Risk: A Meta-analysis. Cancer Epidemiol. Biomark. Prev. 2006, 15, 1159–1169. [Google Scholar] [CrossRef] [PubMed]
- Bond-Smith, D.; Stone, J. Methodological challenges and updated findings from a meta-analysis of the association between mammographic density and breast cancer. Cancer Epidemiol. Biomark. Prev. 2019, 28, 22–31. [Google Scholar] [CrossRef]
- Stone, J.; Dite, G.; Giles, G.G.; Cawson, J.; Hopper, J. Inference about causation from elimination of familial confounding: Application to longitudinal twin data on mammographic density measures that predict breast cancer risk. Cancer Epidemiol. Biomark. Prev. 2012, 21, 1149–1155. [Google Scholar] [CrossRef]
- Boyd, N.; Martin, L.; Stone, J.; Little, L.; Minkin, S.; Yaffe, M. A Longitudinal Study of the Effects of Menopause on Mammographic Features. Cancer Epidemiol. Biomark. Prev. 2002, 11, 1048–1053. [Google Scholar]
- Stone, J.; Dite, G.S.; Gunasekara, A.; English, D.R.; McCredie, M.R.; Giles, G.G.; Cawson, J.N.; Hegele, R.A.; Chiarelli, A.M.; Yaffe, M.J.; et al. The heritability of mammographically dense and nondense breast tissue. Cancer Epidemiol. Biomark. Prev. 2006, 15, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.L.; Schmidt, D.F.; Makalic, E.; Dite, G.S.; Stone, J.; Apicella, C.; Bui, M.; Macinnis, R.J.; Odefrey, F.; Cawson, J.N.; et al. Explaining variance in the Cumulus mammographic measures that predict breast cancer risk: A twins and sisters study. Cancer Epidemiol. Biomark. Prev. 2013, 22, 2395–2403. [Google Scholar] [CrossRef]
- Forman, M.R.; Cantwell, M.M.; Ronckers, C.; Zhang, Y. Through the looking glass at early-life exposures and breast cancer risk. Cancer Investig. 2005, 23, 609–624. [Google Scholar] [CrossRef]
- Gluckman, P.D.; Buklijas, T.; Hanson, M.A. Chapter 1—The Developmental Origins of Health and Disease (DOHaD) Concept: Past, Present, and Future. In The Epigenome and Developmental Origins of Health and Disease; Rosenfeld, C.S., Ed.; Academic Press: Boston, MA, USA, 2016; pp. 1–15. [Google Scholar]
- Hilakivi-Clarke, L.; Forsen, T.; Eriksson, J.G.; Luoto, R.; Tuomilehto, J.; Osmond, C.; Barker, D.J. Tallness and overweight during childhood have opposing effects on breast cancer risk. Br. J. Cancer 2001, 85, 1680–1684. [Google Scholar] [CrossRef]
- Ahlgren, M.; Melbye, M.; Wohlfahrt, J.; Sørensen, T.I.A. Growth Patterns and the Risk of Breast Cancer in Women. N. Engl. J. Med. 2004, 351, 1619–1626. [Google Scholar] [CrossRef]
- Warner, E.T.; Hu, R.; Collins, L.C.; Beck, A.H.; Schnitt, S.; Rosner, B.; Eliassen, A.H.; Michels, K.B.; Willett, W.C.; Tamimi, R.M. Height and Body Size in Childhood, Adolescence, and Young Adulthood and Breast Cancer Risk According to Molecular Subtype in the Nurses’ Health Studies. Cancer Prev. Res. 2016, 9, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Andersen, Z.J.; Baker, J.L.; Bihrmann, K.; Vejborg, I.; Sørensen, T.I.A.; Lynge, E. Birth weight, childhood body mass index, and height in relation to mammographic density and breast cancer: A register-based cohort study. Breast Cancer Res. 2014, 16, R4. [Google Scholar] [CrossRef] [PubMed]
- De Stavola, B.L.; dos Santos Silva, I.; McCormack, V.; Hardy, R.J.; Kuh, D.J.; Wadsworth, M.E. Childhood growth and breast cancer. Am. J. Epidemiol. 2004, 159, 671–682. [Google Scholar] [CrossRef] [PubMed]
- Denholm, R.; De Stavola, B.; Hipwell, J.H.; Doran, S.J.; Busana, M.C.; Leach, M.O.; Hawkes, D.J.; Dos Santos Silva, I. Growth Trajectories, Breast Size, and Breast-Tissue Composition in a British Prebirth Cohort of Young Women. Am. J. Epidemiol. 2018, 187, 1259–1268. [Google Scholar] [CrossRef] [PubMed]
- Boyd, N.; Martin, L.; Chavez, S.; Gunasekara, A.; Salleh, A.; Melnichouk, O.; Yaffe, M.; Friedenreich, C.; Minkin, S.; Bronskill, M. Breast-tissue composition and other risk factors for breast cancer in young women: A cross-sectional study. Lancet Oncol. 2009, 10, 569–580. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, K.A.; Baer, H.J.; Orav, E.J.; Klifa, C.; Shepherd, J.A.; Van Horn, L.; Snetselaar, L.; Stevens, V.J.; Hylton, N.M.; Dorgan, J.F. Body fatness during childhood and adolescence and breast density in young women: A prospective analysis. Breast Cancer Res. 2015, 17, 95. [Google Scholar] [CrossRef] [PubMed]
- Rice, M.S.; Bertrand, K.A.; VanderWeele, T.J.; Rosner, B.A.; Liao, X.; Adami, H.-O.; Tamimi, R.M. Mammographic density and breast cancer risk: A mediation analysis. Breast Cancer Res. 2016, 18, 94. [Google Scholar] [CrossRef] [PubMed]
- Schoemaker, M.J.; Jones, M.E.; Allen, S.; Hoare, J.; Ashworth, A.; Dowsett, M.; Swerdlow, A.J. Childhood body size and pubertal timing in relation to adult mammographic density phenotype. Breast Cancer Res. 2017, 19, 13. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulos, D.; Adami, H.O.; Ekbom, A.; Hsieh, C.C.; Lagiou, P. Early life events and conditions and breast cancer risk: From epidemiology to etiology. Int. J. Cancer 2008, 122, 481–485. [Google Scholar] [CrossRef]
- Jung, S.; Egleston, B.L.; Chandler, D.W.; Van Horn, L.; Hylton, N.M.; Klifa, C.C.; Lasser, N.L.; LeBlanc, E.S.; Paris, K.; Shepherd, J.A.; et al. Adolescent endogenous sex hormones and breast density in early adulthood. Breast Cancer Res. 2015, 17, 77. [Google Scholar] [CrossRef]
- Krishnan, K.; Baglietto, L.; Stone, J.; Simpson, J.A.; Severi, G.; Evans, C.F.; MacInnis, R.J.; Giles, G.G.; Apicella, C.; Hopper, J.L. Longitudinal study of mammographic density measures that predict breast cancer risk. Cancer Epidemiol. Biomark. Prev. 2017, 26, 651–660. [Google Scholar] [CrossRef] [PubMed]
- Colditz, G.A.; Frazier, A.L. Models of breast cancer show that risk is set by events of early life: Prevention efforts must shift focus. Cancer Epidemiol. Biomark. Prev. 1995, 4, 567–571. [Google Scholar]
- Denholm, R.; De Stavola, B.; Hipwell, J.H.; Doran, S.J.; Busana, M.C.; Eng, A.; Jeffreys, M.; Leach, M.O.; Hawkes, D.; dos Santos Silva, I. Pre-natal exposures and breast tissue composition: Findings from a British pre-birth cohort of young women and a systematic review. Breast Cancer Res. 2016, 18, 102. [Google Scholar] [CrossRef]
- Russo, J.; Russo, I.H. Breast Development, Hormones and Cancer. Adv. Exp. Med. Biol. 2008, 630, 52–56. [Google Scholar]
- Yochum, L.; Tamimi, R.M.; Hankinson, S.E. Birthweight, early life body size and adult mammographic density: A review of epidemiologic studies. Cancer Causes Control 2014, 25, 1247–1259. [Google Scholar] [CrossRef]
- Hopper, J.L.; Nguyen, T.L.; Stone, J.; Aujard, K.; Matheson, M.C.; Abramson, M.J.; Burgess, J.A.; Walters, E.H.; Dite, G.S.; Bui, M.; et al. Childhood body mass index and adult mammographic density measures that predict breast cancer risk. Breast Cancer Res Treat. 2016, 156, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Berkey, C.S.; Herman, C.R.; Appleton, C.M.; Alimujiang, A.; Colditz, G.A.; Toriola, A.T. Adiposity Change Over the Life Course and Mammographic Breast Density in Postmenopausal Women. Cancer Prev. Res. 2020, 13, 475–482. [Google Scholar] [CrossRef]
- Cole, T.J. Children grow and horses race: Is the adiposity rebound a critical period for later obesity? BMC Pediatr. 2004, 4, 6. [Google Scholar] [CrossRef] [PubMed]
- The Raine Study. Available online: https://rainestudy.org.au/ (accessed on 11 April 2023).
- Blackmore, K.M.; Knight, J.A.; Walter, J.; Lilge, L. The association between breast tissue optical content and mammographic density in pre- and post-menopausal women. PloS ONE 2015, 10, e0115851. [Google Scholar] [CrossRef]
- Shepherd, J.A.; Herve, L.; Landau, J.; Fan, B.; Kerlikowske, K.; Cummings, S.R. Clinical comparison of a novel breast DXA technique to mammographic density: Breast DXA. Med. Phys. 2006, 33, 1490–1498. [Google Scholar] [CrossRef]
- Walter, E.J.; Knight, J.A.; Lilge, L. A multi-wavelength, laser-based optical spectroscopy device for breast density and breast cancer risk pre-screening. J Biophotonics 2017, 10, 565–576. [Google Scholar] [CrossRef] [PubMed]
- Perera, D.; Pirikahu, S.; Walter, J.; Cadby, G.; Darcey, E.; Llyod, R.; Hickey, M.; Saunders, C.; Hackmann, M.; Sampson, D.D.; et al. The distribution of breast density in women aged 18 years and older. Breast Cancer Res. Treat. 2024, 205, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Walter, E.J.; Lilge, L. Optical assessment of mammographic breast density by a 12-wavelength vs a continuous-spectrum optical spectroscopy device. J. Biophotonics 2018, 11, e201700071. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, J.A.; Kerlikowske, K.M.; Smith-Bindman, R.; Genant, H.K.; Cummings, S.R. Measurement of Breast Density with Dual X-ray Absorptiometry: Feasibility. Radiology 2002, 223, 554–557. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Donaldson, M.D.; Ben-Shlomo, Y. SITAR—A useful instrument for growth curve analysis. Int. J. Epidemiol. 2010, 39, 1558–1566. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Zeng, C.J.; Wang, Q.; Dennis, J.; Dunning, A.M.; Czene, K.; Wen, W.; Long, J.; Li, C.; Alison, M.; et al. Height and Breast Cancer Risk: Evidence from Prospective Studies and Mendelian Randomization. J. Natl. Cancer Inst. 2015, 107, djv219. [Google Scholar] [CrossRef] [PubMed]
- Baer, H.J.; Tworoger, S.S.; Hankinson, S.E.; Willett, W.C. Body Fatness at Young Ages and Risk of Breast Cancer Throughout Life. Am. J. Epidemiol. 2010, 171, 1183–1194. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos Silva, I.; Johnson, N.; De Stavola, B.; Torres-Mejía, G.; Fletcher, O.; Allen, D.S.; Allen, N.E.; Key, T.J.; Fentiman, I.S.; Holly, J.M.P.; et al. The Insulin-Like Growth Factor System and Mammographic Features in Premenopausal and Postmenopausal Women. Cancer Epidemiol. Biomark. Prev. 2006, 15, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Diorio, C.; Pollak, M.; Byrne, C.; Masse, B.; Hebert-Croteau, N.; Yaffe, M.; Cote, G.; Berube, S.; Moring, C.; Brisson, J.; et al. Insulin-Like Growth Factor-I, IGF-Binding Protein-3, and Mammographic Breast Density. Cancer Epidemiol. Biomark. Prev. 2005, 14, 1065–1073. [Google Scholar] [CrossRef]
- Biro, F.M.; Huang, B.; Wasserman, H.; Gordon, C.M.; Pinney, S.M. Pubertal Growth, IGF-1, and Windows of Susceptibility: Puberty and Future Breast Cancer Risk. J. Adolesc. Health 2021, 68, 517–522. [Google Scholar] [CrossRef]
- Boyd, N.F.; Stone, J.; Martin, L.J.; Jong, R.; Fishell, E.; Yaffe, M.; Hammond, G.; Minking, S. The association of breast mitogens with mammographic densities. Br. J. Cancer 2002, 87, 876–882. [Google Scholar] [CrossRef] [PubMed]
- Ward, S.; Burton, A.; Tamimi, R.M.; Pereira, A.; Garmendia, M.L.; Pollan, M.; Boyd, N.; Dos Santos Silva, I.; Maskarinec, G.; Perez-Gomez, B.; et al. The association of age at menarche and adult height with mammographic density in the International Consortium of Mammographic Density. Breast Cancer Res. 2022, 24, 49. [Google Scholar] [CrossRef] [PubMed]
- Dorgan, J.F.; Klifa, C.; Shepherd, J.A.; Egleston, B.L.; Kwiterovich, P.O., Jr.; Himes, J.H.; Gabriel, K.; Horn, L.; Snetselaar, L.G.; Stevens, V.J.; et al. Height, adiposity and body fat distribution and breast density in young women. Breast Cancer Res. 2012, 14, R107. [Google Scholar] [CrossRef] [PubMed]
- Sellers, T.A.; Vachon, C.M.; Pankratz, V.S.; Janney, C.A.; Fredericksen, Z.; Brandt, K.R.; Huang, Y.; Counch, F.J.; Kushi, L.H.; Cerhan, J.R.; et al. Association of Childhood and Adolescent Anthropometric Factors, Physical Activity, and Diet with Adult Mammographic Breast Density. Am. J. Epidemiol. 2007, 166, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Lope, V.; Pérez-Gómez, B.; Moreno, M.P.; Vidal, C.; Salas-Trejo, D.; Ascunce, N.; Gonzalez Roman, I.; Sanchez-Contador, C.; Santamarina, M.C.; Vazquez Carrete, J.A.; et al. Childhood factors associated with mammographic density in adult women. Breast Cancer Res. Treat. 2011, 130, 965–974. [Google Scholar] [CrossRef]
- Oh, H.; Boeke, C.E.; Tamimi, R.M.; Smith-Warner, S.A.; Wang, M.; Willett, W.C.; Eliassen, A.H. The interaction between early-life body size and physical activity on risk of breast cancer. Int. J. Cancer 2015, 137, 571–581. [Google Scholar] [CrossRef] [PubMed]
- McCormack, V.A.; dos Santos Silva, I.; De Stavola, B.L.; Perry, N.; Vinnicombe, S.; Swerdlow, A.J.; Hardy, R.; Kuh, D. Life-course body size and perimenopausal mammographic parenchymal patterns in the MRC 1946 British birth cohort. Br. J. Cancer 2003, 89, 852–859. [Google Scholar] [CrossRef] [PubMed]
- Lokate, M.; Kallenberg, M.G.J.; Karssemeijer, N.; Van Den Bosch, M.A.A.J.; Peeters, P.H.M.; Van Gils, C.H. Volumetric breast density from full-field digital mammograms and its association with breast cancer risk factors: A comparison with a threshold method. Cancer Epidemiol. Biomark. Prev. 2010, 19, 3096–3105. [Google Scholar] [CrossRef] [PubMed]
- Aitken, Z.; McCormack, V.A.; Highnam, R.P.; Martin, L.; Gunasekara, A.; Melnichouk, O.; Mawdsley, G.; Peressotti, C.; Yaffe, M.; Boyd, N.F.; et al. Screen-film mammographic density and breast cancer risk: A comparison of the volumetric standard mammogram form and the interactive threshold measurement methods. Cancer Epidemiol. Biomark. Prev. 2010, 19, 418–428. [Google Scholar] [CrossRef] [PubMed]
- Jeffreys, M.; Warren, R.; Highnam, R.; Davey Smith, G. Breast cancer risk factors and a novel measure of volumetric breast density: Cross-sectional study. Br. J. Cancer 2008, 98, 210–216. [Google Scholar] [CrossRef]
- McCormack, V.A.; Highnam, R.; Perry, N.; Silva, I.D.S. Comparison of a new and existing method of mammographic density measurement: Intramethod reliability and associations with known risk factors. Cancer Epidemiol. Biomark. Prev. 2007, 16, 1148–1154. [Google Scholar] [CrossRef] [PubMed]
- Ghadge, A.G.; Dasari, P.; Stone, J.; Thompson, E.W.; Robker, R.L.; Ingman, W.V. Pubertal mammary gland development is a key determinant of adult mammographic density. Semin. Cell Dev. Biol. 2021, 114, 143–158. [Google Scholar] [CrossRef] [PubMed]
- Kaplowitz, P.B.; Slora, E.J.; Wasserman, R.C.; Pedlow, S.E.; Herman-Giddens, M.E. Earlier onset of puberty in girls: Relation to increased body mass index and race. Pediatrics 2001, 108, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Adair, L.S.; Gordon-Larsen, P. Maturational timing and overweight prevalence in US adolescent girls. Am. J. Public Health 2001, 91, 642–644. [Google Scholar] [PubMed]
- Wang, Y. Is obesity associated with early sexual maturation? A comparison of the association in American boys versus girls. Pediatrics 2002, 110, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Appugliese, D.; Kaciroti, N.; Corwyn, R.F.; Bradley, R.H.; Lumeng, J.C. Weight Status in Young Girls and the Onset of Puberty. Pediatrics 2007, 119, e624–e630. [Google Scholar] [CrossRef] [PubMed]
- Houghton, L.C.; Jung, S.; Troisi, R.; Leblanc, E.S.; Snetselaar, L.G.; Hylton, N.M.; Klifa, C.; Van Horn, L.; Paris, K.; Shepherd, J.A.; et al. Pubertal timing and breast density in young women: A prospective cohort study. Breast Cancer Res. 2019, 21, 122. [Google Scholar] [CrossRef] [PubMed]
- Bodicoat, D.H.; Schoemaker, M.J.; Jones, M.E.; McFadden, E.; Griffin, J.; Ashworth, A.; Swerdlow, A.J. Timing of pubertal stages and breast cancer risk: The Breakthrough Generations Study. Breast Cancer Res. 2014, 16, R18. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, R.; Pirikahu, S.; Walter, J.; Cadby, G.; Darcey, E.; Perera, D.; Hickey, M.; Saunders, C.; Karnowski, K.; Sampson, D.D.; et al. Alternative methods to measure breast density in younger women. Br. J. Cancer 2023, 128, 1701–1709. [Google Scholar] [CrossRef]
- Lloyd, R.; Walter, J.; Pirikahu, S.; Cadby, G.; Hickey, M.; Sampson, D.D.; Karnowski, K.; Hackmann, M.J.; Saunders, C.; Lilge, L.; et al. Assessment of repeated reference measurements to inform the validity of optical breast spectroscopy. Rev. Sci. Instrum. 2022, 93, 044101. [Google Scholar] [CrossRef]
- Cuzick, J.; Warwick, J.; Pinney, E.; Duffy, S.W.; Cawthorn, S.; Howell, A.; Forbes, J.F.; Warren, R.M.L. Tamoxifen-induced reduction in mammographic density and breast cancer risk reduction: A nested case-control study. J. Natl. Cancer Inst. 2011, 103, 744–752. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | OBS Chromophore (N = 453) | DXA (N = 253) |
|---|---|---|
| Age at questionnaire (sd) | 27.3 (0.9) | 27.4 (0.7) |
| BMI (sd) | 25.5 (6.1) | 25.5 (6.1) |
| Ethnicity (%) European/Caucasian | 400 (88.3) | 228 (90.1) |
| Asian | 37 (8.2) | 19 (7.5) |
| Other | 16 (3.5) | 6 (2.4) |
| Ever been pregnant (%) Yes | 129 (28.5) | 65 (25.7) |
| No | 322 (71.1) | 186 (73.5) |
| Missing | 2 (0.4) | 2 (0.8) |
| Number of live births (%) 0 | 374 (82.6) | 216 (85.4) |
| 1 | 36 (7.9) | 19 (7.5) |
| 2 | 34 (7.5) | 13 (5.1) |
| 3 or more | 9 (2.0) | 5 (1.9) |
| Age at first birth (sd) | 23.6 (3.0) | 23.7 (3.2) |
| Age at last birth (sd) | 25.4 (2.5) | 25.3 (3.2) |
| Ever or currently breastfeeding (%) Never | 378 (83.4) | 216 (85.4) |
| Former | 49 (10.8) | 28 (11.1) |
| Current | 24 (5.3) | 7 (2.8) |
| Missing | 2 (0.4) | 2 (0.8) |
| Currently using any contraceptives (%) Yes | 301 (66.4) | 167 (66.0) |
| No | 119 (26.3) | 83 (32.8) |
| Missing | 33 (7.3) | 3 (1.2) |
| Contraceptive Type (%) Pill | 146 (32.2) | 80 (31.6) |
| IUD | 37 (8.2) | 28 (11.1) |
| Injection | 33 (7.3) | 17 (6.7) |
| Other | 83 (18.3) | 42 (16.6) |
| No Contraception | 119 (26.3) | 83 (32.8) |
| Not Stated | 35 (7.7) | 3 (1.2) |
| Age of Menarche (sd) | 12.9 (1.5) | 12.9 (1.5) |
| Missing | 7 | 6 |
| Family history of breast cancer (%) No history | 329 (72.6) | 187 (73.9) |
| 1st Degree | 23 (5.1) | 16 (6.3) |
| 2nd Degree | 99 (21.9) | 50 (19.8) |
| Missing | 2 (0.4) | 0 (0.0) |
| Benign Breast Disease—not removed (%) No | 417 (92.1) | 235 (92.9) |
| Yes—Not removed | 34 (7.5) | 17 (6.7) |
| Missing | 2 (0.4) | 1 (0.4) |
| Smoking Status (%) Never | 225 (49.7) | 139 (54.9) |
| Former | 106 (23.4) | 56 (22.1) |
| Current | 53 (11.7) | 21 (8.3) |
| Missing | 69 (15.2) | 37 (14.6) |
| Alcohol consumption (%) Never | 35 (7.7) | 20 (7.9) |
| Ever | 350 (77.3) | 197 (77.9) |
| Missing | 68 (15.0) | 36 (14.2) |
| OBS Cup Size (%) 1 (A) | 149 (32.9) | 85 (33.6) |
| 2 (B) | 113 (24.9) | 63 (24.9) |
| 3 (C) | 129 (28.5) | 74 (29.2) |
| 4 (D) | 62 (13.7) | 31 (12.3) |
| Measurement: (sd) OBS-%water | 15.9 (8.1) | 14..6 (7.7) |
| OBS-%lipid | 50.7 (13.4) | 53.4 (13.2) |
| OBS-%collagen | 18.4 (7.1) | 18.1 (7.4) |
| OBS-%water + collagen | 34.4 (10.7) | 32.7 (10.2) |
| DXA %FGV | 46.6 (17.8) | |
| DXA FGV (cm3) | 240.0 (112.7) | |
| DXA NFGV (cm3) | 350.8 (291.6) |
| SITAR Model Growth Parameters | Height Min, Max (sd) | Weight Min, Max (sd) | BMI Min, Max (sd) |
|---|---|---|---|
| Size (cm) | −21.5, 16.1 (6.3) | −20.6, 65.9 (13.0) | −7.1, 18.0 (4.0) |
| Timing (years) | −2.6, 3.1 (0.9) | −2.3, 7.7 (1.6) | |
| Velocity (fractional) | −0.4, 0.5 (0.1) | −0.4, 1.0 (0.2) | −0.6, 1.7 (0.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lloyd, R.; Pirikahu, S.; Walter, J.; Cadby, G.; Warrington, N.; Perera, D.; Hickey, M.; Saunders, C.; Hackmann, M.; Sampson, D.D.; et al. The Prospective Association between Early Life Growth and Breast Density in Young Adult Women. Cancers 2024, 16, 2418. https://doi.org/10.3390/cancers16132418
Lloyd R, Pirikahu S, Walter J, Cadby G, Warrington N, Perera D, Hickey M, Saunders C, Hackmann M, Sampson DD, et al. The Prospective Association between Early Life Growth and Breast Density in Young Adult Women. Cancers. 2024; 16(13):2418. https://doi.org/10.3390/cancers16132418
Chicago/Turabian StyleLloyd, Rachel, Sarah Pirikahu, Jane Walter, Gemma Cadby, Nicole Warrington, Dilukshi Perera, Martha Hickey, Christobel Saunders, Michael Hackmann, David D. Sampson, and et al. 2024. "The Prospective Association between Early Life Growth and Breast Density in Young Adult Women" Cancers 16, no. 13: 2418. https://doi.org/10.3390/cancers16132418





