Allostatic Load, Cigarette Smoking, and Lung Cancer Risk
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McEwen, B.S. Allostasis and allostatic load: Implications for neuropsychopharmacology. Neuropsychopharmacology 2000, 22, 108–124. [Google Scholar] [CrossRef] [PubMed]
- Guidi, J.; Lucente, M.; Sonino, N.; Fava, G.A. Allostatic Load and Its Impact on Health: A Systematic Review. Psychother. Psychosom. 2021, 90, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Mathew, A.; Doorenbos, A.Z.; Li, H.; Jang, M.K.; Park, C.G.; Bronas, U.G. Allostatic Load in Cancer: A Systematic Review and Mini Meta-Analysis. Biol. Res. Nurs. 2021, 23, 341–361. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guan, Y.; Shen, J.; Lu, J.; Fuemmeler, B.F.; Shock, L.S.; Zhao, H. Association between allostatic load and breast cancer risk: A cohort study. Breast Cancer Res. 2023, 25, 155. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhao, H.; Song, R.; Ye, Y.; Chow, W.H.; Shen, J. Allostatic score and its associations with demographics, healthy behaviors, tumor characteristics, and mitochondrial DNA among breast cancer patients. Breast Cancer Res. Treat. 2021, 187, 587–596. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.C.; Elsaid, M.I.; Handley, D.; Plascak, J.J.; Andersen, B.L.; Carson, W.E.; Pawlik, T.M.; Fareed, N.; Obeng-Gyasi, S. Association between Neighborhood Opportunity, Allostatic Load, and All-Cause Mortality in Patients with Breast Cancer. J. Clin. Oncol. 2024, 42, 1788–1798. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Obeng-Gyasi, S.; Elsaid, M.I.; Lu, Y.; Chen, J.C.; Carson, W.E.; Ballinger, T.J.; Andersen, B.L. Association of Allostatic Load with All-Cause Mortality in Patients with Breast Cancer. JAMA Netw. Open. 2023, 6, e2313989. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Obeng-Gyasi, S.; Li, Y.; Carson, W.E.; Reisenger, S.; Presley, C.J.; Shields, P.G.; Carbone, D.P.; Ceppa, D.P.; Carlos, R.C.; Andersen, B.L. Association of Allostatic Load with Overall Mortality among Patients with Metastatic Non-Small Cell Lung Cancer. JAMA Netw. Open. 2022, 5, e2221626. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Suvarna, B.; Suvarna, A.; Phillips, R.; Juster, R.P.; McDermott, B.; Sarnyai, Z. Health risk behaviours and allostatic load: A systematic review. Neurosci. Biobehav. Rev. 2020, 108, 694–711. [Google Scholar] [CrossRef] [PubMed]
- Doan, S.N.; Dich, N.; Evans, G.W. Childhood cumulative risk and later allostatic load: Mediating role of substance use. Health Psychol. 2014, 33, 1402–1409. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Bhupathiraju, S.N.; Falcon, L.M.; Gao, X.; Tucker, K.L.; Mattei, J. A Healthy Lifestyle Score Is Associated with Cardiometabolic and Neuroendocrine Risk Factors among Puerto Rican Adults. J. Nutr. 2015, 145, 1531–1540. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rodriquez, E.J.; Livaudais-Toman, J.; Gregorich, S.E.; Jackson, J.S.; Napoles, A.M.; Perez-Stable, E.J. Relationships between allostatic load, unhealthy behaviors, and depressive disorder in U.S. adults, 2005–2012 NHANES. Prev. Med. 2018, 110, 9–15. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shen, J.; Fuemmeler, B.F.; Guan, Y.; Zhao, H. Association of Allostatic Load and All Cancer Risk in the SWAN Cohort. Cancers 2022, 14, 3044. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jafri, S.H.; Ali, F.; Mollaeian, A.; Mojiz Hasan, S.; Hussain, R.; Akkanti, B.; Williams, J.; Shoukier, M.; El-Osta, H. Major Stressful Life Events and Risk of Developing Lung Cancer: A Case-Control Study. Clin. Med. Insights Oncol. 2019, 13, 1179554919835798. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chida, Y.; Hamer, M.; Wardle, J.; Steptoe, A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat. Clin. Pract. Oncol. 2008, 5, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Qiao, Y.; Xiang, S.; Li, W.; Gan, Y.; Chen, Y. Work stress and the risk of cancer: A meta-analysis of observational studies. Int. J. Cancer 2019, 144, 2390–2400. [Google Scholar] [CrossRef] [PubMed]
- Heikkila, K.; Nyberg, S.T.; Theorell, T.; Fransson, E.I.; Alfredsson, L.; Bjorner, J.B.; Williams, J.; Shoukier, M.; El-Osta, H. Work stress and risk of cancer: Meta-analysis of 5700 incident cancer events in 116,000 European men and women. BMJ 2013, 346, f165. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jang, H.J.; Boo, H.J.; Lee, H.J.; Min, H.Y.; Lee, H.Y. Chronic Stress Facilitates Lung Tumorigenesis by Promoting Exocytosis of IGF2 in Lung Epithelial Cells. Cancer Res. 2016, 76, 6607–6619. [Google Scholar] [CrossRef] [PubMed]
- He, X.Y.; Gao, Y.; Ng, D.; Michalopoulou, E.; George, S.; Adrover, J.M.; Sun, L.; Albrengues, J.; Daßler-Plenker, J.; Han, X.; et al. Chronic stress increases metastasis via neutrophil-mediated changes to the microenvironment. Cancer Cell. 2024, 42, 474–486.e12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stubbs, B.; Veronese, N.; Vancampfort, D.; Prina, A.M.; Lin, P.Y.; Tseng, P.T.; Evangelou, E.; Solmi, M.; Kohler, C.; Carvalho, A.F.; et al. Perceived stress and smoking across 41 countries: A global perspective across Europe, Africa, Asia and the Americas. Sci. Rep. 2017, 7, 7597. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lawless, M.H.; Harrison, K.A.; Grandits, G.A.; Eberly, L.E.; Allen, S.S. Perceived stress and smoking-related behaviors and symptomatology in male and female smokers. Addict. Behav. 2015, 51, 80–83. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sudlow, C.; Gallacher, J.; Allen, N.; Beral, V.; Burton, P.; Danesh, J.; Downey, P.; Elliott, P.; Green, J.; Landray, M.; et al. UK biobank: An open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015, 12, e1001779. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chyu, L.; Upchurch, D.M. A Longitudinal Analysis of Allostatic Load among a Multi-Ethnic Sample of Midlife Women: Findings from the Study of Women’s Health Across the Nation. Womens Health Issues 2018, 28, 258–266. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Levav, I.; Kohn, R.; Iscovich, J.; Abramson, J.H.; Tsai, W.Y.; Vigdorovich, D. Cancer incidence and survival following bereavement. Am. J. Public. Health. 2000, 90, 1601–1607. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, S.J.; Kery, C.; An, J.; Rineer, J.; Bobashev, G.; Matthews, A.K. Racial/Ethnic disparities in exposure to neighborhood violence and lung cancer risk in Chicago. Soc. Sci. Med. 2024, 340, 116448. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, B.P.; Zhang, C.; Zhang, Y.P.; Li, K.W.; Song, C. The combination of chronic stress and smoke exacerbated depression-like changes and lung cancer factor expression in A/J mice: Involve inflammation and BDNF dysfunction. PLoS ONE 2022, 17, e0277945. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jung, W.; Irwin, M. Reduction of natural killer cytotoxic activity in major depression: Interaction between depression and cigarette smoking. Psychosom. Med. 1999, 61, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Redondo-Sanchez, D.; Petrova, D.; Rodriguez-Barranco, M.; Fernandez-Navarro, P.; Jimenez-Moleon, J.J.; Sanchez, M.J. Socio-Economic Inequalities in Lung Cancer Outcomes: An Overview of Systematic Reviews. Cancers 2022, 14, 398. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hovanec, J.; Siemiatycki, J.; Conway, D.I.; Olsson, A.; Stucker, I.; Guida, F.; Jöckel, K.-H.; Pohlabeln, H.; Ahrens, W.; Brüske, I.; et al. Lung cancer and socioeconomic status in a pooled analysis of case-control studies. PLoS ONE 2018, 13, e0192999. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hicks, B.; Veronesi, G.; Ferrario, M.M.; Forrest, H.; Whitehead, M.; Diderichsen, F.; Tunstall-Pedoe, H.; Kuulasmaa, K.; Sans, S.; Salomaa, V.; et al. Roles of allostatic load, lifestyle and clinical risk factors in mediating the association between education and coronary heart disease risk in Europe. J. Epidemiol. Community Health 2021, 75, 1147–1154. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Forrester, S.N.; Leoutsakos, J.M.; Gallo, J.J.; Thorpe, R.J.; Jr Seeman, T.E. Association between allostatic load and health behaviours: A latent class approach. J. Epidemiol. Community Health 2019, 73, 340–345. [Google Scholar] [CrossRef] [PubMed]

| Variables | Incident Cases (N = 2517) | Cancer-Free Controls (N = 341,863) | p Value |
|---|---|---|---|
| Age at recruitment, mean (SD) | 61.6 (5.84) | 56.2 (8.10) | <0.001 |
| Years from recruitment to cancer diagnosis, mean (IQR) | 7.0 (4.2, 9.4) | ||
| Gender (%) | <0.001 | ||
| Male | 1310 (52.05) | 161,113 (47.13) | |
| Female | 1207 (47.95) | 180,750 (52.87) | |
| Race/ethnicity (%) | <0.001 | ||
| White | 2437 (96.82) | 322,611 (94.37) | |
| Black | 25 (0.99) | 4905 (1.43) | |
| Asian | 26 (1.03) | 8041 (2.35) | |
| Mixed or others | 23 (0.91) | 5129 (1.50) | |
| Missing | 6 (0.24) | 1177 (0.34) | |
| Family history of lung cancer (%) | <0.001 | ||
| Yes | 350 (13.91) | 26,366 (7.71) | |
| No | 915 (36.35) | 135,222 (39.55) | |
| Missing | 1252 (49.74) | 180,275 (52.73) | |
| Education (%) | <0.001 | ||
| High school or less | 975 (38.74) | 153,541 (44.91) | |
| College/professional | 537 (21.33) | 129,149 (37.78) | |
| Missing | 1005 (39.93) | 59,173 (17.31) | |
| Employment status (%) | <0.001 | ||
| Unemployed | 295 (11.72) | 28,091 (8.22) | |
| Employed | 887 (35.24) | 201,474 (58.93) | |
| Retired | 1309 (52.01) | 109,100 (31.91) | |
| Missing | 26 (1.03) | 3198 (0.94) | |
| Income (%) | <0.001 | ||
| <£31,000 | 1485 (59.00) | 137,853 (40.32) | |
| ≥£31,000 | 557 (22.13) | 155,840 (45.59) | |
| Missing | 475 (18.87) | 48,170 (14.09) | |
| Townsend deprivation score (%) | 0.001 | ||
| Low | 915 (36.35) | 172,446 (50.44) | |
| High | 1601 (63.61) | 169,013 (49.44) | |
| Missing | 1 (0.04) | 404 (0.12) | |
| Smoking (%) | <0.001 | ||
| Never | 336 (13.35) | 188,406 (55.11) | |
| Former | 1121 (44.54) | 117,153 (34.27) | |
| Current | 1039 (41.28) | 35,102 (10.27) | |
| Missing | 21 (0.83) | 1202 (0.35) | |
| Physical activity (%) | 0.001 | ||
| Low | 439 (17.44) | 52,179 (15.26) | |
| Moderate | 781 (31.03) | 112,916 (33.03) | |
| High | 721 (28.65) | 112,585 (32.93) | |
| Missing | 576 (22.88) | 64,183 (18.77) | |
| Alcohol consumption (%) | <0.001 | ||
| Special occasions or never | 602 (23.92) | 65,223 (19.08) | |
| Moderate | 818 (32.50) | 126,285 (36.94) | |
| Heavy | 1093 (43.42) | 150,071 (43.90) | |
| Missing | 4 (0.16) | 284 (0.08) | |
| Sleeplessness (%) | <0.001 | ||
| Never/rarely | 495 (19.67) | 83,804 (24.51) | |
| Sometimes | 1182 (49.96) | 163,086 (47.71) | |
| Usually | 840 (33.37) | 94,676 (27.69) | |
| Missing | 0 (0.08) | 297 (0.09) |
| Incident Cases (N = 2517) | Cancer-Free Controls (N = 341,863) | p Value | |
|---|---|---|---|
| AL Score | <0.001 | ||
| 0 | 65 (2.58) | 23,032 (6.74) | |
| 1 | 245 (9.73) | 61,586 (18.01) | |
| 2 | 401 (15.93) | 67,493 (19.74) | |
| 3 | 569 (22.61) | 69,734 (20.40) | |
| 4 | 540 (21.45) | 57,359 (16.78) | |
| 5 | 411 (16.33) | 38,210 (11.18) | |
| 6 | 206 (8.18) | 17,956 (5.25) | |
| 7 | 70 (2.78) | 5317 (1.56) | |
| 8 | 8 (0.32) | 1047 (0.31) | |
| 9 | 2 (0.08) | 123 (0.04) | |
| 10 | 0 | 5 (<0.01) | |
| 11 | 0 | 1 (<0.01) | |
| AL (continuous), Mean (SD) | 3.47 (1.58) | 3.35 (1.67) | <0.001 |
| AL category | |||
| Low (0~2) | 711 (28.25) | 152,111 (44.49) | <0.001 |
| High (>2) | 1806 (71.75) | 189,752 (55.51) | |
| Univariate | Multivariate * | ||
| HR (95% CI) | HR (95% CI) | ||
| AL, continuous, Per one unit | 1.23 (1.20, 1.26) | 1.02 (0.99, 1.04) | |
| AL category | |||
| Low | Reference | Reference | |
| High | 2.08 (1.91, 2.27) | 1.15(1.05, 1.25) |
| Age group (median) | <57 years old (n = 173,224) | ≥57 years old (n = 171,156) | ||||
| AL: high (>2) vs. Low (≤2) | 1.35 (1.13, 1.62) | 1.26 (1.14, 1.40) | ||||
| Gender | Male (n = 162,423) | Female (n = 181,957) | ||||
| AL: high (>2) vs. Low (≤2) | 1.19 (1.04, 1.37) | 1.36 (1.11, 1.54) | ||||
| Race | White (n = 325,048) | Non-white (n = 18,149) | ||||
| AL: high (>2) vs. Low (≤2) | 1.23 (1.12, 1.35) | 0.74 (0.45, 1.22) | ||||
| Family history of cancer | No (n = 136,137) | Yes (n = 26,716) | ||||
| AL: high (>2) vs. Low (≤2) | 1.14 (0.98, 1.32) | 1.00 (0.79, 1.28) | ||||
| Education | ≤High school (n = 154,516) | >High school (n = 129,686) | ||||
| AL: high (>2) vs. Low (≤2) | 1.11 (0.97, 1.28) | 1.28 (1.06, 1.55) | ||||
| Income | <£31,000 (n = 139,338) | ≥£31,000 (n = 156,397) | ||||
| AL: high (>2) vs. Low (≤2) | 1.15 (1.02, 1.29) | 1.31 (1.09, 1.58) | ||||
| Townsend deprivation score | Low (n = 173,361) | High (n = 170,614) | ||||
| AL: high (>2) vs. Low (≤2) | 1.26 (1.09, 1.47) | 1.18 (1.05, 1.32) | ||||
| Employment | Unemployed (n = 28,386) | Employed (n = 202,361) | Retired (n = 110,409) | |||
| AL: high (>2) vs. Low (≤2) | 1.10 (0.83, 1.43) | 1.23 (1.06, 1.43) | 1.25 (1.10, 1.42) | |||
| Smoking status | Never (n = 188,742) | Former (n = 118,274) * | Current (n = 36,141) * | |||
| AL: high (>2) vs. Low (≤2) | 0.93 (0.74, 1.17) | 1.38 (1.20, 1.59) | 1.17 (1.02, 1.35) | |||
| Alcohol consumption | Occasional/never (n = 65,825) | Moderate (n = 127,103) | Heavy (n = 151,164) * | |||
| AL: high (>2) vs. Low (≤2) | 1.11 (0.93, 1.34) | 1.24 (1.06, 1.46) | 1.25 (1.09, 1.44) | |||
| Physical activity | Low (n = 52,618) | Moderate (n = 113,697) | High (n = 113,306) | |||
| AL: high (>2) vs. Low (≤2) | 1.06 (0.85, 1.33) | 1.27 (1.07, 1.49) | 1.19 (1.01, 1.40) | |||
| Sleeplessness | Never/rarely (n = 84,299) | Sometimes (n = 164,268) | Usually (n = 95,516) | |||
| AL: high (>2) vs. Low (≤2) | 1.32 (1.07, 1.63) | 1.23 (1.07, 1.40) | 1.13 (0.97, 1.32) | |||
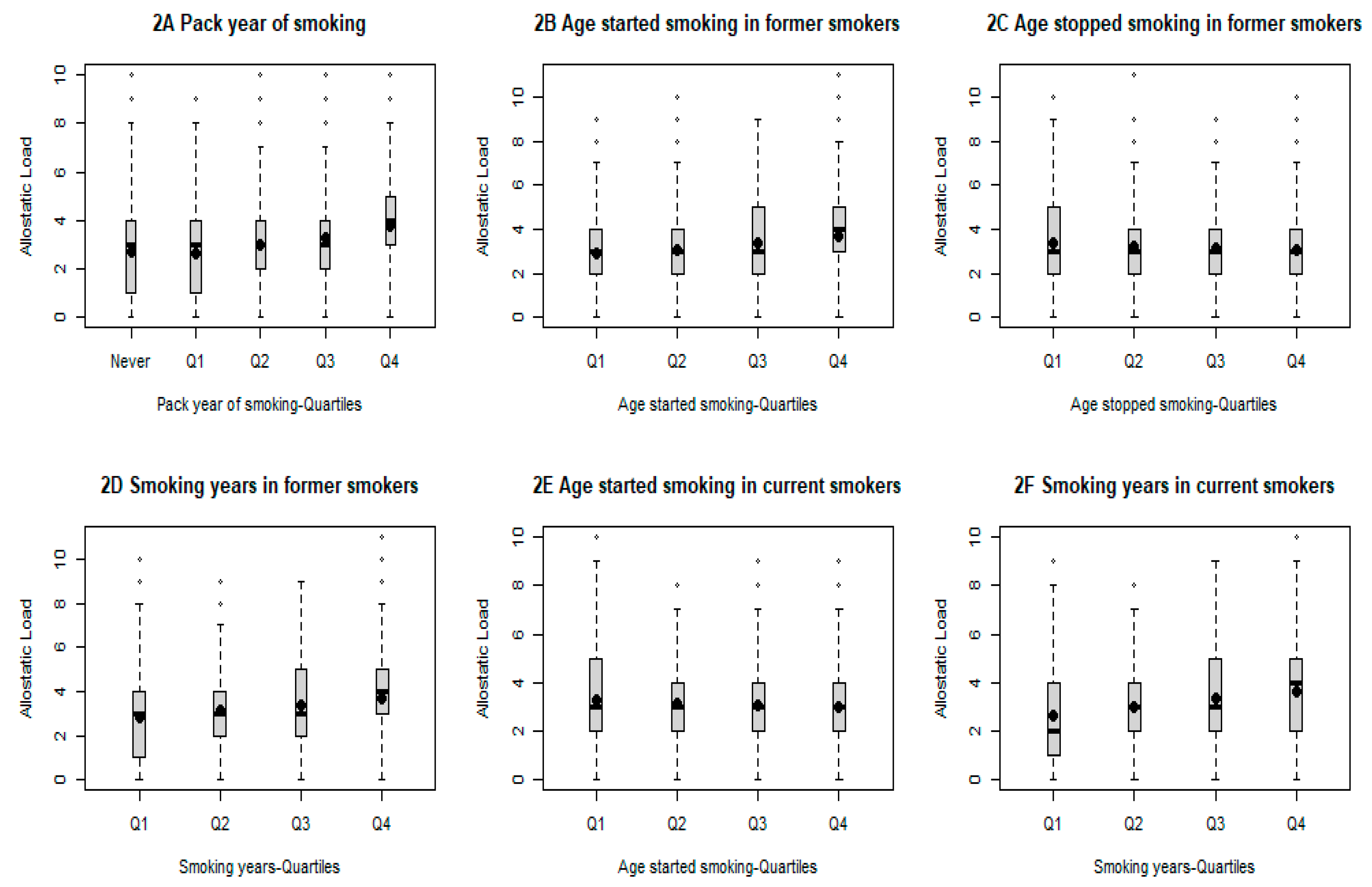
| Smoking-Related Variable | Number | AL (Mean/SD) | p-Value |
|---|---|---|---|
| Smoking status | <0.001 | ||
| Never | 188,742 | 2.70 (1.69) | |
| Former | 118,274 | 3.08 (1.71) | |
| Current | 36,141 | 3.08 (1.75) | |
| p for trend | <0.001 | ||
| Pack-years of smoking | <0.001 | ||
| Never | 188,742 | 2.71 (1.69) | |
| Q1 (>0 to ≤9.75) | 25,252 | 2.66 (1.67) | |
| Q2 (>9.75 to ≤18.75) | 25,648 | 3.00 (1.69) | |
| Q3 (>18.75 to ≤31.50) | 25,796 | 3.27 (1.69) | |
| Q4 (>31.50) | 25,776 | 3.75 (1.65) | |
| p for trend | <0.001 | ||
| Among former smokers | |||
| Age of smoking initiation | <0.001 | ||
| Q1 (≤15 years old) | 23,377 | 3.41(1.72) | |
| Q2 (>15 to ≤17 years old) | 23,385 | 3.23(1.69) | |
| Q3 (>17 to ≤18 years old) | 13,004 | 3.11(1.67) | |
| Q4 (>18 years old) | 18,778 | 3.07(1.70) | |
| p for trend | <0.001 | ||
| Age of smoking cessation | <0.001 | ||
| Q1 (≤30 years old) | 22,129 | 2.87 (1.68) | |
| Q2 (>30 to ≤39 years old) | 18,792 | 3.09 (1.72) | |
| Q3 (>39 to ≤49 years old) | 20,023 | 3.33 (1.69) | |
| Q4 (>49 years old) | 17,676 | 3.67 (1.61) | |
| p for trend | <0.001 | ||
| Years of smoking | <0.001 | ||
| Q1 (≤13 years) | 21,415 | 2.82 (1.68) | |
| Q2 (>13 to ≤21 years) | 19,188 | 3.12 (1.70) | |
| Q3 (>21 to ≤31 years) | 19,529 | 3.34 (1.69) | |
| Q4 (>31 years) | 18,126 | 3.69 (1.62) | |
| p for trend | <0.001 | ||
| Among current smokers | |||
| Age of smoking initiation | <0.001 | ||
| Q1 (≤15 years) | 8973 | 3.29 (1.76) | |
| Q2 (>15 to ≤16 years) | 4399 | 3.16 (1.75) | |
| Q3 (>16 to ≤19 years) | 6881 | 3.07 (1.75) | |
| Q4 (>19 years) | 6053 | 3.02 (1.74) | |
| p for trend | <0.001 | ||
| Years of smoking | <0.001 | ||
| Q1 (≤30 years) | 6837 | 2.62 (1.77) | |
| Q2 (>30 to ≤37 years) | 6386 | 3.00 (1.76) | |
| Q3 (>37 to ≤44 years) | 6830 | 3.36 (1.69) | |
| Q4 (>44 years) | 6253 | 3.65 (1.60) | |
| p for trend | <0.001 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guan, Y.; Shen, J.; Zhang, K.; Fuemmeler, B.F.; Zhao, H. Allostatic Load, Cigarette Smoking, and Lung Cancer Risk. Cancers 2024, 16, 3235. https://doi.org/10.3390/cancers16183235
Guan Y, Shen J, Zhang K, Fuemmeler BF, Zhao H. Allostatic Load, Cigarette Smoking, and Lung Cancer Risk. Cancers. 2024; 16(18):3235. https://doi.org/10.3390/cancers16183235
Chicago/Turabian StyleGuan, Yufan, Jie Shen, Kai Zhang, Bernard F. Fuemmeler, and Hua Zhao. 2024. "Allostatic Load, Cigarette Smoking, and Lung Cancer Risk" Cancers 16, no. 18: 3235. https://doi.org/10.3390/cancers16183235
APA StyleGuan, Y., Shen, J., Zhang, K., Fuemmeler, B. F., & Zhao, H. (2024). Allostatic Load, Cigarette Smoking, and Lung Cancer Risk. Cancers, 16(18), 3235. https://doi.org/10.3390/cancers16183235





