Theranostic Approaches for Gastric Cancer: An Overview of In Vitro and In Vivo Investigations
Abstract
Simple Summary
Abstract
1. Introduction
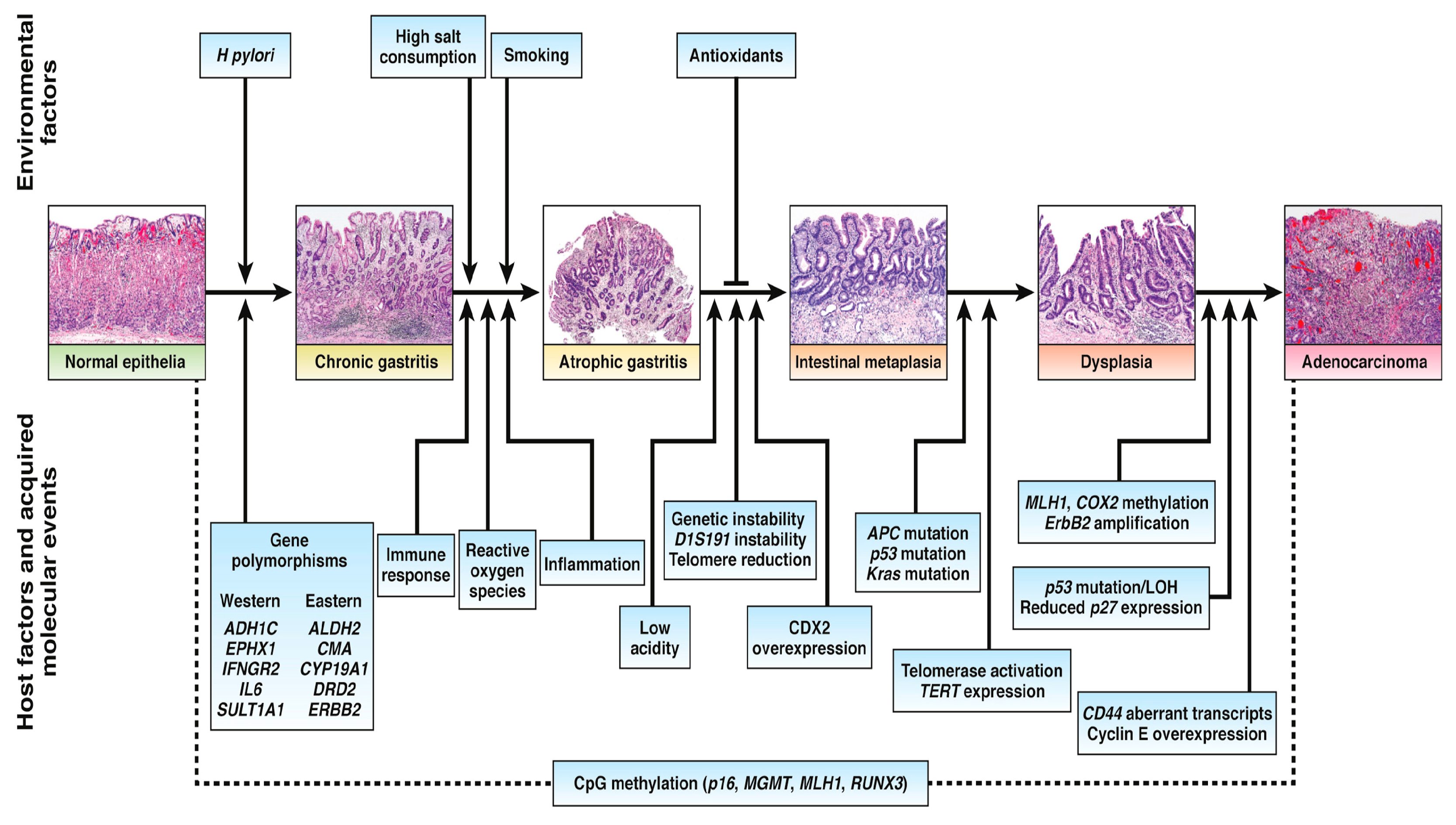
1.1. Molecular Pathology in Gastric Cancer
1.2. The Role of Targeted Therapy in the Treatment of Advanced Gastric Cancer
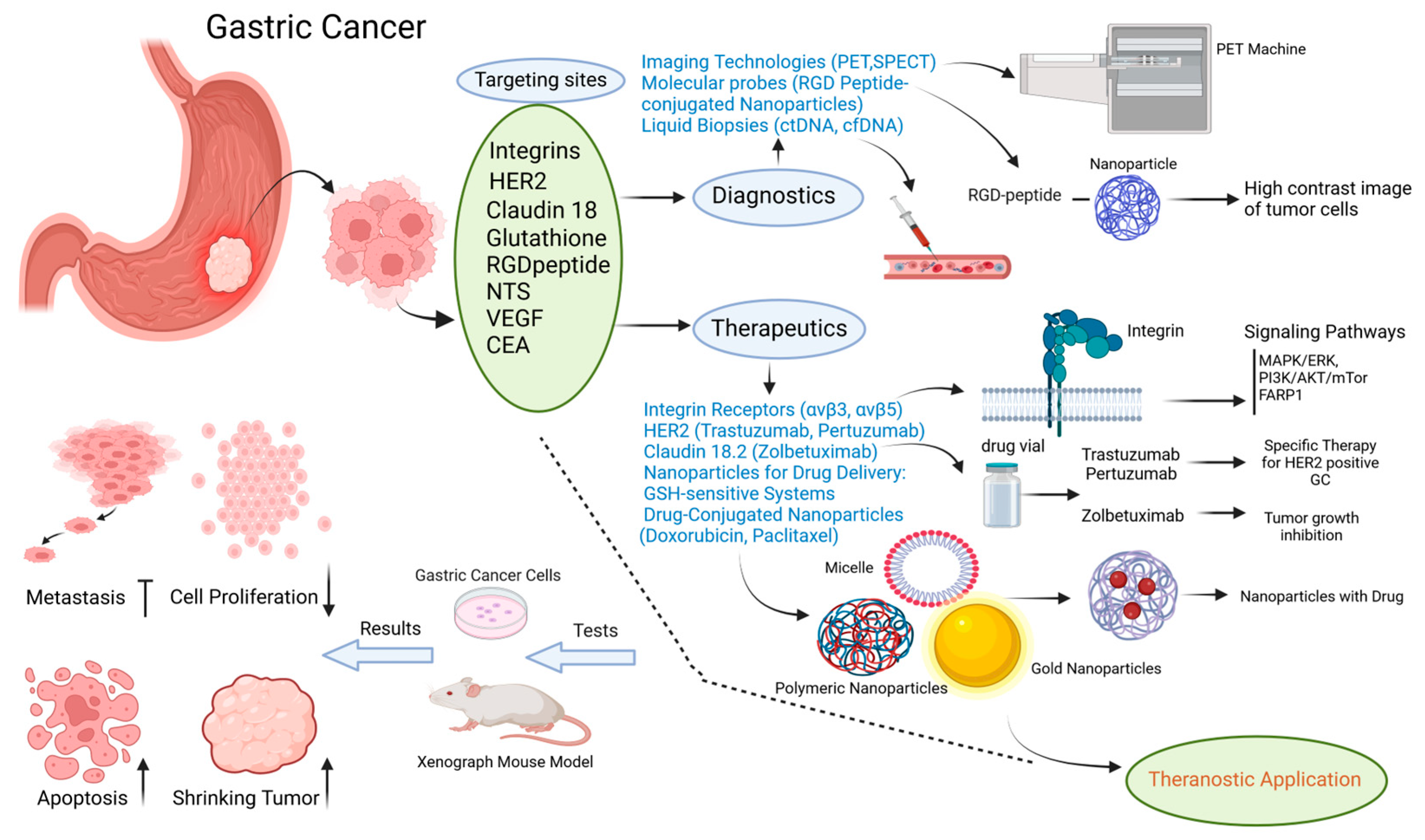
2. Gastric Cancer Targeting Sites
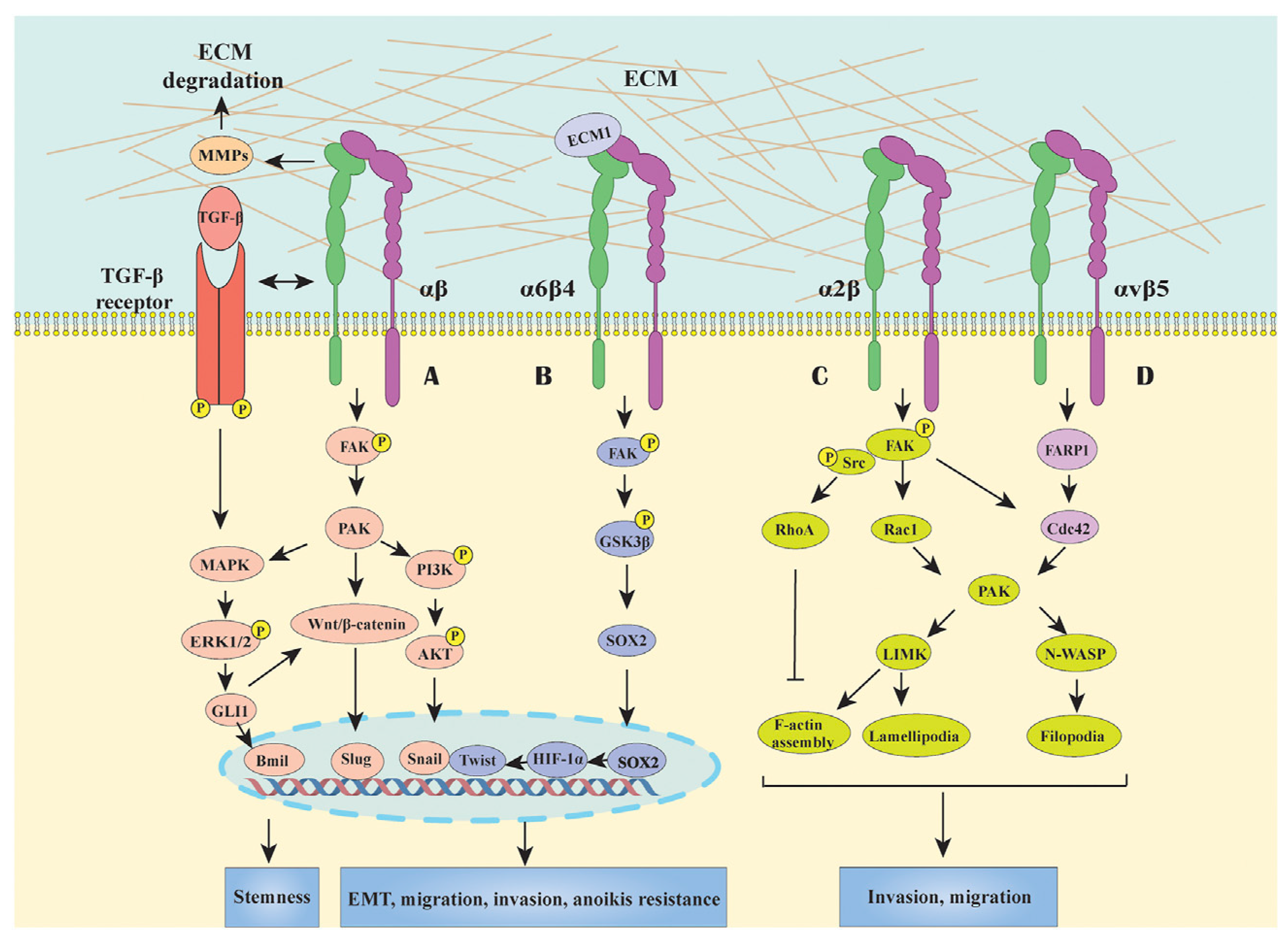
2.1. Integrin Receptor
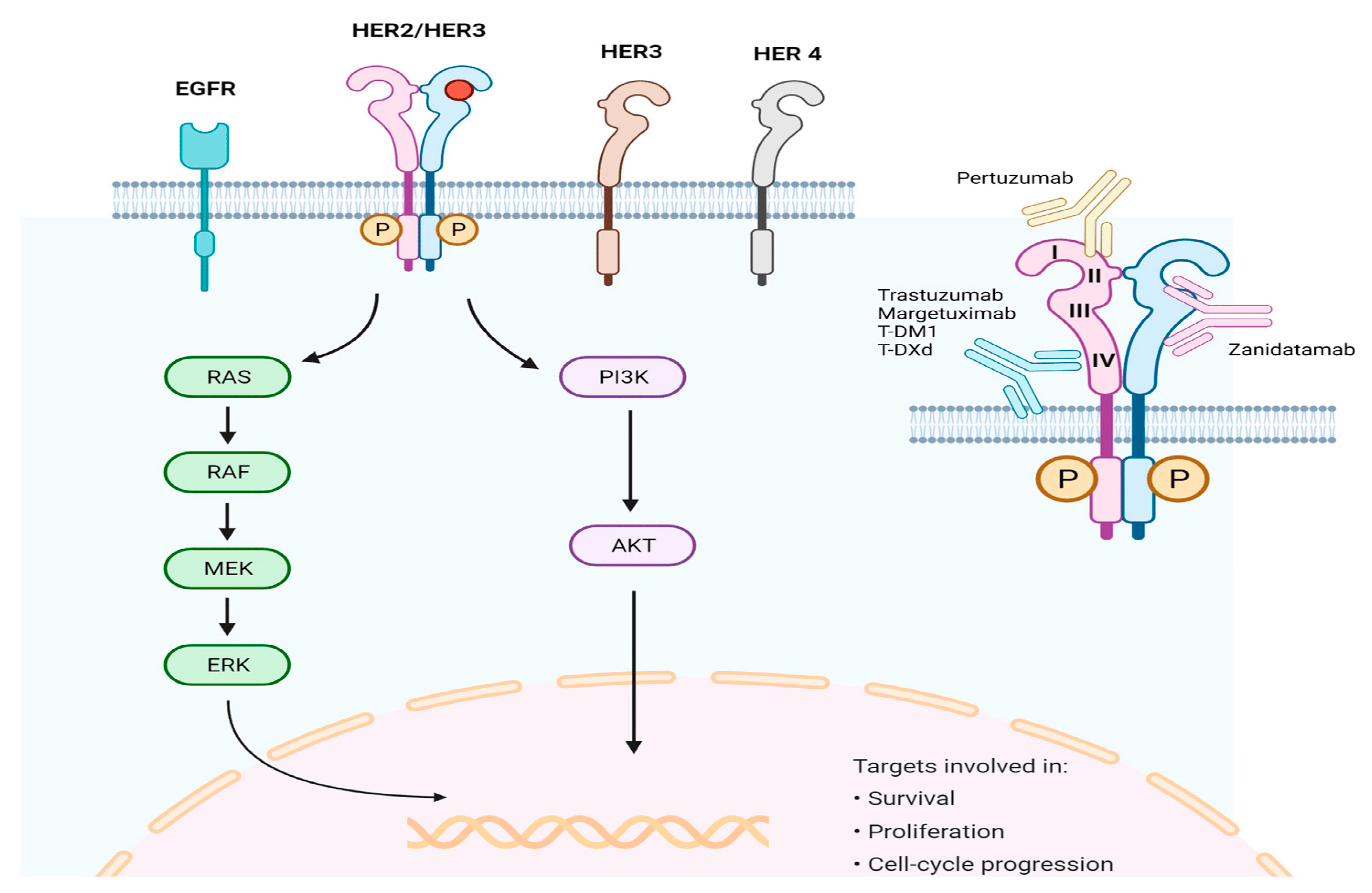
2.2. Human Epidermal Growth Factor Receptor 2 (HER2)
2.3. Claudin 18
2.4. Glutathione
2.5. Cyclic RGD Peptide
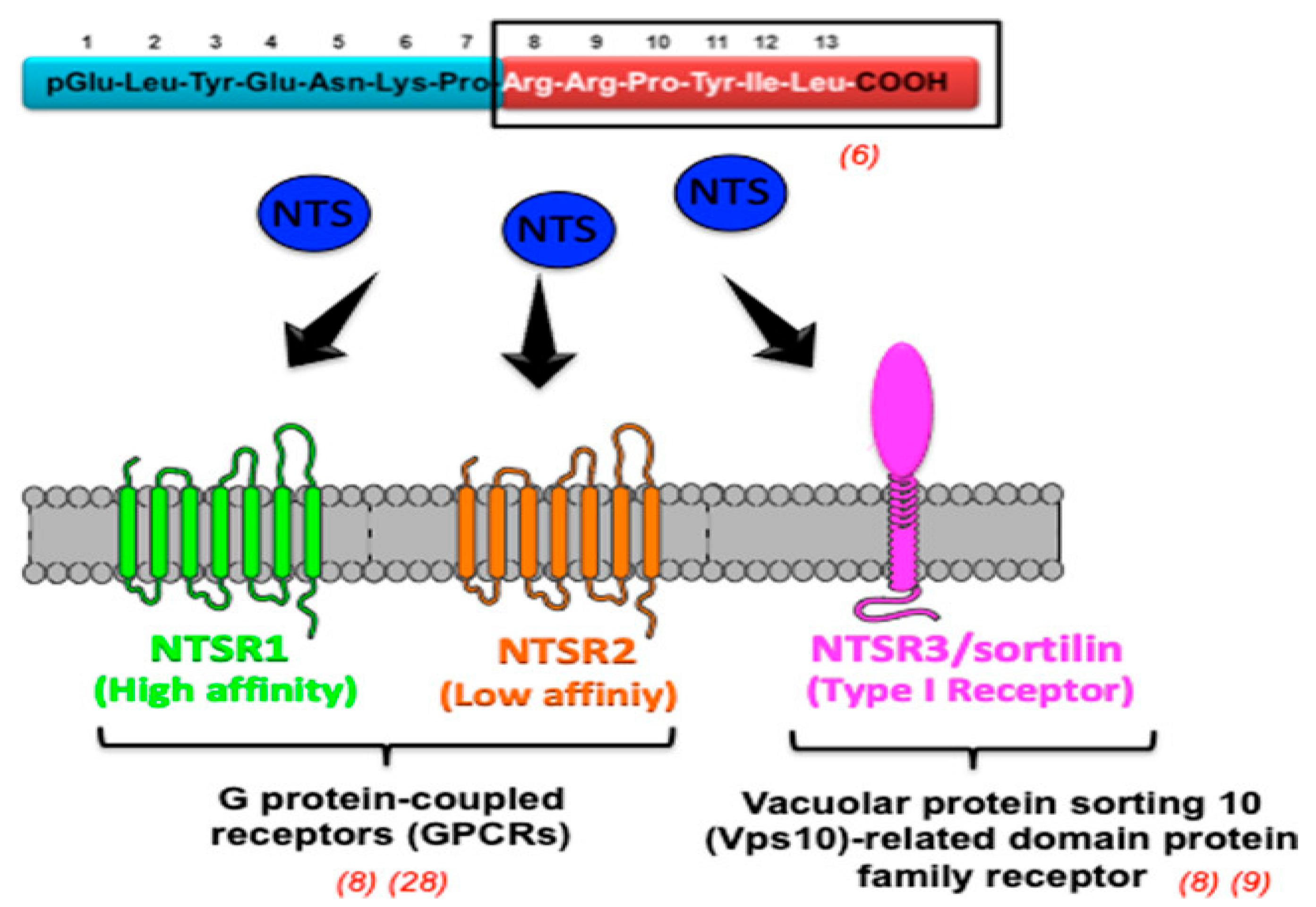
2.6. Neurotensin Receptors
2.7. Angiogenesis
2.8. Carcinoembryonic Antigen
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| GC | gastric cancer |
| IM | intestinal metaplasia |
| ALDH2 | aldehyde dehydrogenase 2 |
| HER2 | human epidermal growth factor receptor 2 |
| MDM2 | mouse double minute 2 homolog |
| pRb | retinoblastoma protein |
| MRP2 | multidrug resistance-associated protein 2 |
| ICIs | Immune checkpoint inhibitors |
| VEGFA | vascular endothelial growth factor A |
| CAR | chimeric antigen receptor |
| CEA | carcinoembryonic antigen |
| CA19-9 | carbohydrate antigen19-9 |
| cfDNA | cell-free DNA |
| ctDNA | circulating tumor DNA |
| NPs | nanoparticles |
| GI | gastrointestinal |
| RGD | arginine glycine–aspartic acid |
| RGD-ICG | RGD-indocyanine green |
| DGC | diffuse type of gastric carcinoma |
| CAFs | cancer-associated fibroblasts |
| FARP1 | pleckstrin domain protein 1 |
| ITGA11 | integrin-subunit alpha 11 |
| FASN | fatty acid synthase |
| CSCs | cancer stem cells |
| CLDNs | claudins |
| CLDN18.2 | CLDN 18 splice variant 2 |
| ADCC | antibody-dependent cellular cytotoxicity |
| CDC | complement-dependent cytotoxicity |
| anti-mPD-1 | anti-mouse programmed cell death-1 |
| GEJ | gastroesophageal junction |
| GSH | glutathione |
| PTX | paclitaxel |
| PEG | polyethylene glycol |
| GPx2 | glutathione peroxidase-2 |
| EMT | epithelial–mesenchymal transition |
| KYNU | kynurenines |
| ROS | reactive oxygen species |
| 5-FU | 5-fluorouracil |
| PDT | photodynamic therapy |
| PCR | polymerase chain reaction |
| MWNTs | multiwalled carbon nanotubes |
| sGNRs | silica-coated gold nanorods |
| NTS | neurotensin |
| MMP | matrix metalloproteinase |
| FRET | fluorescence resonance energy transfer |
| PKC | protein kinase C |
| ERK | extracellular signal-regulated kinase |
| PI3K | phosphatidylinositol 3-kinase |
| NPY | neuropeptide Y |
| AP | apatinib |
| CS-1 | cinobufagin |
| BCAT1 | branch-chain amino acid transaminase 1 |
| SLex | sialyl-Lewis X antigen |
| PLA | proximity ligation assay |
| vcMMAE | monomethyl auristatin E |
References
- Alpízar-Alpízar, W.; Christensen, I.J.; Santoni-Rugiu, E.; Skarstein, A.; Ovrebo, K.; Illemann, M.; Laerum, O.D. Urokinase Plasminogen Activator Receptor on Invasive Cancer Cells: A Prognostic Factor in Distal Gastric Adenocarcinoma. Int. J. Cancer 2012, 131, E329–E336. [Google Scholar] [CrossRef] [PubMed]
- Carnicelli, G.; Disconzi, L.; Cerasuolo, M.; Casiraghi, E.; Costa, G.; De Virgilio, A.; Esposito, A.; Ferreli, F.; Fici, F.; Lo Casto, A.; et al. Image-Guided Intraoperative Assessment of Surgical Margins in Oral Cavity Squamous Cell Cancer: A Diagnostic Test Accuracy Review. Diagnostics 2023, 13, 1846. [Google Scholar] [CrossRef] [PubMed]
- Mazzola, R.; Ferrera, G.; Cucchiara, T.; Figlia, V.; Gueci, M.; Sciumè, F.; Di Paola, G.; Scibetta, N.; Lo Casto, A.; Pappalardo, M.P.; et al. Sequential Boost in Neoadjuvant Irradiation for T3N0-1 Rectal Cancer: Long-Term Results from a Single-Center Experience. Tumori J. 2016, 102, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Alghisi, A.; Borghetti, P.; Maddalo, M.; Roccaro, A.M.; Tucci, A.; Mazzola, R.; Magrini, S.M.; Lo Casto, A.; Bonù, M.L.; Tomasini, D.; et al. Radiotherapy for the Treatment of Solitary Plasmacytoma: 7-Year Outcomes by a Mono-Institutional Experience. J. Cancer Res. Clin. Oncol. 2021, 147, 1773–1779. [Google Scholar] [CrossRef]
- Mazzola, R.; Fersino, S.; Ferrera, G.; Targher, G.; Figlia, V.; Triggiani, L.; Pasinetti, N.; Lo Casto, A.; Ruggieri, R.; Magrini, S.M.; et al. Stereotactic Body Radiotherapy for Lung Oligometastases Impacts on Systemic Treatment-Free Survival: A Cohort Study. Med. Oncol. 2018, 35, 121. [Google Scholar] [CrossRef]
- Narita, Y.; Muro, K. Updated Immunotherapy for Gastric Cancer. J. Clin. Med. 2023, 12, 2636. [Google Scholar] [CrossRef]
- Tan, M.C.; Graham, D.Y. Screening for Gastric Cancer: Focus on the Ants Instead of the Ant Hill. Clin. Gastroenterol. Hepatol. 2021, 19, 1990–1991. [Google Scholar] [CrossRef] [PubMed]
- Nagtegaal, I.D.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, K.M.; Carneiro, F.; Cree, I.A.; The WHO Classification of Tumours Editorial Board. The 2019 WHO Classification of Tumours of the Digestive System. Histopathology 2020, 76, 182–188. [Google Scholar] [CrossRef]
- Hu, B.; El Hajj, N.; Sittler, S.; Lammert, N.; Barnes, R.; Meloni-Ehrig, A. Gastric Cancer: Classification, Histology and Application of Molecular Pathology. J. Gastrointest. Oncol. 2012, 3, 251–261. [Google Scholar] [CrossRef]
- Nagini, S. Carcinoma of the Stomach: A Review of Epidemiology, Pathogenesis, Molecular Genetics and Chemoprevention. World J. Gastrointest. Oncol. 2012, 4, 156–169. [Google Scholar] [CrossRef]
- Correa, P. Gastric Cancer: Overview. Gastroenterol. Clin. N. Am. 2013, 42, 211–217. [Google Scholar] [CrossRef]
- Tan, P.; Yeoh, K.-G. Genetics and Molecular Pathogenesis of Gastric Adenocarcinoma. Gastroenterology 2015, 149, 1153–1162.e3. [Google Scholar] [CrossRef]
- Machlowska, J.; Baj, J.; Sitarz, M.; Maciejewski, R.; Sitarz, R. Gastric Cancer: Epidemiology, Risk Factors, Classification, Genomic Characteristics and Treatment Strategies. Int. J. Mol. Sci. 2020, 21, 4012. [Google Scholar] [CrossRef]
- Keszei, A.P.; Goldbohm, R.A.; Schouten, L.J.; Jakszyn, P.; Van Den Brandt, P.A. Dietary N-Nitroso Compounds, Endogenous Nitrosation, and the Risk of Esophageal and Gastric Cancer Subtypes in the Netherlands Cohort Study. Am. J. Clin. Nutr. 2013, 97, 135–146. [Google Scholar] [CrossRef]
- Shin, C.M.; Kim, N.; Cho, S.-I.; Kim, J.S.; Jung, H.C.; Song, I.S. Association between Alcohol Intake and Risk for Gastric Cancer with Regard to ALDH2 Genotype in the Korean Population. Int. J. Epidemiol. 2011, 40, 1047–1055. [Google Scholar] [CrossRef]
- Machlowska, J.; Maciejewski, R.; Sitarz, R. The Pattern of Signatures in Gastric Cancer Prognosis. Int. J. Mol. Sci. 2018, 19, 1658. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, X.-Y.; Xu, L.; Liu, W.-J.; Zhang, J.; Zhang, J.-P. Expression and Significance of P53 and Mdm2 in Atypical Intestinal Metaplasia and Gastric Carcinoma. Oncol. Lett. 2011, 2, 707–712. [Google Scholar] [CrossRef]
- Gao, P. Alteration of Cyclin D1 in Gastric Carcinoma and Its Clinicopathologic Significance. World J. Gastroenterol. 2004, 10, 2936. [Google Scholar] [CrossRef]
- Boltin, D.; Niv, Y. Mucins in Gastric Cancer—An Update. J. Gastrointest. Dig. Syst. 2013, 3. [Google Scholar] [CrossRef]
- Sandusky, G.E.; Mintze, K.S.; Pratt, S.E.; Dantzig, A.H. Expression of Multidrug Resistance-associated Protein 2 (MRP2) in Normal Human Tissues and Carcinomas Using Tissue Microarrays. Histopathology 2002, 41, 65–74. [Google Scholar] [CrossRef]
- Ali, M.; Benfante, V.; Stefano, A.; Yezzi, A.; Di Raimondo, D.; Tuttolomondo, A.; Comelli, A. Anti-Arthritic and Anti-Cancer Activities of Polyphenols: A Review of the Most Recent In Vitro Assays. Life 2023, 13, 361. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.; Benfante, V.; Di Raimondo, D.; Salvaggio, G.; Tuttolomondo, A.; Comelli, A. Recent Developments in Nanoparticle Formulations for Resveratrol Encapsulation as an Anticancer Agent. Pharmaceuticals 2024, 17, 126. [Google Scholar] [CrossRef] [PubMed]
- Agnello, L.; Comelli, A.; Ardizzone, E.; Vitabile, S. Unsupervised Tissue Classification of Brain MR Images for Voxel-Based Morphometry Analysis. Int. J. Imaging Syst. Technol. 2016, 26, 136–150. [Google Scholar] [CrossRef]
- Vernuccio, F.; Arnone, F.; Cannella, R.; Verro, B.; Comelli, A.; Agnello, F.; Stefano, A.; Gargano, R.; Rodolico, V.; Salvaggio, G.; et al. Diagnostic Performance of Qualitative and Radiomics Approach to Parotid Gland Tumors: Which Is the Added Benefit of Texture Analysis? Br. J. Radiol. 2021, 94, 20210340. [Google Scholar] [CrossRef]
- Solomon, B.L.; Garrido-Laguna, I. Upper Gastrointestinal Malignancies in 2017: Current Perspectives and Future Approaches. Future Oncol. 2018, 14, 947–962. [Google Scholar] [CrossRef]
- Jin, X.; Liu, Z.; Yang, D.; Yin, K.; Chang, X. Recent Progress and Future Perspectives of Immunotherapy in Advanced Gastric Cancer. Front. Immunol. 2022, 13, 948647. [Google Scholar] [CrossRef]
- Feng, F.; Tian, Y.; Xu, G.; Liu, Z.; Liu, S.; Zheng, G.; Guo, M.; Lian, X.; Fan, D.; Zhang, H. Diagnostic and Prognostic Value of CEA, CA19–9, AFP and CA125 for Early Gastric Cancer. BMC Cancer 2017, 17, 737. [Google Scholar] [CrossRef]
- Song, Y.; Huang, X.; Gao, P.; Sun, J.; Chen, X.; Yang, Y.; Zhang, C.; Liu, H.; Wang, H.; Wang, Z. Clinicopathologic and Prognostic Value of Serum Carbohydrate Antigen 19-9 in Gastric Cancer: A Meta-Analysis. Dis. Markers 2015, 2015, 549843. [Google Scholar] [CrossRef]
- Kono, K.; Amemiya, H.; Sekikawa, T.; Iizuka, H.; Takahashi, A.; Fujii, H.; Matsumoto, Y. Clinicopathologic Features of Gastric Cancers Producing Alpha-Fetoprotein. Dig. Surg. 2002, 19, 359–365. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, P.; Zhang, K.; Huang, C. The Application of CA72-4 in the Diagnosis, Prognosis, and Treatment of Gastric Cancer. Biochim. Et Biophys. Acta (BBA) Rev. Cancer 2021, 1876, 188634. [Google Scholar] [CrossRef]
- Fassan, M.; Simbolo, M.; Bria, E.; Mafficini, A.; Pilotto, S.; Capelli, P.; Bencivenga, M.; Pecori, S.; Luchini, C.; Neves, D.; et al. High-Throughput Mutation Profiling Identifies Novel Molecular Dysregulation in High-Grade Intraepithelial Neoplasia and Early Gastric Cancers. Gastric Cancer 2014, 17, 442–449. [Google Scholar] [CrossRef]
- Lee, H.; Nam, K.T.; Park, H.S.; Kim, M.A.; LaFleur, B.J.; Aburatani, H.; Yang, H.; Kim, W.H.; Goldenring, J.R. Gene Expression Profiling of Metaplastic Lineages Identifies CDH17 as a Prognostic Marker in Early Stage Gastric Cancer. Gastroenterology 2010, 139, 213–225.e3. [Google Scholar] [CrossRef]
- Zhang, Q.; Yang, M.; Zhang, P.; Wu, B.; Wei, X.; Li, S. Deciphering Gastric Inflammation-Induced Tumorigenesis through Multi-Omics Data and AI Methods. Cancer Biol. Med. 2023, 21, 312. [Google Scholar] [CrossRef]
- Jeelani, S.; Jagat Reddy, R.; Maheswaran, T.; Asokan, G.; Dany, A.; Anand, B. Theranostics: A Treasured Tailor for Tomorrow. J. Pharm. Bioall. Sci. 2014, 6, 6. [Google Scholar] [CrossRef]
- Setua, S.; Jaggi, M.; Yallapu, M.M.; Chauhan, S.C.; Danilushkina, A.; Lee, H.; Choi, I.S.; Fakhrullin, R.; Esposti, L.D.; Tampieri, A.; et al. Targeted and Theranostic Applications for Nanotechnologies in Medicine. In Nanotechnologies in Preventive and Regenerative Medicine; Elsevier: Amsterdam, The Netherlands, 2018; pp. 399–511. ISBN 978-0-323-48063-5. [Google Scholar]
- Guidolin, K.; Zheng, G. Nanomedicines Lost in Translation. ACS Nano 2019, 13, 13620–13626. [Google Scholar] [CrossRef]
- Laudicella, R.; Comelli, A.; Liberini, V.; Vento, A.; Stefano, A.; Spataro, A.; Crocè, L.; Baldari, S.; Bambaci, M.; Deandreis, D.; et al. [68Ga]DOTATOC PET/CT Radiomics to Predict the Response in GEP-NETs Undergoing [177Lu]DOTATOC PRRT: The “Theragnomics” Concept. Cancers 2022, 14, 984. [Google Scholar] [CrossRef]
- Benfante, V.; Stefano, A.; Comelli, A.; Giaccone, P.; Cammarata, F.P.; Richiusa, S.; Scopelliti, F.; Pometti, M.; Ficarra, M.; Cosentino, S.; et al. A New Preclinical Decision Support System Based on PET Radiomics: A Preliminary Study on the Evaluation of an Innovative 64Cu-Labeled Chelator in Mouse Models. J. Imaging 2022, 8, 92. [Google Scholar] [CrossRef]
- Sharmiladevi, P.; Girigoswami, K.; Haribabu, V.; Girigoswami, A. Nano-Enabled Theranostics for Cancer. Mater. Adv. 2021, 2, 2876–2891. [Google Scholar] [CrossRef]
- Ghosn, M. Gastrointestinal Cancers in the Era of Theranostics: Updates and Future Perspectives. World J. Gastroenterol. 2015, 21, 8473. [Google Scholar] [CrossRef]
- Liu, Y.J.; Shen, D.; Yin, X.; Gavine, P.; Zhang, T.; Su, X.; Zhan, P.; Xu, Y.; Lv, J.; Qian, J.; et al. HER2, MET and FGFR2 Oncogenic Driver Alterations Define Distinct Molecular Segments for Targeted Therapies in Gastric Carcinoma. Br. J. Cancer 2014, 110, 1169–1178. [Google Scholar] [CrossRef]
- Bang, Y.-J.; Van Cutsem, E.; Feyereislova, A.; Chung, H.C.; Shen, L.; Sawaki, A.; Lordick, F.; Ohtsu, A.; Omuro, Y.; Satoh, T.; et al. Trastuzumab in Combination with Chemotherapy versus Chemotherapy Alone for Treatment of HER2-Positive Advanced Gastric or Gastro-Oesophageal Junction Cancer (ToGA): A Phase 3, Open-Label, Randomised Controlled Trial. Lancet 2010, 376, 687–697. [Google Scholar] [CrossRef]
- Lodhi, M.S.; Khan, M.T.; Aftab, S.; Samra, Z.Q.; Wang, H.; Wei, D.Q. A Novel Formulation of Theranostic Nanomedicine for Targeting Drug Delivery to Gastrointestinal Tract Cancer. Cancer Nanotechnol. 2021, 12, 26. [Google Scholar] [CrossRef]
- Cheng, H.; Chi, C.; Shang, W.; Rengaowa, S.; Cui, J.; Ye, J.; Jiang, S.; Mao, Y.; Zeng, C.; Huo, H.; et al. Precise Integrin-Targeting near-Infrared Imaging-Guided Surgical Method Increases Surgical Qualification of Peritoneal Carcinomatosis from Gastric Cancer in Mice. Oncotarget 2017, 8, 6258–6272. [Google Scholar] [CrossRef]
- Miyamoto, S.; Nagano, Y.; Miyazaki, M.; Nagamura, Y.; Sasaki, K.; Kawamura, T.; Yanagihara, K.; Imai, T.; Ohki, R.; Yashiro, M.; et al. Integrin A5 Mediates Cancer Cell-Fibroblast Adhesion and Peritoneal Dissemination of Diffuse-Type Gastric Carcinoma. Cancer Lett. 2022, 526, 335–345. [Google Scholar] [CrossRef]
- Hirano, T.; Shinsato, Y.; Tanabe, K.; Higa, N.; Kamil, M.; Kawahara, K.; Yamamoto, M.; Minami, K.; Shimokawa, M.; Arigami, T.; et al. FARP1 Boosts CDC42 Activity from Integrin Avβ5 Signaling and Correlates with Poor Prognosis of Advanced Gastric Cancer. Oncogenesis 2020, 9, 13. [Google Scholar] [CrossRef]
- Zhang, H.; Zhang, L.; Lu, M. Inhibition of Integrin Subunit Alpha 11 Restrains Gastric Cancer Progression through Phosphatidylinositol 3-Kinase/Akt Pathway. Bioengineered 2021, 12, 11909–11921. [Google Scholar] [CrossRef]
- Espelin, C.W.; Leonard, S.C.; Geretti, E.; Wickham, T.J.; Hendriks, B.S. Dual HER2 Targeting with Trastuzumab and Liposomal-Encapsulated Doxorubicin (MM-302) Demonstrates Synergistic Antitumor Activity in Breast and Gastric Cancer. Cancer Res. 2016, 76, 1517–1527. [Google Scholar] [CrossRef]
- Castagnoli, L.; Corso, S.; Franceschini, A.; Raimondi, A.; Bellomo, S.E.; Dugo, M.; Morano, F.; Prisciandaro, M.; Brich, S.; Belfiore, A.; et al. Fatty Acid Synthase as a New Therapeutic Target for HER2-Positive Gastric Cancer. Cell. Oncol. 2023, 46, 661–676. [Google Scholar] [CrossRef]
- Sharma, R.; Mukherjee, A.; Mitra, J.B.; Sarma, H.D. Unravelling the Potential of Lutetium-177 Labeled Pertuzumab: Targeting HER 2 Receptors for Theranostic Applications. Int. J. Radiat. Oncol. Biol. Phys. 2023, 115, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Ungureanu, B.S.; Lungulescu, C.-V.; Pirici, D.; Turcu-Stiolica, A.; Gheonea, D.I.; Sacerdotianu, V.M.; Liliac, I.M.; Moraru, E.; Bende, F.; Saftoiu, A. Clinicopathologic Relevance of Claudin 18.2 Expression in Gastric Cancer: A Meta-Analysis. Front. Oncol. 2021, 11, 643872. [Google Scholar] [CrossRef] [PubMed]
- Nishibata, T.; Weng, J.; Omori, K.; Sato, Y.; Nakazawa, T.; Suzuki, T.; Yamada, T.; Nakajo, I.; Kinugasa, F.; Türeci, Ö.; et al. Effect of Anti-Claudin 18.2 Monoclonal Antibody Zolbetuximab Alone or Combined with Chemotherapy or Programmed Cell Death-1 Blockade in Syngeneic and Xenograft Gastric Cancer Models. J. Pharmacol. Sci. 2024, 155, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Liu, S.; Yu, Y.; He, C.; Tan, L.; Shen, Y.-M. RGD Peptide-Decorated Micelles Assembled from Polymer–Paclitaxel Conjugates towards Gastric Cancer Therapy. Colloids Surf. B Biointerfaces 2019, 180, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Zhang, Q.; Alfranca, G.; Pan, S.; Huang, Z.; Cheng, J.; Ma, Q.; Song, J.; Pan, Y.; Ni, J.; et al. GSH-Triggered Sequential Catalysis for Tumor Imaging and Eradication Based on Star-like Au/Pt Enzyme Carrier System. Nano Res. 2020, 13, 160–172. [Google Scholar] [CrossRef]
- Xu, H.; Hu, C.; Wang, Y.; Shi, Y.; Yuan, L.; Xu, J.; Zhang, Y.; Chen, J.; Wei, Q.; Qin, J.; et al. Glutathione Peroxidase 2 Knockdown Suppresses Gastric Cancer Progression and Metastasis via Regulation of Kynurenine Metabolism. Oncogene 2023, 42, 1994–2006. [Google Scholar] [CrossRef]
- Chen, Z.; Hu, T.; Zhu, S.; Mukaisho, K.; El-Rifai, W.; Peng, D.-F. Glutathione Peroxidase 7 Suppresses Cancer Cell Growth and Is Hypermethylated in Gastric Cancer. Oncotarget 2017, 8, 54345–54356. [Google Scholar] [CrossRef]
- Mao, B.; Liu, C.; Zheng, W.; Li, X.; Ge, R.; Shen, H.; Guo, X.; Lian, Q.; Shen, X.; Li, C. Cyclic cRGDfk Peptide and Chlorin E6 Functionalized Silk Fibroin Nanoparticles for Targeted Drug Delivery and Photodynamic Therapy. Biomaterials 2018, 161, 306–320. [Google Scholar] [CrossRef]
- Ding, J.; Feng, M.; Wang, F.; Wang, H.; Guan, W. Targeting Effect of PEGylated Liposomes Modified with the Arg-Gly-Asp Sequence on Gastric Cancer. Oncol. Rep. 2015, 34, 1825–1834. [Google Scholar] [CrossRef]
- Wang, C.; Bao, C.; Liang, S.; Fu, H.; Wang, K.; Deng, M.; Liao, Q.; Cui, D. RGD-Conjugated Silica-Coated Gold Nanorods on the Surface of Carbon Nanotubes for Targeted Photoacoustic Imaging of Gastric Cancer. Nanoscale Res. Lett. 2014, 9, 264. [Google Scholar] [CrossRef]
- Zang, J.; Wen, X.; Lin, R.; Zeng, X.; Wang, C.; Shi, M.; Zeng, X.; Zhang, J.; Wu, X.; Zhang, X.; et al. Synthesis, Preclinical Evaluation and Radiation Dosimetry of a Dual Targeting PET Tracer [68Ga]Ga-FAPI-RGD. Theranostics 2022, 12, 7180–7190. [Google Scholar] [CrossRef]
- Akter, H.; Park, M.; Kwon, O.-S.; Song, E.J.; Park, W.-S.; Kang, M.-J. Activation of Matrix Metalloproteinase-9 (MMP-9) by Neurotensin Promotes Cell Invasion and Migration through ERK Pathway in Gastric Cancer. Tumor Biol. 2015, 36, 6053–6062. [Google Scholar] [CrossRef]
- Akter, H.; Yoon, J.H.; Yoo, Y.S.; Kang, M.-J. Validation of Neurotensin Receptor 1 as a Therapeutic Target for Gastric Cancer. Mol. Cells 2018, 41, 591–602. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Guan, R.; Lei, Y.; Chen, J.; Ge, Q.; Zhang, X.; Dou, R.; Chen, H.; Liu, H.; Qi, X.; et al. Lymphangiogenesis in Gastric Cancer Regulated through Akt/mTOR-VEGF-C/VEGF-D Axis. BMC Cancer 2015, 15, 103. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Wang, Z.; Fan, J.; Yuan, L.; Tong, C.; Zhao, Y.; Liu, B. A Hybrid Membrane Coating Nanodrug System against Gastric Cancer via the VEGFR2/STAT3 Signaling Pathway. J. Mater. Chem. B 2021, 9, 3838–3855. [Google Scholar] [CrossRef] [PubMed]
- Shu, X.; Zhan, P.-P.; Sun, L.-X.; Yu, L.; Liu, J.; Sun, L.-C.; Yang, Z.-H.; Ran, Y.-L.; Sun, Y.-M. BCAT1 Activates PI3K/AKT/mTOR Pathway and Contributes to the Angiogenesis and Tumorigenicity of Gastric Cancer. Front. Cell Dev. Biol. 2021, 9, 659260. [Google Scholar] [CrossRef] [PubMed]
- Haffner, M.C.; Kronberger, I.E.; Ross, J.S.; Sheehan, C.E.; Zitt, M.; Mühlmann, G.; Öfner, D.; Zelger, B.; Ensinger, C.; Yang, X.J.; et al. Prostate-Specific Membrane Antigen Expression in the Neovasculature of Gastric and Colorectal Cancers. Hum. Pathol. 2009, 40, 1754–1761. [Google Scholar] [CrossRef]
- Gomes, C.; Almeida, A.; Barreira, A.; Calheiros, J.; Pinto, F.; Abrantes, R.; Costa, A.; Polonia, A.; Campos, D.; Osório, H.; et al. Carcinoembryonic Antigen Carrying SLe X as a New Biomarker of More Aggressive Gastric Carcinomas. Theranostics 2019, 9, 7431–7446. [Google Scholar] [CrossRef]
- Shinmi, D.; Nakano, R.; Mitamura, K.; Suzuki-Imaizumi, M.; Iwano, J.; Isoda, Y.; Enokizono, J.; Shiraishi, Y.; Arakawa, E.; Tomizuka, K.; et al. Novel Anticarcinoembryonic Antigen Antibody–Drug Conjugate Has Antitumor Activity in the Existence of Soluble Antigen. Cancer Med. 2017, 6, 798–808. [Google Scholar] [CrossRef]
- Jin, C.; Zhang, B.-N.; Wei, Z.; Ma, B.; Pan, Q.; Hu, P. Effects of WD-3 on Tumor Growth and the Expression of Integrin Avβ3 and ERK1/2 in Mice Bearing Human Gastric Cancer Using the 18F-RGD PET/CT Imaging System. Mol. Med. Rep. 2017, 16, 9295–9300. [Google Scholar] [CrossRef]
- Alipour, M.; Baneshi, M.; Hosseinkhani, S.; Mahmoudi, R.; Jabari Arabzadeh, A.; Akrami, M.; Mehrzad, J.; Bardania, H. Recent Progress in Biomedical Applications of RGD-based Ligand: From Precise Cancer Theranostics to Biomaterial Engineering: A Systematic Review. J. Biomed. Mater. Res. 2020, 108, 839–850. [Google Scholar] [CrossRef]
- Li, X.; Yu, N.; Li, J.; Bai, J.; Ding, D.; Tang, Q.; Xu, H. Novel “Carrier-Free” Nanofiber Codelivery Systems with the Synergistic Antitumor Effect of Paclitaxel and Tetrandrine through the Enhancement of Mitochondrial Apoptosis. ACS Appl. Mater. Interfaces 2020, 12, 10096–10106. [Google Scholar] [CrossRef]
- He, Y.; Sun, M.M.; Zhang, G.G.; Yang, J.; Chen, K.S.; Xu, W.W.; Li, B. Targeting PI3K/Akt Signal Transduction for Cancer Therapy. Signal Transduct. Target. Ther. 2021, 6, 425. [Google Scholar] [CrossRef] [PubMed]
- Hou, S.; Wang, J.; Li, W.; Hao, X.; Hang, Q. Roles of Integrins in Gastrointestinal Cancer Metastasis. Front. Mol. Biosci. 2021, 8, 708779. [Google Scholar] [CrossRef]
- Badipa, F.; Alirezapour, B.; Yousefnia, H. An Overview of Radiolabeled RGD Peptides for Theranostic Applications. Curr. Radiopharm. 2023, 16, 107–122. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, D.M.; Enserro, D.M.; Mayadev, J.S.; Skeate, J.G.; Matsuo, K.; Pham, H.Q.; Lankes, H.A.; Moxley, K.M.; Ghamande, S.A.; Lin, Y.G.; et al. Immune Activation in Patients with Locally Advanced Cervical Cancer Treated with Ipilimumab Following Definitive Chemoradiation (GOG-9929). Clin. Cancer Res. 2020, 26, 5621–5630. [Google Scholar] [CrossRef]
- Speltri, G.; Porto, F.; Boschi, A.; Uccelli, L.; Martini, P. Recent Advances in Preclinical Studies of the Theranostic Agent [64Cu]CuCl2. Molecules 2024, 29, 4085. [Google Scholar] [CrossRef]
- Pous, A.; Notario, L.; Hierro, C.; Layos, L.; Bugés, C. HER2-Positive Gastric Cancer: The Role of Immunotherapy and Novel Therapeutic Strategies. Int. J. Mol. Sci. 2023, 24, 11403. [Google Scholar] [CrossRef] [PubMed]
- Gravalos, C.; Jimeno, A. HER2 in Gastric Cancer: A New Prognostic Factor and a Novel Therapeutic Target. Ann. Oncol. 2008, 19, 1523–1529. [Google Scholar] [CrossRef]
- Milatz, S.; Piontek, J.; Hempel, C.; Meoli, L.; Grohe, C.; Fromm, A.; Lee, I.M.; El-Athman, R.; Günzel, D. Tight Junction Strand Formation by Claudin-10 Isoforms and Claudin-10a/-10b Chimeras. Ann. N. Y. Acad. Sci. 2017, 1405, 102–115. [Google Scholar] [CrossRef]
- Tabariès, S.; Siegel, P.M. The Role of Claudins in Cancer Metastasis. Oncogene 2017, 36, 1176–1190. [Google Scholar] [CrossRef]
- Sentani, K.; Oue, N.; Tashiro, T.; Sakamoto, N.; Nishisaka, T.; Fukuhara, T.; Taniyama, K.; Matsuura, H.; Arihiro, K.; Ochiai, A.; et al. Immunohistochemical Staining of Reg IV and Claudin-18 Is Useful in the Diagnosis of Gastrointestinal Signet Ring Cell Carcinoma. Am. J. Surg. Pathol. 2008, 32, 1182–1189. [Google Scholar] [CrossRef]
- Zhang, D.; Huang, G.; Liu, J.; Wei, W. Claudin18.2-Targeted Cancer Theranostics. Am. J. Nucl. Med. Mol. Imaging 2023, 13, 64–69. [Google Scholar] [PubMed]
- Cheng, R.; Feng, F.; Meng, F.; Deng, C.; Feijen, J.; Zhong, Z. Glutathione-Responsive Nano-Vehicles as a Promising Platform for Targeted Intracellular Drug and Gene Delivery. J. Control. Release 2011, 152, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.; Benfante, V.; Di Raimondo, D.; Laudicella, R.; Tuttolomondo, A.; Comelli, A. A Review of Advances in Molecular Imaging of Rheumatoid Arthritis: From In Vitro to Clinic Applications Using Radiolabeled Targeting Vectors with Technetium-99m. Life 2024, 14, 751. [Google Scholar] [CrossRef]
- Waheed, S.; Tahir, M.J.; Ullah, I.; Alwalid, O.; Irshad, S.G.; Asghar, M.S.; Yousaf, Z. The Impact of Dependence on Advanced Imaging Techniques on the Current Radiology Practice. Ann. Med. Surg. 2022, 78. [Google Scholar] [CrossRef]
- Ding, Y.; Dai, Y.; Wu, M.; Li, L. Glutathione-Mediated Nanomedicines for Cancer Diagnosis and Therapy. Chem. Eng. J. 2021, 426, 128880. [Google Scholar] [CrossRef]
- Russo, G.; Stefano, A.; Alongi, P.; Comelli, A.; Catalfamo, B.; Mantarro, C.; Longo, C.; Altieri, R.; Certo, F.; Cosentino, S.; et al. Feasibility on the Use of Radiomics Features of 11[C]-MET PET/CT in Central Nervous System Tumours: Preliminary Results on Potential Grading Discrimination Using a Machine Learning Model. Curr. Oncol. 2021, 28, 5318–5331. [Google Scholar] [CrossRef]
- Giannitto, C.; Carnicelli, G.; Lusi, S.; Ammirabile, A.; Casiraghi, E.; De Virgilio, A.; Esposito, A.A.; Farina, D.; Ferreli, F.; Franzese, C.; et al. The Use of Artificial Intelligence in Head and Neck Cancers: A Multidisciplinary Survey. J. Pers. Med. 2024, 14, 341. [Google Scholar] [CrossRef]
- Christou, N.; Blondy, S.; David, V.; Verdier, M.; Lalloué, F.; Jauberteau, M.-O.; Mathonnet, M.; Perraud, A. Neurotensin Pathway in Digestive Cancers and Clinical Applications: An Overview. Cell Death Dis. 2020, 11, 1027. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, S.; Tsukada, J.; Sugimoto, T.; Kikkawa, N.; Sasaki, K.; Chazono, H.; Hanazawa, T.; Okamoto, Y.; Seki, N. Identification of a Novel Therapeutic Target for Head and Neck Squamous Cell Carcinomas: A Role for the Neurotensin-neurotensin Receptor 1 Oncogenic Signaling Pathway. Int. J. Cancer 2008, 123, 1816–1823. [Google Scholar] [CrossRef]
- Khan, I.U.; Beck-Sickinger, A.G. Targeted Tumor Diagnosis and Therapy with Peptide Hormones as Radiopharmaceuticals. Anticancer. Agents Med. Chem. 2008, 8, 186–199. [Google Scholar] [CrossRef]
- Young, K.; Smyth, E.; Chau, I. Ramucirumab for Advanced Gastric Cancer or Gastro-Oesophageal Junction Adenocarcinoma. Ther. Adv. Gastroenterol. 2015, 8, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Vara, J.Á.F.; Casado, E.; De Castro, J.; Cejas, P.; Belda-Iniesta, C.; González-Barón, M. PI3K/Akt Signalling Pathway and Cancer. Cancer Treat. Rev. 2004, 30, 193–204. [Google Scholar] [CrossRef] [PubMed]
- Pungsrinont, T.; Kallenbach, J.; Baniahmad, A. Role of PI3K-AKT-mTOR Pathway as a Pro-Survival Signaling and Resistance-Mediating Mechanism to Therapy of Prostate Cancer. Int. J. Mol. Sci. 2021, 22, 11088. [Google Scholar] [CrossRef] [PubMed]
- Chiao Deficient Histone Acetylation and Excessive Deacetylase Activity as Epigenomic Marks of Prostate Cancer Cells. Int. J. Oncol. 2009, 35, 1417–1422. [CrossRef]
- Hulsen, T. Literature Analysis of Artificial Intelligence in Biomedicine. Ann. Transl. Med. 2022, 10, 1284. [Google Scholar] [CrossRef] [PubMed]
- Giaccone, P.; Benfante, V.; Stefano, A.; Cammarata, F.P.; Russo, G.; Comelli, A. PET Images Atlas-Based Segmentation Performed in Native and in Template Space: A Radiomics Repeatability Study in Mouse Models. In Image Analysis and Processing—ICIAP 2022 Workshops; Mazzeo, P.L., Frontoni, E., Sclaroff, S., Distante, C., Eds.; Lecture Notes in Computer Science; Springer International Publishing: Cham, Switzerland, 2022; Volume 13373, pp. 351–361. ISBN 978-3-031-13320-6. [Google Scholar]
- Cairone, L.; Benfante, V.; Bignardi, S.; Marinozzi, F.; Yezzi, A.; Tuttolomondo, A.; Salvaggio, G.; Bini, F.; Comelli, A. Robustness of Radiomics Features to Varying Segmentation Algorithms in Magnetic Resonance Images. In Image Analysis and Processing—ICIAP 2022 Workshops; Mazzeo, P.L., Frontoni, E., Sclaroff, S., Distante, C., Eds.; Lecture Notes in Computer Science; Springer International Publishing: Cham, Switzerland, 2022; Volume 13373, pp. 462–472. ISBN 978-3-031-13320-6. [Google Scholar]
- Lo Casto, A.; Spartivento, G.; Benfante, V.; Di Raimondo, R.; Ali, M.; Di Raimondo, D.; Tuttolomondo, A.; Stefano, A.; Yezzi, A.; Comelli, A. Artificial Intelligence for Classifying the Relationship between Impacted Third Molar and Mandibular Canal on Panoramic Radiographs. Life 2023, 13, 1441. [Google Scholar] [CrossRef]
- Ali, M.; Benfante, V.; Cutaia, G.; Salvaggio, L.; Rubino, S.; Portoghese, M.; Ferraro, M.; Corso, R.; Piraino, G.; Ingrassia, T.; et al. Prostate Cancer Detection: Performance of Radiomics Analysis in Multiparametric MRI. In Image Analysis and Processing—ICIAP 2023 Workshops; Foresti, G.L., Fusiello, A., Hancock, E., Eds.; Lecture Notes in Computer Science; Springer Nature Switzerland: Cham, Switzerland, 2024; Volume 14366, pp. 83–92. ISBN 978-3-031-51025-0. [Google Scholar]
- Canfora, I.; Cutaia, G.; Marcianò, M.; Calamia, M.; Faraone, R.; Cannella, R.; Benfante, V.; Comelli, A.; Guercio, G.; Giuseppe, L.R.; et al. A Predictive System to Classify Preoperative Grading of Rectal Cancer Using Radiomics Features. In Image Analysis and Processing—ICIAP 2022 Workshops; Mazzeo, P.L., Frontoni, E., Sclaroff, S., Distante, C., Eds.; Lecture Notes in Computer Science; Springer International Publishing: Cham, Switzerland, 2022; Volume 13373, pp. 431–440. ISBN 978-3-031-13320-6. [Google Scholar]
- Benfante, V.; Salvaggio, G.; Ali, M.; Cutaia, G.; Salvaggio, L.; Salerno, S.; Busè, G.; Tulone, G.; Pavan, N.; Di Raimondo, D.; et al. Grading and Staging of Bladder Tumors Using Radiomics Analysis in Magnetic Resonance Imaging. In Image Analysis and Processing—ICIAP 2023 Workshops; Foresti, G.L., Fusiello, A., Hancock, E., Eds.; Lecture Notes in Computer Science; Springer Nature Switzerland: Cham, Switzerland, 2024; Volume 14366, pp. 93–103. ISBN 978-3-031-51025-0. [Google Scholar]
- Jeyamogan, S.; Khan, N.A.; Siddiqui, R. Application and Importance of Theranostics in the Diagnosis and Treatment of Cancer. Arch. Med. Res. 2021, 52, 131–142. [Google Scholar] [CrossRef]
- Gowtham, P.; Girigoswami, K.; Pallavi, P.; Harini, K.; Gurubharath, I.; Girigoswami, A. Alginate-Derivative Encapsulated Carbon Coated Manganese-Ferrite Nanodots for Multimodal Medical Imaging. Pharmaceutics 2022, 14, 2550. [Google Scholar] [CrossRef]
- Boicean, A.; Boeras, I.; Birsan, S.; Ichim, C.; Todor, S.B.; Onisor, D.M.; Brusnic, O.; Bacila, C.; Dura, H.; Roman-Filip, C.; et al. In Pursuit of Novel Markers: Unraveling the Potential of miR-106, CEA and CA 19-9 in Gastric Adenocarcinoma Diagnosis and Staging. Int. J. Mol. Sci. 2024, 25, 7898. [Google Scholar] [CrossRef]
- Benfante, V.; Stefano, A.; Ali, M.; Laudicella, R.; Arancio, W.; Cucchiara, A.; Caruso, F.; Cammarata, F.P.; Coronnello, C.; Russo, G.; et al. An Overview of In Vitro Assays of 64Cu-, 68Ga-, 125I-, and 99mTc-Labelled Radiopharmaceuticals Using Radiometric Counters in the Era of Radiotheranostics. Diagnostics 2023, 13, 1210. [Google Scholar] [CrossRef]
- Boicean, A.; Prisca, D.; Bratu, D.G.; Bacila, C.I.; Tanasescu, C.; Chicea, R.; Fleaca, S.R.; Birsan, S.A.; Ichim, C.; Mohor, C.I.; et al. Uncommon Presentation of Gastric Duplication Cyst with Left-Sided Portal Hypertension: A Case Report and Literature Review. Diagnostics 2024, 14, 675. [Google Scholar] [CrossRef] [PubMed]
- Conti, C.B.; Agnesi, S.; Scaravaglio, M.; Masseria, P.; Dinelli, M.E.; Oldani, M.; Uggeri, F. Early Gastric Cancer: Update on Prevention, Diagnosis and Treatment. Int. J. Environ. Res. Public Health 2023, 20, 2149. [Google Scholar] [CrossRef] [PubMed]
| Targeting Site | Major Finding | Key Results | Ref. |
|---|---|---|---|
| Integrin Receptors | Developed RGD-ICG molecular probe for better gastric cancer diagnostics and surgery. | Achieved 93.93% diagnostic accuracy, reduced tumor size, and operative time. | [44] |
| Targeted integrin α5 to prevent the spread of diffuse gastric carcinoma (DGC). | Blocking integrin α5 reduced cancer invasion and peritoneal spread in mice. | [45] | |
| Found integrin αvβ5 and FARP1 promote cancer cell motility and spread. | Blocking FARP1 reduced cancer cell motility by reducing CDC42 activation. | [46] | |
| Investigated ITGA11’s role in PI3K/AKT signaling in gastric cancer. | ITGA11 knockdown reduced cell proliferation and migration, increased apoptosis. | [47] | |
| HER2 | Combined trastuzumab and MM-302 for enhanced HER2-targeted antitumor effects. | Strong antitumor effects observed, planned for phase II clinical trial. | [48] |
| FASN inhibition helped overcome trastuzumab resistance in HER2-positive gastric cancer. | FASN inhibitors with trastuzumab reduced cancer stem cells and tumor growth. | [49] | |
| Lu177-radiolabeled pertuzumab used for theranostic applications targeting HER2 in gastric cancer. | Effective binding and internalization of HER2 receptors for PET radiopharmaceuticals. | [50] | |
| Claudin 18 | Zolbetuximab targets CLDN18.2 to induce ADCC and CDC in gastric cancer cells. | Zolbetuximab effectively destroyed CLDN18.2-expressing cancer cells. | [51] |
| Zolbetuximab tested in CLDN18.2-positive gastric cancer in vitro and in vivo. | Inhibited tumor growth, especially when combined with chemotherapy and anti-mPD-1 therapy. | [52] | |
| Glutathione | Developed GSH-responsive PEG–PTX micelles for targeted drug delivery in gastric cancer. | Micelles blocked tumor growth in vitro and in vivo with minimal side effects. | [53] |
| Developed GSH-sensitive nanoparticles for phototherapy in gastric cancer. | Accurate tumor targeting, real-time imaging, and therapy demonstrated. | [54] | |
| Studied GPx2’s role in gastric cancer metastasis and progression. | GPx2 knockdown reduced tumor growth and metastasis by inhibiting EMT and ROS accumulation. | [55] | |
| Investigated GPX7 downregulation in gastric cancer. | GPX7 restoration suppressed tumor growth and induced cancer cell death. | [56] | |
| Cyclic RGD Peptide | Developed cRGDyk-tagged silk fibroin nanoparticles for drug delivery and photodynamic therapy. | Nanoparticles reduced tumor size in mice with good biocompatibility and safety. | [57] |
| Created RGD-PLS-ICG liposomes for targeted drug delivery in gastric cancer cells. | Effective targeting of cancer cells and improved imaging using the system. | [58] | |
| Developed RGD-conjugated gold nanorods for NIR absorption and PA imaging. | Probes targeted gastric cancer cells, enhancing imaging accuracy in vivo. | [59] | |
| [68Ga]Ga-FAPI-RGD Compared heterodimeric PET radiotracer with RGD monospecific tracers for gastric cancer imaging. | Improved tumor uptake and retention, showing potential for theranostic applications | [60] | |
| Neurotensin Receptors | Investigated NT’s role in promoting MMP-9 activity in gastric cancer. | Blocking NTSR1 reduced MMP-9 activity, cell invasion, and migration. | [61] |
| NTSR1 mRNA, studied elevated NTSR1 mRNA levels promoting GC metastasis | Blocking NTSR1 decreased cancer cell invasion and metastasis. | [62] | |
| Angiogenesis | Investigated p-Akt and p-mTOR inhibitors targeting VEGF-C/-D in gastric cancer. | Blocking Akt/mTOR pathway reduced lymphangiogenesis and tumor growth. | [63] |
| Developed pH-responsive liposomes for delivering apatinib and cinobufagin for gastric cancer therapy. | Liposomes induced apoptosis and autophagy, reducing tumor metastasis in mouse models. | [64] | |
| Explored BCAT1’s role in angiogenesis and tumor growth in gastric cancer | BCAT1 knockdown decreased tumor growth and angiogenesis. | [65] | |
| Studied PSMA-targeting strategies for gastric cancer neovasculature. | PSMA-targeting offers a complementary approach to antiangiogenic therapy. | [66] | |
| Carcinoembryonic Antigen (CEA) | SLex co-expressed with CEA promoted metastasis and tumor growth in gastric cancer. | CEA-SLex conjugates correlated with lower survival and advanced tumor progression. | [67] |
| Developed a novel anti-CEA antibody conjugated with monomethyl auristatin E for gastric cancer therapy. | Antibody showed enhanced binding to membrane-bound CEA and improved antitumor activity in vivo. | [68] |
| Data Description | Quantitative Result | Statistical Significance | Experimental Model | Ref. |
|---|---|---|---|---|
| Zolbetuximab in CLDN18.2+ GC | Tumor growth inhibition by 91% when combined with chemotherapy | p < 0.05 | NUGC-4, KATO-III, CLS-103 GC cell lines, xenograft models | [52] |
| Diagnostic Accuracy with RGD-ICG Probe | 93.93% diagnostic accuracy, reduced operative time by 3.26 times | p < 0.05 | Mouse xenograft model | [44] |
| FASN Inhibition in Trastuzumab Resistance | FASN inhibition reduced cancer stem cells by 40% and tumor growth by 30% | p < 0.05 | HER2+ GC cell lines | [49] |
| FARP1’s Role in Cell Motility | FARP1 overexpression increased motility by p = 0.025 survival rate | p < 0.05 | Human GC cell lines (MKN74, MKN45) | [46] |
| Integrin α5 Blockade in DGC | Cancer invasion and peritoneal spread reduced by 50% | p < 0.05 | Mouse xenograft model | [45] |
| Glutathione-Sensitive Micelles for Drug Delivery | Tumor growth inhibited by 96.8% | p < 0.01 | Mouse xenograft models | [53] |
| GPx2 Knockdown in GC | Reduced tumor growth by 40% and metastasis by 50% | p < 0.05 | Gastric cancer xenograft models | [55] |
| Neurotensin Receptor Blockade | Reduced MMP-9 activity by 30% and decreased metastasis | p < 0.05 | MKN-45, MKN-1 GC cells | [62] |
| Clinical Trials | Targeted Agent | Biomarker | Stage | Objective | Outcome Measured | Ref. |
|---|---|---|---|---|---|---|
| HER2+ Gastric Cancer Treatment | Trastuzumab + MM-302 | HER2 | Phase II | Test combined therapy to enhance HER2 targeting in gastric cancer | Tumor size reduction, overall survival (OS), progression-free survival (PFS) | [48] |
| Dual HER2 Targeting in Advanced Gastric Cancer | Lu177-radiolabeled Pertuzumab + Trastuzumab | HER2 | Phase I/II | Assess dual HER2-targeting for enhanced radioimmunotherapy | Radiographic response, tumor shrinkage, progression-free survival (PFS) | [50] |
| Integrin αvβ5 in Diffuse Gastric Carcinoma | Monoclonal antibody blocking integrin α5 | Integrin α5 | Phase I | Prevent peritoneal spread of diffuse gastric carcinoma (DGC) | Cancer invasion rates, peritoneal spread, patient safety/tolerability | [45] |
| RGD-ICG Molecular Probe for Gastric Cancer Surgery | RGD-ICG nanoprobe | Integrin αvβ3 | Phase II | Improve diagnostic accuracy and reduce surgical time in gastric cancer | Tumor resection accuracy, operative time, post-surgical recovery | [44] |
| Integrin β5-Targeting to Reduce Cancer Cell Motility | Monoclonal antibody against integrin β5 | Integrin β5/FARP1 | Phase I | Block FARP1–integrin axis to reduce motility and metastasis in GC | Cell motility, metastasis-free survival, adverse events | [46] |
| Zolbetuximab in Combination with Immunotherapy | Zolbetuximab + anti-PD-1 therapy | Claudin 18.2 | Phase II/III | Evaluate enhanced immune response when combined with PD-1 inhibitors | Tumor immune infiltration, response rates, overall survival (OS) | [52] |
| Neurotensin Receptor Blockade | NTSR1 antagonist | Neurotensin receptor (NTSR1) | Phase I | Reduce MMP-9-mediated invasion and metastasis | Metastasis rate, MMP-9 activity, NTSR1 expression changes | [62] |
| Gold-Platinum Star Nanoparticles for Imaging and Therapy | Au/Pt nanostars + IR780 phototherapy | Glutathione | Phase I | Use GSH-sensitive nanoparticles for combined imaging and phototherapy | Tumor targeting accuracy, toxicity, phototherapy success rate | [54] |
| GPx2 Knockdown to Inhibit Metastasis | GPx2 siRNA therapy | GPx2 | Phase I | Inhibit ROS-mediated metastasis through GPX2 knockdown | Metastasis reduction, ROS accumulation, progression-free survival | [55] |
| PSMA-Targeted Theranostic Approach | PSMA-targeting radiopharmaceuticals | PSMA in tumor neovasculature | Phase I/II | Improve theranostic imaging and antiangiogenic therapy in gastric cancer | Tumor blood vessel targeting, imaging accuracy, therapeutic efficacy | [66] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Basirinia, G.; Ali, M.; Comelli, A.; Sperandeo, A.; Piana, S.; Alongi, P.; Longo, C.; Di Raimondo, D.; Tuttolomondo, A.; Benfante, V. Theranostic Approaches for Gastric Cancer: An Overview of In Vitro and In Vivo Investigations. Cancers 2024, 16, 3323. https://doi.org/10.3390/cancers16193323
Basirinia G, Ali M, Comelli A, Sperandeo A, Piana S, Alongi P, Longo C, Di Raimondo D, Tuttolomondo A, Benfante V. Theranostic Approaches for Gastric Cancer: An Overview of In Vitro and In Vivo Investigations. Cancers. 2024; 16(19):3323. https://doi.org/10.3390/cancers16193323
Chicago/Turabian StyleBasirinia, Ghazal, Muhammad Ali, Albert Comelli, Alessandro Sperandeo, Sebastiano Piana, Pierpaolo Alongi, Costanza Longo, Domenico Di Raimondo, Antonino Tuttolomondo, and Viviana Benfante. 2024. "Theranostic Approaches for Gastric Cancer: An Overview of In Vitro and In Vivo Investigations" Cancers 16, no. 19: 3323. https://doi.org/10.3390/cancers16193323
APA StyleBasirinia, G., Ali, M., Comelli, A., Sperandeo, A., Piana, S., Alongi, P., Longo, C., Di Raimondo, D., Tuttolomondo, A., & Benfante, V. (2024). Theranostic Approaches for Gastric Cancer: An Overview of In Vitro and In Vivo Investigations. Cancers, 16(19), 3323. https://doi.org/10.3390/cancers16193323













