Simple Summary
Telomere length (TL) may influence the carcinogenesis process. Short telomeres lead to genomic instability, which is an important event in tumor initiation, while long telomeres may promote cell division and immortality influencing tumor promotion/progression. Despite the numerous observational epidemiological studies available, the association between TL in leukocytes (LTL) and lung cancer risk is currently still uncertain. Therefore, we conducted this systematic review and meta-analysis of prospective studies to summarize the evidence and derive a more accurate estimate of the effect of LTL on lung cancer occurrence. Longer LTL could be a marker to identify subjects at high risk of developing lung cancer. This may help to focus secondary prevention (screening) on specific groups of subjects.
Abstract
Although numerous epidemiological studies are available, the relationship between leukocyte telomere length (LTL) and lung cancer risk is still controversial. This systematic review and meta-analysis, performed according to the PRISMA statement and MOOSE guidelines, aims to summarize the evidence and calculate the risk of lung cancer associated with LTL. The literature search was performed on PubMed, Web of Science, and Scopus databases through May 2024. A random-effects model was used to calculate the pooled risk. Heterogeneity was assessed using I2 and Cochran’s Q statistic. Begg’s and Egger’s tests were used to detect publication bias. Based on 8055 lung cancer cases and 854,653 controls (nine prospective studies), longer LTL was associated with a significant 42% increment in all types of lung cancer risk (OR 1.42, 95% CI 1.24–1.63). The effect was even more evident for adenocarcinomas (OR 1.98, 95% CI 1.69–2.31), while no association was observed for squamous cell carcinoma (OR 0.87, 95% CI 0.72–1.06). Significantly, no association was found for current smokers (OR 1.08, 95% CI 0.90–1.30), while it remained high for both never-smokers (OR 1.92, 95% CI 1.62–2.28) and former smokers (OR 1.34, 95% CI 1.11–1.62). No significant publication bias was evidenced. Longer LTL is associated with an increment in lung cancer risk particularly in never-smoker subjects.
1. Introduction
Telomeres, small repetitive DNA sequences (5′-TTAGGG-3′) associated with a protein complex (shelterin proteins) at the end of chromosomes, have an important role for maintaining stability and integrity of genomes [1,2]. During cell division, because of the incomplete DNA duplication and in the absence of telomerases (an enzyme that catalyzes the addition of telomeric repeats), telomeres lose approximately 50–200 bp each mitotic cycle, becoming shorter [1,2]. When telomere length reaches a critical point, it signals the arrest of cell proliferation, the induction of cellular senescence, and apoptosis [3]. Telomere length (TL) is, thus, a retained “molecular clock”, useful as a biomarker of aging [4]. However, TL may be influenced by many other factors including gender [5], genetic polymorphisms [6], physical activity and smoking [7], air pollution and oxidative stress [8], nutritional status [9], inflammation [10], and cancer therapies [11]. Therefore, TL varies widely even among individuals with the same chronological age.
TL can be estimated either genetically, by identification of several TL-associated SNPs; or measured directly—generally in leukocytes (LTL) as easily obtainable surrogate cells—by various laboratory techniques [12]. Both genetically determined TL and measured LTL have been associated with different health outcomes including cardiovascular diseases, diabetes, Alzheimer’s disease, and various cancers [13,14]. However, the real association between LTL and cancer risk is controversial because telomeres may have dual roles in carcinogenesis: short telomeres lead to genomic instability, which is an important event in tumor initiation, while long telomeres may promote cell division and immortality, influencing tumor promotion/progression [15]. Indeed, previous meta-analyses have found no association between LTL and all cancers combined [16], breast [17], colorectal [18], prostate [19], and lung cancer risk [20]; however, others have found a positive association between short telomere length with an increased risk in all cancers combined [21], and gastrointestinal, head, and neck cancers [22]. Finally, longer LTL was associated with an increase in all cancer combined and lung cancer risks [23], as well as genetic variants related to longer telomeres associated with an increase in prostate cancer [24] and renal cell carcinoma [25].
Lung cancer is the most frequently diagnosed cancer and is still the leading cause of cancer death worldwide [26]. The temporal and spatial differences in the incidence and mortality of lung cancer reflect the different prevalence of smoking, which represents the main risk factor for this disease [26]. However, other important characteristics such as air pollution and an unhealthy diet can influence the risk of lung cancer with a significant impact, especially on non-smokers [27,28]. As reported above, in previous studies, the risk of lung cancer was not associated with LTL or was associated with a longer TL [20,23]. These differences may be due to several factors that may have an impact on TL measurement in different studies. In addition to the age of the subjects at the time of blood sampling and the accuracy of the methods used for TL assessment, the results may depend more profoundly on the different types of studies included. The true association between telomere length and cancer risk may be misled by the study design, whether case-control or cohort. It has been shown that both the presence of cancer and anticancer therapies can shorten telomere length [11]. Therefore, in case-control studies, which enroll subjects who have already developed the disease and who have likely been treated with anticancer therapies, the results may be biased and reflect reverse causality [23]. In other words, the shorter telomere in cases is due to the condition of this group of subjects that does not exist in controls.
The present meta-analysis therefore aimed to investigate the association between LTL and lung cancer risk by selecting only those studies (prospective cohort studies and nested case-control studies) that used DNA samples collected before cancer diagnosis for LTL measurement.
2. Materials and Methods
The present systematic review and meta-analysis was carried out and reported following the MOOSE (Meta-analysis Of Observational Studies in Epidemiology) guidelines and the PRISMA (preferred reporting items for systematic reviews and meta-analyses) statement [29,30]. The study protocol was registered in the International Prospective Register of Systematic Reviews (www.crd.york.ac.uk/PROSPERO/ (accessed on 1 March 2024), Registration No: CRD42024514266).
2.1. Systematic Search Strategy
A wide literature search was conducted up to May 2024 and without restrictions on the following databases: PubMed (http://www.ncbi.nlm.nih.gov/pubmed/ (accessed on 1 May 2024)), Web of Science (http://wokinfo.com/ (accessed on 1 May 2024)), and Scopus (https://www.scopus.com/ (accessed on 1 May 2024)). The PICO (Population, Intervention/exposure, Comparison, Outcome/event) framework was used to determine the eligibility of studies as follows: population (healthy adult participants or adult patients with lung cancer), exposure (measured telomere length in leucocyte DNA), comparison (longer leucocyte telomere length versus shorter leucocyte telomere length) and outcome (lung cancer, lung adenocarcinoma, lung squamous cell carcinoma). Articles of interest were identified using a combination of the following Medical Subject Headings (MeSH) terms and keywords: (cancer OR tumor OR tumour OR neoplasm OR “neoplastic disease”) AND “telomere length” AND lung. Furthermore, to find out additional publications of interest, we examined the reference list of included articles and recent relevant reviews.
2.2. Inclusion and Exclusion Criteria for Study Selection
Studies were considered eligible for inclusion if they met the following criteria: (i) investigated the relationship between measured LTL and lung cancer risk in adult subjects; (ii) presented a prospective study design (cohort studies and nested case-control studies) that used DNA samples extracted from peripheral blood and collected before cancer diagnosis; (iii) reported multivariate-adjusted lung cancer risk estimates (RR, OR, or HR) with 95% confidence intervals (CI) across LTL categories; (iv) the reference group in the categorical analysis being the longest or shortest LTL.
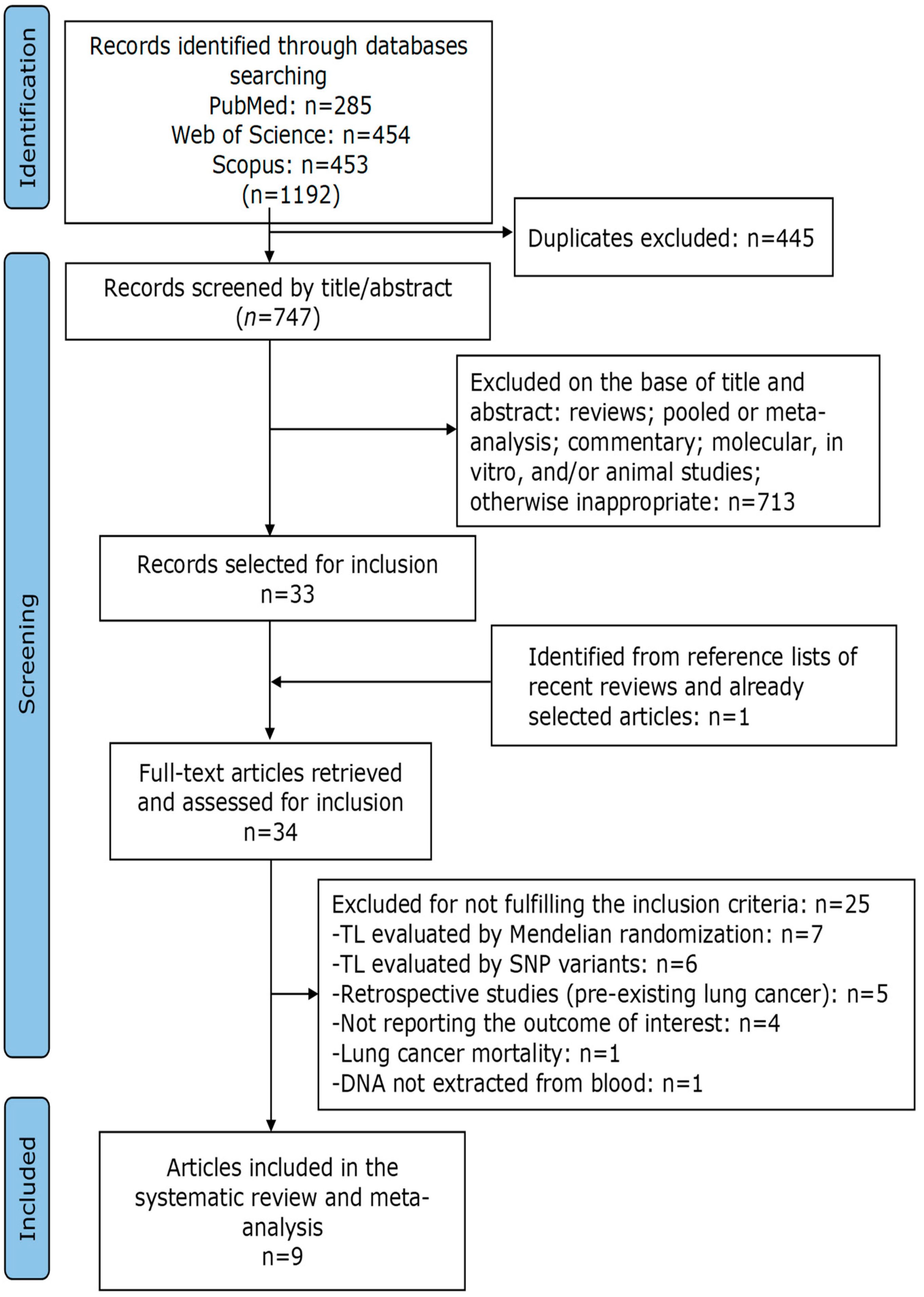
Exclusion criteria were as follows: (i) LTL were genetically predicted by SNPs variants and/or Mendelian randomization; (ii) presented a case-control study design; (iii) reported data on lung cancer mortality; (iii) DNA was not extracted from blood; (iv) the subjects enrolled had another disease in addition to lung cancer. Duplicates, reviews, meta-analyses, comments, editorials, abstracts, summaries, and in vitro, animal, and ecological studies were excluded. Initially, the selection of articles was performed considering the title and abstract, and then the main text was evaluated for all studies not discarded in the first phase. Two authors (R.F. and M.C.) independently performed the study selection. Discrepancies were resolved by discussion with a third author (P.R.). The list of selected studies, the removal of duplicates, and the selection of studies of interest were managed with Zotero. Figure 1 shows the details of the study selection process.
Figure 1.
PRISMA flowchart of the selection process of included studies.
2.3. Data Extraction and Quality Assessment
Two authors (R.F. and P.R.) independently extracted from each selected article the following information: first author, year of publication, location, study design and name, population characteristics (number of cases and controls, incident cases, length of follow-up, age), DNA source and extraction method, TL measurement method, histologic type of lung cancer, telomere length parametrization (units), OR/RR/HR (95% CI) according to gender and smoking habit, matched or adjusted variables, and quality of the study (NOS scores). When multiple estimates were reported in the article, those adjusted for the most confounding factors were extracted. The quality evaluation of the selected studies was performed according to the “Newcastle Ottawa Scale” (NOS) [31]. NOS used a star system, with a total score ranging from 0 to 9. An NOS score equal or superior to 7 indicated a high-quality study. Two investigators individually performed the quality evaluation of each selected study and disagreements were settled by a joint reevaluation of the original article with a third author.
2.4. Statistical Analysis
We estimated the association between LTL and lung cancer risk using the statistical program ProMeta version 3.0 (IDo Statistics-Internovi, Cesena, Italy). The relative risk and hazard ratio were taken as an approximation to the OR, and the meta-analysis was performed as if all types of ratios were ORs. The selected studies divided the LTL into tertile, quartile, and quintile. The combined risk estimates were calculated considering as reference the first quantile (shorter LTL) and the last quantile (longest LTL) using a random effect model.
Heterogeneity between studies was evaluated by the chi-square-based Cochran’s Q statistic and the I2 statistic and considered significant if p < 0.05 or I2 > 50% [32,33].
Publication biases were detected by Begg’s and Egger’s tests [34,35]. Both methods were tested for funnel plot asymmetry—the former was based on the rank correlation between the effect estimates and their sampling variances, and the latter was based on a linear regression of a standard normal deviation on its precision. If a potential bias was detected, we further conducted a sensitivity analysis to assess the robustness of the combined effect estimates, the possible influence of the bias, and to have the bias corrected. We also conducted a sensitivity analysis to investigate the influence of a single study on the overall risk estimate by omitting one study in each turn. We considered the funnel plot to be asymmetrical if the intercept of Egger’s regression line deviated from zero with a p-value < 0.05.
3. Results
3.1. Study Selection
As shown in Figure 1, a total of 1192 articles were identified from the initial search of three different databases.
After removing 445 duplicates, 747 articles remained for title and abstract analysis. Of these, 713 articles were excluded because they were inappropriate. Thirty-three records were selected and one was identified from the bibliography lists of already selected articles, so that thirty-four manuscripts were ultimately included for full-text analysis. Twenty-five items were excluded because they did not meet the inclusion criteria. Specifically, seven studies genetically predicted LTL using Mendelian randomization, five studies genetically predicted LTL using SNP variants, six studies used a retrospective case-control design, four studies did not report lung cancer risk, one study reported the risk of lung cancer mortality, one study did not extract DNA from blood, and one study looked at subjects with COPD (Chronic Obstructive Pulmonary Disease). The list of excluded articles with their reasons is given in Supplementary Table S1. Ultimately, nine articles [36,37,38,39,40,41,42,43,44] were selected for inclusion in the systematic review and meta-analysis (Figure 1).
3.2. Study Characteristics and Quality Assessment
The main characteristics of the included studies are reported in Table 1. Of the nine studies selected, four were conducted in China [37,39,40,43], two in the UK [36,38], two in the USA [41,42], and one in Finland [44]. Four were cohort studies [36,38,39,40] and five were nested case-control [37,41,42,43,44]. The DNA used to assess LTL was extracted from whole blood in eight studies, while in one study, DNA was extracted from buffy coats [43]. The DNA extraction methods used phenol–chloroform in three studies [37,43,44], cartridge-based magnetic bead in three studies [36,38,42], and QIAamp (Qiagen kit) in three studies [39,40,41]. Only one study used a Singleplex qPCR to determine LTL [41], while all the others used a Multiplex qPCR. In all studies, the LTL was expressed as a T/S ratio, which is the telomere repeat copy number (T) relative to that of a single copy gene (S). Risk estimates were calculated in relation to different LTL categories, tertiles were used in two studies [41,43], quartiles in four studies [36,37,42,44], and quintiles in three studies [38,39,40]. Seven studies reported the risk estimates for all types of lung cancer [36,37,38,41,42,43,44], all studies reported the risk estimated for adenocarcinoma, while the risk for squamous cell carcinoma was reported in six studies [36,38,40,41,42,44].

Table 1.
Characteristics of the studies included in the meta-analysis on the association between LTL and lung cancer risk.
The results of the quality assessment, expressed as the NOS score, are reported in the last right column of Table 1. The quality score ranged from 6 to 9. Only one study reported a score of 6 [42], six studies reported a score of 7 [27,36,38,41,43,44], one study reported a score of 8 [39], and one study reported a score of 9 [40].
3.3. Meta-Analysis
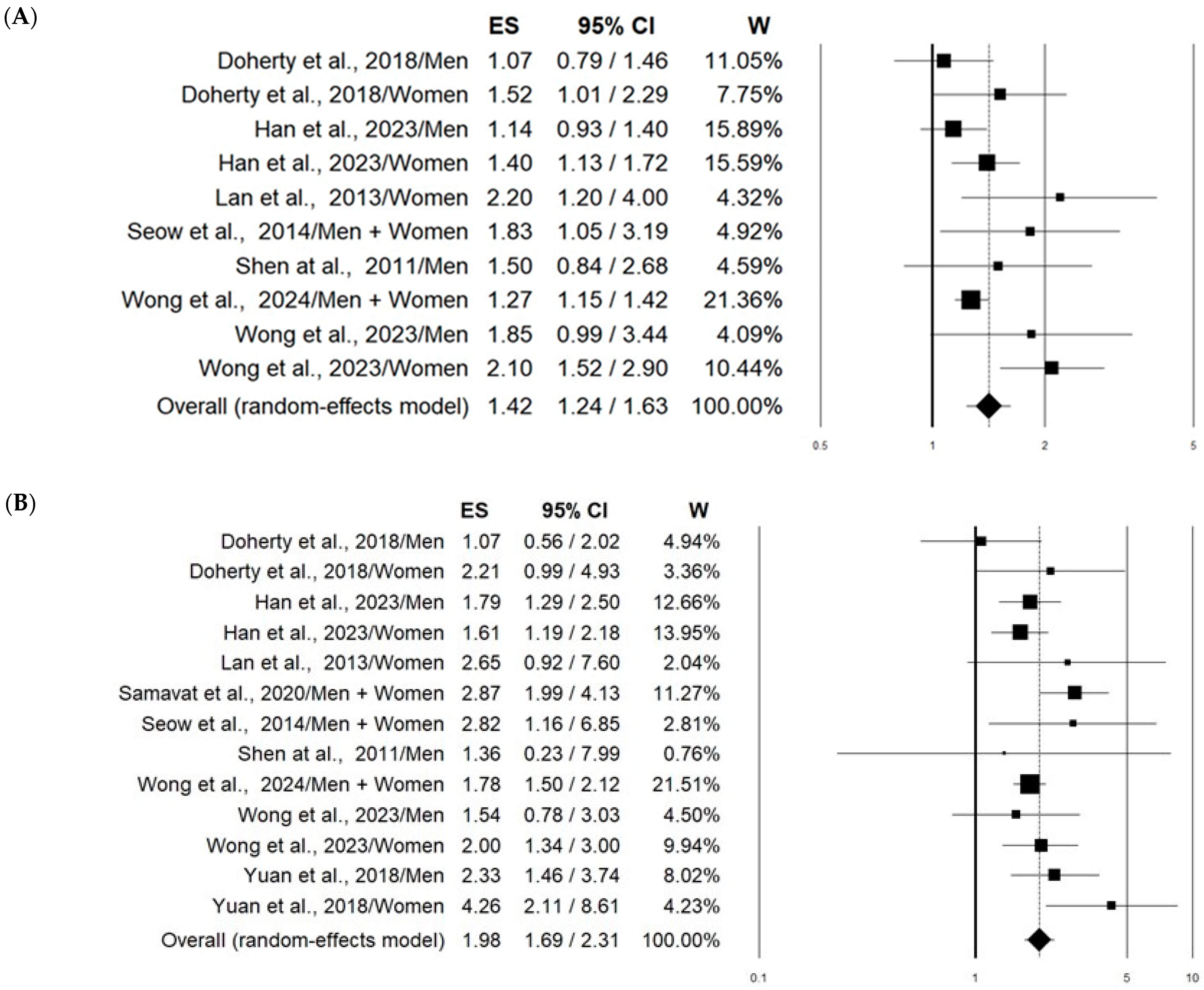
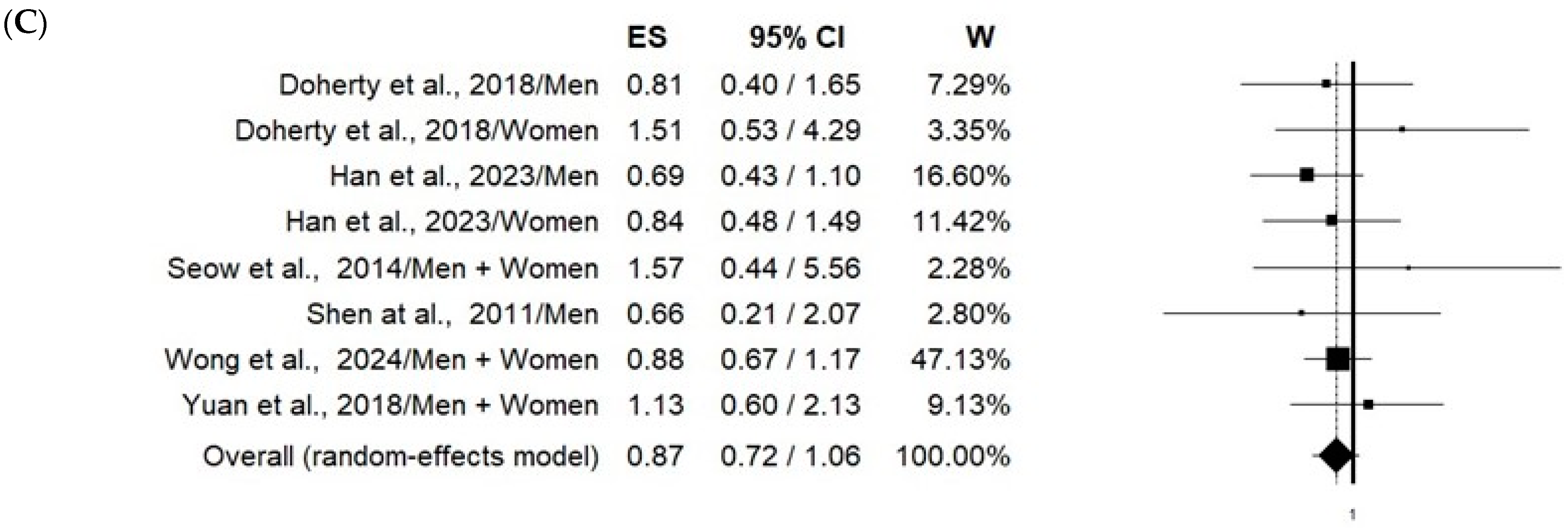
Based on a total of 8055 lung cancer cases and 854,653 controls, the pooled estimates—comparing the longest LTL categories with the shortest—resulted in a statistically significant 42% increment in all types of lung cancer risk (OR 1.42, 95% CI 1.24–1.63) with moderate heterogeneity between studies (I2 =51%, p = 0.031) (Figure 2A). Even more evident was the increment in adenocarcinoma risk associated with the longest LTL, which was found to be 98% (OR 1.98, 95% CI 1.24–1.63) with no significant heterogeneity (I2 = 31%, p = 0.134) (Figure 2B). On the other hand, no significant association with squamous cell carcinoma was found (OR 0.87, 95% CI 0.72–1.06) (Figure 2C).
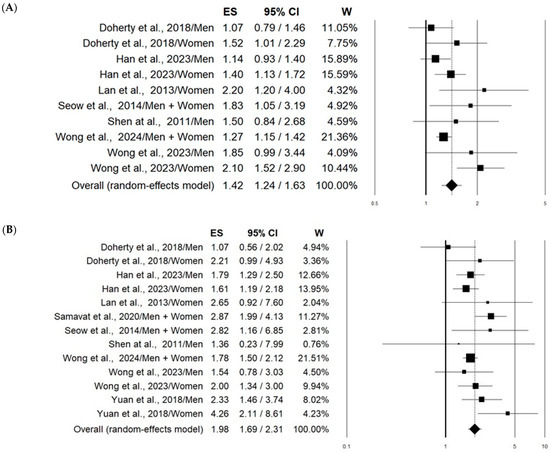
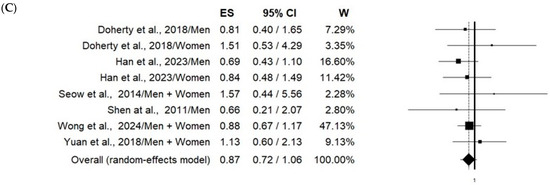
Figure 2.
Forest plots showing the association between telomere length (comparing longest vs. shortest) in peripheral blood leukocytes and risk of all types of lung cancer (A) [36,37,38,41,42,43,44], adenocarcinoma (B) [36,37,38,39,40,41,42,43,44], and squamous cell carcinoma (C) [36,38,40,41,42,44].
The results of the stratified analysis according to gender, smoking habit, and the DNA extraction methods of lung cancer risk estimates associated with the longest LTL are shown in Table 2.

Table 2.
Results of stratified analysis of lung cancer risk estimates associated with the longest LTL.
When all types of lung cancer were considered, the increment in risk in women was higher than in men (68% vs. 19%). Similar effects were observed for adenocarcinoma, the increment in risk was higher in women compared to men (114% vs. 75%). In the case of squamous cell carcinomas, no significant variations in risk were observed in both women and men (Table 2).
Regarding the smoking status, no association between longer LTL and all types of lung cancer was observed in current smokers, while the highest effect (92% increment in risk) was obtained in never-smokers (Table 2). For adenocarcinomas, a significant increment in risk was also noted in current smokers (78%), even if the highest effect was reported in never-smokers (121%). In regard to squamous cell carcinomas, no significant effect was observed in association with smoking status (Table 2).
The analysis of all types of lung cancer risk stratified by the DNA extraction methods shows that the phenol–chloroform method was associated with a higher estimate compared to both the magnetic beads and QIAamp methods. In this last case, the result was not statistically significant (Table 2). Instead, in the case of adenocarcinoma, the higher estimate was observed for the QUIamp method compared to both phenol–chloroform and magnetic beads methods (Table 2). Lung squamous cell carcinoma risk values did not display statistical significance for all three types of methods used to extract DNA (Table 2).
3.4. Sensitivity Analysis
Sensitivity analyses investigating the influence of a single study on the lung risk estimates suggested that these were not substantially modified by any single study. Indeed, the risk estimates for all types of lung cancer ranged from 1.32 (95% CI 1.18–1.46) when removing Wong et al. 2023 [36] to 1.48 (95% CI 1.24–1.63) when removing Han et al. 2023 [38]. The adenocarcinoma risk estimates ranged from 1.85 (95% CI 1.62–2.12) when removing Samavat et al. 2020 [39] to 2.05 (95% CI 1.72–2.44) when removing Han et al. 2023 [3]. Finally, the risk estimates ranged from 0.85 (95% CI 0.70–1.04) when removing Yuan et al. 2018 [40] to 0.92 (95% CI 0.74–1.13) when removing Han et al. 2023 [38] for squamous cell carcinoma.
3.5. Pubblication Bias
No significant publication bias was detected with both Egger’s and Begg’s methods, as shown by the p values (Table 2) and funnel plots (Supplementary Figure S1).
4. Discussion
In the present meta-analysis, based on nine prospective studies, we found a strong association between longer LTL and overall lung cancer risk. The association was more pronounced for adenocarcinoma, in women, and in never-smoker subjects.
These findings are inconsistent with a previous meta-analysis by Karimi et al. [20], who found a non-statistically significant increase in overall lung cancer risk (OR = 1.13, 95% CI: 0.82–1.81) in association with shorter LTL. In addition, they found a smaller effect for adenocarcinoma (OR = 1.00, 95% CI: 0.68–1.47) and a bigger effect for squamous cell carcinoma (OR = 1.78, 95% CI: 1.25–2.53). These differences can essentially be explained by the different studies included in the two meta-analyses. The previous meta-analysis was based on a total of eight studies, including five case-control studies that were excluded from our meta-analysis. Moreover, we have included six additional prospective studies [36,37,38,39,40,41] that were published after the publication of Karimi’s article. We retain that the study design, prospective vs. retrospective, can significantly influence the results. In particular, the lag time of LTL measurement after the onset of lung cancer can increase the likelihood of reverse causation bias. For this reason, we excluded case-control studies in which LTL was measured in patients with the disease. Accordingly, our data are in agreement with another meta-analysis by Zhang et al. [23], who reported a statistically significant increase in lung cancer risk in association with longer LTL (OR: 1.690; 95% CI: 1.253–2.280), based on three prospective studies, which we also included in our meta-analysis [42,43,44].
Our results are further supported by other studies in which the LTL has been genetically determined. Indeed, several Mendelian randomization (MR) investigations—based on a random assortment of genetic variants—suggest a causal relationship between longer LTL and increased lung cancer risk in both Western [45,46] and Asian [47,48] populations. In particular, Zang et al. noted a highly statistically significant increment in lung adenocarcinoma risk per 1 kb increase in LTL (OR: 2.78; 95% CI 2.16–3.58) [45]. Similarly, Kachuri et al. by MR analysis estimated that a 1 kb increase in TL increases the risk of lung cancer (OR: 1.41; 95% CI 1.20–1.65) and lung adenocarcinoma (OR = 1.92; 95% CI 1.51–2.22) but not squamous lung carcinoma (OR: 1.04, 95% CI 0.83–1.29) [46]. Furthermore, similar results in different histological subtypes were reported by Cao et al., who showed that genetic estimation of a longer LTL was strongly associated with lung adenocarcinoma risk (OR: 2.69; 95% CI 2.11–3.42), while lung squamous cell carcinoma showed a marginal association (OR: 1.45; 95% CI 1.01–2.10) [48]. All these data are of particular importance because they should avoid reverse causality errors and not be altered by various confounding factors, which may not be fully controlled in observational studies. In addition, they are in agreement with our results, showing a strong effect on adenocarcinoma and marginal effect on squamous cell carcinoma.
Although in the meta-analysis we noted a low level of heterogeneity, a stratification analysis was carried out considering three important characteristics that may influence the association between LTL and lung cancer risk: gender, smoking habit, and the DNA extraction method. When stratified by gender, we found a stronger association of lung cancer risk in women compared to men. We have no explanation for this effect. We can consider that a meta-analysis showed that on average females had longer telomeres than males [5], and men may be more exposed to factors, including alcohol and smoking, that can shorten telomeres [49]. Indeed, we also found that the association among nonsmokers was higher than among smokers. It is possible that smoking—as a potent determinant of lung cancer—by causing the shortening of telomeres masks the effect of LTL on lung cancer risk estimates. In regard to the DNA extraction methods, we observed contrasting results for the QIAamp method, which produced a non-significant association for all types of lung cancer while being more effective toward adenocarcinoma. Indeed, different methods have been shown to produce pronounced differences in the relative telomere length [50]. In addition, together with DNA extraction methods, the experimental conditions (sample selection, collection, and storage) and, in particular, the assay procedures used to evaluate LTL are very important factors to consider [51]. However, in our meta-analysis, almost all of the studies selected (eight out of nine) used the same Multiplex qPCR method to measure telomere length. Therefore, we did not stratify according to this parameter. Further studies using standardized protocols for the assay itself are necessary to clarify all these methodological aspects.
Regarding the biological plausibility of our findings, it is not surprising that longer telomeres are associated with an increased risk of lung cancer. As mentioned above, the genetic determination of LTL is also consistent with our data. It should be considered that telomere length maintenance is a key step in tumorigenesis and a universal feature of immortalized tumor cells [52]. Cells possessing long telomeres may have a greater replicative capacity because signals produced by short telomeres are less effective in triggering senescence and apoptosis. This allows for continued cell division and increased DNA mutations that may be the basis for cancer development [53]. Some evidence suggests that long telomeres predispose to other cancers besides lung cancer, including acute myeloid leukemia, chronic lymphocytic leukemia, and melanoma [54]. Furthermore, longer leukocyte telomeres have been found to be a significant risk factor for the development of myeloproliferative neoplasms [54].
Our study presents several strengths and limitations. Unlike the previous meta-analysis, we selected only prospective studies, which are less subject to reverse causality bias than retrospective studies. Furthermore, the results were obtained from a substantial number of lung cancer cases, and no evident heterogeneity or significant publication biases were observed. All the included studies included very important characteristics, such as age, gender, and smoking habits in the matched or adjusted variables. This also enabled us to stratify the risk estimates according to gender and smoking habit.
However, due to several limitations, the results reported in this meta-analysis should be interpreted with caution. First, the included studies were observational and, although the quality was quite high (as evidenced by the NOS analysis), they may be subject to risk of bias due to misclassification of the included subjects. Second, although the method used to measure LTL was the same for most studies (Multiplex qPCR), the definition of relative telomere length (reported as T/S ratio) varied among the included studies. This may compromise the reliability of the results and prevent definitive conclusions. Third, the categorization of LTLs into different quantiles (tertiles, quartiles, and quintiles) in various studies can be a further source of data variability and uncertainty. Finally, the use of leukocytes to determine TL may not be truly representative of TL in target lung cells. TL varies between organs and tissue types within an individual, although it has been observed to be highly correlated [55]. However, it is evident that no study has assessed telomere length in cells that are difficult to obtain via invasive procedures.
5. Conclusions
Considering only prospective studies, a longer LTL was significantly associated with an increased risk of lung cancer. The effect was more evident for the adenocarcinoma subtype, in women, and in never-smokers. Due to the complex role that telomere length may play in this phenomenon, further larger studies—adequately designed and standardized for different analytical methods—are needed to validate these results and highlight the biological mechanisms that may be involved.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers16183218/s1, Figure S1: Funnel plots of the meta-analysis on all types of lung cancer (A), adenocarcinoma (B), and squamous cell carcinoma (C); Table S1: List of articles excluded from the meta-analysis and reasons for exclusion. References [45,46,47,48,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76] are cited in the Supplementary Materials.
Author Contributions
Conceptualization: initiated by R.F., agreed by all other authors M.C., P.R., and I.G.; methodology: from the literature search for meta-analysis, R.F., M.C., P.R., and I.G.; formal analysis: meta-analysis, R.F. and M.C.; data curation: M.C., P.R., and I.G.; writing, original draft preparation, R.F., M.C., and P.R.; writing, review, and editing, R.F., M.C., P.R., and I.G.; supervision, M.C. and R.F.; project administration, R.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The data presented in this study are available in this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Lu, W.; Zhang, Y.; Liu, D.; Songyang, Z.; Wan, M. Telomeres-structure, function, and regulation. Exp. Cell Res. 2013, 319, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Alanazi, A.F.R.; Parkinson, G.N.; Haider, S. Structural Motifs at the Telomeres and Their Role in Regulatory Pathways. Biochemistry 2024, 63, 827–842. [Google Scholar] [CrossRef]
- Smith, E.M.; Pendlebury, D.F.; Nandakumar, J. Structural biology of telomeres and telomerase. Cell Mol Life Sci. 2020, 77, 61–79. [Google Scholar] [CrossRef]
- Mather, K.A.; Jorm, A.F.; Parslow, R.A.; Christensen, H. Is telomere length a biomarker of aging? A review. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 202–213. [Google Scholar] [CrossRef]
- Gardner, M.; Bann, D.; Wiley, L.; Cooper, R.; Hardy, R.; Nitsch, D.; Martin-Ruiz, C.; Shiels, P.; Sayer, A.A.; Barbieri, M. Gender and telomere length: Systematic review and meta-analysis. Exp. Gerontol. 2014, 51, 15–27. [Google Scholar] [CrossRef]
- Nelson, C.P.; Codd, V. Genetic determinants of telomere length and cancer risk. Curr. Opin. Genet. Dev. 2020, 60, 63–68. [Google Scholar] [CrossRef]
- Barragán, R.; Ortega-Azorín, C.; Sorlí, J.V.; Asensio, E.M.; Coltell, O.; St-Onge, M.P.; Portolés, O.; Corella, D. Effect of Physical Activity, Smoking, and Sleep on Telomere Length: A Systematic Review of Observational and Intervention Studies. J. Clin. Med. 2021, 11, 76. [Google Scholar] [CrossRef]
- Assavanopakun, P.; Sapbamrer, R.; Kumfu, S.; Chattipakorn, N.; Chattipakorn, S.C. Effects of air pollution on telomere length: Evidence from in vitro to clinical studies. Environ. Pollut. 2022, 312, 120096. [Google Scholar] [CrossRef]
- D’Angelo, S. Diet and Aging: The Role of Polyphenol-Rich Diets in Slow Down the Shortening of Telomeres: A Review. Antioxidants 2023, 12, 2086. [Google Scholar] [CrossRef]
- Jose, S.S.; Bendickova, K.; Kepak, T.; Krenova, Z.; Fric, J. Chronic Inflammation in Immune Aging: Role of Pattern Recognition Receptor Crosstalk with the Telomere Complex? Front. Immunol. 2017, 8, 1078. [Google Scholar] [CrossRef]
- Gallicchio, L.; Gadalla, S.M.; Murphy, J.D.; Simonds, N.I. The Effect of Cancer Treatments on Telomere Length: A Systematic Review of the Literature. J. Natl. Cancer Inst. 2018, 110, 1048–1058. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.J.; Byun, Y.H.; Park, C.K. Techniques for assessing telomere length: A methodological review. Comput. Struct. Biotechnol. J. 2024, 23, 1489–1498. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Yan, Y.; Wang, H.; Xu, J. Association between genetically determined telomere length and health-related outcomes: A systematic review and meta-analysis of Mendelian randomization studies. Aging Cell 2023, 22, e13874. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.; Luchini, C.; Demurtas, J.; Soysal, P.; Stubbs, B.; Hamer, M.; Nottegar, A.; Lawlor, R.T.; Lopez-Sanchez, G.F.; Firth, J. Telomere length and health outcomes: An umbrella review of systematic reviews and meta-analyses of observational studies. Ageing Res. Rev. 2019, 51, 1–10. [Google Scholar] [CrossRef]
- Savage, S.A. Telomere length and cancer risk: Finding Goldilocks. Biogerontology 2024, 25, 265–278. [Google Scholar] [CrossRef]
- Giaccherini, M.; Gentiluomo, M.; Fornili, M.; Lucenteforte, E.; Baglietto, L.; Campa, D. Association between telomere length and mitochondrial copy number and cancer risk in humans: A meta-analysis on more than 300,000 individuals. Crit. Rev. Oncol. Hematol. 2021, 167, 103510. [Google Scholar] [CrossRef]
- Benites-Zapata, V.A.; Ulloque-Badaracco, J.R.; Alarcón-Braga, E.A.; Fernández-Alonso, A.M.; López-Baena, M.T.; Pérez-López, F.R. Telomerase activity and telomere length in women with breast cancer or without malignancy: A systematic review and meta-analysis. Maturitas 2024, 180, 107882. [Google Scholar] [CrossRef]
- Naing, C.; Aung, K.; Lai, P.K.; Mak, J.W. Association between telomere length and the risk of colorectal cancer: A meta-analysis of observational studies. BMC Cancer 2017, 17, 24. [Google Scholar] [CrossRef]
- Hu, R.; Hua, X.G.; Jiang, Q.C. Associations of telomere length in risk and recurrence of prostate cancer: A meta-analysis. Andrologia 2019, 51, e13304. [Google Scholar] [CrossRef]
- Karimi, B.; Yunesian, M.; Nabizadeh, R.; Mehdipour, P.; Aghaie, A. Is Leukocyte Telomere Length Related with Lung Cancer Risk?: A Meta-Analysis. Iran. Biomed. J. 2017, 21, 142–153. [Google Scholar] [CrossRef]
- Ma, H.; Zhou, Z.; Wei, S.; Liu, Z.; Pooley, A.; Dunning, A.M.; Svenson, U.; Roos, G.; Hosgood, H.D.; Shen, M.; et al. Shortened telomere length is associated with increased risk of cancer: A meta-analysis. PLoS ONE 2011, 6, e20466. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Han, W.; Xue, W.; Zou, Y.; Xie, C.; Du, J.; Jin, G. The association between telomere length and cancer risk in population studies. Sci. Rep. 2016, 6, 22243. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhao, Q.; Zhu, W.; Liu, T.; Xie, S.H.; Zhong, L.X.; Cai, Y.Y.; Li, X.N.; Liang, M.; Chen, W.; et al. The Association of Telomere Length in Peripheral Blood Cells with Cancer Risk: A Systematic Review and Meta-analysis of Prospective Studies. Cancer Epidemiol. Biomarkers Prev. 2017, 26, 1381–1390. [Google Scholar] [CrossRef]
- Wan, B.; Lu, L.; Lv, C. Mendelian randomization study on the causal relationship between leukocyte telomere length and prostate cancer. PLoS ONE 2023, 18, e0286219. [Google Scholar] [CrossRef]
- Machiela, M.J.; Hofmann, J.N.; Carreras-Torres, R.; Brown, K.M.; Johansson, M.; Wang, Z.; Foll, M.; Li, P.; Rothman, N.; Savage, S.A.; et al. Genetic Variants Related to Longer Telomere Length are Associated with Increased Risk of Renal Cell Carcinoma. Eur. Urol. 2017, 72, 747–754. [Google Scholar] [CrossRef]
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef]
- Chiavarini, M.; Rosignoli, P.; Sorbara, B.; Giacchetta, I.; Fabiani, R. Benzene Exposure and Lung Cancer Risk: A Systematic Review and Meta-Analysis of Human Studies. Int. J. Environ. Res. Public Health 2024, 21, 205. [Google Scholar] [CrossRef]
- Fabiani, R.; La Porta, G.; Li Cavoli, L.; Rosignoli, P.; Chiavarini, M. Adherence to Data-Driven Dietary Patterns and Lung Cancer Risk: A Systematic Review and Dose-Response Meta-Analysis. Nutrients 2023, 15, 4406. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non Randomised Studies in Meta-Analyses; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2000; Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 30 May 2024).
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Begg, C.B.; Mazumdar, M. Operating Characteristics of a Rank Correlation Test for Publication Bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Wong, J.Y.; Blechter, B.; Hubbard, A.K.; Machiela, M.J.; Shi, J.; Gadalla, S.M.; Hu, W.; Rahman, M.L.; Rothman, N.; Lan, Q. Phenotypic and genetically predicted leucocyte telomere length and lung cancer risk in the prospective UK Biobank. Thorax 2024, 79, 274–278. [Google Scholar] [CrossRef]
- Wong, J.Y.Y.; Shu, X.O.; Hu, W.; Blechter, B.; Shi, J.; Wang, K.; Cawthon, R.; Cai, Q.; Yang, G.; Rahman, M.L.; et al. Associations between Longer Leukocyte Telomere Length and Increased Lung Cancer Risk among Never Smokers in Urban China. Cancer Epidemiol. Biomarkers Prev. 2023, 32, 1734–1737. [Google Scholar] [CrossRef]
- Han, D.; Zhu, Y.; Choudhry, A.A.; Cheng, J.; Liang, H.; Lin, F.; Chang, Q.; Liu, H.; Pan, P.; Zhang, Y. Association of telomere length with risk of lung cancer: A large prospective cohort study from the UK Biobank. Lung Cancer 2023, 184, 107358. [Google Scholar] [CrossRef]
- Samavat, H.; Luu, H.N.; Beckman, K.B.; Jin, A.; Wang, R.; Koh, W.P.; Yuan, J.M. Leukocyte telomere length, cancer incidence and all-cause mortality among Chinese adults: Singapore Chinese Health Study. Int. J. Cancer 2021, 148, 352–362. [Google Scholar] [CrossRef]
- Yuan, J.M.; Beckman, K.B.; Wang, R.; Bull, C.; Adams-Haduch, J.; Huang, J.Y.; Jin, A.; Opresko, P.; Newman, A.B.; Zheng, Y.L.; et al. Leukocyte telomere length in relation to risk of lung adenocarcinoma incidence: Findings from the Singapore Chinese Health Study. Int. J. Cancer 2018, 142, 2234–2243. [Google Scholar] [CrossRef]
- Doherty, J.A.; Grieshober, L.; Houck, J.R.; Barnett, M.J.; De Dieu Tapsoba, J.; Thornquist, M.D.; Wang, C.Y.; Goodman, G.E.; Chen, C. Nested case-control study of telomere length and lung cancer risk among heavy smokers in the β-Carotene and Retinol Efficacy Trial. Br. J. Cancer 2018, 118, 1513–1517. [Google Scholar] [CrossRef]
- Seow, W.J.; Cawthon, R.M.; Purdue, M.P.; Hu, W.; Gao, Y.T.; Huang, W.Y.; Weinstein, S.J.; Ji, B.T.; Virtamo, J.; Hosgood, H.D.; et al. Telomere length in white blood cell DNA and lung cancer: A pooled analysis of three prospective cohorts. Cancer Res. 2014, 74, 4090–4098. [Google Scholar] [CrossRef] [PubMed]
- Lan, Q.; Cawthon, R.; Gao, Y.; Hu, W.; Hosgood, H.D.; Barone-Adesi, F.; Ji, B.T.; Bassig, B.; Chow, W.H.; Shu, X.; et al. Longer telomere length in peripheral white blood cells is associated with risk of lung cancer and the rs2736100 (CLPTM1L-TERT) polymorphism in a prospective cohort study among women in China. PLoS ONE 2013, 8, e59230. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.; Cawthon, R.; Rothman, N.; Weinstein, S.J.; Virtamo, J.; Hosgood, H.D.; Hu, W.; Lim, U.; Albanes, D.; Lan, Q. A prospective study of telomere length measured by monochrome multiplex quantitative PCR and risk of lung cancer. Lung Cancer 2011, 73, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Doherty, J.A.; Burgess, S.; Hung, R.J.; Lindström, S.; Kraft, P.; Gong, J.; Amos, C.I.; Sellers, T.A.; Monteiro, A.N.; et al. Genetic determinants of telomere length and risk of common cancers: A Mendelian randomization study. Hum. Mol. Genet. 2015, 24, 5356–5366. [Google Scholar] [CrossRef]
- Kachuri, L.; Saarela, O.; Bojesen, S.E.; Davey Smith, G.; Liu, G.; Landi, M.T.; Caporaso, N.E.; Christiani, D.C.; Johansson, M.; Panico, S.; et al. Mendelian Randomization and mediation analysis of leukocyte telomere length and risk of lung and head and neck cancers. Int. J. Epidemiol. 2019, 48, 751–766. [Google Scholar] [CrossRef]
- Teng, Y.; Huang, D.Q.; Li, R.X.; Yi, C.; Zhan, Y.Q. Association between telomere length and risk of lung cancer in an asian population: A Mendelian randomization study. World J. Oncol. 2023, 14, 277–284. [Google Scholar] [CrossRef]
- Cao, X.; Huang, M.; Zhu, M.; Fang, R.; Ma, Z.; Jiang, T.; Dai, J.; Ma, H.; Jin, G.; Shen, H.; et al. Mendelian randomization study of telomere length and lung cancer risk in East Asian population. Cancer Med. 2019, 17, 7469–7476. [Google Scholar] [CrossRef]
- Astuti, Y.; Wardhana, A.; Watkins, J.; Wulaningsih, W.; PILAR Research Network. Cigarette smoking and telomere length: A systematic review of 84 studies and meta-analysis. Environ. Res. 2017, 158, 480–489. [Google Scholar] [CrossRef]
- Raschenberger, J.; Lamina, C.; Haun, M.; Kollerits, B.; Coassin, S.; Boes, E.; Kedenko, L.; Köttgen, A.; Kronenberg, F. Influence of DNA extraction methods on relative telomere length measurements and its impact on epidemiological studies. Sci. Rep. 2016, 6, 25398. [Google Scholar] [CrossRef]
- Lin, J.; Smith, D.L.; Esteves, K.; Drury, S. Telomere length measurement by qPCR—Summary of critical factors and recommendations for assay design. Psychoneuroendocrinology 2019, 99, 271–278. [Google Scholar] [CrossRef]
- Shay, J.W. Role of Telomeres and Telomerase in Aging and Cancer. Cancer Discov. 2016, 6, 584–593. [Google Scholar] [CrossRef] [PubMed]
- Aviv, A.; Anderson, J.J.; Shay, J.W. Mutations, Cancer and the Telomere Length Paradox. Trends Cancer 2017, 3, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Lansdorp, P.M. Telomeres, aging, and cancer: The big picture. Blood 2022, 139, 813–821. [Google Scholar] [CrossRef] [PubMed]
- Demanelis, K.; Jasmine, F.; Chen, L.S.; Chernoff, M.; Tong, L.; Delgado, D.; Zhang, C.; Shinkle, J.; Sabarinathan, M.; Lin, H.; et al. Determinants of telomere length across human tissues. Science 2020, 369, eaaz6876. [Google Scholar] [CrossRef]
- Shiraishi, K.; Takahashi, A.; Momozawa, Y.; Daigo, Y.; Kaneko, S.; Kawaguchi, T.; Kunitoh, H.; Matsumoto, S.; Horinouchi, H.; Goto, A.; et al. Identification of telomere maintenance gene variations related to lung adenocarcinoma risk by genome-wide association and whole genome sequencing analyses. Cancer Commun. 2024, 44, 287–293. [Google Scholar] [CrossRef]
- Córdoba-Lanús, E.; Montuenga, L.M.; Domínguez-de-Barros, A.; Oliva, A.; Mayato, D.; Remírez-Sanz, A.; Gonzalvo, F.; Celli, B.; Zulueta, J.J.; Casanova, C. Oxidative damage and telomere length as markers of lung cancer development among chronic obstructive pulmonary disease (COPD) smokers. Antioxidants 2024, 13, 156. [Google Scholar] [CrossRef]
- Bhat, G.R.; Jamwal, R.S.; Sethi, I.; Bhat, A.; Shah, R.; Verma, S.; Sharma, M.; Sadida, H.Q.; Al-Marzooqi, S.K.; Masoodi, T.; et al. Associations between telomere attrition, genetic variants in telomere maintenance genes, and non-small cell lung cancer risk in the Jammu and Kashmir population of North India. BMC Cancer 2023, 23, 874. [Google Scholar] [CrossRef]
- Belić, M.; Sopić, M.; Roksandić-Milenković, M.; Ćeriman, V.; Guzonijić, A.; Vukašinović, A.; Ostanek, B.; Dimić, N.; Jovanović, D.; Kotur-Stevuljević, J. Correlation of short leukocyte telomeres and oxidative stress with the presence and severity of lung cancer explored by principal component analysis. Folia Biol. 2023, 69, 59–68. [Google Scholar] [CrossRef]
- Cortez, C.P.R.; Smith-Byrne, K.; Atkins, J.R.; Haycock, P.C.; Kar, S.; Codd, V.; Samani, N.J.; Nelson, C.; Milojevic, M.; Gabriel, A.A.G.; et al. Common genetic variations in telomere length genes and lung cancer: A Mendelian randomisation study and its novel application in lung tumour transcriptome. eLife 2023, 12, e83118. [Google Scholar] [CrossRef]
- Chang, X.; Gurung, R.L.; Wang, L.; Jin, A.; Li, Z.; Wang, R.; Beckman, K.B.; Adams-Haduch, J.; Meah, W.Y.; Sim, K.S.; et al. Low frequency variants associated with leukocyte telomere length in the Singapore Chinese population. Commun. Biol. 2021, 4, 519. [Google Scholar] [CrossRef]
- Xue, Y.; Guo, X.; Huang, X.; Zhu, Z.; Chen, M.; Chu, J.; Yang, G.; Wang, Q.; Kong, X. Shortened telomere length in peripheral blood leukocytes of patients with lung cancer, chronic obstructive pulmonary disease in a high indoor air pollution region in China. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2020, 858–860, 503250. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Wei, Y.; Zhou, X.; Huang, S.; Zhao, H.; Zeng, P. Assessing the relationship between leukocyte telomere length and cancer risk/mortality in UK Biobank and TCGA datasets with the genetic risk score and Mendelian randomization approaches. Front. Genet. 2020, 11, 583106. [Google Scholar] [CrossRef] [PubMed]
- Autsavapromporn, N.; Klunklin, P.; Threeratana, C.; Tuntiwechapikul, W.; Hosoda, M.; Tokonami, S. Short telomere length as a biomarker risk of lung cancer development induced by high radon levels: A pilot study. Int. J. Environ. Res. Public Health 2018, 15, 2152. [Google Scholar] [CrossRef]
- Doherty, J.A.; Grieshober, L.; Houck, J.R.; Barnett, M.J.; Tapsoba, J.D.; Thornquist, M.; Wang, C.Y.; Goodman, G.E.; Chen, C. Telomere length and lung cancer mortality among heavy smokers. Cancer Epidemiol. Biomarkers Prev. 2018, 27, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Haycock, P.C.; Burgess, S.; Nounu, A.; Zheng, J.; Okoli, G.N.; Bowden, J.; Wade, K.H.; Timpson, N.J.; Evans, D.M.; Willeit, P.; et al. Association between telomere length and risk of cancer and non-neoplastic diseases: A Mendelian randomization study. JAMA Oncol. 2017, 3, 636–651. [Google Scholar] [CrossRef] [PubMed]
- Rode, L.; Nordestgaard, B.G.; Bojesen, S.E. Long telomeres and cancer risk among 95 568 individuals from the general population. Int. J. Epidemiol. 2016, 45, 1634–1643. [Google Scholar] [CrossRef]
- Fernández-Marcelo, T.; Gómez, A.; Pascua, I.; de Juan, C.; Head, J.; Hernando, F.; Jarabo, J.R.; Calatayud, J.; Torres-García, A.J.; Iniesta, P. Telomere length and telomerase activity in non-small cell lung cancer prognosis: Clinical usefulness of a specific telomere status. J. Exp. Clin. Cancer Res. 2015, 34, 78. [Google Scholar] [CrossRef]
- Machiela, M.J.; Hsiung, C.A.; Shu, X.O.; Seow, W.J.; Wang, Z.; Matsuo, K.; Hong, Y.C.; Seow, A.; Wu, C.; Hosgood, H.D.; et al. Genetic variants associated with longer telomere length are associated with increased lung cancer risk among never-smoking women in Asia: A report from the female lung cancer consortium in Asia. Int. J. Cancer 2015, 137, 311–319. [Google Scholar] [CrossRef]
- Sun, B.; Wang, Y.; Kota, K.; Shi, Y.; Motlak, S.; Makambi, K.; Loffredo, C.A.; Shields, P.G.; Yang, Q.; Harris, C.C.; et al. Telomere length variation: A potential new telomere biomarker for lung cancer risk. Lung Cancer 2015, 88, 297–303. [Google Scholar] [CrossRef]
- Sanchez-Espiridion, B.; Chen, M.; Chang, J.Y.; Lu, C.; Chang, D.W.; Roth, J.A.; Wu, X.; Gu, J. Telomere length in peripheral blood leukocytes and lung cancer risk: A large case-control study in Caucasians. Cancer Res. 2014, 74, 2476–2486. [Google Scholar] [CrossRef]
- Weischer, M.; Nordestgaard, B.G.; Cawthon, R.M.; Freiberg, J.J.; Tybjærg-Hansen, A.; Bojesen, S.E. Short telomere length, cancer survival, and cancer risk in 47102 individuals. J. Natl. Cancer Inst. 2013, 105, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Willeit, P.; Willeit, J.; Mayr, A.; Weger, S.; Oberhollenzer, F.; Brandstätter, A.; Kronenberg, F.; Kiechl, S. Telomere length and risk of incident cancer and cancer mortality. JAMA 2010, 304, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Hosgood, H.D.; Cawthon, R.; He, X.; Chanock, S.; Lan, Q. Genetic variation in telomere maintenance genes, telomere length, and lung cancer susceptibility. Lung Cancer 2009, 66, 157–161. [Google Scholar] [CrossRef]
- Jang, J.S.; Choi, Y.Y.; Lee, W.K.; Choi, J.E.; Cha, S.I.; Kim, Y.J.; Kim, C.H.; Kam, S.; Jung, T.H.; Park, J.Y. Telomere length and the risk of lung cancer. Cancer Sci. 2008, 99, 1385–1389. [Google Scholar] [CrossRef]
- Wu, X.; Amos, C.I.; Zhu, Y.; Zhao, H.; Grossman, B.H.; Shay, J.W.; Luo, S.; Hong, W.K.; Spitz, M.R. Telomere dysfunction: A potential cancer predisposition factor. J. Natl. Cancer Inst. 2003, 95, 1211–1218. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).